Abstract
Aim
This study aimed to examine the impact of population density on bystander cardiopulmonary resuscitation (CPR) and survival after out-of-hospital cardiac arrest (OHCA).
Methods
Through the Danish Cardiac Arrest Registry (2001–2013), OHCAs ≥18 years of presumed cardiac cause were identified, and divided according to the OHCA location in four population density groups (inhabitants/km2) based on urban/rural area-definitions: low (<300/km2), medium (300–1499/km2), high (1500–2999/km2), very high (>3000/km2). The association between population density, bystander cardiopulmonary resuscitation (CPR) and survival was examined using logistic regression, adjusted for age, sex, comorbitidies and calendar-year.
Results
18,248 OHCAs were identified. Patients in areas of high compared to low population density were older, more often female, had more comorbidities, more witnessed arrests (very high: 59.6% versus low: 55.0%), shorter response time (very high: 10 min versus low: 14 min), but less bystander CPR (very high: 34.3% versus low: 45.1%). Thirty-day survival was higher in areas of higher population density (very high: 10.2% vs. low 5.3%), also in best-cases of witnessed arrests with bystander CPR and response time <10 min (very high: 33.6% versus low: 13.8%). The same trends were found in adjusted analyses with lower odds for bystander CPR (odds ratio [OR] 0.55 95% confidence interval [CI] 0.46–0.66) and higher odds for 30-day survival (OR 2.78, 95%CI 1.95–3.96) in the highest population density areas compared to low.
Conclusions
Having an OHCA in higher populated areas were found associated with less bystander CPR, but higher survival. Identification of area-related factors can help target future pre-hospital care.
Keywords: OHCA, Survival, Bystander CPR, Population density
Introduction
Despite improvements over time in cardiac arrest management, out-of-hospital cardiac arrest (OHCA) remains an important medical emergency associated with a poor prognosis1, 2, 3, 4, 5 that needs to be further improved.
The focus of cardiac arrest research has primarily been on factors in the “Chain-of-Survival”6 and it is well known that having a cardiac arrest in a public place,7 witnessed,5 with immediate bystander cardiopulmonary resuscitation (CPR) and defibrillation,8 and fast emergency medical service (EMS) response9 increases the chance of survival. Regional variation in all of these factors and survival has previously been described worldwide,10, 11, 12, 13 but only few studies have examined the contribution of more specific geographical factors of the cardiac arrest area including the contribution of population density (urban versus rural areas).13, 14, 15, 16 In case of an OHCA, the population density could be expected to affect the time for both recognition and intervention, and thereby survival. This is supported by a few studies primarily showing higher survival in higher populated areas.14, 15, 16 Yet, the studies have mainly examined data from limited geographic areas and limited time periods, with different definitions of urban/rural areas, and primarily focused on survival after OHCA and less on other important characteristics such as bystander interventions. Additionally, the studies have not included other potential important factors as, e.g. patient comorbidity-status that may also contribute to the association between population density, care and outcomes.13, 14, 15, 16
Therefore, this nationwide study analyzed whether the population density of the OHCA area affects cardiac arrest-related factors and survival overall and over time (2001–2013). We hypothesized that OHCAs happening in higher populated areas have a better chance of (1) having a witnessed arrest, (2) receiving bystander CPR, and (3) achieving survival.
Methods
Data sources
This nationwide study is based on the Danish Cardiac Arrest Registry in linkage with other Danish administrative registries.
Danish Cardiac Arrest Registry
Cardiac arrest data for the Danish Cardiac Arrest Registry are collected by the Danish EMS, which is activated for all medical emergencies in Denmark. For every OHCA patient attempted resuscitated (either by EMS or a bystander) they fill out a mandatory case report, ensuring a high degree of completeness of the registry. The EMS is organized into five regions with five dispatch centers working under the same nationwide legislation. The dispatchers are uniformly trained for OHCA-identification and CPR and AED-assistance for bystanders, including guidance to nearest AED.37, 38 However, data regarding dispatch-assisted CPR was not available for this study.
From the registry we included information on: time, date, and location (public vs. private home) of the arrest; witnessed-status of the arrest (unwitnessed or witnessed by bystander or EMS); if a bystander initiated CPR and/or used an automated external defibrillator (AED); the first recorded heart rhythm (shockable vs. non-shockable); time interval from recognition of OHCA (based on the time the EMS received a call and/or based on interviews of bystanders on the location) to rhythm analysis by EMS personnel, and if the patient achieved survival upon hospital arrival.
Location of OHCA
The geographical location of the OHCA was obtained from the dispatch centers and linked to urban/rural areas of Denmark with the corresponding number of inhabitants living in the area (km2) at night time with help from the Danish Geodata Agency.17 These areas are defined by Statistics Denmark with reference to guidelines from the United Nations.18
Other registries
By linkage to other Danish administrative registries via the unique civil registration number that is assigned each Danish resident, we obtained information on the patients’ age and sex from the Central Person Registry; vital status and diagnosis codes from death certificates from the National Causes of Death Registry; discharge diagnosis codes used for definition of comorbidities up to ten years prior to OHCA, as well as admission and discharge dates from the Danish National Patient Registry. All diagnosis codes were coded as in International Classification of Diseases (ICD8/ICD-10) system.
