Abstract
Purpose
The Westlake BioBank for Chinese (WBBC) pilot cohort is a population-based prospective study with its major purpose to better understand the effect of genetic and environmental factors on growth and development from adolescents to adults.
Participants
A total of 14 726 participants (4751 males and 9975 females) aged 14–25 years were recruited and the baseline survey was carried out from 2017 to 2019. The pilot cohort contains rich range of information regarding of demographics and anthropometric measurements, lifestyle and sleep patterns, clinical and health outcomes. Visit the WBBC website for more information (https://wbbc.westlake.edu.cn/index.html).
Findings to date
The mean age of the study samples were 18.6 years for males and 18.5 years for females, respectively. The mean height and weight were 172.9 cm and 65.81 kg for males, and 160.1 cm and 52.85 kg for females. Results indicated that the prevalence of underweight in female was much higher than male, but the prevalence of overweight and obesity in female was lower than male. The mean serum 25(OH)D level in the 14 726 young participants was 22.4±5.3 ng/mL, and male had a higher level of serum 25(OH)D than female, overall, 33.5% of the participants had vitamin D deficiency and even more participants suffered from vitamin D insufficiency (58.2%). The proportion of deficiency in females was much higher than that in males (41.8 vs 16.4%). The issue of underweight and vitamin D deficiency in young people should be paid attention, especially in females. These results reflected the fact that thinness and paler skin are preferred in modern aesthetics of Chinese culture.
Future plans
WBBC pilot is designed as a prospective cohort study and provides a unique and rich data set analysing health trajectories from adolescents to young adults. WBBC will continue to collect samples with old age.
Keywords: epidemiology, nutrition & dietetics, health informatics
Strengths and limitations of this study.
This is a comprehensive cohort study to pay attention to the health of adolescence and young adults, including over ~14 000 participants.
The Westlake BioBank for Chinese (WBBC) pilot cohort is rich in longitudinal phenotypic data and archived biospecimens, including whole blood and serum as well as DNA samples. These resources will facilitate to digitise the information of the genomic, proteomic and metabolomic and microbiome of the participants.
Although the participants covered all around the country, most of them were mainly from three provinces (Jiangxi, Shandong and Zhejiang), and the selection of participants was not random.
The participants were collected in three phases at different time points; the phenotypic data were not always uniform in three phases.
Introduction
The Westlake BioBank for Chinese (WBBC) cohort is a population-based prospective study with its major purpose to better understand the effect of genetic and environmental factors on growth and development from adolescents to adults. WBBC is designed as a large-scale cohort with its aim to recruit at least 100 000 Chinese samples at different age. The pilot project of WBBC has focused on the study on the young population (Late adolescence), and has already collected a wide range of information including demographics and anthropometric measures, serological tests, physical activity, sleep quality, age at menarche, bone mineral density and so on. The main purpose of this particular paper is to profile the cohort; therefore, only limited findings were reported and few questions were asked, for example (1) what is the prevalence of underweight, overweight, obesity and vitamin D deficiency in Chinese late adolescence? What is the reference value of serum vitamin D level in the young people? (2) What is the difference between male and female in term of height, weight, blood pressure, lifestyle and bone health in the young people.
It is known that adolescence is a period of life with marked psychosocial, behavioural and biological changes1; therefore, monitoring the trajectories of health-risk behaviours in adolescents is one of the important concerns of public health. Among health problems during adolescence, overweight and obesity are highly prevalent.2 3 Following the rapid economic development since the 1980s, China experiences a rapidly increasing of overweight and obesity among children and adolescents.4 5 In 2019, a cross-sectional study6 found that the prevalence of overweight in college students (aged 18–26 years) was 8.0%, and the prevalence of obesity was 3.5%. A recent study from 12 provinces in China showed that the prevalence of overweight and obesity were 14.0% and 10.5% in boys, and 9.7% and 7.1% in girls, respectively.7 And obesity, in adolescence conferred very high risks for obesity in adults2; 70% of overweight adolescents had one or more concomitant conditions such as high blood pressures and fasting insulin, which were also risk factors for cardiovascular disease, and 23% of those accompanied with three or more concomitant conditions.8 Further, elevated body mass index (BMI) in adolescence had been associated with several obesity-related morbidities in adult life, such as diabetes, metabolic syndromes and some types of cancer.9 However, little is known about how underweight or severe low BMI could affect the health in adolescence, what are the long-term medical consequences. In adolescents, underweight was reported to be associated with scoliosis,10 pubertal delay11 and psychiatric disorders.12 Therefore, in this study, it is also important to recognise the issue of underweight in adolescents.
Hypovitaminosis D in children and adolescents is another re-emerging public health problem.13 Besides its effect on the musculoskeletal system, vitamin D showed a pleiotropic effect on human health, such as cardiovascular diseases,14 common infectious diseases15 and autoimmune diseases.16 Serum 25(OH)D is a good indicator of vitamin D storage and is an optimal method of assessing vitamin D levels.17 According to the Endocrine Society clinical practice guidelines, vitamin D levels were defined as a deficiency [25(OH)D<20 ng/mL], insufficiency [25(OH)D: 20–29 ng/mL)] and sufficiency [25(OH)D≥30 ng/mL], respectively.18 Many people in central and western Europe had vitamin D concentration of 11–20 ng/mL in winter.19 Studies from other countries, including Canada,20 Japan,21 Australia22 and Iran,23 presented similar situations, with high prevalence of vitamin D insufficiency in different ethnicities. A study in northern China found that more than 40% of adolescent girls had vitamin D-deficient in the winter.24 Another study in Shanghai showed that more than one-third newborns had plasma 25(OH)D less than 20 ng/mL.25 Even in Hong Kong (latitude 22° north), 72% of young adults were reported to have vitamin D deficiency.26 To the best of our knowledge, there was no large survey to assess levels of vitamin D deficiency in adolescents in China mainland; however, findings from some surveys suggest that vitamin D deficiency is prevalent in young people.26–28 Moreover, the problem of vitamin D deficiency among young people in China has not been paid sufficient attention.
The overall goal of the WBBC pilot cohort is to recruit individuals at their late adolescence/young adulthood. The biological samples such as whole blood, serum, urine and faeces were collected, genomic DNA was extracted and the DNA sequence information was acquired through sequencing technique. A long questionnaire with questions concerning the environmental factors such as nutrition, sleep quality, physical activity, medication, and so on, was provided. These data will help us to understand the association between the genetics, environmental factors, microbiome and health statue of adolescence population. With a broad range of phenotype collection on many aspects of participants’ daily life, a wide range of scientific questions could be addressed.
