Abstract
Background:
Although effective treatments exist, alcohol use disorder (AUD) is undertreated. We used a cascade of care framework to understand gaps in care for persons with AUD.
Methods:
Using 2015–2019 National Survey on Drug Use and Health data, we evaluated the following steps in the cascade of care: 1) adult prevalence of AUD; 2) proportion of adults with AUD who utilized health care in the past 12 months; 3) proportion with AUD screened about their alcohol use; 4) proportion with AUD who received a brief intervention about their alcohol misuse; 5) proportion with AUD who received information about treatment for alcohol misuse; and 6) proportion with AUD who received treatment. Analyses were stratified by AUD severity.
Results:
Of the 214,505 persons included in the sample, weighted prevalence of AUD was 7.8% (95% CI 7.6–8.0%). Cascades of care showed the majority of individuals with AUD utilized health care and were screened about alcohol use, but only a minority received subsequent steps of care: 81.4% (95% CI 80.7%−82.1%) of persons with AUD utilized health care in the past 12 months and 69.9% (95% CI 68.9–70.8%) reported being screened about alcohol use, but 11.6% (95% CI 11.0–12.2%) reported receiving a brief intervention, 5.1% (95% CI 4.6–5.6%) were referred to treatment, and 5.8% (95% CI 5.4–6.3%) received treatment. Similar patterns were observed when cascades of care were stratified by AUD severity.
Conclusions:
Persons with AUD utilize health care and are screened about alcohol use with high prevalence, but few receive treatment. Health care settings- particularly primary care settings- represent a prime opportunity to implement AUD treatment to improve outcomes in this high-risk population.
Keywords: alcohol use disorder, cascade of care, alcohol use screening, evidence-based treatment
INTRODUCTION
Alcohol use disorder (AUD) is one of the most prevalent substance use disorders (SUDs) in the world. An estimated 93,000 people die of alcohol-related causes in the United States each year (Esser et al., 2020), and alcohol-related deaths are one of the leading causes of preventable death (Mokdad et al., 2004, U.S. Burden of Disease Collaborators, 2013). Of particular concern, mortality associated with AUD has increased in recent years (Case and Deaton, 2017, Spillane et al., 2020).
Importantly, effective treatments for AUD exist. Evidence-based psychotherapy interventions, including motivational interviewing, cognitive behavioral therapy, and contingency management improve outcomes in persons with AUD (Carvalho et al., 2019, Knox et al., 2019), as does Alcoholics Anonymous (Kelly et al., 2020). In addition, there are three Food and Drug Administration (FDA)-approved medications for treatment of AUD–naltrexone (available in oral and extended-release depot formulations), acamprosate, and disulfiram. Naltrexone and acamprosate in particular have been shown to improve duration of sobriety, and naltrexone has also been shown to decrease number of heavy drinking days (Jonas et al., 2014). Given their demonstrated efficacy, pharmacotherapy with either naltrexone or acamprosate is considered first-line treatment for persons with moderate or severe AUD (Kranzler and Soyka, 2018). Despite the efficacy of AUD treatments, however, prevalence of treatment remains low: Fewer than 10% of persons with AUD receive treatment (Substance Abuse and Mental Health Services Administration, 2020). This significant implementation gap in AUD treatment highlights the need for an improved understanding of barriers to treatment.
A cascade of care model is a useful framework for identifying gaps in a care trajectory for illnesses. First developed in response to the HIV/AIDS epidemic (Gardner et al., 2011), a cascade of care tracks the proportion of the population of interest engaged in each step of a care continuum including diagnosis, engagement in medical care, receipt of treatment, retention in care and remission of disease (U.S. Department of Health & Human Services, 2020). A cascade of care framework has been adopted for other chronic diseases (Thomas, 2020, Prabhakar and Kwo, 2019, Kazemian et al., 2019), including opioid use disorder (Williams et al., 2019), to illustrate where gaps in care occur so that interventions can be targeted with the ultimate goal of decreasing mortality and improving disease outcomes. Constructing a cascade of care for AUD can therefore serve as a helpful tool to visualize gaps in the care continuum so that interventions to mitigate identified gaps can be appropriately targeted.
An important first step in an AUD care cascade is an understanding prevalence of AUD, for which nationally-representative data are needed. The National Survey of Drug Use and Health (NSDUH), conducted annually by the Substance Abuse and Mental Health Services Administration, is routinely used by both researchers and policy makers for determining prevalence of AUD (National Institute on Alcohol Abuse and Alcoholism, 2021, Kranzler and Soyka, 2018, Substance Abuse and Mental Health Services Administration, 2020), and thus is a particularly important data source for this purpose. As health care providers play critical roles in the identification and diagnosis of persons with AUD, characterizing health care utilization patterns of persons with AUD is an important second step in the care cascade.
The screening, brief intervention, and referral to treatment (SBIRT) framework also informs the cascade construction for AUD. Since 1996, the U.S. Preventative Services Task Force (USPSTF) has recommended that physicians universally screen adult patients for alcohol misuse in health care settings and provide brief intervention for those with problem drinking (Bazzi and Saitz, 2018). There are several well-validated screening tools for alcohol misuse that can be incorporated easily into health care settings (Bohn et al., 1995, Bush et al., 1998, Steinweg and Worth, 1993). Brief interventions generally consist of one or more brief counseling sessions with a health care provider and can include education about a patient’s drinking patterns relative to recommended guidelines, long-term sequelae of heavy drinking, and advice on how to minimize or stop alcohol use completely (Fleming, 2004, O’Connor et al., 2018). These combined efforts–screening with brief intervention–are effective at decreasing self-reported problematic drinking among those with heavy drinking or milder forms of AUD (Moyer et al., 2002, Willenbring, 2013). However, for those with more severe forms of AUD, screening and brief intervention have been shown to be insufficient (Willenbring, 2013), and more intensive treatment is recommended (Knox et al., 2019, Substance Abuse and Mental Health Services Administration and National Institute on Alcohol Abuse and Alcoholism, 2015, Kranzler and Syoka, 2018). Given that for mild forms of AUD, brief intervention can be an adequate treatment “end step” in the cascade, it is important to stratify cascades by illness severity.
Previous studies have identified gaps in the care of persons with AUD. For example, using data from the 2013 NSDUH, Glass et al. (2016) found that 81% of persons with alcohol dependence who utilized ambulatory care in the past year reported being screened by a health care provider about alcohol use, but far fewer reported receiving subsequent steps in care, with only 25% of respondents indicating that they were advised to cut down on their drinking or received information about treatment. Extending this work to 2013 and 2014 NSDUH data, Bandara et al. (2018) found a similar pattern: most persons with AUD who used ambulatory care reported being screened about alcohol use, but only 6.8% of those with AUD received treatment. This low level of AUD treatment has changed little over past decades (Cohen et al., 2007, Dawson et al., 2005); whether there has been improvement in these gaps in more recent years is an important area of study.
Using data from 2015–2019 NSDUH, we evaluated the following steps in the cascade of care, stratifying our analyses by AUD severity: 1) adult prevalence of AUD; 2) proportion of adults with AUD who utilized health care in the past 12 months and 3) proportion with AUD screened about their alcohol use; 4) proportion with AUD who received a brief intervention about alcohol misuse; 5) proportion with AUD who received information about treatment for alcohol misuse; and 6) proportion with AUD who received treatment.
