Abstract
Background and Objectives:
The diagnosis of malignant pancreatic cystic lesions (PCLs) remains challenging. Needle-based confocal laser endomicroscopy (nCLE) is an emerging promising imaging technique capable of real-time in vivo microscopic imaging of the cyst wall. We aimed to develop and validate a new nCLE diagnostic criteria for malignant mucinous cystic lesions (MLs).
Methods:
Patients referred for EUS-FNA of indeterminate PCLs with at least one worrisome features according to Fukouka consensus were consecutively prospectively enrolled from July 2016 to July 2018. The final diagnosis was based on surgical histology, cytopathology, or committee consensus. Five investigators nonblindly reviewed nCLE features and identified potential diagnostic feature for malignant MLs, which was also reviewed in histology imaging accordingly. Furthermore, the nCLE diagnostic feature was evaluated with an independent nCLE dataset by two investigators in a double-blind manner.
Results:
A nCLE pattern of dark aggregates of neoplastic cells was identified as diagnostic for MLs, which was consistent with histological findings of irregular branching and budding in malignant MLs. An independent validation revealed that the accuracy, sensitivity, and specificity of this feature for the diagnosis of malignant MLs were 94%, 75%, and 100%, respectively.
Conclusion:
The new nCLE criterion is promising for diagnosis of malignant MLs which warrants further confirmation in large cohort.
Keywords: diagnosis, malignancy, needle-based confocal laser endomicroscopy, pancreatic cystic lesion
INTRODUCTION
Pancreatic cystic lesions (PCLs) are increasingly diagnosed, with a prevalence of 2.1%–2.6% in general population and 13.5%–45% in computed tomography scans (CTs)[1,2] and magnetic resonance imaging (MRI),[3,4] respectively. PCLs have malignancy potential,[5] and surgical resection is recommended for malignant PCLs, therefore closely surveillance is required for lesions with malignant potential, including branch-duct intraductal papillary mucinous neoplasms (BD-IPMNs) and mucinous cystadenomas.
However, it is challenging to differentiate between malignant and nonmalignant PCLs.[6,7] Currently, only a few biomarkers are available to identify high-grade dysplasia or cancer;[8,9] however, they are not easily obtained in clinical practice. The 2012 International Consensus Guidelines for the diagnosis of advanced pancreatic cystic neoplasms had a diagnostic sensitivity of 97% and low specificity of 58% in a surgical series of patients.[10] EUS-FNA is recommended due to better performance for diagnosing PCLs. Although cytology is highly specific, it is relatively insensitive, resulting in low diagnostic yield (8%–59%).[11] Because of the limited diagnostic accuracy of these methods, the management of patients with PCLs remains challenging, both for patients in terms of mortality and morbidity,[12,13] and for health care systems supporting the costs of inappropriate treatments.
Confocal laser endomicroscopy is an emerging endoscopy technique for real-time in vivo microscopic imaging of luminal or ductal structures.[14] Needle-based confocal laser endomicroscopy (nCLE) provides visualization of the inner wall of pancreatic cysts during EUS-FNA procedure.[15,16] Recent studies have identified nCLE patterns as well as corresponding histological features of PCLs and have established comprehended nCLE criteria for the characterization of common PCLs, including serous and mucinous cystadenomas, BD-IPMN, neuroendocrine neoplasm (NEN), and pseudocysts.[17,18,19,20] However, the characterization of malignant PCLs by nCLE remains poorly understood. An nCLE imaging pattern, namely dark round aggregated cells, had been proposed for suspected malignant PCLs in a pilot study[16] and in one case report.[21]
To evaluate and validate the diagnostic performance of this nCLE image pattern, we prospectively performed nCLE in patients with PCLs, identified the nCLE imaging pattern closely related with malignant mucinous PCL, and further validated the diagnostic potential of the nCLE imaging pattern for malignant mucinous PCL.
METHODS
Study design
Patients
Patients with PCLs underwent EUS-FNA evaluation were prospectively and consecutively screened for eligibility from July 2016 to July 2018 in Peking Union Medical College Hospital (PUMCH), Beijing, China.
The inclusion criteria were: Age e18 years; CT- or MRI-confirmed pancreatic cyst with worrisome feature(s) defined by Fukouka consensus, such as history of pancreatitis, dilation of main pancreatic duct (MPD) 5–9 mm, enhanced and thickened cyst wall, size >3 cm, change in MPD caliper and distal atrophy, non-enhanced mural nodule; lymphadenopathy. The exclusion criteria were: Allergy to fluorescein contrast agent; pregnancy; EUS-FNA procedure performed within 3 months; contraindicated for EUS-FNA chronic calcifying pancreatitis; high-risk stigmata defined by Fukuoka consensus, including jaundice, dilation of MPD >10 mm, enhanced solid component, or criteria for malignancy (distant metastases, ascites, and vascular infiltration).
