Abstract
Background And Objectives:
Spigelian hernias (SH) are a rare variant of abdominal wall defects that require prompt surgical intervention. With the advancement of abdominal wall surgery capabilities, there are several possible approaches of repairing SH. The aim of the study was to present our experience in performing laparoscopic or robotic transabdominal preperitoneal (TAPP) repairs of SH and discuss the advantages of TAPP in such hernias.
Methods:
Retrospective review of a prospectively maintained database of SH TAPP repairs between February 1, 2015 and February 29, 2020. Data included clinical details, size and location of fascial defect, presence of concomitant hernias, surgery duration, length of stay (LOS), mesh type, mesh size, and fixation method. Follow up visits at 1 month postoperative and telephone survey for pain assessment and subsequent hernia-related treatment.
Results:
During the study period 16 patients underwent TAPP SH repairs, 13 laparoscopically and 3 robotic. Seven (44%) patients had a concomitant inguinal hernia with 1 patient having bilateral inguinal defects. Mean surgery duration and mean LOS were 78 (range 41 – 120) minutes & 1.6 (range 1 – 3) days, respectively. Immediate postoperative complications included 2 seromas and 1 port-site hematoma. Mean telephone survey follow up was 17 months (range 3 – 49). Mean visual analogue scale scores were significantly lower at follow-up compared to discharge (1.9 vs 0.5, P = 0.0015).
Conclusion:
Advantages of TAPP SH repair include low postoperative chronic pain, potential low wound complications, intra-abdominal visualization of hernia contents, and repairing of concomitant inguinal hernias simultaneously.
Keywords: Spigelian Hernia, Abdominal Wall, TAPP, rTAPP
INTRODUCTION
Spigelian hernias (SH) occur at the Spigelian aponeurosis, where the semilunar line meets the lateral edge of the rectus abdominis muscle, along the “spigelian belt”, which spans 6 cm below the umbilicus. SH represent less than 2% of all abdominal wall hernias, are more frequent in older women, are usually small, and below the arcuate line. Approximately 35% of SH cases have a concomitant inguinal hernia upon diagnosis. Although SH is a rare presentation of abdominal wall hernias, it entails a high rate of incarceration between 20% – 30%.1–4 While traditionally repair of SH has been described in the “open” approach,1 with the advancement of minimally invasive techniques, development of versatile meshes and proper understanding of abdominal wall anatomy, several minimally invasive procedures for ventral hernia repairs have been proposed as acceptable reconstruction methods. These methods include intraperitoneal onlay mesh (IPOM) repair, totally extraperitoneal (TEP) repair, and transabdominal preperitoneal repair (TAPP), by either laparoscopic or robotic approach.4–9 Although several methods and approaches exist with apparent advantages and limitations, the optimal procedure for SH repair has yet to be determined and the literature is scarce regarding which repair is superior.
The aim of the study was to present our experience in performing laparoscopic or robotic TAPP repairs of SH.
MATERIALS & METHODS
Retrospective review of a prospectively maintained database of SH TAPP repairs between February 1, 2015 and February 29, 2020. Data collected included demographics, anthropometrics, clinical presentation, previous abdominal surgeries, American Society of Anesthesiology (ASA) score, smoking status, size and location of fascial defect, presence of concomitant hernias, pre-operative imaging, surgery duration, length of stay (LOS), mesh type, mesh size, and fixation method. Follow-up via outpatient clinic visits at 1 month postoperative and a further follow-up via telephone survey included a pain assessment by visual analogue scale (VAS), analgesic medication use, readmissions, and recurrent abdominal surgery (Table 1). Postoperative complications were graded using the Clavien-Dindo Classification (CD) where major complications were considered a CD grade > 3.10
Table 1.
