Abstract
Background
Despite the proven effectiveness of rapid initiation of cardiopulmonary resuscitation (CPR) for patients with out-of-hospital cardiac arrest (OHCA) by bystanders, fewer than half of the victims actually receive bystander CPR. We aimed to review the evidence of the barriers and facilitators for bystanders to perform CPR.
Methods
This scoping review was conducted as part of the continuous evidence evaluation process of the International Liaison Committee on Resuscitation (ILCOR), and followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews. This review included studies assessing barriers or facilitators for the lay rescuers to perform CPR in actual emergency settings and excluded studies that overlapped with other ILCOR systematic reviews/scoping reviews (e.g. dispatcher instructed CPR etc). The key findings were classified into three kinds of factors: personal factors; CPR knowledge; and procedural issues.
Results
We identified 18 eligible studies. Of these studies addressing the reduced willingness to respond to cardiac arrest, 14 related to “personal factors”, 3 to “CPR knowledge”, and 2 to “procedural issues”. On the other hand, we identified 5 articles assessing factors increasing bystanders’ willingness to perform CPR. However, we observed significant heterogeneity among study populations, methodologies, factors definitions, outcome measures utilized and outcomes reported.
Conclusions
We found that a number of factors were present in actual settings which either inhibit or facilitate lay rescuers’ performance of CPR. Interventional strategies to improve CPR performance of lay rescuers in the actual settings should be established, taking these factors into consideration.
Keywords: Out-of-hospital cardiac arrest, Willingness to perform CPR, Lay rescuers, Scoping review
Introduction
Rationale
The “chain of survival” plays a well-known key role for the successful resuscitation of patients with out-of-hospital cardiac arrest (OHCA).1, 2 Many studies have demonstrated that bystander-initiated CPR and rapid public-access defibrillation (PAD) with automated external defibrillators (AEDs) significantly improve the likelihood of survival.3, 4, 5, 6, 7 Especially, the combination of bystander CPR and PAD leads to a synergistic positive effect on outcome after OHCA.8 Therefore, a lay rescuer plays an essential role in improving outcome after OHCA.
Despite the proven effectiveness of rapid initiation of CPR and PAD by bystanders, bystander CPR is performed in fewer than 50% of cases and AEDs are used even less often in most areas across the world, even if they are frequently available in public places.9, 10, 11 Data from the Cardiac Arrest Registries to Enhance Survival observed substantial variation among counties regarding survival and neurologic outcome, which came partially from the wide range of frequencies of bystander CPR and PAD.12, 13 Therefore, as previous guidelines have emphasized, increasing the willingness of individuals to respond to cardiac arrest (with early recognition, calling for help, initiation of CPR, and use of an AED) is vital to improve survival after OHCA.14 A better understanding of the reasons why the proportion of bystander CPR and PAD remains low is essential to establish effective interventions to increase bystander response and improve survival after OHCA.
Objectives
We aimed to review the evidence for barriers and facilitators for bystanders to perform CPR. ‘Willingness of bystanders to perform CPR’ was selected for a new scoping review by the International Liaison Committee on Resuscitation (ILCOR) Education, Implementation and Teams (EIT) Task Force in this current round of evidence assessment because of the low incidence of provision of CPR and AED use by bystanders in most areas across the world and thus the need to identify barriers and facilitators for bystanders to perform CPR.
Methods
Protocol
This study was conducted as part of the ILCOR EIT Task Force continuous evidence evaluation process. The task force ranked all their research questions, and this topic was decided to be of high interest for the current review phase. Before starting the evidence review for this topic, the EIT Task Force discussed which type of review should be performed, i.e. a narrative summary of the barriers or facilitators to perform CPR as in the International Consensus on CPR and Emergency Cardiovascular Care Science With Treatment Recommendations [CoSTR] 201014 or a systematic review to evaluate interventions to improve willingness to perform CPR as in CoSTR 201515. In general, scoping reviews are performed instead of systematic reviews for the purpose of determining the scope or coverage of a body of literature on a giving topic as well as an overview (broad or detailed), or identifying key factors related to a certain topic and knowledge gaps.16 Therefore, it was decided to conduct a scoping review with a narrative summary on barriers or facilitators for the lay rescuers to perform CPR in actual emergency settings to focus more on nowadays implementation topics than when the PICO was originally drafted about 15 years ago. A specific review protocol for this scoping review was approved in advance according to the ILCOR Task Force Scoping Reviews (TFScR) Guidance v 1.05.17 This review follows a recommended methodological framework18 and the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR).19
The EIT Task Force agree to follow the PICO (Population. Intervention, Comparators, Outcome) approach and formulated the question for the review: In actual situation of OHCA, bystanders (lay persons) (P), factors that increase the willingness of bystanders to perform CPR (I), factors that decrease the willingness of bystanders to perform CPR (C), bystander CPR performance or willingness to provide CPR (O).
Randomized controlled trials (RCTs) and nonrandomized studies (non-randomized controlled trials, interrupted time series, controlled before-and-after studies, cohort studies, and questionnaire surveys) over all years were eligible for inclusion.