Study population
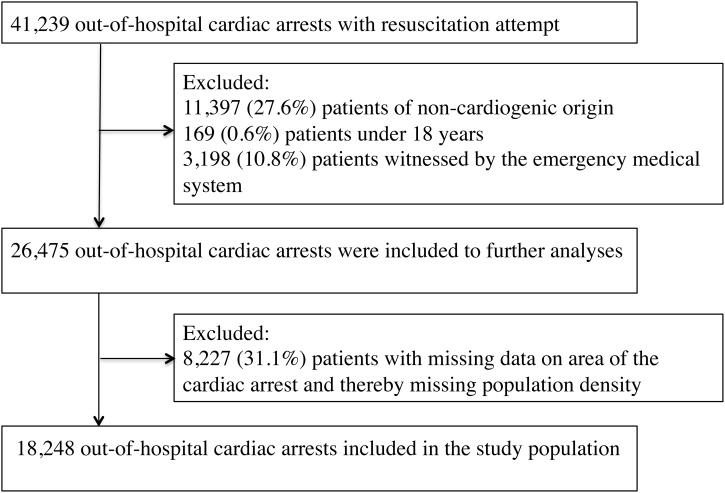
All OHCA patients of presumed cardiac cause from June 1st 2001 to December 31st 2013 with age ≥18 years and known OHCA location were included in the final study population. An OHCA of presumed cardiac cause included diagnoses with cardiac disease, unknown disease and unexpected collapse. Presumed non-cardiac causes were defined as OHCA cases with other medical disorders (not involving the above mentioned) and regardless of other diagnoses also trauma, drowning, drug-overdose and suicide attempts. Patients with presumed non-cardiac causes of arrest and EMS witnessed arrest were excluded to achieve a more homogenous study population.5 The selection process is shown in detail in Fig. 1.
Fig. 1.
Patient selection process, 2001–2013. Flowchart of the patient selection process.
The final study population was stratified according to four preselected groups of population densities of the OHCA area: (1) low <300 inhabitants/km2, (2) medium 300–1499 inhabitants/km2, (3) high 1500–2999 inhabitants/km2 and (4) very high ≥3000 inhabitants/km2. The groups were inspired by existing literature in this field15, 16 and adjusted to the Danish scale as follows. In Denmark the population density is on average 130 inhabitants/km2 ranging from rural areas of <10 inhabitants/km2 to the capital area of >3000 inhabitants/km2 with 7900 inhabitants/km2 in Copenhagen.36 Based on this we defined four groups of appropriate sizes including rural areas and small towns in the low group, and the capital area in the very high group.
Outcome measures
The main outcome measures were bystander CPR, survival upon hospital arrival and 30-day survival. They were all analyzed according to the preselected groups of population densities.
Statistics
Categorical variables were presented as frequencies with percentages and compared with Chi-square tests and continuous variables were presented as medians with interquartile-ranges and compared with Kruskall–Wallis tests. A two-sided p-value <0.05 was considered statistically significant.
Time trend analyses (2001–2013) of bystander CPR, survival upon hospital arrival and 30-day survival in relation to the pre-defined groups of population densities were performed and presented as crude percentages with associated 95% confidence intervals (CI). We tested trend over time within each population density group using the Cochran–Armitage test.
Multiple logistic regression analyses with calculated odds ratios (ORs) and associated 95%CI were used to examine the primary outcome measures (bystander CPR, survival upon hospital arrival and 30-day survival) in both overall and stratified analyses on important cardiac arrest-related factors (location of arrest, witnessed status, bystander CPR, EMS response time <10 min and initial shockable rhythm) showing both crude and adjusted estimates. We also performed (1) best-case analyses for survival of witnessed arrests with bystander CPR and EMS response time <10 min. Further, as the number of inhabitants living in the area is based on a night time population we performed analyses divided by time of the day (daytime = 7 am to 3 pm, evening time = 3 pm to 11 pm, night time = 11 pm to 7 am) for bystander CPR, survival upon hospital arrival and 30-day survival to accommodate potential daily variation due to commuting (supplemental). All adjusted models are adjusted for age in 10-years intervals, sex, comorbidities listed in Table 1 and calendar year.
Table 1.
Patient characteristics in relation to groups of population density.
| OHCA according to population density groups (18,248) |
||||||
|---|---|---|---|---|---|---|
| Low (<300/km2) | Medium (300–1499/km2) | High (1500–2999/km2) | Very high (≥3000/km2) | p-value | Missing data, n (%) | |
| Number of OHCA | 721 (4.0) | 6939 (38.0) | 7001 (38.4) | 3587 (19.7) | – | – |
| Patient factors | ||||||
| Median age (IQR) | 69 (61–76) | 72 (62–80) | 72 (62–81) | 73 (62–83) | <0.001 | – |
| Female sex, n (%) | 181 (25.1) | 2118 (30.5) | 2282 (32.6) | 1335 (37.2) | <0.001 | – |
| Comorbidities: | ||||||
| - Peripheral vascular disease, n (%) | 82 (11.4) | 774 (11.2) | 819 (11.7) | 408 (11.4) | 0.794 | – |
| - Ischemic heart disease incl. previous myocardial infarction, n (%) | 198 (27.5) | 2008 (28.9) | 2004 (28.6) | 976 (27.2) | 0.265 | – |
| - Arrhythmia, n (%) | 129 (17.9) | 1309 (18.9) | 1450 (20.7) | 755 (21.1) | 0.007 | – |
| - Congestive heart failure, n (%) | 126 (17.5) | 1330 (19.2) | 1531 (21.9) | 881 (24.6) | <0.001 | – |
| - Diabetes, n (%) | 110 (15.3) | 1109 (16.0) | 1110 (15.9) | 596 (16.6) | 0.704 | – |
| - COPD, n (%) | 74 (10.3) | 1010 (14.6) | 994 (14.2) | 589 (16.4) | <0.001 | – |
| - Malignancy, n (%) | 69 (9.6) | 708 (10.2) | 872 (12.5) | 469 (13.1) | <0.001 | – |
| Cardiac arrest-related factors | ||||||
| Arrest in public, n (%) | 226 (32.8) | 1434 (22.2) | 1626 (24.5) | 1020 (29.1) | <0.001 | 958 (5.3) |
| Witnessed arrests, n (%) | 394 (55.0) | 3633 (52.7) | 3656 (52.6) | 1535 (59.6) | <0.001 | 1102 (6.0) |
| Bystander CPR, n (%) | 324 (45.1) | 2948 (42.6) | 2494 (35.8) | 883 (34.3) | <0.001 | 1074 (5.9) |
| - Bystander CPR in witnessed arrests, n (%) | 196 (49.9) | 1836 (50.7) | 1628 (44.7) | 602 (39.4) | <0.001 | 31 (0.3) |
| - Bystander CPR in EMS response time <10 min, n (%) | 81 (37.9) | 980 (39.4) | 1155 (35.9) | 351 (35.1) | 0.024 | 21 (0.3) |
| AED use by bystander, n (%) | 17 (2.4) | 167 (2.4) | 134 (2.0) | 32 (1.5) | 0.057 | 1701 (9.3) |
| - AED use by bystander in witnessed arrests, n (%) | 16 (4.1) | 128 (3.5) | 108 (3.1) | 29 (2.3) | 0.137 | 423 (4.6) |
| Median EMS response time (estimated median time from recognition of arrest to EMS arrival) (IQR) | 14 (9–22) | 13 (8–20) | 10 (6–16) | 10 (6–16) | <0.001 | 3069 (16.8) |
| Shockable heart rhythm, n (%) | 194 (28.1) | 1807 (27.4) | 1908 (28.6) | 860 (28.5) | 0.437 | 1264 (6.9) |
| Outcomes | ||||||
| Survival upon hospital arrival, n (%) | 81 (11.5) | 1012 (14.8) | 1184 (17.6) | 513 (24.7) | <0.001 | 1913 (10.5) |
| 30-day survival, n (%) | 38 (5.3) | 487 (7.0) | 621 (8.9) | 367 (10.2) | <0.001 | – |
| - 30-day survival in survivors upon hospital arrival, n (%) | 36 (44.4) | 461 (45.6) | 575 (48.6) | 225 (43.9) | 0.265 | – |
COPD = chronic obstructive pulmonary disease; EMS = emergency medical service; IQR = interquartile range; OHCA = out-of-hospital cardiac arrest
For data management and statistical analyses we used SAS version 9.4 (SAS Institute Inc, Cary, NC, USA) and R version 3.6.119 were used in performing statistical analyses.
