The year 1754 was decisive for understanding the development of the placental circulation. In May of that year, John Hunter and Colin Mackenzie, both surgeons and anatomists of Scottish origin, carried out an experiment that established the basis of modern concepts of the maternal–fetal interrelationship before birth. By injecting melted wax into the uterine and umbilical arteries of hysterectomy specimens with placenta in situ, they demonstrated that maternal and fetal circulations are separated, thus putting to rest a debate that had divided anatomists, including Galen, Da Vinci and Vesalius, for many centuries (Jaffe et al. AJOG 1997;176:695–705).
More than 200 years later, Boyd and Hamilton from Cambridge, investigating 151 hysterectomy specimens with placenta in situ, including some injected with coloured gelatine or India ink, using a similar technique to that described by Hunter and Mackenzie (J Obstet Gynaecol Br Commonw 1967;74:161–226), were the first to describe in detail the development and structure of the human placenta from the end of the first trimester of gestation. Inspired by their work, Hustin and Schaaps (AJOG 1987;157:162–8), using ultrasound imaging, direct vision chorionic biopsy and hysterectomy specimens with a placenta in situ, showed that the intervillous circulation is limited by the cytotrophoblastic plugs in the tips of the spiral arteries during the first trimester. The plugging of the spiral arteries restricts exposure of the fetus to oxygen (O2) and creates a utero‐placental O2 gradient which exerts a regulatory effect on placental tissue development and function (Jauniaux et al. Placenta 2003;24:s86–93). The premature opening of the intervillous circulation leading to excessive intraplacental oxidative stress is the main mechanism of early pregnancy failure in humans (Jauniaux et al. Am J Pathol 2000;157:2111–22).
Modern ultrasound imaging including colour‐Doppler imaging and 3D ultrasound has enabled us to investigate in vivo both placental circulations in normal pregnancies and pregnancies complicated by placenta‐related disorders (Figure 1). Measuring trophoblast volume at 6–12 weeks’ gestational age is now possible with 3D‐ultrasound and the off‐line VOCAL technique. Maternal placental bed vascular volume (PBVV; arcuate‐, radial‐, basal and spiral arteries) and fetal vascular volume (FVV; fetal‐, umbilical‐ and villous vasculature) have been measured using 3D power Doppler (3D‐PD) in combination with 3D‐virtual reality (VR) at 12 weeks’ gestational age (Reus et al. Ultrasound Med Biol 2014;40:1796–803). Automated image processing in 3D‐PD recordings has enabled quantification of spiral artery blood flow between 11 and 13 weeks’ gestational age at 2–5 mm from the utero‐placental interface (Stevenson et al. Ultrasound Med Biol 2018;44;522–31). Detailed 3D‐PD‐VR enables vascular volume measurements preconceptionally and at 7, 9 and 11 weeks’ gestational age (Reijnders et al. Placenta 2018;61:96–102).
Figure 1.
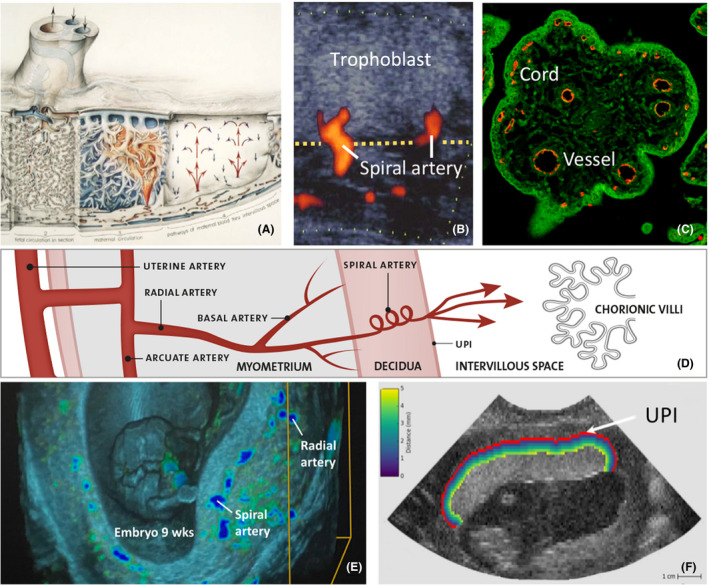
(A) Classic drawing of the placenta by Ranice W. Crosby, showing structure and circulation, based on Elisabeth Ramsey's work. (B) Spiral artery jet entering the intervillous space from the utero‐placental interface (yellow line; UPI) at 15 weeks’ pregnancy. (C) Confocal microscopy section of a 9‐week villus with CD31‐stained vessels and cords (Lisman et al. Human Reprod 2007). (D) Detailed drawing of arcuate‐, radial‐ and spiral arteries. (E) 3D‐VR image of spiral‐ and radial arteries at the UPI of a 9‐week pregnancy. (F) Area of interest used in automated 3D power Doppler fractional moving blood volume measurements from the whole UPI to 5 mm in the intervillous space (Collins et al. Plos One 2017;12:e0178675).
Recently, it has been shown that larger first‐trimester placental volume (VOCAL) and utero‐placental vascular volume (3D‐PD‐VR) are associated with lower pressure and more flow‐mediated vasodilatation of the feto‐placental vasculature after delivery (Hitzerd et al. Front Physiol 2020;11:6). If only Boyd and Hamilton could have seen what progress in diagnostic imaging their findings would lead to.
Disclosure of interests
None declared. Completed disclosure of interests forms are available to view online as supporting information.
Supporting information
Supplementary Material
Supplementary Material
Supplementary Material
Data availability statement
All data used are available in PubMed.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Supplementary Material
Supplementary Material
Data Availability Statement
All data used are available in PubMed.