Simulation studies, survey data not from actual experience, unpublished studies (e.g., conference abstracts, trial protocols), letters, editorials, comments, case reports, systematic reviews, and grey literature, as well as studies that overlap with other ILCOR systematic reviews or scoping reviews (e.g. dispatcher instructed CPR, Community initiatives to improve CPR) and non-English studies were excluded from this scoping review.
Information sources and search
A formal literature search strategy was developed by a local information specialist, and the bibliographic databases PubMed/Medline and Cochrane Database of Systematic Reviews were searched for the eligibility, on 29 November 2019. The search was re-run on July 18, 2020 – but no additional studies were identified. The detailed search strategy is described in Supplemental Table 1. Furthermore, the additional eligible studies were searched by retrieving and screening references cited by previous ILCOR CoSTRs,14, 15 prior related systematic reviews20, 21 and included studies.
Selection of sources of evidence
Three reviewers (SA, PT, TM) screened the found articles independently through the following two screening stages. First, the search results were screened by title and abstract for relevance to the PICO by the reviewers with the use of Rayyan.22 Second, after eliminating non-relevant studies the reviewers evaluated the eligibility of studies addressing the PICO by thorough screening of the full texts. Disagreements were resolved by discussion with another investigator (TI).
Data charting process and synthesis of results
Data charting was done with the use of the format outlined in the ILCOR TFScR Guidance v 1.0.5 (Supplemental Table).17 Data of each article were charted independently by pairs of reviewers (TM and TI, or SA and PT), discussed, updated and summarized. Disagreements were discussed and resolved by other reviewers. We extracted data on year, study country, study characteristics (design, key factor, patient, duration, size), and factors that increase or decrease the willingness of bystanders to perform CPR.
Key findings were summarized for each study and the synthesis was edited (TI). The key findings were classified into three categories (personal factors, CPR knowledge, and procedural issues) according to a recent qualitative review of emergency calls.22
Results
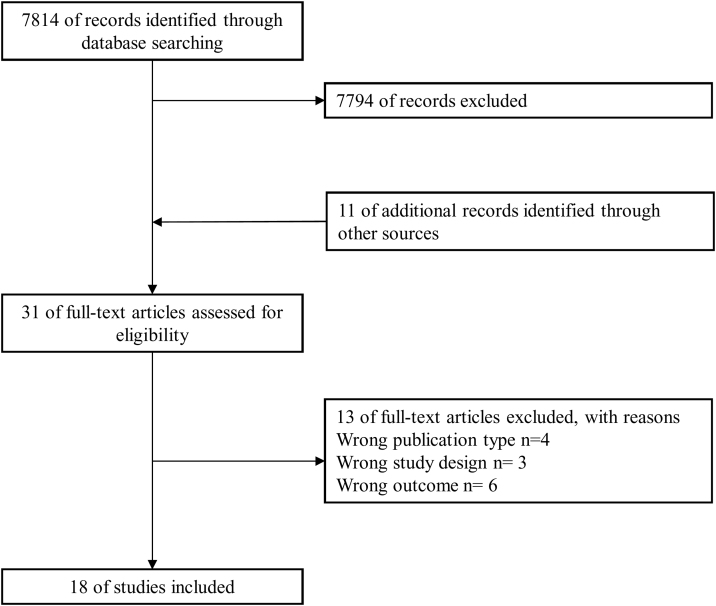
Electronic literature searches yielded 7814 articles. After the first screening, 20 potentially eligible studies were identified for full text assessment. Following the second screening and hand search, a total of 18 articles were considered eligible (Fig. 1).23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40 Characteristics and results of individual sources of evidence were summarized in Table 1. There were no randomized controlled trials identified. The most common study design was 7 prospective and 7 retrospective observational, and 3 questionnaire surveys were identified. The number of patients included in the studies ranged from 12028 to 816,315.39 More than half of the included articles were published after the year of 2015, when the most recent guideline was published.23, 26, 27, 29,31, 32, 35, 36,38, 39, 40 The study population and setting showed significant heterogeneity among the included studies.
Fig. 1.
Overview of study selection process.
Table 1.
Characteristics and results of individual sources of evidence.