Ethics
This study has been approved by The Danish Data Protection Agency (2007-58-0015, local ref.nr. GEH-2014-017, I-Suite.nr. 02735). Ethical approval is not required in Denmark for retrospective register-based studies.
Results
The final study population consisted of 18,248 OHCA patients divided by: 721 patients in the low (<300 inhabitants/km2) density area; 6939 patients in the medium (300–1499 inhabitants/km2) density area; 7001 patients in the high (1500–2999 inhabitants/km2) density area and 3587 patients in the very high (≥3000 inhabitants/km2) density area (Table 1).
Patient and cardiac arrest-related factors
Table 1 shows the overall characteristics of the population. OHCAs happening in areas of the highest population density were older, more often female and with more comorbidities. They had the highest proportion of witnessed arrests, but the lowest chance of bystander CPR (very high 34.3%, high 35.8%, medium 42.6%, low 45.1%) and defibrillation (very high 1.5%, high 2.0%, medium 2.4%, low 2.4%), both overall, in witnessed arrests and in arrests with smaller intervals of estimated EMS response time (Suppl. Table 2). Response time was found shortest in the highest population density group.
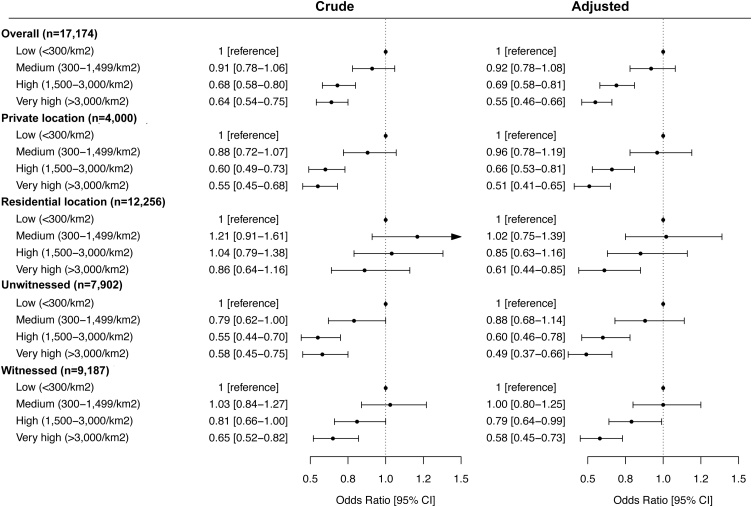
Fig. 4 shows the logistic regression analyses examining the associations of population density and bystander CPR. Higher population density was associated with lower odds of receiving bystander CPR compared to the group of the lowest population density in both crude and adjusted analyses, as well as in stratified analyses on both residential and public arrests and in witnessed and un-witnessed arrests (Fig. 4). The same trends were also observed in relation to time of the day (Suppl. Fig. 3).
Fig. 4.
Crude and adjusted association of population density and bystander CPR, Reference group = Low population density (<300/km2). Logistic regression analysis for the association of population density and bystander CPR showing the crude and the adjusted odds for bystander CPR in groups of population density: medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2) in reference to low (<300/km2). The adjusted analyses were adjusted for age, gender, calendar year and comorbidities from baseline Table 1. Odds ratio >1.00 indicates that patients in areas of medium, high and very high population densities in reference to low are positively associated with bystander CPR. CPR, cardiopulmonary resuscitation; OHCA, out-of-hospital cardiac arrest; OR, odds ratio. CPR, cardiopulmonary resuscitation; EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; OR, odds ratio.
