Summary
Physician burnout and poor mental health are prevalent and often stigmatised. Anaesthetists may be at particular risk and this is further increased for women anaesthetists due to biases and inequities within the specialty. However, gender‐related risk factors for and experiences of burnout and poor mental health remain under‐researched and under‐reported. This negatively impacts individual practitioners, the anaesthesia workforce and patients and carries significant financial implications. We discuss the impact of anaesthesia and gender on burnout and mental health using the COVID‐19 pandemic as an example illustrating how women and men differentially experience stressors and burnout. COVID‐19 has further accentuated the gendered effects of burnout and poor mental health on anaesthetists and brought further urgency to the need to address these issues. While both personal and organisational factors contribute to burnout and poor mental health, organisational changes that recognise and acknowledge inequities are pivotal to bolster physician mental health.
Keywords: anaesthesia, burnout, COVID‐19, gender, gender equity, mental health, women
Introduction
Physician burnout and poor mental health are prevalent [1, 2, 3, 4], with specific aspects of the role of the anaesthetist placing individuals at particular risk [5]. While data on gender are conflicting [4, 6], there are particular gendered risk factors contributing to burnout and poor mental health [7]. Although these are under‐researched and under‐reported, they likely interact with additional risk factors associated with being a woman anaesthetist [8, 9]. The COVID‐19 pandemic has amplified inequities, to the detriment of women, such as disproportionate job and wage losses and disproportionate care‐giving responsibilities [10]. To date, little attention has been paid to the intersection of how COVID‐19 may contribute to disproportionate strains on physicians' mental health through amplification of pre‐existing inequities particularly affecting women within medicine. Insufficient exploration of this topic may have a substantial impact on the medical workforce now and in the coming years; thus, it is imperative we examine and address the impact of gender on the mental health of anaesthetists and specifically the additional influence of COVID‐19. This paper aims to highlight some of the ways in which women anaesthetists may differentially experience stressors and, by extension, burnout, with COVID‐19 illustrating an extreme version of these effects. This paper not only highlights issues that need to be considered by our colleagues, leaders and policy creators to assist in providing support to one another now, but also in the aftermath of the pandemic and in the longer term to protect the mental health of our healthcare workers.
We take the opportunity to discuss sex and gender as constructs. Although sex and gender remain active topics of discussion with differing opinions and theories, sex can be defined as biological differences between male and female (e.g. chromosomal complement, hormonal differences); sex‐related terminology consists of male and female. Gender is a social construct that is rooted in history, politics, and culture; gender‐related terminology consists of man and woman. Gender binaries are typically discussed (i.e. man and woman). However, according to post‐structuralism, the binary opposition (i.e. man and woman) does not hold when discussing, for example, people who identify as non‐binary, as gender fluid. As we are depicting a gendered phenomenon, not a sex‐related phenomenon, we prefer to employ gender and gender‐related terminology. Furthermore, it is universally accepted that literature using sex‐related terminology be cited with such terms as male and female and that literature using gender‐related terminology be cited with such terms as man and woman.
Burnout and poor mental health in medicine and anaesthetics
Physicians face enormous pressures and challenges on a daily basis: they are expected to be excellent clinicians; researchers; educators; administrators; and colleagues, all the while experiencing external pressures to be academically productive. The stress experienced is both significant and chronic and when combined with other organisational and personal stressors, may contribute to burnout: a psychological state characterised by high levels of depersonalisation, emotional exhaustion and low levels of personal accomplishment [11, 12]. Burnout primarily results from repeated and prolonged exposure to work‐related stressors including: work overload; lack of job control; lack of autonomy and time pressures [13], although psychosocial risk factors such as personality characteristics, low job social support and work–home conflict have also been identified [1, 8, 14]. Psychosocial effects of burnout include: absenteeism; disengagement; seclusion; and strained relationships within the home and work environment.