| Citation: 1st Author, Year, 1st page (Country) | Study characteristics (design, key factor, patient, duration, size) | Factors that increase or decrease the willingness of bystanders to perform CPR | Key findings |
|---|---|---|---|
| Swor, 2011, 596 (United States) | • Prospective observational study • CPR training • Individuals who called 911 at the time of an OHCA • 1997 – 2003 • N = 684 |
Promote CPR: • Bystander age (<50yrs) • CPR training (within 5yrs) • High school education Barriers to CPR: • Panic • Lack of confidence • Afraid to hurt Patient |
CPR provision was more common in CPR-trained bystanders with more than a high-school education and when CPR training had been within five years. "Bystander age (<50 yr) (AOR, 2.30; 95% CI, 1.39−3.79), Bystander CPR trained (AOR, 6.63; 95% CI, 3.51−12.5), and bystander educational level (beyond high school)(AOR, 1.95; 95% CI, 1.23−3.09) In particular, among CPR-trained bystanders, CPR training within 5yrs (AOR, 4.51; 95% CI, 2.8−7.3)" |
| Case, 2018, 43 (Australia) | • Retrospective observational study • Barriers for bystander-CPR • Emergency calls for adults with OHCA in regions with low rates of bystander CPR • 2013–2014 • N = 139 |
Barriers to CPR: • Procedural barriers (time lost due to language barriers and communication issues; telephone problems), • CPR knowledge (skill deficits; perceived benefit) • Personal factors (physical frailty or disability; patient position; emotional factors). |
Study identified a wide range of barriers to the provision of bystander CPR, primarily because of knowledge and skill deficits in the caller. The Authors suggested that this and other procedural barriers associated with the emergency call can be addressed with public education |
| McCormack, 1989, 283 (United States) | • Questionnaire survey • Disagreeable physical characteristics • ALL EMS or bystander-treated non-traumatic OHCAs • 1986 • N = 121 |
Barriers to CPR: • Disagreeable physical characteristics (vomit, alcohol on patient's breath, visible blood) |
Disagreeable physical characteristics present in 71 (59%) of 121 patients with out-of-hospital cardiac arrest. Forty (33%) patients vomited; 39 (33%) wore dentures; five (4%) had alcohol on their breath; and nine (7%) had visible blood. |
| Blewer, 2018, e004710 (United States, Canada) | • Retrospective observational study • Sex • Adult, non-traumatic OHCA • 2011−2015 • N = 19331 |
Barriers to CPR: • Female sex |
Among public OHCAs, males had significantly increased odds of receiving BCPR compared to females (OR: 1.27, 95% CI: 1.05–1.53, p = 0.01); this was not the case in the private setting (OR: 0.93, 95% CI: 0.87–1.01, p = ns). |
| Matsuyama, 2019, 577 (Japan) | • Prospective observational study • Sex • Adult (> = 18yrs) OHCA of medical origin, in public or residential locations, witnessed, • 2013–2015 • N = 84734 |
Barriers to CPR: • Female sex |
In public locations, women aged 18–64 years were less likely to receive BCPR (AOR, 0.86; 95% CI, 0.74−0.99), and when witnessed by a non-family member, women were less likely to receive BCPR regardless of age group. |
| Tanigawa, 2011, 523 (Japan) | • Prospective observational study • CPR training • Adult (> = 18yrs) OHCA of medical origin • 2008 • N = 120 |
Promote CPR: • Previous CPR training Barriers to CPR: • Female sex |
People who had experienced CPR training had a greater tendency to perform bystander CPR than people without experience of CPR training (AOR, 3.4; 95% CI 1.31–8.85). |
| Matsui, 2019, e195111 (Japan) | • Prospective observational study • Sex • Pediatric OHCAs occurring under school supervision • 2008–2015 • N = 232 |
Barriers to CPR: • Female sex |
Among students who experienced OHCA in schools in Japan, female sex was associated with lower odds of receiving public-access AED pad application compared with male sex. |
| Chiang, 2014, 53 (Taiwan) | • Retrospective observational study • Socio-economic status • OHCA cases activating EMS • 2008–2009 • N = 3573 |
Barriers to CPR: • Low Socio-economic status |
Odds ratio of receiving bystander-initiated CPR in low-SES areas was 0.72(95 CI:[0.60–0.88]) after adjusting for potential confounders |
| Moncur, 2015, 105 (United Kingdom) | • Retrospective observational study • Socio-economic status • OHCA with an attempt at resuscitation • 2011–2011 • N = 3179 |
Barriers to CPR: • Low Socio-economic status |
Increase in bystander CPR rates from 14.5% in Q1 (most deprived) to 23.2% in Q5 (least deprived) (p < 0.001) (OR = 1.78, 95% CI 1.32–2.39, p = 0.001) |
| Dahan, 2017, 107 (France) | • Prospective observational study • Socio-economic status • OHCA occurring in streets, public areas, private facilities, and private dwellings • 2000–2010 • N = 777 |
Barriers to CPR: • Low Socio-economic status |
Bystander CPR provision was significantly less frequent in low than in higher SES neighborhoods (OR 0.85; 95% confidence interval [CI] 0.72–0.99) |
| Vaillancourt, 2008, 417 (Canada) | • Prospective observational study • Socio-economic status • OHCA of cardiac origin • 1995–1999 • N = 3600 |
Barriers to CPR: • Low Socio-economic status |
For each $100,000 increment in property value, the likelihood of receiving bystander CPR increased (OR = 1.07; 95% CI 1.01–1.14; p = 0.03) |
| Sasson, 2012, 1607 (United States) | • Retrospective observational study • Socio-economic status • Bystander-initiated CPR • 2005–2009 • N = 4068 |
Barriers to CPR: • Race • Low socio-economic status (Low income) |