Survival
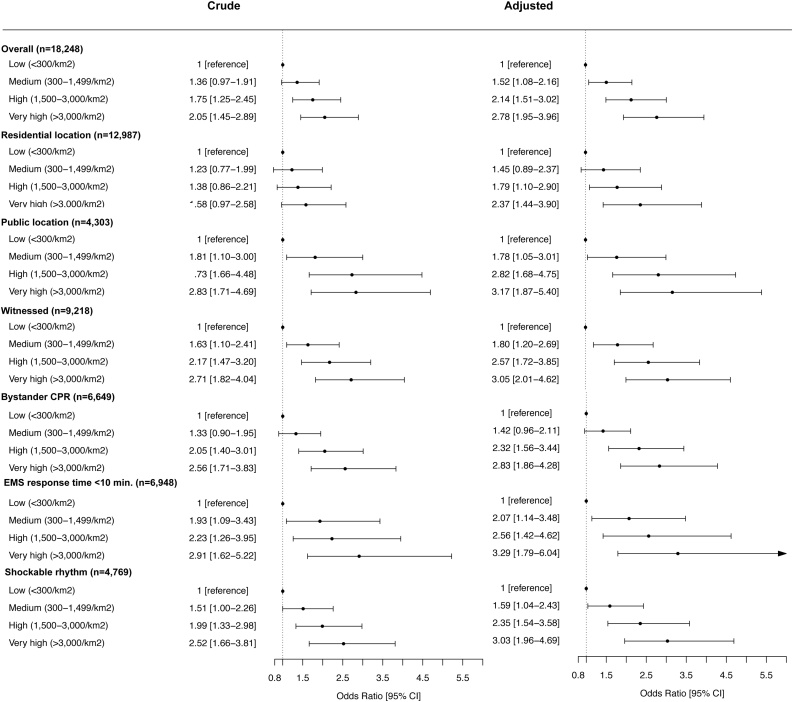
Overall survival upon hospital arrival and 30-day survival were found to be significantly higher in OHCAs in areas of higher population density (30-day survival: very high 10.2%, high 8.9%, medium 7.0%, low 5.3%) (Table 1). The same was observed in both the crude and adjusted logistic regression analyses for survival upon hospital arrival (Suppl. Fig. 1) and 30-day survival (Fig. 5) for the total population and in stratified analyses on residential and public arrests, in witnessed and un-witnessed arrests, arrests receiving bystander CPR, arrests with response time ≤10 min, in shockable arrests, and in arrests occurring in day time, evening and night (Suppl. Fig. 4). The same was found in smaller intervals of estimated EMS response time (Suppl. Table 2).
Fig. 5.
Crude and adjusted association of population density and 30-day survival. Reference group = Low population density (<300/km2). Logistic regression analysis for the association of population density and 30-day showing the crude and the adjusted odds for 30-day survival in groups of population density: medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2) were analyzed in reference to low (<300/km2). The adjusted analyses were adjusted for age, gender, calendar year, comorbidities from baseline Table 1 and EMS response time. Odds ratio >1.00 indicates that patients in areas of medium, high and very high population densities in reference to low are positively associated with 30-day survival. CPR, cardiopulmonary resuscitation; EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; OR, odds ratio.
Bystander CPR and survival over time
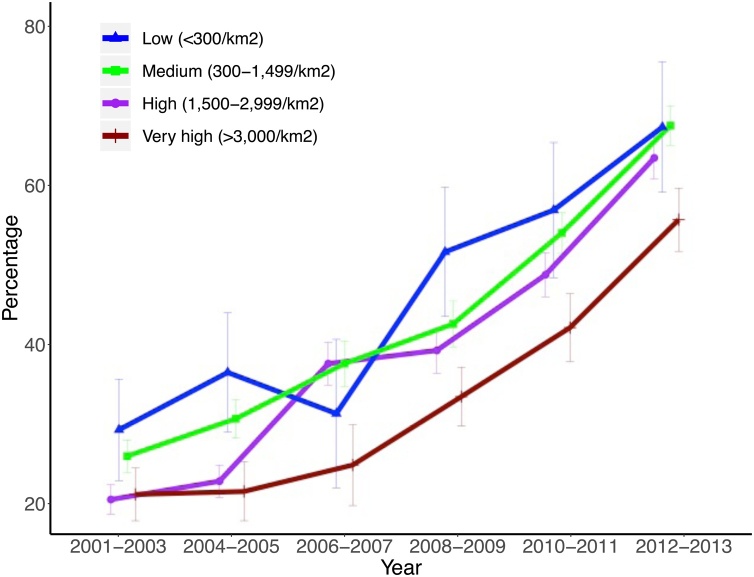
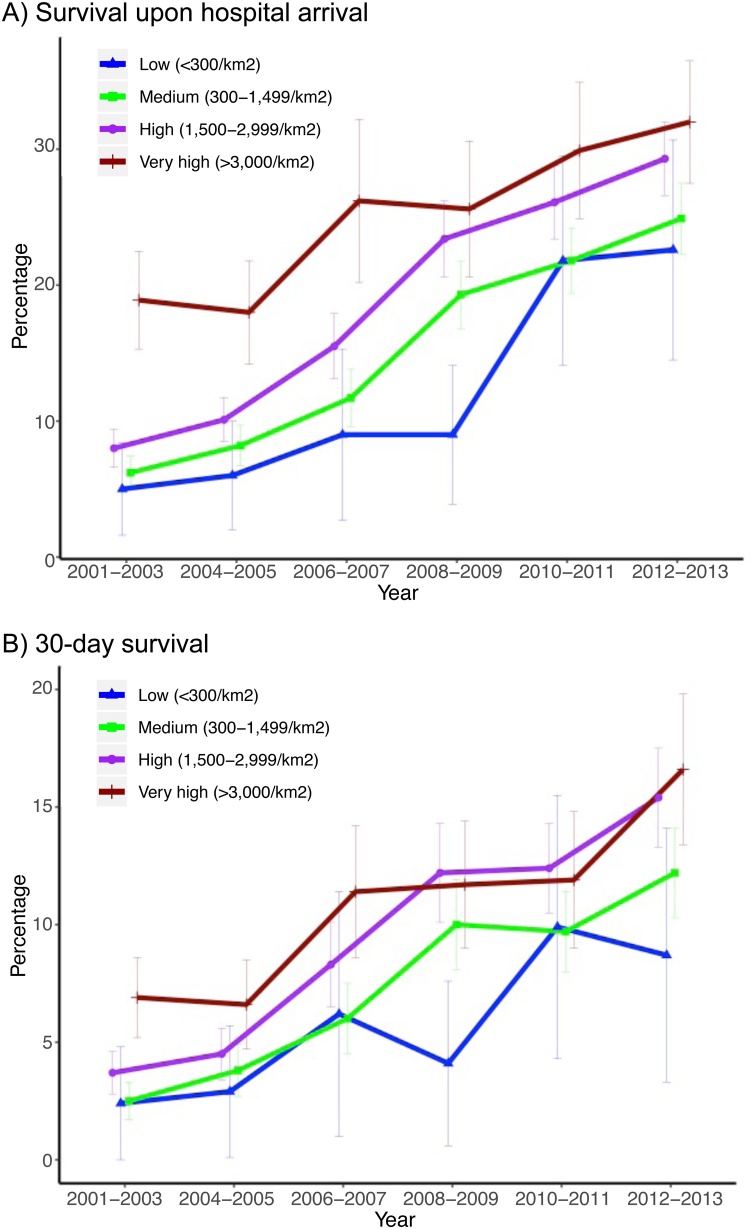
Over time (2001–2013) both bystander CPR rate and survival outcomes increased significantly in all four population density groups (Figs. 2 and 3).
