Abstract
The Ready Steady 3.0 trial is designed to test the main and interactive effects of two behavior change intervention components, within an 8-week physical activity intervention, on older adults’ physical activity (PA). Each component is comprised of behavior change strategies that emphasize two different evidence-based ways to motivate older adults to be active: interpersonal and intrapersonal. 308 adults ≥ 70 years old will be randomized to 1 of 4 conditions in a 2 × 2 full factorial trial in which the two factors represent the receipt (No, Yes) of interpersonal or intrapersonal behavior change strategies. Participants will also receive two core intervention components: the Otago Exercise Program adapted for small groups and a PA monitor. Interventions across conditions will be delivered during 8 weekly, small group, meetings in community settings. The primary outcome of PA, measured objectively, and secondary outcomes of falls and the quality of life will be assessed at baseline and post-intervention: 1 week, 6 months, and 12 months. Findings will enable the identification of behavior change content that contributes to physical activity outcomes within a physical activity intervention for older adults. This study is one of the first to use the MOST framework to guide the development of a community-based physical activity intervention for older adults to reduce the public health problems of low PA and falls. The results will enable the optimization of behavior change content within a PA intervention for older adults and, in turn, other PA interventions for older adults.
Keywords: Older persons, Fall Prevention, Physical Activity, Multi-phase Optimization Strategy, Behavior Change
1. Introduction
Every year, 1 in 4 people aged 65 and older fall.1 Twenty-five percent of these falls cause injury or death2 and have devastating effects on quality of life.3 Evidence-based exercises that target increased leg-strength and balance effectively reduce falls and related injuries.4 However, less than 14% of older adults perform these exercises regularly,5 and fall rates remain high across older adult populations.1,2,6 This knowledge-behavior gap is in part due to the scarce and inconclusive evidence regarding which behavior change strategies motivate the increased performance of physical activity in older adults. In this paper, we describe the protocol for a randomized optimization trial (Ready Steady 3.0) to identify behavior change strategies within a physical activity intervention that elicit sustained increases in physical activity among community-dwelling adults who are ≥ 70 years old.
Although evidence generated in the field of falls prevention identifies the types of exercises that effectively prevent falls (balance-challenging, leg-strengthening),4 it does not identify the types of strategies that effectively motivate behavior change in older adults.7 Thus, while it is known which physical activity content should be included in interventions for older adults, it is not known which behavior change content should be included.8,9 We aim to optimize behavior change content within a promising physical activity intervention with guidance from the engineering-inspired Multiphase Optimization Strategy (MOST) framework.10
The MOST framework includes phases for preparing, optimizing, and evaluating multicomponent behavioral interventions.10 The intervention we aim to optimize was prepared by first separating its behavior change strategies into two sets: interpersonal and intrapersonal, based on theories of behavior change11,12 and life span development13 as well as prior research.9,14 The interpersonal strategies emphasize interactions, such as social support and social comparison. The intrapersonal strategies emphasize personal reflection and considerations such as goal setting and action planning. Results from our preparation study showed that it was feasible to deliver both sets of strategies, together or independently, to small groups of older adults as part of a community-based physical activity intervention.15 Additionally, we found that participants who received the interpersonal component, compared to those who did not, increased their physical activity for up to 6 months post-intervention. Although the preparation study confirmed both sets of behavior change strategies as candidate intervention components, it had limitations. Results did not show the effects of behavior change components on sustained changes in physical activity (e.g., > 6 months), falls, or quality of life in older adults--all essential outcomes for identifying active intervention component(s).
Thus, the study protocol described in this paper builds upon our earlier study with three enhancements: increased sample size, extended follow-up time, and additional relevant outcomes. The objective of this trial is to examine the effects of the interpersonal and intrapersonal behavior change intervention components on older adults’ physical activity, fall rates, and quality of life for up to 12 months, via a full 2×2 factorial experiment (See Table 1). The results will allow for the optimization of behavior change content within an 8-week physical activity intervention and, in turn, other physical activity interventions for older adults.
Table 1.
2×2 Factorial Study Design
| Core Components | Experimental Components | |||
|---|---|---|---|---|
| Condition | Otago Exercise | Physical Activity | Interpersonal | Intrapersonal |
| Program* | Monitor | BCS | BCS | |
| 1 | Yes | Yes | No | No |
| 2 | Yes | Yes | Yes | No |
| 3 | Yes | Yes | No | Yes |
| 4 | Yes | Yes | Yes | Yes |
Notes: Adapted for small groups, BCS = Behavior Change Strategies
2. Methods
2.1. Study overview and aims
The design and protocol for this study adhere to the Consolidated Standards of Reporting -Social and Psychological Intervention Trials (CONSORT-SPI 2018)16 and is registered with ClinicalTrials.gov (Identifier: NCT03326141). Three hundred and eight community-dwelling older adults will be enrolled and randomized to 1 of 4 conditions, which represent distinct combinations of the core and experimental intervention components (Table 1). Enrollment will occur in phases so that the 8-week intervention can be delivered simultaneously to participants in all 4 conditions. To do this we will enroll 13 cohorts each comprised of 16 to 24 participants over 60 months: approximately one cohort per quarter between November 2017 and August 2021.1
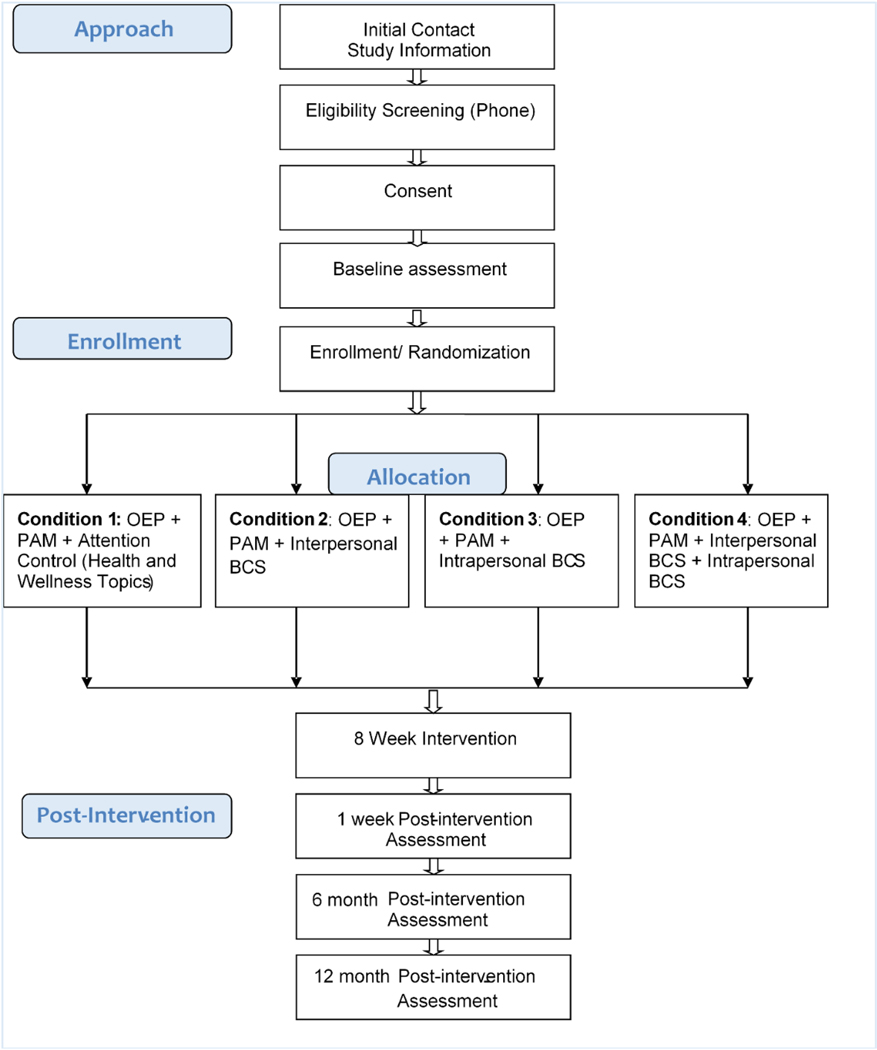
Study participants’ physical activity, falls, quality of life and targeted mechanisms of action will be assessed at baseline and three time points post-intervention: one week, 6 months, and 12 months. Figure 1 summarizes participant flow through the study. Informed consent will be obtained from all participants. This study is approved by the University of Minnesota’s Institutional Review Board (IRB # 1607S90922).
Figure 1.
Study Flow Diagram.