Direct relationship between the median income and racial composition of a neighborhood and the probability that a person with OHCA received bystander-initiated CPR. This association was most apparent in low-income black neighborhoods, where the odds of receiving bystander-initiated CPR were approximately 50% lower than in high-income non-black neighborhoods. Even in high-income black neighborhoods, patients with OHCA were approximately 23% less likely to receive bystander-initiated CPR than were patients in high-income nonblack neighborhoods. |
| Chang, 2016, 26 (Korea) | • Retrospective observational study • Family members • Paediatric OHCAs (<19 years old) • 2012–2014 • N = 1477 |
Promote CPR: • Family members Barriers to CPR: • Low community education level |
In paediatric OHCA cases, family members were more likely than strangers to perform BCPR except in communities with the lowest educational level (AOR, 1.75; 95% CI, 1.31–2.34). |
| Langlais, 2017, 163 (United States) | • Retrospective observational study • Patients’ positioning • 911 audio recordings of OHCA • 2011–2013 • N = 802 |
Promote CPR: • Multiple bystanders Barriers to CPR: • Difficulties to move the patient to the ground and into a supine position |
Telecommunicator-directed bystander chest compressions were more than twice as likely to start in the non-barrier group (OR: 2.2, 95% CI: 1.6–3.2; p < 0.001). Rescuers were 3.7 times more likely to overcome a barrier and start compressions (OR: 3.7, 95% CI: 2.0–6.8; p < 0.001) when multiple bystanders were present. Roughly 26% had a barrier. A barrier reduced likelihood of TCPR and delayed time-to-first compression. Approx. 50% of all callers facing a barrier. |
| Axelsson, 1996, 3 (Sweden) | • Questionnaire survey • Bystander experiences • Bystanders who initiated CPR • 1990−1994 • N = 742 |
Barriers to CPR: • Mouth-to-mouth ventilation • Vomiting • Disagreeable characteristics • Uncertainty as to whether it was a cardiac arrest • Fear of causing injury or doing something wrong • Had no ventilation mask • Person’s age • Rescuer perception of futile situation |
Rescuers rarely hesitated about initiating CPR. Technical problems were common but do not appear to have had a great impact on the bystanders in this population prone to selection bias. Over 90% regarded their intervention as mainly positive. Almost everybody was prepared to start CPR again. |
| Nishiyama, 2019, 63 (Japan) | • Questionnaire survey • CPR training • 2nd through 4th-year university students who attended CPR and AED use training when they entered the University • 2018 • N = 5549 |
Promote CPR: • Hands-on mass training Barriers to CPR: • Another person had already done • Panic • Difficulty in judging cardiac arrest or finding AED • Lack of confidence • Fear • Burden of responsibility • Sex difference with patient |
The incidence rate of encountering OHCA patients was 1.1 per 100 person-years and half of those who encountered a collapsed person performed at least one resuscitation action in the emergency setting. Hands-on mass training would encourage university students to perform any resuscitation actions on the emergency scene. |
| Iwami, 2015, 415 (Japan) | • Prospective observational study • Chest compression only CPR • All EMS-treated OHCAs • 2005–2012 • N = 816385 |
Promote CPR: • CCCPR |
Wider dissemination of CCCPR was associated with the increase in bystander-initiated CPR and the incidence of OHCA survival with favorable neurological outcome at the population level. |
| Ro, 2016, 17 (Korea) | • Cross-sectional study • Public awareness • ALL EMS-treated OHCAs with presumed cardiac etiology, • 2012–2013 • N = 29052 |
Promote CPR: • CPR-Awareness, • CPR-Any-Training • CPR-Recent-Training • CPR-Manikin Training • CPR-Self-Efficacy |
Higher CPR capacity at community level was associated with higher bystander CPR and survival to discharge rates after OHCA. AORs for BCPR were 1.06 (1.03–1.10) per 10% increment in CPR-Awareness, 1.10 (1.04–1.15) for CPR-Any-Training, and 1.08 (1.03–1.13) for CPR-Self-Efficacy |
Factors that reduce bystanders’ willingness to respond to a cardiac arrest
Personal factors (emotional barriers, and physical and background factors)
We found 14 articles addressing personal factors that reduce bystanders’ willingness to perform CPR.23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36 In a study of actual bystanders interviewed after an emergency call and the emergency medical service (EMS) dispatcher instruction of performance of CPR, the most frequently cited reason why non-responders were unable to perform CPR was “panic” (37.5%).24 According to one study, emotional factors such as panic and hysteria were reported in 20% of the emergency calls and were dominant barriers against dispatcher-assisted CPR among bystander-witnessed cardiac arrests.23 A study interviewing EMS personnel or bystanders who initiated or participated in CPR for OHCA patients demonstrated that disagreeable physical characteristics such as vomiting were observed in 59% of cases and had a negative impact on willingness of bystanders to perform CPR.25 Some studies from different geographical regions observed that female OHCA patients were less likely to receive bystander CPR26, 27, 28 or have an AED pad application26, especially in a public place26, 27 or when they were of reproductive age.29 Observational studies from different parts of the world consistently demonstrated that OHCA patients in low socioeconomic status areas were less likely to receive bystander CPR, although its association with survival outcomes showed inconsistency across studies.30, 31, 32, 33 The association between race and probability of bystander CPR was controversial. However, again it is more likely to be attributed to socioeconomic differences among neighborhood subgroups than to ethnical differences themselves,34 since it has been described even in local contexts where ethnicity but not economic composition is homogeneous.32 A study focusing on pediatric OHCA cases demonstrated that family members had higher likelihood of performing CPR than strangers except in communities with the lowest educational level.35