Fig. 2.
Time trends of bystander CPR in groups of population densities. Time trends (2001–2013) of bystander CPR in OHCA patients with associated 95% confidence intervals according to groups of population densities: low (<300/km2), medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2). CPR, cardiopulmonary resuscitation; OHCA, out-of-hospital cardiac arrest.
Fig. 3.
Time trends of survival in groups of population densities. Time trends (2001–2013) of survival upon hospital arrival (A) and 30-day survival (B) in OHCA patients with associated 95% confidence intervals according to groups of population densities: low (<300/km2), medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2). OHCA, out-of-hospital cardiac arrest.
Supplemental
We compared the patients with known address of arrest (patients included in our study population) to the patients excluded due to unknown address of arrest in Suppl. Table 1. The patients with unknown address had more public located arrests, a higher proportion of bystander CPR and a shorter response time, but no significant difference was observed in 30-day survival between the two groups: p = 0.762.
Discussion
This nationwide study from Denmark aimed to examine how the population density of the OHCA area potentially affects cardiac arrest-related factors and survival after OHCA. Despite that we found significant increases in both bystander CPR and survival over time in all our four population density groups, we found that cardiac arrests happening in higher populated areas received less bystander CPR, but had higher survival upon hospital arrival and 30-day survival. These area-related differences persisted in adjusted analyses and in analyses stratified after known important factors as location of arrest, witnessed status, bystander CPR, EMS response time and shockable rhythm.
From 2001 to 2013 we found significant increases in both bystander CPR and survival in all four population density groups, indicating that the initiatives in OHCA management5 are working irrespective of population density in Denmark (urban versus rural areas). However, when we overall compared cardiac arrest-related factors and survival according to the four groups differences were observed.
Our study found that OHCAs happening in areas of higher population density were associated with more negative prognostic factors as older age20 and higher prevalence of comorbidities,21 and lower bystander CPR rates even though they had the highest proportion of witnessed arrests. The difference in bystander CPR persisted in adjusted analyses both overall and stratified in residential or public located arrests, witnessed or unwitnessed arrests, and in relation to time of the day. This finding is supported by a few other studies and has earlier been found difficult to explain.15, 16, 22 Studies have suggested accumulation of area-specific patient and population factors including differences in CPR training23, 24 and perhaps a bigger individual investment in the local area in the smaller communities of lower population density, with a different relationship between people in smaller communities than in the cities. For example in Denmark voluntary first aid groups in smaller local communities have been introduced on the individuals own initiative.25, 26 Such initiatives together with strategic placement of AEDs, CPR- and AED-training could be important strategies for improvements in more remote areas. Another aspect could be due to selection, i.e. there could be area-related differences in whether patients are recognized and registered either as a cardiac arrest with a resuscitation attempt (patients included in the registry and thereby in this study), or are being declared “found dead” by an EMS physician (patient not included in the registry and thereby not in this study). Hence, if patients without bystander CPR more often are declared dead in rural areas than in cities, and thus are not registered in the cardiac arrest registry, that could explain the observed higher rate of bystander CPR in areas of lower population density There could also be differences in the assistance from the dispatch centers when calling 9-1-1 in for example arrest-recognizing and CPR-guidance. Though, we would not expect this to affect our results substantially, since the EMS and the dispatch centers in Denmark are following overall the same training and guidelines. Unfortunately, our study does not provide data to examine these factors further.
Despite that, patients in higher populated areas received less bystander CPR, they still had higher survival, both in adjusted analyses and when stratifying after important prognostic factors for survival: location witnessed status, arrests receiving bystander CPR, arrests with EMS response time ≤10 min and shockable arrests. EMS response time has earlier been suggested as an important factor related to both population density and survival,14, 16, 27, 28 and survival from OHCA has been found to decline with increasing response time.39 This was also found by our study, though when examining survival in relation to response time ≤10 min, in smaller intervals of response time and in best-case scenario of witnessed arrests with bystander CPR and response time ≤10 min, survival was still higher in areas of higher population density. Altogether, other factors than represented in the first three links of the “Chain-of-Survival” seem to play a role for the observed survival differences between population density groups. Previous studies have suggested area-level differences in general patient health including comorbidities, risk factors, and socioeconomic factors that all have been found associated with bystander interventions and survival, including area-level differences in when and how people contact the healthcare system.8, 29 However, our analyses were adjusted for comorbidities and overall no differences in healthcare contacts between urban and rural areas have been observed in Denmark.30 It could also be speculated that area-level differences in the structure and function of the EMS including geographical factors as driving distances to nearest hospital and/or heart center, as well as the hospital care could have an impact.31, 32, 33 However, in Denmark, all OHCA patients are transported to a heart center following the same guidelines for hospital care, and even though the most heart centers are located in high-density areas with the shortest distances from patient to centers for high-density patients, studies from Denmark have previously showed no overall difference in outcome in relation to time/distance from patient to hospital.40, 41 We would therefore not expect this to have a major impact on our results.
This study provides knowledge on how bystander interventions, the EMS and the survival outcomes differ geographically, and improvements are still needed. The observed differences are probably a result of many different factors, however tailored strategies of education, CPR- and AED-training,34, 35 strategic placement of AEDs, and citizen responders in more remote areas are probably still the best investment to strengthen the important modifiable factors (early recognition and early bystander intervention) to try and improve survival further. But more research on this field is warranted.