Demographics, Clinical Data, Defect, and Repair Details
| n | Range | ||
|---|---|---|---|
| Mean Age | 63.5 ± 14.1 | 38 – 79 | |
| Female:Male | 13:3 | ||
| Mean ASA | 2.3 ± 0.7 | 1 – 3 | |
| Mean BMI | 25.7 ± 2.4 | 23 – 31 | |
| n | % | ||
| Smoking | 4 | 25% | |
| PSH | 6 | 38% | |
| Appendectomy | 1 | ||
| BSO | 1 | ||
| Whipple's Procedure | 1 | ||
| Cesarean | 1 | ||
| Open Umbilical Hernia | 1 | ||
| Lap Cholecystectomy | 1 | ||
| Antiplatelet | 6 | 38% | |
| Approach | |||
| Laparoscopic | 13 | 81% | |
| Robotic | 3 | 19% | |
| Emergency | 3 | 19% | |
| Side | Left:Right | 11:5 | |
| Concomitant groin hernia | Overall | 7 | 44% |
| Ipsilateral | 5 | 31% | |
| Contralateral | 1 | 6% | |
| Bilateral | 1 | 6% | |
| Direct | 0 | 0% | |
| Indirect | 7 | 44% | |
| Femoral | 2 | 13% | |
| Mean Defect diameter (cm) | 1.9 * 2.0 | 3.8 | |
| Mean Overall defect area (cm2) | 4.5 | ||
| Below arcuate line | 12 | 75% | |
| Primary closure | 11 | 69% | |
| Mean Mesh size (cm) | 14.3 * 12.7 | 181.61 | |
| Mean Overall mesh area (cm2) | 163 | ||
| Fixation | 11 | 69% | |
| Mean Surgery time (minutes) | 78 ± 20.9 | 41 – 120 | |
| Mean LOS (days) | 1.6 ± 0.6 | 1 – 3 | |
| Overall | 3 | 19% | |
| Morbidity | |||
| Hematoma | 1 | 6% | |
| Seroma | 2 | 13% | |
| Mortality | 0 | ||
| Reoperation | 0 | ||
| Readmission | 0 | ||
| VAS score at discharge | 1.9 | 0 – 5 | |
| VAS score at 2 weeks | 1.1 | 0 – 5 | |
| VAS score at telephone survey | 0.8 | 0 – 5 | |
ASA, American Society of Anesthesiology; BMI, body mass index; PSH, previous surgical history; BSO, bilateral salpingoophorectomy; LOS, length of stay; VAS, visual analogue scale.
Oral informed consent was obtained during the telephone survey. A separate institutional review board approved the study protocol at each medical center included in the study.
Surgical Technique
Patients were placed in the supine position with both hands tucked to the sides with a foley catheter inserted following induction of general anesthesia. The abdomen was prepped and draped in the usual sterile fashion. Insertion of Veress needle at left upper quadrant and inflation with CO2 to achieve pneumoperitoneum of 15 mmHg.
Laparoscopic SH Repair
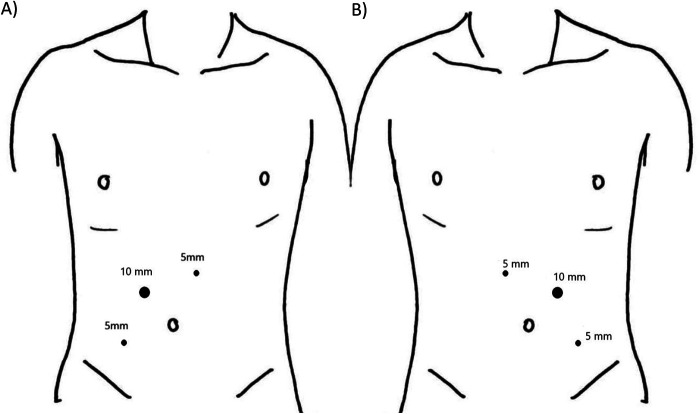
Upon gaining access to the abdominal cavity with a 10 mm camera port, triangulation of additional ports were placed under vision as depicted in Figure 1. Inspection of abdominal viscera was followed by reduction of hernia contents to the abdominal cavity, hernia size, and contents assessment. A large peritoneal flap was developed linearly using endoscopic scissors, beginning at the midline towards the side of the defect, approximately 3 cm above the cranial edge of the defect. Blunt and cautery dissection allowed separation of the peritoneum and transversalis fascia from the rectus abdominis muscle to develop the preperitoneal space. The dissection