Abstract
Background and Objectives:
Laparoscopic cholecystectomy with common bile duct exploration (LC with LCBDE) remains the preferred technique for difficult common bile duct stone (CBDS) removal. The chopstick method uses commonly available instruments and may be cost-saving compared to other techniques. We studied the outcome of LCBDE using the chopstick technique to determine if it could be considered a first-choice method.
Methods:
Data from all patients that underwent LCBDE from January 1, 2012 to April 30, 2019 were retrospectively analyzed. A standard 4-port incision and CBDS permitted extraction with two laparoscopic instruments by chopstick technique via vertical choledochotomy. Demographic data, stone clearance rate, surgical outcomes, complications, and other associated factors were evaluated.
Results:
Thirty-two patients underwent LCBDE. The mean number of preoperative endoscopic retrograde cholangiopancreatography (ERCP) sessions was 2.4. In 65.5% of cases, the CBDS was completely removed by the chopstick technique, while 96.9% of stones were removed after using additional tools. The need for additional instruments was associated with increased age, increased numbers of stones, longer period from the latest ERCP session, and previous upper abdominal surgery. The conversion rate to open surgery was 28.1% and was significantly associated with a history of upper abdominal surgery.
Conclusion:
The chopstick technique is a good alternative and could be considered as a first-line technique in LCBDE to remove the CBDS in cases with 1 to 2 large suprapancreatic CBDS due to instrument availability, cost-effectiveness, and comparable surgical outcomes.
Keywords: Choledocholithiasis, Common bile duct stone, Laparoscopic common bile duct exploration, Chopstick technique
INTRODUCTION
Up to 19% of patients with gallstone (GS) may have concomitant choledocholithiasis (common bile duct stone [CBDS]) that may be asymptomatic or complicated by obstructive jaundice, cholangitis, and pancreatitis, which are associated with increased morbidity and mortality. Therefore, CBDS should be treated even if the patient is asymptomatic.1–3
Treatment options of CBDS include: endoscopic retrograde cholangiopancreatography (ERCP) with stone extraction followed by laparoscopic cholecystectomy (LC); LC with intraoperative ERCP (Rendez-Vous technique); same-day approach of ERCP followed by LC, or LC followed by postoperative ERCP; one-step laparoscopic cholecystectomy with common bile duct exploration (LC with LCBDE); and one-step open surgery.1,2,4 Previous studies reported that one-step LC with LCBDE was not inferior to preoperative ERCP followed by LC.2,5,6 Moreover, a recent meta-analysis showed higher CBDS clearance rate in LCBDE compared with ERCP followed by LC (94.1% vs. 90.1%; P = .012), retained stones rate (1.2% vs. 7.9%; P = .004), and stone recurrence rate (1.8% vs. 5.6%; P = .005).7
LCBDE is becoming less common because international guidelines recommend ERCP with stone extraction followed by LC. Moreover, advanced techniques for stone removal in ERCP such as mechanical lithotripsy, cholangioscopy-assisted lithotripsy, electrohydraulic lithotripsy (EHL), extracorporeal shock wave lithotripsy (ESWL), and laser lithotripsy are increasingly common. However, surgical treatment remains the treatment of choice in difficult CBDS, especially in patients with large impacted CBDS or altered upper gastrointestinal tract anatomy.5,8,9
The chopstick technique was first reported in the ophthalmology field for nucleus removal during phacoemulsification in posterior capsule tear and impending dropped nucleus.10 With the advent of minimally-invasive surgery, several techniques in LCBDE procedure were developed. Special instruments may be required for some techniques, such as the Dormia basket, Fogarty catheter, and laser lithotripsy. We initially performed the LCBDE using the chopstick technique that requires only two basic laparoscopic instruments, such as the blunt-tipped graspers and bowel clamps. This technique may be particularly advantageous in rural hospitals where few instruments are available and budgets are restricted. Therefore, we studied the surgical outcomes of the chopstick technique.
MATERIALS AND METHODS
This study was reviewed and approved by the Institutional Review Board. We searched a database for all patients that underwent LCBDE in our center between January 1, 2012 to April 30, 2019. We excluded patients with active cholangitis grade B and C, primary CBDS, and patients with choledochal cyst or bile duct malignancy. The primary outcome was the stone clearance rate by chopstick technique. Patient demographic data, preoperative data, operative technique, and operative results including stone clearance rate, the conversion rate, the operative time, blood loss, length of hospital stay, complication and other associated factors were collected. Data analysis was performed using SPSS version 21.0.