Physician burnout has been the focus of increasing research and the topic of much discussion given the detrimental impact it can have on both physician and patient well‐being. Reported prevalence rates of physician burnout vary substantially across studies, due in large part to the lack of a single agreed‐on measurement tool and associated criteria. For example, a systematic review on physician burnout prevalence noted 142 unique definitions for burnout in 182 studies [2]. This problem underlies a major issue in the field, namely, varied conceptualisation and operationalisation of burnout. Is it truly a distinct phenomenon from depression and/or exhaustion? Should it still be considered as arising only as a result of human relations‐induced stress [2, 3]? Nevertheless, burnout and mental health issues affect between 30 and 60% of physicians and trainees [1, 2, 3, 4], with highest rates of burnout seen in specialising trainees [1]. Reviews of the literature have found that work‐related characteristics such as long hours and excessive workloads are key causes of burnout in physicians, due in large part to strained work–personal life balance [1, 4]. Notably, however, burnout rates in physicians remain higher than in other professions even after adjusting for other factors such as work hours [4]. Burnout in physicians is associated with negative consequences for physicians, patients and the healthcare system overall. Physician burnout is linked with: poorer mental and physical health in physicians; problems in personal life; decreased job satisfaction; increased medical errors and patient safety risks; worse quality of patient care; and lower patient satisfaction [1, 4, 15]. Burnout is also associated with: reduced work hours and number of patients seen; increased sick leave; intent to leave medicine or change jobs; and early retirement [1, 16]. These have significant financial implications on healthcare systems, for example, they have been estimated to cost over $213 million in Canada alone (£123 million; €137 million) [16].
Rates of burnout symptoms differ across medical specialties with up to three‐fold increased odds in acute care physicians such as emergency medicine, general internal medicine and neurology [4]. However, data are conflicting on whether burnout rates in anaesthetists follow this pattern [5]. Anaesthetists' peri‐operative work requires constant vigilance, relative isolation and remaining well‐informed on emerging and evolving technologies, anaesthetic techniques and work environments. This is all while working with increasingly complex patients, where decisions and actions have potentially profound implications [17]. These features of clinical work point to the possibility that manifestations of burnout, such as fatigue and impaired cognitive function, may result in a heightened risk of patient harm. Indeed, several research studies illustrate that fatigue is a highly pervasive and problematic issue among anaesthetists and anaesthetic trainees with significant negative impacts on physical health, well‐being and personal relationships [18, 19]. Preliminary evidence suggests that fatigue‐reducing strategies such as a reduced on‐call model may improve anaesthetic trainee well‐being and reduce the risk of burnout [20]. As anaesthetists, we must refute the notion that fatigue is an acceptable sacrifice. It is imperative that anaesthetists continue to advance a culture that ensures education about fatigue, reasonable workloads, regular rest breaks and rest facilities are de facto provided and accessible.
Gender contributes to the risk for and experience of burnout in anaesthetists
Much has been written on the relationship between gender and physician burnout. Although gender is associated with burnout in some studies [6], others suggest that after controlling for age and other variables, gender may not be a consistent risk factor [4]. The conflicting findings in burnout prevalence according to sex likely arise from substantial between‐study differences in burnout assessment tools, as well as study populations [2, 5]. Moreover, these distract from the more useful question of whether the experiences of and contributors to burnout differ by physician gender. For example, a UK study of anaesthetists reported elevated work‐related fatigue in women respondents across all age categories [18]. There are well‐known sex‐ and gender‐related differences in stress responses [21, 22] and vulnerability to stress‐related mental health disorders [23, 24, 25] as well as differences in symptomatic expression of the same mental health problem [15, 26]. Similar findings are reported in the burnout literature with some studies reporting that women's experiences of burnout are linked with emotional exhaustion, whereas men's experiences are linked with depersonalisation [27, 28]. In some cases, higher rates of burnout in anaesthetists who are men appear to result from significantly higher levels of depersonalisation [29, 30]. Of additional interest, one study of Norwegian physicians found not only higher exhaustion levels in women and higher disengagement levels among men, but also gender differences in predictors of burnout with work–home conflicts predominating in women and workload the strongest predictor in men [7].
Gender bias and gender‐related inequities are significant stressors, to which medicine, and anaesthesia in particular, is not immune. Women physicians report inequities in opportunity, recognition and credibility [8] that may impact their work, working relationships and mental health. There are fewer women in leadership positions within anaesthesia compared with men [31, 32], resulting in less gender‐concordant allyship opportunities and gender‐concordant mentorship, which has been identified as particularly important for anaesthesia trainees [33]. It is unclear whether the gender gap in leadership arises from differences in a desire to pursue a leadership career [9, 34] or from the numerous systemic barriers that prevent women from attaining leadership roles, as women anaesthetists report a greater frequency of barriers to career promotion than their counterparts who are men [34, 35]. There are also substantial gender inequities in professional and academic opportunities in anaesthesia. Reports reveal that women receive fewer grants, awards and are under‐represented as speakers at conferences [36]; they are also assigned lower academic rank and pay [37, 38].