Cohort description
Sampling design
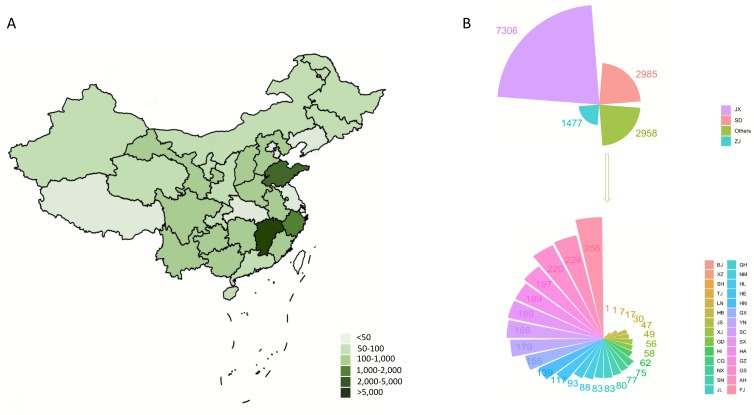
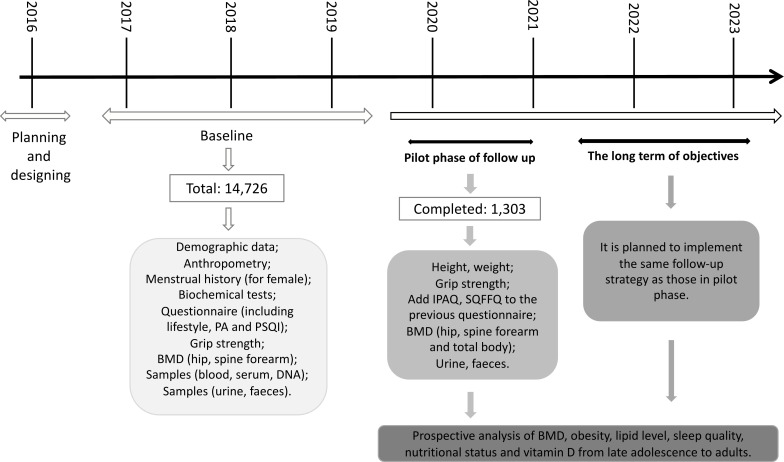
The WBBC pilot study was collected in three main regions in China (Zhejiang province, Jiangxi province and Shandong province), but the participants covered all around the country (table 1 and figure 1). The baseline survey was carried out from 2017 to 2019. The target population was young people aged 14–25 years who were college students and available for follow-up studies. In the first phase of baseline (WBBC pilot 1), the participants were recruited from two colleges at Zhejiang province and Jiangxi province in Southeast China from September 2017 to March 2018 (figure 2), and 1258 and 2769 participants were from Zhejiang and Jiangxi provinces, respectively, and 1263 participants were from other 25 provinces of China (table 1). From September 2018 to December 2018, the second phase of WBBC pilot project was initiated (WBBC pilot 2), the participants were recruited at the same college in Jiangxi province and a college in Shandong province in Northeast China (figure 2). There were 2920 participants from Shandong province, 2032 participants from Jiangxi province and 1306 participants from other 28 provinces of China in WBBC pilot 2 (table 1). From September 2019, the WBBC pilot project phase 3 (WBBC pilot 3) recruited participants from the same college in Jiangxi province (figure 2), most of the participants (2,504) of WBBC pilot 3 were from Jiangxi province and 674 participants were from other 26 provinces of China (table 1). All participants provided their Chinese unique national identity (ID) number for unique reference at the health examination centre in the campus. The inclusion criteria were: (1) All study participants signed the informed consent form before taking part in the survey; (2) participants should complete the physical examination, and should finish at least one of other items including bone mineral density scan, blood test and questionnaire. And the exclusion criteria were: (1) age <14 year old or >25 year old; (2) participants have taken drugs which could affect bone metabolism (eg, glucocorticoids); (3) participants have illness which could cause secondary osteoporosis (eg, hyperparathyroidism). In WBBC pilot 3, the urine and faeces of the participants were collected; therefore, participants taking antibiotics should be excluded.
Table 1.
The participants of the cohort at baseline
| Year | Phase | Area | Total | Sex | |
| Male | Female | ||||
| 2017 | WBBC pilot 1 | Zhejiang province | 1258 | 460 | 798 |
| Jiangxi province | 2769 | 862 | 1907 | ||
| Other 25 provinces | 1263 | 336 | 927 | ||
| 2018 | WBBC pilot 2 | Shandong province | 2920 | 1115 | 1805 |
| Jiangxi province | 2032 | 578 | 1454 | ||
| Other 28 provinces | 1306 | 438 | 868 | ||
| 2019 | WBBC pilot 3 | Jiangxi province | 2504 | 761 | 1743 |
| Other 26 provinces | 674 | 201 | 473 | ||
| Total | 14726 | 4751 | 9975 | ||
WBBC, Westlake BioBank for Chinese.
Figure 1.
Maps showing the sources of the samples in the Westlake BioBank for Chinese (WBBC) pilot cohort. (A) provides a range of sample size in each province with different colour, and (B) provides the exact number of sample size in each province. AH, Anhui province; BJ, Beijing; CQ, Chongqing; FJ, Fujian province; GD, Guangdong province; GS, Gansu province; GX, Guangxi Autonomous Region; GZ, Guizhou province; HA, Henan province; HB, Hubei province; HE, Hebei province; HI, Hainan province; HL, Heilongjiang province; HN, Hunan province; JL, Jilin province; JS, Jiangsu province; JX, Jiangxi province; LN, Liaoning province; NM, Neimeng Autonomous Region; NX, Ningxia Autonomous Region; QH, Qinghai province; SC, Sichuang province; SD, Shandong province; SH, Shanghai; SN, Shanxi province; SX, Shanxi province; TJ, Tianjin; XJ, Xinjiang Autonomous Region; XZ, Xizang Autonomous Region; YN, Yunnan province; ZJ, Zhejiang province.
Figure 2.
Data collection timeline. IPAQ, International Physical Activity Questionnaire; PA, Physical Activity; PSQI, Pittsburgh Sleep Quality Index; SQFFQ, Semi-Quantitative Food Frequency Questionnaire.