extended 5 cm cranial, caudal, and lateral from the edges of the defect. In cases of a concomitant inguinal hernia, the dissection extended caudally and medially to allow visualization of the myopectineal orifice with all potential groin defects according to the critical view of the myopectineal orifice described by Daes and Felix.11 Continuous 2-0 nonabsorbable V-LOCK sutures (Medtronic, Minneapolis, MN) were used whenever a primary closure of the defect was performed prior to mesh placement. Concomitant ipsilateral inguinal hernias were repaired in the same preperitoneal plain by extending caudal dissection and using additional meshes as needed to maintain covering of both spigelian and inguinal defects. In case of concomitant bilateral inguinal hernias, a large peritoneal flap was developed to include the contralateral side and separate meshes were used on each side. Mesh overlap of at least 5 cm was ensured on each border of the defect. Mesh type and fixation was chosen by surgeon preference: 11 (68%) patients underwent mesh fixation, with 3 cases using nonabsorbable fixation device (Spire’it, Microval, Saint-Just-Malmont, France) and 8 cases using absorbable fixation device (Securestrap, Ethicon J&J medical devices, Summerville, NJ, USA). The remaining 5 cases involved a self-fixating mesh and thus did not necessitate additional fixation. Closure of the peritoneal flap by running nonabsorbable V-Lock (Medtronic, Minneapolis, MN) 2/0 suture.
Figure 1.
Laparoscopic port placement for (A) left-sided and (B) right-sided spigelian hernia repairs.
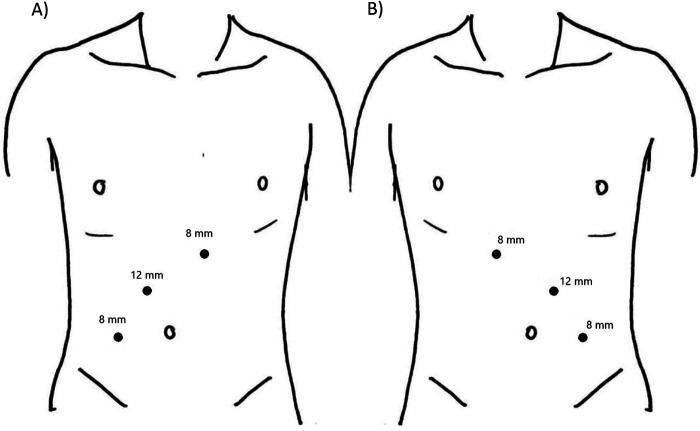
Robotic SH TAPP Repair
The Da Vinci® SI system (Intuitive surgical, San-Francisco, USA) cart was placed on the ipsilateral side of the hernia. A 12-mm optical port was placed 3 cm above and lateral to the umbilicus below the costal margin in the midclavicular line on the contralateral side of the hernia. Upon gaining access to the abdominal cavity, triangulation of additional ports were placed under vision as depicted in Figure 2. Using the da Vinci® Surgical System, EndoWrist® Instruments including the curved scissors connected to monopolar electrical current and forceps, the preperitoneal dissection was performed in a similar fashion as the above mentioned laparoscopic approach. A ProGrip (Medtronic, Minneapolis, MN) self-fixating mesh was utilized while ensuring a 5 cm mesh overlap beyond the defect border. Peritoneal flap closure by a running nonabsorbable V-Lock 3/0 (Medtronic, Minneapolis, MN) suture using the Da Vinci® needle driver.
Figure 2.
Robotic port placement for (A) left-sided and (B) right-sided spigelian hernia repairs.
Continuous 2-0 nonabsorbable V-LOCK sutures (Medtronic, Minneapolis, MN) were used whenever a primary closure of the defect prior to mesh placement was performed per surgeon preference in either laparoscopic or robotic approach.
