Abstract
Background
The COVID‐19 pandemic introduced unparalleled uncertainty into the lives of pregnant women, including concerns about where it is the safest to give birth, while preserving their rights and wishes. Reports on the increased interest in community births (at home or in birth centers) are emerging. The purpose of this project was to quantitatively investigate psychological factors related to this birth preference.
Methods
This study included 3896 pregnant women from the COVID‐19 Pregnancy Experiences (COPE) Study who were anticipating a vaginal birth. COPE Study participants were recruited online between April 24 and May 15, 2020, and completed a questionnaire that included preference with respect to place of birth and psychological constructs: fear of childbirth, basic beliefs about birth, pandemic‐related preparedness stress, and pandemic‐related perinatal infection stress.
Results
Women who preferred a community birth, on average, had less childbirth fear, had stronger beliefs that birth is a natural process, were less likely to see birth as a medical process, and were less stressed about being unprepared for birth and being infected with COVID‐19. In multivariate models, higher stress about perinatal COVID‐19 infection was associated with greater likelihood of preferring a community birth. The effect of perinatal infection stress on preference was stronger when preparedness stress was high.
Discussion
Women's birth preferences during the COVID‐19 pandemic are associated with psychological processes related to risk perception. Community births are more appealing to women who view being in a hospital as hazardous because of the pandemic. Policies and prenatal care aimed to increase access to safe in‐hospital and out‐of‐hospital birth services should be encouraged.
Keywords: beliefs about birth, COVID‐19 pandemic, fear of birth, pandemic‐related pregnancy stress, place of birth
1. INTRODUCTION
Choosing to give birth in an out‐of‐hospital environment—at home or in a birth center—also known as community birth, 1 is an uncommon choice in the United States. Although rates of community births have increased in the United States since 2004, they still accounted for < 2% of births in 2017. 2 The outbreak of the novel coronavirus (COVID‐19) pandemic in Spring 2020 has sparked growing interest among pregnant women, legislators, and policymakers in community births. The purpose of this study was to investigate contributors to preference for community birth among women residing in the United States who were pregnant at the beginning of the COVID‐19 pandemic.
1.1. Choosing community births
There are two main types of community births, those at home (usually with the accompaniment of a midwife) and those at birth centers (also called freestanding birth centers or natural birth centers). Community births are not suitable for women with high‐risk pregnancies who are more likely to have complicated deliveries. Although over the years there has been debate over the safety of community births for low‐risk pregnancies, 3 , 4 accumulating evidence suggests that they are a safe birth option for these women; they are associated with fewer interventions (eg, lower unplanned cesarean rates), 5 , 6 greater patient satisfaction, 7 and lower cost 8 than in‐hospital births. Over the last 15 years, there has been a rise in the United States community birth rate (both home births and birth centers), but it remains uncommon. 2 , 9 , 10
Over the last two decades, studies have explored reasons related to community birth preference including psychological factors and maternal characteristics associated with this preference. Fear of birth has been explored as a predictor of place of birth, and evidence suggests that women with high levels of fear are more likely to choose a hospital birth. 11 Basic beliefs about birth have emerged in the last few years as pivotal contributors to women's birth choices. 12 These beliefs are closely related to conceptualizations of midwifery/holistic/social birth models and obstetric/medical/technocratic birth models 13 , 14 , 15 and operationalize the extent to which women view birth as a natural and safe process and as a medical and risky one. 16 Birth beliefs are predictive of type and place of birth preference, emergency birth modes (ie, unplanned cesarean, assisted vaginal birth), and birth satisfaction. 17 , 18 , 19 In addition, qualitative research highlights risk, empowerment, control, and autonomy as key concepts in community birth preferences: Women who elect to birth at home or in birth centers often wish to conserve their autonomy, to feel empowered and to remain in control of their birth (eg, not have medical professionals manage their birth and use medication to control labor pain). They may also view hospitals and obstetric/medical/technocratic birth models as themselves risky (eg, concerned about a cascade of interventions, worried their rights will not be respected, worried they will be subjected to unnecessary surgery). 20 , 21 , 22 , 23 Although knowledge about women's choices of community birth is growing and evolving, little is known about how the unprecedented COVID‐19 pandemic changed the risk calculus surrounding birth setting and affected women's birth preferences.
1.2. COVID‐19 pandemic and place of birth
The COVID‐19 pandemic has dramatically affected the lives of pregnant women and potentially affected their childbirth preferences, including place of birth. 24 , 25 In Spring 2020, COVID‐19 was declared a global pandemic by the World Health Organization followed by rapid growth in the numbers of infected individuals. In addition, various restrictions to minimize exposure to the virus were put in place, such as social distancing, limiting companions during delivery, and forbidding postpartum in‐hospital visitations. 24 , 26 , 27 These issues along with concerns about perinatal infection when giving birth at a hospital, and a desire to reduce the burden on overextended hospitals may have made community births more desirable for some pregnant people during the COVID‐19 pandemic. Anecdotal reports highlight the possible shift in women's preferences about place of birth, 28 , 29 but to our knowledge, there has not been a thorough analysis of the psychological factors related to preferred place of delivery during the COVID‐19 pandemic.