OPERATIVE TECHNIQUES
Ports were placed in the reverse Trendelenburg right-side up position (Figure 1). The peritoneum covering Calot’s triangle was opened in infundibular approach. To characterize the CBDS size and location, we controlled the cystic artery then routinely performed the transcystic intraoperative cholangiography (IOC). In the CBD exploration phase, the peritoneum and fat covering anterior side of CBD was partially excised, aspirated by the 25G needle to confirm bile, and vertical choledochotomy was performed anteriorly with the incision size calibrated to the largest stone diameter. To extract CBDS, we first attempted the chopstick technique using two atraumatic blunt-tipped instruments, such as the bowel clamp or grasper, to press and milk the CBD stone in both distal and proximal sides according to the IOC. The left-handed instrument, via the port just lateral to midclavicular line, was placed on the posterolateral side that the blunt-tipped instrument was gently applied just across the CBDS, avoiding portal vein injury. The other (right-handed), via epigastric port, was placed on the anteromedial side of CBD to form a chopstick to extract CBDS via the choledochotomy (Figure 2).
Figure 1.
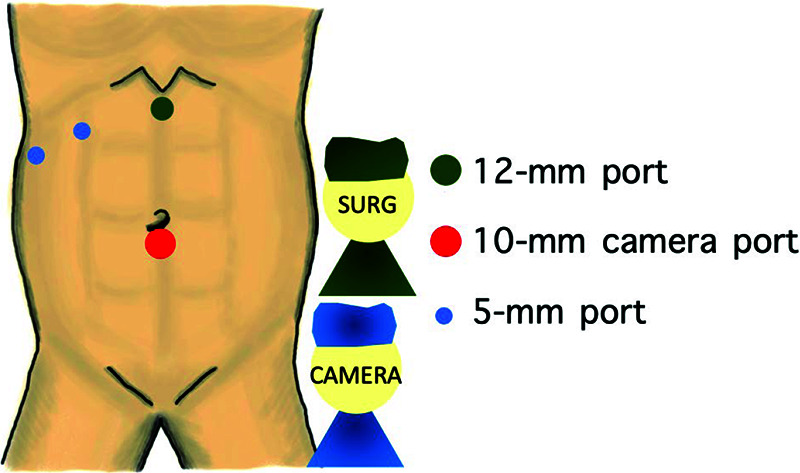
Positioning and port placement.
Figure 2.
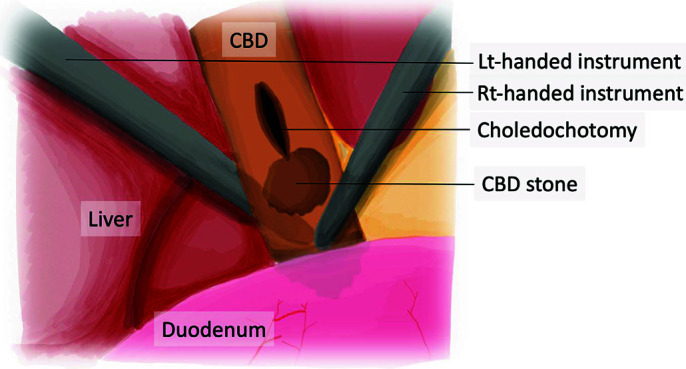
Instrument position for chopstick technique.
If a retained stone was detected, other instruments for stone extraction (e.g., Dormia basket, Fogarty catheter) were requested and extraction was reattempted. After stone removal, the completeness of CBDS clearance was confirmed by intraoperative choledochoscopy with irrigation in all cases. After CBDS complete clearance, the choledochotomy was closed with interrupted intracorporeal absorbable sutures via the previous 12-mm port. We generally required no T–Tube placement, except in cases with incomplete ductal clearance or unhealthy tissue. A closed-system drainage was then placed at the subhepatic area.