MATERIALS AND METHODS
Data Source
NSDUH is conducted annually by the Substance Abuse and Mental Health Services Administration to measure substance use patterns in the United States. Respondents are sampled from non-institutionalized, domiciled U.S. citizens aged 12 and older from all 50 states and the District of Columbia. The NSDUH provides nationally representative data on the prevalence and correlates of past-year AUD and includes questions about past-year health care utilization, alcohol screening, brief intervention, and referral to treatment as well as receipt of AUD treatment. Field workers interview participants in person; however, questions about potentially sensitive behaviors, including alcohol use, are administrated via audio-computer-assisted self-interview to maximize confidentiality. Reliability of NSDUH past-year AUD diagnosis has been previously shown to have a kappa statistic of 0.64 (SE=0.06) and past-year alcohol or drug treated has been shown to have a kappa statistic of 0.87 (SE 0.04) (Substance Abuse and Mental Health Services Administration, 2010). We focused our analyses on persons aged 18 years and older. Interview response rates and final sample size per year of data analyzed were as follows: 71.2% and 68,073 for 2015; 68.4% and 67, 942 for 2016; 67.1% and 68,032 for 2017; 66.6% and 67,791 for 2018; and 64.9% and 67,625 for 2019.
The study was exempted from human subjects review by the Institutional Review Board at Washington University School of Medicine.
Cascade of Care Step 1: Prevalence of Mild, Moderate and Severe AUD
NSDUH uses DSM-IV (American Psychiatric Association, 1994) criteria to generate diagnoses for past 12-month alcohol abuse and the more severe alcohol dependence. Under DSM-IV criteria, it is possible to endorse one symptom and meet criteria for alcohol abuse; a diagnosis of alcohol dependence requires endorsement of at least three of seven criteria. DSM-5 criteria (American Psychiatric Association, 2013), which have been used clinically since 2013, removed the distinction between abuse and dependence and instead categorize AUD severity by the number of 11 possible criteria endorsed to define mild, moderate and severe AUD. The NSDUH includes questions that map to 10 of the 11 DSM-5 AUD criteria; cravings for alcohol, which are a criterion of DSM-5, are not assessed in the NSDUH. Using similar methodology to that described by Johnson et al. 2020 (Johnson et al., 2020), we took a DSM-5-like graded severity approach, classifying persons with 0–1 criterion as not having AUD, those with 2–3 criteria as having mild AUD, those with 4–5 criteria as having moderate AUD, and those with 6 or more criteria as having severe AUD. We used DSM-5 criteria to define past 12-month AUD severity for two reasons: DSM-5 is the current diagnostic system in use clinically, and by requiring endorsement of at least two criteria to qualify for AUD, and six criteria to qualify for severe AUD, we increased the likelihood of correctly classifying those with a clinically significant use disorder. Supplementary Table 1 lists variables used to define each of the AUD criteria. There was more than 96% concordance between DSM-5 AUD and DSM-IV alcohol abuse or dependence (Supplementary Table 2). 100% of persons with moderate or severity DSM-5 AUD diagnosis also had a DSM-IV diagnosis of alcohol abuse or dependence; approximately 50% of persons with mild DSM-5 AUD diagnosis also had a DSM-IV alcohol abuse or dependence diagnosis (Supplementary Table 2).
Cascade of Care Step 2: Health Care Utilization
NSDUH includes questions about past 12-month visits to ambulatory care settings, emergency room (ER) visits, and overnight inpatient hospitalizations; specific wording of questions is included in Supplementary Table 3. We recoded questions about utilization of each type of health care into dichotomous “yes”/”no” variables. The variable NMVSOPT2 was used for past 12-month ambulatory care visits, NMERTMT2 was used for past 12-month ER visits, and INHOSPYR was used for past 12-month overnight inpatient hospitalizations. We then created a summary variable denoting whether a participant accessed at least one of these three health care settings in the past 12 months.
Cascade of Care Step 3: Alcohol Screening
Respondents who indicated accessing health care in the past 12 months were asked the following question: “During the past 12 months, did any doctor or other health care professional ask, either in person or on a form, if you drink alcohol?” (variable HPUSEALC). Those who indicated that they had utilized health care and had consumed at least one alcoholic drink in the past 12 months were additionally asked to indicate whether the following happened in the past 12 months: “The doctor asked how much I drink” (variable HPALCAMT); “the doctor asked how often I drink” (variable HPALCFRQ); and “the doctor asked if I have any problems because of my drinking” (variable HPALCPRB). We used similar methodology as Glass et al. (2016) and counted a positive response to any of these four items as indicative of having been screened for alcohol use. We intentionally used this broad definition to maximize sensitivity of our screening variable.
Cascade of Care Step 4: Doctor or other health care professional provided brief intervention for drinking
Those who indicated that they had utilized health care and had consumed at least one alcoholic drink in the past 12 months were asked to indicate whether the following happened in the past 12 months: “The doctor advised me to cut down on my drinking” (variable HPALCCUT). Agreement with this statement was defined as receiving a brief intervention for drinking.
Cascade of Care Step 5: Doctor or other health professional provided referral to treatment
Those who indicated that they had utilized health care and had consumed at least one alcoholic drink in the past 12 months were asked to indicate whether the following happened in the past 12 months: “The doctor offered to give me more information about alcohol use and treatment for problems with alcohol use” (variable HPALCTX). Agreement with this statement was defined as receiving referral to treatment.
Cascade of Care Step 6: AUD Treatment Receipt
Respondents who had consumed at least one alcoholic drink in the past 12 months were asked whether they had received treatment or counseling for use of alcohol or any drug, not including cigarettes, during the past 12 months. Those who answered yes were then asked whether the treatment was for alcohol use only, drug use only, or both alcohol and drug use. NSDUH used these responses to create a recoded dichotomous past 12-month alcohol treatment variable (TXYRALC) with the following responses: “yes” or “no/unknown.” We used this variable in our analyses to define AUD treatment receipt (see Supplementary Table 3).
Analytic Plan
Analyses were conducted using SAS version 9.4 (Cary, NC, USA). To account for NSDUH’s complex sampling design, we applied survey weights created by NSDUH to all analyses so that estimates were representative of the national population. We used descriptive statistics to calculate observed proportions and corresponding confidence intervals for demographic variables, health care utilization patterns, and screening, brief intervention, and referral to treatment patterns. Chi Square statistics were used to examine differences between AUD groups for demographic, health care utilization, SBIRT and treatment variables. As there were no significant differences in key variables of interest (any health care utilization, screening, brief intervention, referral to treatment and treatment) by year, we combined years 2015–2019 for our analyses to improve precision of estimates.
Missing Data
Responses entered as “bad data,” “don’t know,” “refused” or “blank” were treated as missing data.
RESULTS
AUD Prevalence and Sample Demographics
Demographic and clinical characteristics of the sample are presented in Table 1. Among the 214,505 persons included in the sample, the weighted prevalence of AUD as defined by DSM-5 criteria was 7.8% (95% CI 7.6–8.0%). Among those with AUD, mild AUD was most common and severe AUD was least common. As compared to those without AUD, persons with AUD were more likely to have a co-occurring illicit drug use disorder and to have received mental health treatment in the past 12 months. The 1,365 missing responses for past 12-month mental health treatment variable (0.6% of total sample) were not included in analyses; there were no other missing data for demographic variables.