Limitations
This observational study presents associations and do not prove causality. Hence, our data does not allow us to conclude which exact factors that are responsible for the observed differences. Also, the study was limited by the data available; more data on, e.g. dispatch center assistance, EMS registration of OHCA patients including arrests that are declared dead without resuscitation attempt, and in-hospital factors are only some of the missing information that could have helped explore the density-related differences further. Another limitation is the 31.1% observations with missing geographical information and thereby unknown population density. This proportion was excluded from the final study population and all main analyses. However, we performed a sensitivity analysis (Suppl. Table 1) comparing OHCA patients with unknown geographical information with the included OHCA patients with known geographical information on the cardiac arrest-related factors and the survival outcomes. This showed small differences in cardiac arrest-related factors but no significant difference in 30-day survival. Overall we did not find any indication of informative missing or that the patients with missing geographical information was associated with one specific group of population density; thus missing geographical information should not have biased our results. Additionally our data did not allow us to calculate incidence of OHCA for the four density-groups since we did not have information about the size of the background population according to the population density groups. A third limitation is that our population density data is based on the Danish night population that for some areas could be different during the daytime due to commuting. We tried to explore the potential effect of this by examining the outcomes in arrests occurring in three separate times of the day, which showed overall the same trends as our main results. Hence, this limitation should not have affected the conclusion of the study.
Conclusion
Over time bystander CPR and survival increased in all four groups of population density, yet overall higher population density was found associated with lower proportion of bystander CPR, but higher survival. These differences persisted in adjusted analyses and when stratifying on important cardiac arrest-related factors. This knowledge can help future strategies in pre-hospital cardiac arrest management with supporting first-responder programs in specific locations.
Sources of funding
Dr. Møller has received a grant from Karen Elise Jensens Fond. Dr. Malta Hansen has received grants from TrygFonden, Helsefonden, and the Laerdal Foundation. Dr. Hansen has received a grant from TrygFonden. Dr. Kragholm has received grants from the Laerdal Foundation. Dr. Lippert is a board member for TrygFonden. Dr. Køber has received payment for speaking at a symposium arranged by Servier. Dr. Folke has received a grant from TrygFonden and the Novo Nordisk Foundation. Dr. Gislason has received a grant from the Novo Nordisk Foundation. Dr. Torp-Pedersen has received grants from Bayer and Novo Nordisk.
Conflict of interest
None of the other authors have reported any conflicts of interest.
Acknowledgements
The Danish foundation TrygFonden has supported this study, but had no influence in design, management, data collection, analysis, interpretation of data, preparation, reviewing, reporting, approval of the manuscript and the submission-decision for publication. TrygFonden also supports the Danish Cardiac Arrest Registry, but has no commercial interests in the area of OHCAs.
The Danish Cardiac Arrest Registry data are based on the EMS filling out an obligatory case report for every OHCA – therefore a great thank you to this personnel.
Footnotes
Supplementary material related to this article can be found, in the online version, at http://dx.doi.org/10.1016/j.resplu.2020.100036.
Appendix A. Supplementary data
The following are Supplementary data to this article:
Supplemental Fig. 1 Crude and adjusted association of population density and survival upon hospital arrival. Reference group = Low population density (<300/km2). Logistic regression analysis for the association of population density and survival upon hospital arrival showing the crude and the adjusted odds for survival upon hospital arrival in groups of population density: medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2) were analyzed in reference to low (<300/km2). The adjusted analyses were adjusted for age, gender, calendar year, comorbidities from baseline Table 1, and EMS response time. Odds ratio >1.00 indicates that patients in areas of medium, high and very high population densities in reference to low are positively associated with survival upon hospital arrival.
Supplemental Fig. 2 Survival in best-case scenario of witnessed arrests with bystander CPR and response time <10 min in groups of population density. Percentages of survival upon hospital arrival and 30-day survival with associated 95% confidence intervals in best-case scenario of witnessed arrest with bystander CPR and response time <10 min in relation to groups of population densities (low (<300/km2), medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2). CPR, cardiopulmonary resuscitation; OHCA, out-of-hospital cardiac arrest.
Supplemental Fig. 3 Crude and adjusted association of population density and bystander CPR in relation to time of the day. Reference group = Low population density (<300/km2). Logistic regression analysis for the association of population density and 30-day showing the crude and the adjusted odds for bystander CPR in groups of population density: medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2) in reference to low (<300/km2). The adjusted analyses were adjusted for age, gender, calendar year, and comorbidities from baseline Table 1. Odds ratio >1.00 indicates that patients in areas of medium, high and very high population densities in reference to low are positively associated with 30-day survival. CPR, cardiopulmonary resuscitation; OHCA, out-of-hospital cardiac arrest; OR, odds ratio.
Supplemental Fig. 4 Crude and adjusted association of population density and survival in relation to time of the day. Reference group = Low population density (<300/km2). Logistic regression analysis for the association of population density, survival upon hospital arrival and 30-day survival in relation to time of the day (daytime = 7 am to 3 pm, evening time = 3 pm to 11 pm, night time = 11 pm to 7 am) showing the crude and the adjusted odds for survival in groups of population density: medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2) in reference to low (<300/km2). The adjusted analyses were adjusted for age, gender, calendar year, and comorbidities from baseline Table 1. Odds ratio >1.00 indicates that patients in areas of medium, high and very high population densities in reference to low are positively associated with 30-day survival. CPR, cardiopulmonary resuscitation; OHCA, out-of-hospital cardiac arrest; OR, odds ratio.