The study was approved by Institutional Review Board of PUMCH and was registered on ClinicalTrials.gov (NCT03182270). All patients provided written consent.
Pancreatic cystic lesions diagnosis
The diagnosis of PCLs was stringent when histological analysis of the surgical and/or FNA samples were undoubted. For the other patients, a committee of three endoscopist and two pathologists nonblindedly reviewed all available information to make a consensus diagnosis as previously described.[16,17,18,19] The published validated nCLE criteria of serous cystadenoma (SCN), mucinous cystadenoma (MCN), IPMN, and pseudocyst were also implemented,[20] and patients were diagnosed with mucinous lesion if the “epithelial border” or “papillae” nCLE criteria were met, whom were closely followed up for 6 months. Patients without a final consensus diagnosis were excluded from the study.
Pancreatic cystic lesion classification
PCLs were classified as follows: (1) malignant PCLs, including IPMN, MCN with high-grade dysplasia or invasive carcinoma, (2) nonmalignant PCLs: (a) benign PCLs, including SCN and pseudocyst; (b) premalignant PCLs, including mucinous cystadenoma, IPMN, cystic NEN, and cystic schwannoma.
EUS-FNA and needle-based confocal laser endomicroscopy procedures
All procedures were performed by the investigators (Y.F., A.Y., and X.W.) as follows. First, EUS examinations were performed using a linear echoendoscope (Olympus, GF-UCT240, Tokyo, Japan) after prophylactic antibiotic therapy. Second, a 19-G needle (Cook Medical EchoTip Ultra) preloaded with AQ-Flex 19 confocal miniprobe (Cellvizio, Mauna Kea Technologies, Paris, France) was inserted into the cyst and securely positioned under EUS guidance through a transgastric or transduodenal approach. Third, an intravenous injection of fluorescein (2 ml, 10%) was administered and the video of the inner structure of cyst was simultaneously recorded in <10 min. Fourth, after the miniprobe was retrieved from the needle, the cyst was completely drained and the cyst wall was punctured if possible.
The cyst fluid and cyst wall specimen underwent cytopathological examination, and carcinoembryonic antigen (CEA) and amylase level were quantified. Data regarding clinical record, MRI, CT, EUS imaging, EUS-FNA sampling, and nCLE procedure, were prospectively recorded on a dedicated case report form.
Patients were closely monitored for 48 h after procedure. All adverse events including pancreatitis, bleeding, perforation, infection, and allergic reaction to fluorescein were recorded.
Development of diagnostic value of needle-based confocal laser endomicroscopy for malignant pancreatic cystic lesions
A two-phase analysis was performed [Figure 1]. In first discovery phase, we first summarized the nCLE findings of PCLs diagnosed with histology of surgical samples and/or cytopathology. We than correlated the nCLE findings with malignant PCLs to identify the CLE findings specific for malignant PCLs. In second validation phase, two independent nCLE experts were trained with 6 nCLE imaging sequences and blindly assessed 43 nCLE videos from all patients. The interobserver agreements (IOAs) and the diagnostic performance of nCLE findings were evaluated. The reviewers were blinded to all clinical data and independently documented the type of cyst on a standardized sheet (if mucinous vs. nonmucinous, malignant vs. nonmalignant and then specific diagnosis of cyst type).
Figure 1.
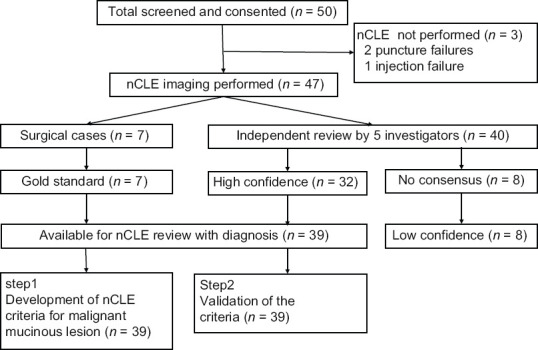
Study diagram
Statistical analysis and data management
Categorical and continuous variables were summarized as percentage and mean (standard deviation), respectively. Fisher's exact test was used to examine the association between nCLE features and malignant PCLs. A two-tailed P < 0.05 was considered statistically significant. The IOA were estimated using multirater Fleiss' kappa statistics, with a κ = 0.61–0.80 and 0.81–1.00 as substantial and excellent, respectively.