RESULTS
A total of 32 cases were included consisting of 15 males (46.9%) and 17 females (53.1%) with the mean age of 62.5 +/− 14.6 years. The average body mass index (BMI) was 24.3 +/− 4.0 kg/m.2 Ten (31.3%) patients had diabetes, 17 (53.1%) had hypertension, 13 (40.6%) had dyslipidemia, 1 (3.1%) had chronic kidney disease, 5 (15.6%) had underlying cardiac problems such as coronary artery disease or arrhythmia, and 2 (6.3%) had liver cirrhosis. Five (15.6%) were American Society of Anesthesiologists (ASA) class I, 22 (68.8%) were ASA class II, and 5 (15.6%) were ASA class III. Previous cholangitis treated by antimicrobials with or without ERCP was found in 17 cases (53.1%), previous upper abdominal surgery, such as gastrectomy, gastrojejunostomy, cholecystectomy, in 5 cases (15.6%), and previous lower abdominal surgery, such as appendectomy or Caesarean delivery, in 4 cases (12.5%). The average number of preoperative ERCP sessions were 2.41 +/− 1.2 times, ranging from 1 – 6 sessions, which 53.1% of cases had undergone 2 sessions of ERCP. In average, LCBDE was performed after the latest ERCP around 77.34 ±/− 58.61 days. The most common indication for LCBDE was a large impacted stone unable to be removed by ERCP (22 cases, 68.8%). The other indications included Mirizzi’s syndrome 4 cases (12.5%), altered anatomy 3 cases (9.4%), distal CBD stricture 2 cases (6.3%), and recurrent stone 1 case (3.1%).
To identify the CBDS characteristics, ERCPs were used as the latest preoperative imaging in 21 cases (65.62%), computed topography (CT) of upper abdomen in eight cases (25.0%), and magnetic resonance cholangiopancreatography (MRCP) in three cases (9.38%). The preoperative imaging showed that the mean of maximal CBDS diameter was 16.25 +/− 7.6 mm, the average number of CBDS was 1.66 +/− 1.3, and the mean CBD diameter was 15.22 +/− 4.2 mm.
All patients were managed with the previously described LCBDE step. The average operative time was 195.1 +/− 50.0 minutes and estimated blood loss was 110.03 mL +/– 114.9 mL. Complete CBDS clearance was demonstrated by choledochoscopy in all cases where the chopstick technique with normal saline solution flushing via choledochoscopy could achieve complete CBDS removal in 21 cases (65.5%). In the remaining cases, other stone extraction devices were used that the overall CBDS clearance rate observed by complete choledochoscopy was 96.88%. The conversion to open surgery was found in nine cases (28.13%). The causes of conversion were tight intraabdominal adhesion in five cases (15.6%), CBDS removal failure in two cases (6.3%), and uncontrolled bleeding from liver base in two cases (6.3%). One patient (3.1%) with failed CBDS removal, T tube was placed then was managed by interventional radiologists and endoscopists. In ductal closure, the CBD was primarily sutured in 29 cases (90.6%) and T tube placement in three cases (9.4%).
The average length of hospital stay was 7.7 +/− 4.5 days. There was no major complication or 30-day mortality. Minor complications consisted of superficial surgical site infection in four cases (12.5%), bile leakage in four cases (12.5%). Two cases (6.3%) needed an additional course of antimicrobials while two cases (6.3%) needed further percutaneous drainage. Liver failure occurred in one case (3.1%), atelectasis in one case (3.1%), ileus in one case (3.1%), and electrolyte imbalance in one case (3.1%). No surgical intervention was requested to correct these complications.
Increased age, increased stone number, longer period of the latest ERCP session, and history of previous upper abdominal surgery were significantly associated with the need for additional extraction instruments (p-value 0.028, 0.024, 0.032, and 0.037 respectively), while BMI, maximal stone and CBD size, the number of ERCP sessions, history of cholangitis, and previous lower abdominal surgery were not associated. Focusing on the operations that needed additional tools, the mean patients’ age was 68.5 years, average stone number was 3.07, and the duration of latest ERCP was 100.67 days.
Previous upper abdominal surgery was significantly associated with the conversion to open surgery (Relative risk (RR) 4.32, p-value 0.015), while age, BMI, the number of stone, maximal stone and CBD size, the number of ERCP sessions, history of cholangitis, and previous lower abdominal surgery were not associated.