Data collection procedures
The WBBC pilot study is a multidisciplinary study and contains a rich range of information regarding of demographics, anthropometric measurements, blood pressure and heart rate (HR), lifestyle and sleep patterns, biological, clinical and health outcomes. Data and samples were collected via examinations, questionnaire and venipuncture (table 2).
Table 2.
Summary of data collected in the Cohort
| Measures | Instruments |
| Anthropometry* | |
| Height and weight, bust, waist, hip and thigh circumference | |
| Strength | |
| Grip strength (right and left hand) | |
| Cardiovascular system | |
| Blood pressure (SBP and DBP), heart rate | |
| Bone mineral density | |
| Lumar spine, hip and forearm | |
| Questionnaires | |
| Demographic data | Age, sex, ethnicity, family economic status, birthplace |
| Menstrual history (for female) | Age of menarche, gynaecological disease history |
| Sleeping situation | Pittsburgh Sleep Quality Index, PSQI |
| Lifestyle | Smoking status, alcohol, tea and coffee consumption, exercise |
| Supplementations | Calcium, vitamin D |
| Health status | Medical history and medications |
| Physical activity† | International Physical Activity Questionnaire, IPAQ |
| Dietary pattern† | Semi-Quantitative Food Frequency Questionnaire (SQFFQ) |
| Routine biochemistry and Haematology | |
| Lipid metabolism | Total cholesterol, triglycerides, HDL-cholesterol, LDL-cholesterol |
| Kidney-related measures | Uric acid, creatinine and urea |
| Hepatic-related measures | Alanine aminotransferase, glutamic oxaloacetylase, |
| total bilirubin, direct bilirubin, albumin, globulin | |
| Thyroid and parathyroid function | TSH, PTH, T3, T4, FT3, FT4, |
| Routine diabetes test | Fasting plasma glucose, glycosylated haemoglobin (HbA1c) |
| Bone-related measures | Bone turnover markers (Osteocalcin, PINP, NBAP and β-CTX), |
| serum 1,25(OH)2D3, seruum IGF-1 | |
| Mineral elements | Calcium (Ca), phosphorus (P) and magnesium (Mg) |
| Samples | |
| Blood | 25 mL |
| Serum | 2 mL |
| Urine† | 10 mL |
| Faeces† | 15 g |
*Direct measures carried out by trained interviewers according to standardised protocols.
†Measured only on WBBC pilot 3.
BAP, bone alkaline phosphatase; β-CTx, β-isomerised C-terminal telopeptides; DBP, diastolic blood pressure; FT3, free triiodothyronine; FT4, free tetraiodothyronine; HDL, high-density lipoprotein; IGF-1, insulin-like growth factor 1; LDL, low-density lipoprotein; PINP, N-terminal propeptide of procollagen type I; PTH, parathyroid hormone; SBP, systolic blood pressure; T3, triiodothyronine; T4, tetraiodothyronine; TSH, thyroid stimulating hormone.
Measurements of anthropometric parameters
Anthropometric data included height, body weight, bust, waist, hip and thigh circumference, resting blood pressure, HR and hand grip. Height was measured to the nearest 0.1 cm with participants’ light-weight clothes and shoes off; weight was measured to the nearest 0.01 kg with the weight scale (Ultrasonic surveying instrument, Beryl BYH01, China) calibrated daily before each series of measurements. Bust, waist, hip and thigh circumference were measured to the nearest 0.5 cm by using a measuring tape with the subject standing comfortably. Resting blood pressure and HR were measured on the left arm supported at heart-level sitting position using electronic Sphygmomanometers (Yuwell YE660A, China). To ensure accurate data of resting blood pressure and HR, the participants were asked to take a rest for at least 5 min and have no excessive physical activity. Using a handgrip dynamometer (CAMRY EH101, China), grip strength with both hands were tested for most of the participants in WBBC pilot 2 and WBBC pilot 3. In order to get more accurate results, the participants should make sure the arm that’s being tested was at a 90° angle at the elbow29 until the test was finished. Details of the methods and instruments used for measurements of anthropometric parameters were provided in table 3.
Table 3.
List of anthropometric collected and platforms for biochemical tests at baseline in the cohort
| Variables | Analysis method/platform used |
| Height and weight | Ultrasonic surveying instrument, Beryl BYH01, China |
| Waist, hip and thigh circumference | Manufactured instrument (tape) |
| Resting blood pressure | Electronic sphygmomanometer, Yuwell YE660A, China |
| Heart rate | Electronic sphygmomanometer, Yuwell YE660A, China |
| Grip strength | Digital hand dynamometer, CAMRY EH101, China |
| Bone mineral density (BMD) | DXA, Discovery QDR 4500, Hologic, Waltham, Massachusetts, USA |
| Blood routine (five items) | SYSMEX 2100, Japan |
| Serum IGF-1 | CLIA, DPC immulite 2000, Siemens, Germany |
| Serum calcium, phosphorus | ARCHITECT C16000, Abbott, USA |
| Fasting blood glucose | Cobas c501, Roche, Switzerland |
| Bone turnover markers | ECLIA, Cobas e602, Roche, Switzerland |
| Serum 1,25(OH)2D3 | LC-MS/MS, AB Sciex API 4000, USA |
| Thyroid and parathyroid function | Chemical luminescence, ARCHITECT System i2000, USA |
| Lipid metabolism | ARCHITECT C16000, Abbott, USA |
| Kidney-related measures | ARCHITECT C16000, Abbott, USA |
| Hepatic-related measures | ARCHITECT C16000, Abbott, USA |
CLIA, chemiluminescent immunoassay; ECLIA, electrochemoluminescence immunoassay; LC-MS/MS, liquid chromatography-tandem mass spectrometry.