Notes: OEP = Otago Exercise Program adapted for small groups; PAM = Physical Activity Monitor; BCS = Behavior Change Strategies
A conceptual model for this study (See Figure 2) illustrates the main intervention content as two core components (a physical activity protocol and monitor) and two experimental components (sets of interpersonal and intrapersonal behavior change strategies), and their linkages to constructs targeted as putative mechanisms of action and outcomes. The intervention is based on the wellness motivation theory (WMT), which posits that social contextual resources such as environmental and social support, and behavioral change processes such as self-knowledge, readiness, self-regulation, influence older adults’ health-related actions, including physical activity.11
Figure 2.
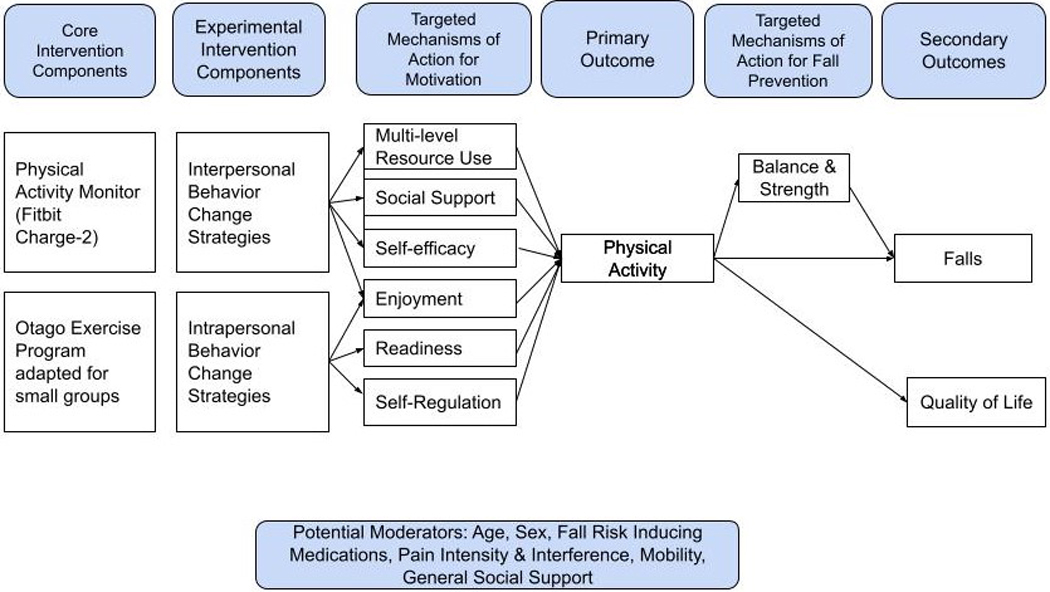
Intervention Conceptual Model
A 2×2 full factorial experimental design will be used to test the effects of the experimental components. The two factors represent the receipt (No versus Yes) of the experimental components comprised of interpersonal behavior change strategies (e.g., social support) and intrapersonal behavior change strategies (e.g., goal setting). The full factorial design will enable simultaneous tests of the main and interaction effects of the experimental intervention components.17 Other research designs are appropriate for comparing a whole intervention package to a control group, or determining if a single component is best by comparing simple effects of individual components to a control arm (e.g., multiple arm comparative experiment). However, such designs are inefficient when investigating the relative contributions of more than one experimental intervention component.17 The factorial experiment design used in this study will enable us to identify which components meaningfully contribute to outcomes using the criterion10 of a positive effect on sustained increases in physical activity, falls prevention, and quality of life.
2.2. The aims of this study are to:
Determine which behavior change intervention components increase physical activity among community- dwelling older adults at three time points post-intervention: 1 week, 6 months, and 12 months. We hypothesize that participants receiving the interpersonal component (conditions 2 and 4 in Table 1) will have clinically meaningful increases in physical activity post-intervention (at all 3 time-points), compared to those not receiving this component (conditions 1, 3 Table 1).
Determine which intervention components decrease fall occurrence and increase quality of life among community-dwelling older adults. We hypothesize that participants receiving the interpersonal component will have clinically meaningful reductions in falls and increases in quality of life, 12 months post intervention, compared to those not receiving this component.
Evaluate intervention component effects on constructs targeted as putative mechanisms of action: motivational constructs (environmental support; social support; readiness; self-efficacy; enjoyment; self-regulation) and physical markers of fall risk (functional leg strength and balance), and whether these mechanisms mediate the intervention component effects on physical activity and falls.
2.3. Setting
This study will be conducted at the University of Minnesota and in community centers across Minneapolis and Saint Paul, Minnesota. Research staff will conduct telephone screening and coordinate study communications, meetings, and reports in research offices at the University of Minnesota, School of Nursing. Assessments and intervention meetings with participants will be conducted in community centers in Minneapolis and Saint Paul. Our research team has longstanding partnerships with several centers that have goals to promote physical activity and prevent falls among older adults. Each community center values service to diverse populations in easily accessible locations and can host small gatherings in meeting rooms.
2.4. Participants
2.4.1. Entrance Criteria
Entrance criteria will be broad, consistent with recommendations to promote physical activity across older adult populations, including those with frailty, multiple chronic conditions, and pain.18 The inclusion criteria will consist of: a) the ability to speak English; b) age ≥ 70 years old; c) the ability to walk (with or without an aid); d) self-reported performance of strength training exercises less than twice per week, balance-challenging exercises less than three times per week, and endurance activity (light, moderate, vigorous) less than 150 minutes per week,19 and e) the presence of at least one self-reported risk for falls.20 Additionally, we will administer the Exercise and Screening for You.21 Potential participants who respond “Yes” to questions about current untreated cardiovascular symptoms, frequent falls, or dizziness, must obtain clearance from their primary care provider. The exclusion criteria will consist of: a) lower extremity injury or surgery within the last six weeks and b) self-reported diagnosis of a neurocognitive disorder, or a score of < 4 on the Callahan Cognitive screener,22 because the current intervention does not include tailoring or adaptations for these conditions which impede a person’s ability to implement the intervention content.
2.4.2. Recruitment, screening, and informed consent
Community-dwelling adults who are ≥ 70 years old will be recruited using several approaches. We will place advertisements in local newspapers, on Facebook, and in church bulletins near community centers that host the study meetings. We will also present information about the study at local wellness fairs and community centers and display fliers in local businesses frequented by older adults, such as coffee shops, clinics, and coops. Finally, details about our study will be maintained on two University of Minnesota websites. One website will be dedicated to information about our research and community partners. The other will be the University’s Study Finder,23 which helps individuals quickly and easily identify contacts for all studies that need volunteers. All advertisements, fliers, and websites will direct potential participants to contact the research team via a study-dedicated phone number or email address. A trained researcher will then inform potential participants about the research.
Interested potential participants will be screened for study eligibility via telephone interviews, guided by a screening case report form in Research Electronic Data Capture (REDCap). This form will include questions that address each entrance criteria and the potential participant’s availability. Eligible participants will be mailed a consent form and letter about the study and will also be scheduled for the consenting procedure and the baseline assessment.
Before baseline assessments, researcher staff will review and discuss the consent with potential participants, focusing on the study’s purpose, procedures, risks, benefits, and options. Researcher staff will encourage potential participants, their families, partners, and providers to ask questions or meet privately with the principal investigator to further clarify questions or express concerns about the study. Potential participants will provide written and verbal consent before proceeding with baseline assessments and data collection. Copies of each written consent will be shared with the participant and filed in an electronic consent case report form within REDCap.
2.4.4. Retention
We will encourage retention through communication and participant-centered scheduling. We will provide participants with written and verbal communication as they progress through each study event. We will also address questions and requests from participants’ as they occur. To do this, we will staff the study-dedicated phone and email from 8 am to 5 pm Monday through Friday. All meetings with participants will be scheduled according to their availability and will be adjusted upon request. If a participant misses an intervention or assessment meeting, the study staff will attempt to contact them at least five times using at least two methods (e.g., phone, text, email, US mail). Thank-you cards will be given to participants after each assessment and greeting cards will also be sent to participants on special occasions (e.g., birthdays). Finally, transportation to meetings will be coordinated and subsidized upon request.
2.5. Intervention
The dose of the intervention, 8-weeks with 8 weekly contacts lasting 90 minutes each, is based on triangulated data from prior research and feedback from community stakeholders.14 The Centers for Disease Control and Prevention compendium of evidence-based fall prevention interventions describes a broad range of intervention doses that elicit positive effects.24 Results from our preparation studies show that intervention session attendance to our eight-week course was good across conditions.14,15 Participants indicated this dose was acceptable during post-intervention interviews. Community stakeholders, including older adults, center leaders, and healthcare providers, advised us that contacts should be 90 minutes (not 60) to ensure participants did not feel “rushed,” and encouraged us to conduct the intervention meetings between 9 am and 4 pm to groups of 4 to 6 people.