Furthermore, gender discrimination is experienced significantly more frequently by women anaesthetists compared with men during training [39, 40] and throughout their careers, with one survey revealing that women anaesthetists report experiencing the highest rate of maternal discrimination in the workplace of all medical specialties [41]. In addition to this, large‐scale studies report very high levels of gender‐based mistreatment in anaesthesia. Particularly alarming is the finding from an international survey of over 11,000 anaesthetists from 148 countries, which showed that women anaesthetists are 10 times more likely to report being mistreated in the workplace compared with men [9]. Likewise, a study of over 27,000 medical students in the USA found women students were significantly more likely to report mistreatment compared with men students, with over 40% of women students reporting at least one episode of mistreatment [40]. These inequities undoubtedly contribute to feelings of frustration and mistrust of colleagues and leadership among women anaesthetists [39]. These various forms of bias, mistreatment and discrimination may significantly impact patient safety and, for trainees, their performance evaluations. In a randomised experiment, anaesthesia trainees who were exposed to incivility in a simulated operating room crisis, involving a rude environment, showed worse technical and non‐technical performance in areas including vigilance, diagnosis, communication and patient management [42].
It is crucial at this time to also acknowledge that vigilance in detecting and addressing the mental health needs of anaesthetists and healthcare workers more generally must include attention to disparities experienced across multiple axes and social locations, for example: gender; race; ability; and sexual orientation. Furthermore, research and policies should extend gender binaries (women or men) to be inclusive of anyone who does not identify with the woman–man gender binary or who does not take on ‘traditional’ social gender roles [43]. Anaesthetists from around the world report experiencing bias as a result of being foreign‐born and/or of the region's non‐dominant race, as well as bias related to religion or caste [9]. Recent studies also report significantly elevated frequencies of mistreatment and discrimination in anaesthetic trainees who are non‐White and not heterosexual [40], as well as compounded gender bias for women anaesthetic trainees from an ethnic minority background. More research in this area is clearly needed, particularly as the anaesthetist workforce composition shifts towards the inclusion and broader representation of Black, indigenous and people of colour as well as all socially marginalised people. Historically, research examining gender differences did not include members of these groups due to the lack of representation in the field [44]. For example, in a study examining gender differences in anaesthetists' annual incomes, the number of Black respondents was so small that the researchers had to limit their analyses to White respondents only [44].
Gender and burnout in anaesthesia during COVID‐19
Globally, the COVID‐19 pandemic has posed challenges to both health systems and humanity. The efforts and scholarly work recognising and offering potential solutions to healthcare workers' mental health challenges during the COVID‐19 pandemic that result from a unique combination of factors including, but not limited to: high rates of COVID‐19 exposure and infection; constantly changing protocols and procedures; long work hours; and insufficient resources including personal protective equipment, which altogether contribute to unprecedented levels of emotional distress [45, 46, 47, 48], should be applauded.
From the pandemic's inception, anaesthetists have played and continue to play a vital role as frontline physicians. Anaesthetists and the range of services they offer are in high demand, which has translated to longer working hours in high‐risk environments such as increased participation in aerosol‐generating medical procedures. These conditions, paired with the general uncertainty regarding long‐term availability of scarce resources needed to care for themselves (such as personal protective equipment) and their patients (e.g. ventilators or medication), compound the stress experienced and are likely to increase the risk of burnout among anaesthetists. Previous work shows that the risk of burnout among anaesthetists’ increases significantly with longer number of hours worked and increased workload [5], but this risk decreases with proper supervision and/or job support [5] as well as higher perceived workplace resource availability [49]. This points to the pivotal role of organisational factors in supporting anaesthetists' mental health during the ongoing COVID‐19 pandemic. Additionally, support from family and the maintenance of a healthy work–life balance, both of which are protective factors against burnout in anaesthetists [4, 49], have been disrupted for most during the current pandemic, further increasing the potential for developing burnout. Altogether, this amounts to the critical realisation that anaesthetists working during the COVID‐19 pandemic may be at an increased risk of burnout and other stress‐related mental health issues.
