Abstract
Eagle syndrome (ES) is a rare clinical syndrome characterized by the elongation of the temporal bone's styloid process, or calcification of stylohyoid ligament, compressing surrounding structures causing pharyngalgia. One of its variants, the styloid-carotid artery syndrome, produces symptoms by compression of the external or internal carotid arteries (ICA). Here, we present a case of a 43-year-old woman with ES and bilateral ICA dissections. The patient underwent staged bilateral angioplasty and covered stent placement, followed by styloidectomy. A computerized tomography angiogram revealed patency of both stents at a two-year follow-up.
Keywords: Eagle syndrome, Bilateral carotid dissection, Styloid-carotid artery syndrome, Elongated styloid process
Highlights
-
•
Bilateral carotid artery dissection due to Eagle Syndrome is extremely rare.
-
•
Limited evidence exists on the management of styloid-carotid artery syndrome.
-
•
There is a strong male predominance and high rates of infarcts on this entity.
-
•
Endovascular treatment in the acute phase may help reduce new/recurrent strokes.
1. Background
Eagle syndrome (ES) is a rare condition characterized by the elongation of the temporal bone's styloid process, or calcification of stylohyoid ligament, compressing surrounding cervical structures causing pharyngalgia [1]. A prolonged styloid process is approximately present in 4.0–7.3% of the population, but only a small percentage exhibits symptoms, hence ES [2]. The styloid-carotid artery syndrome, a variant of the ES, is defined by the carotid arteries' mechanical compression, more commonly the internal carotid artery (ICA) [1,2]. Given its rarity, a paucity of evidence exists on the management of styloid-carotid artery syndrome, mainly when associated with carotid dissections.
2. Case report
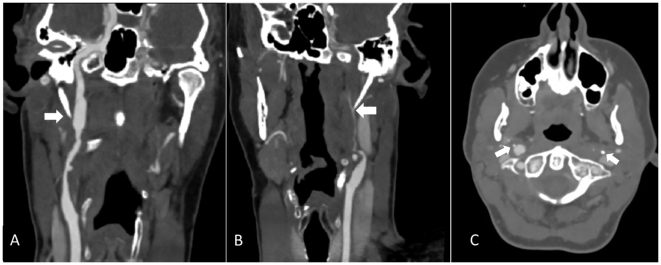
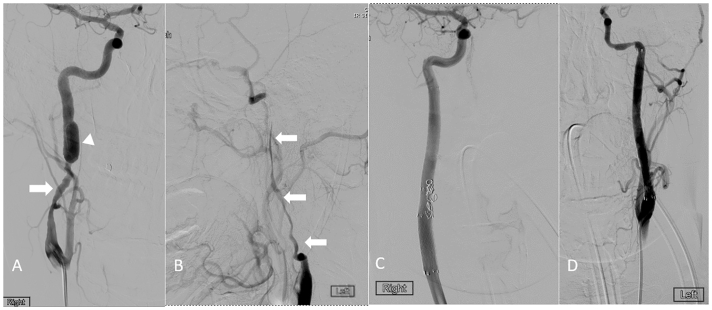
A 43-year-old female with no significant past medical history was admitted to evaluate new-onset headaches over the left temporal and periorbital regions, associated to generalized pharyngalgia. The patient denied recent head trauma. An initial neurological exam demonstrated a preganglionic left-sided Horner's syndrome. A non-contrast computed tomography (CT) of the head was unrevealing. A Magnetic Resonance Imaging (MRI) demonstrated a dissection of the left ICA at the cervical segment. A subsequent CT Angiography (CTA) of the head and neck confirmed a long-segment dissection of the cervical left ICA beginning rostral to the carotid bifurcation with near-total occlusion of the distal left ICA segment and also showed a large right ICA pseudoaneurysm in the distal cervical segment. We identified an elongated styloid process abutting the diseased carotid segments (Fig. 1). A digital subtraction angiography confirmed the results (Fig. 2A, B). Angioplasty was followed by stenting the bilateral ICAs with Fluency (BARD™ Tempe, Arizona) covered stents. We treated the right carotid artery with two tandemly placed stents extending from the right common to the right ICA (7 × 60 and 8 × 40 mm). Two days later, we performed angioplasty and stenting of the left ICA with a single covered stent (6 × 80 mm) (Fig. 2C, D).