References
- 1.Benjamin E.J., Virani S.S., Callaway C.W. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–e492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 2.Atwood C., Eisenberg M.S., Herlitz J., Rea T.D. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation. 2005;67:75–80. doi: 10.1016/j.resuscitation.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 3.Hollenberg J., Herlitz J., Lindqvist J. Improved survival after out-of-hospital cardiac arrest is associated with an increase in proportion of emergency crew – witnessed cases and bystander cardiopulmonary resuscitation. Circulation. 2008;118:389–396. doi: 10.1161/CIRCULATIONAHA.107.734137. [DOI] [PubMed] [Google Scholar]
- 4.Sasson C., Rogers M.A., Dahl J., Kellermann A.L. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 5.Wissenberg M., Lippert F.K., Folke F. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310:1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
- 6.2017. Association AH. https://cpr.heart.org/AHAECC/CPRAndECC/AboutCPRFirstAid/CPRFactsAndStats/UCM_475731_CPR-Chain-of-Survival.jsp. [Google Scholar]
- 7.Folke F., Gislason G.H., Lippert F.K. Differences between out-of-hospital cardiac arrest in residential and public locations and implications for public-access defibrillation. Circulation. 2010;122:623–630. doi: 10.1161/CIRCULATIONAHA.109.924423. [DOI] [PubMed] [Google Scholar]
- 8.Sasson C., Magid D.J., Chan P. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367:1607–1615. doi: 10.1056/NEJMoa1110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rajan S., Wissenberg M., Folke F. Association of bystander cardiopulmonary resuscitation and survival according to ambulance response times after out-of-hospital cardiac arrest. Circulation. 2016;134:2095–2104. doi: 10.1161/CIRCULATIONAHA.116.024400. [DOI] [PubMed] [Google Scholar]
- 10.Girotra S., van Diepen S., Nallamothu B.K. Regional variation in out-of-hospital cardiac arrest survival in the United States. Circulation. 2016;133:2159–2168. doi: 10.1161/CIRCULATIONAHA.115.018175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nichol G., Thomas E., Callaway C.W. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grasner J.T., Lefering R., Koster R.W. EuReCa ONE-27 nations, ONE Europe, ONE Registry: a prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 13.Hiltunen P., Kuisma M., Silfvast T. Regional variation and outcome of out-of-hospital cardiac arrest (ohca) in Finland – the Finnresusci study. Scand J Trauma Resusc Emerg Med. 2012;20:80. doi: 10.1186/1757-7241-20-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stromsoe A., Svensson L., Claesson A., Lindkvist J., Lundstrom A., Herlitz J. Association between population density and reported incidence, characteristics and outcome after out-of-hospital cardiac arrest in Sweden. Resuscitation. 2011;82:1307–1313. doi: 10.1016/j.resuscitation.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 15.Nehme Z., Andrew E., Cameron P.A. Population density predicts outcome from out-of-hospital cardiac arrest in Victoria, Australia. Med J Aust. 2014;200:471–475. doi: 10.5694/mja13.10856. [DOI] [PubMed] [Google Scholar]
- 16.Yasunaga H., Miyata H., Horiguchi H. Population density, call-response interval, and survival of out-of-hospital cardiac arrest. Int J Health Geograph. 2011;10:26. doi: 10.1186/1476-072X-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Danish Geodata Agency. Geocoding of the Danish cardiac arrest data. https://eng.gst.dk [cited 2020].
- 18.Statistics Denmark . 2019. Information about urban/rural areas of Denmark. http://www.dst.dk/da/Statistik/dokumentation/statistikdokumentation/byopgoerelsen/indhold [cited 2020] [Google Scholar]
- 19.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2019. R: a language and environment for statistical computing. https://www.R-project.org/ [Google Scholar]
- 20.Wissenberg M., Folke F., Hansen C.M. Survival after out-of-hospital cardiac arrest in relation to age and early identification of patients with minimal chance of long-term survival. Circulation. 2015;131:1536–1545. doi: 10.1161/CIRCULATIONAHA.114.013122. [DOI] [PubMed] [Google Scholar]
- 21.Lee C.C., Tsai M.S., Fang C.C. Effects of pre-arrest comorbidities on 90-day survival of patients resuscitated from out-of-hospital cardiac arrest. Emerg Med J. 2011;28:432–436. doi: 10.1136/emj.2009.087593. [DOI] [PubMed] [Google Scholar]
- 22.Masterson S., Wright P., O’Donnell C. Urban and rural differences in out-of-hospital cardiac arrest in Ireland. Resuscitation. 2015;91:42–47. doi: 10.1016/j.resuscitation.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 23.Axelsson A.B., Herlitz J., Holmberg S., Thoren A.B. A nationwide survey of CPR training in Sweden: foreign born and unemployed are not reached by training programmes. Resuscitation. 2006;70:90–97. doi: 10.1016/j.resuscitation.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 24.Straney L.D., Bray J.E., Beck B., Bernard S., Lijovic M., Smith K. Are sociodemographic characteristics associated with spatial variation in the incidence of OHCA and bystander CPR rates? A population-based observational study in Victoria, Australia. BMJ Open. 2016;6:e012434. doi: 10.1136/bmjopen-2016-012434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.2016. Article about voluntary first aid groups in a smaller local community. https://amtsavisen.dk/randers/Det-kan-godt-knase-lidt-naar-man-giver-hjertemassage/artikel/255578 [cited 2016] [Google Scholar]
- 26.2013. Article about voluntary first aid groups in smaller local communities, Danish people wants to help Danish people in need. https://www.dr.dk/nyheder/regionale/midtvest/udkants-danskere-vil-hjaelpe-hinanden-i-noed. [Google Scholar]
- 27.Nordberg P., Jonsson M., Forsberg S. The survival benefit of dual dispatch of EMS and fire-fighters in out-of-hospital cardiac arrest may differ depending on population density – a prospective cohort study. Resuscitation. 2015;90:143–149. doi: 10.1016/j.resuscitation.2015.02.036. [DOI] [PubMed] [Google Scholar]
- 28.Jennings P.A., Cameron P., Walker T., Bernard S., Smith K. Out-of-hospital cardiac arrest in Victoria: rural and urban outcomes. Med J Aust. 2006;185:135–139. doi: 10.5694/j.1326-5377.2006.tb00498.x. [DOI] [PubMed] [Google Scholar]