RESULTS
Patient population
A total of 50 patients with PCL was evaluated for eligibility. Three patients were excluded due to puncture failure (n = 2) and injection failure of fluorescein (n = 1). Of 47 patients underwent EUS-nCLE, seven patients had surgical histopathology, including 4 malignant mucinous lesions, 1 schwannoma, 1 mucinous cystadenoma with low-grade dysplasia, and 1 serous cystadenoma. The demographic and clinical features of the patients without surgical histopathology were listed in Supplementary Table 1. Eight patients were excluded due to no diagnosis consensus. Finally, 39 patients were enrolled, including 8 malignant mucinous lesions, 15 premalignant lesions including 13 mucinous lesions, 1 NENs, 1 schwannoma, 7 serous cystadenomas, and 9 pseudocysts. The demographic and clinical features of the patients were summarized in Table 1. Thirty cases of cyst fluid underwent CEA and amylase level examination.
Supplementary Table 1.
Demographic and clinical features of the patients without surgical histopathology
| Patient | Age | Gender | Symptom | Intracystic CEA (ng/mL) | Cytology |
|---|---|---|---|---|---|
| 1 | 47 | Female | No symptom | 2.46 | Mucinous cells |
| 2 | 67 | Female | Abdominal pain and pancreatitis | N/A | Negative for neoplasm |
| 3 | 57 | Male | Abdominal pain and pancreatitis | 661.4 | Negative for neoplasm |
| 4 | 43 | Male | Abdominal pain | N/A | Negative for neoplasm |
| 5 | 75 | Male | No symptom | N/A | Mucinous cells |
| 6 | 60 | Male | Abdominal pain | 43337 | Suspicious malignant cells |
| 7 | 56 | Male | Abdominal pain and pancreatitis | 3.4 | Mucinous cells |
| 8 | 34 | Male | Abdominal pain and pancreatitis | <0.2 | Negative for neoplasm |
| 9 | 37 | Female | Abdominal pain and jaundice | 27.4 | Negative for neoplasm |
| 10 | 35 | Male | Abdominal pain | 1.1 | Mucinous cells |
| 11 | 36 | Female | Abdominal pain and diarrhea | N/A | Neuroendocrine tumor cells |
| 12 | 35 | Female | No symptom | 0.2 | Negative for neoplasm |
| 13 | 60 | Male | No symptom | 13040 | Mucinous cells with dysplasia |
| 14 | 54 | Female | No symptom | 2.4 | Negative for neoplasm |
| 15 | 68 | Male | No symptom | 86 | Mucinous cells |
| 16 | 35 | Female | Abdominal pain | 2.4 | Negative for neoplasm |
| 17 | 48 | Male | Abdominal pain and pancreatitis | 37.8 | Negative for neoplasm |
| 18 | 55 | Female | No symptom | 10.2 | Mucinous cells |
| 19 | 64 | Female | No symptom | N/A | Negative for neoplasm |
| 20 | 61 | Male | No symptom | 95.6 | Negative for neoplasm |
| 21 | 68 | Female | Abdominal pain | N/A | Negative for neoplasm |
| 22 | 52 | Female | No symptom | 305 | Mucinous cells |
| 23 | 43 | Male | Abdominal pain and pancreatitis | 1.2 | Inflammatory cells |
| 24 | 65 | Female | No symptom | 922 | Negative for neoplasm |
| 25 | 44 | Female | No symptom | 113 | Inflammatory cells |
| 26 | 37 | Male | Abdominal pain | 0.7 | Negative for neoplasm |
| 27 | 66 | Male | No symptom | 0.2 | Negative for neoplasm |
| 28 | 32 | Female | Abdominal pain | 2638 | Suspicious malignant cells |
| 29 | 62 | Female | Abdominal pain | 0.6 | Negative for neoplasm |
| 30 | 40 | Male | Abdominal pain and pancreatitis | N/A | Inflammatory cells |
| 31 | 61 | Male | Abdominal pain | 1.1 | Negative for neoplasm |
| 32 | 37 | Female | Abdominal pain and pancreatitis | 22.7 | Negative for neoplasm |
| 33 | 47 | Female | Abdominal pain | 0.6 | Negative for neoplasm |
| 34 | 51 | Female | Abdominal pain | N/A | Negative for neoplasm |
| 35 | 61 | Male | Abdominal pain and jaundice | N/A | Negative for neoplasm |
| 36 | 60 | Male | No symptom | 1.6 | Atypical cells |
| 37 | 67 | Female | No symptom | 0.2 | Negative for neoplasm |
| 38 | 63 | Male | Jaundice | 2 | Atypical cells |
| 39 | 27 | Male | No symptom | 1.1 | Negative for neoplasm |
CEA: Carcinoembryonic antigen; N/A: Not available.
