Abstract
Clinical and molecular phenotypes of asthma are complex. The main phenotypes of adult asthma are characterized by eosinophil and/or neutrophil cell dominant airway inflammation that represent distinct clinical features. Upper and lower airways constitute a unique system and their interaction shows functional complementarity. Although human upper airway contains various indigenous commensals and opportunistic pathogenic microbiome, imbalance of this interactions lead to pathogen overgrowth and increased inflammation and airway remodeling. Competition for epithelial cell attachment, different susceptibilities to host defense molecules and antimicrobial peptides, and the production of proinflammatory cytokine and pattern recognition receptors possibly determine the pattern of this inflammation. Exposure to environmental factors, including infection, air pollution, smoking is commonly associated with asthma comorbidity, severity, exacerbation and resistance to anti-microbial and steroid treatment, and these effects may also be modulated by host and microbial genetics. Administration of probiotic, antibiotic and corticosteroid treatment for asthma may modify the composition of resident microbiota and clinical features. This review summarizes the effect of some environmental factors on the upper respiratory microbiome, the interaction between host-microbiome, and potential impact of asthma treatment on the composition of the upper airway microbiome.
Keywords: Asthma, Eosinophils, Inflammation, Microbiome, Neutrophils, 16S rRNA
INTRODUCTION
Asthma is a common chronic airway disease that affects people of all ages. Over 300 million people worldwide are affected by asthma, and the prevalence is high in children and in the elderly (1,2). After 40-50 years of age, most new cases of asthma are nonallergic and related to obesity, more severe disease, and having a lower lung function (3,4). Asthma-related morbidity and mortality are higher in older patients (1). The pathophysiology of asthma is complex, and involves airway inflammation that contributes to respiratory symptoms, airway hyperresponsiveness, and airflow limitation leading to a variety of more permanent changes in the airway which is commonly known as airway remodeling (5).
Asthma is a polygenic, multifactorial disorder and its etiology is related with interactions between genetic susceptibility, host factors, and environmental exposures. Genome-wide association studies of asthma have identified potential risk alleles and loci in different ethnic groups, providing an understanding of its genetic basis and functional role involved in disease pathogenesis (6). Genotype-specific risk factors are critical modifiers of the disease development, and host factors include age, gender, obesity and diet, whereas environmental exposures include tobacco smoke, air pollution, pollens, infection, mold and damp, animal exposure, occupational exposures, antibiotics, aspirin and non-steroidal anti-inflammatory drugs (7,8). These factors have been associated with either risk for or protection against upper and lower airway disease. Imbalance of resident microbial communities in the airways is affected by these factors and could be important in defining states of health or disease. Microbial exposures can be considered as plausible mechanisms for many of these associations, and the upper airway might be the direct site of important host-environment interactions (9).
According to the united airway concept, upper and lower airways constitute a unique system and their interactions show functional complementarity (10). In healthy adults, microbiome biomass decreases from the upper to lower respiratory tract, and community composition in the lung is not largely indistinguishable from upper airway microbiota (11). Microbiome sampling in upper airway is non-invasive and easy to assess (12), and may predict similar changes occurring in the lower airways. Our team showed that Staphylococcal enterotoxin sensitization was associated with asthma, especially in the adult and elderly asthma with sputum eosinophilia and chronic rhinosinusitis (CRS), which suggests that microbiome in upper airway could play an important role in the pathogenesis of asthma (13,14,15).
The Human Microbiome Project reported bacterial distribution by body sites as a reference, and the majority of the bacteria reside in the gastrointestinal tract with 29%, and the distribution in the airway is 14% (16). The total number of bacteria across the whole body of the adult is approximately 3.8×1013 and this number is close to human cells in the body (17). Although members of the host microbiota are referred to as commensals, their interaction with a host can be contextual according to host genetic and other risk factors.
Most recent studies have been using advanced molecular techniques such as 16S rRNA gene sequencing (partial genomes), shotgun sequencing (complete genomes), metabolomics (non-protein small molecules), metaproteomics (protein) and metatranscriptomics (RNA) that are revolutionizing our understanding of the human microbiome (18). The pathobiological impact of the airway microbiome in asthma is only partially known. This review summarizes recent findings and emerging concepts on the role of environmental and genetic factors in the dysbiosis of upper airway microbiota, immune regulation of microbiome, and the effect of asthma therapies on the composition of nasal microbiome in adult asthma.
AIRWAY INFLAMMATION AND ASTHMA PHENOTYPES
Airway inflammation is a key component in the asthma pathogenesis and has been divided into two types based on dominant cells present in the airway: eosinophilic (T2) and neutrophilic (non-T2). T2 asthma can be further split into allergic eosinophilic asthma and non-allergic eosinophilic asthma, while non-T2 asthma can be divided in three inflammatory phenotypes based on sputum neutrophilia: neutrophilic, mixed granulocytic and paucigranulocytic (19).
Allergic T2 inflammation is mediated by antigen specific Th2 cells that produce IL-4, IL-5, IL-9, and IL-13 resulting IgE-mediated mast cell and basophil degranulation and eosinophil activation (20). Th2 derived cytokines play an important role in airway eosinophilia, airway hyperreactivity and mucus hypersecretion, and IgE mediated mast cell activation induce airway inflammation, mucus production, smooth muscle cell contraction and airway remodeling (21). Biological actions of current monoclonal antibody and corticosteroid therapies are both effective in these patients (19), while nonallergic eosinophilic asthma patients have persistent high numbers of eosinophils despite treatment of corticosteroids (22). Air pollutants, microbes and glycolipids induce the release of epithelium-derived cytokines such as IL-33, IL-25, or TSLP, stimulating group 2 innate lymphoid cells (ILC2s) to secrete high amounts of IL-5 and IL-13, leading to eosinophilic inflammation (20). Though the secretion of IL-4 by ILC2 is disparate, IL-4 is critical to promote Th2 activation (23,24). A recent study revealed that ILC2s are accumulated predominantly in lung tissue and led to a pronounced T2 inflammation in the lung after allergen challenge (25). Eosinophilic asthma that develops in adulthood has a greater probability of chronic rhinosinusitis with nasal polyposis (CRSwNP) and it is often nonallergic (26).
Nonallergic asthma is defined with negative skin prick or in vitro-specific IgE tests to common allergens (27). The mechanisms contributing nonallergic asthma is less understood, and suggested mechanisms are hypersensitivity reactions to unidentified allergens such as fungi, recurrent or persistent infections, autoimmune mechanism, neutrophil mediated immune response or the activation of the IL-17-dependent pathway (28). Non-T2 neutrophilic asthma biomarkers are YKL-40 (chitinase-like protein) and IL-17 that are correlated with airway neutrophilia, obesity and asthma severity by inducing relative steroid unresponsiveness (29,30). Paucigranulocytic asthma patients have lower levels of fractional exhaled nitric oxide (FeNO), eosinophil cationic protein (ECP) and IL-8 in induced sputum, and 14.8% of these patients had poor asthma control despite the absence of inflammatory cells in their sputum (31). As similar to neutrophilic asthma, inhaled corticosteroid (ICS) treatment could be less effective in these patients (32). Th2/Th17 (IL-4 and IL-17) predominant asthmatics show blood eosinophilia, airway obstruction and hyperresponsiveness, and relative corticosteroid insensitivity (33). Also, in mixed granulocytic asthma patients, sputum IL-8, ECP and FeNO levels are elevated (31). Macrolides could be effective for non-T2 asthma patients through decreasing airway concentrations of IL-8 and neutrophil numbers and improving quality-of-life scores (34).
Certain airway bacterial taxa have potential influence on immunity. For example, Streptococcus pneumoniae and Haemophilus influenzae increase IL-8 production through an NF-κB-dependent mechanism (35). Staphylococcus aureus manipulates the airway mucosal immunology by releasing IL-33 from respiratory epithelium and activates ILC2 and Th2 cells, mast cell degranulation, B-cell activation and IgE formation, and eosinophil stimulation leading to epithelial damage (36). Proteobacteria is associated with epithelial expression of Th17 inflammation-related genes and negatively correlated with bronchial eosinophil (37).
HOST-MICROBIOTA AND INTERRELATIONSHIPS BETWEEN MICROBIOTA
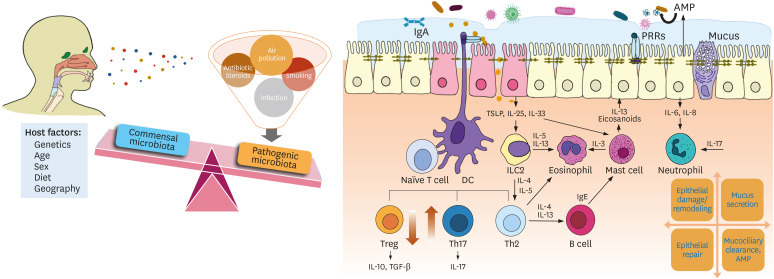
Commensals are a critical and active inducer of immune regulatory responses. The epithelial mucosa and the dendritic cells (DCs), which are in continuous contact with the airway lumen, and antimicrobial peptides (AMP) produced by immune cells play an important role in the response to environmental agents (Fig. 1).