One study reviewing emergency calls observed that physical factors had an influence on their ability to provide CPR in 37.5% OHCA cases, although this was primarily related to their ability to place the patient flat on their back on the floor, rather than to administer CPR.23 Another study reviewing audio recordings of telephone CPR also found a barrier associated with patient positioning where inability to move patients to a hard, flat surface was associated with a decreased rate of CPR and delayed time to the initiation of chest compression.36
CPR knowledge (skill deficits, perceived benefit)
We identified 3 observational studies assessing lack of CPR knowledge as barriers to the administration of CPR.23, 24, 37 A study reviewing emergency calls demonstrated that lack of CPR knowledge or skills was recognized most frequently (81.3% of calls) as a barrier to the initiation of CPR, as many bystanders reported poor confidence and sense of incompetence due to lack of prior CPR exposure even under the dispatcher instructions.23 The study also observed that patient assessments and dispatcher-assisted CPR instructions were declined since bystanders perceived that the patient was already deceased in 28.1% of calls.23
Similarly, one study reviewing actual experiences of bystanders of OHCAs reported that hesitation came mostly from the fear of causing injury or doing something wrong or from the rescuer considering the intervention to be futile.37 In another study interviewing actual bystanders, lack of confidence (9.1%) was described as the reason why they were unable to perform CPR.24
Procedural issues
We identified 2 observational studies addressing procedural issues as factors that reduce bystanders’ willingness to perform CPR.23, 37 A qualitative review of emergency calls cited communication or language barriers, and late identification of arrest as procedural issues.23 A study reviewing actual experiences of bystanders also noted the causes for hesitation, such as uncertainty about whether the case was a cardiac arrest.37
Factors that increase bystanders’ willingness to perform CPR (excluding dispatcher instructions, community initiatives, and social media technologies)
We identified 5 studies investigating factors facilitating bystanders’ willingness to perform CPR.24, 28, 38, 39,40 A study in which actual bystanders were interviewed reported that CPR was more likely to be provided by CPR-trained bystanders with more than a high-school education and when CPR training had been received within five years.24 Another study interviewing actual OHCA bystanders reported that people who had prior experience of CPR training had a higher likelihood of performing bystander CPR than people without experience of CPR training.28 A cross sectional study interviewing 5549 university students in Japan who had attended hands-on mass training of CPR and AED use demonstrated that the incidence rate of encountering suspected OHCA patients was 1.1 per 100 person-years and half of those who encountered a collapsed person did at least one resuscitation action.38 Large nationwide observations in Japan reported a positive association between wider dissemination of chest compression-only CPR and an increase in bystander CPR and in survival with favorable neurological outcome. This suggests a potential benefit of simplified chest compression-only CPR training to increase bystanders’ willingness to perform CPR.39 Interestingly, in a study conducted in US, a very low proportion (1.1%) of actual bystanders were reluctant to perform mouth-to-mouth ventilation, which suggested that mouth-to-mouth ventilation was not a barrier for bystanders to perform CPR.24 A large cross-sectional study from Korea with an OHCA registry database reported that higher CPR capacity (e.g. CPR-Awareness, CPR-Any-Training, CPR-Recent-Training, CPR-Manikin-Training, and CPR-Self-Efficacy) at community level was associated with higher rate of bystander CPR and survival rate after OHCA.40
Discussion
Summary of evidence
This scoping review assessed the evidence of barriers and facilitators for bystanders to perform CPR. The 2010 ILCOR CoSTR performed a narrative review for this topic and showed the barriers and facilitators for bystanders (both lay rescuers and health care providers) to perform CPR.14 On the other hand, the 2015 ILCOR CoSTR focused on high-risk populations and recommended BLS training interventions for them, based on the willingness to be trained and the fact that there is low harm and high potential benefit (strong recommendation, low-quality evidence).15, 41 In this update, even though the EIT Task Force was reviewing the effectiveness of other specific interventions such as CPR training, community initiatives to improve delivery of CPR, social media technologies and dispatcher-assisted CPR to increase bystander CPR rate, it was considered important and helpful to develop strategies to foster bystander CPR to review positive and negative factors on bystanders’ actions in actual emergency settings. Therefore, the EIT Task Force decided to focus only on a lay rescuer (excluding a health care provider) and evidence from actual emergency situations and experiences (excluding simulation studies and survey data not from actual experience). Unfortunately, we identified no randomized controlled studies, but 18 observational studies addressing this topic.
