Abstract
Background
Despite the recognition of the importance of indoor microbial exposures on children’s health, the role of different microbial agents in development and aggravation of respiratory symptoms and diseases is only poorly understood. This study aimed to assess whether exposure to microbial aerosols within the indoor environment are associated with respiratory symptoms among children under-5 years of age.
Methods
A systematic literature search was conducted on PubMed, Web of Science, GreenFILE, ScienceDirect, EMBASE and Cochrane library through February 2020. Studies that investigated the exposure–response relationship between components of the indoor microbial communities and respiratory symptoms among under-five children were eligible for inclusion. A random-effect meta-analysis was applied to estimate pooled relative risk (RR) and 95% confidence interval (CI) for study specific high versus low microbial exposures. The potential effect of individual studies on the overall estimate was evaluated using leave-one-out analysis, while heterogeneity was evaluated by I2 statistics using RevMan 5.3.
Results
Fifteen studies were eligible for inclusion in a meta-analysis. The pooled risk estimate suggested that increased microbial exposure was associated with an increased risk of respiratory symptoms [pooled relative risk (RR): 1.24 (1.09, 1.41), P = 0.001]. The association was strongest with exposure to a combination of Aspergillus, Penicillium, Cladosporium and Alternaria species [pooled RR: 1.73 (1.30, 2.31), P = 0.0002]. Stratified analysis revealed an increased risk of wheeze [pooled RR: 1.20 (1.05, 1.37), P = 0.007 and allergic rhinitis [RR: 1.18 (0.94, 1.98), P = 0.16] from any microbial exposure.
Conclusions
Microbial exposures are, in general, associated with risk of respiratory symptoms. Future studies are needed to study the indoor microbiome more comprehensively, and to investigate the mechanism of these associations.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12940-021-00759-2.
Keywords: Indoor microbiome, Respiratory symptoms, Asthma, Under-five children, Meta-analysis
Background
The microbial community within indoor environments such as dwellings where humans, especially under-five children, spend more than 90% of their time, consists of a wide range of microorganisms including bacteria, fungi, and viruses [1–4]. The microbial load and composition within the indoor environment is determined and influenced by the presence, identity and activities of human occupants [5–7]. Non-human occupants, such as dogs [8, 9] and household insects [10], can also influence the microbial profile of the indoor environment. In addition, indoor microbial communities can be influenced by differences in ventilation, building design, the environmental characteristics found within buildings [9, 11, 12] or prior water damage [13]. The interest in the indoor microbiome has increased over the last few decades [1]. This is largely because of the wider recognition that exposures to microbes in the residential indoor environment are associated with a vast number of adverse health outcomes with major public health importance, including infectious diseases, acute toxic effects, allergies and cancer [1].
Most epidemiological studies have been heterogeneous in assessing different respiratory health effects associated with exposure to specific microbial components, especially endotoxins, and culturable molds [14–17] while very few have investigated indoor microbial communities [18, 19]. These studies have shown inconsistent findings, suggesting protective, detrimental, and no health effects in relation to asthma and allergy [14]. Greater diversity of fungal and bacterial agents has been shown to reduce the risk of asthma and wheeze in children [17, 20, 21] while others found a positive association between elevated levels of total viable mold and risk of rhinitis with persistent cough [22–24].
Respiratory health effects have been the subject of recent research among preschool children [25, 26] and children under the age of 5 years [27]. Children under the age of 5 years are more at risk of respiratory outcomes from exposure to indoor microbial agents due to the fact that they spend a considerable proportion of time in the home environment during a period of intense growth and development of the immunologic and respiratory systems [28, 29]. Despite the recognition of the importance of exposure to the indoor microbiome on children’s health, the precise role of different microbial agents in the development and aggravation of symptoms and diseases is only poorly understood. It is therefore not clear which specific component(s) primarily contribute to the presumed respiratory health effects. To the best of our knowledge, there has been no systematic review or meta-analysis exploring the role of the indoor microbial exposure on respiratory health outcomes among children under 5. Therefore, this systematic review and meta-analysis aims to summarize evidence of associations between different indoor microbial agents and their combined role in the incidence of respiratory allergies and asthma, thereby providing opportunities to improve future respiratory health interventions among under-five children.
Methods and design
Literature search
The protocol for this meta-analysis was reported using MOOSE guideline [30] and registered in the International Prospective Register of Systematic Reviews (Reg ID: CRD42020178514). Two reviewers independently explored PUBMED, WEB OF SCIENCE, GREEN FILE (EBSCO), ScienceDirect, EMBASE and Cochrane databases independent of date through February 2020 to identify appropriate previously published studies using the following search terms; “home” OR “house” OR “dwelling” OR “residence” OR “residential” OR “indoor” OR “domicile” OR “living unit” OR “property” OR “build” OR “built environment” OR “domestic environment” OR “bedroom” OR “living room” OR “wall” OR “floor” OR “ceiling” OR “construction material” AND “damp” OR “fungi” OR “mold” OR “mould” OR “fungal” OR “fungus” OR “bacteria” OR “virus” OR “microbial” OR “microbiome” OR “microbial diversity” OR “microbial load” OR “microbial burden” OR “microbiota” OR “biodiversity” AND “respiratory symptoms” OR “allergy” OR “hay fever” OR “cough” OR “fever” OR “difficulty breathing” OR “wheeze” OR “allergic rhinitis” OR “sinusitis” OR “asthma”. Title and abstract of each article was evaluated independently and differences on which publication(s) to include were clarified by recourse to a third reviewer. A snowball search was also carried out by screening reference lists of publications and reviews.
Inclusion criteria and study selection
Studies eligible for inclusion in the meta-analysis were epidemiological reports in humans with exposure–response relationship between indoor microbial aerosols and respiratory symptoms. Inclusion criteria were: (I) qualitative or quantitative assessment of indoor microbial aerosols. Studies that reported exposure to specific microbial communities (bacteria, fungi, viruses, and/or microbial by-products) or presence/absence of visible molds were included; (II) studies conducted among children aged ≤ 5 years; (III) respiratory symptoms (including wheeze/allergic rhinitis) and/or asthma adequately defined and described; (IV) full text articles in English originally published in peer reviewed journals. Literature reviews, abstracts, letters to the editor, case reports, and non-human studies were excluded.
Assessment of articles was performed in EndNote databases. All duplicates were removed and studies were selected based on title or abstract for full text-screening. For studies that were excluded, the reasons for exclusion were listed.
Data extraction
From the studies that met the inclusion criteria, the following information was extracted: (1) name and initials of the first author, (2) year of publication, (3) country, (4) type of sample, (5) sampling equipment, (6) microbial agent(s), (7) analytical method, (8) level and measure of exposure, (9) respiratory outcome definition, (10) number of cases, (11) sample size and (12) effect estimate. All incongruities from the data extracted were resolved by a third author.
Quality assessment of included studies
Two team members (AGF and NJ) assessed the methodological quality and risk of bias of the included studies using the Cochrane Collaboration guidelines [31] and the Newcastle–Ottawa scales [32]. The quality of the studies was graded by rating nine items representing the study selection procedure, comparability, and outcome/exposure definition. Each item was scored as ‘yes’ (if present) and ‘no’ (if absent) in the included studies and the overall scores were presented as percentages. Studies with median a score ≥ 80% (median in our study) were arbitrarily considered to have a low risk of bias while those with a score < 80% were considered to have a high risk of bias.
Statistical analyses
All statistical analysis was carried out using Review Manager 5.3. We applied the inverse of variance method for weighting and computed the summary effect estimates by first log-transforming all relative risk (RR) and 95% confidence interval (CI) for high vs low category (as reference) of microbial exposure. The standard error (SE) was estimated based on the formula:
| 1 |
The extent of variability across studies and heterogeneity of the summary effect estimates were evaluated using I2 test statistics. Where I2 statistics ≥ 50%, a random effect model was employed, otherwise, a fixed effect model [30, 33]. The area of the black square in forest plots implies the weighted contribution by each study. Sensitivity analyses of the results and publication bias was evaluated using leave-one-out and funnel plot techniques respectively. P < 0.05 (two-tailed) was considered statistically significant [34].