Figure 1. Upper-airway dysbiosis and potential immunopathology in the airway inflammation. Persistent exposure to pathogens and other risk factors promotes airway inflammation through induction of both innate immune cells and adaptive immune cells. Although some risk factors are prominently related to upper airway dysbiosis, host factors are also considerably overlap in the development of airway diseases. Mucins in interaction with IgA and AMP contribute to innate immunity. Upon microbial signals, DCs activate antigen-specific naïve T cells which further drive development in effector Th cells. Tregs can suppress various effector Th cell subsets releasing anti-inflammatory and immunoregulatory cytokines, yet are downregulated in chronic airway inflammation. Th2 derived cytokine IL-13 upregulates the expression of mucin genes that initiate mucus hypersecretion. Pathogen invasion also induces epithelium-derived IL-6 and IL-8 production via interaction with PRR leading to neutrophilic inflammation.
Respiratory mucin proteins contribute to mucociliary clearance and host defense in human nasal mucosa and are (mucin 5AC [MUC5AC] and MUC5B) produced at similar levels in the upper and lower airways (38). In patients with asthma, the abnormal expression of MUC5AC, MUC5B, and MUC2 are the principal gel-forming mucins secreted predominantly in upper airway diseases (39), and MUC5AC is upregulated in the epithelium of asthmatic airways (40). Excessive mucus formation in upper airway may trap more inhaled micro-organisms and this, in turn might result ciliary dysfunction and give bacteria opportunity to adhere and promote biofilm formation (41). Both gram-positive and gram-negative bacterial products upregulate mucin genes expression and mucin secretion in respiratory epithelial cells (42), and microbial binding to mucin is essential for nasal colonization (43). Airway inflammation with Th2 cells stimulates mucus production by IL-13 in asthma (44). IL-13 has been shown to increase goblet cell numbers in airways that asthma patients experience severe mucus obstruction and airway hyperresponsiveness.
Airway epithelium produces AMP that contribute to barrier function, including human β-defensin 2 (hBD-2). hBD-2 is expressed in nasal mucosa and the expression is induced by microbial components, proinflammatory cytokines and TLR signaling pathway (45). hBD-2 has chemotactic activity for T cells and immature DCs, and can activate mast cells leading to release histamine and prostaglandin D2 in allergic inflammation (46). The reduction of hBD-2 expression affects the abnormal microbial colonization and immune responses in CRSwNP (47).
Pattern recognition receptors (PRRs) are essential for host and microbial interactions in nasal sinus mucosa. Sinonasal epithelial cells express 10 TLRs, and the signaling through TLRs initiates immune responses in the respiratory epithelium (48). TLRs bind to and recognize damage-associated molecular patterns and pathogen-associated molecular patterns such as peptidoglycan (TLR2 ligand), double-stranded RNA (TLR3 ligand) and LPS (TLR4 ligand) (49). Thus, TLR signaling induces distinct stimulation of cytokines, chemokines and costimulatory molecules based on the exposure (e.g., TLR2 and TLR4 potentially induce the release of IL-1β and IL-8, whereas TLR3 and TLR7/8 may induce the production of IL-4, IL-5, and IL-13) (50). Genetic variations in TLR-related pathway genes are important factors for asthma development, and our previous study demonstrated that TLR2 and CD14 impact the abundances of nasal microbiota and clinical phenotypes in adult asthma (51). Besides, bacterial pathogens express numerous virulence factors and seek to evade PRR-induced innate immune responses that assist the bacterium colonize the host (52).
Th17 cells are also important in host defense against pathogen, and IL-17 signaling has a significant role in maintaining the nasal normal microbiome composition by reducing colonization with potentially pathogenic bacteria (53). Inhibitory Tregs play opposing roles by suppressing effector T-cells to limit excessive immune responses during infections. Downregulated Treg-related cytokines and elevated Th2 cytokines exhibited in eosinophilic CRS, whereas upregulated Treg cells and increased Th1 and Th17 cytokines presented in non-eosinophilic rhinosinusitis (54). Therefore, microbiome dependent imbalance of Treg and Th cell subsets leads to different inflammatory patterns in airway diseases.
ILCs are preferentially located close to the epithelial barriers that are in direct contact with microbiota. ILC1s and ILC3s produce Th1 and Th17 cytokines, while ILC2s produce Th2 cytokines. In vivo, rhinovirus challenge induced IL-33 and T2 cytokines in bronchial and nasal fluid in asthma patients (55). In same study, culture of human T cells and ILC2s with supernatants of rhinovirus-infected epithelium led to IL-33-dependent Th2 cytokine production in vitro (55). ILC2s are elevated in the eosinophilic nasal polyp, and polyp ILC2 is reduced by systemic corticosteroid treatment (56).
Members of the microbiota interact with each other in mutualistic or antagonistic way. Particularly, the commensal genus Dolosigranulum spp. is responsible for the acidification of the local environment which promote the expansion of Corynebacterium spp. (57), while this effect inhibits the growth of acidophobic bacteria S. aureus (58). In addition, S. aureus forms polymicrobial biofilm with Candida albicans and enhance antimicrobial resistance (59) resulting persistent inflammatory changes in the upper airway. Also, common respiratory bacteria H. influenzae and Pseudomonas aeruginosa can promote the production of pro-inflammatory cytokines in response to subsequent infection with respiratory syncytial virus in airway epithelial cell (60).
NORMAL UPPER AIRWAY MICROBIOTA
The Human Microbiome Project Consortium evaluated microbiome composition sampling at 18 body sites from 242 healthy adults (61). The most abundant genera in the anterior nares were Propionibacterium (Propionibacterium acnes), Corynebacterium (Corynebacterium accolens) and Staphylococcus, and abundant pathogenic species were P. acnes, S. aureus and S. epidermidis. Similarly, Zhou et al. (62) determined prevalent genera in the nasal cavity of 236 healthy adults, and it included Staphylococcus, Propionibacterium, Corynebacterium, and Moraxella. When healthy adults sinus microbiota was assayed with CRS nasal samples, genera Corynebacterium and Staphylococcus were common in the majority of the nasal samples including healthy controls (63). These findings suggest that a healthy nasal cavity contains various opportunistic pathogenic bacteria within genera and potential to be as reservoir.
INFLUENTIAL FACTORS ON THE COMPOSITION OF UPPER AIRWAY MICROBIOME
Smoking
In asthma patients, tobacco smoking is associated with more severe asthma symptom, frequent exacerbation, and corticosteroid insensitivity (64). Persistent smoking exposure enhances mixed Th1/Th2 immune response that develops more severe asthma phenotype, and induces neutrophils and oxidative stress which cause resistance to corticosteroids (65). In general, smoking induces pro-inflammatory cytokines as well as IgE production, and alters immune cells such as alveolar macrophages, neutrophils, lymphocytes and NK cells which are the major cells in pathogen clearance and defense against pathogens (66).
Cigarettes are direct source of potentially pathogenic microorganisms that include fifteen different classes of bacteria and wide range of pathogenic organisms including Acinetobacter, Bacillus, Burkholderia, Clostridium, Klebsiella, Pseudomonas aeruginosa, and Serratia (67). In healthy adults nasopharynx, smoking status is positively associated with Corynebacterium and Staphylococcus (68). In airway exposure study, the presence of nine bacterial genera in pharynx was correlated positively with smoking: Actinomyces, Actinobacillus, Anaerococcus, Peptoniphilus, Staphylococcus, Streptococcus, Gemella, Psychrobacter, and Treponema (69). In a univariate analysis and a machine learning approach, nasopharyngeal microbial communities were compared between smoking and non-smoking healthy adults (70). Haemophilus spp., Campylobacter spp. and Abiotrophia spp. were dominant in smokers, whereas only Shigella spp. was lower in nasopharyngeal communities of smokers compared with non-smokers. Newly detected genera with increased abundance in the nasopharynx of smokers included Eggerthella, Erysipelotrichaceae I.S., Dorea, Anaerovorax, and Eubacterium spp. that constitute gram-positive anaerobic bacterial colonization in the nasopharynx (70). Recently, we reported that genera Corynebacterium, Propionibacterium, Streptococcus, Haemophilus and Rothia in the upper airway were correlated with the exposure to smoking and clinical phenotypes in adult asthma (51). In different studies, although smoking cessation improved asthma symptom and lung function in smoking asthma patients (64), it did not change the sputum bacterial community in 12-wk follow-up study (71). Thus, in addition to smoking and cessation duration, distinct bacterial colonization in smokers and potential influence of airway microenvironment on particular microbiota should be carefully considered in future research (72).
Air pollution
Air pollution is associated with the prevalence of adults asthma (with particulate matter [PM] of less than 10 μm [PM10] and nitrogen dioxide), decreased lung function, asthma severity and exacerbation (with ozone, sulfur dioxide, nitrogen dioxide) (73). PM contributes to airway inflammation through genetic variation, oxidative stress induction, airway epithelial barrier disruption, altered cell signaling pathways, production of T2 cytokines, and inflammatory cell recruitment (74).