Table 1.
Characteristics associated with past 12-month alcohol use disorder± in the 2015–2019 National Survey of Drug Use and Health.
| No AUD (n=193,235) | All AUD (n=21,270) | Mild AUD (n=14,134) | Moderate AUD (n=4,178) | Severe AUD (n=2,958) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Weighted % (95% CI) | Weighted % (95% CI) | Weighted % (95% CI) | Weighted % (95% CI) | Weighted % (95% CI) | |||||
| Prevalence | 92.2 (92.0–92.4) | 7.8 (7.6–8.0) | 5.2 (5.1–5.3) | 1.6 (1.5–1.7) | 1.1 (1.0–1.1) | ||||
| Past 12-Month AUD Treatment | 0.5 (0.5–0.6) | 5.8 (5.4–6.3) | p <.001 | 2.7 (2.3–3.1) | p <.001 | 6.0 (4.9–7.0) | p <.001 | 20.7 (18.5–22.8) | p <.001 |
| Sex | |||||||||
| Male | 47.1 (46.8–47.5) | 61.3 (60.1–62.5) | p <.001 | 60.6 (59.2–62.1) | p <.001 | 62.8 (60.1–65.5) | p <.001 | 62.2 (59.7–64.7) | p <.001 |
| Female | 52.9 (52.5–53.2) | 38.7 (37.5–39.9) | 37.9 (38.8–40.8) | 37.2 (34.5–39.9) | 37.8 (35.3–40.3) | ||||
| Age | |||||||||
| 18–25 years old | 13.0 (12.8–13.2) | 24.7 (23.9–25.4) | p <.001 | 26.3 (25.6–27.1) | p <.001 | 22.9 (21.4–24.4) | p <.001 | 19.1 (17.6–20.6) | p <.001 |
| 26–34 years old | 15.4 (15.1–15.6) | 23.3 (22.4–24.2) | 22.5 (21.5–23.5) | 23.8 (21.6–26.0) | 26.5 (24.3–28.7) | ||||
| 35–49 years old | 24.6 (24.3–24.9) | 25.1 (24.2–26.0) | 23.4 (22.3–24.4) | 26.7 (24.4–29.1) | 31.2 (28.7–33.7) | ||||
| 50 or older | 47.0 (46.6–47.5) | 26.9 (25.6–28.2) | 27.8 (26.3–29.3) | 26.5 (23.6–29.5) | 23.1 (20.6–25.7) | ||||
| Race/ethnicity | |||||||||
| Non-Hispanic White | 63.7 (63.3–64.3) | 64.9 (63.8–66.1) | p=.002 | 64.3 (62.9–65.7) | p =.025 | 66.8 (64.5–69.1) | p =.005 | 65.1 (62.7–67.5) | p=.188 |
| Non-Hispanic Black | 11.9 (11.5–12.2) | 11.7 (10.9–12.4) | 12.4 (11.7–13.2) | 9.8 (8.5–11.0) | 10.7 (9.2–12.1) | ||||
| Non-Hispanic Other/Multi- Race | 8.3 (8.1–8.6) | 7.1 (6.5–7.8) | 7.1 (6.3–8.0) | 7.1 (5.8–8.3) | 7.2 (6.1–8.4) | ||||
| Hispanic | 16.0 (15.6–16.4) | 16.3 (15.4–17.1) | 16.1 (14.9–17.3) | 16.4 (14.6–18.2) | 17.0 (14.5–19.5) | ||||
| Health Insurance | |||||||||
| Yes | 90.3 (90.1–90.5) | 86.6 (86.0–87.3) | p <.001 | 87.3 (86.5–88.0) | p <.001 | 87.0 (85.4–88.5) | p<.001 | 83.0 (80.9–85.0) | p <.001 |
| Past 12-Month Mental Health Treatment | 14.0 (13.8–14.2) | 25.0 (24.0–26.0) | p <.001 | 21.3 (20.2–22.4) | p <.001 | 28.0 (25.7–30.2) | p <.001 | 38.3 (35.9–40.8) | p <.001 |
| Past 12-month illicit SUD | 2.0 (1.9–2.1) | 12.9 (12.4–13.5) | p <.001 | 9.0 (8.3–9.6) | p <.001 | 16.9 (15.3–18.4) | p <.001 | 26.3 (24.4–28.2) | p <.001 |
Abbreviations: AUD= alcohol use disorder; CI= confidence interval; SUD= substance use disorder.
AUD definition derived from Diagnostic and Statistical Manual of Mental Disorders, 5th Edition diagnostic criteria.
Past 12-Month Health Care Utilization by AUD Severity
There were 4,358 missing responses for past 12-month emergency room visits (2.0% of total sample) and 919 missing responses for past 12-month overnight hospitalizations (0.4% of total sample). These missing data were excluded from health care utilization analyses.
As shown in Table 2, the vast majority of respondents (>80%) reported utilizing at least one of the three health care settings queried, regardless of AUD diagnosis or severity. Those without AUD were statistically significantly more likely to report past 12-month health care utilization than those with AUD, however absolute prevalence differences were smaller than three percent.
Table 2.
Prevalence of past 12-month health care utilization by severity of alcohol use disorder± from 2015–2019 National Survey of Drug Use and Health data.
| No AUD (n=193,235) | Any AUD (n=21,270) | Mild AUD (n=14,134) | Moderate AUD (n=4,178) | Severe AUD (n=2,958) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Weighted % (95% CI) | Weighted % (95% CI) | Weighted % (95% CI) | Weighted % (95% CI) | Weighted % (95% CI) | |||||
| Any Healthcare Utilization | 84.1 (83.9–84.3) | 81.4 (80.7–82.1)*** | 81.3 (80.5–82.1)*** | 80.9 (79.2–82.7)*** | 82.7 (80.5–84.9) | ||||
| Ambulatory Care Visit | 82.6 (82.3–82.8) | 78.8 (78.0–79.5)*** | 79.0 (78.1–79.8)*** | 77.8 (76.1–79.6)*** | 79.1 (76.8–81.5)** | ||||
| Emergency Room Visit | 25.7 (25.3–26.0) | 30.0 (29.2–30.9)*** | 27.8 (26.7–28.9)*** | 30.4 (28.3–32.5)*** | 40.4 (37.4–43.4)*** | ||||
| Overnight Hospitalization | 10.0 (9.8–10.3) | 9.7 (9.0–10.3) | 8.3 (7.6–9.1)* | 9.8 (8.4–11.1) | 16.0 (14.0–17.9)*** |
Abbreviations: AUD= alcohol use disorder; CI=Confidence Interval.
AUD definition derived from Diagnostic and Statistical Manual of Mental Disorders, 5th Edition diagnostic criteria.
p<.05;
p<.001. Reference group for each comparison was “No AUD” group.
Ambulatory care settings were the most commonly accessed health care setting among all groups: more than 75% of persons in each group reported attending an outpatient appointment in the past year, with specific prevalence ranging from 79.1% (95% CI 76.8–81.5%) for persons with severe AUD to 82.6% (95% CI 82.3–82.8%) for persons without AUD. Notably, persons with severe AUD were the most likely of all groups to have used the ER or overnight hospitalization in the past year. Compared to persons without AUD, persons with severe AUD were approximately 60% more likely to have utilized the ER and to have been hospitalized in the past year.