Statistical Analysis
Paired variables were compared using non-parametric Wilcoxon test as appropriate. All tests were 2-tailed and considered significant at P < .05. Calculations were done using the SPSS software.
RESULTS
During the study period, 16 patients underwent TAPP SH repair. Thirteen were female (81%), mean body mass index was 25.7 (range 23 – 31) kg/m2 and 6 (38%) patients had previous abdominal surgery. All patients underwent pre-operative abdominal-pelvic computed tomography (CT) scan with 7 (44%) patients found to have a concomitant inguinal hernia including 1 (6.6%) patient having bilateral inguinal defects. Thirteen procedures (81%) were performed laparoscopically and 3 robotic (19%). Primary closure of the defect was performed in 11 cases (69%) and 3 cases (19%) were performed emergently due to bowel incarceration. Mean defect diameter was 3.8 (range 1 – 5) cm, mean defect area was 4.5 (range 1 – 9) cm,2 the mean mesh surface area was 12.6 * 12.2 (range 10 – 17) cm and the mean mesh area was 181 (100 – 300) cm. Fixation of the mesh to the abdominal wall was performed in 11 cases (69%). Self-fixating mesh (ProGrip, Medtronic, Minneapolis, MN) was used in 5 patients (31%) while various meshes were used in the rest of the cases. Mean surgery duration and mean LOS were 78 (range 41 – 120) minutes and 1.6 (range 1 – 3) days, respectively, with patients undergoing emergent surgery or requiring postoperative analgesics staying 2 – 3 days. Immediate postoperative complications included 2 (13%) seromas and 1 (6%) port-site hematoma, all classified as CD = 1. There were no conversions to “open” surgery and no bowel resections. Mean telephone survey follow up was 17 (range 3 – 49) months and was available for 13 patients (81%). Mean VAS scores were significantly lower at follow up compared to discharge (10.9 vs 00.5, P = .0015), 1 patient (6%) reported over-the-counter analgesia medication at 3 months postoperative, none of the patients were on opiate analgesics, there were no readmissions, none of the patients underwent additional surgery following their TAPP SH repair, and there were no mortalities.
DISCUSSION
SH are a rare variant of abdominal wall defects that have a high incarceration rate and necessitate prompt surgical intervention. Although multiple repair techniques have been described, due to paucity of data and lack of randomized control trials in the field of minimally invasive SH repairs, determining the optimal procedure of choice is challenging.
In a randomized prospective trial comparing “open” SH repairs to TEP and IPOM SH repairs, Morengo-Egea, et al.12 established that the laparoscopic approach offers a shorter LOS and decreased morbidity compared to traditional “open” approach. A systematic review of 50 articles of laparoscopic SH repairs by Barnes and McWhinnie13 illustrates IPOM as the most common utilized repair technique (n = 97, 42%) followed by TAPP (n = 80), and TEP (n = 40). The review also determined that most surgeons refrain from closing the defect primarily prior to mesh fixation and that all procedures showed low rates of recurrence and complications. In a case series and literature review by Rankin et al.14 where over 200 laparoscopic SH repairs were reviewed, the authors showed an increased LOS to 5.6 vs 1.6 days following emergent vs elective SH repairs. In a large retrospective review of SH repairs, Webber et al.15 have reviewed over 100 SH repairs in which 65 were performed “open” and 2 were TAPPs, and determined that SH are smaller in younger adults and less likely to have a peritoneal sac compared to elderly. The authors also defined three stages of SH, from small preperitoneal sac-less protrusions, peritoneal component with defects up to 5 cm, and large (> 5cm) defects distorting abdominal wall structures. Their recommendation for stages 1 and 3 advocated an “open” approach to allow visualization of herniated preperitoneal fat, which is difficult in laparoscopy, and in large hernias following reduction of hernia contents.