Results
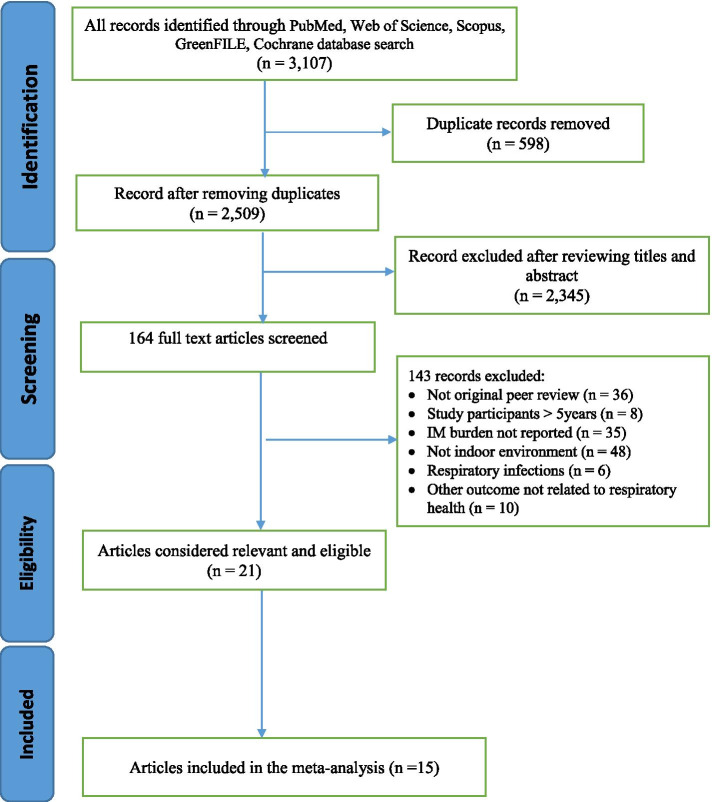
The PRISMA flowchart describing the process used to identify the studies eligible for our meta-analyses yielded 3,107 records (Fig. 1). In addition, duplicates (n = 598) and other records (n = 2,345) after screening titles and abstracts were excluded, resulting in 164 articles for full text assessment. In total, fifteen articles that fulfilled all inclusion criteria were included in the meta-analyses [23, 35–48].
Fig. 1.
PRISMA Flow chart of the literature search for studies investigating Exposure to IM and respiratory symptoms among U-5C. IM = Indoor Microbiome; U-5C = Under-five Children
Detailed characteristics of the included studies are presented in Tables 1 and 2. All fifteen studies had a cohort design with follow-up period between 1 [35, 37–39, 41, 42, 48] and 4 [40, 47] years. Eleven studies were carried out in the United States and four in Europe all between 2000 and 2019. All studies included examined indoor microbial exposure among children under the age of 5 years. The methods of assessment of exposure to indoor microbial aerosols used among studies included air sampling [35, 39], dust sampling [37, 38, 40–44, 46–48] and home inspection using a standard observational checklist [45]. In addition, two studies [23, 36] applied a combination of air and dust sampling techniques. The indoor air samples were collected using Burkard portable air sampler [35] and Hirst-type sampler [39] respectively. The dust samples were collected using high volume vacuum cleaners such as Eureka Mighty-Mite vacuum cleaner, Filter Queen Majestic vacuum cleaner and Rowenta Dymbo vacuum cleaner. Microbial agents assessed were total bacteria [36], total fungi [23, 36, 39], specific fungal genera such as Aspergillus spp. [23, 36, 39], Penicillium spp. [23, 35, 36, 39], Cladosporium spp. [23, 35, 36, 39], Alternaria spp. [23, 36], yeast [23, 36, 49], visible molds [23, 45] and endotoxins [37, 38, 40–44, 46–48]. In terms of the analytical methods employed, the bacterial and fungal agents were assessed using conventional plate count methods [23, 35, 36] while endotoxins were analysed using the kinetic chromogenic Limulus amebocyte lysate (LAL) test [41–44, 46–48]. Respiratory outcomes in the included studies were allergic rhinitis [23, 42, 43, 45], wheeze [35–44, 46–48] and asthma [44, 47]. These outcomes were assessed by doctors’ diagnosis using clinical examination [23, 39, 47] and parental/caregiver’s recall [35–38, 40–46, 48]. After a detailed quality assessment of the included studies based on the Newcastle–Ottawa scale for assessing the quality of non-randomized studies, most of the studies (n = 8) had a score < 80% (median in our study) and were categorized as high risk of bias. Others (n = 7) were considered to have a low risk of bias (score ≥ 80%) (Table S1).
Table 1.
Participants characteristics of eligible studies included in the meta-analysis
| Author | Year | Country | Microbial assessment/definition of measure | Assessment of Respiratory health Outcome | Effect estimate | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Type of sample | Sampling equipment | Agent | Analytical method | Measure of Exposure | Definition | N Cases | N total (baseline) | ||||
| Gent et al., | 2002 | USA | Indoor Air | Burkard portable air sampler | Fungi | Plate count; | Undetectable® Vs ≥ 1000 cfu/m3 | Reported wheeze and persistent cough measured as number of days of symptoms (0, < 30 and ≥ 30 days) | 119 | 880 |
RPW: 2.15 (1.34 – 3.46)a PC: 2.06 (1.31 – 3.24)a |
| Rosenbaum et al., | 2010 | USA | Indoor Air; Dust sample | Single-stage Andersen air sampler; High volume vacuum cleaner | Bacteria; Fungi; Endotoxin | Plate count; KLARE | Not detectable® Vs > 75th percentile | Primary care provider documented wheeze; Wheeze heard on physical examination by a clinician | 39 | 103 | 6.18 (1.34—28.46)a |
| Horick et al., | 2006 | USA | Dust sample | High volume vacuum cleaner | Endotoxin | KLARE | TEC < 100 EU/mg® Vs ≥ 100EU/mg | Primary care provider reported “any wheeze” ≥ 1 episode | 42 | 360 | 5.56 (1.19 – 26.03)a |
| Park et al., | 2001 | USA | Dust sample | Eureka Mighty-Mite vacuum cleaner | Endotoxin | KLARE | TEC < 100 EU/mg® Vs ≥ 100EU/mg | Primary care provider reported “any wheeze” ≥ 1 episode or repeated episode of wheeze | 211 | 499 |
AW: 1.33 (0.99–1.79)a RW: 1.55 (1.00 – 2.42)a |
| Harley et al., | 2009 | USA | Indoor Air | Hirst-type sampler | Fungi spores | Spore count | Not detectable® Vs ≥ 1000 cfu/m3 | A child was considered to have early wheezing if medical records indicated a clinician’s diagnosis of asthma at any time between birth and 24 months of age | 35 | 514 | 1.2 (0.7 – 2.7)a |
| Litonjua et al., | 2002 | USA | Dust sample | High volume vacuum cleaner | Endotoxin | KLARE | TEC < 81.3 EU/mg® Vs ≥ 81.3EU/mg | Wheezing in the past 12 month or repeated wheezing twice in the 4 years of follow-up | 57 | 226 |
W: 1.52 (1.07—2.14)a RW: 2.57 (1.00 – 6.62)a |
| Campo et al., | 2006 | USA | Dust sample | Filter Queen Majestic vacuum cleaner | Endotoxin | Kinetic Chromogenic -LAL | TEC < 100 EU/mg® Vs ≥ 100EU/mg | Recurrent wheeze; ≥ 2 wheezing episodes in the past 12 months or any wheezing: ≥ 1 wheezing episode in the past 12 months | 137 | 532 |
RCW: 0.4 (0.1–0.9)a AW: 0.3 (0.1–0.8)a |
| Gillespie et al., | 2006 | New Zealand | Dust sample | High volume vacuum cleaner | Endotoxin | Kinetic Chromogenic -LAL | TEC < 100 EU/mg® Vs ≥ 100EU/mg | Reported wheeze for at least 6 months. Rhinitis defined as blocked or runny nose when the child do not have a cold or flu | 342 | 881 | 1.54 (1.03 – 2.30)a |
| Perzanowski et al., | 2006 | USA | Dust sample | Eureka Mighty-Mite vacuum cleaner | Endotoxin | Kinetic Chromogenic -LAL | TEC < 100 EU/mg® Vs ≥ 100EU/mg | Wheezing defined as presence of runny nose, sneezing, itchy eyes without cold at age 12, 24 and 36 months | 163 | 301 | 1.04 (0.71 – 1.5)a |
| Karvonen et al., | 2012 | EU | Dust sample | High volume vacuum cleaner | Endotoxin | Kinetic Chromogenic -LAL | TEC < 100 EU/mg® Vs ≥ 100EU/mg | Primary care provider reported “any wheeze” ≥ 1 episode | 984 | 1133 | 0.71 (0.51 – 0.99)a |
| Stark et al., | 2005 | USA |
Indoor Air Dust sample |
Burkard portable air sampler; Eureka Mighty Mite canister vacuum cleaner | Fungi | Plate count |
Low® Vs High TEC < 100 EU/mg® Vs ≥ 100EU/mg |
Doctor diagnosed allergic rhinitis or hay fever | 52 | 405 | 3.13 (1.51 – 6.47)a |
| Biagini et al., | 2006 | USA | Home inspection | Walkthrough Checklist | Mold | Observation | Low® Vs High | Rhinitis defined as parents’ report of sneezing or a runny or blocked nose not associated with a cold or chest infection’ in the past 30 days | 242 | 495 | 1.7 (0.7 – 3.8)a |
| Bolte et al., | 2003 | Germany | Dust sample | High volume vacuum cleaner | Endotoxin | Kinetic Chromogenic -LAL | Highest quartile Vs Lowest quartile® | Repeated wheeze defined as having had at least 2 episode of wheezing | 378 | 1,942 | 1.77 (1.14 – 2.73)a |
| Douwes et al., | 2006 | The Netherlands | Dust sample | Rowenta Dymbo vacuum cleaner | Endotoxin | Kinetic Chromogenic -LAL | Highest quartile Vs Medium quartile® | Doctor-diagnosed asthma was defined as a reported diagnosis confirmed by a doctor at any time in the past 4 years | 547 | 696 | 0.40 (0.21 – 0.77)a |
| Phipatanakul et al., | 2005 | USA | Dust sample | High volume vacuum cleaner | Endotoxin | Kinetic Chromogenic -LAL | 4th quartile Vs 1st quartile® | Any report of wheeze (any wheeze) in the first year of life | 197 | 498 | 2.39 (1.22 – 4.68)a |
YOF Year of Follow-up, EU Europe, NA Not applicable, W Wheeze in the past 12 months, KLARE Kinetic Limulus assay with the resistant-parallel-line estimation, LAL Limulus amebocyte lysate, AW Any wheeze, RW Repeated wheeze, RPW Reported wheeze, RCW Recurrent wheeze, ® Reference value, PC Persistent cough, SPT Skin Prick Test
aMultivariable adjusted effect estimate for LRTI risk
Table 2.