Pregnant women experience a variety of stressors related specifically to being pregnant. 30 These include concerns about bodily changes and physical symptoms, the birth, the health of the child, and being able to financially provide for a newborn. The COVID‐19 pandemic has added to the pregnancy‐specific stress that expectant mothers are experiencing. Pandemic‐related pregnancy stress is a particular type of pregnancy‐specific stress that focuses on two main concerns related to being pregnant during the pandemic: preparedness concerns and perinatal infection concerns. 31 , 32 Preparedness stress refers to feeling unprepared for the birth and postpartum period because of pandemic‐related restrictions, such as not being able to exercise and eat well, concerns about not receiving adequate prenatal care because of the pandemic, and not being able to receive help in the postpartum period. Perinatal infection stress relates to concerns about COVID‐19 infection for mother and fetus/newborn and includes worries about infection harming the pregnancy and contracting COVID‐19 during hospital delivery. An instrument to assess pandemic‐related pregnancy stress was recently introduced and validated and yielded evidence that both types of pandemic stress contribute to prenatal mental health. Although preparedness stress and infection stress are correlated, they are distinct constructs that are associated with different predictors; individually and together, they predict general anxiety symptoms in pregnant women. 31
As a result of their central role in women's emotions during the COVID‐19 pandemic, we hypothesized that pandemic‐related stresses would affect women's preferences related to where they give birth during the COVID‐19 pandemic. Community births may be appealing to some women based on the expectation that they will offer more control for women, greater autonomy, and self‐efficacy. 21 , 23 Therefore, opting for such a birth may require more mental and physical preparation than a hospital birth. We reasoned that women who feel unprepared for birth, or in other words, have high pandemic‐related preparedness stress, would be less likely to prefer a community birth. Conversely, high pandemic‐related perinatal infection stress might be a reason why women would prefer a community birth as a strategy to reduce risk of infection for themselves and their newborn. To summarize, we hypothesized that women with lower preparedness stress and higher infection stress would be more likely to prefer a community birth.
2. METHODS
2.1. Participants and procedure
Data for the current study are from the first time point of the COVID‐19 Pregnancy Experiences (COPE) Study. Between April 24 and May 15, 2020, pregnant women 18 years or older were invited to participate in the COPE Study through social media. Facebook paid advertisements targeted women in the United States with pregnancy‐related interests (95% of participants). In addition, research assistants posted an identical advertisement for the study on various pregnancy‐related social media groups and pages (Facebook, Instagram, and Reddit). The advertisement included a request to share pregnancy‐related experiences during COVID‐19. The online questionnaire was completed through a HIPAA‐compliant online survey platform. Inclusion criteria were being currently pregnant, ≥18 years old, and able to read and write in English. Research assistants reviewed all participants’ responses, consequently removing 189 women who had not completed the entire questionnaire and women who did not meet inclusion criteria (ie, were postpartum or had experienced fetal demise before completing the questionnaire), resulting in 4424 participants. Participants who completed the questionnaire were enrolled in a raffle with a 1/100 chance to win a $100 gift card. The study was approved on April 21, 2020, by the Institutional Review Board of Stony Brook University. Since the main outcome of the current analysis is preference for community birth, we included only women who were anticipating a vaginal birth, resulting in a final sample of 3896 women.
2.2. Measures
Sociodemographic and obstetric factors included maternal age, ethnicity and race, financial status (based on subjective impression of financial state being below average/ average/ above average), relationship status (married or cohabiting/ serious relationship/ single/ other), and health insurance status (private, Medicaid, uninsured). Obstetric factors included parity, gestational age, and self‐reported high‐risk pregnancy status (No vs Yes or unsure).
Childbirth preferences assessed how and where women preferred to give birth. Women were asked: “For this pregnancy, how would you prefer to give birth? (select the most likely)” with the following options: (a) cesarean birth at my own request (without medical reason); (b) cesarean birth for a medical reason; (c) vaginal birth with epidural pain medication in a hospital; (d) vaginal birth without pain medication in a hospital; (e) birth at a natural birth center or freestanding birthing facility; (f) home birth; and (g) other. Women preferring cesarean deliveries (1 & 2) and choosing other (7) were excluded; women preferring in‐hospital births (3 & 4) were coded as 0, and women preferring community births (5 & 6) were coded as 1.
Fear of childbirth was measured using the two‐item Fear of Birth Scale. 33 Women were asked about their feelings about the upcoming birth on a 0‐100 visual analog scale (VAS) with the following anchors: Calm versus Worried and No Fear versus Strong Fear. Internal consistency was excellent (α = 0.90), and scale scores were calculated as the mean response of the two VAS items (range 0‐100).
Basic beliefs about birth were assessed using the Birth Beliefs Scale. 16 Women reported their agreement with 11 items related to the physiological nature of the birth process on a scale from 1 = strongly disagree to 5 = strongly agree. The instrument is comprised of two factors: beliefs about birth as a natural process (five items; eg, “The body knows how to give birth”) and beliefs about birth as a medical process (six items; eg, “There are many things that could go wrong during birth”). Scale scores were calculated as the mean response of items on the corresponding factor (range 1‐5). The natural and the medical factors had acceptable internal consistency (αs = 0.68 and 0.75, respectively).
Pandemic‐related pregnancy stress was assessed using the Pandemic‐Related Pregnancy Stress Scale (PREPS)—a novel instrument that was recently validated in the United States 32 and several other countries. 34 , 35 , 36 We used the two PREPS factors: preparedness stress (seven items; eg, “I am worried that the pandemic could ruin my birth plans”) and perinatal infection stress (five items; eg, “I am worried that my baby could get COVID‐19 at the hospital after birth”) with a response scale from 1 = very little to 5 = very much. Scale scores were calculated as the mean response of items on the corresponding factor (range 1‐5). The preparedness and stress factors were internally consistent (αs = 0.81 and 0.86, respectively).