Similar to previous publications, our cohort of 16 minimally invasive SH TAPP repairs shows similar demographics and presentation with a female gender, left-sided, and below the arcuate line predominance of SH (Table 1). Overall LOS was 1.6 days regardless of urgency. In all cases, the hernia defect was covered with at least 4.5 cm mesh overlap in each direction. The postoperative complications occurred in 3 patients were self-limited with a CD grade of 1 without any need of readmission or intervention. The majority (n = 11, 70%) of defects were closed primarily prior to mesh fixation. Significant reduction in VAS scores at a mean follow-up time of 17 months postoperative, the lack of major complications and lack of additional surgeries following SH repair supports TAPP as a potential treatment option and a preferable approach with an acceptable safety profile and low rates of postop chronic pain.
Due to the rarity of SH occurrence, a notable common feature of our study and other prominent publications regarding SH repair, is a long study period duration which spans over more than a decade and small cohorts of patients. During this prolonged time and over the last decade, abdominal wall surgery has seen several significant advancements with the introduction of novel minimally invasive techniques and a thorough understanding of abdominal wall anatomy.8,16,17 These advancements have led to further optimization of the reconstruction approach as tailored patient-directed treatment, rather than a one size fits all approach. Furthermore, these considerable advancements may explain the shift from “open” and IPOM SH repairs to TAPP and TEP repairs.
While taking into account surgeon experience, concomitant inguinal hernias, incarceration of additional abdominal visceral organs, the TAPP repair offers multiple advantages compared to its other minimally invasive counterparts and “open” repairs. Aside from the longer LOS and increased pain, “open” repairs are prone to more wound complications and entail transection of a viable external oblique aponeurosis. Furthermore, because a concomitant inguinal hernia is a common finding during SH repairs and vice-versa, an “open” approach will require additional incisions or combining a laparoscopic procedure for a simultaneous repair. An additional advantage of TAPP is the ability to create a large space aimed at large mesh placement, which is necessary when encountering a concomitant inguinal hernia that requires simultaneous repair and covering of the entire myopectineal orifice. Although foreknowledge of concomitant inguinal hernias in all cases in our study were diagnosed pre-operatively via CT scan and/or physical examination, it is our opinion that inguinal defects found incidentally should also undergo simultaneously preperitoneal repair during the SH repair.
TAPP allows complete visualization and inspection of the preperitoneal space, the hernia sac, and the abdominal cavity, which allows potential bowel resection if needed. Furthermore, TAPP repair permits a dynamic positioning of trocars which allows creation of large peritoneal flaps and thus treating both large defects and both cranial or caudal SH in regard to the arcuate line. Because the preperitoneal fat is thicker on the lateral aspects of the abdominal wall, creating the preperitoneal space is technically favorable from the intra-abdominal approach and in obese patients. Compared to the laparoscopic TAPP approach, using the robotic platform makes the development of the preperitoneal flap even faster and easier, especially in thin patients. Although uncommon, in case peritoneal flaps tears, an IPOM repair may be performed as a salvage procedure without violation of the abdominal wall layers.
Other options for large (> 5cm) or more cranially situated SH, are enhanced-view totally extraperitoneal (eTEP) repairs, which allow creating a large preperitoneal space without entering the peritoneal cavity. The advantages of eTEP include formation of a wider space for larger meshes with a more flexible placement of trocars, in order to provide comfortable access to the groin if needed.18
It is our opinion that for such a defect as SH with a high rate of incarceration, an approach which visualizes the abdominal cavity is preferred, such as TAPP. The high rate of incarceration described throughout the literature3,19,20 of SH repairs raises a question regarding the paucity of data regarding the incidence of bowel strangulation and resection secondary to SH incarceration.21 Our cases-series of 16 patients with SH had 3 patients (19%) with incarcerated bowel but luckily did not require bowel resection. Guidelines from the World Society of Emergency Surgery and the International Endohernia Society both advocate contamination assessment following bowel resection, prior to choosing between synthetic or biologic mesh.22,23 Although severity of contamination and type of mesh play a significant role in the risk of mesh infection, TAPP repair allows positioning of the mesh in the preperitoneal plain, potentially decreasing the chances of mesh infection.