Screening, Brief Intervention, and Referral to Treatment (SBIRT) by AUD Severity
There were 3,871 missing responses for the composite screening variable (1.8% of total sample) and 3,591 missing responses for the brief intervention and referral to treatment variables (1.7% of total sample). Missing responses were excluded from analyses.
Table 3 shows the prevalence of alcohol screening, brief intervention, and referral to treatment among persons who reported utilizing health care in the past year. A majority of respondents reported being screened about alcohol use. The likelihood of being screened increased with AUD severity, ranging from 76.1% (95% CI 75.8%) of those without AUD to 89.8% (95% CI 88.1–91.4%) of those with severe AUD. Brief intervention occurred much less frequently than screening, but also increased with AUD severity, ranging from 1.2% (95% CI 1.1–1.3%) of those without AUD to 28.4% (95% CI 25.0–31.7%) of those with severe AUD. Even fewer respondents with AUD were referred to treatment: 4.3% (95% CI 3.7–5.0%) of those with mild AUD, 7.1% (95% CI 5.9–8.2%) of those with moderate AUD and 15.5% (95% CI 13.3–17.7%) of those with severe AUD reported being given information by their health care provider about AUD treatment. Of note, the 0.6% of persons without AUD who referred to treatment corresponded to a raw prevalence of n=1,211 and an estimated population prevalence of N=1,114,137; the 6.4% of persons referred in the AUD group corresponded to a raw prevalence of n=1,081 and estimated population prevalence of N=986,530.
Table 3.
Prevalence of alcohol screening, brief intervention, and referral to treatment by alcohol use disorder± severity among those who utilized health care in the past 12 months from 2015–2019 National Survey of Drug Use and Health data.
| No AUD (n=156,410) | Any AUD (n=17,095) | Mild AUD (n=11,284) | Moderate AUD (n=3,371) | Severe AUD (n=2,440) | ||||
|---|---|---|---|---|---|---|---|---|
| Weighted % (95% CI) | Weighted % (95% CI) | Weighted % (95% CI) | Weighted % (95% CI) | Weighted % (95% CI) | ||||
| Alcohol Screening | 76.1 (75.8–76.4) | 87.2 (86.5–87.9)*** | 86.2 (85.2–87.2)*** | 88.9 (87.3–90.4)*** | 89.8 (88.1–91.4)*** | |||
| Brief Intervention | 1.2 (1.1–1.3) | 14.6 (13.8–15.4)*** | 10.5 (9.5–11.5)*** | 18.5 (16.9–20.2)*** | 28.4 (25.0–31.7)*** | |||
| Referral to Treatment | 0.6 (0.5–0.6) | 6.4 (5.8–7.0)*** | 4.3 (3.7–5.0)*** | 7.1 (5.9–8.2)*** | 15.5 (13.3–17.7)*** |
Abbreviations: AUD= alcohol use disorder; CI=Confidence Interval.
AUD definition derived from Diagnostic and Statistical Manual of Mental Disorders, 5th Edition diagnostic criteria.
p<.001. Reference group for each comparison was “No AUD” group.
Receipt of Treatment for AUD by AUD Severity
Overall, 5.8% (95% CI 5.4–6.3%) of persons with AUD reported receiving treatment in the past year. As shown in Table 1, prevalence of treatment increased with severity of illness: 2.7% (95% CI 2.3–3.1%) for mild AUD, 6.0% (95% CI 4.9–7.0%) for moderate AUD, and 20.7% (95% CI 18.5–22.8%) for severe AUD.
Cascade of Care for AUD