Compositions of total airborne bacteria and pathogenic bacteria have been measured in different PM sizes and air quality levels (75). The dominant bacterial phyla in all the airborne PM samples were Proteobacteria, Cyanobacteria, Actinobacteria, Firmicutes, and Bacteroidetes. The most common classes were Alphaproteobacteria, Actinobacteria, Betaproteobacteria, Oscillatoriophycideae and Clostridia. The most abundant genera were Thiobacillus, Methylobacterium, Rubellimicrobium, and Paracoccus. The relative abundance (RA) of pathogenic bacteria was different in PM10 samples from those of particulate matter of less than 2.5 μm (PM2.5) and total suspended particulate. Staphylococcus, Bacillus, Clostridium, Enterobacter, and Klebsiella were the dominant pathogenic genera in all the airborne PM samples. The proportions of the total and pathogenic bacterial community were correlated with wind scale, relative humidity, carbon monoxide, sulfur dioxide and ozone concentrations (75).
Exposure to high levels of PM2.5/PM10 critically alters airway microbiota composition. Qin et al. (69) studied pharyngeal microbiota in 83 subjects after exposure to high concentrations of PM2.5/PM10. The RA of 38 phyla increased in the post-smog samples, such as Firmicutes, Fusobacteria, and Actinobacteria, and 11 newly detected phyla including Caldiserica, Chlamydiae, Parcubacteria, Atribacteria, and Microgenomates (69). A total of 559 genera were increased including Leptotrichia, Corynebacterium, Veillonella, Dolosigranulum, unidentified-Chloroplast, Moraxella, Gemella, Actinomyces, Granulicatella, and Haemophilus. Main recognized prevalent respiratory pathogens in the post-smog swabs were Streptococcus, Haemophilus, Moraxella, and Staphylococcus, while significantly reduced genus was Neisseria after exposure to smog for two days. At the species level, RA of H. influenzae and Moraxella catarrhalis were dominant in the smog exposed samples (69). In a study on the association among air pollutants, immune markers and adult-onset asthma, 15% of the effect of air pollution on the risk of adult-onset asthma was mediated through immune system (76). IL-1RA was suggested to be associated with adult-onset asthma and air pollutants in the study. IL-1RA has an anti-inflammatory effect and its functional role was identified in the inflammatory process of asthma (77) and fungal-associated allergic airway inflammation (78). Although air pollutants are well known to cause asthma exacerbations, there is lack of supporting evidence on how air pollution may influence on upper airway microbiome in adult asthma.
Host and microbial genetics
Host genetic factors can contribute to the susceptibility of asthma. Recent advances in sequencing technology bring enormous genetic variation data from a large number of individuals. Igartua et al. (79) performed genome-wide association studies (GWAS) to determine host-microbial interaction using 16S rRNA gene sequencing of nasal swabs in 144 adult Hutterite population and whole genome sequencing data of the same population. They identified 37 microbiome quantitative trait loci which was associated with the RA of 22 genera and highly contained genes involved in mucosal immunity pathways. The most significant association was between RA of Dermacoccus (phylum Actinobacteria) and an intergenic variant near TINCR (rs117042385), a long non-coding RNA that binds to peptidoglycan recognition protein 3 (PGLYRP3) mRNA. Another association was between the RA of an unclassified genus of family Micrococcaceae (phylum Actinobacteria) and a missense variant in PGLYRP4 (rs3006458), a pattern receptor that binds to murein peptidoglycan of gram-positive bacteria. Currently no other research has done for host-microbiome association in adults' upper airway.
We previously observed higher composition of microbiome genes in non-asthmatics that are related with lysine degradation, N-glycan biosynthesis, caprolactam degradation, and peroxisome proliferator-activated receptor signaling pathway, and prevalent genes associated with pentose phosphate pathway, LPS biosynthesis, flagella assembly, and bacterial chemotaxis in young adult asthmatics (80), revealing possible role of microbiome in adult asthma.
MICROBIOTA COMPOSITION IN UPPER AIRWAY DISEASE
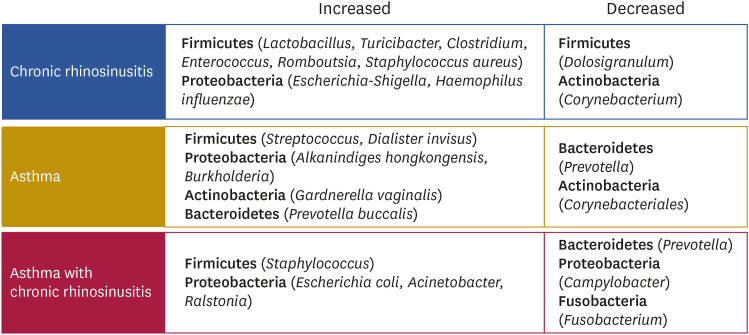
We summarized the upper airway dysbiosis in patients with CRS (with/without nasal polyposis [NP]) and asthma in Fig. 2. In a recent study, CRSwNP patients contained reduced Corynebacterium and Dolosigranulum in the nasal sample compared to healthy controls (81). Bacterial genera such as Lactobacillus, Escherichia-Shigella, Turicibacter, Clostridium, Enterococcus, and Romboutsia were positively correlated with the severity of CRSwNP, while no correlation observed with age, body mass index and symptom score (81). Another group compared bacterial communities in nasal tissues of CRSwNP with and without asthma and healthy controls. Interestingly, CRSwNP patients had significantly enriched H. influenzae, while healthy controls had higher P. acnes. S. aureus, common colonizer of the upper airways that aggravate allergy and induce IgE formation, was dominant in the CRSwNP without asthma group, and Escherichia coli was higher in CRSwNP with asthma group (82,83). E. coli was positively correlated with ECP and IL-5 in the nasal polyp tissues which promote T2 inflammation in CRSwNP patients.
Figure 2. A summary of upper airway dysbiosis in asthma and CRS.
UPPER AIRWAY MICROBIOTA IN ADULT ASTHMA
Microbiota composition in asthma phenotypes and upper airway varies between research articles due to population characteristics including age, sex, ethnicity, diet, geography, and study design, sampling site, technique, analysis method and disease status. As asthma is a heterogenous disease with different phenotypes and variable clinical manifestations, understanding airway microbiome diversity in disease progression and propagation is crucial and phenotype-specific alterations are summarized in Table 1.
Table 1. Clinical relevance of upper airway microbiota in adult asthma.
| Cohort | Subjects | Collection site | Microbiota variation | Phenotype association | Ref. | |
|---|---|---|---|---|---|---|
| CRSwNP | 59 CRSwNP and 27 controls | Nasal swab | • CRSwNP: reduction of Corynebacterium and Dolosigranulum | Lactobacillus, Escherichia-Shigella, Turicibacter, Clostridium, Enterococcus, and Romboutsia are associated with severity of CRSwNP. | (81) | |
| CRSwNP with and without asthma | 21 CRSwNP patients without asthma, 20 CRSwNP patients with co-morbid asthma, 17 healthy subjects | Nasal swab | • Enrichment in each group: | CRSwNP is associated with high concentrations of IgE, SE-IgE, and IL5. | (82) | |
| CRSwNP: H. influenzae | ||||||
| Healthy group: P. acnes | ||||||
| CRSwNP without asthma: S. aureus | ||||||
| CRSwNP with asthma: E. coli | ||||||
| Asthma with and without CRS | 56 patients with CRS and 26 control subjects | Sinus swabs | • Asthma patients with CRS: lower abundance of Prevotella, Fusobacterium, Campylobacter and higher Staphylococcus, Acinetobacter, Ralstonia compared with non-asthmatic patients with CRS | Higher relative abundances of Actinobacteria can be predictive of better surgical outcome of CRS. | (84) | |
| Asthma and COPD | 5 patients with COPD, 11 patients with asthma and 8 controls | Nose, oropharynx, left upper lobe | • Asthma and COPD: reduction of Bacteroidetes (Prevotella spp.). | NA | (85) | |
| • Nasal samples were characterized by Actinobacteria and Firmicutes. | ||||||
| Young adult and elderly asthma | 60 patients with asthma and 20 controls | Nasopharyngeal swab | • Young adult asthma: high Proteobacteria | • Young adult: Prevotella, Neisseria, Fusobacterium negatively correlated with FEV1. | (80) | |
| • Young non-asthma: high uncultured Corynebacteriales | • Elderly: Burkholderia and Psychrobacter positively correlated with FEV1, while Corynebacterium negatively correlated with FEV1. | |||||
| • Elderly non-asthma: high Moraxella | ||||||
| Asthma | 72 exacerbated asthma, 31 non-exacerbated asthma and 21 healthy controls | Nasal swab | • Asthma: high Bacteroidetes and Proteobacteria | • Prevotella buccalis, Gardnerella vaginalis and Alkanindiges hongkongensis are associated with exacerbated asthma. | (86) | |
| • Dialister invisus is associated with non-exacerbated asthma. | ||||||
| Asthma | 111 CRS: 46 asthma, 65 non-asthma | Nasal swab | • Asthmatic CRS: high Streptococcus genus | Asthmatics with emergency visit had high Proteobacteria phylum (Burkholderia spp.) | (87) | |
SE-IgE, IgE against S. aureus superantigens; NA, not applicable.