As for concern of chronic pain following mesh fixation using tackers at areas close to the neurovascular bundles,15 the significant reduction to minimal VAS scores reported by patients in our case series at an average 17 months postoperatively advocates safe utilization of TAPP SH repairs. Lower VAS scores may be explained by the fact that in the last 5 cases (31%), a self-fixating mesh was used in order to minimize the incidence of postoperative pain.
Abdominal wall surgery has made tremendous advancement in the last 3 decades and the overall minimally invasive capabilities of surgeons is becoming prevalent with more surgeons performing laparoscopic and robotic preperitoneal repairs. In our opinion, the low morbidity rate, excellent postoperative pain control, and the multiple technical advantages of TAPP make it the procedure of choice for SH repair.
Limitations of the study are inherent in its small population size and retrospective nature. The short- to midterm follow up via telephone survey is also suboptimal but a viable evaluation of chronic pain and recurrence, as the assessment is subjective to patient-reported data. Despite these limitations, our study offers some insight to approaching minimally invasive repairs of SH.
CONCLUSION
Advantages of TAPP SH repair include low postoperative chronic pain, potential low wound complications, intra-abdominal visualization of hernia contents, preperitoneal mesh placement, and repairing of concomitant inguinal hernias simultaneously.
TAPP SH repair offers several advantages compared to other minimally invasive or “open” repairs with a low rate of postoperative chronic pain.
Footnotes
Disclosure: None
Funding sources: None
Conflict of interests: Hazzan David has an honorarium for speaking engagements from Dover LTD and an educational grant from Medtronic. All other authors have nothing to disclose.
Informed consent: Dr. Shlomi Rayman declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
Shlomi Rayman, Department of General Surgery, Assuta Ashdod Public Hospital, Ashdod, Israel. Affiliated with the Faculty of Health and Science, Ben-Gurion University, Beer-Sheba, Israel..
Mnouskin Yuori, Department of General Surgery, Assuta Ashdod Public Hospital, Ashdod, Israel. Affiliated with the Faculty of Health and Science, Ben-Gurion University, Beer-Sheba, Israel..
Rachmuth Jacob, Department of General Surgery, Assuta Ashdod Public Hospital, Ashdod, Israel. Affiliated with the Faculty of Health and Science, Ben-Gurion University, Beer-Sheba, Israel..
Katz Ephraim, Minimally Invasive and Robotic Surgery, Sheba Medical Center, Tel-Hashomer, Israel. Affiliated with The Sackler Faculty of Medicine, Tel Aviv University, Israel..
Adileh Mohammad, Minimally Invasive and Robotic Surgery, Sheba Medical Center, Tel-Hashomer, Israel. Affiliated with The Sackler Faculty of Medicine, Tel Aviv University, Israel..
Segev Lior, Minimally Invasive and Robotic Surgery, Sheba Medical Center, Tel-Hashomer, Israel. Affiliated with The Sackler Faculty of Medicine, Tel Aviv University, Israel..
Hazzan David, Minimally Invasive and Robotic Surgery, Sheba Medical Center, Tel-Hashomer, Israel. Affiliated with The Sackler Faculty of Medicine, Tel Aviv University, Israel..