Table 1.
Characteristics of patients and cyst
| Characteristic | Patients (n=39) |
|---|---|
| Age, mean (range), years | 51 (27-75) |
| Male gender, n (%) | 19 (49) |
| Symptoms, n (%) | |
| Abdominal pain | 25 (64) |
| Asymptomatic | 13 (33) |
| Cholestasis | 1 (3) |
| Cyst location, n (%) | |
| Body | 7 (20) |
| Head | 17 (44) |
| Neck | 3 (8) |
| Tail | 10 (26) |
| Uncinate | 2 (5) |
| Cyst size, mean (range), mm | 33 (12-105) |
| Number of cavities, n (%) | |
| Single | 19 (49) |
| Multiple | 20 (51) |
| Cyst wall thickness (≥1 mm), n (%) | 4 (10) |
| Cyst calcification, n (%) | 6 (15) |
| Main pancreatic duct dilation, n (%) | 7 (18) |
| Intracystic CEA, n/N (%) | |
| >192 ng/mL | 7/30 (23) |
| <5 ng/mL | 14/30 (47) |
CEA: Carcinoembryonic antigen.
Step 1: The development of needle-based confocal laser endomicroscopy criteria for malignant mucinous lesion
Three gastroenterologists (Y.F., A.Y., and X.W.) and two gastrointestinal pathologists (Z.M. and X.C.) reviewed a total of 39 nCLE videos from 39 patients whose final diagnosis was based on a surgical specimen and/or positive cytopathology. Histology images [Figure 2] and nCLE imaging were reviewed side by side. Dark aggregates of cells, villous structures, floating black or bright particles, and superficial vascular network were frequently observed in nCLE imaging [Table 2]. Among them, dark aggregates of cells were the only feature closely related with malignant ML (P < 0.001). The dark aggregates of compact cells on nCLE were surrounded by various quantities of irregular small vessels or gray tissue [Figure 3 and Video 1]. Therefore, we used the dark aggregates of cells as the nCLE criterion for malignant ML.
Figure 2.
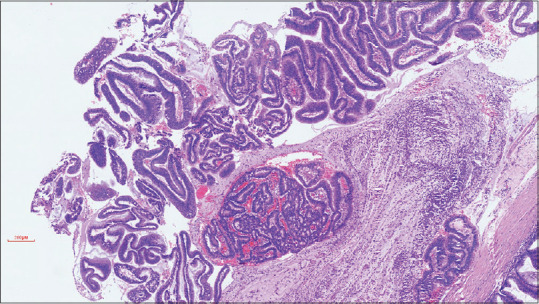
Representative H and E staining of malignant mucinous cystic lesions
Table 2.
Findings on needle-based confocal laser endomicroscopy and the association with malignant pancreatic mucinous cystic lesions (n=39)
| nCLE finding | Malignant PCLs (n=8) | Non-malignant PCLs (n=29b) | Pa |
|---|---|---|---|
| Dark aggregates of cells | 7 | 0 | <0.001 |
| Villous structures | 1 | 13 | 0.218 |
| Floating black or bright particles | 0 | 9 | 0.160 |
| Superficial vascular network | 0 | 7 | 0.308 |
aP value from Fisher’s exact test, bNeuroendocrine neoplasm and schwannoma are not included. nCLE: Needle-based confocal laser endomicroscopy; Malignant PCLs: Including intraductal mucinous neoplasm or mucinous cystadenoma with high-grade dysplasia or with invasive carcinoma; PCLs: Pancreatic cystic lesions.
Figure 3.
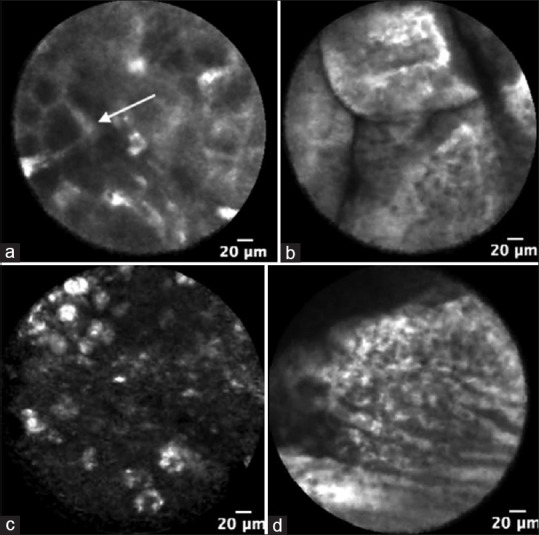
Needle-based confocal laser endomicroscopy images of mucinous cystic lesions. (a) Dark aggregates of cells (white arrow); (b) Villous structures; (c) Floating black or bright particles; (d) Superficial vascular network.