Organisations and individuals must be cognisant of potential differences in contributors, experiences and consequences of COVID‐19‐related burnout. For example, gender differences may be observed in the frequency and/or manifestations of anxieties related to COVID‐19 infection. At least one study has found women healthcare workers involved in tracheal intubation of patients with suspected or confirmed COVID‐19 were at increased risk of subsequent COVID‐19 diagnosis or symptoms requiring self‐isolation or hospitalisation [50], with speculation that this may be related to gendered designs of personal protective equipment [51]. The COVID‐19 pandemic may also bring about anxieties about protecting oneself and one's family. Similarly, anaesthetists' workload is increased due to COVID‐19 as hospitals attempt to ‘make up for lost time’ for elective or non‐emergency surgeries that were delayed, potentially increasing the risk for burnout in all anaesthetists [7].
In drawing attention to the gender inequity among anaesthetists during COVID‐19, we must also address the role that structural racism plays in workplace discrimination and access to opportunities, such as promotions and leadership roles. Currently, women anaesthetists of varying racial and ethnic backgrounds might be experiencing heightened forms of burnout given the racial climate following the death of George Floyd in the USA. Women anaesthetists who identify as Black, indigenous or people of colour may carry additional stress related to the multiple forms of racial discrimination and/or microaggressions experienced on a daily basis within the workplace [52, 53]. Repeated and prolonged exposure to these stressors contributes to the onset of burnout or similar mental health issues as well as worse physical health and job performance [54].
Emerging research on the intersections of gender, mental health and COVID‐19 suggests that healthcare workers who identify as women are more likely to experience mental health symptoms during the pandemic [4]. In a cross‐sectional survey in China of over 1200 healthcare workers in 34 hospitals treating patients exposed to COVID‐19, of whom 77% were women and 61% were nurses, women reported more symptoms of depression and anxiety, more distress and more severe insomnia [23]. Similarly, controlling for confounders, being a woman was associated with severe symptoms of depression, anxiety and distress [23]. There may also be ill effects on healthcare workers' mental health in the longer term, as was observed up to one year following the SARS outbreak [55], with women at potentially greater risk given the numerous gender differences in the development and maintenance of post‐traumatic stress disorder [56]. Indeed, one recent study found that women were more likely to report post‐traumatic stress symptoms of re‐experiencing negative alterations in cognition and mood and hyper‐rousability one month after the COVID‐19 outbreak in Wuhan, China [57].
These findings are further exacerbated when analysed in the context of limited social support or experiences of gender‐based violence. Social isolation and loneliness are strongly associated with symptoms of depression and anxiety, whereas strong social networks and social relationships are negatively associated with depression, anxiety and suicide [58]. This appears to hold true during the current pandemic as at least one small cross‐sectional study of 180 medical staff treating patients with COVID‐19 found social support was negatively associated with anxiety and stress levels and positively associated with self‐efficacy and sleep quality [59]. Thus, gender differences in perceived social support, types of social support, social networks and willingness to seek out social support may moderate the relationship between COVID‐19‐related stress and poor mental health. Globally, approximately 243 million women have experienced physical and/or sexual abuse by an intimate partner or a perpetrator [10]. In Australia, 40% of healthcare workers have had victims of domestic violence request help from them [10]. Violence against women tends to increase during emergencies [10]. Staying at home during the current pandemic has increased the likelihood of gender‐based violence and domestic abuse [45]. The United Nations reported a ‘horrifying global surge’ [60] in domestic violence linked to the imposed quarantine. Although data are scarce, one Australian study shows that nearly half of healthcare workers who are women have experienced domestic abuse, highlighting the need to be aware of and attentive to signs of domestic abuse within our colleagues [61] as gender‐based violence can occur in all women irrespective of social or economic circumstances.
Burnout is more likely to occur when physicians do not perceive adequate and/or appropriate support from managers, supervisors and healthcare organisations [5]. Moving forward, during and following the COVID‐19 pandemic, it is imperative that anaesthesia departmental and organisational leadership create and implement strategies that support a culture of self‐care and organisational justice [48], demonstrating their ongoing commitment to engage and support physicians. This includes acknowledgment that existing gender and other social disparities within anaesthesia are heightened given the public health‐related restrictions and closures, and amplifications of work and home duties. To ensure proper support for all anaesthetists, feedback regarding work hours, resources, opportunities and other pertinent work‐related issues should be actively sought in a safe and open environment to ensure all voices are heard and attended to.
As anaesthetists, we work in dynamic multidisciplinary settings with the same collective group over years; working in such close proximity with trainees, nurses, surgeons and fellow anaesthetists, we become familiar with our colleagues' personalities and develop friendships. We are thus in a privileged position to be able to detect first clues in changes in colleagues' mental health, thereby providing us the opportunity to offer support or suggest resources to others who are experiencing burnout, mental health issues or intimate‐partner violence (see Fig. 1). Given the negative physical and psychosocial impacts of burnout, it is important for anaesthetists to remain vigilant and attentive to their own needs while also remaining open and receptive to the needs of others.