Figure 1a–d shows the number of people who received each step in a cascade of care for all persons with AUD (Figure 1a), and stratified by mild (Figure 1b), moderate (Figure 1c) and severe (Figure 1d) AUD. For each figure, the weighted prevalence estimates are presented in lieu of the raw sample size to approximate trends on a population level. The estimated number of individuals who completed each step is relative to the baseline prevalence of AUD, not conditional on the number of individuals who completed the previous step. To calculate percentage of the population who completed each step of care relative to the baseline prevalence of AUD, missing data were treated as “no” responses for the cascade figure.
Figure 1a-d.
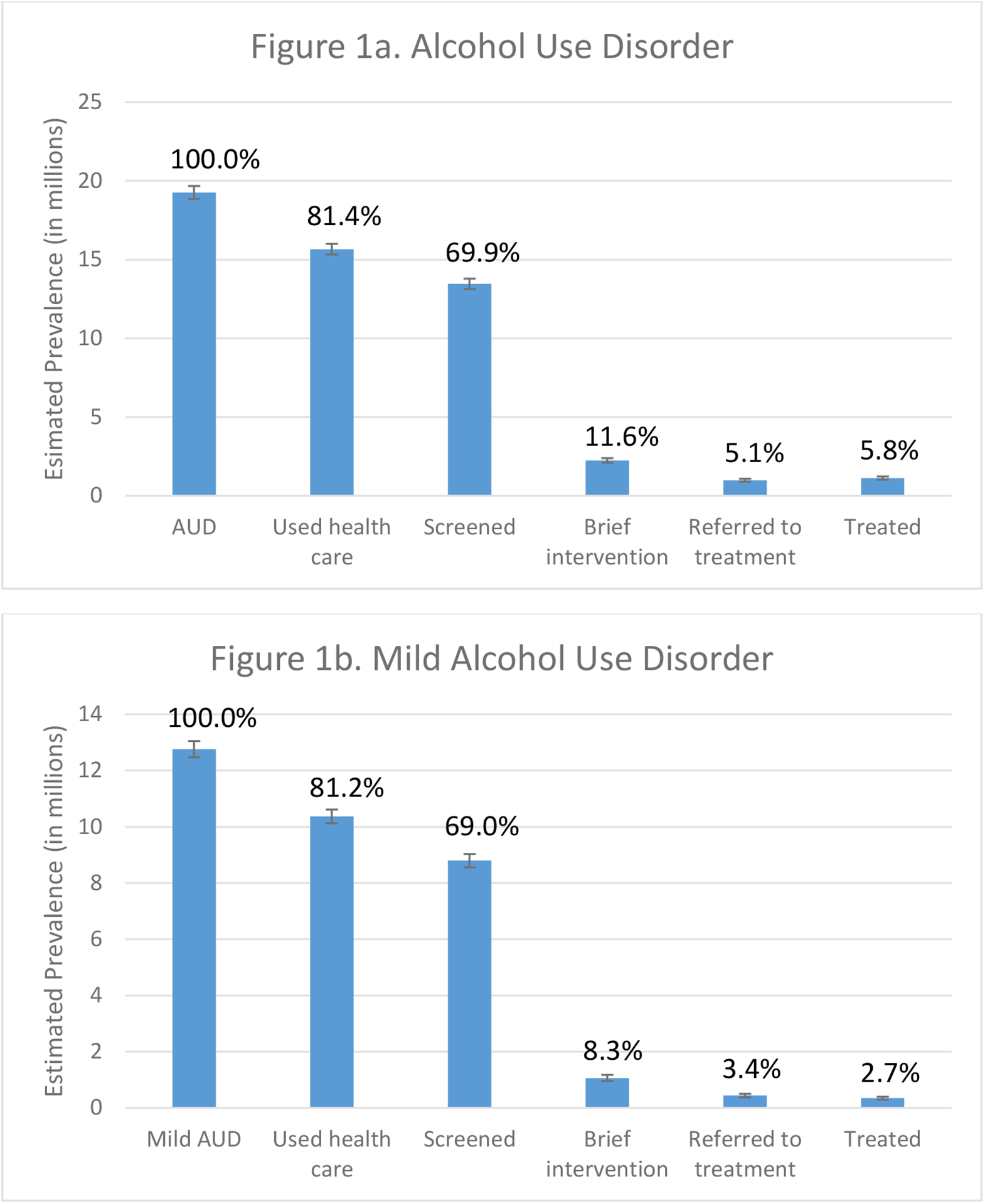
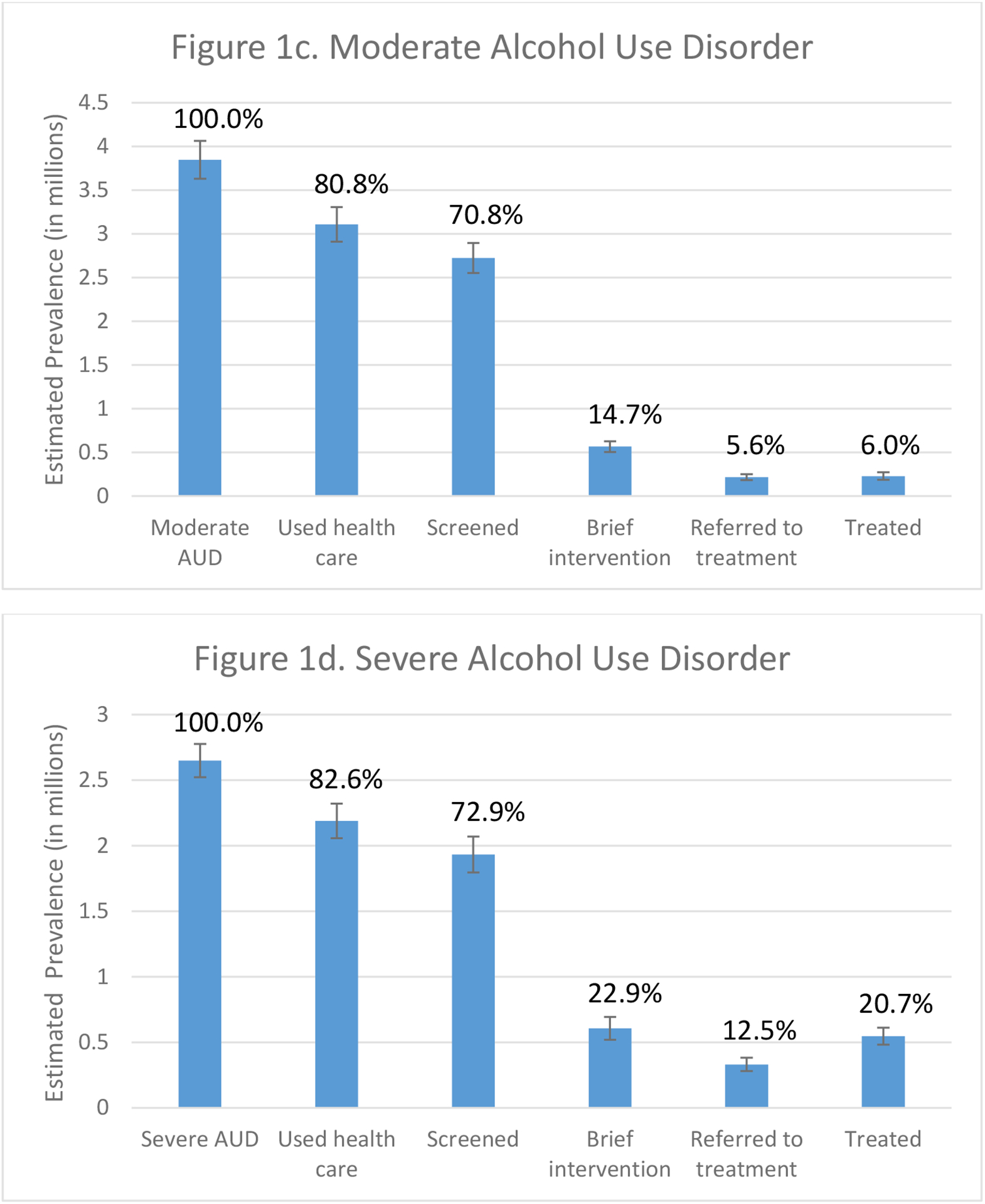
Cascade of care for combined severities (1a), mild (1b), moderate (1c), and severe (1d) alcohol use disorder using data from persons 18 years of age and older from the 2015–2019 National Surveys on Drug Use and Health. All data refer to past-year prevalence. Error bars represent 95% confidence intervals.
Among the estimated 19,251,648 adults with past-year AUD (Figure 1a), 81.4% (95% CI 80.7–82.1%; N=15,662,020) reported utilizing health care in the past 12 months. A majority of those with AUD (69.9%; 95% CI 68.9–70.8%; N=13,452,914) also reported being screened for alcohol use. However, more than 11,000,000 persons with AUD were “lost” from the next step in care: only 11.6% of persons with AUD (95% CI 11.0–12.2%; N=2,236,045) reported being advised to cut down on drinking. Further, only 5.1% (95% CI 4.6–5.6%; N=986,530) reported being referred to treatment. Slightly more persons (5.8%; 95% CI 5.4–6.3%; N=1,121,837) received treatment than who were referred to treatment.
Similar patterns were observed within each AUD severity group: the majority of people utilized health care and were screened about alcohol use, but the proportion who received subsequent steps of care decreased substantially. The proportion of individuals who fell off the care continuum from alcohol screening to brief intervention was greatest for persons with mild AUD (Figure 1b). For moderate and severe AUD, more people received treatment than who were referred to treatment (Figures 1c and 1d). In addition, an estimated 21.3% (95% CI 10.3–32.2%) of persons with moderate AUD, and approximately 8.3% (95% CI 5.5–11.3%) of persons with severe AUD who received treatment in the past year reported they had not utilized health care in the past year.
DISCUSSION
Individuals with AUD are woefully untreated. Using a cascade of care framework, we observed that this lack of treatment was not because individuals with AUD were unlinked to health care: Over 80% of individuals with AUD utilized health care in the past 12 months, and did so at similar rates as those without AUD. In addition, the magnitude of the observed treatment gap was not due to a lack of health care providers screening about alcohol use: over 85% of persons with AUD who used health care reported being asked about alcohol use by a health care professional. Thus, the high utilization of health care by individuals with AUD and the frequent screening for alcohol use during health care visits in the past 12 months presents the opportunity for widespread access to evidence-based AUD care.