- 29.Vaillancourt C., Lui A., De Maio V.J., Wells G.A., Stiell I.G. Socioeconomic status influences bystander CPR and survival rates for out-of-hospital cardiac arrest victims. Resuscitation. 2008;79:417–423. [Google Scholar]
- 30.2016. Ministry of Health D. https://sundhedsdatastyrelsen.dk/-/media/sds/filer/find-tal-og-analyser/sundhedsvaesnet/almen-praksis/almen-praksis_befokningens-kontakter_sum.pdf. [Google Scholar]
- 31.Stiell I.G., Wells G.A., Field B. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med. 2004;351:647–656. doi: 10.1056/NEJMoa040325. [DOI] [PubMed] [Google Scholar]
- 32.Spaite D.W., Stiell I.G., Bobrow B.J. Effect of transport interval on out-of-hospital cardiac arrest survival in the OPALS study: implications for triaging patients to specialized cardiac arrest centers. Ann Emerg Med. 2009;54:248–255. doi: 10.1016/j.annemergmed.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 33.Woodall J., McCarthy M., Johnston T., Tippett V., Bonham R. Impact of advanced cardiac life support-skilled paramedics on survival from out-of-hospital cardiac arrest in a statewide emergency medical service. Emerg Med J. 2007;24:134–138. doi: 10.1136/emj.2005.033365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Malta Hansen C., Kragholm K., Pearson D.A. Association of bystander and first-responder intervention with survival after out-of-hospital cardiac arrest in North Carolina, 2010–2013. JAMA. 2015;314:255–264. doi: 10.1001/jama.2015.7938. [DOI] [PubMed] [Google Scholar]
- 35.White R.D., Bunch T.J., Hankins D.G. Evolution of a community-wide early defibrillation programme experience over 13 years using police/fire personnel and paramedics as responders. Resuscitation. 2005;65:279–283. doi: 10.1016/j.resuscitation.2004.10.018. [DOI] [PubMed] [Google Scholar]
- 36.Anon. https://www.statistikbanken.dk/BY3.
- 37.Hansen C.M., Lippert F.K., Wissenberg M. Temporal trends in coverage of historical cardiac arrests using a volunteer-based network of automated external defibrillators accessible to laypersons and emergency dispatch centers. Circulation. 2014;130:1859–1867. doi: 10.1161/CIRCULATIONAHA.114.008850. [DOI] [PubMed] [Google Scholar]
- 38.Karlsson L., Malta Hansen C., Wissenberg M. Automated external defibrillator accessibility is crucial for bystander defibrillation and survival: a registry-based study. Resuscitation. 2019;136:30–37. doi: 10.1016/j.resuscitation.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 39.Rajan S., Wissenberg M., Folke F. Association of bystander cardiopulmonary resuscitation and survival according to ambulance response times after out-of-hospital cardiac arrest. Circulation. 2016;134:2095–2104. doi: 10.1161/CIRCULATIONAHA.116.024400. [DOI] [PubMed] [Google Scholar]
- 40.Tranberg T., Lippert F.K., Christensen E.F. Distance to invasive heart centre, performance of acute coronary angiography, and angioplasty and associated outcome in out-of-hospital cardiac arrest: a nationwide study. Eur Heart J. 2017;38:1645–1652. doi: 10.1093/eurheartj/ehx104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mills E.H.A., Aasbjerg K., PhD M.D., Hansen S.M. Prehospital time and mortality in patients requiring a highest priority emergency medical response: a Danish registry-based cohort study. BMJ Open. 2019;9:e023049. doi: 10.1136/bmjopen-2018-023049. Published 2019 November 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Fig. 1 Crude and adjusted association of population density and survival upon hospital arrival. Reference group = Low population density (<300/km2). Logistic regression analysis for the association of population density and survival upon hospital arrival showing the crude and the adjusted odds for survival upon hospital arrival in groups of population density: medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2) were analyzed in reference to low (<300/km2). The adjusted analyses were adjusted for age, gender, calendar year, comorbidities from baseline Table 1, and EMS response time. Odds ratio >1.00 indicates that patients in areas of medium, high and very high population densities in reference to low are positively associated with survival upon hospital arrival.
Supplemental Fig. 2 Survival in best-case scenario of witnessed arrests with bystander CPR and response time <10 min in groups of population density. Percentages of survival upon hospital arrival and 30-day survival with associated 95% confidence intervals in best-case scenario of witnessed arrest with bystander CPR and response time <10 min in relation to groups of population densities (low (<300/km2), medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2). CPR, cardiopulmonary resuscitation; OHCA, out-of-hospital cardiac arrest.
Supplemental Fig. 3 Crude and adjusted association of population density and bystander CPR in relation to time of the day. Reference group = Low population density (<300/km2). Logistic regression analysis for the association of population density and 30-day showing the crude and the adjusted odds for bystander CPR in groups of population density: medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2) in reference to low (<300/km2). The adjusted analyses were adjusted for age, gender, calendar year, and comorbidities from baseline Table 1. Odds ratio >1.00 indicates that patients in areas of medium, high and very high population densities in reference to low are positively associated with 30-day survival. CPR, cardiopulmonary resuscitation; OHCA, out-of-hospital cardiac arrest; OR, odds ratio.
Supplemental Fig. 4 Crude and adjusted association of population density and survival in relation to time of the day. Reference group = Low population density (<300/km2). Logistic regression analysis for the association of population density, survival upon hospital arrival and 30-day survival in relation to time of the day (daytime = 7 am to 3 pm, evening time = 3 pm to 11 pm, night time = 11 pm to 7 am) showing the crude and the adjusted odds for survival in groups of population density: medium (300–1499/km2), high (1500–2999/km2) and very high (>3000/km2) in reference to low (<300/km2). The adjusted analyses were adjusted for age, gender, calendar year, and comorbidities from baseline Table 1. Odds ratio >1.00 indicates that patients in areas of medium, high and very high population densities in reference to low are positively associated with 30-day survival. CPR, cardiopulmonary resuscitation; OHCA, out-of-hospital cardiac arrest; OR, odds ratio.