Figure 1.
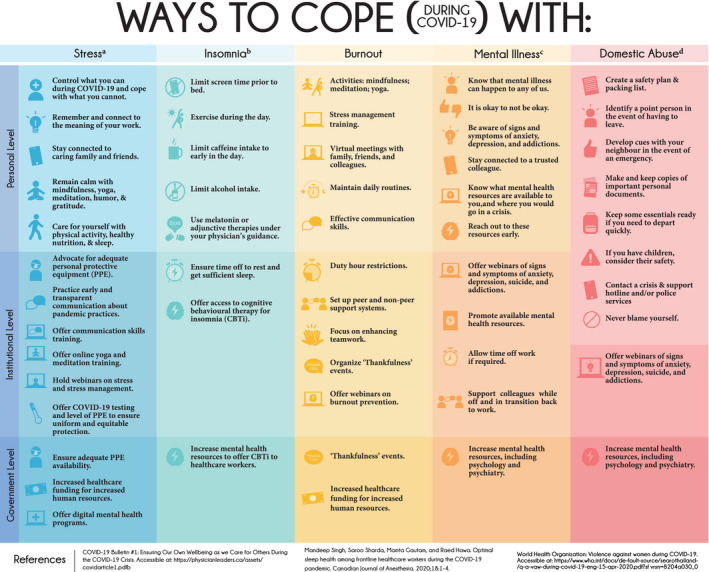
A non‐exhaustive list of steps that can be implemented to mitigate burnout and stress‐related COVID‐19 issues at all levels.
Studies on gender differences in coping style and in the use of mental health services show that women are more likely to reach out for help and do so earlier than men [62]. Despite this, we cannot count on these trends being applicable to all anaesthetists, all women, or women who work in healthcare. In fact, studies show that people from socially marginalised racial and ethnic backgrounds are less likely to seek mental health support, not necessarily due to stigma, but more so due to the view that the current mental health systems and services in place cause harm to people who identify as Black, indigenous or people of colour [63]. While there have been worldwide efforts to reduce the negative attitudes and beliefs associated with mental illness, the stigma in healthcare settings remains high and likely contributes to a lack of help‐seeking behaviour [64]. Pre‐existing biased and tenacious representations of men as ‘agentic’ and women as ‘communal’ that have repeatedly been demonstrated to occur in healthcare settings, as well as in anaesthesia [35], may also contribute to gender differences in both stress‐related coping styles and help‐seeking behaviours. Men may be less likely to report burnout as social expectations dictate ‘toughness’; on the other hand, women may be reluctant to report burnout so as to not confirm gendered preconceptions of women as ‘weak’ or vulnerable. Thus, it is even more imperative that healthcare leaders ensure there are accessible programmes in place to allow for informal sharing and debriefing of experiences, implementation of peer support and offering counselling and psychiatric assistance if required, all the while dismantling these socialised gender roles. However, equally important is ensuring that these programmes are tailored to the needs of all anaesthetists and healthcare workers, including features proven beneficial to men, women, gender non‐binary and people from various racial and cultural backgrounds [43].
We conclude by encouraging anaesthetists and all healthcare workers to stand true to the value of solidarity by looking out for each other and creating a safe, equitable and caring environment for all. Although we may not be able to single‐handedly address all the pre‐existing gender differences and inequities intensified during the current pandemic, we can certainly do our part by being mindful and cognisant of people's lived realities and the multiple intersecting burdens they may experience; we can strive to treat each other, and ourselves, with understanding, kindness and compassion.
Acknowledgements
The authors would like to thank V. Robinson and R. Brewster at COVID Creatives for producing Fig. 1. GL would like to thank the Department of Anesthesia and Pain Medicine at the University Health Network‐Sinai Health System for the protected academic time. Unrelated to this work, MG is Chief Executive Officer of PEAK MD Inc., through which she receives fees for academic grand rounds, conference keynote presentations, medical leadership development, healthcare consulting and coaching physician leaders. No other competing interests declared.