Summary effect estimate for the relationship between any IM exposure (highest estimates in the studies) and Respiratory symptoms (n = 15), and stratified analysis according to study characteristics
| Stratification | Study Characteristics (Number of studies) | I2 (%) | Summary Effect Estimate for pooled adjusted data [95% CI] | P-value |
|---|---|---|---|---|
| Population | All studies (15) [12, 18, 25–37] | 78 | 1.24 [1.09, 1.41] | 0.001 |
| Study sizea | Large (6) [25, 30, 32, 34–36] | 82 | 1.14 [1.02, 1.38] | 0.04 |
| Small (9) [12, 18, 26–29, 31, 33, 37] | 67 | 1.33 [1.11, 1.59] | 0.002 | |
| Geographical Location | United States (11) [12, 18, 25–31, 33, 37] | 63 | 1.35 [1.15, 1.57] | 0.0001 |
| Europe (4) [32, 34–36] | 81 | 1.06 [0.87, 1.28] | 0.56 | |
| Year of Publication | 2010 – 2019 (2) [12, 34] | 84 | 1.34 [0.58, 3.09] | 0.49 |
| 2000 – 2009 (13) [18, 25–33, 35–37] | 60 | 1.25 [1.12, 1.41] | 0.0002 | |
| Method of IM Assessment | Air sampling (3) [12, 25, 28] | 2 | 1.48 [1.25, 1.75] | 0.00001 |
| Dust sampling (11) [18, 26, 27, 29, 31–37] | 76 | 1.12 [0.98, 1.29] | 0.11 | |
| Home Inspection (1) [30] | NA | 1.66 [0.85, 3.21] | 0.14 | |
| Method of diagnosis | Doctor diagnosed (2) [18, 28] | NA | 1.60 [1.28, 2.01] | < 0.0001 |
| Self-reported (13) [12, 25–27, 29–37] | 76 | 1.19 [1.04, 1.35] | 0.009 | |
| Study Quality | Low risk of bias (7) [12, 18, 25, 27, 28, 31, 32] | 59 | 1.31 [1.12, 1.55] | 0.001 |
| High risk of bias (8) [26, 29, 30, 33–37] | 75 | 1.17 [0.99, 1.37] | 0.06 |
NA Not applicable
aA large study was defined as a cohort study with a sample size of greater than 600
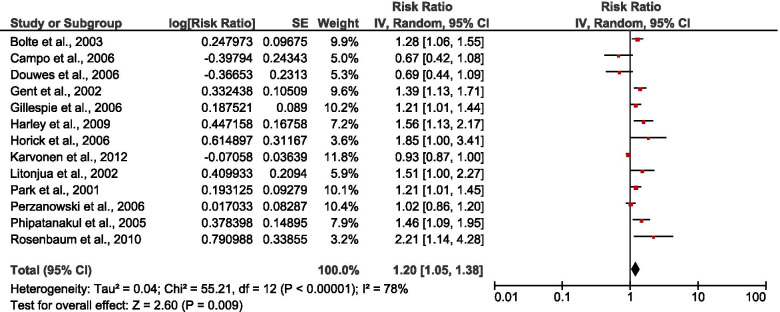
Tables 2 and 3 provided study characteristics and summary effect estimates of all 15 studies [23, 35–48] addressing the association between different indoor microbial exposures and respiratory symptoms among children under 5. The pooled risk estimate from the random effect model showed a significant association between microbial exposure and respiratory symptoms; RR: 1.24 (1.09, 1.41), P = 0.001, I2 = 78% (Fig. 2A). The risk estimate was observed to vary geographically: RR: 1.35 (1.15, 1.57), P = 0.0001; I2 = 63% (United States) and RR: 1.06 (0.87, 1.28, P = 0.56; I2 = 81% (Europe). Further stratification showed that the risk estimates were RR: 1.48 (1.25, 1.75), P < 0.00001 for studies that used air sampling for exposure assessment and RR: 1.12 (0.98, 1.29), P = 0.11 for studies based on dust sampling techniques. Also, indoor microbial exposure was found to be associated with an increased risk of wheeze independent of the risk of bias of studies included in the meta-analysis.
Table 3.