DISCUSSION
Several approaches may be used to manage choledocholithiasis. The two most common approaches are ERCP followed by LC, the current standard, and the single-step LCBDE. In meta-analysis from 1,757 patients, Pan L., et al. reported that the CBDS clearance rate in LCBDE was higher than ERCP then LC (94.1% vs. 90.1%; P = .012), but less in retained CBDS (1.2% vs. 7.9%; P = .004) and CBDS recurrence (1.8% vs. 5.6%; P = .005).7 LCBDE can avoid ERCP-related complications, such as pancreatitis, cholangitis, bleeding, or perforation; and permanent injury to Oddi’s sphincter that can cause papillary stenosis, and sine-materia cholangitis (refluxing cholangitis). Furthermore, single-step LCBDE decreased the number of hospital admissions, shortened the length of stay, and lowered hospital costs.6,11 Anyhow, preoperative ERCP may facilitate LCBDE in some ways. Firstly, endoscopic stent may decrease the stone size, soften stone, and reduce the cholangitis events.12 Secondly, stent and endoscopic sphincterotomy (EST) released CBD pressure resulting in decreased leakage rate.13 Thirdly, if EST size was sufficient, CBDS could be removed into duodenum by pushing technique in experienced surgeons. Thereby, the difficult CBDS treatment needs the multidisciplinary team, consisted of endoscopists, surgeons, and interventional radiologists.
If evidence supporting LCBDE in CBDS treatment becomes clearer, the single-step LCBDE may become the first line treatment. Therefore, learning how to perform the LCBDE by several techniques and intracorporeal suturing are essential. The learning curve of surgeons to perform LCBDE with primary closure, observed by reduction in operative time and complication rate, required more than 54 cases.14
The chopstick method for LCBDE is effective and could be considered a first-line technique in hospitals with experienced surgeons. It is relatively simple and reduces costs associated with more complex instruments. In our study, this technique resulted in complete stone removal in 65.5% of cases. Moreover, other CBDS extraction techniques are associated with specific complications. For example, Dormia basket can cause ductal mucosal injury during extraction and EHL can cause cholangitis.15,16 Although the limitation of chopstick technique was the CBDS in intrapancreatic, intraduodenal, and intrahepatic location, the possible perfect candidates for this technique were 1 – 2 large CBDS superior to pancreatic border without previous upper abdominal surgery. CBD diameter should be greater than 6 mm for transcholedochotomy removal.17 In intrapancreatic or intraduodenal CBDS, the additional surgical extraction techniques or other advanced endoscopic treatments may be beneficial. From our results, preparation of additional extraction instruments, or referral to a tertiary center with advanced skills in LCBDE, may be considered in patients with advanced age, multiple CBDS, longer period of preoperative ERCP, and history of previous upper abdominal surgery. The waiting period after ERCP seemed to be long in our institute because we believed that the decrease in inflammation degree over the time may simplify the operation; however, the results revealed that the longer waiting time was associated with failed chopstick technique.
To confirm CBDS removal, IOC or choledochoscopy were used. In a randomized trial, Vindal, et al. reported that choledochoscopy was better than IOC for CBD stone clearance confirmation after transcholedochal LCBDE because the non-passage of contrast into the duodenum could be a false-positive in IOC group due to Oddi’s sphincter transient spasm. Moreover, IOC consumed more operative time than cholangioscopy (170 vs. 140 minutes, P < .001).18,19 In our center, we prefer to use the choledochoscopy via the epigastrium port to confirm the complete CBDS clearance via the choledochotomy site. However, if instrument availability was an issue, particularly in a rural or secondary hospital, IOC can be used as the confirmation tool after laparoscopic CBDS removal with additional glucagon administration for sphincter relaxation.
The open conversion rate of LCBDE varies from 4.2 – 43.1%.20–22 Multivariable analysis indicated that the conversion to open surgery was associated with the maximal CBDS diameter (odds ratio, [OR] 2.23), edema of CBD (OR 12.5), and the number of stones (OR 3.438).21 Another report found that prior antibiotic use (OR 2.98), previous ERCP (OR 4.99), and abnormal biliary anatomy (OR 9.37) were predictors of failed LCBDE.20 In our study, the conversion to open surgery rate was 28.13% and was significantly associated with a history of previous upper abdominal surgery (RR 4.32) while age, BMI, stone size and number, history of cholangitis, or history of ERCP were not significant. The most common causes of conversion in our study were tight intraabdominal adhesion, Calot’s triangle distortion, and difficult CBD identification, possibly related from previous upper abdominal surgery. Patients with previous upper abdominal surgery may have increased risk for open conversion and needed to be informed preoperatively. However, they were not contraindicated for LCBDE and chopstick technique. Another cause of conversion was the large impacted CBDS making complete laparoscopic removal difficult. In these cases, open surgery with additional instruments, such as stone forceps or T tube placement were required. We mostly avoided T tube placement owing to no difference in recurrent CBDS or stricture, but increase in complications (e.g., dislodgement, infection, fluid and electrolyte imbalance, bile peritonitis, unhealed fistula, delayed ductal stricture, etc.).23,24 Therefore, we placed T tube only in selected cases, such as retained CBDS and massive adhesion around CBD or unhealthy tissue that may result in ischemia. Our 7.7-day-hospital stay seemed to be long as a result of open conversion rate and postoperative complications. However, all complications were minor, required for radiologic intervention in 6.3% of cases, and no surgical intervention.