2.3. Statistical analysis
Statistical analysis was conducted using the SPSS version 26.0. 37 Initially, we conducted univariate analysis (chi‐square, t test and one‐way analysis of variance, and Pearson's correlations). Thereafter, we performed multivariate analysis by conducting a binary logistic regression using all of the study variables as predictors of preference (in‐hospital vs out‐of‐hospital birth), including the interaction between preparedness stress and perinatal infection stress. Finally, we examined the interaction between the two PREPS factors using PROCESS Macros. 38 Because missing data for study variables were minimal, ranging from 0.0% to 0.1%, listwise deletion of cases was used. A P value < 0.05 was considered significant.
3. RESULTS
3.1. Sample characteristics and descriptive results
The average age of the 3896 study participants who anticipate having a vaginal birth was 30.6 ± 4.6 years, their average gestational age at survey completion was 26.6 ± 8.7 weeks, and 55.2% (n = 2151) were nulliparas. The majority of participants (91.7%, n = 3574) preferred having a hospital birth. Additional sample characteristics can be found in Table 1. Mean scores of psychological variables can be found in Table 2.
TABLE 1.
Maternal sociodemographic and obstetric characteristics of 3896 pregnant women during the COVID‐19 pandemic outbreak, the United States, April‐May 2020
| n (%) | |
|---|---|
| Race/Ethnicity a | |
| Non‐Hispanic White | 3195 (82.0) |
| Non‐White and/or Hispanic/Latino | 701 (18.0) |
| Relationship status | |
| Married or cohabiting | 3579 (91.9) |
| Some or no relationship | 371 (8.1) |
| Financial security | |
| Below average | 628 (16.1) |
| Average | 2300 (59.1) |
| Above average | 967 (24.8) |
| Insurance | |
| Private | 3319 (85.2) |
| Medicaid | 538 (13.8) |
| Uninsured | 39 (1.0) |
| Maternal age | |
| Less than 35 years old | 3122 (80.2) |
| 35 years or older | 770 (19.8) |
| Parity | |
| Nullipara | 2151 (55.3) |
| Multipara | 1741 (44.7) |
| High‐risk pregnancy | |
| No | 2632 (67.6) |
| Unsure | 261 (6.7) |
| Yes | 1003 (25.7) |
| Preferred birth | |
| Hospital birth with epidural | 2217 (56.9) |
| Hospital birth without epidural | 1355 (34.8) |
| Freestanding birthing facility | 178 (4.6) |
| Home birth | 146 (3.7) |
Women who endorsed any racial or ethnic identity other than White non‐Hispanic were included in this group.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
TABLE 2.
Descriptive information and associations between perceptions about birth and pandemic‐related pregnancy stress among 3896 pregnant women during the COVID‐19 pandemic outbreak, the United States, April‐May 2020
| Range | M + SD | 1 | 2 | 3 | 4 | |
|---|---|---|---|---|---|---|
| 1. Fear of childbirth | 0‐100 | 55.65 ± 23.32 | ‐ | |||
| 2. Beliefs about birth—natural | 1‐5 | 3.98 ± 0.51 | −0.22 | ‐ | ||
| 3. Beliefs about birth—medical | 1‐5 | 3.38 ± 0.65 | 0.26 | −0.49 | ‐ | |
| 4. PREPS—preparedness | 1‐5 | 3.46 ± 0.87 | 0.59 | −0.08 | 0.15 | ‐ |
|
5. PREPS—infection |
1‐5 | 3.24 ± 0.99 | 0.48 | −0.08 | 0.18 | 0.59 |
All correlations P < 0.001.
Abbreviation: PREPS, Pandemic‐Related Pregnancy Stress Scale.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Pandemic‐related stress was correlated with perceptions of birth (Table 2). Both Preparedness stress and perinatal infection stress were strongly and positively correlated with fear of birth. PREPS factors were correlated significantly, although modestly, with beliefs about birth—medical and were inversely and weakly correlated with beliefs about birth—natural.
3.2. Univariate correlates of place of birth preference
More women preferring a community birth reported below mean income compared with those preferring a hospital birth (24.4% vs 15.4%; χ2(1) = 17.74, P < 0.001), more of the former were insured through Medicaid or were uninsured (25.0% vs 13.9%, χ2(1) = 28.95, P < 0.001), and they were less likely to be nulliparas (41.7% vs 56.5%, χ2(1) = 26.33, P < 0.001). Participants with high‐risk pregnancies and those who were unsure about having a high‐risk pregnancy were less likely to prefer a community birth (5.4% and 4.2% vs 10.2%, χ2(2) = 37.43, P < 0.001). For this reason, women who reported a high‐risk pregnancy and those who were unsure were grouped together in further analyses; the rest were considered low risk. Race/ethnicity, relationship status, age, and gestational age were unrelated to preference for in‐hospital or out‐of‐hospital birth (Table 3).
TABLE 3.