Step 2: Validation of the needle-based confocal laser endomicroscopy criteria for malignant mucinous lesion
We further validated the nCLE criterion in an independent set of 43 nCLE video sequences from 39 patients, which were not used in previous phase. Two independent nCLE experts (C.X. and N.Z.) underwent fundamental training based on six representative videos, one of which featured the newly defined findings, and then reviewed the nCLE videos in a randomized order. In 95% patients (n = 37), all reviewers provided a definite diagnosis. Furthermore, IOA of the new pattern for diagnosis of malignant ML was substantial (κ = 0.75), and global IOA was substantial (κ = 0.70). Finally, a conclusive consensus diagnosis was obtained in 35 patients (90%).
Diagnostic performance of needle-based confocal laser endomicroscopy and EUS-FNA for malignant mucinous lesion
The conclusive nCLE diagnoses were compared with the final diagnoses. The overall accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the nCLE criterion for malignant ML were 94%, 75%, 100%, 100%, and 93%, respectively. Furthermore, we also compared the diagnostic performance of EUS-FNA and EUS-FNA combined with nCLE.
EUS-FNA was conclusive in 3 of 8 malignant ML cases (37%). The overall accuracy, sensitivity, specificity, PPV, and NPV of EUS-FNA for malignant ML were compared with nCLE performance. Surprisingly, the EUS-FNA combined with nCLE showed similar overall accuracy, sensitivity, specificity, PPV, and NPV with nCLE alone. The accuracy, sensitivity, and negative likelihood ratio (LR-) of nCLE for the diagnosis of malignant ML were significantly better than EUS-FNA [Table 3].
Table 3.
Diagnostic value for malignant versus nonmalignant mucinous cystic lesions of needle-based confocal laser endomicroscopy, EUS-FNA and needle-based confocal laser endomicroscopy + EUS-FNA in 35 conclusive patients (per protocol analysis)
| EUS-FNA | nCLEa | nCLE+FNA | |
|---|---|---|---|
| TP (n) | 3 | 6 | 6 |
| FP (n) | 0 | 0 | 0 |
| TN (n) | 27 | 27 | 27 |
| FN (n) | 5 | 2 | 2 |
| Accuracy | 84 (67-95) | 94 (80-99) | 94 (80-99) |
| Sensitivity | 38 (9-76) | 75 (36-96) | 75 (36-96) |
| Specificity | 100 (86-100) | 100 (84-100) | 100 (84-100) |
| PPV | 100 (100-100) | 100 (52-100) | 100 (52-100) |
| NPV | 83 (74-89) | 93 (76-99) | 93 (76-99) |
| LR+ | Infinity | Infinity | Infinity |
| LR- | 62 (37-100) | 25 (8-83) | 25 (8-83) |
aDark aggregates of cells, Data are shown in percentage (95% CI) unless otherwise indicated. nCLE: Needle-based confocal laser endomicroscopy; PPV: Positive predictive value; NPV: Negative predictive value; CI: Confidence interval.
DISCUSSION
In this study, we found dark aggregates of compact cells surrounded by irregular small vessels on nCLE were a highly specific feature for malignant mucinous cystic lesions. We further demonstrated that these nCLE criteria were reliable and reproducible, with higher sensitive than traditional EUS-FNA. In addition, these nCLE criteria remained high specificity for malignant ML, suggesting it was a promising diagnostic tool for malignant ML.
Highly specific nCLE criteria for the classification of different pancreatic cyst types have been reported in several studies.[17,18,19,20] However, these studies focused on differentiation mucinous lesions from nonmucinous lesions, or premalignant lesions from benign lesions. However, in this study, we aimed to develop a new nCLE criteria specifically for malignant MLs.