The social milieu in each 90-minute meeting will support friendly interactions, discussions, and time for reflection guided by the course curricula that vary by study condition. Across conditions, week one will include an orientation to the course, expectations, safety, and resources. The curricula for weeks two through eight are organized such that each 90-minute contact, across conditions, dedicates a comparable number of minutes to the Otago Exercise Program (OEP) adapted for small groups, and the behavior change content or the attention control content. Each interventionist manual, organized by weekly meeting, will include objectives with scripted delivery tactics and activities, as well as timing for each. One interventionist with experience leading small groups and training for this intervention will facilitate meetings for all study conditions, according to curricula and manuals. Trained research assistants, who do not have assessment or data collection responsibilities, will assist with intervention processes such as scheduling meetings, setting up and cleaning up meeting spaces, and managing meeting materials.
Participants will receive workbooks with five main sections: contact information, safety, physical activity monitor information, weekly meeting information, and the original OEP diagrams with instructions, which were copy-edited with permission to have an appearance that is consistent with the rest of the workbook. Content in the weekly meeting section will vary according to the four study conditions. Content in interventionist manuals and participant workbooks will be augmented with pre-designed flipcharts that are also organized by condition and meeting. All content (experimental, attention control, core) is summarized in the next six paragraphs and in Table 2.
Table 2.
Intervention content by condition and week
| Intervention Condition | ||||
|---|---|---|---|---|
| Meeting | Health and Wellness+OEP | Interpersonal BCS+ OEP | Intrapersonal BCS+ OEP | Interpersonal BCS+Intrapersonal BCS +OEP |
| Week 1 | Orientation | Orientation | Orientation | Orientation |
| Safety | Safety | Safety | Safety | |
| OEP | OEP | OEP | OEP | |
| Week 2 | Safety | Safety | Safety | Safety |
| Reducing Falls | Managing Environmental Barriers: I | Managing Personal Barriers: I | Managing Environmental & Personal barriers: I | |
| OEP | OEP | OEP | OEP | |
| Week 3 | Technical QA | Technical QA | Technical QA | Technical QA |
| Pain | Friendly Social Comparison: I | Goal Setting | Goal Setting Friendly Social Comparison: I |
|
| OEP | OEP | OEP | OEP | |
| Week 4 | Technical QA | Technical QA | Technical QA | Technical QA |
| Supplements | Prompts & Cues: I | Building a Habit: I | Building a Habit: I Prompts & Cues: I | |
| OEP | OEP | OEP | OEP | |
| Week 5 | Technical QA | Technical QA | Technical QA | Social Support for Exercise |
| Sleep | Social Support for Exercise | Action Planning | Action Planning | |
| OEP | OEP | OEP | OEP | |
| Week 6 | Technical QA | Technical QA | Technical QA | Technical QA |
| Memory | Managing Environmental Barriers: II | Managing Personal Barriers: II | Managing Environmental Barriers: II | |
| OEP | OEP | OEP | OEP | |
| Week 7 | Technical QA | Technical QA | Technical QA | Identify self as a role model |
| Hearing | Identify Self as a Role Model Friendly Social Comparison II |
Self-Assessment (goals & action plan) | Friendly Social Comparison II Self-Assessment (goals & action plan) |
|
| OEP | OEP | OEP | OEP | |
| Week 8 | Technical QA | Technical QA | Technical QA | Prompts & Cues: II |
| Vaccinations | Prompts & Cues:I | Building a Habit:II | Building a Habit: II | |
| OEP | OEP | OEP | OEP | |
Notes: OEP = Otago Exercise Program adapted for small groups, BCS = Behavior Change Strategies, Technical QA = technical questions about the exercises and/ or the physical activity monitors, PA = Physical activity
2.5.1. Core Intervention Components
2.5.1.1. Otago Exercise Program (OEP) adapted for small groups
Our decision to use the OEP as the physical activity component in this study was based on evidence and practicality. The OEP was successfully used in our prior studies.14,15 It requires the least number of contacts among the evidence-based, fall-reducing physical activity interventions.7 It is safe and cost-effective25 when delivered to individuals and small groups in a variety of settings by a variety of providers.26,27 Individuals who perform the OEP as recommended increase their functional balance and leg strength, and in turn, decrease their fall risk.25
The OEP includes guidance for four types of exercise: balance-challenging, leg-strengthening, flexibility, and endurance 28. The 11 OEP balance-challenging exercises include knee bends (4 levels of difficulty), backward walking (2 levels), walking and turning (2 levels), sideways walking (2 levels), heel-toe stand (2 levels), heel-toe walking forward (2 levels), one leg stands (3 levels), heel walking (2 levels), toe walking, heel-toe walking backward (1 level), sit to stand (4 levels), and stair-walking (1 level). The five leg-strengthening exercises include the front knee (knee extensor, 4 levels), back knee (knee flexor, 4 levels), side hip (hip abductor, 4 levels), calf raise (ankle plantar flexors, 2 levels), and toe raise (ankle dorsiflexors, 2 levels). The five flexibility exercises include back extensions, ankle movements, head movements, neck movements, and trunk movements. Finally, the OEP includes guidance for encouraging endurance excercise and physical activity, such as walking at a comfortable pace. Thus, we will also encourage participants to increase their walking time by 10 to 20% of their current average -every 2 to 4 weeks.
Finally, the OEP includes guidance for encouraging endurance activities, such as walking at a comfortable pace. Thus, we will also encourage participants to increase their walking time by 10 to 20% of their current average –every 2 to 4 weeks.
The number, intensity, and duration of exercises will be gradually increased and adjusted according to individual abilities and preferences.28 Time spent on the combined movements and activities will slowly increase across the 8-week intervention from approximately 25 to 60 minutes per meeting. Participants will master and individualize the OEP so that they can self-direct their practice between meetings, and after the intervention ends. Participants will be encouraged to practice their individualized OEP every other day and their endurance activities (e.g., walking) every day, which is consistent with national and international guideline recommendations for minimal physical activity among older adults.29
Several safety procedures will be integrated into this core intervention component. By design, the OEP emphasizes safety during each exercise.28 The program will begin with a limited number of exercises with low levels of difficulty and then slowly progress according to individual ability, capacity, and preferences. Both interventionists and participants will monitor exercise tolerance throughout each meeting and make adaptations accordingly. Exercises will be performed slowly and near support structures (e.g., a sturdy chair, counter), according to the OEP protocol. Participants will agree to stop exercises and seek assistance if they experience dizziness, shortness of breath, or pain of any type. Interventionists will complete in-person and online OEP training annually and as needed. Additionally, a physical therapist with expertise in geriatrics will consult with the research team throughout the study. Finally, the principal investigator, who is a board-certified gerontological nurse practitioner with extensive OEP experience, will supervise the interventionist and intervention delivery.
2.5.1.2. Physical activity monitor
A physical activity monitor (Fitbit Charge 2) is included as a core component in this intervention for two primary reasons. First, although the ownership of a physical activity monitor does not independently change behavior30, the monitors are used to augment some of behavior change content in the intervention. Second, it will capture objectively measured physical activity data for the study, which is preferred to self-reported measures that are associated with recall bias 53. The triaxial accelerometers built into the Fitbit Charge 2 physical activity monitors are valid and reliable measures of physical activity in older adult research 31–34. We will distribute the monitors to all study participants using general management procedures described below.
We developed three stages in a physical activity monitor management procedure to facilitate basic use by all participants and to ensure consistent use for data capture by research staff. The preparation stage will occur before assessments and data collection. Research staff will register each physical activity monitor (e.g., Fitbit Charge 2), which were all purchased before implementing the study protocol. Each monitor will be programmed using unique research-specific monitor identification, email address, and password not related to participants’ study identifications or personal-identifying information. Staff will deactivate all visual displays in the physical activity monitor except time and calories.
The distribution stage of physical activity monitor management will occur during the baseline assessment when research staff give participants a physical activity monitor and a charging block. They will also orient participants to the basics of wearing and charging the monitor using teach-back methods.35 Importantly, research staff will instruct participants not to connect their monitor to a computer or phone and will not provide information about synchronizing in this phase. Research staff will verify that the monitor display shows time and calories only. They will instruct participants not to read or interpret the calorie counter on their monitor displays and instead to focus on charging and wearing it during their waking hours while engaging in their usual, everyday activities. Research staff will explain that these initial restrictions help to minimize participants’ interaction with the monitor during the baseline assessment period and also helps provide a gradual orientation to the technology.