Mean differences in psychological variables between women preferring in‐hospital or out‐of‐hospital birth among 3896 pregnant women during the COVID‐19 pandemic outbreak, the United States, April‐May 2020
| In‐hospital birth (n = 325) | Community birth (n = 3574) | t | |
|---|---|---|---|
| Maternal age | 30.61 ± 4.63 | 30.64 ± 4.81 | 0.14 |
| Gestational week | 26.56 ± 8.70 | 26.94 ± 9.31 | 0.71 |
| Fear of birth | 56.61 ± 22.78 | 44.32 ± 26.12 | 8.19*** |
| Birth belief—natural | 3.94 ± 0.49 | 4.52 ± 0.45 | 20.63*** |
| Birth belief—medical | 3.47 ± 0.58 | 2.42 ± 0.65 | 27.93*** |
| Preparedness stress | 3.48 ± 0.85 | 3.15 ± 1.02 | 5.71*** |
| Perinatal infection stress | 3.26 ± 0.97 | 3.05 ± 1.19 | 3.01** |
P < 0.05
P < 0.01
P < 0.001.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
As can be seen in Table 3, on average, women who preferred a community birth had less Fear of Birth, weaker beliefs about birth—medical, stronger beliefs about birth—natural, lower pandemic preparedness stress, and lower perinatal infection stress.
3.3. Multivariate prediction of place of birth preference
We conducted a binary logistic regression that included background and obstetric characteristics, pandemic stress variables, and birth perception variables (Table 4). In the multivariate adjusted model, of the background variables, older maternal age, having Medicaid insurance or being uninsured, and having a low‐risk pregnancy were associated with higher likelihood of preferring a community birth. Of the psychological variables, all of the predictors except for Fear of Birth independently predicted preference for community birth. Stronger beliefs about birth—natural and higher perinatal infection stress increased the odds of preferring a community birth. In contrast, stronger beliefs about birth—medical and higher preparedness stress lowered the odds of preferring a community birth. It is notable that the main effect of perinatal infection stress on community birth (odds ratio 0.81, 95% confidence interval 0.73, 0.91) indicated an inverse association—higher perinatal infection stress was associated with lower preference for community birth. However, in the multivariate models, when controlling for other variables confounded with place of birth preference, perinatal infection stress predicted greater odds of preferring community birth (adjusted odds ratio 1.40, 95% confidence interval 1.17, 1.68). The interaction between the two types of PREPS factors was significant in the regression model, and therefore, we explored this further using PROCESS Macros to examine and plot the interaction. The model predicted 42% of the variance in preference for place of birth.
TABLE 4.
Binary logistic regression predicting community birth preference among 3896 pregnant women during the COVID‐19 pandemic outbreak, the United States, April‐May 2020
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| OR | 95% CI | AOR | 95% CI | |
| Older maternal age | 1.28 | (0.97, 1.67) | 1.47* | (1.03, 2.11) |
| Racial/ethnic minority | 0.97 | (0.72, 1.31) | 1.08 | (0.74, 1.57) |
| Married/cohabiting | 0.73 | (0.45, 1.16) | 0.84 | (0.47, 1.49) |
| Below‐average income | 1.78*** | (1.36, 2.32) | 1.47 | (0.99, 2.21) |
| Medicaid or uninsured | 2.06*** | (1.58, 2.71) | 1.77** | (1.18, 2.66) |
| Nullipara | 0.55*** | (0.44, 0.69) | 0.87 | (0.65, 1.16) |
| Gestational age | 1.02 | (0.99, 1.02) | 0.99 | (0.98, 1.01) |
| High risk a | 0.41*** | (0.30, 0.55) | 0.52** | (0.36, 0.75) |
| Fear of birth | 0.59*** | (0.53, 0.67) | 0.99 | (0.83, 1.18) |
| Birth belief—natural | 4.05*** | (3.47, 4.71) | 1.54*** | (1.28, 1.86) |
| Birth belief—medical | 0.21*** | (0.18, 0.24) | 0.28*** | (0.23, 0.33) |
| Preparedness stress | 0.69*** | (0.62, 0.77) | 0.78*** | (0.64, 0.95) |
| Perinatal infection stress | 0.82*** | (0.73, 0.91) | 1.41*** | (1.18, 1.68) |
| Preparedness × Infection | 1.38*** | (1.27, 1.50) | 1.29*** | (1.14, 1.45) |
| R 2 = 0.42 | ||||
Abbreviations: CI, confidence interval; OR, odds ratio; PREPS, Pandemic‐Related Pregnancy Stress Scale.
Women who reported being high risk and those who were unsure were grouped together.
P < 0.05
P < 0.01
P < 0.001.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
3.4. Exploring the role of pandemic stress on place of birth preference
Variables that were independently associated with preferred place of birth in the adjusted model (age, health insurance, pregnancy risk, and both beliefs about birth) were included as covariates in the PROCESS Macros model. As can be seen in Figure 1, after controlling for covariates, women most likely to prefer a community birth were those with high Infection Stress and those with low preparedness stress. The association between Infection Stress and preference for community birth was nonsignificant when preparedness stress was low (β = 0.10, P = 0.35), the effect size was medium and significant when preparedness stress was average (β = 0.34, P < 0.001), and the effect was large and significant when preparedness stress was high (β = 0.59, P < 0.001). In other words, women who felt the most stress about their preparedness for birth were more likely to prefer a community birth when their perinatal infection stress was high. Women with high preparedness stress who also had low perinatal infection stress were least likely to prefer a community birth, and women who had low preparedness stress were more likely to express this preference regardless of their Infection Stress.