Effect estimates (EEs) of studies for the association between IM and respiratory symptoms among U-5C (the highest EEs reported for any IM exposure)
| Author, year/Country |
Type of Exposure and EEs Adjusted EE (95% CI) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Any IM exposure | TFC | Aspergillus spp. | Penicillium spp. | Cladosporium spp. | Alternaria spp. | Visible molds | Endotoxin | |
| Gent et al., 2002/USA [35] | 2.15 (1.34, 3.46) | - | - | 2.15 (1.34, 3.46) | 0.91 (0.53, 1.56) | - | - | |
| Rosenbaum et al., 2010/USA [36] | 6.18 (1.34, 28.46) | 3.64 (0.67, 19.65) | 1.58 (0.43, 5.79) | 6.18 (1.34, 28.46) | 2.28 (0.41, 12.67) | 0.96 (0.27, 3.45) | - | |
| Horick et al., 2006/USA [37] | 4.12 (1.03, 16.83) | - | - | - | - | - | 4.12 (1.03, 16.83) | |
| Park et al., 2001/USA [38] | 1.56 (1.03, 2.38) | - | - | - | - | - | 1.56 (1.03, 2.38) | |
| Harley et al., 2009/USA [39] | 2.80 (1.30, 5.90) | 1.20 (0.70, 2.00) | 1.3 (1.10, 1.50) | 1.3 (1.10, 1.50) | 0.90 (0.50, 1.60) | - | - | |
| Litonjua et al., 2002/USA [40] | 2.57 (1.00, 6.62) | - | - | - | - | - | 2.57 (1.00, 6.62) | |
| Campo et al., 2006/USA [41] | 0.40 (0.10, 0.90) | - | - | - | - | - | 0.40 (0.10, 0.90) | |
| Gillespie et al. 2006/Europe [42] | 1.54 (1.03, 2.30) | - | - | - | - | - | 1.54 (1.03, 2.30) | |
| Perzanowski et al. 2006/USA [43] | 1.04 (0.71, 1.50) | - | - | - | - | - | 1.04 (0.71, 1.50) | |
| Karvonen et al. 2012/Europe [44] | 0.85 (0.72, 1.00) | - | - | - | - | - | 0.85 (0.72, 1.00) | |
| Bolte et al., 2003/Europe [46] | 1.77 (1.14, 2.73) | - | - | - | - | - | 1.77 (1.14, 2.73) | |
| Douwes et al., 2006/Europe [47] | 0.40 (0.21, 0.77) | - | - | - | - | - | 0.40 (0.21, 0.77) | |
| Phipatanakul et al., 2005/USA [48] | 2.39 (1.22, 4.68) | - | - | - | - | - | 2.39 (1.22, 4.68) | |
| Stark et al., 2005/USA [23] | 3.13 (1.51, 6.47) | 3.13 (1.51, 6.47) | 2.57 (1.22, 4.40) | 1.51 (0.63, 3.64) | 1.88 (0.81, 4.35) | 2.34 (1.12, 4.91) | 1.66 (0.87, 3.17) | - |
| Biagini et al., 2006/USA [45] | 1.70 (0.70, 3.80) | - | - | - | - | - | 1.70 (0.70, 3.80) | - |
TFC Total Fungal Count
Adjusted model in each study:
- Gent et al., adjusted for socioeconomic factors and housing characteristics
- Rosenbaum et al., adjusted for season of visit, maternal smoking during pregnancy, any smoker in the home, day care center or nonrelative care, and endotoxin
- Horick et al., adjusted for race, presence of dog in home, former (not current) dog in home, use of dehumidifier, total mass of dust sample collected (in log scale), presence of concrete floor, missingness indicator for presence of concrete floor, and presence of water damage
- Park et al., adjusted for age, race/ethnicity and socioeconomic characteristics
- Harley et al., adjusted for gas stove in home, respiratory infection in first year of life, and PM2.5 in first 3 months of life (residuals independent of spores)
- Litongua et al., adjusted for maternal asthma, maternal age, sex, prematurity, and area of residence
- Campo et al., adjusted for sex, daycare attendance, number of siblings, mother smokes, parental history of asthma
- Gillespie et al., adjusted for household size, number of rooms in the house, pet in home, dampness, musty smell, maternal smoking, open fireplace, type of flooring in the bedroom, and New Zealand Deprivation index
- Perzanowski et al., adjusted for sex, maternal asthma, ethnicity and tobacco smoke exposure in the home
- Karvonen et al., adjusted for study centre, farming status, gender, maternal history of allergic disease, smoking during pregnancy and number of sibling
- Bolte et al., adjusted for gender, study region, breastfeeding, elder siblings, parental education, mite and cat allergen levels, frequent respiratory infections and smoking during pregnancy
- Douwes et al., adjusted for sex, region, parental education level, exposure to indoor tobacco smoke in the past 4 years, and other children in the household at 4 years of age
- Phipatanakul et al., adjust for sex, household income, and paternal history of asthma
- Stark et al., adjusted for water damage or mold or mildew in year 1, African-American ethnicity, maternal Alternaria, IgE > 0.35 U/mL
- Biagini et al., adjusted for mother’s education, gender, cat and dog ownership, daycare attendance, breastfeeding and number of diaries returned
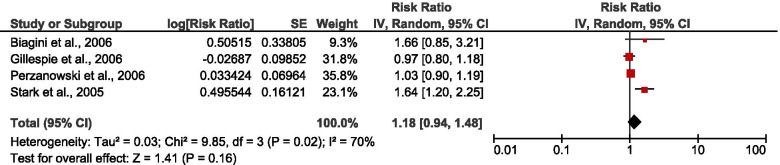
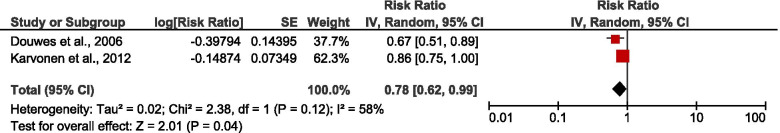
Fig. 2.
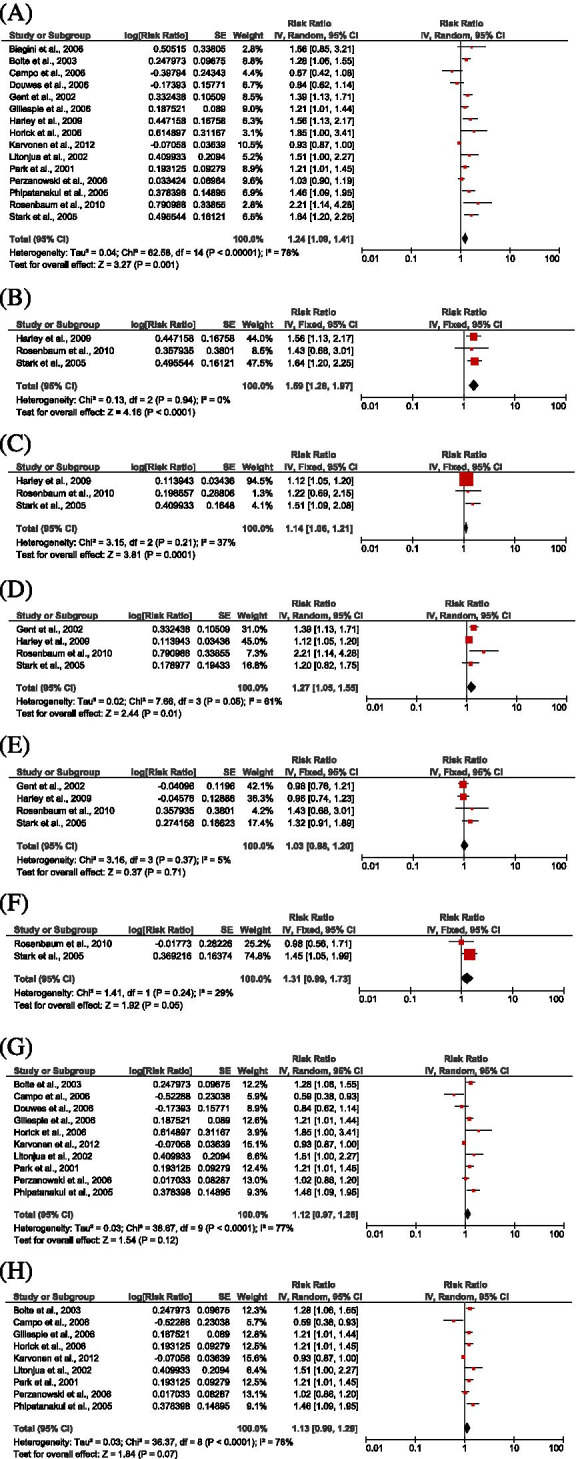
Forest plot for the relationship between any IM exposure and Respiratory symptoms among U-5C with pooled effect estimates (A); between TFC and Respiratory symptoms (B); between Aspergillus species and Respiratory symptoms (C); between Penicillium species and Respiratory symptoms (D); between Cladosporium species and Respiratory symptoms (E); between Alternaria species and Respiratory symptoms (F); between Endotoxin and Respiratory symptoms (G); between Endotoxin and Wheeze (H)
Three studies [23, 36, 39] provided study-specific estimates for risk of respiratory symptoms from exposure to total fungal concentration; TFC (CFU/m3), resulting in a risk estimate of RR: 1.59 [1.28. 1.97], P < 0.0001; I2 = 0% (Fig. 2B). Risk of respiratory symptoms based on exposure to specific fungal genera revealed a pooled risk estimate of RR: 1.14 [1.06, 1.21], P = 0.0001 for Aspergillus species (Fig. 2C), RR: 1.27 [1.05, 1.55], P = 0.01 for Penicillium species (Fig. 2D), RR: 1.03 [0.88, 1.20], P = 0.71 for Cladosporium species (Fig. 2E) and RR: 1.31 [0.99, 1.73], P = 0.05 for Alternaria species (Fig. 2F). The combined model based on four studies [23, 35, 36, 39] showed a significantly increased risk of respiratory symptoms when under-five children were exposed to a combination of two most reported fungal genera; Penicillium spp. and Cladosporium spp. compared to unexposed under-five children [RR: 1.51 (1.31, 1.76), P < 0.00001; I2 = 0%] (model 1). Three studies [23, 36, 39] revealed that exposure to a combination of three commonly reported fungal genera; Aspergillus spp., Penicillium spp. and Cladosporium spp. produced a stronger risk of respiratory symptoms [RR: 1.66 (1.34, 2.06), P < 0.00001; I2 = 0%] (model 2). The study-specific estimates based on two studies [23, 36] showed that exposure to a combination of Aspergillus spp., Penicillium spp., Cladosporium spp. and Alternaria spp. significantly increase the risk of respiratory symptoms by 73% [RR: 1.73 (1.30, 2.31), P = 0.0002; I2 = 0%] (model 3) (Table 4). Ten studies [37, 38, 40–44, 46–48] investigated the relationship between endotoxins and respiratory symptoms, resulting in a pooled estimate that was not statistically significant [1.12 (0.97, 1.28), P = 0.12, I2 = 77%] (Fig. 2G) likewise the relationship between endotoxins and wheeze among under-five children (Fig. 2H) obtained from a pooled risk estimate of nine studies.