Even with the arrival of endoscopic technologies such as mechanical lithotripsy, cholangioscopy-assisted lithotripsy, EHL, laser lithotripsy, and ESWL,9,25 surgeons must try to improve the effectiveness of CBD clearance in laparoscopic surgery that still fails in 10%–15% of cases.8,11 To improve the operative technique for LCBDE in the tertiary or referral center, there are many novel techniques for difficult CBDS management during surgery (e.g., intraoperative EHL or ESWL), which performed under the direct visualization to avoid the ductal mucosal injury, or laser lithotripsy that can be used without visual control.11
Our study has limitations. We used a retrospective approach with a small sample size that may limit the generalizability of our findings. To improve understanding of the value of this operative technique, a prospective large-scale randomized trial is needed.
CONCLUSION
LCBDE is the main technique for difficult CBDS where endoscopic treatment has failed and has the potential to become a first-line treatment in the future. The chopstick technique can be considered as first choice to remove CBDS due to instrument availability and cost-effectiveness with comparable surgical outcomes. The 1 – 2 large CBDS superior to pancreas without previous upper abdominal surgery were good candidates for the chopstick technique. Additional extraction instruments should be readied during the LCBDE in patients with increased age, multiple CBDS, longer period of preoperative ERCP, and previous upper abdominal surgery.
Footnotes
Funding/Financial Support: none.
Disclosure: none.
Conflicts of Interest: none.
Informed consent: Dr. Thawatchai Akaraviputh declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
Tharathorn Suwatthanarak, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand..
Thawatchai Akaraviputh, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand..
Chainarong Phalanusitthepha, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand..
Vitoon Chinswangwatanakul, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand..
Asada Methasate, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand..
Jirawat Swangsri, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand..
Atthaphorn Trakarnsanga, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand..
Thammawat Parakonthun, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand..
Voraboot Taweerutchana, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand..
Nicha Srisuworanan, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand (All authors)..
References:
- 1.Costi R, Gnocchi A, Di Mario F, Sarli L. Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World J Gastroenterol. 2014;20(37):13382–13401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh AN, Kilambi R. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with gallbladder stones with common bile duct stones: systematic review and meta-analysis of randomized trials with trial sequential analysis. Surg Endosc. 2018;32(9):3763–3776. [DOI] [PubMed] [Google Scholar]
- 3.Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M. Guidelines on the management of common bile duct stones (CBDS). Gut. 2008;57(7):1004–1021. [DOI] [PubMed] [Google Scholar]
- 4.Akaraviputh T, Rattanapan T, Lohsiriwat V, Methasate A, Aroonpruksakul S, Lohsiriwat D. A same day approach for choledocholithiasis using endoscopic stone removal followed by laparoscopic cholecystectomy: a retrospective study. J Med Assoc Thai. 2009;92(1):8–11. [PubMed] [Google Scholar]
- 5.Rogers SJ, Cello JP, Horn JK, et al. Prospective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone disease. Arch Surg. 2010;145(1):28–33. [DOI] [PubMed] [Google Scholar]
- 6.Boonmee C, Summart U, Arayajarernwong N, et al. Synchronous approach versus the sequential approach in laparoscopic cholecystectomy with endoscopic retrograde cholangiopancreatography in patients with gallstones and suspected common bile duct stones. JCDR. 2019;13:8–11. [Google Scholar]
- 7.Pan L, Chen M, Ji L, et al. The safety and efficacy of laparoscopic common bile duct exploration combined with cholecystectomy for the management of cholecysto-choledocholithiasis: an up-to-date meta-analysis. Ann Surg. 2018;268(2):247–253. [DOI] [PubMed] [Google Scholar]