FIGURE 1.
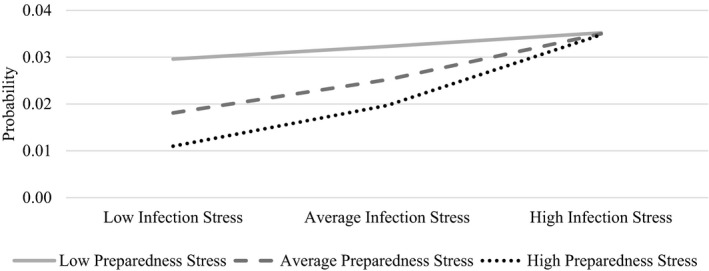
Interaction between pandemic‐related preparedness stress and perinatal infection stress in predicting community birth preference among 3896 pregnant women during the COVID‐19 pandemic outbreak, the United States, April‐May 2020
4. DISCUSSION
Our findings suggest that women's birth preferences may be affected by the COVID‐19 pandemic and that pandemic‐related stress can contribute to shifts in childbirth practices. Women may choose where to give birth based on risk perceptions, 39 , 40 , 41 with common notions that giving birth in a hospital is the safest option. 42 , 43 , 44 , 45 However, the possibility of contracting the virus in the hospital appears to be shifting pregnant people's risk perceptions in complex ways that intersect with a range of pregnancy‐related beliefs and stressors. Results of this study suggest that perceptions of COVID‐19 risk, combined with additional psychological factors (eg, feeling prepared for birth, fear of birth, beliefs about birth as natural or as a medical process), are affecting women's preference for community birth during the uncertain time of the COVID‐19 pandemic.
Pandemic‐related stresses, namely preparedness stress and perinatal infection stress, were positively related to fear of birth and to a basic belief that birth is a medical process. These stresses were also inversely related to the belief that birth is a natural process. In addition, as hypothesized, community birth preference was related to lower preparedness stress and higher perinatal infection stress. Our findings also corroborate previous studies, which emphasize the pivotal role of birth beliefs in birth decision making—beliefs that have been shown to precede fear of birth. 12 Choosing a community birth in the United States is an uncommon choice, yet anecdotal reports and preferences reported by our study participants indicate that the COVID‐19 pandemic could produce an increase in rates of births at home and in freestanding birth centers where these are legally permitted 25 and even where they are not permitted or advised. 24 On average, women who preferred a hospital birth were more concerned about perinatal infection. This is most likely related to underlying health anxiety dispositions associated with a stronger belief that birth is a medical process. 46 After controlling for other associated variables, however, it was evident that infection concerns were associated with a greater likelihood of preferring a community birth. When considering the multitude of factors that are associated with women's preference, having high levels of infection stress is associated with greater probability of preferring a community birth.
Overall, women who felt prepared for birth despite the pandemic (ie, low pandemic preparedness stress) had the highest probability of preferring a community birth, and their stress about infection did not affect this preference. Choosing a community birth is well aligned with midwifery modes of care, which emphasize women's autonomy during birth. 23 Relationships between mother and maternity care practitioner are often more egalitarian in midwifery models of care and, consequently, in community births, placing more control in women's hands; this level of responsibility may not be comfortable or preferable for all mothers. Choosing a community birth is an active decision that requires preparation, both mentally and physically, especially since pharmaceutical pain relief is not an option. 47 This choice also requires greater confidence related to feeling prepared. 17 , 18
Alternately, women who felt least prepared for birth (ie, high pandemic preparedness stress) were least likely to prefer a community birth, but this association was tempered among those who were also greatly concerned about infection. Women likely balance risks when choosing their place of birth, and the scales may be tilted during the COVID‐19 pandemic, such that fears of infection in a hospital setting outweigh concerns about being unprepared. 9 , 20 , 48
To our knowledge, this study is the first to quantitatively investigate psychological factors related to place of birth preferences during the COVID‐19 pandemic. Despite its strengths, including a large sample and assessment of validated psychological constructs related to birth choices, it has several limitations. First, women of color are underrepresented—a population that has less access to high‐quality maternity care, both before and during the COVID‐19 pandemic. 49 Future studies should engage more relationship‐based approaches that specifically target and engage a more representative sample of persons giving birth in the United States. We recognize that the same institutionalized racism that drives poor maternity care outcomes in the United States also restricts access to choice of birth setting and practitioner type for many indigenous people and people of color in the United States. 50 In order to be able to study diverse birth experiences and preferences among marginalized groups, these individuals would need to have access to such rights and opportunities. Second, the study relied on online recruitment and self‐reported data (which could reflect recall bias and misperceptions) which further limits the generalizability of findings. Finally, although preferences for community births are four times higher in this study (8.3%) than national rates of these births before the pandemic (2%), 2 the overall percentage of women preferring out‐of‐hospital birth remains small.