Asthmatic patients with CRS had a lower abundance of Prevotella, Fusobacterium, and Campylobacter species, and more abundant of Staphylococcus, Acinetobacter, and Ralstonia species compared with non-asthmatic patients with CRS (84). Hilty et al. (85) identified nasal microbial communities in adults with asthma, chronic obstructive pulmonary disease (COPD) and healthy controls as part of their study. When nasal microbiota was compared with oropharynx and left upper lobe, nasal specimens were characterized by Actinobacteria and Firmicutes. However, the authors did not report the comparisons between the nasal microbiota of asthmatics versus control groups. Previously we have shown a higher abundance of uncultured Corynebacteriales in non-asthmatic young adults, and a higher abundance of Moraxella in non-asthmatic elderly individuals (80). The comparison of upper airway microbiota between young adults and elderly also showed different composition including Staphylococcus, Propionibacterium, and Moraxella. The high abundances of Prevotella, Neisseria, and Fusobacterium were correlated with forced expiratory volume in 1 s (FEV1) in young adults, whereas Burkholderia and Psychrobacter and Corynebacterium revealed contrary relationship with FEV1 among elderly individuals.
In an association study of nasal microbiome in asthma exacerbation and healthy controls, taxa from Proteobacteria and Bacteroidetes were dominant in subjects with exacerbated and non-exacerbated asthma relative to healthy controls (86). More specifically, enrichment of Prevotella buccalis, Alkanindiges hongkongensis, and Gardnerella vaginalis were identified in patients with exacerbated asthma, while Dialister invisus was greater in patients with non-exacerbated asthma. According to Yang et al., asthmatic CRS patients had prevalent RA of the Streptococcus genus, and asthmatics with at least one emergency department visits were associated with higher RA of Proteobacteria phylum (Burkholderia spp.) (87).
Microbiome community in lower airways of adult asthmatic patients were reviewed to compare with upper airway microbiome. Similar to nasal microbiota, reduced prevalence of sputum Bacteroidetes and Fusobacteria in patients with severe and non-severe asthma, and increased prevalence of Firmicutes were identified in severe asthma patients (88). In addition, higher abundance of Lactobacillus (Firmicutes), Pseudomonas (Proteobacteria) and Rickettsia (Proteobacteria) in asthmatic patients, and higher abundance of Prevotella (Bacteroidetes), Streptococcus (Firmicutes) and Veillonella (Firmicutes) were detected in healthy controls when measured in endobronchial brush samples (89).
These findings suggest that genera Dolosigranulum and Prevotella are more likely play protective effect against asthma, whereas enriched genus Streptococcus, and phyla Proteobacteria and Firmicutes in asthmatics are probably influencers of asthma development and disease severity.
THERAPEUTIC EFFECT ON THE COMPOSITION OF UPPER AIRWAY MICROBIOTA
Probiotics
Microbial colonization begins in utero and the composition is modified by consumption of probiotics during pregnancy, breastfeeding, mode of delivery, early respiratory infections (90), antibiotics, environmental factors and genetic/epigenetic regulation (9). Numerous studies reported the influential effect of the upper airway microbiome in the development of early onset rhinitis, wheeze and chronic inflammation in upper airway (91), and the symptoms were improved by probiotics intake (92). Probiotics are live microorganisms that provide health benefits to the host through promotion of epithelial barrier function, regulation of the mRNA levels of TLRs, and stimulate Tregs and reduce Th1 and Th2 cells development (93).
In a double-blind, randomized, placebo-controlled study, 49 young adults with perennial allergic rhinitis (AR) received either Lactobacillus acidophilus strain L-92 in fermented milk or without lactic acid bacteria (94). The result shows that oral administration of L-92 significantly improved nasal symptom-medication score, and decreased the scores of swelling and color of the nasal mucosa at 6 and 8 weeks of ingestion. However, there were no significant differences in serum specific IgE levels nor in Th1/Th2 ratio between groups (94). In different placebo-controlled study, co-administration of allergen specific immunotherapy with Clostridium butyricum significantly enhanced the therapeutic effect on AR (lowered 81.2% of the AR symptoms) (95). This combination effect decreased nasal symptom score, medication score, serum specific IgE, Th2 cytokines and skin prick test index, and elevated the frequency of regulatory B cell. When the immune modulatory effect of probiotic Bifidobacterium lactis NCC2818 was examined in individuals suffering from seasonal AR, concentrations of Th2 cytokines and total nasal symptom scores, and basophil cell activation were significantly lower in the probiotic group (96). Probiotic (Lactobacillus gasseri KS-13, Bifidobacterium bifidum G9-1, and Bifidobacterium longum MM-2) intake during spring allergy season improved rhinoconjunctivitis-specific quality of life in individuals with seasonal allergy (97). Although majority of the findings suggest the beneficial effect of probiotic treatment for CRS, nasal administration of honeybee lactic acid bacteria did not reduce symptom severity or inflammatory biomarkers and did not affect commensal bacteria of the nasal cavity (98). Due to the distinct study design, probiotic species and strains, administered dose and timing, the studies may represent inconsistent results which needs to be considered in future studies. Also, individual genetic variation, age, sex and resident microbiota should be taken into consideration when evaluating the effect of probiotics.
Antibiotics
Prolonged medical therapies such as corticosteroids, antihistamines, and antibiotics are the main therapy for inflammatory sinonasal disorders. Antibiotic perturbs the original microbiome composition as it damages bacterial cell wall, inhibits bacterial growth, and alters genes and protein fluxes (99). In addition to its anti-microbial effect, antibiotics also have an anti-inflammatory and immunomodulatory effects. Macrolide downregulates pro-inflammatory cytokine (IL-8) (100) and inhibits the activation of transcriptional factors (NF-κB, AP-1) (101) in human epithelial cells, which are important regulators in the inflammatory process.
The most common microbiota influenced by the antibiotic treatments are phyla Actinobacteria (Bifidobacterium-by 40 antibiotic treatments), Bacteroidetes (Bacteroides-30), Firmicutes (Faecalibacterium-30), and Proteobacteria (Escherichia-13) (102). Antibiotics for respiratory tract infection such as azithromycin and clarithromycin alone affect less than six genera each, whereas a combination of these macrolide antibiotics could alter the abundance of 15 genera (102).
The evidence supporting antibiotic efficacy in asthma symptoms and exacerbation are inconsistent. Although treatment with azithromycin in eosinophilic NP improved polyposis staging and quality-of-life (103), and decreased asthma exacerbation in persistent symptomatic asthma patients (104), these are not in the same line with other report (105). The previous study of sinus microbiota in CRS have shown that antibiotic use and asthma are associated with loss of microbial diversity and high S. aureus abundance (106). A combination of antibiotics and anti-inflammatory therapy significantly reduced sinus microbiota biodiversity in post-operative maxillary sinuses (107). Although the sinus bacterial composition after treatment was unique to each individual, the expansion was observed in Pseudomonas, non-aureus Staphylococcus, Corynebacterium, Propionibacterium, Haemophilus, and Delftia.
It is essential to choose pathogen-selective antibiotics in order to minimize disturbance to the microbiome, as inappropriate antibiotic treatments are able to shift the commensal microbiota to long-term alternative dysbiotic states, resulting in a variety of negative health consequences (108). As most common antibiotics reduce beneficial resident microbiota (Faecalibacterium, Bifidobacterium, and Blautia), it is crucial to consider combination or selective effect of antibiotics, administration type, concentration and resistance of antibiotics in clinical practice.
Corticosteroids
Inhaled corticosteroids are the most effective medication for asthma. In the meta-analysis study, the intranasal corticosteroid medication improved asthma-specific outcome measures in patients with both AR and asthma (109). The impact of intranasal corticosteroids in the management of CRS and asthma shows the alteration of nasal microbiota composition. In healthy adults with and without chronic non-infectious rhinitis, the administration of topical corticosteroid spray (mometasone furoate, 200 µg per day) for 1 month increased the RA of staphylococci (phylum Firmicutes), while suppressing Moraxella spp. (phylum Proteobacteria) and streptococci (phylum Firmicutes) in the nasal cavity (110). In asthma, nasal abundance of P. buccalis, A. hongkongensis, G. vaginalis, and D. invisus remained associated with asthma in multivariate models adjusted for steroids (86). In contrast, inhaled and oral corticosteroid treatments affected the alpha and beta diversity, and increased abundance of Proteobacteria and decreased abundance of Bacteroidetes and Fusobacteria in the lower airway samples of asthmatics patients (89). Effect of corticosteroids in lung microbiome concerning to asthma has been summarized in another review and has shown strong impact on bacterial community which in turn contributes to corticosteroid responsiveness (111).