However, despite the prevalence of health care utilization and alcohol screening, we found that the subsequent steps in the cascade of care were grossly underutilized, reiterating previous findings of large quality in care gaps for AUD (Bandara et al., 2018, Glass et al., 2016), and indicating these gaps have not improved in recent years (Dawson et al., 2005, Cohen et al., 2007). Stratifying our analyses by DSM-5 criteria allowed us to extend previous studies’ findings and investigate patterns of gaps by disease severity. Gaps observed for severe AUD are particularly alarming and point to suboptimal care of a high-risk population. Those with severe AUD frequently have comorbid illnesses, and in our analyses they were significantly more likely to utilize the most expensive health care settings: emergency rooms and inpatient hospitalizations. Yet, even among this high-acuity group, only 21% reported receiving any AUD treatment in the past 12 months. The low prevalence of AUD treatment is especially striking when compared to treatment rates for other chronic diseases: indeed, recent cascade of care models for HIV and diabetes indicate that 65% of persons with HIV (HIV.gov, 2021) and 94% of persons with diabetes (Kazemian et al., 2019) receive treatment for their respective illnesses.
Our results add further support to the finding that pharmacologic treatment for moderate and severe AUD is underutilized given its documented efficacy (Jonas et al., 2014). Though we were not able to identify the prevalence of pharmacologic treatment for AUD in the current study for our time period of interest (prior to 2019, NSDUH did not contain questions about specific type of AUD treatment other than self-help groups), only 6% of those with moderate AUD and 21% of those with severe AUD reported receiving any treatment, which provides a ceiling for the frequency of pharmacologic treatment in this serously ill group. Previous studies have found that even when AUD is documented in the medical record and thus theoretically known to the the provider, fewer than 10% of persons with AUD receive pharmacologic treatment (Hallgren et al., 2020, Harris et al., 2010). Given the known mortality associated with severe AUD (Laramee et al., 2015), this consistent low proportion of individuals with severe AUD who receive efficacious treatment, and particularly pharmacologic treatment, is disconcerting.
The cascades of care constructed for less severe forms of AUD also showed dramatic implementation gaps. In particular, only 8% of persons with mild AUD reported receiving a brief intervention about alcohol misuse. As persons with mild AUD are most likely to potentially benefit from brief intervention without additional intervention, our findings demonstrate an disporportionate underutilization of an effective tool for this population. In addition, it is notable that while the 6% relative prevalence of persons with AUD referred to treatment was, as expected, substantially larger than the 0.5% relative prevalence of persons without AUD, the absolute prevlaence estimates showed that fewer people with AUD were referred to treatment than persons without AUD (986,530 versus 1,114,137, respectively). This pattern has been previously observed (Glass et al., 2016) and likely reflects that a substantial number of persons who may not carry a formal diagnosis of AUD but engage in drinking patterns that are sufficiently problematic that a health care provider thinks AUD treatment would be beneficial.
The implementation gap between health care screening for alcohol misuse and receipt of treatment highlights the fact that AUD treatment has historically been separated from mainstream health care settings and instead delivered via specialty care settings, including rehabilitation facilities, mental health centers, and non-health care settings such as peer support groups. Referral to specialized AUD treatment is an established approach in health care systems, and this approach is generally favorably viewed by health care providers who may prefer to refer patients to an expert rather than deliver AUD treatment themselves. Yet, this referral approach has significant drawbacks; chief among these is the low frequency with which individuals are successfully linked to treatment.
We therefore advocate for increased engagement of this high-risk population by implementing evidence-based treatment in the primary care setting. Primary care can be an effective setting for team-based AUD treatment at the-point-of-care, facilitated by electronic health records, and this approach has constituted a highly promising model for smoking cessation and opioid use disorder treatment (Ramsey et al., 2020, Ramsey et al., 2019a, Krantz and Mehler, 2004, National Institute on Drug Abuse, 2018, Gunderson and Fiellin, 2008). This model may involve a team approach, with medical assistants or nurses conducting alcohol use assessment on every patient who presents for care facilitated by a prompt from the electronic health record, and providing brief advice about at risk alcohol use to those with problematic drinking, and nurses queuing an AUD medication order for the physician to prescribe. The physician can also provide further advice and encouragement and referral to further specialized treatment if indicated. The most commonly accessed health care setting reported by persons with AUD in our study was the ambulatory care setting, further underscoring its importance as a critical potential leverage point for providing AUD treatment (Knox et al., 2019, Jonas et al., 2014, Anton et al., 2006, Grucza et al., 2020, McNeely et al., 2018). Similar to other chronic illnesses, persons with severe AUD may also require specialized care, particularly for acute exacerbations; however, the need for specialty treatment should not preclude initiating pharmacologic treatment for many patients with AUD in mainstream health care settings.
Thus a proposed conceptual cascade for AUD treatment—with fewer opportunities for leakage from care—is illustrated in Figure 2, as are potential barriers to completion of each step. Different barriers may play roles at each point in the cascade of care (e.g., lack of insurance may prevent utilization of health care; stigma may affect a physician’s likelihood of asking about alcohol use). Possible barriers to the largest observed leakage point in our cascade- from being asked about alcohol use to getting treatment for AUD—are many. Stigma associated with AUD from both patient and clinician perspectives has been cited multiple times as a barrier to treatment (Willenbring, 2013); we argue that the separation of AUD treatment from mainstream health care settings has contributed to this stigma. It is notable that approximately 10% of persons with severe AUD and 20% of persons with moderate AUD who received treatment indicated they had not utilized health care in the past year, suggesting individuals with moderate and severe AUD are finding their way to treatment through avenues other than the medical system. While reasons for this finding are likely multifactorial, the historic separation of SUD treatment from mainstream health care may be a contributing factor. In addition, physician time constraints and lack of knowledge about AUD treatment have also been cited as barriers (Rahm et al., 2015). As our group has observed for smoking cessation, there may also be a disconnect between physician and patient perspectives about the patient’s desire for care (Ramsey et al., 2019b). Whether this disconnect exists for AUD is an important area for future research.
Figure 2.