The COVID‐19 pandemic has introduced a great deal of uncertainty into the lives of childbearing people, including whether they can protect themselves and their infants from the virus and the extent to which they can choose who will be present and what happens when they give birth. 27 Community births are a safe, less‐expensive birth option for low‐risk pregnancies that may offer a means to improve birth outcomes for many United States families and especially those from marginalized populations who experience disproportionate rates of poor birth outcomes. 10 In contrast to previous data, our findings suggest that community birth preference is associated with below‐average financial status (univariate analyses). It is possible that pandemic‐related economic strains are steering women away from hospitals because of concerns about out‐of‐pocket costs. Legislation and health policy aimed to make community births more accessible to all, 51 , 52 providing evidence‐based information about birth to women, and helping pregnant people feel more prepared for birth might help promote a shift in birth practices with potential to reduce the elevated and persistent rates of adverse maternal and infant outcomes that differentiate the United States from many other nations. In a separate study of individuals in this cohort, we found that those who experienced more stress associated with feeling unprepared for birth were more likely to have an unplanned operative birth. 53 The pandemic has radically affected maternity care and may result in substantial changes in women's preparation and their perceptions about how and where they wish to give birth. Providing a wider range of options to women for a safe and fulfilling birth experience, especially in states where various birth options are limited, may be one of the long‐lasting silver linings of the current pandemic. 54
ETHICAL APPROVAL
The study was approved on April 21, 2020, by the Institutional Review Board of Stony Brook University (IRB2020‐00227).
ACKNOWLEDGMENTS
We would like to thank all the study participants for their time and their willingness to share their experiences from being pregnant during the COVID‐19 pandemic. We would like to thank the research assistants who helped in carrying out this project: Emily Rehbein, Donna Wilcox, Ilka St. Denis, Francine Chirico, Lucero Molina and Katya Potkin.
Preis H, Mahaffey B, Lobel M. The role of pandemic‐related pregnancy stress in preference for community birth during the beginning of the COVID‐19 pandemic in the United States. Birth. 2021;48:242–250. 10.1111/birt.12533
Funding information
Funding for this study was provided by a Stony Brook University Office of the Vice President for Research and Institute for Engineering‐Driven Medicine COVID‐19 Seed Grant. Heid Preis revieved support from NIH Grant R21DA049827 during preperation of this article. Brittain Mahaffey received support from NIH Grant K23HD092888 during preparation of this article.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Cheyney M, Bovbjerg ML, Leeman L, Vedam S. community versus out‐of‐hospital birth: what's in a name? J Midwifery Womens Health. 2019;64(1):9‐11. [DOI] [PubMed] [Google Scholar]
- 2. MacDorman MF, Declercq E. Trends and state variations in out‐of‐hospital births in the United States, 2004–2017. Birth. 2019;46:279‐288. 10.1111/birt.12411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Snowden JM, Tilden EL, Snyder J, Quigley B, Caughey AB, Cheng YW. Planned out‐of‐hospital birth and birth outcomes. N Engl J Med. 2015;373:2642‐2653. 10.1056/nejmsa1501738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. de Jonge A, Mesman JAJM, Manniën J, Zwart JJ, van Dillen J, van Roosmalen J. Severe adverse maternal outcomes among low risk women with planned home versus hospital births in the Netherlands: nationwide cohort study. BMJ. 2013;346:f3263. 10.1136/bmj.f3263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Scarf VL, Rossiter C, Vedam S, et al. Maternal and perinatal outcomes by planned place of birth among women with low‐risk pregnancies in high‐income countries: a systematic review and meta‐analysis. Midwifery. 2018;62:240‐255. 10.1016/j.midw.2018.03.024 [DOI] [PubMed] [Google Scholar]
- 6. Alliman J, Phillippi JC. Maternal outcomes in birth centers: an integrative review of the literature. J Midwifery Womens Health. 2016;61:21‐51. 10.1111/jmwh.12356 [DOI] [PubMed] [Google Scholar]
- 7. Hitzert M, Hermus MAA, Scheerhagen M, et al. Experiences of women who planned birth in a birth centre compared to alternative planned places of birth. results of the Dutch birth centre study. Midwifery. 2016;40:70‐78. 10.1016/j.midw.2016.06.004 [DOI] [PubMed] [Google Scholar]
- 8. Attanasio LB, Alarid‐Escudero F, Kozhimannil KB. Midwife‐led care and obstetrician‐led care for low‐risk pregnancies: a cost comparison. Birth. 2020;47(1):57‐66. 10.1111/birt.12464 [DOI] [PubMed] [Google Scholar]
- 9. Miller AC, Shriver TE. Women's childbirth preferences and practices in the United States. Soc Sci Med. 2012;75(4):709‐716. 10.1016/j.socscimed.2012.03.051 [DOI] [PubMed] [Google Scholar]