CONCLUDING REMARKS
Commensal microbiota plays an important role to maintain the host-microbe mutualism. Nasal commensals are primarily responsible for the health of respiratory tract. The microbial imbalance could have a causative role in the pathogenesis of upper and lower airway diseases including asthma. Environmental exposures, genetics and medications could shape the composition of upper airway microbiome through epithelial barrier disruption and the modulation of innate and adaptive immune response. Current review focused on most recent findings that assessed the composition of upper airway microbiota in adult asthma patients using 16S rRNA gene sequencing. However, we should count that genus can have a wide range of strains which are genomically distinct and may have either protective or disease-causing effects. Therefore, further investigation is warranted to perform network approaches to better understand the complex molecular mechanisms involved in these processes and develop effective therapies for asthma.
ACKNOWLEDGEMENTS
This work was supported by Brain Pool Program through the National Research Foundation of Korea (NRF) funded by Ministry of Science and ICT (grant No. 2019H1D3A2A02102333). We appreciate Ms. Sunhee An from Gyeonggi-do Atopy Asthma Education Information Center for illustrations.
Abbreviations
- AMP
antimicrobial peptides
- AR
allergic rhinitis
- COPD
chronic obstructive pulmonary disease
- CRS
chronic rhinosinusitis
- CRSwNP
chronic rhinosinusitis with nasal polyposis
- DC
dendritic cell
- ECP
eosinophil cationic protein
- FeNO
fractional exhaled nitric oxide
- FEV1
forced expiratory volume in 1 s
- GWAS
genome-wide association studies
- hBD-2
human β-defensin 2
- ICS
inhaled corticosteroid
- ILC2
group 2 innate lymphoid cell
- MUC5AC
mucin 5AC
- NA
not applicable
- NP
nasal polyposis
- PM
particulate matter
- PM10
particulate matter of less than 10 μm
- PM2.5
particulate matter of less than 2.5 μm
- PRR
pattern recognition receptor
- SE-IgE
IgE against S. aureus superantigens
Footnotes
Conflict of Interest: The authors declare no potential conflicts of interest.
- Conceptualization: Losol P, Chang YS.
- Project administration: Chang YS.
- Writing - original draft: Losol P.
- Writing - review & editing: Choi JP, Kim SH, Chang YS.
References
- 1.Global Asthma Network. The Global Asthma Report. Auckland: Global Asthma Network; 2018. [Google Scholar]
- 2.Kang SY, Song WJ, Cho SH, Chang YS. Time trends of the prevalence of allergic diseases in Korea: a systematic literature review. Asia Pac Allergy. 2018;8:e8. doi: 10.5415/apallergy.2018.8.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pakkasela J, Ilmarinen P, Honkamäki J, Tuomisto LE, Andersén H, Piirilä P, Hisinger-Mölkänen H, Sovijärvi A, Backman H, Lundbäck B, et al. Age-specific incidence of allergic and non-allergic asthma. BMC Pulm Med. 2020;20:9. doi: 10.1186/s12890-019-1040-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song WJ, Chang YS. Respiratory allergies in the elderly: findings from the Korean Longitudinal Study on Health and Aging phase I study (2005–2006) Asia Pac Allergy. 2017;7:185–192. doi: 10.5415/apallergy.2017.7.4.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holgate ST. A look at the pathogenesis of asthma: the need for a change in direction. Discov Med. 2010;9:439–447. [PubMed] [Google Scholar]
- 6.Kim KW, Ober C. Lessons learned from GWAS of asthma. Allergy Asthma Immunol Res. 2019;11:170–187. doi: 10.4168/aair.2019.11.2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomsen SF. Genetics of asthma: an introduction for the clinician. Eur Clin Respir J. 2015;2:24643. doi: 10.3402/ecrj.v2.24643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murrison LB, Brandt EB, Myers JB, Hershey GK. Environmental exposures and mechanisms in allergy and asthma development. J Clin Invest. 2019;129:1504–1515. doi: 10.1172/JCI124612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Man WH, de Steenhuijsen Piters WA, Bogaert D. The microbiota of the respiratory tract: gatekeeper to respiratory health. Nat Rev Microbiol. 2017;15:259–270. doi: 10.1038/nrmicro.2017.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giavina-Bianchi P, Aun MV, Takejima P, Kalil J, Agondi RC. United airway disease: current perspectives. J Asthma Allergy. 2016;9:93–100. doi: 10.2147/JAA.S81541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Charlson ES, Bittinger K, Haas AR, Fitzgerald AS, Frank I, Yadav A, Bushman FD, Collman RG. Topographical continuity of bacterial populations in the healthy human respiratory tract. Am J Respir Crit Care Med. 2011;184:957–963. doi: 10.1164/rccm.201104-0655OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abdel-Aziz MI, Vijverberg SJH, Neerincx AH, Kraneveld AD, Maitland-van der Zee AH. The crosstalk between microbiome and asthma: exploring associations and challenges. Clin Exp Allergy. 2019;49:1067–1086. doi: 10.1111/cea.13444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Song WJ, Chang YS, Lim MK, Yun EH, Kim SH, Kang HR, Park HW, Tomassen P, Choi MH, Min KU, et al. Staphylococcal enterotoxin sensitization in a community-based population: a potential role in adult-onset asthma. Clin Exp Allergy. 2014;44:553–562. doi: 10.1111/cea.12239. [DOI] [PubMed] [Google Scholar]
- 14.Song WJ, Sintobin I, Sohn KH, Kang MG, Park HK, Jo EJ, Lee SE, Yang MS, Kim SH, Park HK, et al. Staphylococcal enterotoxin IgE sensitization in late-onset severe eosinophilic asthma in the elderly. Clin Exp Allergy. 2016;46:411–421. doi: 10.1111/cea.12652. [DOI] [PubMed] [Google Scholar]
- 15.Song WJ, Jo EJ, Lee JW, Kang HR, Cho SH, Min KU, Chang YS. Staphylococcal enterotoxin specific IgE and asthma: a systematic review and meta-analysis. Asia Pac Allergy. 2013;3:120–126. doi: 10.5415/apallergy.2013.3.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.NIH HMP Working Group. Peterson J, Garges S, Giovanni M, McInnes P, Wang L, Schloss JA, Bonazzi V, McEwen JE, Wetterstrand KA, et al. The NIH Human Microbiome Project. Genome Res. 2009;19:2317–2323. doi: 10.1101/gr.096651.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sender R, Fuchs S, Milo R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016;14:e1002533. doi: 10.1371/journal.pbio.1002533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allaband C, McDonald D, Vázquez-Baeza Y, Minich JJ, Tripathi A, Brenner DA, Loomba R, Smarr L, Sandborn WJ, Schnabl B, et al. Microbiome 101: studying, analyzing, and interpreting gut microbiome data for clinicians. Clin Gastroenterol Hepatol. 2019;17:218–230. doi: 10.1016/j.cgh.2018.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carr TF, Zeki AA, Kraft M. Eosinophilic and noneosinophilic asthma. Am J Respir Crit Care Med. 2018;197:22–37. doi: 10.1164/rccm.201611-2232PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brusselle GG, Maes T, Bracke KR. Eosinophils in the spotlight: eosinophilic airway inflammation in nonallergic asthma. Nat Med. 2013;19:977–979. doi: 10.1038/nm.3300. [DOI] [PubMed] [Google Scholar]
- 21.Maes T, Joos GF, Brusselle GG. Targeting interleukin-4 in asthma: lost in translation? Am J Respir Cell Mol Biol. 2012;47:261–270. doi: 10.1165/rcmb.2012-0080TR. [DOI] [PubMed] [Google Scholar]
- 22.van Veen IH, Ten Brinke A, Gauw SA, Sterk PJ, Rabe KF, Bel EH. Consistency of sputum eosinophilia in difficult-to-treat asthma: a 5-year follow-up study. J Allergy Clin Immunol. 2009;124:615–617. doi: 10.1016/j.jaci.2009.06.029. [DOI] [PubMed] [Google Scholar]
- 23.Walker JA, Barlow JL, McKenzie AN. Innate lymphoid cells--how did we miss them? Nat Rev Immunol. 2013;13:75–87. doi: 10.1038/nri3349. [DOI] [PubMed] [Google Scholar]
- 24.Pelly VS, Kannan Y, Coomes SM, Entwistle LJ, Rückerl D, Seddon B, MacDonald AS, McKenzie A, Wilson MS. IL-4-producing ILC2s are required for the differentiation of TH2 cells following Heligmosomoides polygyrus infection. Mucosal Immunol. 2016;9:1407–1417. doi: 10.1038/mi.2016.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Winkler C, Hochdörfer T, Israelsson E, Hasselberg A, Cavallin A, Thörn K, Muthas D, Shojaee S, Lüer K, Müller M, et al. Activation of group 2 innate lymphoid cells after allergen challenge in asthmatic patients. J Allergy Clin Immunol. 2019;144:61–69.e7. doi: 10.1016/j.jaci.2019.01.027. [DOI] [PubMed] [Google Scholar]