The activation stage will occur after the baseline assessments are complete. During this phase, research staff will change the numeric “goals” for daily steps, distance, and active minutes that come physical activity monitors (Fitbit Charge 2) -- from 10,000, 5 miles, and 30 minutes respectively, to 2500, 1 mile, and 10 minutes. These changes ensure that messages from monitor displays are within a safe and relevant range for our study population who, on average, have activity levels ranging from sedentary to just below the recommended guidelines for older adults. Research staff will re-program the monitor to display steps, activity minutes, and distance instead of calories. They will also provide participants with an advanced orientation about physical activity features on the monitor’s display. Finally, research staff will assist participants in connecting their monitors to a computer of their choice (e.g., phone, tablet, laptop, desktop), access the Fitbit application, inform them about their research email and password, and provide an overview of synchronizing their monitor.
Curricula across intervention conditions include encouragement for participants to use the monitor during the intervention per personal preferences with attention to physical activity features. The interventionist will be available before and after intervention meetings to help participants troubleshoot their monitors as needed. Participants will also be encouraged to contact the study-dedicated phone or email with technical questions and troubleshooting needs. Some intervention meetings will include discussions about the physical activity monitors, but topics vary according to assigned condition.
2.5.2. Experimental Intervention Components
The manuals that will guide the delivery of behavior change strategies in both the interpersonal and intrapersonal experimental components include introductions to each strategy followed by a facilitated discussion or personal reflection time, a summary, and encouragement to implement the strategy outside course meetings.
2.5.2.1. Interpersonal component
Our decision to include the behaviors change strategies of managing environmental barriers, friendly social comparison, environmental prompts and cues, social support, and recognizing self as a role model, in the interpersonal component was based on their cohesiveness and evidence. All five strategies in this component require communication between group members about physical activity-related ideas, experiences, and knowledge to elicit change. There is theoretical and empirical evidence that each of these is associated with physical activity in older adult adults.36–38 Strategies in this component targets the motivational constructs of environmental resources, social support, enjoyment, and self-efficacy as theoretical mechanisms of action.
Each strategy in this component will be used in at least one intervention meeting in conditions 2 and 4 (See Tables 1 and 2). Following is a description of each strategy, basic delivery tactics, and its location in the course. The strategy of managing environmental barriers will be delivered in Meetings two and six during facilitated discussions about barriers to physical activity rooted in one’s environment (physical or social surroundings), as well as possible solutions (approximately 35 minutes total). The strategy of friendly social comparison will be delivered in Meetings three and seven during facilitated discussions about performing the exercises and implementing behavior change strategies outside of the group meetings (approximately 35 minutes total). Additionally, participants are invited to discuss how they use data from their physical activity monitors in both these meetings. The strategy of environmental prompts and cues will be delivered during facilitated discussions in Meetings four and eight about things in participants’ physical and social surroundings they might use as reminders to walk or perform at least one OEP (approximately 30 minutes total). The strategy of social support will be delivered during facilitated discussions in Meeting five about the types of social support that individual participants have experienced and observed, as well as what types work for them (approximately 20 minutes total). The strategy of recognizing self as a role model will be delivered during a facilitated discussion in meeting seven, about role models and the direct and indirect ways that participants may positively influence families, friends, neighbors, and acquaintances (approximately 10 minutes total).
2.5.2.2. Intrapersonal component
Similar to the interpersonal component, our decision to include the five strategies of personal barrier management, goal setting, building a habit, action planning, and self-assessment in the intrapersonal component was based on their cohesiveness and evidence. These strategies all require reflection about personal preferences, values, goals, and schedules to elicit change. Also, there is theoretical and empirical evidence that each of these strategies is associated with physical activity in older adult adults: 8,36,39,40 Strategies in this component target the motivational constructs of enjoyment, self-efficacy, and self-regulation as theoretical mechanisms of action.
Each strategy in this component will be used in at least one intervention meeting in conditions 3 and 4 (See Tables 1 and 2). Following is a description of each strategy, basic delivery tactics, and its location in the course. The strategy of managing personal barriers will be delivered during facilitated discussions in Meetings two and six about barriers to exercise that originate in one’s mind or body, as well as possible solutions (approximately 35 minutes total). The strategy of goal setting will be delivered during designated reflection time in meetings three and seven for drafting physical activity goals that are specific, measurable, attainable, personally relevant, and time-limited (25 minutes total). The strategy of building a habit will be delivered in Meetings’ four and eight (approximately 35 minutes total). In Meeting four, the interventionist will guide participants to reflect on potential opportunities for building a habit based on performing one or more OEP exercises before, during, or after an existing personal routine and then encourages them to experiment with one or two of their ideas. In Meeting eight, the interventionist will facilitate a follow-up conversation focused on what participants have tried since Meeting four and are considering in the future. The strategy of action planning will be delivered during designated reflection time in Meetings’ five and seven for drafting and refining action plans for personal physical activity goals, according to preferences and routines (approximately 20 minutes total). The strategy of self-assessment will be delivered during designated reflection time in Meeting seven when participants assess the extent to which they have progressed toward their desired goals and the extent to which they have implemented their action plans. Also, participants will be encouraged to adjust their goals and plans accordingly (approximately 15 minutes in total). Worksheets will be provided to augment the delivery of strategies that rely on reflection time.
2.5.3. Attention Control Intervention Content
Condition 1 will include attention control topics related to health and wellness to ensure that the duration of each intervention meeting is similar in all conditions. Background information about the health topic and key considerations will be introduced each week, followed by a facilitated discussion about the ways that participants think about and manage the topic. Participants will also receive written information about each topic with additional resources from either the National Institutes of Health or the Centers for Disease Control and Prevention. Topics, similar to those we used in prior studies, will include reducing falls, pain, supplements, sleep, memory, hearing, and vaccinations.
Meetings in conditions 1, 2, and 3 will also include attention control time focused on technical questions and answers about the OEP exercises and the physical activity monitors (approximately 10 minutes). Time dedicated to technical questions and answers in condition four will be less or integrated into the OEP portion of the meeting.
2.5.4. Intervention Fidelity
The extent to which the intervention is delivered as intended, received, and enacted will be monitored using strategies recommended by the NIH Behavior Change Consortium.41 The interventionist will audiotape meetings, and document meeting processes in REDCap case report forms that capture details about the group and individual participation. Group meeting forms will consist of questions about the extent to which weekly content was delivered as planned and observations about the receipt, and enactment by participants, using an index of procedural consistency and field notes.41 Individual forms will include details about attendance, observed balance, strength, and mastery of the exercises, and which exercises were performed during the meeting. These individual notes will also include the daily step count averaged over the previous week, as recorded on each participant’s physical activity monitor. The principal investigator will randomly select 25% of the meetings’ audiotapes to evaluate against the interventionist manual, and meet with the interventionist weekly to discuss the group and individual notes and the evaluations. They will also problem-solve any challenges. Constructs and measures used to evaluate intervention fidelity are summarized in Table 4.
Table 4.
Intervention Fidelity Measures
| Intervention Component | Measure |
|---|---|
| Core | Attendance to 8-week course |
| Time spent leading the OEP exercises by week across the 8- week course | |
| Type and amount of OEP exercises performed, by week across the 8-week course | |
| Daily total step count, averaged each week of the 8-week course | |
| Experimental | Time spent delivering each experimental BCS |
| Procedural Index: Delivery. Assessment of the extent to which a BCS was delivered as planned, by week | |
| Procedural Index: Receipt. Assessment of the extent to which a BCS was received by participants, by week | |
| Procedural Index: Enactment. Assessment of the extent to which a BCS was enacted by participants, by week |
Notes: OEP = Otago Exercise Program adapted for small groups, BCS = Behavior Change Strategies.
2.6. Assessments and Outcomes
2.6.1. Baseline Assessments and Data Collection
Trained research staff will lead three individual baseline assessment meetings with each participant over three weeks, according to study procedures and checklists. The first 60–90-minute meeting will include structured interviews comprised of questionnaires addressing baseline and health data, and observations of functional strength and balance. The purpose of the second 10-minute meeting will be to synchronize the participant’s physical activity monitor and instruct them to continue wearing the monitor during their waking hours. The third 60-minute meeting will include questionnaires about physical activity patterns and motivation. Objective physical activity data will also be captured at this time. See Table 3 for a summary of data collected across assessment time points.
Table 3.