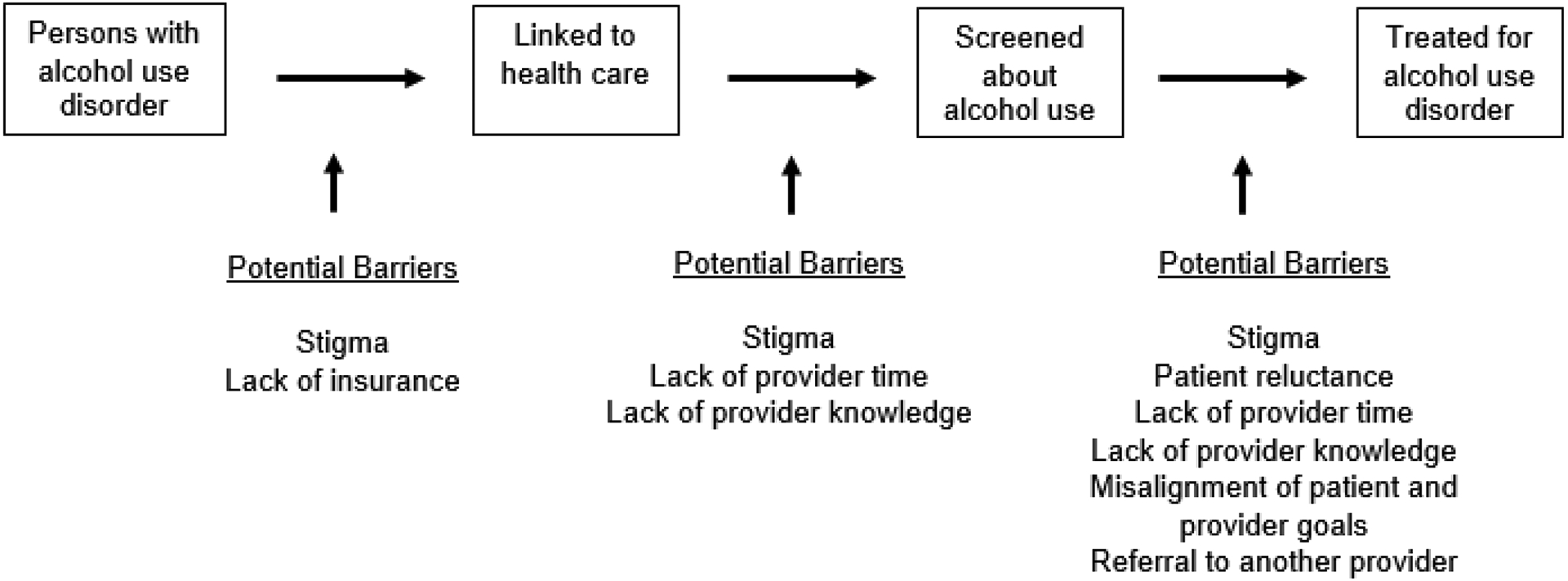
Conceptual model of cascade of care for alcohol use disorder.
LIMITATIONS
As with all studies, there are limitations to this work. Our study was cross-sectional, preventing the determination of temporal relations and causal inference. NSDUH does not sample those who are institutionalized, incarcerated, or homeless; persons with AUD are overrepresented in those settings, our findings may not generalize to these subpopulations of persons with AUD. As NSDUH responses are based on self-report, the validity of the results is based on the accuracy of participant response. There is potential for recall bias given that questions require participants to reflect upon the past 12 months. The reliability of past 12-month recall for AUD and treatment has been previously demonstrated (Substance Abuse and Mental Health Services Administration, 2010), however, the past 12-month recall of items about screening, brief intervention and referral to treatment are not known, and thus should be interpreted with caution. It is worth emphasizing, however, that our results are similar to studies examining previous years of NSDUH data using these items, lending support for adequate reliability of questions. Potential for social desirability bias must also be considered given the stigma associated with substance use disorders, however, this bias is theoretically minimized by use of the computer-assisted self-reporting system.
It should be noted that approximately half of persons with a diagnosis of DSM-5 mild AUD did not have a diagnosis of alcohol abuse or dependence using DSM-IV criteria, likely due to differing classifications for disease presence used in DSM-IV and DSM-5. Even with not meeting DSM-IV criteria for alcohol abuse or dependence, however, those with a DSM-5 mild AUD diagnosis endorsed at least two criteria of AUD indicating problematic alcohol use. As persons with problematic alcohol use but without a more severe alcohol use disorder may be the most likely to benefit from brief counseling and education regarding their alcohol use, the large decrease in percentage of those screened about alcohol use and those who received a brief intervention in persons with mild AUD further underscores a missed opportunity to engage this subpopulation in evidence-based care.
In addition, NSDUH does not include detailed queries about the specific nature of screening efforts, brief intervention or treatment for AUD. Thus, we cannot comment with certainty on the degree to which evidence-based screening tools were used. . Questions can also be raised about what constitutes treatment for AUD. For example, a brief intervention may be adequate treatment for those with mild AUD given the natural history of recovery in AUD (Dawson et al., 2005). Finally, NSDUH does not evaluate for whether respondents who received treatment benefited from treatment. An improved understanding of the real-world effectiveness of AUD treatment is an important area of future study.
Though these limitations exist, the analysis of this large, general population sample nonetheless offers important insights into the care—and lack of care—for persons with AUD, and in particular for severe AUD.
Conclusions:
Persons with AUD utilize health care and a high proportion are screened about alcohol use, however only a minority receive AUD treatment. Ambulatory care settings- the most commonly used form of health care for persons with AUD- represent a prime opportunity to implement point-of-care AUD treatment to improve outcomes in this high-risk population.
Supplementary Material
ACKNOWLEDGMENTS
We thank Jingling Chen for her assistance creating figures.
Sources of Support:
This work was supported by National Institute on Drug Abuse grants K12 DA041449 (CMM, LJB, SLF, ATK), R21 DA044744 (RAG); National Institute on Alcohol Abuse and Alcoholism grants R21 AA025689 (RAG) and R01 AA029308 (SMH); National Institute of Allergy and Infectious Diseases grant K24 AI134413 (EHG); Substance Abuse and Mental Health Services Administration H79TI082566 (CMM, SMH). Research for this publication was also supported by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR002345 from the National Center for Advancing Translational Sciences of the National Institutes of Health. The content is solely the responsible of the authors and does not necessarily represent the official view of the NIH.
Footnotes
CONFLICT OF INTEREST
LJB is listed as an inventor on Issued U.S. Patent 8,080,371,“Markers for Addiction” covering the use of certain SNPs in determining the diagnosis, prognosis, and treatment of addiction. The other authors report no conflict of interest.
REFERENCES
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders: DSM5. 5th ed., American Psychiatric Association, Washington, D.C. [Google Scholar]
- Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, Gastfriend DR, Hosking JD, Johnson BA, LoCastro JS, Longabaugh R, Mason BJ, Mattson ME, Miller WR, Pettinati HM, Randall CL, Swift R, Weiss RD, Williams LD, Zweben A, Group CSR (2006) Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA 295:2003–2017. [DOI] [PubMed] [Google Scholar]
- Bandara SN, Samples H, Crum RM, Saloner B (2018) Is screening and intervention associated with treatment receipt among individuals with alcohol use disorder? Evidence from a national survey. J Subst Abuse Treat 92:85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazzi A, Saitz R (2018) Screening for Unhealthy Alcohol Use. JAMA 320:1869–1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohn MJ, Babor TF, Kranzler HR (1995) The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol 56:423–432. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA (1998) The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med 158:1789–1795. [DOI] [PubMed] [Google Scholar]
- Carvalho AF, Heilig M, Perez A, Probst C, Rehm J (2019) Alcohol use disorders. Lancet 394:781–792. [DOI] [PubMed] [Google Scholar]
- Case A, Deaton A (2017) Mortality and morbidity in the 21(st) century. Brookings Pap Econ Act 2017:397–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen E, Feinn R, Arias A, Kranzler HR (2007) Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend 86:214–221. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ (2005) Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction 100:281–292. [DOI] [PubMed] [Google Scholar]
- Esser MB, Sherk A, Liu Y, Naimi TS, Stockwell T, Stahre M, Kanny D, Landen M, Saitz R, Brewer RD (2020) Deaths and years of potential life lost from excessive alcohol use - United States, 2011–2015. Morb Mortal Wkly Rep 69:981–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming MF (2004) Screening and brief intervention in primary care settings. Alcohol Res Health 28:57–62. [PMC free article] [PubMed] [Google Scholar]
- Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ (2011) The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis 52:793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Bohnert KM, Brown RL (2016) Alcohol Screening and Intervention Among United States Adults who Attend Ambulatory Healthcare. J Gen Intern Med 31:739–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Bello-Kottenstette JK, Mintz CM, Borodovsky JT (2020) The changing landscape of alcohol use disorder and problem drinking in the USA: implications for primary care. Fam Pract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunderson EW, Fiellin DA (2008) Office-based maintenance treatment of opioid dependence: how does it compare with traditional approaches? CNS Drugs 22:99–111. [DOI] [PubMed] [Google Scholar]
- Hallgren KA, Witwer E, West I, Baldwin LM, Donovan D, Stuvek B, Keppel GA, Mollis B, Stephens KA (2020) Prevalence of documented alcohol and opioid use disorder diagnoses and treatments in a regional primary care practice-based research network. J Subst Abuse Treat 110:18–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris AH, Kivlahan DR, Bowe T, Humphreys KN (2010) Pharmacotherapy of alcohol use disorders in the Veterans Health Administration. Psychiatr Serv 61:392–398. [DOI] [PubMed] [Google Scholar]
- HIV.gov (2021) HIV Care Continuum. Available at: https://www.hiv.gov/federal-response/policies-issues/hiv-aids-care-continuum. Accessed 3/10/21.