Malignant mucinous cystic lesions include IPMN and MCN with high-grade dysplasia or with invasive carcinoma. Histologically, the internal surface of nonmalignant MCN is typically smooth, whereas those of high-grade neoplasms frequently have papillary projections with irregular branching and budding [Figure 4]. The epithelium of nonmalignant IPMNs is usually flat or form papillae with fibrovascular cores, while those of IPMNs with high-grade dysplasia are characterized with the formation of irregular branching papillae and sometimes cribriform growth architecturally.[22] Two studies found CLE has potential for grading dysplasia.[23,24] The irregularity and fragmentation can be seen in the papillary structures on the confocal image of cases with high-grade dysplasia and invasive cancer.[23] Krishna found the thickness and the darkness of the papillary epithelium were the variables with the highest diagnostic accuracy and IOA for IPMN with high-grade dysplasia and invasive cancer.[24] However, qualitative image analysis among different endoscopists is prone to interobserver disagreement. Simple criteria are better for clinical practice. On CLE, the malignant papillary projection was presented as a dark aggregates of neoplastic cells surrounded with irregular white or gray fibrotic vascular stroma, and it is easier for real-time evaluation. The nCLE analyses of cystic NEN revealed a similar pattern of dark spots of cell aggregates, surrounded by gray areas of fibrosis and vessels, the cell aggregates of NEN were not papillary projections but nesting, glandular or tubuloacinar arrangements of well-differentiated cells, which were not as round as the cluster of malignant mucinous cells. Moreover, given the nonuniform nature of the epithelium in malignant MLs, the characteristic of nonmalignant MLs may also be visualized by nCLE, which facilitated to differentiate malignant MLs from cystic NEN on endomicroscopy. Sometimes, walled off necrotic cavities or MCN with significant burden of inflammation can also reveal dark clumps of inflammatory cells; however, these clumps are floating and irregular compared to the malignant mucinous lesions, which can be differentiated by experienced nCLE endoscopists.
Figure 4.
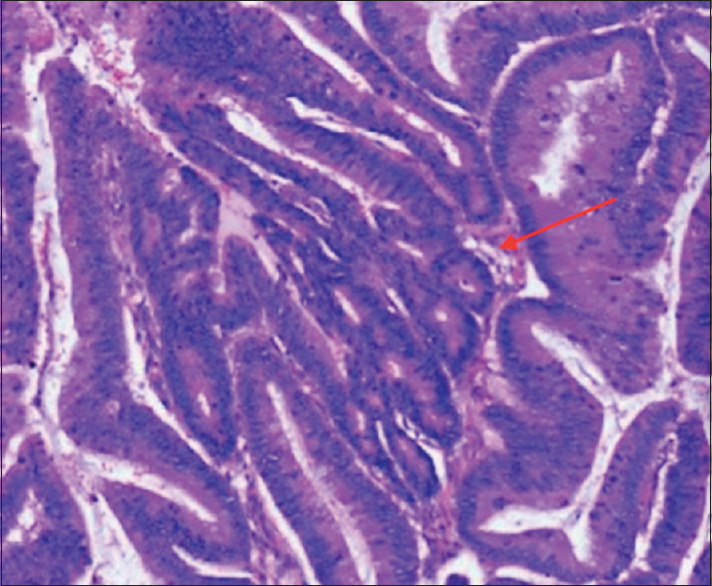
Representative H and E staining of malignant mucinous cystic lesions. Histology of cyst wall with papillary projections (red arrow)
According to international consensus guidelines, further evaluation with EUS and/or cytology is recommended for patients with imaging findings of “worrisome features.”[25] However, the accuracy of EUS without contrast-enhancing technique for malignant MLs were as low as 56%.[26] Consistently, we found the sensitivity of EUS-FNA for malignant MLs was 38%, albeit high specificity. In contrast, our nCLE criteria showed significantly higher sensitivity and LR-than EUS-FNA for malignant MLs, and maintained high specificity, PPV, and accuracy. Moreover, EUS combined with nCLE easily detected malignant papillary projection 20–100 μ in diameter, an “earlier” change of malignancy, which was undetected with other conventional imaging modalities.
However, concerning about the nCLE-associated adverse events, the updated the European guidelines on pancreatic cystic neoplasms recommended against using nCLE for the diagnosis of PCLs.[11] Of the two trials included in the European guideline, the postprocedure pancreatitis rate is 7% and 3% in one study without time limitation for nCLE imaging[27] and one study with time limitation.[16] A maximum time limit of 10 min in nCLE imaging might improve safety. In our study, we maintained a strict imaging time limitation of 10 min, and no procedure-related pancreatitis or bleeding after nCLE were observed.