Contributor Information
G. R. Lorello, Email: gianni.lorello@uhn.ca, @GianniLorelll.
M. Gautam, @PEAKMD.
References
- 1. Mihailescu M, Neiterman E. A scoping review of the literature on the current mental health status of physicians and physicians‐in‐training in North America. BMC Public Health 2019; 19: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. Journal of the American Medical Association 2018; 320: 1131–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schaufeli WB, Taris TW, Van Rhenen W. Workaholism, burnout, and work engagement: three of a kind or three different kinds of employee well‐being? Applied Psychology 2008; 57: 173–203. [Google Scholar]
- 4. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. Journal of Internal Medicine 2018; 283: 516–29. [DOI] [PubMed] [Google Scholar]
- 5. Sanfilippo F, Noto A, Foresta G, et al. Incidence and factors associated with burnout in anesthesiology: a systematic review. BioMed Research International 2017; 4: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Amoafo E, Hanbali N, Patel A. What are the significant factors associated with burnout in doctors? Occupational Medicine 2015; 65: 117–21. [DOI] [PubMed] [Google Scholar]
- 7. Langballe EM, Innstrand ST, Aasland OG, Falkum E. The predictive value of individual factors, work‐related factors, and work–home interaction on burnout in female and male physicians: a longitudinal study. Stress and Health 2011; 27: 73–87. [Google Scholar]
- 8. Sibeoni J, Bellon‐Champel L, Mousty A, Manolios E, Verneuil L, Revah‐Levy A. Physicians' perspectives about burnout: a systematic review and metasynthesis. Journal of General Internal Medicine 2019; 34: 1578–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zdravkovic M, Osinova D, Brull SJ, et al. Perceptions of gender equity in departmental leadership, research opportunities, and clinical work attitudes: an international survey of 11 781 anaesthesiologists. British Journal of Anaesthesia 2020; 124: e160–e170. [DOI] [PubMed] [Google Scholar]
- 10. United Nations . Policy Brief: The Impact of COVID‐19 on Women. 2020. https://reliefweb.int/report/world/policy‐brief‐impact‐covid‐19‐women (accessed 06/01/20).
- 11. Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry 2016; 15: 103–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schaufeli WB, Leiter MP, Maslach C. Burnout: 35 years of research and practice. Career Development International 2009; 14: 204–20. [Google Scholar]
- 13. Escribà‐Agüir V, Martín‐Baena D, Pérez‐Hoyos S. Psychosocial work environment and burnout among emergency medical and nursing staff. International Archives of Occupational and Environmental Health 2006; 80: 127–33. [DOI] [PubMed] [Google Scholar]
- 14. Taku K. Relationships among perceived psychological growth, resilience and burnout in physicians. Personality and Individual Differences 2014; 59: 120–3. [Google Scholar]
- 15. Panagioti M, Geraghty K, Johnson J, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta‐analysis. Journal of the American Medical Association Internal Medicine 2018; 178: 1317–31. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 16. Dewa CS, Jacobs P, Thanh NX, Loong D. An estimate of the cost of burnout on early retirement and reduction in clinical hours of practicing physicians in Canada. BMC Health Service Research 2014; 14: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kuhn CM, Flanagan EM. Self‐care as a professional imperative: physician burnout, depression, and suicide. Canadian Journal of Anesthesia 2017; 64: 158–68. [DOI] [PubMed] [Google Scholar]
- 18. McClelland L, Plunkett E, McCrossan R, et al. A national survey of out‐of‐hours working and fatigue in consultants in anaesthesia and paediatric intensive care in the UK and Ireland. Anaesthesia 2019; 74: 1509–23. [DOI] [PubMed] [Google Scholar]
- 19. McClelland L, Holland J, Lomas JP, Redfern N, Plunkett E. A national survey of the effects of fatigue on trainees in anaesthesia in the UK. Anaesthesia 2017; 72: 1069–77. [DOI] [PubMed] [Google Scholar]
- 20. Sussman D, Paul JE. The impact of transitioning from a 24‐hour to a 16‐hour call model amongst a cohort of Canadian anesthesia residents at McMaster University – a survey study. Advances in Medical Education and Practice 2015; 6: 501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brivio E, Lopez JP, Chen A. Sex differences: Transcriptional signatures of stress exposure in male and female brains. Genes, Brain and Behavior 2020; 19: 447. [DOI] [PubMed] [Google Scholar]
- 22. Dedovic K, Wadiwalla M. The role of sex and gender socialization in stress reactivity. Developmental Psychology 2009; 45: 45–55. [DOI] [PubMed] [Google Scholar]