Table 4.
Combined effect estimate for the relationship between exposure to fungal genera and respiratory symptoms among U-5C
| Model in subgroup analysis | Number of studies | I2 (%) |
Summary Effect Estimate for pooled adjusted data [95% CI] |
P-value |
|---|---|---|---|---|
| Model 1: Two most reported fungal genera; Penicillium and Cladosporium species | (4) | 0 | 1.51 [1.31, 1.76] | < 0.00001 |
| Model 2: Three commonly reported fungal genera; Aspergillus, Penicillium, Cladosporium | (3) | 0 | 1.66 [1.34, 2.06] | < 0.00001 |
| Model 3: Four reported fungal genera; Aspergillus, Penicillium, Cladosporium and Alternaria | (2) | 0 | 1.73 [1.30, 2.31] | 0.0002 |
Thirteen studies [35–44, 46–48] assessed the association between different microbial exposures and wheeze. The pooled risk estimate from the random effect model showed a significant association between indoor microbial exposure and wheeze [RR: 1.20 (1.05, 1.37), P = 0.007, I2 = 78% (Fig. 3). Only four studies [23, 42, 43, 45] investigated the association between different microbial exposure and allergic rhinitis with no significant relationship (Fig. 4). In addition, two studies [44, 47] investigated the association between any exposure and asthma among under-five children with a significant protective effect [RR: 0.78 (0.62, 0.99), P = 0.04], (Fig. 5).
Fig. 3.
Forest plot for the relationship between any IM exposure and wheeze among U-5C with pooled effect estimates
Fig. 4.
Forest plot for the relationship between any IM exposure and allergic rhinitis among U-5C with pooled effect estimates
Fig. 5.
Forest plot for the relationship between endotoxin and asthma among U-5C with pooled effect estimates
The funnel plots showed no significant evidence of publication bias among the studies included in the meta-analyses (Supplementary Figures S1, S2 and S3). We tested the effect of excluding individual studies on the stability of the pooled effect estimates and found no single study exerted significant effect on the overall effect estimate of the meta-analysis. Details of the sensitivity analysis are provided in Supplementary Table S2.
Discussion
This systematic review and meta-analysis summarizes the current knowledge on the association between qualitative and quantitative estimates of microbial agents within the indoor environment and respiratory symptoms among children under the age of 5 years. To the best of our knowledge, our meta-analysis is the most comprehensive overview to investigate whether exposure to indoor microbial aerosols is associated with respiratory health of children under the age of 5 years. First, we observed that exposure to a combination of Aspergillus, Penicillium and Cladosporium species increased the risk of wheeze by 67%. Secondly, the association of indoor microbial exposure with allergic rhinitis was not significant. Thirdly, exposure to microbial agents such as endotoxins was protective against asthma, although the estimate was from two studies.
The combined analysis revealed an increased risk of wheeze when children under 5 were exposed to a combination of Aspergillus and Penicillium species, which was reduced by the addition of Cladosporium species to the model. This suggests that microbial interaction within the indoor environment may play a role in the respiratory health of children under the age of 5 years. These specific fungi within the indoor environment have also been shown to be associated with an increased risk of wheeze [17, 36] and asthma [24, 35, 50] in longitudinal studies. A similar meta-analysis on fungal exposure and respiratory health in children aged 6–12 years [51] compares well to the pooled estimate reported in our meta-analyses. Relevant studies both in vitro and in vivo have demonstrated that repeated activation of immune responses and inflammation from fungal exposures may contribute to inflammation-related diseases, and the resulting inflamed mucosal tissue may provide a diminished barrier to respiratory infections [17]. Also, prolonged exposure to aerosolized fungal components mainly target the respiratory and nervous system causing specific pathological changes in the host characterized by inflammation and continuous activation of immune responses as a result of fungal exposures may contribute to inflammation-related diseases [52]. Our review considered exposure to visible molds only or in association with dampness, but excluded studies considering dampness alone. Indeed, mold and dampness exposures are often connected, leading to increased fungal growth and correlated microbial exposures, such as fungal spores, hyphae, fragments [53], microbial volatile organic compounds [54, 55], mycotoxins [56], house dust mite allergens [57] and endotoxins [58, 59].
The definitions of respiratory outcomes among children < 6 years of age are often poorly described and confusing, thereby making the diagnosis of the disease in preschool children difficult [60]. As a result, the European Respiratory Society task force proposed the use of terms such as “episodic (viral) wheeze” (among children with recurrent wheeze and who are well between episodes) and “multiple-trigger wheeze” (among children who wheeze both during and after discrete episodes) [61]. In fact, some other definitions have also been used to describe the different phenotypes of preschool wheezing disorders such as the presence of transient early wheezing in children < 3 years, non-atopic wheezing in children aged 3–6 years, and IgE-mediated wheeze in older children [62]. More recent studies have suggested that these definitions may reflect disease severity and that they are likely to vary with time [63]. Specific factors responsible for the development of respiratory diseases in children < 6 years has not been identified; however, interactions between the environment and genetic factors of each individual play a vital role [64]. These factors include infections, atopy, prematurity, exposure to tobacco smoke, exposure to elevated levels of air pollution or family history of asthma [62, 65, 66]. A recent meta-analysis reported an increased risk of lower respiratory tract infection among under-five children as a result of increased exposure to indoor microbes with emphasis on detailed microbial characterization using modern molecular techniques [67].
It was interesting to discover that none of the studies included in the present meta-analysis employed molecular-based techniques in the analysis of microbial agents. Although, studies have investigated the burden of indoor microbial exposures using sequencing-based assessment [9, 68–70] but very few demonstrated a link with disease epidemiology such as respiratory outcomes as revealed in the present study. This is probably due to the complexity of the microbial exposure and the lack of clear understanding of the mechanism involved in the association between indoor microbial agents and disease outcomes.
Recent studies have emphasized the protective effect of exposure to endotoxins [25, 26, 71–73] against respiratory allergies and allergic asthma. Our findings corroborate these reports but contradicts some findings among older children [74–76] and adults [77–79]. A previous study reported that exposure to endotoxin has been associated with reduced risk of childhood atopy but an increased risk of wheeze [80]. A comprehensive meta-analysis confirmed this contradiction with respect to endotoxin exposure [73]. Among pre-school children, in whom asthma is more strongly associated with atopy, endotoxin exposure resulted in reduced risk, whereas among infants and toddlers with virus-triggered wheeze, endotoxin increased the risk [73]. Similar findings were reported from the survey carried out by the National Health and Nutrition Examination Survey study enrolling more than 6,000 subjects across the United States. They found that endotoxin was a risk for wheeze but not asthma [59]. Less is known about other bacterial and fungal exposures in indoor urban homes. In the Boston cohort increased levels of muramic acid as a marker for gram-positive bacteria were inversely associated with current asthma but not with allergic sensitization [80]. However, the mechanisms are still not fully understood. Possible explanation indicate that endotoxin is a potent inducer of interleukin-12 and interferon gamma, which downregulate the production of T-lymphocyte helper 2 (Th2) cells involved in the development of allergic diseases [81]. Besides, the potential of T-lymphocyte helper 1 (Th1) inducers like endotoxin and other microbial exposures to mitigate allergy and asthma is consistent with clinical studies. Overall, evidence of the mechanism of association between exposure to indoor microbes and respiratory outcomes is limited. Nevertheless, further longitudinal studies of the effect of early-life exposure to endotoxins on subsequent child health will be needed to understand this mechanism more fully.
In addition, studies included in the meta-analyses have used proxy measures for estimating respiratory health outcome, such as outcome obtained from parental or other caregiver interviews, questionnaires, and medical records. None of the studies quantified indoor microbial contamination to the species level using molecular techniques, which restricted analyses to the fungal genera and potentially underestimate exposures. Also, the differences in the RRs across the included studies could have also contributed to the high heterogeneity. Regardless of these limitations, this study has provided sufficient evidence required in designing future longitudinal studies to further investigate and explain the mechanism involved in the exposure–response relationship between indoor microbial exposure and respiratory symptoms among children under 5.
Conclusions
Indoor microbial aerosol exposures increase the risk of respiratory symptoms such as wheeze and allergic rhinitis but protect against asthma in children under 5. More research regarding these relationships is required using modern analytical approaches such as molecular-based sequencing techniques to better inform/advise parents, form guidelines to reduce exposure to microbial agents within the indoor environment and provide useful intervention strategies for managing the impact of exposure to microbial agents in association with respiratory symptoms among children under the age of 5 years.