- 26.Kaur R, Chupp G. Phenotypes and endotypes of adult asthma: moving toward precision medicine. J Allergy Clin Immunol. 2019;144:1–12. doi: 10.1016/j.jaci.2019.05.031. [DOI] [PubMed] [Google Scholar]
- 27.Peters SP. Asthma phenotypes: nonallergic (intrinsic) asthma. J Allergy Clin Immunol Pract. 2014;2:650–652. doi: 10.1016/j.jaip.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 28.Baos S, Calzada D, Cremades-Jimeno L, Sastre J, Picado C, Quiralte J, Florido F, Lahoz C, Cárdaba B. Nonallergic asthma and its severity: biomarkers for its discrimination in peripheral samples. Front Immunol. 2018;9:1416. doi: 10.3389/fimmu.2018.01416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu L, Zhang X, Liu Y, Zhang L, Zheng J, Wang J, Hansbro PM, Wang L, Wang G, Hsu AC. Chitinase-like protein YKL-40 correlates with inflammatory phenotypes, anti-asthma responsiveness and future exacerbations. Respir Res. 2019;20:95. doi: 10.1186/s12931-019-1051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen JH, Qin L, Shi YY, Feng JT, Zheng YL, Wan YF, Xu CQ, Yang XM, Hu CP. IL-17 protein levels in both induced sputum and plasma are increased in stable but not acute asthma individuals with obesity. Respir Med. 2016;121:48–58. doi: 10.1016/j.rmed.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 31.Ntontsi P, Loukides S, Bakakos P, Kostikas K, Papatheodorou G, Papathanassiou E, Hillas G, Koulouris N, Papiris S, Papaioannou AI. Clinical, functional and inflammatory characteristics in patients with paucigranulocytic stable asthma: comparison with different sputum phenotypes. Allergy. 2017;72:1761–1767. doi: 10.1111/all.13184. [DOI] [PubMed] [Google Scholar]
- 32.Demarche S, Schleich F, Henket M, Paulus V, Van Hees T, Louis R. Detailed analysis of sputum and systemic inflammation in asthma phenotypes: are paucigranulocytic asthmatics really non-inflammatory? BMC Pulm Med. 2016;16:46. doi: 10.1186/s12890-016-0208-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Irvin C, Zafar I, Good J, Rollins D, Christianson C, Gorska MM, Martin RJ, Alam R. Increased frequency of dual-positive TH2/TH17 cells in bronchoalveolar lavage fluid characterizes a population of patients with severe asthma. J Allergy Clin Immunol. 2014;134:1175–1186.e7. doi: 10.1016/j.jaci.2014.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Simpson JL, Powell H, Boyle MJ, Scott RJ, Gibson PG. Clarithromycin targets neutrophilic airway inflammation in refractory asthma. Am J Respir Crit Care Med. 2008;177:148–155. doi: 10.1164/rccm.200707-1134OC. [DOI] [PubMed] [Google Scholar]
- 35.Ratner AJ, Lysenko ES, Paul MN, Weiser JN. Synergistic proinflammatory responses induced by polymicrobial colonization of epithelial surfaces. Proc Natl Acad Sci U S A. 2005;102:3429–3434. doi: 10.1073/pnas.0500599102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bachert C, Humbert M, Hanania NA, Zhang N, Holgate S, Buhl R, Bröker BM. Staphylococcus aureus and its IgE-inducing enterotoxins in asthma: current knowledge. Eur Respir J. 2020;55:1901592. doi: 10.1183/13993003.01592-2019. [DOI] [PubMed] [Google Scholar]
- 37.Huang YJ, Nariya S, Harris JM, Lynch SV, Choy DF, Arron JR, Boushey H. The airway microbiome in patients with severe asthma: associations with disease features and severity. J Allergy Clin Immunol. 2015;136:874–884. doi: 10.1016/j.jaci.2015.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Groneberg DA, Peiser C, Dinh QT, Matthias J, Eynott PR, Heppt W, Carlstedt I, Witt C, Fischer A, Chung KF. Distribution of respiratory mucin proteins in human nasal mucosa. Laryngoscope. 2003;113:520–524. doi: 10.1097/00005537-200303000-00023. [DOI] [PubMed] [Google Scholar]
- 39.Ali MS, Pearson JP. Upper airway mucin gene expression: a review. Laryngoscope. 2007;117:932–938. doi: 10.1097/MLG.0b013e3180383651. [DOI] [PubMed] [Google Scholar]
- 40.Takeyama K, Fahy JV, Nadel JA. Relationship of epidermal growth factor receptors to goblet cell production in human bronchi. Am J Respir Crit Care Med. 2001;163:511–516. doi: 10.1164/ajrccm.163.2.2001038. [DOI] [PubMed] [Google Scholar]
- 41.Mao YJ, Chen HH, Wang B, Liu X, Xiong GY. Increased expression of MUC5AC and MUC5B promoting bacterial biofilm formation in chronic rhinosinusitis patients. Auris Nasus Larynx. 2015;42:294–298. doi: 10.1016/j.anl.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 42.Dohrman A, Miyata S, Gallup M, Li JD, Chapelin C, Coste A, Escudier E, Nadel J, Basbaum C. Mucin gene (MUC 2 and MUC 5AC) upregulation by Gram-positive and Gram-negative bacteria. Biochim Biophys Acta. 1998;1406:251–259. doi: 10.1016/s0925-4439(98)00010-6. [DOI] [PubMed] [Google Scholar]
- 43.Shuter J, Hatcher VB, Lowy FD. Staphylococcus aureus binding to human nasal mucin. Infect Immun. 1996;64:310–318. doi: 10.1128/iai.64.1.310-318.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cohn L, Whittaker L, Niu N, Homer RJ. Cytokine regulation of mucus production in a model of allergic asthma. Novartis Found Symp. 2002;248:201–213. [PubMed] [Google Scholar]
- 45.Hiemstra PS, McCray PB, Jr, Bals R. The innate immune function of airway epithelial cells in inflammatory lung disease. Eur Respir J. 2015;45:1150–1162. doi: 10.1183/09031936.00141514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Niyonsaba F, Someya A, Hirata M, Ogawa H, Nagaoka I. Evaluation of the effects of peptide antibiotics human beta-defensins-1/-2 and LL-37 on histamine release and prostaglandin D(2) production from mast cells. Eur J Immunol. 2001;31:1066–1075. doi: 10.1002/1521-4141(200104)31:4<1066::aid-immu1066>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 47.Mahdavinia M, Keshavarzian A, Tobin MC, Landay AL, Schleimer RP. A comprehensive review of the nasal microbiome in chronic rhinosinusitis (CRS) Clin Exp Allergy. 2016;46:21–41. doi: 10.1111/cea.12666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vareille M, Kieninger E, Edwards MR, Regamey N. The airway epithelium: soldier in the fight against respiratory viruses. Clin Microbiol Rev. 2011;24:210–229. doi: 10.1128/CMR.00014-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zakeri A, Russo M. Dual role of Toll-like receptors in human and experimental asthma models. Front Immunol. 2018;9:1027. doi: 10.3389/fimmu.2018.01027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dong Z, Xiong L, Zhang W, Gibson PG, Wang T, Lu Y, Wang G, Li H, Wang F. Holding the inflammatory system in check: TLRs and their targeted therapy in asthma. Mediators Inflamm. 2016;2016:2180417. doi: 10.1155/2016/2180417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Losol P, Kim SH, Ahn S, Lee S, Choi JP, Kim YH, Hong SJ, Kim BS, Chang YS. Genetic variants in the TLR-related pathway and smoking exposure alter the upper airway microbiota in adult asthmatic patients. Allergy. 2021 doi: 10.1111/all.14970. [DOI] [PubMed] [Google Scholar]