Construct measures and assessment schedule
| Construct | Measure | Assessment Time points | Purpose | |||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| Physical Activity | Fitbit accelerometer activity minutes | X | X | X | X | Primary Outcome |
| Physical Activity Scale for the Elderly42 | X | X | X | X | Primary Outcome | |
| Falls | Monthly fall occurrence | X | X | X | X | Secondary Outcome |
| Monthly Injurious fall occurrence | X | X | X | X | Secondary Outcome | |
| Quality of Life | PROMIS SF1.143 | X | X | X | X | Secondary Outcome |
| Functional Strength and Balance | Short Physical Performance Battery44 | X | X | X | X | Putative MOA |
| Lower Extremity Function45 | X | X | X | X | Putative MOA | |
| Environmental Support | Health and Physical Activity Resources46 | X | X | X | X | Putative MOA |
| Social Support | Social support for Exercise 47 | X | X | X | X | Putative MOA |
| Duke-UNC Functional Social Support Questionnaire48 | X | Baseline Characteristic | ||||
| Physical Activity Group Environment Questionnaire -Modified49 | X | Putative MOA | ||||
| Readiness | Index of Readiness50 | X | X | X | X | Putative MOA |
| Self-Efficacy | Self-efficacy for exercise51 | X | X | X | X | Putative MOA |
| Enjoyment | Physical Activity Enjoyment Scale-852 | X | X | X | X | Putative MOA |
| Self-Regulation | Index of Self-Regulation53 | X | X | X | X | Putative MOA |
| Behavioral Regulation in Exercise Questionnaire -364 | X | X | X | X | Putative MOA | |
| Baseline | Age, sex, number living in the home, | X | Baseline Characteristic | |||
| Characteristics | highest formal education, monthly household income, ethnicity, race | |||||
| Health Characteristics | Medication Inventory | X | X | X | X | Potential Confounder |
| Brief Pain Inventory54 | X | X | X | X | Potential Confounder | |
| Self-reported chronic diseases | X | X | X | X | Health Characteristic | |
| Life-Space Mobility55 | X | X | X | X | Baseline Characteristic | |
| Fall risk (self-report)20 | X | X | X | X | Health Characteristic | |
Notes: Time point 1 = baseline; time point 2 = 1-week post-intervention; time point 3 = 6-month post-intervention; time point 4 = 12-month post-intervention; MOA = constructs targeted as putative mechanism of action
2.6.2. Post-intervention Assessments and Data Collection
Trained research staff will also lead individual meetings with participants for three assessments post-intervention: 1 week, 6 months, and 12 months, each lasting approximately 60 minutes. Post-intervention assessments will be preliminarily scheduled after enrollment and randomization, according to participant preferences. Research staff will communicate Information about what to expect during each meeting via US mail during week five of the intervention course and again approximately 10 days before each scheduled meeting. They will also call participants 24 to 48 hours before each scheduled appointment to confirm its date, time, and location. Brief additional meetings will be planned with participants who do not routinely synchronize their Fitbits to a computer or need technical assistance. Similar to baseline assessments, post-intervention assessments include structured interviews with questionnaires about health, fall risk, physical activity, and motivation. Additionally, research staff will assess functional strength and balance and capture objective physical activity data during these assessments (See Tables 3 and 4).
2.6.3. Compensation
Participants will be compensated $50 after wearing the physical activity monitor for each 7-day data collection period (4) and $20 after completing each assessment meeting (4). The intervention meetings, including participant workbooks, ankle weights, and physical activity monitors, will be free. Therefore, the total possible compensation for participating in the study will be $280 per participant.
2.7. Constructs and Measures
2.7.1. Baseline Characteristics
Data representing age at the time of enrollment; sex; the number of people living in the home; approximate monthly household income; highest formal education attained; ethnicity and race, will be captured during the baseline assessment via self-report. Additionally, perceived social support (general) will be measured using the validated Duke-UNC Functional Social Support Questionnaire.48
2.7.2. Health Characteristics
Health status, problems, and needs that may influence fall risk56,57 will be assessed at all four time points via self-reports. Research staff will ask participants if they have the following chronic conditions: osteoporosis, diabetes, heart disease, lung disease, foot problems, and arthritis. The intensity of participants’ pain and its interference with their daily function will be measured using the validated Brief Pain Inventory-short form.54 Medication and supplement use, dose, and schedule will be captured via participants’ self-reports. Research staff will then categorize each medication and supplement according to its association with fall risk, with guidance from a Doctor of Pharmacy who has expertise in gerontology. Finally, mobility at home and in the community will be measured using the Life-Space Assessment instrument.55
2.7.3. Primary Outcome: Quantity of Physical Activity
The quantity of physical activity will be measured as the average daily minutes of all physical activity intensities (light, moderate, vigorous) averaged over seven days, using objective and self-report approaches at all four assessment time points. At each of the four time points, participants will be instructed to wear the Fitbit Charge 2 wristband on their nondominant wrist during waking hours, except for time bathing, showering, or swimming.
A secure research database will capture accelerometer data, Fitabase,58 that aggregates, stores, reduces and enables visualization of de-identified participant data. At each assessment time point, data will be checked for three validation criteria. The presence of minute-level heart rate data will be checked to validate that participants wore the monitor for at least 10 continuous hours during typical waking hours. The presence of daily intensity and step data will also be checked. When data does not meet the criteria, participants will be asked to continue wearing the monitor, and a follow-up assessment will be scheduled. Data from days that meet validation criteria will be transferred, via an application programming interface (API) between Fitabase and REDCap with variables representing the quantity of daily physical activity. The variables in the REDCap-Fitabase API form will include total daily minutes of physical activity, by intensity level (light, moderate, vigorous), the total number of daily steps, and total daily metabolic equivalents. These metrics will be sensed, counted, categorized, and calculated via proprietary algorithms proprietary to Fitbit. Light intensity physical activity will be included because many older adults prefer it and evidence suggests it provides health benefits.59 Average daily minutes of physical activity will be estimated based on the sample of at least 7 valid days during the assessment time-frame when the physical activity monitor is worn for ≥10 hours each day.60,61
Self-reported physical activity will be captured using the Physical Activity Scale for the Elderly (PASE), which is a reliable and valid instrument used widely across epidemiological and intervention studies that include adults who are over the age of 65.42 The instrument quantifies the frequency and duration of physical activity in the last seven days that are part of a person’s lifestyle (e.g., housework, caring for others), walking, and their structured exercise routines, rated by level of intensity. All data is used to estimate an exercise score, ranging from 0 to >400, with higher scores indicating greater physical activity. The PASE scoring algorithm was derived from physical activity measured by movement counts from an electronic, physical activity monitor, activity diaries, and self-assessed activity levels in a general population of non-institutionalized older individuals.51 In this study, one item is added to the PASE that addresses the OEP balance movements. However, the responses to this item are not included in the total PASE score.
2.7.4. Secondary Outcomes: Falls and Quality of Life
Falls in this study will be defined as “an unexpected event in which the participant comes to rest on the ground, floor, or lower level.”52 Falls will be measured retrospectively at the baseline and 1 week post intervention assessment, after which they will be measured prospectively using monthly one-page, postal calendars for tracking both injurious and non-injurious falls.62 A questionnaire about fall circumstances and consequences will be included on the opposite side of each calendar page. Examples of questions include: “Where were you when you fell? What do you think caused you to fall? And what health care did you receive?” Although this measurement method of falls is considered the gold standard in this field,<sup>63</sup> we will augment it in three ways. First, we will call participants who do not return calendars to identify and problem-solve barriers to using them. Second, we call participants who report falls to confirm and further explore their circumstances. Third, we will collect retrospective, self- reported fall risk data, at each data collection timeframe. Fall risk questions inquire about the number of falls since the last interview, changes in balance, difficulty walking, and fear of falling.20
Quality of Life will be measured using the Patient-Reported Outcomes Measurement Information System (PROMIS) Global Health Scale, which captures an individual’s self-assessment of their physical, mental, and social health.43 It generates two scores: Physical Health and Mental Health.
2.7.5. Exploratory Outcomes: Constructs Targeted as Putative Mechanisms of Action
WMT-based motivational constructs targeted by behavior change strategies within the intervention components will be assessed at all four assessment and data collection time points using measures validated in prior physical activity research that includes older adults. The motivational construct of environmental support will be measured using the Chronic Illness Resources Survey.46 The construct of social support will be measured using the Social Support for Exercise Survey47 and the Physical Activity Group Environment Questionnaire.49 The motivational constructs of readiness, self-efficacy, and enjoyment will be measured using the Index of Readiness,50 the Self- Efficacy for Exercise Scale51, and the Physical Activity Enjoyment Scale52, respectively. Finally, the motivational construct of self-regulation will be measured using the Index of Self-Regulation53 and the Behavioral Regulations in Exercise Questionnaire.64
Physical function, considered a markers of fall risk targeted by the OEP exercises, will be assessed at all four time points, objectively and via self-report. The assessment will consist of observing functional strength and balance via the Short Physical Performance Battery (SPPB) 44 and eliciting participant ratings of lower extremity function via the Physical Function-Short Form-6b (PROMIS).