Supplementary Information
Additional file 1: Table S1. Quality Assessment of studies included in the meta-analysis using the Newcastle-Ottawa Scaling. Table S2. Leave-one-out sensitivity Analysis of pooled effect estimates of studies included in the meta-analysis. Figure S1. Funnel plots with pseudo-95% confidence limit for any IM exposure and wheeze among U-5C (A); TFC and wheeze (B); Aspergillus spp. and wheeze (C); Penicillium spp. and wheeze (D); Cladosporium spp and wheeze (E); Endotoxin and wheeze (F). Figure S2. Funnel plots with pseudo-95% confidence limit for any IM exposure and allergic rhinitis among U-5C (A); visible mold and allergic rhinitis (B); Endotoxin and allergic rhinitis (C). Figure S3. Funnel plots with pseudo-95% confidence limit for any IM exposure/endotoxin and asthma among U-5C.
Acknowledgements
We acknowledged support of the European Respiratory Society – ERS Short-term Research Fellowship April 2020 (STRF April 2020)- STRTF202004-00799.
Abbreviations
- CI
Confidence interval
- NOS
Newcastle-Ottawa Scale
- OR
Odds ratio
- RR
Relative risk
- SE
Standard error
- EEs
Summary effect estimates
- P
P-Value
- Th1
T-lymphocyte helper 1
- Th2
T-lymphocyte helper 2
- CD14
Cluster of differentiation 14
- PRISMA
Preferred Reporting Item for Systematic Review and Meta-analyses
Authors’ contributions
AGF and NJ performed the literature search, evaluated the titles and abstracts of each articles independently and the differences on which article to include were clarified by recourse to RNN. AGF and NJ independently performed the data extraction. AGF developed the first manuscript draft, carried out the statistical analyses, and quality assessment on the included studies. RNN and LAMS supervised the whole process and reviewed the manuscript. All authors contributed to the interpretation of the data, read and approved the final manuscript.
Funding
None.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its additional files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interest to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Adekunle Gregory Fakunle, Email: fakunz@yahoo.com.
Nkosana Jafta, Email: jaftan@ukzn.ac.za.
Rajen N. Naidoo, Email: naidoon@ukzn.ac.za
Lidwien A. M. Smit, Email: l.a.smit@uu.nl
References
- 1.National Academies of Sciences EaMN . Microbiomes of the built environment: a research agenda for indoor microbiology, human health and buildings. Washington, DC: The National Academies Press; 2017. [PubMed] [Google Scholar]
- 2.Nevalainen A, Seuri M. Of microbes and men. Indoor Air. 2005;15(Suppl 9):58–64. doi: 10.1111/j.1600-0668.2005.00344.x. [DOI] [PubMed] [Google Scholar]
- 3.Brasche S, Bischof W. Daily time spent indoors in German homes - Baseline data for the assessment of indoor exposure of German occupants. Int J Hyg Environ Health. 2005;208(4):247–253. doi: 10.1016/j.ijheh.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Nazaroff WW. Embracing microbes in exposure science. J Expo Sci Environ Epidemiol. 2019;29(1):1–10. doi: 10.1038/s41370-018-0075-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dunn RR, Fierer N, Henley JB, Leff JW, Menninger HL. Home life: factors structuring the bacterial diversity found within and between homes. PLoS One. 2013;8(5):e64133. doi: 10.1371/journal.pone.0064133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sordillo JE, Alwis UK, Hoffman E, Gold DR, Milton DK. Home characteristics as predictors of bacterial and fungal microbial biomarkers in house dust. Environ Health Perspect. 2011;119(2):189–195. doi: 10.1289/ehp.1002004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shelton BG, Kirkland KH, Flanders WD, Morris GK. Profiles of airborne fungi in buildings and outdoor environments in the United States. Appl Environ Microbiol. 2002;68(4):1743–1753. doi: 10.1128/AEM.68.4.1743-1753.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fujimura KE, Johnson CC, Ownby DR, Cox MJ, Brodie EL, Havstad SL, et al. Man’s best friend? The effect of pet ownership on house dust microbial communities. J Allergy Clin Immunol. 2010;126(2):410–2. doi: 10.1016/j.jaci.2010.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kettleson EM, Adhikari A, Vesper S, Coombs K, Indugula R, Reponen T. Key determinants of the fungal and bacterial microbiomes in homes. Environ Res. 2015;138:130–135. doi: 10.1016/j.envres.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gliniewicz A, Czajka E, Laudy AE, Kochman M, Grzegorzak K, Sawicka B, et al. German cockroaches (Blattella Germanica L.) as a potential source of pathogens causing nosocomial infections. Indoor Built Environ. 2003;12:55–60. doi: 10.1177/1420326X03012001009. [DOI] [Google Scholar]
- 11.Adams RI, Miletto M, Lindow SE, Taylor JW, Bruns TD. Airborne bacterial communities in residences: similarities and differences with fungi. PLoS One. 2014;9(3):e91283. doi: 10.1371/journal.pone.0091283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meadow JF, Altrichter AE, Kembel SW, Kline J, Mhuireach G, Moriyama M, et al. Indoor airborne bacterial communities are influenced by ventilation, occupancy, and outdoor air source. Indoor Air. 2014;24(1):41–48. doi: 10.1111/ina.12047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emerson J, Keady P, Brewer T, Clements N, Morgan E, Awerbuch J, et al. Impacts of flood damage on airborne bacteria and fungi in homes after the 2013 Colorado Front Range flood. Environ Sci Technol. 2015;49(5):2675–84. doi: 10.1021/es503845j. [DOI] [PubMed] [Google Scholar]
- 14.Norback D, Cai GH. Dampness, indoor mould, fungal DNA and respiratory health - molecular methods in indoor epidemiology. Clin Exp Allergy. 2015;45(5):840–843. doi: 10.1111/cea.12524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharpe RA, Bearman N, Thornton CR, Husk K, Osborne NJ. Indoor fungal diversity and asthma: a meta-analysis and systematic review of risk factors. J Allergy Clin Immunol. 2015;135(1):110–122. doi: 10.1016/j.jaci.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Jaakkola MS, Quansah R, Hugg TT, Heikkinen SA, Jaakkola JJ. Association of indoor dampness and molds with rhinitis risk: a systematic review and meta-analysis. J Allergy Clin Immunol. 2013;132(5):1099–110.e18. doi: 10.1016/j.jaci.2013.07.028. [DOI] [PubMed] [Google Scholar]
- 17.Fisk WJ, Eliseeva EA, Mendell MJ. Association of residential dampness and mold with respiratory tract infections and bronchitis: a meta-analysis. Environ Health. 2010;9:72–82. doi: 10.1186/1476-069X-9-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirjavainen PV, Karvonen AM, Adams RI, Täubel M, Roponen M, Tuoresmäki P, et al. Farm-like indoor microbiota in non-farm homes protects children from asthma development. Nat Med. 2019;25(7):1089–1095. doi: 10.1038/s41591-019-0469-4. [DOI] [PubMed] [Google Scholar]
- 19.O’Connor GT, Lynch SV, Bloomberg GR, Kattan M, Wood RA, Gergen PJ, et al. Early-life home environment and risk of asthma among inner-city children. J Allergy Clin Immunol. 2018;141(4):1468–1475. doi: 10.1016/j.jaci.2017.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ege MJ, Mayer M, Normand AC, Genuneit J, Cookson WO, Braun-Fahrlander C, et al. Exposure to environmental microorganisms and childhood asthma. N Engl J Med. 2011;364(8):701–709. doi: 10.1056/NEJMoa1007302. [DOI] [PubMed] [Google Scholar]
- 21.Jacobs J, Borras-Santos A, Krop E, Taubel M, Leppanen H, Haverinen-Shaughnessy U, et al. Dampness, bacterial and fungal components in dust in primary schools and respiratory health in schoolchildren across Europe. Occup Environ Med. 2014;71(10):704–712. doi: 10.1136/oemed-2014-102246. [DOI] [PubMed] [Google Scholar]
- 22.Simoni M, Cai GH, Norback D, Annesi-Maesano I, Lavaud F, Sigsgaard T, et al. Total viable molds and fungal DNA in classrooms and association with respiratory health and pulmonary function of European schoolchildren. Pediatr Allergy Immunol. 2011;22(8):843–852. doi: 10.1111/j.1399-3038.2011.01208.x. [DOI] [PubMed] [Google Scholar]
- 23.Stark PC, Celedon JC, Chew GL, Ryan LM, Burge HA, Muilenberg ML, et al. Fungal levels in the home and allergic rhinitis by 5 years of age. Environ Health Perspect. 2005;113(10):1405–1409. doi: 10.1289/ehp.7844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reponen T, Lockey J, Bernstein DI, Vesper SJ, Levin L, Khurana Hershey GK, et al. Infant origins of childhood asthma associated with specific molds. J Allergy Clin Immunol. 2012;130(3):639–44.e5. doi: 10.1016/j.jaci.2012.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carlsten C, Ferguson A, Dimich-Ward H, Chan H, DyBuncio A, Rousseau R, et al. Association between endotoxin and mite allergen exposure with asthma and specific sensitization at age 7 in high-risk children. Pediatr Allergy Immunol. 2011;22(3):320–326. doi: 10.1111/j.1399-3038.2010.01123.x. [DOI] [PubMed] [Google Scholar]
- 26.Tischer C, Gehring U, Chen CM, Kerkhof M, Koppelman G, Sausenthaler S, et al. Respiratory health in children, and indoor exposure to (1,3)- -D-glucan, EPS mould components and endotoxin. Eur Respir J. 2011;37(5):1050–1059. doi: 10.1183/09031936.00091210. [DOI] [PubMed] [Google Scholar]
- 27.Fakunle GA, Olusola B, Jafta N, Faneye A, Heederik D, Smit AML, et al. Home Assessment of Indoor Microbiome (HAIM) in relation to lower respiratory tract infections among under-five children in Ibadan, Nigeria: the study protocol. Int J Environ Res Public Health. 2020;17(6):1857. doi: 10.3390/ijerph17061857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zeldin DC, Eggleston P, Chapman M, Piedimonte G, Renz H, Peden D. How exposures to biologics influence the induction and incidence of asthma. Environ Health Perspect. 2006;114(4):620–626. doi: 10.1289/ehp.8379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med. 1995;332(3):133–8. doi: 10.1056/NEJM199501193320301. [DOI] [PubMed] [Google Scholar]
- 30.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration; 2011. Available from www.cochrane-handbook.org.