Fig. 1.
Curved planar reformatted CTA showing (A) pseudoaneurysmal dilatation of right ICA (arrow) and (B) stenosis of left ICA from dissection (arrow). (C) Axial plane shows tips of elongated styloid process (arrows) abutting ICAs bilaterally.
Fig. 2.
Digital subtraction angiography: (A) Antero-posterior view of the right ICA stenosis (arrow) and pseudoaneurysm (arrowhead). (B) Antero-posterior view of the left ICA with near complete occlusion of the lumen. (C) and (D) shows recanalization of the flow in the right and left internal carotid arteries post-stenting respectively.
Upon initial diagnosis, we initiated full-dose enoxaparin, which was transitioned to aspirin and clopidogrel following carotid stenting. Otolaryngology performed elective styloidectomies of the right then left styloid processes at 5 and 8 months, respectively, following discharge. Genetic screening for soft tissue disease was negative. A one-year MRI demonstrated a small T2 hyperintensity in the left centrum semiovale concerning for a silent infarct. Two years following her initial presentation, the patient continued to have headaches, remained neurological intact, and a follow-up CTA demonstrated bilateral stent patency.
3. Discussion
The styloid process' average length is between 2 and 3 cm, and it is deemed elongated when greater than 3 cm [1]. Symptoms associated with an elongated styloid process are thought to be related to the impingement of soft tissue or neurovascular structures in the neck [2]. Eagle syndrome may cause carotid artery disease, including vessel stenosis, artery dissection, or pseudoaneurysm, and may be complicated by cerebrovascular events [3]. Bilateral carotid dissection from ES is rare, and only a few cases are reported in the available literature (Supplementary Table 1) [[3], [4], [5], [6], [7], [8], [9], [10], [11], [12]]. As previously reported, there exists a strong male predominance on carotid dissection cases secondary to ES [3]. To our knowledge, our case is the only female case and the youngest patient without an identified connective tissue disorder who presented with bilateral carotid dissection secondary to ES.
Previous case series have documented high rates of recurrent infarcts in patients with ICA dissection secondary to ES [9]. We identified 12 cases of bilateral carotid dissection secondary to ES [[3], [4], [5], [6], [7], [8], [9], [10], [11], [12]]. Of the cases identified, 7 documented an acute ischemic strokes on admission [4,5,[7], [8], [9], [10],12]. Nine cases were treated medically or with thrombectomy on arrival, and five of them ended up having new or recurrent cerebrovascular events [[3], [4], [5],7,8,[10], [11], [12]]. Only two cases were identified where acute carotid artery stenting was performed, including our case [9]. To our knowledge, our patient is the first case described of bilateral angioplasty followed by covered stents placement as initial management.
Bilateral styloidectomy [7,9,11], unilateral styloidectomy [8,11], and C1 transverse process removal [10] were reported in the revised cases. It remains unknown if styloidectomy mitigates the future risk of carotid artery injury or cerebrovascular accidents. In our case, carotid stenting followed by styloidectomy led to improved neck pain, but the effect on the patient's headache was minimal.
4. Conclusion
Eagle syndrome is a rare cause of bilateral internal carotid artery dissection. Given the significant cerebrovascular consequences and recurrence of this condition's events, physicians need to be aware of this rare disease. Limited information is available about the acute and long-term management of carotid artery dissection secondary to ES. Treatment with endovascular procedures in the acute phase, followed by elective styloidectomy, may help reduce the chance of new or recurrent devastating vascular complications.
The following is the supplementary data related to this article.
Summary of reported cases of bilateral carotid artery dissection caused by an elongated styloid process.
Funding
The research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional ethics committee clearance
Not applicable.
Contributors
W.D., D.J., and G.N. reviewed the literature, and W.D., D.J., G.N., and T.W. contributed to the to the writing of the report.
Declaration of Competing Interest
None.