Biochemistry assessment
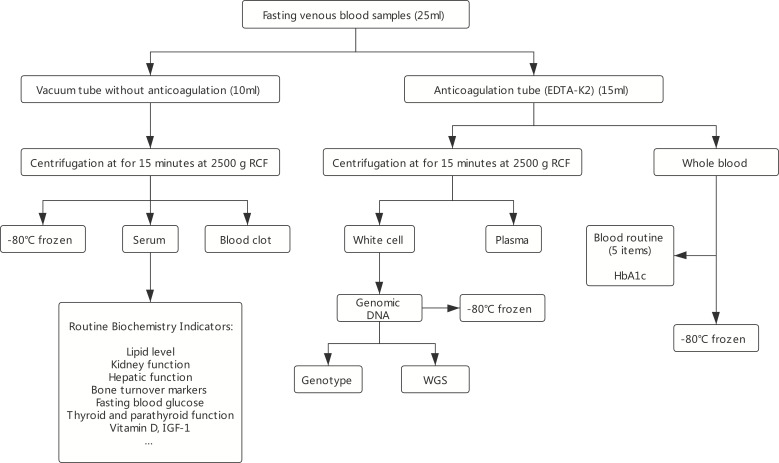
Participants came to the examination centre in each college in the morning with at least 8 hours of overnight fasting, about 25 mL of venous blood samples was collected for routine blood measurements, biochemical indexes, DNA extraction and so on. To ensure accurate data, the participants were asked not to have tea or alcohol intake or smoking for at least one night before blood sample collection. Venous blood samples were collected using ethylenediamine tetraacetic acid dipotassium (EDTAK2) anticoagulation tube (3×5.0 mL) and vacuum tube without anticoagulation (2×5.0 mL). Serum and plasma samples were separated from whole blood through centrifugation for 10 min at the relative centrifugal force 3000 g (figure 3). Serum samples were forwarded to test biochemical indexes that included serum 25(OH)D level, serum calcium level, fasting blood glucose, kidney function test, hepatic function test, blood lipids (triglyceride, cholesterol, low-density lipoprotein, high-density lipoprotein), triiodothyronine (T3), thyroid and parathyroid function and bone turnover markers (table 2). Details of the platforms used for biochemical analysis are provided in table 3. We also reserved serum samples (2×0.5 mL) for each participant at - 80℃ for future use. Figure 3 displays the detail of the flow diagram of blood separation and detection of main blood biochemical indexes.
Figure 3.
Flow diagram of main blood biochemical detection and blood conservation. RCF, relative centrifugal force; WGS, whole genome sequence.
Questionnaire-based assessments
Baseline data collection for participants included a self-completion questionnaire. In table 2, a list of core questions within the aforementioned domains, was provided. The questionnaire included social and demographic measures data (eg, age, sex, ethnicity, family economic status and born place), menstrual history (for female), lifestyle (eg, physical activity, smoking, alcohol, tea and coffee intake), additional supplement (eg, calcium and vitamin D), health status and other information. In WBBC pilot 1, the questionnaire only had “yes” and “no” choices for current smoking and alcohol status, in WBBC pilot 2 and 3, we updated the questionnaire to include the frequency information for smoking and alcohol. Sleep duration and sleep quality were assessed by the Pittsburgh Sleep Quality Index.30 This is composed of 19 questions which reflect seven major components, all seven components are then summed up to create a scale from 0 to 21 points.
Bone mineral density assessment
Bone mineral density (BMD) is expressed in terms of bone mass per cm2 (g/cm2) and were assessed by dual-energy X-ray absorptiometry31 (DXA, Discovery QDR 4500; Hologic, Waltham, Massachusetts, USA). In WBBC pilot, the main sites for BMD evaluation were lumbar spine (L1–L4), femur (femoral neck and total hip) and distal third of the radius.
Whole genome sequencing and genotyping
In the process of collecting fasting venous blood, 5 mL whole blood was used for isolation of genomic DNA. These genomic DNA was used for whole genome sequencing (WGS) and genotyping (figure 3). WGS was completed by NovaSeq 6000 system (Illumina Co.), and for now, 4535 participants have been sequenced at a mean depth of 14×, with highest depth of 65×. A Chinese specific reference panel will be constructed for imputation for the Chinese population. Whole genome genotyping was completed with Infinium Asian Screening Array (Illumina Co., Ltd), and 5841 participants have been genotyped in approximately 700 000 SNPs.
Follow-up and outcome measures
We are seeking funding to follow the cohort to examine the development and growth of the participants, and to investigate the effect of environmental factors on later outcomes. An important area of future research will focus on the development of bone mineral density and body weight from late adolescence to adulthood. Figure 2 shows the overall study plan. Follow-up surveys will be conducted according to the design of the subsequent research projects, the participants will be invited for survey with repeat interviews, including the questionnaire, anthropometric measurements, grip strength and bone mineral density collection as those used in the baseline stage and the data of nutritional status by food frequency questionnaire.
We have started a pilot follow-up study for WBBC pilot 2 since December 2019, and 1303 participants had completed all examinations (figure 2). The collected information included height, weight, grip strength and the updated questionnaire. Besides, we retested bone mineral density at the spine (L1-L4), hip and distal third of the radius.
Statistical analysis
To test the differences in means and proportions between male and female, we used t-test and χ2 tests for continuous and categorical variables, respectively. All variables were presented by unadjusted proportions for categorical variables and unadjusted means with SD for continuous variables. The variables demonstrating a p value of less than 0.05 were considered statistically significant. All statistical analyses were analysed using Stata V.12.0 software.
Findings to date
This pilot cohort of WBBC is a large, longitudinal survey conducted among adolescents and young adults in China. We surveyed 14 726 young people aged 14–25 years who were college students and available for completing follow-up studies. The baseline survey was carried out from 2017 to 2019, including WBBC pilot 1 (5290 participants), WBBC pilot 2 (6258 participants) and WBBC pilot 3 (3178 participants).
We have several ongoing projects under WBBC pilot study. One of the most significant ongoing projects is the WGS study for Chinese population, the results were reported elsewhere.32 In brief, 4535 WGS individuals and 5481 high-density genotyping individuals were available in WBBC pilot project, covering 30 provincial regions of China. Since our previous study33 demonstrated that the existing reference panels, such as the 1000 Genome Phase3 panel34 and the HRC (Haplotype Reference Consortium) panel,35 were not the best fit for imputation for the Chinese population, our WGS data provided a population specific reference panel to improve the imputation accuracy of Chinese GWAS study. We also provided an online imputation server (https://imputationserver.westlake.edu.cn/) which could result in higher imputation accuracy compared with the existing panels, especially for lower frequency variants.32
Given the extensive range of data collected in the WBBC study (https://wbbc.westlake.edu.cn/index.html), it is not feasible to present all the results, only limited findings were described in the present study. In summary, a total of 17 407 college students were invited, of whom, 14 983 (86.07 %) responded. After removing participants with missing data and invalid data, the final study included an effective sample size of 14 726 (84.60%) adolescents and young adults (with age from 14 to 25 years, and mean age 18.5 years). Table 4 provides an overview of sociodemographic, anthropometry, cardiovascular system, lifestyle, grip strength and BMD characteristics of the WBBC pilot participants at baseline. Briefly, within the 14 726 samples, there were more females than males (67.7 vs 32.3%), with a mean age of 18.5 years for female and 18.6 years for males, respectively. Most of the participants were Chinese Han ethnic (97.8%), and more than 60% of them were originally from rural areas (60.2% of males and 69.6% of females). For anthropometry measurements, the mean height and weight were 172.9 cm and 65.81 kg for males, and 160.1 cm and 52.9 kg for females; the mean waist, hip and thigh circumference were 75.5 cm, 90.8 cm and 51.6 cm in males, and 71.7 cm, 89.8 cm and 51.7 among females. The mean systolic blood pressure, diastolic blood pressure and HR in participants were 113 mm Hg, 71 mm Hg and 86 beats/min, respectively. In the cohort, only 5.5% of the participants were current smokers and 38.8% of them were regular drinkers. Regarding the current smoking status, there was a significant difference between males and females (16.3 vs 1.6%, p<0.001). As for alcohol, the proportion of current drinker in males and females was 62.0% and 29.2%, respectively, which is much higher in males (p<0.001). The mean sleeping time estimated in females was higher than males (8.3 vs 8.0 hours, p<0.001). As for grip strength, the data collection was started from WBBC pilot 2, the mean of grip strength in males were much higher than females (grip-left: 36.66 vs 27.38 kg and grip-right: 39.90 vs 29.76 kg, both p<0.001).