- Johnson K, Rigg KK, Hopkins Eyles C (2020) Receiving addiction treatment in the US: Do patient demographics, drug of choice, or substance use disorder severity matter? Int J Drug Policy 75:102583. [DOI] [PubMed] [Google Scholar]
- Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, Kim MM, Shanahan E, Gass CE, Rowe CJ, Garbutt JC (2014) Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA 311:1889–1900. [DOI] [PubMed] [Google Scholar]
- Kazemian P, Shebl FM, McCann N, Walensky RP, Wexler DJ (2019) Evaluation of the cascade of diabetes care in the United States, 2005–2016. JAMA Intern Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Humphreys K, Ferri M (2020) Alcoholics Anonymous and other 12-step programs for alcohol use disorder. Cochrane Database Syst Rev 3:CD012880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knox J, Hasin DS, Larson FRR, Kranzler HR (2019) Prevention, screening, and treatment for heavy drinking and alcohol use disorder. Lancet Psychiatry 6:1054–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krantz MJ, Mehler PS (2004) Treating opioid dependence. Growing implications for primary care. Arch Intern Med 164:277–288. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, Soyka M (2018) Diagnosis and Pharmacotherapy of Alcohol Use Disorder: A Review. JAMA 320:815–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laramee P, Leonard S, Buchanan-Hughes A, Warnakula S, Daeppen JB, Rehm J (2015) Risk of all-cause mortality in alcohol-dependent individuals: A systematic literature review and meta-analysis. EBioMedicine 2:1394–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely J, Kumar PC, Rieckmann T, Sedlander E, Farkas S, Chollak C, Kannry JL, Vega A, Waite EA, Peccoralo LA, Rosenthal RN, McCarty D, Rotrosen J (2018) Barriers and facilitators affecting the implementation of substance use screening in primary care clinics: a qualitative study of patients, providers, and staff. Addict Sci Clin Pract 13:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL (2004) Actual causes of death in the United States, 2000. Journal of the American Medical Association 291:1238–1245. [DOI] [PubMed] [Google Scholar]
- Moyer A, Finney JW, Swearingen CE, Vergun P (2002) Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction 97:279–292. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Medication treatment for opioid use disorder in the prmiary care setting. Available at: https://www.drugabuse.gov/nidamed-medical-health-professionals/science-to-medicine/medication-treatment-opioid-use-disorder/in-primary-care-setting. Accessed 10/06/20.
- O’Connor EA, Perdue LA, Senger CA, Rushkin M, Patnode CD, Bean SI, Jonas DE (2018) Screening and Behavioral Counseling Interventions to Reduce Unhealthy Alcohol Use in Adolescents and Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 320:1910–1928. [DOI] [PubMed] [Google Scholar]
- Prabhakar V, Kwo PY (2019) Toward elimination of hepatitis C infection: How best to address gaps in the cascade of care? Hepatol Commun 3:1174–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahm AK, Boggs JM, Martin C, Price DW, Beck A, Backer TE, Dearing JW (2015) Facilitators and barriers to implementing screening, brief intervention, and referral to treatment (SBIRT) in primary care in integrated health care settings. Subst Abus 36:281–288. [DOI] [PubMed] [Google Scholar]
- Ramsey AT, Baker TB, Pham G, Stoneking F, Smock N, Colditz GA, James AS, Liu J, Bierut LJ, Chen LS (2020) Low burden strategies are needed to reduce smoking in rural healthcare settings: a lesson from cancer clinics. Int J Environ Res Public Health 17:1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsey AT, Chiu A, Baker T, Smock N, Chen J, Lester T, Jorenby DE, Colditz GA, Bierut LJ, Chen LS (2019a) Care-paradigm shift promoting smoking cessation treatment among cancer center patients via a low-burden strategy, Electronic Health Record-Enabled Evidence-Based Smoking Cessation Treatment. Transl Behav Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsey AT, Prentice D, Ballard E, Chen LS, Bierut LJ (2019b) Leverage points to improve smoking cessation treatment in a large tertiary care hospital: a systems-based mixed methods study. BMJ Open 9:e030066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillane S, Shiels MS, Best AF, Haozous EA, Withrow DR, Chen Y, Berrington de Gonzalez A, Freedman ND (2020) Trends in Alcohol-Induced Deaths in the United States, 2000–2016. JAMA Netw Open 3:e1921451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2020). Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20 07-01-001, NSDUH Series H-55). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Available at https://www.samhsa.gov/data/. Accessed 3/10/21. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2010). Reliability of Key Measures in the National Survey on Drug Use and Health [Internet]. Rockville (MD): Substance Abuse and Mental Health Services Administration (US). Available at https://www.ncbi.nlm.nih.gov/books/NBK519794/. Accessed 3/10/21. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration and National Institute on Alcohol Abuse and Alcoholism (2015). Medication for the Treatment of Alcohol Use Disorder: A Brief Guide. HHS Publication No. (SMA) 15–4907. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Steinweg DL, Worth H (1993) Alcoholism: the keys to the CAGE. Am J Med 94:520–523. [DOI] [PubMed] [Google Scholar]
- Thomas DL (2020) State of the Hepatitis C virus care cascade. Clinical Liver Disease 16:8–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Burden of Disease Collaborators (2013) The state of US health, 1990–2010: Burden of diseases, injuries, and risk factors. Journal of the American Medical Association 310:591–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health & Human Services. HIV Care Continuum. Available at: https://www.hiv.gov/federal-response/policies-issues/hiv-aids-care-continuum. Accessed July 24, 2020.
- Willenbring ML (2013) Gaps in clinical prevention and treatment for alcohol use disorders: costs, consequences, and strategies. Alcohol Research: Current Reviews 35:238–243. [PMC free article] [PubMed] [Google Scholar]
- Williams AR, Nunes EV, Bisaga A, Levin FR, Olfson M (2019) Development of a cascade of care for responding to the opioid epidemic. Am J Drug Alcohol Abuse 45:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