2.7.6. Process Evaluation
2.7.6.1. Implementation in community settings
In addition to study outcomes and potential mechanisms of action, the research team will also evaluate the barriers and facilitators of implementing interventions using qualitative methods. Research staff will conduct semi-structured interviews with community center participant representatives using an interview guide informed by the reach- effectiveness–adoption-implementation-maintenance (RE-AIM) framework.65 All interviews will be audiotaped and professionally transcribed. Data will be stored and managed in NVivo, a qualitative research software program. A coding team will conduct content analysis, including the development of codes, categories, and themes.66 A matrix table will be used to compare themes identified from older adults and community center leaders.
2.8. Sample Size
According to results from meta-analyses, standardized effect sizes of physical activity interventions for older adults range from .18 8 to .26,69 which translates to 670 to 870 additional steps per day or 73 to 94 extra minutes of physical activity per week. Although these effects are small, they are clinically meaningful in older populations whose overall activity levels are low, often sedentary.70 Thus, we base our sample size estimates on a small standardized effect size of .20. We also anticipate 15% attrition at 12 months, based on our preliminary studies, which showed 7% attrition at 6 months.15 Considering these assumptions and the use of repeated measures, we used the FactorialPowerPlan Macro in SAS67 to calculate the sample size of 308 participants, 77 per condition. This will enable us to detect small but clinically meaningful (effect sizes of .20) main effects of the experimental intervention components on the quantity of physical activity among participants who receive the interpersonal behavior change strategies in conditions 2 and 4, compared to those who do not receive these strategies in conditions 1 and 3, as well as their interactions, with 80% power under a two-tailed hypothesis test at a significance level of .05. This sample size will also enable us to detect medium to large effects on our outcome of falls (fall rate ratios of .40 to .70), with 80% power, under a two-tailed hypothesis test at a significance level of .05. This medium to large effect size on falls is consistent with prior research that shows that OEP reduces falls (fall rate ratios 0.56 to 0.79).27
2.9. Randomization
After completing baseline assessments, eligible participants will be randomly assigned to 1 of 4 intervention conditions using blocks of 16 to 24 (multiples of 4), according to cohort size. Random allocation will be implemented centrally by study staff who are responsible for analysis and coordination, not assessment or intervention delivery. The following procedures will be used to implement random allocation and conceal condition assignments:
After all potential participants in a cohort complete their baseline assessments, the study analyst will provide computer-generated random numbers and the allocation sequence of sequential numbers for the block (4 conditions) to the study manager. Computer-generated random numbers will be from SAS 9.1, the code for which will be stored in a secured and encrypted file in BOX, accessible only to the study analyst and manager.
The sequence of random numbers for each block will be concealed to all research staff until the study manager assigns each participant in the cohort.
The study manager will document random assignments in REDCap and notify the study interventionist. The manager will also inform study participants of the meeting logistics for the intervention group to which they were assigned.
2.9.1. Masking
Although the study design does not permit masking the study interventionist and participants to study content and condition, the analyst, manager, and research staff who conduct assessments will be masked to the experimental content and curricula in each condition. To do this, we will maintain codes for the four conditions using numbers and colors. The key to these codes and corresponding intervention components and the content will be stored separately from the randomization scheme and other research files. Throughout the study, research staff other than the interventionist will minimize their bias by not attaining knowledge, skill, or training about the intervention content and by not having access to intervention manuals.
2.10. Staff Training
All study staff will have continual access to the training courses, manuals of procedures and checklists, the study protocol, and the Principal Investigator for reference and consultation as needed. Training will be delivered using online and in-person strategies.
Training curricula and enduring training materials will focus on the interventionist role and the assessor role. Interventionists will be trained to deliver all manualized intervention content. Core interventionist competencies include facilitating small-group discussions, maintaining a positive social milieu, delivering all intervention content (behavior change strategies, OEP for small groups, health, and wellness information) according to manuals and the OEP protocol, and documentation. Assessors will be trained to prepare for, conduct, and maintain data from all non-intervention participant encounters. Core assessor role competencies include screening, consenting, and conducting structured interviews with older adults., accurately capturing and verifying physical activity data as well as data from questionnaires, doing the SPPB, and using secure iPads, Fitabase, and REDCap to capture, store, and manage data. Additionally, assessors will have competencies for all phases of physical activity monitor management and providing as-needed assistance to study participants and research staff to troubleshoot physical activity monitors.
2.11. Data Management
We will use REDCap to capture and manage data. REDCap uses a MySQL database via a secure web interface with checks used during data entry to ensure quality.68 Interview and observational data will be entered directly into a REDCap database from encrypted, password-protected iPad tablet computers. Accelerometer data from each participant will be downloaded into REDCap from a secure research database, Fitabase, using an API developed for this study. Fitabase will enable capturing, aggregating, reducing, and securely storing de-identified accelerometer data from physical activity-monitors.
2.12. Analyses
Descriptive statistics such as means, standard deviations, ranges for continuous variables, and counts/ percentages for categorical variables, will be used to summarize the biologic, demographic, outcome, and exploratory variables by condition, actual and projected accrual, attendance and retention rates, quality control data (e.g., missing data), and fidelity data. Tables, graphs, and charts will be used to visualize data when appropriate.
Contact data will be reviewed at least weekly throughout recruitment phases and, along with enrollment data, will be cumulatively summarized each month throughout the study. The effect of condition assignment on the dependent variables will be examined using ANOVA tests for continuous variables and Fisher’s exact test or chi-square tests for categorical variables, as appropriate. Any identified confounders will be adjusted for in subsequent analyses. All analyses will be pre-planned and conducted while masked to condition. We will include all cases in analyses, regardless of intervention attendance rates or attrition.
Missing data will be analyzed. We anticipate, based on preliminary research, 15 that the rate of missing data will be low and similar across conditions, but that it may be associated with a severe illness that leads to dropping out or inability to capture follow- up physical activity data. Thus, similar to preliminary analyses, we will conduct a sensitivity analysis of complete cases and imputing the worst-case carried forward.
2.12.1. Analysis Plan for Aim 1
The effects of the experimental intervention components on physical activity will be assessed using 2×2 full factorial analysis of covariance (ANCOVA) using the General Linear Model approach, with the duration of total physical activity as the outcome (average minutes per week). Checks will be conducted to ensure that there are no egregious violations of normality, linearity, homogeneity of variances, or homogeneity of regression slopes prior to ANCOVA. Additionally, although individuals--not clusters of individuals--is the unit of randomization in this study, the intervention is delivered to small groups of individuals (“cohorts”). In our prior study, cohort membership was not significantly correlated with outcomes.15 Results from generalized estimating equation (GEE) models accounting for cohort membership were similar to those from ANCOVA models. In the current study, we will assess the influence of cohorts on outcomes similarly by first calculating the interclass correlations (ICCs) to evaluate the within- and between-cohort variation in the quantity of physical activity at each measurement time points, using a random effect ANOVA model. If the ICCs are significant, we will assess factor effects and interactions over time using linear mixed effect models (LMMs) with the cohorts being a random component.
The factors, or independent variables, are interpersonal and intrapersonal behavior change components that will be effect-coded with two levels indicating exposure (No as −1 versus Yes as +1).69 Different models will be developed for physical activity measured directly and physical activity measured via self-report. Each model will include baseline physical activity values as a covariate. The main and interaction effects of the experimental components on the duration of physical activity will be tested immediately, 6 months, and 12 months post-intervention. Further, we will apply longitudinal data analyses using LMMs to examine the variation of component effects across assessment time points and include interactions between experimental components (e.g., interpersonal factor x intrapersonal factor x time). This longitudinal analysis will enable us to see when an older adult might benefit from additional support to maintain physical activity.
2.12.2. Analysis Plan for Aim 2
Falls will first be described using the number of falls, fallers, fall rates, and time to first fall post-intervention.62 Given the expected distribution of falls, we will use negative binomial regression models to estimate the between-group difference in fall rates 12 months post-intervention. Quality of Life data will be assessed using 2×2 full factorial ANCOVA and longitudinal analyses described for Aim 1 with total mean quality of life as the outcome variable.