Table 4.
Basic characteristics of participants in baseline of Westlake BioBank for Chinese pilot
| Variables(unit) | Total | Sex | *P value | ||
| Male | Female | ||||
| Sociodemographic | |||||
| Age (years) | N† | 14 726 | 4751 | 9975 | 0.001 |
| M (SD)‡ | 18.5 (1.3) | 18.6 (1.2) | 18.5 (1.3) | ||
| Gender | N (%)§ | 14 726 (100) | 4751 (32.3) | 9975 (67.7) | <0.001 |
| Ethnicity | 0.305 | ||||
| Han | N (%) | 11136 (97.8) | 3642 (98.0) | 7494 (97.7) | |
| Others | N (%) | 253 (2.2) | 75 (2.0) | 178 (2.3) | |
| Hukou status | <0.001 | ||||
| Rural | N (%) | 5951 (66.6) | 1739 (60.2) | 4212 (69.6) | |
| Urban | N (%) | 2986 (33.4) | 1148 (39.8) | 1838 (30.4) | |
| Anthropometry | |||||
| Height (cm) | N | 14277 | 4588 | 9689 | <0.001 |
| M (SD) | 164.2 (8.5) | 172.9 (6.6) | 160.1 (5.8) | ||
| Weight (kg) | N | 14279 | 4587 | 9692 | <0.001 |
| M (SD) | 57.01 (12.32) | 65.81 (13.60) | 52.85 (9.07) | ||
| Waist (cm) | N | 12 396 | 3905 | 8491 | <0.001 |
| M (SD) | 71.7 (9.8) | 75.5 (11.1) | 69.9 (8.7) | ||
| Hip (cm) | N | 12388 | 3902 | 8486 | <0.001 |
| M (SD) | 89.8 (7.3) | 90.8 (8.3) | 89.3 (6.7) | ||
| Thigh (cm) | N | 12351 | 3880 | 8471 | 0.102 |
| M (SD) | 51.7 (5.7) | 51.6 (6.5) | 51.7 (5.3) | ||
| Cardiovascular system | |||||
| SBP (mm Hg) | N | 14277 | 4595 | 9682 | <0.001 |
| M (SD) | 113 (12) | 121 (12) | 110 (11) | ||
| DBP (mm Hg) | N | 14276 | 4595 | 9681 | <0.001 |
| M (SD) | 71 (9) | 73 (9) | 70 (8) | ||
| Heart rate (beats/min) | N | 14295 | 4599 | 9696 | <0.001 |
| M (SD) | 86 (13) | 83 (13) | 87 (13) | ||
| Lifestyle | |||||
| Smoking | N (%) | 435 (5.9) | 350 (16.3) | 85 (1.6) | <0.001 |
| Alcohol status | N (%) | 2844 (38.8) | 1333 (62.0) | 1511 (29.2 | <0.001 |
| Sleeping time (hours) | N | 7247 | 2115 | 5132 | |
| M (SD) | 8.2 (1.4) | 8.0 (1.3) | 8.3 (1.4) | <0.001 | |
| Grip strength (kg) | |||||
| Left hand | N | 8932 | 2958 | 5974 | <0.001 |
| M (SD) | 27.38 (8.77) | 36.66 (7.53) | 22.79 (4.82) | ||
| Right hand | N | 8941 | 2967 | 5974 | <0.001 |
| M (SD) | 29.76 (9.66) | 39.90 (8.32) | 24.72 (5.35) | ||
| BMD (g/cm2) | |||||
| Lumar spine | N | 10154 | 3293 | 6861 | <0.001 |
| M (SD) | 0.910 (0.105) | 0.926 (0.112) | 0.903 (0.100) | ||
| Total hip | N | 10160 | 3296 | 6864 | <0.001 |
| M (SD) | 0.868 (0.127) | 0.932 (0.139) | 0.837 (0.108) | ||
| Femoral neck | N | 10160 | 3296 | 6864 | <0.001 |
| M (SD) | 0.778 (0.125) | 0.846 (0.138) | 0.746 (0.104) | ||
| Forearm | N | 9917 | 3238 | 6679 | <0.001 |
| M (SD) | 0.657 (0.059) | 0.705 (0.057) | 0.634 (0.453) | ||
*T-test and χ2 tests for continuous and categorical variables, respectively, to refer the significant differences between males and females.
†N: sample size.
‡M (SD): mean (SD).
§N (%): sample size (percentage).
DBP, diastolic blood pressure; SBP, systolic blood pressure.