- 52.Askarian F, Wagner T, Johannessen M, Nizet V. Staphylococcus aureus modulation of innate immune responses through Toll-like (TLR), (NOD)-like (NLR) and C-type lectin (CLR) receptors. FEMS Microbiol Rev. 2018;42:656–671. doi: 10.1093/femsre/fuy025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ritchie ND, Ijaz UZ, Evans TJ. IL-17 signalling restructures the nasal microbiome and drives dynamic changes following Streptococcus pneumoniae colonization. BMC Genomics. 2017;18:807. doi: 10.1186/s12864-017-4215-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baba S, Kagoya R, Kondo K, Suzukawa M, Ohta K, Yamasoba T. T-cell phenotypes in chronic rhinosinusitis with nasal polyps in Japanese patients. Allergy Asthma Clin Immunol. 2015;11:33. doi: 10.1186/s13223-015-0100-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jackson DJ, Makrinioti H, Rana BM, Shamji BW, Trujillo-Torralbo MB, Footitt J, Del-Rosario J, Telcian AG, Nikonova A, Zhu J, et al. IL-33-dependent type 2 inflammation during rhinovirus-induced asthma exacerbations in vivo . Am J Respir Crit Care Med. 2014;190:1373–1382. doi: 10.1164/rccm.201406-1039OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Walford HH, Lund SJ, Baum RE, White AA, Bergeron CM, Husseman J, Bethel KJ, Scott DR, Khorram N, Miller M, et al. Increased ILC2s in the eosinophilic nasal polyp endotype are associated with corticosteroid responsiveness. Clin Immunol. 2014;155:126–135. doi: 10.1016/j.clim.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.de Steenhuijsen Piters WA, Sanders EA, Bogaert D. The role of the local microbial ecosystem in respiratory health and disease. Philos Trans R Soc Lond B Biol Sci. 2015;370:20140294. doi: 10.1098/rstb.2014.0294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen CH, Wang Y, Nakatsuji T, Liu YT, Zouboulis C, Gallo R, Zhang L, Hsieh MF, Huang CM. An innate bactericidal oleic acid effective against skin infection of methicillin-resistant Staphylococcus aureus: a therapy concordant with evolutionary medicine. J Microbiol Biotechnol. 2011;21:391–399. [PubMed] [Google Scholar]
- 59.Harriott MM, Noverr MC. Candida albicans and Staphylococcus aureus form polymicrobial biofilms: effects on antimicrobial resistance. Antimicrob Agents Chemother. 2009;53:3914–3922. doi: 10.1128/AAC.00657-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bellinghausen C, Gulraiz F, Heinzmann AC, Dentener MA, Savelkoul PH, Wouters EF, Rohde GG, Stassen FR. Exposure to common respiratory bacteria alters the airway epithelial response to subsequent viral infection. Respir Res. 2016;17:68. doi: 10.1186/s12931-016-0382-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486:207–214. doi: 10.1038/nature11234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhou Y, Mihindukulasuriya KA, Gao H, La Rosa PS, Wylie KM, Martin JC, Kota K, Shannon WD, Mitreva M, Sodergren E, et al. Exploration of bacterial community classes in major human habitats. Genome Biol. 2014;15:R66. doi: 10.1186/gb-2014-15-5-r66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Biswas K, Hoggard M, Jain R, Taylor MW, Douglas RG. The nasal microbiota in health and disease: variation within and between subjects. Front Microbiol. 2015;9:134. doi: 10.3389/fmicb.2018.00134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Polosa R, Thomson NC. Smoking and asthma: dangerous liaisons. Eur Respir J. 2013;41:716–726. doi: 10.1183/09031936.00073312. [DOI] [PubMed] [Google Scholar]
- 65.Ito K, Lim S, Caramori G, Chung KF, Barnes PJ, Adcock IM. Cigarette smoking reduces histone deacetylase 2 expression, enhances cytokine expression, and inhibits glucocorticoid actions in alveolar macrophages. FASEB J. 2001;15:1110–1112. [PubMed] [Google Scholar]
- 66.Arnson Y, Shoenfeld Y, Amital H. Effects of tobacco smoke on immunity, inflammation and autoimmunity. J Autoimmun. 2010;34:J258–JJ265. doi: 10.1016/j.jaut.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 67.Sapkota AR, Berger S, Vogel TM. Human pathogens abundant in the bacterial metagenome of cigarettes. Environ Health Perspect. 2010;118:351–356. doi: 10.1289/ehp.0901201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.De Boeck I, Wittouck S, Wuyts S, Oerlemans EF, van den Broek MF, Vandenheuvel D, Vanderveken O, Lebeer S. Comparing the healthy nose and nasopharynx microbiota reveals continuity as well as niche-specificity. Front Microbiol. 2017;8:2372. doi: 10.3389/fmicb.2017.02372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Qin T, Zhang F, Zhou H, Ren H, Du Y, Liang S, Wang F, Cheng L, Xie X, Jin A, et al. High-level PM2.5/PM10 exposure is associated with alterations in the human pharyngeal microbiota composition. Front Microbiol. 2019;10:54. doi: 10.3389/fmicb.2019.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Charlson ES, Chen J, Custers-Allen R, Bittinger K, Li H, Sinha R, Hwang J, Bushman FD, Collman RG. Disordered microbial communities in the upper respiratory tract of cigarette smokers. PLoS One. 2010;5:e15216. doi: 10.1371/journal.pone.0015216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Munck C, Helby J, Westergaard CG, Porsbjerg C, Backer V, Hansen LH. Smoking cessation and the microbiome in induced sputum samples from cigarette smoking asthma patients. PLoS One. 2016;11:e0158622. doi: 10.1371/journal.pone.0158622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Huang C, Shi G. Smoking and microbiome in oral, airway, gut and some systemic diseases. J Transl Med. 2019;17:225. doi: 10.1186/s12967-019-1971-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383:1581–1592. doi: 10.1016/S0140-6736(14)60617-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.De Grove KC, Provoost S, Brusselle GG, Joos GF, Maes T. Insights in particulate matter-induced allergic airway inflammation: focus on the epithelium. Clin Exp Allergy. 2018;48:773–786. doi: 10.1111/cea.13178. [DOI] [PubMed] [Google Scholar]
- 75.Liu H, Zhang X, Zhang H, Yao X, Zhou M, Wang J, He Z, Zhang H, Lou L, Mao W, et al. Effect of air pollution on the total bacteria and pathogenic bacteria in different sizes of particulate matter. Environ Pollut. 2018;233:483–493. doi: 10.1016/j.envpol.2017.10.070. [DOI] [PubMed] [Google Scholar]
- 76.Mostafavi N, Jeong A, Vlaanderen J, Imboden M, Vineis P, Jarvis D, Kogevinas M, Probst-Hensch N, Vermeulen R. The mediating effect of immune markers on the association between ambient air pollution and adult-onset asthma. Sci Rep. 2019;9:8818. doi: 10.1038/s41598-019-45327-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Whelan R, Kim C, Chen M, Leiter J, Grunstein MM, Hakonarson H. Role and regulation of interleukin-1 molecules in pro-asthmatic sensitised airway smooth muscle. Eur Respir J. 2004;24:559–567. doi: 10.1183/09031936.04.00133803. [DOI] [PubMed] [Google Scholar]
- 78.Godwin MS, Reeder KM, Garth JM, Blackburn JP, Jones M, Yu Z, Matalon S, Hastie AT, Meyers DA, Steele C. IL-1RA regulates immunopathogenesis during fungal-associated allergic airway inflammation. JCI Insight. 2019;4:e129055. doi: 10.1172/jci.insight.129055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Igartua C, Davenport ER, Gilad Y, Nicolae DL, Pinto J, Ober C. Host genetic variation in mucosal immunity pathways influences the upper airway microbiome. Microbiome. 2017;5:16. doi: 10.1186/s40168-016-0227-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lee JJ, Kim SH, Lee MJ, Kim BK, Song WJ, Park HW, Cho SH, Hong SJ, Chang YS, Kim BS. Different upper airway microbiome and their functional genes associated with asthma in young adults and elderly individuals. Allergy. 2019;74:709–719. doi: 10.1111/all.13608. [DOI] [PubMed] [Google Scholar]
- 81.Gan W, Yang F, Tang Y, Zhou D, Qing D, Hu J, Liu S, Liu F, Meng J. The difference in nasal bacterial microbiome diversity between chronic rhinosinusitis patients with polyps and a control population. Int Forum Allergy Rhinol. 2019;9:582–592. doi: 10.1002/alr.22297. [DOI] [PubMed] [Google Scholar]