- 23. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. Journal of the American Medical Association Network Open 2020; 3: e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research 2012; 21: 169–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Seedat S, Scott KM, Angermeyer MC, et al. Cross‐national associations between gender and mental disorders in the World Health Organization world mental health surveys. Archives of General Psychiatry 2009; 66: 785–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Altemus M, Sarvaiya N, Neill EC. Sex differences in anxiety and depression clinical perspectives. Frontiers in Neuroendocrinology 2014; 35: 320–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Houkes I, Winants Y, Twellaar M, Verdonk P. Development of burnout over time and the causal order of the three dimensions of burnout among male and female GPs. A three‐wave panel study. BMC Public Health 2011; 11: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Purvanova RK, Muros JP. Gender differences in burnout: a meta‐analysis. Journal of Vocational Behavior 2010; 77: 168–85. [Google Scholar]
- 29. Ferguson C, Low G, Shiau G. Resident physician burnout: insights from a Canadian multispecialty survey. Postgraduate Medical Journal 2020; 96: 331–8. [DOI] [PubMed] [Google Scholar]
- 30. Hyman SA, Shotwell MS, Michaels DR, et al. A survey evaluating burnout, health status, depression, reported alcohol and substance use, and social support of anesthesiologists. Anesthesia and Analgesia 2017; 125: 2009–18. [DOI] [PubMed] [Google Scholar]
- 31. Lorello GR, Flexman AM. 75 years of leadership in the Canadian Anesthesiologists' Society: a gender analysis. Canadian Journal of Anesthesia 2019; 66: 843–4. [DOI] [PubMed] [Google Scholar]
- 32. Lorello GR, Parmar A, Flexman AM. Representation of women on the editorial board of the Canadian Journal of Anesthesia: a retrospective analysis from 1954 to 2018. Canadian Journal of Anesthesia 2019; 66: 989–90. [DOI] [PubMed] [Google Scholar]
- 33. Plyley T, Cory J, Lorello GR, Flexman AM. A survey of mentor gender preferences amongst anesthesiology residents at the University of British Columbia. Canadian Journal of Anesthesia 2018; 66: 342–3. [DOI] [PubMed] [Google Scholar]
- 34. Matot I, De Hert S, Cohen B, Koch T. Women anaesthesiologists' attitudes and reported barriers to career advancement in anaesthesia: a survey of the European Society of Anaesthesiology. British Journal of Anaesthesia 2020; 124: e171–e177. [DOI] [PubMed] [Google Scholar]
- 35. Lorello GR, Cil T, Flexman AM. Women anesthesiologists' journeys to academic leadership: a constructivist grounded theory‐inspired study. Canadian Journal of Anesthesia 2020; 67: 1130–9. [DOI] [PubMed] [Google Scholar]
- 36. Lorello GR, Parmar A, Flexman AM. Representation of women amongst speakers at the Canadian Anesthesiologists' Society annual meeting: a retrospective analysis from 2007 to 2019. Canadian Journal of Anesthesia 2019; 67: 430–6. [DOI] [PubMed] [Google Scholar]
- 37. Chandrabose RK, Pearson ACS. Organizing women in anesthesiology. International Anesthesiology Clinics 2018; 56: 21–43. [DOI] [PubMed] [Google Scholar]
- 38. Bosco L, Lorello GR, Flexman AM, Hastie MJ. Women in anaesthesia: a scoping review. British Journal of Anaesthesia 2020; 124: e134–e147. [DOI] [PubMed] [Google Scholar]
- 39. Pearce G, Sidhu N, Cavadino A, Shrivathsa A, Seglenieks R. Gender effects in anaesthesia training in Australia and New Zealand. British Journal of Anaesthesia 2020; 124: e70–e76. [DOI] [PubMed] [Google Scholar]
- 40. Hill KA, Samuels EA, Gross CP, et al. Assessment of the prevalence of medical student mistreatment by sex, race/ethnicity, and sexual orientation. Journal of the American Medical Association Internal Medicine 2020; 180: 653–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Adesoye T, Mangurian C, Choo EK, Girgis C, Sabry‐Elnaggar H, Linos E. Perceived discrimination experienced by physician mothers and desired workplace changes: a cross‐sectional survey. Journal of the American Medical Association Internal Medicine 2017; 177: 1033–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Katz D, Blasius K, Isaak R, et al. Exposure to incivility hinders clinical performance in a simulated operative crisis. British Medical Journal Quality and Safety 2019; 28: 750–7. [DOI] [PubMed] [Google Scholar]
- 43. Lorello GR, Kuper A, Soklaridis S, Schrewe B. How discourses of gender equity during COVID‐19 become exclusionary: lessons from parenthood. Journal of Evaluation in Clinical Practice 2021; 27: 9–11. [DOI] [PubMed] [Google Scholar]