Height and weight were measured using the standardised procedures. BMI was calculated based on the formula: weight in kilograms divided by height in meters squared (kg/m2). According to the Working Group on Obesity in China (WGOC),36 participants were defined as underweight (< 18.5 kg/m2), normal weight (18.5–23.9 kg/m2), overweight (24–27.9 kg/m2) and obese (≥ 28 kg/m2). Therefore, the WBBC pilot study provided an overall prevalence of underweight, overweight and obesity among young participants of 24.3%, 11.5% and 5.0%, respectively (table 5). The prevalence of underweight in female was much higher than male (26.4% vs 19.7%, p<0.0001), but the prevalence of overweight in female was much lower than male (9.0% vs 16.7%, p<0.0001) (table 5), similarly, the prevalence of obesity in female (3.2%) was lower than in male (8.9%) (p<0.0001) (table 5). Waist circumference (WC) is a good indicator of abdominal visceral fat distribution and is a strong predictor of diabetes mellitus and cardiovascular disease.37 It is meaningful to investigate the WC along with BMI among adolescents and young people. In WBBC pilot study, central obesity was defined as WC ≥85 cm for males and as WC ≥80 cm for females based on the recommendations of the WGOC.36 In the cohort of 12 396 participants, the prevalence of central obesity was 14.6%, which was higher in male than in female (19.1% vs 12.6%, p<0.0001) (table 5).
Table 5.
Distribution of body mass index or waist by sex in participants in Westlake BioBank for Chinese pilot, 2017–2019 (N=14264)
| Variables | Total | Male | Female | P value* |
| Underweight, N (%) | 3460 (24.3%) | 903 (19.7%) | 2557 (26.4%) | <0.0001 |
| Normal, N (%) | 8446 (59.2%) | 2507 (54.7%) | 5939 (61.4%) | <0.0001 |
| Overweight, N (%) | 1640 (11.5%) | 766 (16.7%) | 874 (9.0%) | <0.0001 |
| Obesity, N (%) | 718 (5.0%) | 407 (8.9%) | 311 (3.2%) | <0.0001 |
| Central obesity†, N (%) | 1812 (14.6%) | 746 (19.1%) | 1066 (12.6%) | <0.0001 |
*χ2 tests was calculated between male and female. Participants were defined as underweight (< 18.5 kg/m2), normal weight (18.5–23.9 kg/m2), overweight (24–27.9 kg/m2) and obese (≥ 28 kg/m2). Central obesity was defined as WC ≥85 cm for males and as WC ≥80 cm for females.
†Total sample size for central obesity was 12396.
In WBBC pilot study, the prevalence of underweight were high in both male (19.7 %) and female (26.4%), though the prevalence of moderate and severe underweight decreased from 9.2% in 1975 to 8.4% in 2016 in girls and from 14.8% in 1975 to 12.4% in 2016 in boys in the world.38 These results might be due to the modern aesthetics of human stature that thinness is preferred, especially in China.39 40 Recently, a study involving 2023 young female participants (70.5% subjects aged 20–25 years) from eight Chinese universities40 showed that 30.55% of the participants were underweight, and 57.39% of them would like to be much thinner, which would lead to more underweight individuals. A silhouette-matching test was administered in mainland China and found that the majority of the female participants indicated a preference to be more slender.41 Their ideal figure was underweight and was far smaller than the most attractive female figure chosen by male participants.41 Therefore, future studies should not only pay attention to the problem of obesity/overweight, but also to the underweight issue with young people.
Using simple anthropometric indices of body composition, such as BMI and WC, has been considered as a practical and valuable approach to the assessment of obesity for a long time. Waist-to-hip ratios, waist-to-height ratios, a body shape index42 and body roundness index43 were also as parameters of body fat and visceral adipose tissue volume. In WBBC pilot cohort, we had collected several anthropometric measures including height, weight, bust, waist, hip and thigh circumference and these data could help us examine the usefulness of these anthropometric parameters and identify the optimal cut-off of the parameters to evaluate overweight and obesity among adolescents and young people in future study.
In WBBC pilot study, the mean serum 25(OH)D level was 22.4±5.3 ng/mL for all the participants (male: 25.2 ng/mL, and female: 21.1 ng/mL, p<0.0001) (table 6).
Table 6.
Distribution of vitamin D level by sex in subjects in Westlake BioBank for Chinese pilot, 2017–2018 (N=11 370)
| Variables | Total | Male | Female | P value |
| Serum 1,25(OH)D, mean (SD) | 22.4 (5.3) | 25.2 (5.4) | 21.1 (4.7) | <0.0001* |
| Vitamin D deficient, N (%) | 3806 (33.5%) | 610 (16.4%) | 3196 (41.8%) | <0.0001† |
| Vitamin D insufficient, N (%) | 6614 (58.2%) | 2452 (65.7%) | 4162 (54.5%) | <0.0001† |
| Vitamin D sufficient, N (%) | 950 (8.4%) | 668 (17.9%) | 282 (3.7%) | <0.0001† |
| Vitamin D supplementation‡, N (%) | 164 (2.2%) | 67 (3.1%) | 97 (1.9%) | 0.00098† |
*T-test was calculated between male and female.
†χ2 tests was calculated between male and female.
‡The sample size for vitamin D supplementation was 7326.
Overall, 33.5% of the participants had vitamin D deficiency and even more participants suffered from vitamin D insufficiency (58.2%) (table 6). In addition, the proportion of females with sufficient vitamin D was much lower than that of males (3.7 vs 17.9%, p<0.0001), while the proportion of deficiency in females was much higher than that in males (41.8 vs 16.4%, p<0.0001) (table 6). Most of the participants (86.9%) preferred to stay indoors in spare time, the females were less willing to do exercise than males (53.7% vs 70.6%) (table 7), and 44.6% of females hardly had outdoor activities, only 5.9% of females often had outdoor activities every week (table 7). These results, jointly suggested that the females had not enough sun exposure. Although food sources of vitamin D were not commonly recognised, only 10%–20% of vitamin D in human bodies was obtained through food sources.44 In WBBC pilot study, there was only 2.2% of the participants used vitamin D supplements (3.1% in male and 1.9% in female, p=0.00098) (table 6) and this was consistent with Zhou et al,45 which found that only 5.6% of the students used vitamin D supplements in a university of Nanjing, China. It is noteworthy that vitamin D deficiency in females was significantly worse than in males. This may due to the modern aesthetics of Chinese culture that paler skin is preferred, especially in females. A questionnaire related to vitamin D and sun exposure was conducted at a university in Nanjing, China and found that 75.0% of the students lacked sun exposure because they would like to avoid dark skin.45 In addition, most of the students (82.7 %) used sun protection, and sunscreen use was more popular in females.45 However, it was reported that using the amount of sun cream recommended by WHO exponentially suppressed vitamin D synthesis in the skin.46
Table 7.