Although there was significant heterogeneity among study populations and methodologies, definitions of factors and outcomes, we were able to reveal both, factors that are associated with improving as well as hindering the willingness to provide CPR. All these studies were based-on actual emergency settings observed, and we confirm the usability to divided these factors into “personal factors”, “CPR knowledge based factors”, and “factors related to procedural issues”. A better understanding of these factors would be the key and helpful to overcome the current low proportion of bystander actions including CPR and an AED use across the world and improve outcomes after OHCA.42 In addition, the difficulties in early recognition of cardiac arrest both by bystanders and dispatchers described in the prior CoSTRs remain to be a major issue to overcome.43, 44
Knowledge gaps
Although we did not identify sufficient evidence to prompt a systematic review, this scoping review highlights significant knowledge gaps associated with the willingness to perform CPR by lay rescuers, as follows: There is a need to assess the efficacy of interventions aiming to address known barriers and enhance facilitating factors for actual bystanders to provide CPR, to use of AEDs, and to call for help for OHCA victims. The best methods to teach how to overcome known barriers to perform CPR in CPR training course needs to be assessed. The better understanding of those factors that enhance the willingness of bystanders to perform CPR and the barriers for those bystanders who were unwilling to perform CPR need to trigger the translation of measures to foster higher rate of bystander CPR.
Limitations
Several inherent limitations should be noted. First, as a scoping review, a systematic synthesis of research findings was not performed. In this scoping review, instead of increasing the number of search databases, we preferred to add considerable hand searches in addition to selected database searches, because studies for this research question were so heterogeneous that establishing the search strategy was difficult. Second, in this scoping review we did not address the quality of evidence identified or potential biases systematically like in a systematic review. We observed the significant heterogeneity among study populations, study methodologies, definitions of factors associated with willingness to provide CPR, outcome measures utilized and outcomes reported. Therefore, factors identified by this study may not be applicable to all areas across the world equally. Third, as mentioned in the knowledge gaps section, the interventional methods to address known barriers and enhance facilitators and its efficacy in the actual setting remains uncertain.
Conclusions
Our findings indicate that a number of factors are present in actual OHCA settings which either inhibit or facilitate lay rescuers’ performance of CPR. CPR training, regional and national education programs, and dispatch instructions should take these factors into consideration, to improve CPR performance of lay rescuers in the actual settings.
Funding sources
None.
Conflict of interest
This scoping review was part of the ILCOR continuous evidence evaluation process which is guided by a rigorous conflict of interest policy (see www.ilcor.org). Taku Iwami is Japanese Resuscitation Council director of training and education, and ILCOR EIT task force member. Robert Greif is ERC director of training and education, and ILCOR EIT Task Force chairperson. None of the other authors declared a conflict of interest.
Ethics approval and consent to participate
Not applicable.
Availability of data and materials
Not applicable.
Acknowledgements
The following non-task force members are acknowledged for their contributions: Information specialist Lorena Romero at the Alfred Hospital, Melbourne, Australia. The following ILCOR EIT Taskforce Members are acknowledged as collaborators on this scoping review: Farhan Bhanji, Blair L. Bigham, Janet Bray, Jan Breckwoldt, Adam Cheng, Koenraad G. Monsieurs, Jonathan P. Duff, Kasper Glerup Lauridsen, Andrew S. Lockey, Elaine Gilfoyle, Ming-Ju Hsieh, Matthew Huei-Ming Ma, Deems Okamoto, Jeffrey L. Pellegrino, Joyce Yeung, and Judith Finn and Peter Morley as members of the ILCOR Scientific Advisory Committee (SAC).
References
- 1.Kronick S.L., Kurz M.C., Lin S. Part 4: systems of care and continuous quality improvement: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(November (18 Suppl 2)) doi: 10.1161/cir.0000000000000258. S397–413. [DOI] [PubMed] [Google Scholar]
- 2.Monsieurs K.G., Nolan J.P., Bossaert L.L. European Resuscitation Council Guidelines for Resuscitation 2015: section 1. Executive summary. Resuscitation. 2015;95(October):1–80. doi: 10.1016/j.resuscitation.2015.07.038. [DOI] [PubMed] [Google Scholar]
- 3.Iwami T., Nichol G., Hiraide A. Continuous improvements in “chain of survival” increased survival after out-of-hospital cardiac arrests: a large-scale population-based study. Circulation. 2009;119(February (5)):728–734. doi: 10.1161/circulationaha.108.802058. [DOI] [PubMed] [Google Scholar]