2.12.3. Analysis Plan for Aim 3
We will assess if this study’s experimental intervention component(s) changed motivational constructs and physical markers of fall risk targeted as putative mechanisms of action. Analyses will also examine whether these constructs and markers mediated the intervention effects on physical activity and falls. Using the general approach to mediation analysis described by MacKinnon,70, we will assess the effects of intervention components on constructs targeted as putative mechanisms of action and the association of these constructs with outcomes. We will report these, as well as the total direct and indirect effects of intervention components on physical activity and falls. If nonlinearities or interactions between exposure and mediator variables are observed, we will use counterfactual approaches, described by Vanderweele and colleagues.71
2.12.4. Exploratory Analysis
We will conduct stratified, exploratory analysis to assess for possible effect modification of outcomes by level of pain, use of fall risk-inducing medications, mobility, sex, and social support (general). Although this study is not designed to conduct confirmatory subgroup analyses of these factors, we will report values for these variables as well as differences observed, which may be valuable for future research and meta-analyses.
2.13. Data Monitoring and Safety Plan
Research staff will monitor for potential adverse events during assessment and intervention meetings. Also, participants will be asked to inform the researchers about any concerns regarding potential adverse events during or between study meetings. The principal investigator, in conjunction with an Independent Safety Monitor, will be available to review and recommend appropriate action regarding all potential adverse events and safety issues. Data on all potential adverse events will be maintained in a REDCap adverse event form, regardless of their relationship to the study and reported to the investigator team monthly. The principal investigator will submit information about all reportable events as they occur to the University of Minnesota Institutional Review Board, and the National Institutes of Health and the National Institutes of Health, National Institutes of Nursing Research.
2.14. Dissemination
We will disseminate information about this study and results to the public as well as our participants and community partners via multiple platforms. For example, we will publicly present information about all aspects of this proposal; study protocol; intervention content; recruitment and retention strategies; and findings at national, and international scientific meetings. We will also make annual presentations locally through the University of Minnesota, School of Nursing’s Annual Research Conference; during meetings with community partners; and during Minnesota’s annual Falls Awareness Day. We will post information about summaries of our national and local presentations on our Web site, written in plain language for a general audience. Finally, we will publish manuscripts in peer-reviewed journals based on our national presentations of this proposal’s study protocol and findings.
3.0. Discussion
The complex public health problems of falls and inactivity create significant social and economic burdens. Every year, 1 in 4 people aged 65 and older falls; 25% of which result in serious injury or death.1 Injurious and fatal fall rates increase exponentially with age, particularly after age 70.2 Decreased leg strength, poor balance, and altered gaits are the most common causes of falls.72 These causes can be mitigated with the regular practice of leg strengthening and balance-challenging activities. Walking and flexibility movements augment these activities. Previous research demonstrates that approximately 39% of injurious and fatal falls can be prevented with fall-reducing physical activity,4 and that physical activity is associated with improved quality of life.3 Despite public health efforts to disseminate and implement this evidence, less than 12% of people aged 65+ engage in physical activity as recommended, and remain high.2,5 Thus, knowledge of fall-reducing physical activity has not translated to increased physical activity rates in the community of older adults or made an impact on falls. Therefore, it is essential to augment evidence-based fall-reducing physical activity interventions with evidence-based behavior change content that motivates older adults to sustain increased physical activity.
The current study is designed, guided by the MOST framework, to determine the effects of two experimental intervention components comprised of distinct sets of behavior change strategies.10 The components represent two different ways of motivating people to act: interpersonal and intrapersonal, consistent with theories of behavior change11,12 and life-span development,13 as well as empirical evidence.9,14 Examining the unique and interactive effects of these experimental components on older adults’ physical activity will enable the identification of behavior change content that motivates them to sustain increased physical activity. Experimental components in this study are combined with the core intervention components of an evidence-based physical activity protocol, OEP adapted for small groups, and a physical activity monitor. The rationale behind the experimental and core components are based on the WMT, prior falls prevention research, our preliminary studies, and feedback from community stakeholders.
This study has potential limitations. One is that we will use one optimization criterion: the effect of experimental components on the sustained increase of physical activity, falls, and quality of life. Other optimization criteria, such as intervention characteristics (e.g., delivery mode, provider), were also considered. However, prior research suggests that a diverse set of these characteristics are feasible, acceptable, and associated with positive effects.73 A second potential limitation is that the study design prohibits examining the unique effect of each behavior change strategy within each experimental component. There may be some strategies within each component that do not contribute meaningfully to intervention effects. However, similar to physical activity research in which cohesive types and sets of exercises are tested for their effects on outcomes, research that realistically addresses behavior change content will test cohesive types and interrelated sets of behavior change strategies. That is, testing the effects of a single exercise or a single behavior change strategy would not mirror current guidelines, theory, or practice.
In addition to limitations in the study design, the dynamism of social contextual factors may complicate study implementation at some phase in the five-year study. For example, community centers and partners may experience changes that prohibit them from hosting the intervention courses and assessment meetings as planned. To address this, we will maintain community relationships and continuously monitor the capacity and readiness of community centers to host this study’s intervention meetings, creating alternative plans as needed.
This study is one of the first to use the MOST framework to guide the optimization of a community-based physical activity intervention for older adults to reduce the public health problems of low physical activity and falls, as well as their devastating effects on quality of life. This work will advance knowledge about the promotion of physical activity, fall prevention, and underlying mechanisms of action. In particular, the results will enable the optimization of behavior change content within a fall-reducing physical activity intervention and, in turn, other physical activity interventions for older adults. This contribution will be significant because it is expected to foster the integration of evidence-based physical activity content and behavior change content within interventions that, in turn, impact health outcomes.
Acknowledgements
Research reported in this publication is supported by the National Institute Of Nursing Research of the National Institutes of Health under Award Number 5 R01NR016705. We would like to thank our study participants and community partners. We would also like to thank our research staff for their time, dedication and skillful implementation of this protocol. This work would not be possible without them.
Footnotes
Adjustments for Covid-19
We adjusted our protocol on March 16, 2020 according to recommendations from the Centers for Disease Control and the Minnesota Department of Health, and received approval from the University of Minnesota Institutional Review Board. Although the small groups in cohort 11, which were underway at this time, were able to complete their 7th and 8th intervention meetings via telephone conference calls, the enrollment and randomization of additional participants was stopped on March 16th. We will resume delivering the intervention to additional cohorts when recommendations for COVID-19 allow small group gatherings.
Adjustments for COVID-19.