Contributor Information
Walter R. Duarte-Celada, Email: wr.duarte-celada@ttuhsc.edu.
Dongkwan Jin, Email: dongkwan.jin@ttuhsc.edu.
Gabriel Neves, Email: gabriel.neves@ttuhsc.edu.
Thomas Windisch, Email: twindisch@covhs.org.
References
- 1.Eagle W.W. Elongated styloid process; symptoms and treatment. AMA Arch. Otolaryngol. 1958;67:172–176. doi: 10.1001/archotol.1958.00730010178007. [DOI] [PubMed] [Google Scholar]
- 2.Badhey A., Jategaonkar A., Anglin Kovacs A.J., Kadakia S., De Deyn P.P., Ducic Y. Eagle syndrome: a comprehensive review. Clin. Neurol. Neurosurg. 2017;159(May 2017):34–38. doi: 10.1016/j.clineuro.2017.04.021. [DOI] [PubMed] [Google Scholar]
- 3.Zammit M., Chircop C., Attard V., D’Anastasi M. Eagle’s syndrome: a piercing matter. BMJ Case Rep. 2018;11(1) doi: 10.1136/bcr-2018-226611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faivre A., Abdelfettah Z., Rodriguez S., Nicoli F. Bilateral internal carotid artery dissection due to elongated styloid processes and shaking dancing. J. Neurol. Neurosurg. Psychiatry. 2009;80(10):1154–1155. doi: 10.1136/jnnp.2008.159954. [DOI] [PubMed] [Google Scholar]
- 5.Todo T., Alexander M., Stokol C., Lyden P., Braunstein G., Gewertz B. Eagle syndrome revisited: Cerebrovascular complications. Ann. Vasc. Surg. 2012;26(5) doi: 10.1016/j.avsg.2011.12.005. 729.e1–729.e5. [DOI] [PubMed] [Google Scholar]
- 6.Vodopivec I., Klein J.P., Prasad S. Bilateral cervical internal carotid artery dissections in Eagle syndrome. Neurol. Clin. Pract. 2013;3(2):173–174. doi: 10.1212/CPJ.0b013e31828d9fdb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naito Y., Yamazaki K. Perioperative management of Eagle syndrome complicated by cartoid artery dissection. J. Anesth. 2014;28:291–293. doi: 10.1007/s00540-013-1713-6. [DOI] [PubMed] [Google Scholar]
- 8.Ogura T., Mineharu Y., Todo K., Kohara N., Sakai N. Carotid artery dissection caused by an elongated styloid process: three case reports and review of the literature. NMC Case Rep. J. 2015;2(1):21–25. doi: 10.2176/nmccrj.2014-0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Torikoshi S., Yamao Y., Ogino E., Taki W., Sunohara T., Nishimura M. A staged therapy for internal carotid artery dissection caused by vascular eagle syndrome. World Neurosurg. 2019;129:133–139. doi: 10.1016/j.wneu.2019.05.208. [DOI] [PubMed] [Google Scholar]
- 10.Galletta K., Granata F., Longo M., Alafaci C., de Ponte F.S., Squillaci D. An unusual internal carotid artery compression as a possible cause of Eagle syndrome – A novel hypothesis and an innovative surgical technique. Surg. Neurol. Int. 2019;10(174):1–4. doi: 10.25259/SNI_317_2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baldino G., Di Girolamo C., De Blasis G., Gori A. Eagle syndrome and internal carotid artery dissection: description Of 5 cases treated in two italian institutions and review of the literature. Ann. Vasc. Surg. 2020;67 doi: 10.1016/j.avsg.2020.02.033. 565.e17–565.e24. [DOI] [PubMed] [Google Scholar]
- 12.Ikenouchi H., Takagi M., Nishimura A., Yamaguchi E., Koge J., Saito K. Bilateral carotid artery dissection due to Eagle syndrome in a patient with vascular Ehlers-Danlos syndrome : a case report. BMC Neurol. 2020;20:285. doi: 10.1186/s12883-020-01866-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Summary of reported cases of bilateral carotid artery dissection caused by an elongated styloid process.