Our study has limitations. First, a gold standard diagnosis of MLs, which was confirmation by histopathological analysis of surgical specimen or histocytopathological analysis of cystic fluid or cystic wall, was not available for 11 mucinous PCLs patients. Therefore, inherent sampling error with the presence of mixed types of epithelium in mucinous lesions or variable placement of the probe is inevitable, and the sensitivity and NPV of the nCLE criteria for malignant MLs might be overestimated. A future study evaluating the performance of the new nCLE criteria with histopathological-confirmed ML is warranted. Second, only patients with worrisome features defined by Fukouka consensus were enrolled, and those cysts with high-risk features as displayed in the Fukouka consensus were excluded. Given the fact that, the specificity of Fukouka consensus was only about 58% and efforts had been made to improve the diagnostic performance,[25] future studies might also aim to compare the performance of Fukouka consensus with or without the new nCLE criteria in a surgical cohort. However, to the best of our knowledge, this is the first prospective study on diagnostic finding of nCLE for malignant MLs, and we believe that our findings worth further prospective studies.
CONCLUSION
We proposed a new nCLE criteria, namely dark round cluster of neoplastic cells surrounded with irregular white or gray fibrotic vascular stroma, is sensitive and specific for the diagnose of malignant ML, which is warranted to confirm in a larger prospective multi-center study.
Supplementary materials
Supplementary information is linked to the online version of the paper on the Endoscopic Ultrasound website.
Financial support and sponsorship
Supported by the Capital Health Research and Development of Special Project (2018-2-4014) and the Fundamental Research Funds for the Central Universities (3332019033).
Conflicts of interest
There are no conflicts of interest.
Video Available on: www.eusjournal.com
Acknowledgment
The authors thank Professor Can Xu, from Changhai Hospital, China, and Professor Ning Zhong, from Qilu Hospital, China, for their kind help in validation phase.
REFERENCES
- 1.Spinelli KS, Fromwiller TE, Daniel RA, et al. Cystic pancreatic neoplasms: Observe or operate. Ann Surg. 2004;239:651–7. doi: 10.1097/01.sla.0000124299.57430.ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laffan TA, Horton KM, Klein AP, et al. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol. 2008;191:802–7. doi: 10.2214/AJR.07.3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee KS, Sekhar A, Rofsky NM, et al. Prevalence of incidental pancreatic cysts in the adult population on MR imaging. Am J Gastroenterol. 2010;105:2079–84. doi: 10.1038/ajg.2010.122. [DOI] [PubMed] [Google Scholar]
- 4.Zhang XM, Mitchell DG, Dohke M, et al. Pancreatic cysts: Depiction on single-shot fast spin-echo MR images. Radiology. 2002;223:547–53. doi: 10.1148/radiol.2232010815. [DOI] [PubMed] [Google Scholar]
- 5.Chiang AL, Lee LS. Clinical approach to incidental pancreatic cysts. World J Gastroenterol. 2016;22:1236–45. doi: 10.3748/wjg.v22.i3.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belsley NA, Pitman MB, Lauwers GY. Serous cystadenoma of the pancreas: Limitations and pitfalls of endoscopic ultrasound-guided fineneedle aspiration biopsy. Cancer. 2008;114:102–10. doi: 10.1002/cncr.23346. [DOI] [PubMed] [Google Scholar]
- 7.Park WG, Mascarenhas R, Palaez-Luna M, et al. Diagnostic performance of cyst fluid carcinoembryonic antigen and amylase in histologically confirmed pancreatic cysts. Pancreas. 2011;40:42–5. doi: 10.1097/MPA.0b013e3181f69f36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singhi AD, McGrath K, Brand RE, et al. Preoperative next-generation sequencing of pancreatic cyst fluid is highly accurate in cyst classification and detection of advanced neoplasia. Gut. 2018;67:2131–41. doi: 10.1136/gutjnl-2016-313586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Das KK, Geng X, Brown JW, et al. Cross validation of the monoclonal antibody das-1 in identification of high-risk mucinous pancreatic cystic lesions. Gastroenterology. 2019;157:720–3000. doi: 10.1053/j.gastro.2019.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sighinolfi M, Quan SY, Lee Y, et al. Fukuoka and AGA criteria have superior diagnostic accuracy for advanced cystic neoplasms than sendai criteria. Dig Dis Sci. 2017;62:626–32. doi: 10.1007/s10620-017-4460-y. [DOI] [PubMed] [Google Scholar]