- 32.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Canada: Ottawa Hospital Research Institute; 2014. [Google Scholar]
- 33.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 34.The Cochrane Collaboration . Review Manager (RevMan) [Computer program]. Version 5.3. ed The Nordic Cochrane Centre. Copenhagen: The Cochrane Collaboration; 2014. [Google Scholar]
- 35.Gent JF, Ren P, Belanger K, Triche E, Bracken MB, Holford TR, et al. Levels of household mold associated with respiratory symptoms in the first year of life in a cohort at risk for asthma. Environ Health Perspect. 2002;110(12):A781–A786. doi: 10.1289/ehp.021100781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosenbaum PF, Crawford JA, Anagnost SE, Wang CJ, Hunt A, Anbar RD, et al. Indoor airborne fungi and wheeze in the first year of life among a cohort of infants at risk for asthma. J Expo Sci Environ Epidemiol. 2010;20(6):503–515. doi: 10.1038/jes.2009.27. [DOI] [PubMed] [Google Scholar]
- 37.Horick N, Weller E, Milton DK, Gold DR, Li R, Spiegelman D. Home endotoxin exposure and wheeze in infants: correction for bias due to exposure measurement error. Environ Health Perspect. 2006;114(1):135–140. doi: 10.1289/ehp.7981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Park JH, Gold DR, Spiegelman DL, Burge HA, Milton DK. House dust endotoxin and wheeze in the first year of life. Am J Respir Crit Care Med. 2001;163(2):322–328. doi: 10.1164/ajrccm.163.2.2002088. [DOI] [PubMed] [Google Scholar]
- 39.Harley KG, Macher JM, Lipsett M, Duramad P, Holland NT, Prager SS, et al. Fungi and pollen exposure in the first months of life and risk of early childhood wheezing. Thorax. 2009;64(4):353–358. doi: 10.1136/thx.2007.090241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Litonjua AA, Milton DK, Celedon JC, Ryan L, Weiss ST, Gold DR. A longitudinal analysis of wheezing in young children: the independent effects of early life exposure to house dust endotoxin, allergens, and pets. J Allergy Clin Immunol. 2002;110(5):736–742. doi: 10.1067/mai.2002.128948. [DOI] [PubMed] [Google Scholar]
- 41.Campo P, Kalra HK, Levin L, Reponen T, Olds R, Lummus ZL, et al. Influence of dog ownership and high endotoxin on wheezing and atopy during infancy. J Allergy Clin Immunol. 2006;118(6):1271–1278. doi: 10.1016/j.jaci.2006.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gillespie J, Wickens K, Siebers R, Howden-Chapman P, Town I, Epton M, et al. Endotoxin exposure, wheezing, and rash in infancy in a New Zealand birth cohort. J Allergy Clin Immunol. 2006;118(6):1265–1270. doi: 10.1016/j.jaci.2006.07.051. [DOI] [PubMed] [Google Scholar]
- 43.Perzanowski MS, Miller RL, Thorne PS, Barr RG, Divjan A, Sheares BJ, et al. Endotoxin in inner-city homes: associations with wheeze and eczema in early childhood. J Allergy Clin Immunol. 2006;117(5):1082–1089. doi: 10.1016/j.jaci.2005.12.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karvonen AM, Hyvarinen A, Gehring U, Korppi M, Doekes G, Riedler J, et al. Exposure to microbial agents in house dust and wheezing, atopic dermatitis and atopic sensitization in early childhood: a birth cohort study in rural areas. Clin Exp Allergy. 2012;42(8):1246–1256. doi: 10.1111/j.1365-2222.2012.04002.x. [DOI] [PubMed] [Google Scholar]
- 45.Biagini JM, LeMasters GK, Ryan PH, Levin L, Reponen T, Bernstein DI, et al. Environmental risk factors of rhinitis in early infancy. Pediatr Allergy Immunol. 2006;17(4):278–284. doi: 10.1111/j.1399-3038.2006.00386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bolte G, Bischof W, Borte M, Lehmann I, Wichmann HE, Heinrich J. Early endotoxin exposure and atopy development in infants: results of a birth cohort study. Clin Exp Allergy. 2003;33:770–6. doi: 10.1046/j.1365-2222.2003.01665.x. [DOI] [PubMed] [Google Scholar]
- 47.Douwes J, van Strien R, Doekes G, Smit J, Kerkhof M, Gerritsen J, et al. Does early indoor microbial exposure reduce the risk of asthma? The prevention and incidence of asthma and mite allergy birth cohort study. J Allergy Clin Immunol. 2006;117(5):1067–1073. doi: 10.1016/j.jaci.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 48.Phipatanakul W, Celedon JC, Sredl DL, Weiss ST, Gold DR. Mouse exposure and wheeze in the first year of life. Ann Allergy Asthma Immunol. 2005;94(5):593–599. doi: 10.1016/S1081-1206(10)61139-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stark PC, Burge HA, Ryan LM, Milton DK, Gold DR. Fungal levels in the home and lower respiratory tract illnesses in the first year of life. Am J Respir Crit Care Med. 2003;168(2):232–237. doi: 10.1164/rccm.200207-730OC. [DOI] [PubMed] [Google Scholar]
- 50.Matheson MC, Abramson MJ, Dharmage SC, Forbes AB, Raven JM, Thien FC, et al. Changes in indoor allergen and fungal levels predict changes in asthma activity among young adults. Clin Exp Allergy. 2005;35(7):907–913. doi: 10.1111/j.1365-2222.2005.02272.x. [DOI] [PubMed] [Google Scholar]
- 51.Antova T, Pattenden S, Brunekreef B, Heinrich J, Rudnai P, Forastiere F, et al. Exposure to indoor mould and children’s respiratory health in the PATY study. J Epidemiol Community Health. 2008;62(8):708–714. doi: 10.1136/jech.2007.065896. [DOI] [PubMed] [Google Scholar]
- 52.Desoubeaux G, Cray C. Animal models of aspergillosis. Comp Med. 2018;68(2):109–123. [PMC free article] [PubMed] [Google Scholar]
- 53.Reponen T, Seo SC, Grimsley F, Lee T, Crawford C, Grinshpun SA. Fungal fragments in moldy houses: a field study in homes in New Orleans and Southern Ohio. Atmos Environ. 2007;41(37):8140–8149. doi: 10.1016/j.atmosenv.2007.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Korpi A, Jarnberg J, Pasanen AL. Microbial volatile organic compounds. Crit Rev Toxicol. 2009;39(2):139–193. doi: 10.1080/10408440802291497. [DOI] [PubMed] [Google Scholar]
- 55.Moularat S, Robine E, Ramalho O, Oturan MA. Detection of fungal development in a closed environment through the identification of specific VOC: demonstration of a specific VOC fingerprint for fungal development. Sci Total Environ. 2008;407(1):139–146. doi: 10.1016/j.scitotenv.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 56.Wong J, Magun BE, Wood LJ. Lung inflammation caused by inhaled toxicants: a review. Int J Chron Obstruct Pulmon Dis. 2016;11:1391–1401. doi: 10.2147/COPD.S106009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zock JP, Heinrich J, Jarvis D, Verlato G, Norback D, Plana E, et al. Distribution and determinants of house dust mite allergens in Europe: the European Community Respiratory Health Survey II. J Allergy Clin Immunol. 2006;118(3):682–690. doi: 10.1016/j.jaci.2006.04.060. [DOI] [PubMed] [Google Scholar]
- 58.Caillaud D, Evrard B, Laurichesse H, Souweine B. Role of indoor endotoxins in asthma symptoms. Rev Mal Respir. 2009;26(8):893–899. doi: 10.1016/S0761-8425(09)73684-8. [DOI] [PubMed] [Google Scholar]