- 4.Deakin C.D. The chain of survival: not all links are equal. Resuscitation. 2018;126(May):80–82. doi: 10.1016/j.resuscitation.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Malta Hansen C., Kragholm K., Pearson D.A. Association of bystander and first-responder intervention with survival after out-of-hospital cardiac arrest in North Carolina, 2010-2013. JAMA. 2015;314(July (3)):255–264. doi: 10.1001/jama.2015.7938. [DOI] [PubMed] [Google Scholar]
- 6.Nakahara S., Tomio J., Ichikawa M. Association of bystander interventions with neurologically intact survival among patients with bystander-witnessed out-of-hospital cardiac arrest in Japan. JAMA. 2015;314(July (3)):247–254. doi: 10.1001/jama.2015.8068. [DOI] [PubMed] [Google Scholar]
- 7.Kitamura T., Kiyohara K., Sakai T. Public-access defibrillation and out-of-hospital cardiac arrest in Japan. N Engl J Med. 2016;375(October (17)):1649–1659. doi: 10.1056/NEJMsa1600011. [DOI] [PubMed] [Google Scholar]
- 8.Sayre M.R., Berg R.A., Cave D.M., Page R.L., Potts J., White R.D. Hands-only (compression-only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out-of-hospital sudden cardiac arrest: a science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation. 2008;117(April (16)):2162–2167. doi: 10.1161/circulationaha.107.189380. [DOI] [PubMed] [Google Scholar]
- 9.Mozaffarian D., Benjamin E.J., Go A.S. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(January (4)) doi: 10.1161/cir.0000000000000152. e29–322. [DOI] [PubMed] [Google Scholar]
- 10.Agerskov M., Nielsen A.M., Hansen C.M. Public access defibrillation: great benefit and potential but infrequently used. Resuscitation. 2015;96(November):53–58. doi: 10.1016/j.resuscitation.2015.07.021. [DOI] [PubMed] [Google Scholar]
- 11.Weisfeldt M.L., Sitlani C.M., Ornato J.P. Survival after application of automatic external defibrillators before arrival of the emergency medical system: evaluation in the resuscitation outcomes consortium population of 21 million. J Am Coll Cardiol. 2010;55(April (16)):1713–1720. doi: 10.1016/j.jacc.2009.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Girotra S., van Diepen S., Nallamothu B.K. Regional variation in out-of-hospital cardiac arrest survival in the United States. Circulation. 2016;133(May (22)):2159–2168. doi: 10.1161/circulationaha.115.018175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dyson K., Brown S.P., May S. International variation in survival after out-of-hospital cardiac arrest: a validation study of the Utstein template. Resuscitation. 2019;138(May):168–181. doi: 10.1016/j.resuscitation.2019.03.018. [DOI] [PubMed] [Google Scholar]
- 14.Mancini M.E., Soar J., Bhanji F. Part 12: education, implementation, and teams: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation. 2010;122(October (16 Suppl 2)) doi: 10.1161/circulationaha.110.971143. S539–581. [DOI] [PubMed] [Google Scholar]
- 15.Bhanji F., Finn J.C., Lockey A. Part 8: education, implementation, and teams: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation. 2015;132(October (16 Suppl 1)) doi: 10.1161/cir.0000000000000277. S242–268. [DOI] [PubMed] [Google Scholar]
- 16.Munn Z., Peters M.D.J., Stern C., Tufanaru C., McArthur A., Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. 2018/11/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.International Liaison Committee on Resuscitation. ILCOR - Continuous Evidence Evaluation - Task Force Scoping Reviews Guidance Document v 1.0 SAC approved 2019:1–7. https://www.ilcor.org/documents/continuous-evidence-evaluation-guidance-and-templates. [Accessed 15 November 2019].
- 18.Arksey H., O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 19.Tricco A.C., Lillie E., Zarin W. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(October (7)):467–473. doi: 10.7326/m18-0850. [DOI] [PubMed] [Google Scholar]
- 20.Riggs M., Franklin R., Saylany L. Associations between cardiopulmonary resuscitation (CPR) knowledge, self-efficacy, training history and willingness to perform CPR and CPR psychomotor skills: a systematic review. Resuscitation. 2019;138(May):259–272. doi: 10.1016/j.resuscitation.2019.03.019. [DOI] [PubMed] [Google Scholar]
- 21.Smith C.M., Lim Choi Keung S.N., Khan M.O. Barriers and facilitators to public access defibrillation in out-of-hospital cardiac arrest: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2017;3(October (4)):264–273. doi: 10.1093/ehjqcco/qcx023. [DOI] [PubMed] [Google Scholar]
- 22.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. 2016/12/05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Case R., Cartledge S., Siedenburg J. Identifying barriers to the provision of bystander cardiopulmonary resuscitation (CPR) in high-risk regions: a qualitative review of emergency calls. Resuscitation. 2018;129(August):43–47. doi: 10.1016/j.resuscitation.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 24.Swor R., Khan I., Domeier R., Honeycutt L., Chu K., Compton S. CPR training and CPR performance: do CPR-trained bystanders perform CPR? Acad Emerg Med. 2006;13(June (6)):596–601. doi: 10.1197/j.aem.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 25.McCormack A.P., Damon S.K., Eisenberg M.S. Disagreeable physical characteristics affecting bystander CPR. Ann Emerg Med. 1989;18(March (3)):283–285. doi: 10.1016/s0196-0644(89)80415-9. [DOI] [PubMed] [Google Scholar]