- 10. Alliman J, Stapleton SR, Wright J, Bauer K, Slider K, Jolles D. Strong start in birth centers: socio‐demographic characteristics, care processes, and outcomes for mothers and newborns. Birth. 2019;46:234‐243. 10.1111/birt.12433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sluijs A, Cleiren MPHD, van Lith JMM, Wijma B, Wijma K. Is fear of childbirth related to the woman’s preferred location for giving birth? A Dutch low‐risk cohort study. Birth. 2020;47:144‐152. 10.1111/birt.12456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Preis H, Gozlan M, Dan U, Benyamini Y. A quantitative investigation into women's basic beliefs about birth and planned birth choices. Midwifery. 2018;63:46‐51. 10.1016/j.midw.2018.05.002 [DOI] [PubMed] [Google Scholar]
- 13. Gibson E. Women, birth practitioners, and models of pregnancy and birth—Does consensus exist? Health Care Women Int. 2014;35:149‐174. 10.1080/07399332.2013.810219 [DOI] [PubMed] [Google Scholar]
- 14. Bryers HM, Van Teijlingen E. Risk, theory, social and medical models: A critical analysis of the concept of risk in maternity care. Midwifery. 2010;26:488‐496. 10.1016/j.midw.2010.07.003 [DOI] [PubMed] [Google Scholar]
- 15. Davis‐Floyed RE. Birth Models that Work. Berkeley, CA: Univ of California Press; 2009. [Google Scholar]
- 16. Preis H, Benyamini Y. The birth beliefs scale – a new measure to assess basic beliefs about birth. J Psychosom Obstet Gynecol. 2016;38:73‐80. 10.1080/0167482x.2016.1244180 [DOI] [PubMed] [Google Scholar]
- 17. Preis H, Eisner M, Chen R, Benyamini Y. First‐time mothers’ birth beliefs, preferences, and actual birth: a longitudinal observational study. Women Birth. 2019;32:e110‐e117. 10.1016/j.wombi.2018.04.019 [DOI] [PubMed] [Google Scholar]
- 18. Preis H, Mor P, Grisaru‐Granovsky S, et al. Women's preferences for mode of second birth—A prospective study of two Israeli birth cohorts. Birth. 2020;47:237‐245. 10.1111/birt.12484 [DOI] [PubMed] [Google Scholar]
- 19. Yilmaz FA, Ozan YD. Women's birth beliefs and associated factors in an obstetrics clinic in the Southeastern Anatolian region of turkey. J Health Res. 2020;34:345‐351. 10.1108/JHR-07-2019-0166 [DOI] [Google Scholar]
- 20. Chadwick RJ, Foster D. Negotiating risky bodies: childbirth and constructions of risk. Health Risk Soc. 2014;16:68‐83. 10.1080/13698575.2013.863852 [DOI] [Google Scholar]
- 21. Wood RJ, Mignone J, Heaman MI, Robinson KJ, Roger KS. Choosing an out‐of‐hospital birth centre: exploring women's decision‐making experiences. Midwifery. 2016;39:12‐19. 10.1016/j.midw.2016.04.003 [DOI] [PubMed] [Google Scholar]
- 22. Coxon K, Chisholm A, Malouf R, Rowe R, Hollowell J. What influences birth place preferences, choices and decision‐making amongst healthy women with straightforward pregnancies in the UK? A qualitative evidence synthesis using a ‘best fit’ framework approach. BMC Pregnancy Childbirth. 2017;17:103. 10.1186/s12884-017-1279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hadjigeorgiou E, Kouta C, Papastavrou E, Papadopoulos I, Martensson LB. Women's perceptions of their right to choose the place of childbirth: an integrative review. Midwifery. 2012;28:380‐390. 10.1016/j.midw.2011.05.006 [DOI] [PubMed] [Google Scholar]
- 24. Ecker JL, Minkoff HL. Laboring alone? brief thoughts on ethics and practical answers during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM. 2019;2020:100141. 10.1016/j.ajogmf.2020.100141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Davis‐Floyd R, Gutschow K, Schwartz DA. Pregnancy, birth and the COVID‐19 pandemic in the United States. Med Anthropol. 2020;1–15: 10.1080/01459740.2020.1761804 [DOI] [PubMed] [Google Scholar]
- 26. Renfrew MJ, Cheyne H, Craig J, et al. Sustaining quality midwifery care in a pandemic and beyond. Midwifery. 2020;88:102759. 10.1016/j.midw.2020.102759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dethier D, Abernathy A. Maintaining certainty in the most uncertain of times. Birth. 2020;47:257‐258. 10.1111/birt.12496 [DOI] [PubMed] [Google Scholar]
- 28. Illinois midwives face surge of interest in home birth during coronavirus pandemic. Chicago Tribune. April 22, 2020. https://www.chicagotribune.com/coronavirus/ct‐coronavirus‐midwives‐pregnancy‐home‐birth‐20200422‐bi3wxbdgufgdhjlhv6bj2rgk6i‐story.html. Accessed August 11, 2020 [Google Scholar]
- 29. de Freytas‐Tamura K. Pregnant and scared of ‘Covid hospitals’, they’re giving birth at home. NY Times. April 21, 2020. https://www.nytimes.com/2020/04/21/nyregion/coronavirus‐home‐births.html?smid. Accessed May 12 2020 [Google Scholar]
- 30. Ibrahim SM, Lobel M. Conceptualization, measurement, and effects of pregnancy‐specific stress: review of research using the original and revised prenatal distress questionnaire. J Behav Med. 2020;43:16‐33. [DOI] [PubMed] [Google Scholar]
- 31. Preis H, Mahaffey B, Heiselman C, Lobel M. Pandemic‐related pregnancy stress and anxiety among women pregnant during the COVID‐19 pandemic. Am J Obstet Gynecol MFM. 2020;2:100155. 10.1016/j.ajogmf.2020.100155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Preis H, Mahaffey B, Lobel M. Psychometric properties of the pandemic‐related pregnancy stress scale (PREPS). J Psychosom Obstet Gynecol. 2020;41:191‐197. 10.1080/0167482X.2020.1801625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Haines HM, Pallant JF, Karlstrom A, Hildingsson I. Cross‐cultural comparison of levels of childbirth‐related fear in an Australian and Swedish sample. Midwifery. 2011;27:560‐567. 10.1016/j.midw.2010.05.004 [DOI] [PubMed] [Google Scholar]