- 11.European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018;67:789–804. doi: 10.1136/gutjnl-2018-316027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Valsangkar NP, Morales-Oyarvide V, Thayer SP, et al. 851 resected cystic tumors of the pancreas: A 33-year experience at the Massachusetts General Hospital. Surgery. 2012;152:S4–12. doi: 10.1016/j.surg.2012.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gaujoux S, Brennan MF, Gonen M, et al. Cystic lesions of the pancreas: Changes in the presentation and management of 1,424 patients at a single institution over a 15-year time period. JAm Coll Surg. 2011;212:590–600. doi: 10.1016/j.jamcollsurg.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fugazza A, Gaiani F, Carra MC, et al. Confocal laser endomicroscopy in gastrointestinal and pancreatobiliary diseases: A systematic review and meta-analysis. Biomed Res Int. 2016;2016:4638683. doi: 10.1155/2016/4638683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Konda VJ, Aslanian HR, Wallace MB, et al. First assessment of needle-based confocal laser endomicroscopy during EUS-FNA procedures of the pancreas (with videos) Gastrointest Endosc. 2011;74:1049–60. doi: 10.1016/j.gie.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 16.Konda VJ, Meining A, Jamil LH, et al. A pilot study of in vivo identification of pancreatic cystic neoplasms with needle-based confocal laser endomicroscopy under endosonographic guidance. Endoscopy. 2013;45:1006–13. doi: 10.1055/s-0033-1344714. [DOI] [PubMed] [Google Scholar]
- 17.Napoléon B, Lemaistre AI, Pujol B, et al. A novel approach to the diagnosis of pancreatic serous cystadenoma: Needle-based confocal laser endomicroscopy. Endoscopy. 2015;47:26–32. doi: 10.1055/s-0034-1390693. [DOI] [PubMed] [Google Scholar]
- 18.Napoleon B, Lemaistre AI, Pujol B, et al. In vivo characterization of pancreatic cystic lesions by needle-based confocal laser endomicroscopy (nCLE): Proposition of a comprehensive nCLE classification confirmed by an external retrospective evaluation. Surg Endosc. 2016;30:2603–12. doi: 10.1007/s00464-015-4510-5. [DOI] [PubMed] [Google Scholar]
- 19.Krishna SG, Swanson B, Hart PA, et al. Validation of diagnostic characteristics of needle based confocal laser endomicroscopy in differentiation of pancreatic cystic lesions. Endosc Int Open. 2016;4:E1124–35. doi: 10.1055/s-0042-116491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Napoleon B, Palazzo M, Lemaistre AI, et al. Needle-based confocal laser endomicroscopy of pancreatic cystic lesions: A prospective multicenter validation study in patients with definite diagnosis. Endoscopy. 2019;51:825–35. doi: 10.1055/a-0732-5356. [DOI] [PubMed] [Google Scholar]
- 21.Feng YL, Yang AM, Wu X, et al. Use of needle-based confocal laser endomicroscopy in the diagnosis of multifocal intraductal papillary mucinous neoplasm with high grade dysplasia. Endoscopy. 2017;49:E277–8. doi: 10.1055/s-0043-115889. [DOI] [PubMed] [Google Scholar]
- 22.Nagtegaal ID, Odze RD, Klimstra D, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76:182–8. doi: 10.1111/his.13975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kadayifci A, Atar M, Yang M, et al. Imaging of pancreatic cystic lesions with confocal laser endomicroscopy: An ex vivo pilot study. Surg Endosc. 2017;31:5119–26. doi: 10.1007/s00464-017-5577-y. [DOI] [PubMed] [Google Scholar]
- 24.Krishna SG, Hart PA, DeWitt JM, et al. EUS-guided confocal laser endomicroscopy: Prediction of dysplasia in intraductal papillary mucinous neoplasms (with video) Gastrointest Endosc. 2020;91:551–630. doi: 10.1016/j.gie.2019.09.014. [DOI] [PubMed] [Google Scholar]
- 25.Tanaka M, Fernández-Del Castillo C, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017;17:738–53. doi: 10.1016/j.pan.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 26.Hwang J, Kim YK, Min JH, et al. Comparison between MRI with MR cholangiopancreatography and endoscopic ultrasonography for differentiating malignant from benign mucinous neoplasms of the pancreas. Eur Radiol. 2018;28:179–87. doi: 10.1007/s00330-017-4926-5. [DOI] [PubMed] [Google Scholar]
- 27.Nakai Y, Iwashita T, Park DH, et al. Diagnosis of pancreatic cysts: EUS-guided, through-the-needle confocal laser-induced endomicroscopy and cystoscopy trial: DETECT study. Gastrointest Endosc. 2015;81:1204–14. doi: 10.1016/j.gie.2014.10.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