- 82.Chalermwatanachai T, Vilchez-Vargas R, Holtappels G, Lacoere T, Jáuregui R, Kerckhof FM, Pieper DH, Van de Wiele T, Vaneechoutte M, Van Zele T, et al. Chronic rhinosinusitis with nasal polyps is characterized by dysbacteriosis of the nasal microbiota. Sci Rep. 2018;8:7926. doi: 10.1038/s41598-018-26327-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Losol P, Kim SH, Hwang EK, Shin YS, Park HS. IL-5 promoter polymorphism enhances IgE responses to staphylococcal superantigens in adult asthmatics. Allergy Asthma Immunol Res. 2013;5:106–109. doi: 10.4168/aair.2013.5.2.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ramakrishnan VR, Hauser LJ, Feazel LM, Ir D, Robertson CE, Frank DN. Sinus microbiota varies among chronic rhinosinusitis phenotypes and predicts surgical outcome. J Allergy Clin Immunol. 2015;136:334–342.e1. doi: 10.1016/j.jaci.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 85.Hilty M, Burke C, Pedro H, Cardenas P, Bush A, Bossley C, Davies J, Ervine A, Poulter L, Pachter L, et al. Disordered microbial communities in asthmatic airways. PLoS One. 2010;5:e8578. doi: 10.1371/journal.pone.0008578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fazlollahi M, Lee TD, Andrade J, Oguntuyo K, Chun Y, Grishina G, Grishin A, Bunyavanich S. The nasal microbiome in asthma. J Allergy Clin Immunol. 2018;142:834–843.e2. doi: 10.1016/j.jaci.2018.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yang HJ, LoSavio PS, Engen PA, Naqib A, Mehta A, Kota R, Khan RJ, Tobin MC, Green SJ, Schleimer RP, et al. Association of nasal microbiome and asthma control in patients with chronic rhinosinusitis. Clin Exp Allergy. 2018;48:1744–1747. doi: 10.1111/cea.13255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhang Q, Cox M, Liang Z, Brinkmann F, Cardenas PA, Duff R, Bhavsar P, Cookson W, Moffatt M, Chung KF. Airway microbiota in severe asthma and relationship to asthma severity and phenotypes. PLoS One. 2016;11:e0152724. doi: 10.1371/journal.pone.0152724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Denner DR, Sangwan N, Becker JB, Hogarth DK, Oldham J, Castillo J, Sperling AI, Solway J, Naureckas ET, Gilbert JA, et al. Corticosteroid therapy and airflow obstruction influence the bronchial microbiome, which is distinct from that of bronchoalveolar lavage in asthmatic airways. J Allergy Clin Immunol. 2016;137:1398–1405.e3. doi: 10.1016/j.jaci.2015.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Biesbroek G, Tsivtsivadze E, Sanders EA, Montijn R, Veenhoven RH, Keijser BJ, Bogaert D. Early respiratory microbiota composition determines bacterial succession patterns and respiratory health in children. Am J Respir Crit Care Med. 2014;190:1283–1292. doi: 10.1164/rccm.201407-1240OC. [DOI] [PubMed] [Google Scholar]
- 91.Ta LDH, Yap GC, Tay CJX, Lim ASM, Huang CH, Chu CW, De Sessions PF, Shek LP, Goh A, Van Bever HPS, et al. Establishment of the nasal microbiota in the first 18 months of life: correlation with early-onset rhinitis and wheezing. J Allergy Clin Immunol. 2018;142:86–95. doi: 10.1016/j.jaci.2018.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Miraglia Del Giudice M, Indolfi C, Capasso M, Maiello N, Decimo F, Ciprandi G. Bifidobacterium mixture (B longum BB536, B infantis M-63, B breve M-16V) treatment in children with seasonal allergic rhinitis and intermittent asthma. Ital J Pediatr. 2017;43:25. doi: 10.1186/s13052-017-0340-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Martens K, Pugin B, De Boeck I, Spacova I, Steelant B, Seys SF, Lebeer S, Hellings PW. Probiotics for the airways: potential to improve epithelial and immune homeostasis. Allergy. 2018;73:1954–1963. doi: 10.1111/all.13495. [DOI] [PubMed] [Google Scholar]
- 94.Ishida Y, Nakamura F, Kanzato H, Sawada D, Hirata H, Nishimura A, Kajimoto O, Fujiwara S. Clinical effects of Lactobacillus acidophilus strain L-92 on perennial allergic rhinitis: a double-blind, placebo-controlled study. J Dairy Sci. 2005;88:527–533. doi: 10.3168/jds.S0022-0302(05)72714-4. [DOI] [PubMed] [Google Scholar]
- 95.Xu LZ, Yang LT, Qiu SQ, Yang G, Luo XQ, Miao BP, Geng XR, Liu ZQ, Liu J, Wen Z, et al. Combination of specific allergen and probiotics induces specific regulatory B cells and enhances specific immunotherapy effect on allergic rhinitis. Oncotarget. 2016;7:54360–54369. doi: 10.18632/oncotarget.10946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Singh A, Hacini-Rachinel F, Gosoniu ML, Bourdeau T, Holvoet S, Doucet-Ladeveze R, Beaumont M, Mercenier A, Nutten S. Immune-modulatory effect of probiotic Bifidobacterium lactis NCC2818 in individuals suffering from seasonal allergic rhinitis to grass pollen: an exploratory, randomized, placebo-controlled clinical trial. Eur J Clin Nutr. 2013;67:161–167. doi: 10.1038/ejcn.2012.197. [DOI] [PubMed] [Google Scholar]
- 97.Dennis-Wall JC, Culpepper T, Nieves C, Jr, Rowe CC, Burns AM, Rusch CT, Federico A, Ukhanova M, Waugh S, Mai V, et al. Probiotics (Lactobacillus gasseri KS-13, Bifidobacterium bifidum G9-1, and Bifidobacterium longum MM-2) improve rhinoconjunctivitis-specific quality of life in individuals with seasonal allergies: a double-blind, placebo-controlled, randomized trial. Am J Clin Nutr. 2017;105:758–767. doi: 10.3945/ajcn.116.140012. [DOI] [PubMed] [Google Scholar]
- 98.Mårtensson A, Greiff L, Lamei SS, Lindstedt M, Olofsson TC, Vasquez A, Cervin A. Effects of a honeybee lactic acid bacterial microbiome on human nasal symptoms, commensals, and biomarkers. Int Forum Allergy Rhinol. 2016;6:956–963. doi: 10.1002/alr.21762. [DOI] [PubMed] [Google Scholar]
- 99.Pérez-Cobas AE, Gosalbes MJ, Friedrichs A, Knecht H, Artacho A, Eismann K, Otto W, Rojo D, Bargiela R, von Bergen M, et al. Gut microbiota disturbance during antibiotic therapy: a multi-omic approach. Gut. 2013;62:1591–1601. doi: 10.1136/gutjnl-2012-303184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Suzuki H, Shimomura A, Ikeda K, Furukawa M, Oshima T, Takasaka T. Inhibitory effect of macrolides on interleukin-8 secretion from cultured human nasal epithelial cells. Laryngoscope. 1997;107:1661–1666. doi: 10.1097/00005537-199712000-00016. [DOI] [PubMed] [Google Scholar]
- 101.Desaki M, Takizawa H, Ohtoshi T, Kasama T, Kobayashi K, Sunazuka T, Omura S, Yamamoto K, Ito K. Erythromycin suppresses nuclear factor-kappaB and activator protein-1 activation in human bronchial epithelial cells. Biochem Biophys Res Commun. 2000;267:124–128. doi: 10.1006/bbrc.1999.1917. [DOI] [PubMed] [Google Scholar]
- 102.Ferrer M, Méndez-García C, Rojo D, Barbas C, Moya A. Antibiotic use and microbiome function. Biochem Pharmacol. 2017;134:114–126. doi: 10.1016/j.bcp.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 103.de Oliveira IS, Borges Crosara PF, Cassali GD, Dos Reis DC, Rodrigues DS, Nunes FB, Guimarães RE. Azithromycin for the treatment of eosinophilic nasal polyposis: clinical and histologic analysis. Allergy Rhinol (Providence) 2016;7:55–61. doi: 10.2500/ar.2016.7.0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gibson PG, Yang IA, Upham JW, Reynolds PN, Hodge S, James AL, Jenkins C, Peters MJ, Marks GB, Baraket M, et al. Effect of azithromycin on asthma exacerbations and quality of life in adults with persistent uncontrolled asthma (AMAZES): a randomised, double-blind, placebo-controlled trial. Lancet. 2017;390:659–668. doi: 10.1016/S0140-6736(17)31281-3. [DOI] [PubMed] [Google Scholar]
- 105.Johnston SL, Szigeti M, Cross M, Brightling C, Chaudhuri R, Harrison T, Mansur A, Robison L, Sattar Z, Jackson D, et al. Azithromycin for acute exacerbations of asthma: the AZALEA randomized clinical trial. JAMA Intern Med. 2016;176:1630–1637. doi: 10.1001/jamainternmed.2016.5664. [DOI] [PubMed] [Google Scholar]
- 106.Feazel LM, Robertson CE, Ramakrishnan VR, Frank DN. Microbiome complexity and Staphylococcus aureus in chronic rhinosinusitis. Laryngoscope. 2012;122:467–472. doi: 10.1002/lary.22398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Liu CM, Soldanova K, Nordstrom L, Dwan MG, Moss OL, Contente-Cuomo TL, Keim P, Price LB, Lane AP. Medical therapy reduces microbiota diversity and evenness in surgically recalcitrant chronic rhinosinusitis. Int Forum Allergy Rhinol. 2013;3:775–781. doi: 10.1002/alr.21195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yao J, Carter RA, Vuagniaux G, Barbier M, Rosch JW, Rock CO. A pathogen-selective antibiotic minimizes disturbance to the microbiome. Antimicrob Agents Chemother. 2016;60:4264–4273. doi: 10.1128/AAC.00535-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lohia S, Schlosser RJ, Soler ZM. Impact of intranasal corticosteroids on asthma outcomes in allergic rhinitis: a meta-analysis. Allergy. 2013;68:569–579. doi: 10.1111/all.12124. [DOI] [PubMed] [Google Scholar]
- 110.Ramakrishnan VR, Holt J, Nelson LF, Ir D, Robertson CE, Frank DN. Determinants of the nasal microbiome: pilot study of effects of intranasal medication use. Allergy Rhinol (Providence) 2018;9:2152656718789519. doi: 10.1177/2152656718789519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chung KF. Airway microbial dysbiosis in asthmatic patients: a target for prevention and treatment? J Allergy Clin Immunol. 2017;139:1071–1081. doi: 10.1016/j.jaci.2017.02.004. [DOI] [PubMed] [Google Scholar]