- 34. Schaal NK, La Marca‐Ghaemmaghami P, Preis H, Mahaffey B, Lobel M, Castro RA. The German version of the pandemic‐related pregnancy stress scale: a validation study. Eur J Obstet Gynecol Reprod Biol. 2020;256:40‐45. 10.1016/j.ejogrb.2020.10.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yirmiya K, Yakirevich‐Amir N, Preis H, Atzil S, Reuveni I Women’s Mental Health During the COVID‐19 Pandemic: The Role of Pregnancy. Unpublished data. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ilska M, Kołodziej‐Zaleska A, Brandt‐Salmeri A, Preis H, Lobel M Pandemic‐Related Pregnancy Stress Assessment – Psychometric Properties of the Polish PREPS and its Relationship with Childbirth Fear. Unpublished data. [DOI] [PubMed] [Google Scholar]
- 37. IBM Corp . IBM SPSS statistics for windows, version 24.0. 2016. [Google Scholar]
- 38. Hayes AF. A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. [White paper] 40. http://www.afhayes.com/public/process2012.pdf. Access date August, 2020. [Google Scholar]
- 39. Possamai‐Inesedy A. Confining risk: choice and responsibility in childbirth in a risk society. Health Soc Rev. 2006;15:406‐414. 10.5172/hesr.2006.15.4.406 [DOI] [Google Scholar]
- 40. Coxon K, Sandall J, Fulop NJ. To what extent are women free to choose where to give birth? How discourses of risk, blame and responsibility influence birth place decisions. Health Risk Soc. 2014;16:51‐67. 10.1080/13698575.2013.859231 [DOI] [Google Scholar]
- 41. Petrovska K, Watts N, Sheehan A, Bisits A, Homer C. How do social discourses of risk impact on women's choices for vaginal breech birth? A qualitative study of women's experiences. Health, Risk Soc. 2017;19:19‐37. 10.1080/13698575.2016.1256378 [DOI] [Google Scholar]
- 42. Luce A, Cash M, Hundley V, Cheyne H, Van Teijlingen E, Angell C. “Is it realistic?” the portrayal of pregnancy and childbirth in the media. BMC Pregnancy Childbirth. 2016;16:40. 10.1186/s12884-016-0827-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Morris T, McInerney K. Media representations of pregnancy and childbirth: an analysis of reality television programs in the United States. Birth. 2010;37(2):134‐140. 10.1111/j.1523-536X.2010.00393.x [DOI] [PubMed] [Google Scholar]
- 44. Fleming SE, Vandermause R, Shaw M. First‐time mothers preparing for birthing in an electronic world: internet and mobile phone technology. J Reprod Infant Psychol. 2014;32:240‐253. 10.1080/02646838.2014.886104 [DOI] [Google Scholar]
- 45. De Benedictis S, Johnson C, Roberts J, Spiby H. Quantitative insights into televised birth: a content analysis of one born every minute. Crit Stud Media Commun. 2019;36:1‐17. 10.1080/15295036.2018.1516046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Preis H, Chen R, Eisner M, et al. Testing a biopsychosocial model of the basic birth beliefs. Birth. 2018;45:79‐87. 10.1111/birt.12313 [DOI] [PubMed] [Google Scholar]
- 47. van Haaren‐Ten H, Tamar M, Hendrix MJ, Nieuwenhuijze MJ, deVries RG, Nijhuis JG. Birth place preferences and women’s expectations and experiences regarding duration and pain of labor. J Psychosom Obstet Gynecol. 2018;39:19‐28. 10.1080/0167482X.2017.1285900 [DOI] [PubMed] [Google Scholar]
- 48. Fage‐Butler AM. Risk resistance: constructing home birth as morally responsible on an online discussion group. Health Risk Soc. 2017;19:130‐144. 10.1080/13698575.2017.1327038 [DOI] [Google Scholar]
- 49. Onwuzurike C, Meadows A, Nour N. Examining inequities associated with changes in obstetric and gynecologic care delivery during the coronavirus disease 2019 (COVID‐19) pandemic. Obstet Gynecol. 2020;136:37‐41. 10.1097/AOG.0000000000003933 [DOI] [PubMed] [Google Scholar]
- 50. National Academies of Sciences, Engineering, and Medicine . Birth Settings in America: Outcomes, Quality, Access, and Choice. Washington, DC: National Academies Press: 2020. [PubMed] [Google Scholar]
- 51. Jolles DR, Stapleton SR, Alliman J. Strong start for mothers and newborns: moving birth centers to scale in the United States. Birth. 2019;46:207‐210. 10.1111/birt.12430 [DOI] [PubMed] [Google Scholar]
- 52. New York State COVID‐19 Maternity Task Force . Recommendations to the governor to promote increased choice and access to safe maternity care during the COVID‐19 pandemic. 2020. https://www.governor.ny.gov/sites/governor.ny.gov/files/atoms/files/042920_CMTF_Recommendations.pdf. Access August, 2020. [Google Scholar]
- 53. Preis H, Mahaffey B, Pati S, Heiselman C, Lobel M. Adverse perinatal outcomes predicted by prenatal maternal stress among U.S. women at the COVID‐19 pandemic onset. Ann Behav Med. 2021;266:113348. 10.1093/abm/kaab005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Profit J, Edmonds BT, Shah N, Cheyney M. The COVID‐19 pandemic as a catalyst for more integrated maternity care. Am J Public Health. 2020;110:1663‐1665. 10.2105/AJPH.2020.305935 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