- 59.Thorne PS, Mendy A, Metwali N, Salo P, Co C, Jaramillo R, et al. Endotoxin exposure: predictors and prevalence of associated asthma outcomes in the United States. Am J Respir Crit Care Med. 2015;192(11):1287–1297. doi: 10.1164/rccm.201502-0251OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vogelberg C. Preschool children with persistent asthmatic symptoms. Ther Clin Risk Manag. 2019;15:451–460. doi: 10.2147/TCRM.S170979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Brand PL, Baraldi E, Bisgaard H, Boner AL, Castro-Rodriguez JA, Custovic A, et al. Definition, assessment and treatment of wheezing disorders in preschool children: an evidence-based approach. Eur Respir J. 2008;32(4):1096–1110. doi: 10.1183/09031936.00002108. [DOI] [PubMed] [Google Scholar]
- 62.Martinez FD. Development of wheezing disorders and asthma in preschool children. Pediatrics. 2002;109(2):362–367. [PubMed] [Google Scholar]
- 63.Schultz A, Devadason SG, Savenije OE, Sly PD, Le Souëf PN, Brand PL. The transient value of classifying preschool wheeze into episodic viral wheeze and multiple trigger wheeze. Acta Paediatr. 2010;99(1):56–60. doi: 10.1111/j.1651-2227.2009.01508.x. [DOI] [PubMed] [Google Scholar]
- 64.van Aalderen WM. Childhood asthma: diagnosis and treatment. Scientifica. 2012;2012:674204. doi: 10.6064/2012/674204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Beasley R, Semprini A, Mitchell EA. Risk factors for asthma: is prevention possible? Lancet. 2015;386(9998):1075–1085. doi: 10.1016/S0140-6736(15)00156-7. [DOI] [PubMed] [Google Scholar]
- 66.Kravitz-Wirtz N, Teixeira S, Hajat A, Woo B, Crowder K, Takeuchi D. Early-life air pollution exposure, neighborhood poverty, and childhood asthma in the United States, 1990-2014. Int J Environ Res Public Health. 2018;15(6):1114. doi: 10.3390/ijerph15061114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fakunle AG, Jafta N, Okekunle AP, Naidoo RN. Indoor microbiome and risk of lower respiratory tract infections among children under-five years: a meta-analysis. Indoor Air. 2020;30(5):795–804. doi: 10.1111/ina.12698. [DOI] [PubMed] [Google Scholar]
- 68.Prussin AJ, 2nd, Garcia EB, Marr LC. Total virus and bacteria concentrations in indoor and outdoor air. Environ Sci Technol Lett. 2015;2(4):84–88. doi: 10.1021/acs.estlett.5b00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Prussin AJ, Torres PJ, Shimashita J, Head SR, Bibby KJ, Kelley ST, et al. Seasonal dynamics of DNA and RNA viral bioaerosol communities in a daycare center. Microbiome. 2019;7(1):53. doi: 10.1186/s40168-019-0672-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Blachere FM, Lindsley WG, Pearce TA, Anderson SE, Fisher M, Khakoo R, et al. Measurement of airborne influenza virus in a hospital emergency department. Clin Infect Dis. 2009;48(4):438–440. doi: 10.1086/596478. [DOI] [PubMed] [Google Scholar]
- 71.Sordillo J, Hoffman PE, Celedon J, Litonjua A, Milton D, Gold D. Multiple microbial exposures in the home may protect against asthma or allergy in childhood. Clin Exp Allergy. 2010;40:902–10. doi: 10.1111/j.1365-2222.2010.03509.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ober C, Vercelli D. Gene-environment interactions in human disease: nuisance or opportunity? Trends Genet. 2011;27(3):107–115. doi: 10.1016/j.tig.2010.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mendy A, Gasana J, Vieira ER, Forno E, Patel J, Kadam P, et al. Endotoxin exposure and childhood wheeze and asthma: a meta-analysis of observational studies. J Asthma. 2011;48(7):685–693. doi: 10.3109/02770903.2011.594140. [DOI] [PubMed] [Google Scholar]
- 74.Gehring U, Strikwold M, Schram-Bijkerk D, Weinmayr G, Genuneit J, Nagel G, et al. Asthma and allergic symptoms in relation to house dust endotoxin: phase two of the International Study on Asthma and Allergies in Childhood (ISAAC II) Clin Exp Allergy. 2008;38(12):1911–1920. doi: 10.1111/j.1365-2222.2008.03087.x. [DOI] [PubMed] [Google Scholar]
- 75.Lawson JA, Dosman JA, Rennie DC, Beach J, Newman SC, Senthilselvan A. Relationship between indoor environment and asthma and wheeze severity among rural children and adolescents. J Agromedicine. 2009;14(2):277–285. doi: 10.1080/10599240902772910. [DOI] [PubMed] [Google Scholar]
- 76.Lai PS, Sheehan WJ, Gaffin JM, Petty CR, Coull BA, Gold DR, et al. School endotoxin exposure and asthma morbidity in inner-city children. Chest. 2015;148(5):1251–1258. doi: 10.1378/chest.15-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Thorne PS, Kulhánková K, Yin M, Cohn R, Arbes SJ, Jr, Zeldin DC. Endotoxin exposure is a risk factor for asthma: the national survey of endotoxin in United States housing. Am J Respir Crit Care Med. 2005;172(11):1371–1377. doi: 10.1164/rccm.200505-758OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Carnes MU, Hoppin JA, Metwali N, Wyss AB, Hankinson JL, O’Connell EL, et al. House dust endotoxin levels are associated with adult asthma in a U.S. farming population. Ann Am Thorac Soc. 2017;14(3):324–31. doi: 10.1513/AnnalsATS.201611-861OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kanchongkittiphon W, Mendell MJ, Gaffin JM, Wang G, Phipatanakul W. Indoor environmental exposures and exacerbation of asthma: an update to the 2000 review by the Institute of Medicine. Environ Health Perspect. 2015;123(1):6–20. doi: 10.1289/ehp.1307922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Celedón JC, Milton DK, Ramsey CD, Litonjua AA, Ryan L, Platts-Mills TA, et al. Exposure to dust mite allergen and endotoxin in early life and asthma and atopy in childhood. J Allergy Clin Immunol. 2007;120(1):144–149. doi: 10.1016/j.jaci.2007.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gereda JE, Leung DY, Thatayatikom A, Streib JE, Price MR, Klinnert MD, et al. Relation between house-dust endotoxin exposure, type 1 T-cell development, and allergen sensitisation in infants at high risk of asthma. Lancet. 2000;355(9216):1680–1683. doi: 10.1016/S0140-6736(00)02239-X. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Quality Assessment of studies included in the meta-analysis using the Newcastle-Ottawa Scaling. Table S2. Leave-one-out sensitivity Analysis of pooled effect estimates of studies included in the meta-analysis. Figure S1. Funnel plots with pseudo-95% confidence limit for any IM exposure and wheeze among U-5C (A); TFC and wheeze (B); Aspergillus spp. and wheeze (C); Penicillium spp. and wheeze (D); Cladosporium spp and wheeze (E); Endotoxin and wheeze (F). Figure S2. Funnel plots with pseudo-95% confidence limit for any IM exposure and allergic rhinitis among U-5C (A); visible mold and allergic rhinitis (B); Endotoxin and allergic rhinitis (C). Figure S3. Funnel plots with pseudo-95% confidence limit for any IM exposure/endotoxin and asthma among U-5C.
Data Availability Statement
All data generated or analysed during this study are included in this published article and its additional files.