Participants’ general react about activity status in Westlake BioBank for Chinese pilot, 2017–2018 (N=7326*)
| Total | Male | Female | |
| What would you like to do in spare time? | |||
| Stay indoors | 6364 (86.9%) | 1754 (81.6%) | 4610 (89.1%) |
| Take part in some activities | 962 (13.1%) | 395 (18.4%) | 567 (11.0. %) |
| Do you do exercise initiatively? | |||
| Yes | 4296 (58.6%) | 1517 (70.6%) | 2779 (53.7%) |
| No | 3030 (41.4%) | 632 (29.4%) | 2398 (46.3%) |
| How often do you have outdoor activities every week? | |||
| Hardly | 2785 (38.0%) | 477 (22.2%) | 2308 (44.6%) |
| Occasionally | 3865 (52.8%) | 1301 (60.5%) | 2564 (49.5%) |
| Often | 676 (9.2%) | 371 (17.3%) | 305 (5.9%) |
*Data are showed as n (%) of participants.
Collaboration
Participants have agreed to provide their pseudonymised data being made available to other approved researchers. The WBBC pilot study welcomes and offers global collaboration. The data are not freely available in the public domain, but specific proposals and ideas for future collaboration would be very welcome. Applicants for collaboration and more information are encouraged to contact Dr. Hou-Feng Zheng (email address: zhenghoufeng@westlake.edu.cn), the person in charge of this project.
Supplementary Material
Acknowledgments
We gratefully acknowledge all the participants of this project, and thank all the people who helped us in the sample recruitment, including volunteers, laboratory technicians, nurses and clerical workers. We also thank the High-Performance Computing Center at Westlake University for the facility support and technical assistance. In addition, we would like to thank Shanghai AvanTech BioSciences Co., Ltd for their support and assistance in sample storage and management.
Footnotes
Contributors: H-FZ gained funds and conceived of the study, and K-QL, P-YW, J-YC, X-JX, J-JX, M-CQ, CL and S-YX were involved in the sample collection. J-QL and YS were involved in the blood biochemistry testing. W-YB, P-PZ, JX, S-RG, P-LG, YQ and P-KC were involved in the DNA extraction. X-WZ and H-FZ analysed the data and wrote the paper. All authors read and approved the final manuscript.
Funding: This study was supported by the National Natural Science Foundation of China (81871831 and 32061143019), and by the Westlake Biobank for Chinese (WBBC) funds from Westlake University
Map disclaimer: The depiction of boundaries on the map(s) in this article does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests: Jun-Quan Liu and Yi Sun are employees of Hangzhou Kingmed Diagnostics Co. The other authors have no conflict of interest to declare.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. The data are not freely available in the public domain, but specific proposals and ideas for future collaboration would be very welcome. Applicants for collaboration and more information are encouraged to contact Dr. Hou-Feng Zheng (Email address: zhenghoufeng@westlake.edu.cn), the person in charge of this project.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study protocol and informed consent procedure were approved by the Ethics Committees at Westlake University. All study participants signed the informed consent form before taking part in the study.
References
- 1.Steinbeck K, Hazell P, Cumming RG, et al. The study design and methodology for the ARCHER study-adolescent rural cohort study of hormones, health, education, environments and relationships. BMC Pediatr 2012;12:143. 10.1186/1471-2431-12-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patton GC, Coffey C, Carlin JB, et al. Overweight and obesity between adolescence and young adulthood: a 10-year prospective cohort study. J Adolesc Health 2011;48:275–80. 10.1016/j.jadohealth.2010.06.019 [DOI] [PubMed] [Google Scholar]
- 3.Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: a foundation for future health. Lancet 2012;379:1630–40. 10.1016/S0140-6736(12)60072-5 [DOI] [PubMed] [Google Scholar]
- 4.Yu Z, Han S, Chu J, et al. Trends in overweight and obesity among children and adolescents in China from 1981 to 2010: a meta-analysis. PLoS One 2012;7:e51949. 10.1371/journal.pone.0051949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet 2014;384:766–81. 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jiang Y, Wang J, Wu S, et al. Association between Take-Out food consumption and obesity among Chinese university students: a cross-sectional study. Int J Environ Res Public Health 2019;16. 10.3390/ijerph16061071. [Epub ahead of print: 25 03 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang J, Wang H, Wang Z, et al. Prevalence and stabilizing trends in overweight and obesity among children and adolescents in China, 2011-2015. BMC Public Health 2018;18:571. 10.1186/s12889-018-5483-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freedman DS, Kahn HS, Mei Z, et al. Relation of body mass index and waist-to-height ratio to cardiovascular disease risk factors in children and adolescents: the Bogalusa heart study. Am J Clin Nutr 2007;86:33–40. 10.1093/ajcn/86.1.33 [DOI] [PubMed] [Google Scholar]
- 9.Llewellyn A, Simmonds M, Owen CG, et al. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta-analysis. Obes Rev 2016;17:56–67. 10.1111/obr.12316 [DOI] [PubMed] [Google Scholar]
- 10.Jeon K, Kim D-I. The association between low body weight and scoliosis among Korean elementary school students. Int J Environ Res Public Health 2018;15. 10.3390/ijerph15122613. [Epub ahead of print: 22 11 2018]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He Q, Karlberg J. Bmi in childhood and its association with height gain, timing of puberty, and final height. Pediatr Res 2001;49:244–51. 10.1203/00006450-200102000-00019 [DOI] [PubMed] [Google Scholar]
- 12.Hudson LD, Nicholls DE, Lynn RM, et al. Medical instability and growth of children and adolescents with early onset eating disorders. Arch Dis Child 2012;97:779–84. 10.1136/archdischild-2011-301055 [DOI] [PubMed] [Google Scholar]
- 13.Antonucci R, Locci C, Clemente MG, et al. Vitamin D deficiency in childhood: old lessons and current challenges. J Pediatr Endocrinol Metab 2018;31:247–60. 10.1515/jpem-2017-0391 [DOI] [PubMed] [Google Scholar]
- 14.Trehan N, Afonso L, Levine DL, et al. Vitamin D deficiency, supplementation, and cardiovascular health. Crit Pathw Cardiol 2017;16:109–18. 10.1097/HPC.0000000000000122 [DOI] [PubMed] [Google Scholar]
- 15.Watkins RR, Lemonovich TL, Salata RA. An update on the association of vitamin D deficiency with common infectious diseases. Can J Physiol Pharmacol 2015;93:363–8. 10.1139/cjpp-2014-0352 [DOI] [PubMed] [Google Scholar]