- 44. Weeks WB, Wallace AE, Mackenzie TA. Gender differences in anesthesiologists' annual incomes. Anesthesiology 2007; 106: 806–11. [DOI] [PubMed] [Google Scholar]
- 45. Wu PE, Styra R, Gold WL. Mitigating the psychological effects of COVID‐19 on health care workers. Canadian Medical Association Journal 2020; 192: E459–E460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Adams JG, Walls RM. Supporting the health care workforce during the COVID‐19 global epidemic. Journal of the American Medical Association 2020; 323: 1439–40. [DOI] [PubMed] [Google Scholar]
- 47. Santarone K, McKenney M, Elkbuli A. Preserving mental health and resilience in frontline healthcare workers during COVID‐19. American Journal of Emergency Medicine 2020; 38: 1530–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Heath C, Sommerfield A, von Ungern‐Sternberg BS. Resilience strategies to manage psychological distress among healthcare workers during the COVID‐19 pandemic: a narrative review. Anaesthesia 2020; 75: 1364–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sun H, Warner DO, Macario A, Zhou Y, Culley DJ, Keegan MT. Repeated cross‐sectional surveys of burnout, distress, and depression among anesthesiology residents and first‐year graduates. Anesthesiology 2019; 131: 668–77. [DOI] [PubMed] [Google Scholar]
- 50. El‐Boghdadly K, Wong DJN, Owen R, et al. Risks to healthcare workers following tracheal intubation of patients with COVID‐19: a prospective international multicentre cohort study. Anaesthesia 2020; 75: 1437–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wong DJN, El‐Boghdadly K, Johnstone C, Ahmad I. Can gendered personal protective equipment design account for high infection rates in female healthcare workers following intubation? A reply. Anaesthesia 2021; 76: 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Nunez‐Smith M, Pilgrim N, Wynia M, et al. Race/ethnicity and workplace discrimination: results of a national survey of physicians. Journal of General Internal Medicine 2009; 24: 1198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Tolbert Coombs AA, King RK. Workplace discrimination: experiences of practicing physicians. Journal of the National Medical Association 2005; 97: 467. [PMC free article] [PubMed] [Google Scholar]
- 54. O'Brien KR, McAbee ST, Hebl MR, Rodgers JR. The impact of interpersonal discrimination and stress on health and performance for early career STEM academicians. Frontiers in Psychology 2016; 7: 623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. McAlonan GM, Lee AM, Cheung V, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Canadian Journal of Psychiatry 2007; 52: 241–7. [DOI] [PubMed] [Google Scholar]
- 56. Street AE, Dardis CM. Using a social construction of gender lens to understand gender differences in posttraumatic stress disorder. Clinical Psychology Review 2018; 66: 97–105. [DOI] [PubMed] [Google Scholar]
- 57. Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID‐19 outbreak in China hardest‐hit areas: gender differences matter. Psychiatry Research 2020; 287: 112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Leigh‐Hunt N, Bagguley D, Bash K, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017; 152: 157–71. [DOI] [PubMed] [Google Scholar]
- 59. Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with Coronavirus Disease 2019 (COVID‐19) in January and February 2020 in China. International Medical Journal of Experimental and Clinical Research 2020; 26: e923549–e923551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. UN News . UN chief calls for domestic violence ‘ceasefire’ amid ‘horrifying global surge. https://news.un.org/en/story/2020/04/1061052 (accessed October 2020).
- 61. McLindon E, Humphreys C, Hegarty K. “It happens to clinicians too”: an Australian prevalence study of intimate partner and family violence against health professionals. BMC Women's Health 2018; 18: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Matheson FI, Smith KLW, Fazli GS, Moineddin R, Dunn JR, Glazier RH. Physical health and gender as risk factors for usage of services for mental illness. Journal of Epidemiology and Community Health 2014; 68: 971–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Joseph AJ. Constituting “lived experience” discourses in mental health: the ethics of racialized identification/representation and the erasure of intergeneration colonial violence. Journal of Ethics in Mental Health 2019; 10: 1–23. [Google Scholar]
- 64. Wallace JE. Mental health and stigma in the medical profession. Health 2017; 16: 3–18. [DOI] [PubMed] [Google Scholar]