- 26.Blewer A.L., McGovern S.K., Schmicker R.H. Gender disparities among adult recipients of bystander cardiopulmonary resuscitation in the public. Circ Cardiovasc Qual Outcomes. 2018;11(August (8)) doi: 10.1161/circoutcomes.118.004710. e004710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matsuyama T., Okubo M., Kiyohara K. Sex-based disparities in receiving bystander cardiopulmonary resuscitation by location of cardiac arrest in Japan. Mayo Clin Proc. 2019;94(April (4)):577–587. doi: 10.1016/j.mayocp.2018.12.028. [DOI] [PubMed] [Google Scholar]
- 28.Tanigawa K., Iwami T., Nishiyama C., Nonogi H., Kawamura T. Are trained individuals more likely to perform bystander CPR? An observational study. Resuscitation. 2011;82(May (5)):523–528. doi: 10.1016/j.resuscitation.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 29.Matsui S., Kitamura T., Kiyohara K. Sex disparities in receipt of bystander interventions for students who experienced cardiac arrest in Japan. JAMA Netw Open. 2019;2(May (5)) doi: 10.1001/jamanetworkopen.2019.5111. e195111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chiang W.C., Ko P.C., Chang A.M. Bystander-initiated CPR in an Asian metropolitan: does the socioeconomic status matter? Resuscitation. 2014;85(January (1)):53–58. doi: 10.1016/j.resuscitation.2013.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dahan B., Jabre P., Karam N. Impact of neighbourhood socio-economic status on bystander cardiopulmonary resuscitation in Paris. Resuscitation. 2017;110(January):107–113. doi: 10.1016/j.resuscitation.2016.10.028. [DOI] [PubMed] [Google Scholar]
- 32.Moncur L., Ainsborough N., Ghose R., Kendal S.P., Salvatori M., Wright J. Does the level of socioeconomic deprivation at the location of cardiac arrest in an English region influence the likelihood of receiving bystander-initiated cardiopulmonary resuscitation? Emerg Med J. 2016;33(February (2)):105–108. doi: 10.1136/emermed-2015-204643. [DOI] [PubMed] [Google Scholar]
- 33.Vaillancourt C., Lui A., De Maio V.J., Wells G.A., Stiell I.G. Socioeconomic status influences bystander CPR and survival rates for out-of-hospital cardiac arrest victims. Resuscitation. 2008;79(December (3)):417–423. doi: 10.1016/j.resuscitation.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 34.Sasson C., Magid D.J., Chan P. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367(October (17)):1607–1615. doi: 10.1056/NEJMoa1110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chang I., Kwak Y.H., Shin S.D., Ro Y.S., Kim D.K. Characteristics of bystander cardiopulmonary resuscitation for paediatric out-of-hospital cardiac arrests: a national observational study from 2012 to 2014. Resuscitation. 2017;111(February):26–33. doi: 10.1016/j.resuscitation.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 36.Langlais B.T., Panczyk M., Sutter J. Barriers to patient positioning for telephone cardiopulmonary resuscitation in out-of-hospital cardiac arrest. Resuscitation. 2017;115(June):163–168. doi: 10.1016/j.resuscitation.2017.03.034. [DOI] [PubMed] [Google Scholar]
- 37.Axelsson A., Herlitz J., Ekstrom L., Holmberg S. Bystander-initiated cardiopulmonary resuscitation out-of-hospital. A first description of the bystanders and their experiences. Resuscitation. 1996;33(November (1)):3–11. doi: 10.1016/s0300-9572(96)00993-8. [DOI] [PubMed] [Google Scholar]
- 38.Nishiyama C., Sato R., Baba M. Actual resuscitation actions after the training of chest compression-only CPR and AED use among new university students. Resuscitation. 2019;141(August):63–68. doi: 10.1016/j.resuscitation.2019.05.040. [DOI] [PubMed] [Google Scholar]
- 39.Iwami T., Kitamura T., Kiyohara K., Kawamura T. Dissemination of chest compression-only cardiopulmonary resuscitation and survival after out-of-hospital cardiac arrest. Circulation. 2015;132(August (5)):415–422. doi: 10.1161/circulationaha.114.014905. [DOI] [PubMed] [Google Scholar]
- 40.Ro Y.S., Shin S.D., Song K.J. Public awareness and self-efficacy of cardiopulmonary resuscitation in communities and outcomes of out-of-hospital cardiac arrest: a multi-level analysis. Resuscitation. 2016;102(May):17–24. doi: 10.1016/j.resuscitation.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 41.Finn J.C., Bhanji F., Lockey A. Part 8: education, implementation, and teams: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. 2015;95(October) doi: 10.1016/j.resuscitation.2015.07.046. e203–224. [DOI] [PubMed] [Google Scholar]
- 42.Kiguchi T., Okubo M., Nishiyama C. Out-of-hospital cardiac arrest across the World: first report from the International Liaison Committee on Resuscitation (ILCOR) Resuscitation. 2020;152(July):39–49. doi: 10.1016/j.resuscitation.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 43.Sayre M.R., Koster R.W., Botha M. Part 5: adult basic life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2010;122(October (16 Suppl 2)) doi: 10.1161/circulationaha.110.970996. S298–324. [DOI] [PubMed] [Google Scholar]
- 44.Perkins G.D., Travers A.H., Berg R.A. Part 3: adult basic life support and automated external defibrillation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. 2015;95(October) doi: 10.1016/j.resuscitation.2015.07.041. e43–69. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.