- 8.Manes G, Paspatis G, Aabakken L, et al. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51(5):472–491. [DOI] [PubMed] [Google Scholar]
- 9.Veld JV, van Huijgevoort NCM, Boermeester MA, et al. A systematic review of advanced endoscopy-assisted lithotripsy for retained biliary tract stones: laser, electrohydraulic or extracorporeal shock wave. Endoscopy. 2018;50(09):896–909. [DOI] [PubMed] [Google Scholar]
- 10.Lal H, Sethi A, Bageja S, Popli J. Chopstick technique for nucleus removal in an impending dropped nucleus. J Cataract Refract Surg. 2004;30(9):1835–1839. [DOI] [PubMed] [Google Scholar]
- 11.Yang T, Ma Z, Xu B, et al. Clinical role of frequency-doubled double-pulse neodymium YAG laser lithotripsy for removal of difficult biliary stones in laparoscopic common bile duct exploration. ANZ J Surg. 2019;89(9):E358–E62. [DOI] [PubMed] [Google Scholar]
- 12.Horiuchi A, Nakayama Y, Kajiyama M, et al. Biliary stenting in the management of large or multiple common bile duct stones. Gastrointest Endosc. 2010;71(7):1200–1203 e2. [DOI] [PubMed] [Google Scholar]
- 13.Kim KH, Kim TN. Endoscopic management of bile leakage after cholecystectomy: a single-center experience for 12 years. Clin Endosc. 2014;47(3):248–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu H, Wu L, Yuan R, et al. Learning curve for performing choledochotomy bile duct exploration with primary closure after laparoscopic cholecystectomy. Surg Endosc. 2018;32(10):4263–4270. [DOI] [PubMed] [Google Scholar]
- 15.Varban O, Assimos D, Passman C, Westcott C. Laparoscopic common bile duct exploration and holmium laser lithotripsy: a novel approach to the management of common bile duct stones. Surg Endosc. 2010;24(7):1759–1764. [DOI] [PubMed] [Google Scholar]
- 16.Buxbaum J. Modern management of common bile duct stones. Gastrointest Endosc Clin N Am. 2013;23(2):251–275. [DOI] [PubMed] [Google Scholar]
- 17.Zerey M, Haggerty S, Richardson W, et al. Laparoscopic common bile duct exploration. Surg Endosc. 2018;32(6):2603–2612. [DOI] [PubMed] [Google Scholar]
- 18.Vindal A, Chander J, Lal P, Mahendra B. Comparison between intraoperative cholangiography and choledochoscopy for ductal clearance in laparoscopic CBD exploration: a prospective randomized study. Surg Endosc. 2015;29(5):1030–1038. [DOI] [PubMed] [Google Scholar]
- 19.Gupta N. Role of laparoscopic common bile duct exploration in the management of choledocholithiasis. World J Gastrointest Surg. 2016;8(5):376–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chue KM, Aw JWB, Chua SHM, et al. A predictive nomogram to identify factors influencing the success of a concomitant laparoscopic cholecystectomy with common bile duct exploration for choledocholithiasis. HPB (Oxford). 2018;20(4):313–320. [DOI] [PubMed] [Google Scholar]
- 21.Xu B, Wang YX, Qiu YX, et al. Risk factors and consequences of conversion to open surgery in laparoscopic common bile duct exploration. Surg Endosc. 2018;32(12):4990–4998. [DOI] [PubMed] [Google Scholar]
- 22.Tunruttanakul S. Laparoscopic Bile Duct Exploration in Treating Difficult Common Bile Duct Stones in Sawanpracharak Hospital, A Tertiary Center in the Lower Northern Region of Thailand. Siriraj Medical Journal. 2018;70:12–16. [Google Scholar]
- 23.Podda M, Polignano FM, Luhmann A, et al. Systematic review with meta-analysis of studies comparing primary duct closure and T-tube drainage after laparoscopic common bile duct exploration for choledocholithiasis. Surg Endosc. 2016;30(3):845–861. [DOI] [PubMed] [Google Scholar]
- 24.Liu D, Cao F, Liu J, et al. Risk factors for bile leakage after primary closure following laparoscopic common bile duct exploration: a retrospective cohort study. BMC Surg. 2017;17(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phalanusitthepha C, Augkurawaranon C, Sriprayoon T, Hokierti C, Akaraviputh T. Outcomes of Endoscopic Sphincteroplasty Using Large Balloon Dilatation for Difficult Common Bile Duct Stone Removal: A Single Endoscopist Experience. J Med Assoc Thai. 2014;97(7):699–704. [PubMed] [Google Scholar]