References:
- 1.Spangen L. Spigelian hernia. World J Surg. 1989;13(5):573–580. [DOI] [PubMed] [Google Scholar]
- 2.Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P. Spigelian hernia: surgical anatomy, embryology, and technique of repair. Am Surg. 2006;72(1):42–48. [PubMed] [Google Scholar]
- 3.Nagarsheth KH, Nickloes T, Mancini G, Solla JA. Laparoscopic repair of incidentally found spigelian hernia. JSLS. 2011;15(1):81–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moreno-Egea, A, L Girela, E, Martın, J-G, Aguayo, JL, Canteras M P. Open vs laparoscopic repair of spigelian hernia. Arch Surg. 2002;137:1266–1268. [DOI] [PubMed] [Google Scholar]
- 5.Donovan K, Denham M, Kuchta K, et al. Laparoscopic totally extraperitoneal and transabdominal preperitoneal approaches are equally effective for spigelian hernia repair. Surg Endosc. 2020;(0123456789). [DOI] [PubMed] [Google Scholar]
- 6.Jamshidian M, Stanek S, Sferra J, Jamil T. Robotic repair of symptomatic spigelian hernias: a series of three cases and surgical technique review. J Robotic Surg. 2018;12(3):557–560. [DOI] [PubMed] [Google Scholar]
- 7.LeBlanc KA, Booth WV. Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc. 1993;3(1):39–41. [PubMed] [Google Scholar]
- 8.Belyansky I, Daes J, Radu VG, et al. A novel approach using the enhanced-view totally extraperitoneal (eTEP) technique for laparoscopic retromuscular hernia repair. Surg Endosc. 2018;32(3):1525–1532. [DOI] [PubMed] [Google Scholar]
- 9.Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic ventral and incisional hernia repair in 407 patients. J Am Coll Surg. 2000;190(6):645–650. [DOI] [PubMed] [Google Scholar]
- 10.Clavien PA, Barkun J, De Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196. [DOI] [PubMed] [Google Scholar]
- 11.Daes J, Felix E. Critical view of the myopectineal orifice. Ann Surg. 2017;266(1):e1–e2. [DOI] [PubMed] [Google Scholar]
- 12.Moreno-Egea A, Torralba-Martinez JA, Morales G, Fernández T, Girela E, Aguayo-Albasini JL. Open vs laparoscopic repair of secondary lumbar hernias: a prospective nonrandomized study. Surg Endosc. 2005;19(2):184–187. [DOI] [PubMed] [Google Scholar]
- 13.Barnes TG, McWhinnie DL. Laparoscopic spigelian hernia repair: a systematic review. Surg Laparosc Endosc Percutaneous Tech. 2016;26(4):265–270. [DOI] [PubMed] [Google Scholar]
- 14.Rankin A, Kostusiak M, Sokker A. Spigelian hernia: case series and review of the literature. Visc Med. 2019;35(2):133–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Webber V, Low C, Skipworth RJE, Kumar S, de Beaux AC, Tulloh B. Contemporary thoughts on the management of spigelian hernia. Hernia. 2017;21(3):355–361. [DOI] [PubMed] [Google Scholar]
- 16.Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ. Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg. 2012;204(5):709–716. [DOI] [PubMed] [Google Scholar]
- 17.Daes J. The enhanced view-totally extraperitoneal technique for repair of inguinal hernia. Surg Endosc. 2012;26(4):1187–1189. [DOI] [PubMed] [Google Scholar]
- 18.Daes J. Enhanced-view totally extraperitoneal approach (eTEP) access in hernia repair. Cirugía Española (English Ed). 2020;98(5):249–250. [DOI] [PubMed] [Google Scholar]
- 19.Moreno-Egea A, Campillo-Soto Á, Morales-Cuenca G. Which should be the gold standard laparoscopic technique for handling spigelian hernias? Surg Endosc. 2015;29(4):856–862. [DOI] [PubMed] [Google Scholar]
- 20.Larson DW, Farley DR. Spigelian hernias: repair and outcome for 81 patients. World J Surg. 2002;26(10):1277–1281. [DOI] [PubMed] [Google Scholar]
- 21.Leff DR, Hassell J, Sufi P, Heath D. Emergency and elective laparoscopic repair of spigelian hernias: two case reports and a review of the literature. Surg Laparosc Endosc Percutaneous Tech. 2009;19(4):152–155. [DOI] [PubMed] [Google Scholar]
- 22.Bittner R, Bingener-Casey J, Dietz U, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS) - Part 1. Surg Endosc. 2014;28(1):2–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Birindelli A, Sartelli M, Di SS, et al. 2017 update of the WSES guidelines for emergency repair of complicated abdominal wall hernias. World J Emerg Surg. 2017;12(1):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]