- 16.Illescas-Montes R, Melguizo-Rodríguez L, Ruiz C, et al. Vitamin D and autoimmune diseases. Life Sci 2019;233:116744. 10.1016/j.lfs.2019.116744 [DOI] [PubMed] [Google Scholar]
- 17.Holick MF. Vitamin D deficiency. N Engl J Med 2007;357:266–81. 10.1056/NEJMra070553 [DOI] [PubMed] [Google Scholar]
- 18.Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2011;96:1911–30. 10.1210/jc.2011-0385 [DOI] [PubMed] [Google Scholar]
- 19.Pludowski P, Grant WB, Bhattoa HP, et al. Vitamin D status in central Europe. Int J Endocrinol 2014;2014:589587. 10.1155/2014/589587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Newhook LA, Sloka S, Grant M, et al. Vitamin D insufficiency common in newborns, children and pregnant women living in Newfoundland and Labrador, Canada. Matern Child Nutr 2009;5:186–91. 10.1111/j.1740-8709.2008.00157.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoshimura N, Muraki S, Oka H, et al. Profiles of vitamin D insufficiency and deficiency in Japanese men and women: association with biological, environmental, and nutritional factors and coexisting disorders: the road study. Osteoporos Int 2013;24:2775–87. 10.1007/s00198-013-2372-z [DOI] [PubMed] [Google Scholar]
- 22.Hirani V, Cumming RG, Blyth FM, et al. Vitamin D status among older community dwelling men living in a sunny country and associations with lifestyle factors: the Concord health and ageing in men project, Sydney, Australia. J Nutr Health Aging 2013;17:587–93. 10.1007/s12603-013-0013-z [DOI] [PubMed] [Google Scholar]
- 23.Faghih S, Abdolahzadeh M, Mohammadi M, et al. Prevalence of vitamin D deficiency and its related factors among university students in Shiraz, Iran. Int J Prev Med 2014;5:796–9. [PMC free article] [PubMed] [Google Scholar]
- 24.Fraser DR. Vitamin D-deficiency in Asia. J Steroid Biochem Mol Biol 2004;89-90:491–5. 10.1016/j.jsbmb.2004.03.057 [DOI] [PubMed] [Google Scholar]
- 25.Yu X, Wang W, Wei Z, et al. Vitamin D status and related factors in newborns in Shanghai, China. Nutrients 2014;6:5600–10. 10.3390/nu6125600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang EW-L, Pang MY-C, Siu PM-F, et al. Vitamin D status and cardiometabolic risk factors in young adults in Hong Kong: associations and implications. Asia Pac J Clin Nutr 2018;27:231–7. 10.6133/apjcn.022017.08 [DOI] [PubMed] [Google Scholar]
- 27.Guo Y, Ke H-J, Liu Y, et al. Prevalence of vitamin D insufficiency among children in southern China: a cross-sectional survey. Medicine 2018;97:e11030. 10.1097/MD.0000000000011030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yan X, Zhang N, Cheng S, et al. Gender differences in vitamin D status in China. Med Sci Monit 2019;25:7094–9. 10.12659/MSM.916326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roberts HC, Denison HJ, Martin HJ, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing 2011;40:423–9. 10.1093/ageing/afr051 [DOI] [PubMed] [Google Scholar]
- 30.Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 31.Bazzocchi A, Ponti F, Albisinni U, et al. DXA: technical aspects and application. Eur J Radiol 2016;85:1481–92. 10.1016/j.ejrad.2016.04.004 [DOI] [PubMed] [Google Scholar]
- 32.Cong P, Bai W-Y, Li J. Genomic analyses of 10,376 individuals provides comprehensive map of genetic variations, structure and reference haplotypes for Chinese population. bioRxiv 2021. [Google Scholar]
- 33.Bai W-Y, Zhu X-W, Cong P-K, et al. Genotype imputation and reference panel: a systematic evaluation on haplotype size and diversity. Brief Bioinform 2019. 10.1093/bib/bbz108. [Epub ahead of print: 06 Nov 2019]. [DOI] [PubMed] [Google Scholar]
- 34., Auton A, Brooks LD, et al. , 1000 Genomes Project Consortium . A global reference for human genetic variation. Nature 2015;526:68–74. 10.1038/nature15393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McCarthy S, Das S, Kretzschmar W, et al. A reference panel of 64,976 haplotypes for genotype imputation. Nat Genet 2016;48:1279–83. 10.1038/ng.3643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou B-F, Cooperative Meta-Analysis Group of the Working Group on Obesity in China . Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci 2002;15:83–96. [PubMed] [Google Scholar]
- 37.Asia Pacific Cohort Studies Collaboration . Central obesity and risk of cardiovascular disease in the Asia Pacific region. Asia Pac J Clin Nutr 2006;15:287–92. [PubMed] [Google Scholar]
- 38.NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017;390:2627–42. 10.1016/S0140-6736(17)32129-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen H, Jackson T. Predictors of changes in weight Esteem among mainland Chinese adolescents: a longitudinal analysis. Dev Psychol 2009;45:1618–29. 10.1037/a0016820 [DOI] [PubMed] [Google Scholar]
- 40.Zhang L, Qian H, Fu H. To be thin but not healthy - The body-image dilemma may affect health among female university students in China. PLoS One 2018;13:e0205282. 10.1371/journal.pone.0205282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang K, Liang R, Ma Z-L, et al. Body image attitude among Chinese college students. Psych J 2018;7:31–40. 10.1002/pchj.200 [DOI] [PubMed] [Google Scholar]
- 42.Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One 2012;7:e39504. 10.1371/journal.pone.0039504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thomas DM, Bredlau C, Bosy-Westphal A, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013;21:2264–71. 10.1002/oby.20408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mithal A, Wahl DA, Bonjour J-P, et al. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int 2009;20:1807–20. 10.1007/s00198-009-0954-6 [DOI] [PubMed] [Google Scholar]
- 45.Zhou M, Zhuang W, Yuan Y, et al. Investigation on vitamin D knowledge, attitude and practice of university students in Nanjing, China. Public Health Nutr 2016;19:78–82. 10.1017/S1368980015000373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Faurschou A, Beyer DM, Schmedes A, et al. The relation between sunscreen layer thickness and vitamin D production after ultraviolet B exposure: a randomized clinical trial. Br J Dermatol 2012;167:391–5. 10.1111/j.1365-2133.2012.11004.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. The data are not freely available in the public domain, but specific proposals and ideas for future collaboration would be very welcome. Applicants for collaboration and more information are encouraged to contact Dr. Hou-Feng Zheng (Email address: zhenghoufeng@westlake.edu.cn), the person in charge of this project.