During COVID-19 mitigation and containment efforts, assessments and data collection will be conducted over the phone instead of in community centers, libraries, or participants’ until it is safe to meet in person. Similar to our procedures before Covid-19, we will schedule and confirm the logistics of these assessment meetings via phone and US mail. We will also send participants a copy of the response scales to each questionnaire in the structured interview. We anticipate that we will use this adjusted assessment protocol for 24 post-intervention assessments, 47 6-month post-intervention assessments, and 24 12-month post-intervention assessments.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Important Facts about Falls | Home and Recreational Safety | CDC Injury Center. Accessed June 10, 2020. https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html
- 2.Moreland B, Kakara R, Henry A, Trends in Nonfatal Falls and Fall-Related Injuries Among Adults Aged ≥65 Years — United States, 2012–2018, MMWR Morb Mortal Wkly Rep 69 (2020) 875–881), doi:, 10.15585/mmwr.mm6927a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stenhagen M, Ekström H, Nordell E, Elmståhl S. Accidental falls, health-related quality of life and life satisfaction: A prospective study of the general elderly population. Arch Gerontol Geriatr. 2014;58(1):95–100. doi: 10.1016/j.archger.2013.07.006 [DOI] [PubMed] [Google Scholar]
- 4.Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;(2). doi: 10.1002/14651858.CD012424.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services O of DP and HP. Healthy People 2020. [Internet]. Washington, DC. Accessed August 12, 2018. https://www.healthypeople.gov/2020/data-search/Search-the-Data#topicarea=3493;topic-area=3504; [Google Scholar]
- 6.Hartholt KA, Lee R, Burns ER, Van Beeck EF. Mortality from Falls among US Adults Aged 75 Years or Older, 2000–2016. JAMA - J Am Med Assoc. 2019;321(21):2131–2133. doi: 10.1001/jama.2019.4185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Libr. Published online 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chase JA. Interventions to Increase Physical Activity Among Older Adults: A Meta-Analysis. Gerontologist. Published online October 7, 2014. doi:gnu090 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.French DP, Olander EK, Chisholm A, Mc Sharry J. Which Behaviour Change Techniques Are Most Effective at Increasing Older Adults’ Self-Efficacy and Physical Activity Behaviour? A Systematic Review. Ann Behav Med. Published online 2014. http://www.scopus.com/inward/record.url?eid=2-s2.0-84896418074&partnerID=40&md5=ddf800a1023fd66d43523c88307897df [DOI] [PubMed] [Google Scholar]
- 10.Collins LM. Optimization of Behavioral, Biobehavioral, and Biomedical Interventions : The Multiphase Optimization Strategy (MOST). [Google Scholar]
- 11.Fleury J. Wellness motivation theory: An exploration of theoretical relevance. Nurs Res. 1996;45(5):277–283. [DOI] [PubMed] [Google Scholar]
- 12.Greaney ML, Lees FD, Blissmer BJ, Riebe D, Clark PG. Psychosocial Factors Associated With Physical Activity in Older Adults. Annu Rev Gerontol Geriatr. 2016;36(1):273–291. doi: 10.1891/0198-8794.36.273 [DOI] [Google Scholar]
- 13.Charles ST, Carstensen LL. Social and emotional aging. Annu Rev Psychol. 2010;61:383–409. doi: 10.1146/annurev.psych.093008.100448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McMahon SK, Hekler EB, Belyea MJ, Shearer N, Wyman JF, Fleury J. Combining Motivational and Physical Intervention Components to Promote Fall-Reducing Physical Activity Among Community-Dwelling Older Adults. Am J Heal Promot. 2015;30(8):638–644. doi: 10.4278/ajhp.130522-arb-265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McMahon SK, Lewis B, Oakes JM, Wyman JF, Guan W, Rothman AJ. Assessing the Effects of Interpersonal and Intrapersonal Behavior Change Strategies on Physical Activity in Older Adults: a Factorial Experiment. Ann Behav Med. 2017;51(3):1–15. doi: 10.1007/s12160-016-9863-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Montgomery P, Grant S, Mayo-Wilson E, et al. Reporting randomised trials of social and psychological interventions: The CONSORT-SPI 2018 Extension. Trials. 2018;19(1):407. doi: 10.1186/s13063-018-2733-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Collins LM, Dziak JJ, Kugler KC, Trail JB. Factorial experiments: efficient tools for evaluation of intervention components. Am J Prev Med. 2014;47(4):498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dipietro L, Campbell WW, Buchner DM, Erickson KI, Powell KE, Bloodgood B, Hughes T, Day KR, Piercy KL, Vaux-Bjerke A, Olson RD & 2018 PAGAC. Physical Activity, Injurious Falls, and Physical Function in Aging: An Umbrella Review. Med Sci Sports Exerc. 2019;51(6):1303–1313. doi: 10.1249/MSS.0000000000001942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Topolski TD, LoGerfo J, Patrick DL, Williams B, Walwick J, Patrick MB. The Rapid Assessment of Physical Activity (RAPA) among older adults. Prev Chronic Dis. 2006;3(4):A118. doi:A118 [pii] [PMC free article] [PubMed] [Google Scholar]
- 20.Stevens JA, Phelan EA. Development of STEADI: A Fall Prevention Resource for Health Care Providers. Health Promot Pract. 2013;14(5):706–714. doi: 10.1177/1524839912463576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Resnick B, Ory MG, Hora K, et al. A proposal for a new screening paradigm and tool called Exercise Assessment and Screening for You (EASY). J Aging Phys Act. 2008;16(2):215–233. [DOI] [PubMed] [Google Scholar]
- 22.Perkins AJ, Hendrie HC, Unverzagt FW, Hui SL, Callahan CM. Six-Item Screener to Identify Cognitive Impairment Among Potential Subjects for Clinical Research. Med Care. 2003;40(9):771–781. doi: 10.1097/00005650-200209000-00007 [DOI] [PubMed] [Google Scholar]
- 23.UMN - Study Finder. Accessed June 10, 2020. https://studyfinder.umn.edu/ [Google Scholar]
- 24.Judy A. Stevens EB. A CDC Compendium of Effective Fall Interventions: What Works for Community-Dwelling Older Adults. 3rd ed. Division of Unintentional Injury Prevention National Center for Injury Prevention and Control Centers for Disease Control and Prevention; 2015. https://www.cdc.gov/homeandrecreationalsafety/falls/compendium.html [Google Scholar]
- 25.Thomas S, Mackintosh S, Halbert J. Does the ‘Otago exercise programme’reduce mortality and falls in older adults?: a systematic review and meta-analysis. Age Ageing. 2010;39(6):681–687. [DOI] [PubMed] [Google Scholar]
- 26.Campbell JA, Robertson MC. Otago Exercise Programme to Prevent Falls in Older Adults. ACC2007; 2003. [Google Scholar]
- 27.Shubert TE, Goto L, Smith ML, Ory MG, Jiang L. Otago Exercise Program in the United States: Comparison of 2 Implementation Models. Phys Ther. 2017;97(2):187–197. doi: 10.2522/ptj.20160236 [DOI] [PubMed] [Google Scholar]
- 28.Gardner MM, Buchner DM, Robertson MC, Campbell AJ. Practical implementation of an exercise-based falls prevention programme. Age Ageing. 2001;30(1):77–83. [DOI] [PubMed] [Google Scholar]
- 29.2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report.; 2018. [Google Scholar]
- 30.Patel MSD, Asch DA, Volpp KG, et al. Wearable Devices as Facilitators, Not Drivers, of Health Behavior Change. Jama. 2015;313(5):459–460. [DOI] [PubMed] [Google Scholar]
- 31.Straiton N, Alharbi M, Bauman A, et al. The validity and reliability of consumer-grade activity trackers in older, community-dwelling adults: A systematic review. Maturitas. 2018;112:85–93. doi: 10.1016/j.maturitas.2018.03.016 [DOI] [PubMed] [Google Scholar]
- 32.Brewer W, Swanson BT, Ortiz A. Validity of Fitbit’s active minutes as compared with a research-grade accelerometer and self-reported measures. BMJ Open Sport Exerc Med. 2017;3(1). doi: 10.1136/bmjsem-2017-000254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Diaz KM, Krupka DJ, Chang MJ, et al. Fitbit®: An accurate and reliable device for wireless physical activity tracking. Int J Cardiol. 2015;185:138–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tedesco S, Sica M, Ancillao A, Timmons S, Barton J, O’Flynn B. Validity evaluation of the fitbit charge2 and the garmin vivosmart HR+ in free-living environments in an older adult cohort. J Med Internet Res. 2019;21(6). doi: 10.2196/13084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ha Dinh TT, Bonner A, Clark R, Ramsbotham J, Hines S. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: a systematic review. JBI database Syst Rev Implement reports. 2016;14(1):210–247. doi: 10.11124/jbisrir-2016-2296 [DOI] [PubMed] [Google Scholar]
- 36.Arnautovska U, O’Callaghan F, Hamilton K. Behaviour change techniques to facilitate physical activity in older adults: What and how. Ageing Soc. 2018;38(12):2590–2616. doi: 10.1017/S0144686X17001027 [DOI] [Google Scholar]
- 37.Lindsay Smith G, Banting L, Eime R, O’Sullivan G, van Uffelen JGZ. The association between social support and physical activity in older adults: A systematic review. Int J Behav Nutr Phys Act. 2017;14(1):1–21. doi: 10.1186/s12966-017-0509-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Devereux-Fitzgerald A, Powell R, Dewhurst A, French DP. The acceptability of physical activity interventions to older adults: a systematic review and meta-synthesis. Soc Sci Med. 2016;158:14–23. doi: 10.1016/j.socscimed.2016.04.006 [DOI] [PubMed] [Google Scholar]
- 39.Floegel T, Florez-Pregonero A, Hekler E, Buman MP. SIMULTANEOUS VALIDATION OF FIVE COMMERCIALLY-AVAILABLE ACTIVITY MONITORS IN OLDER ADULTS WITH VARIED AMBULATORY ABILITIES. In: GERONTOLOGIST. Vol 54. OXFORD UNIV PRESS INC JOURNALS DEPT, 2001 EVANS RD, CARY, NC 27513 USA; 2014:187. [Google Scholar]
- 40.Ashe MC, Clemson L, Chen P. Health behaviour change theory meets falls prevention: Feasibility of a habit-based balance and strength exercise intervention for older adults. Psychol Sport Exerc. 2016;22:114–122. doi: 10.1016/j.psychsport.2015.07.002 [DOI] [Google Scholar]
- 41.Bellg AJ, Borrelli B, Resnick B, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Heal Psychol. 2004;23(5):443. [DOI] [PubMed] [Google Scholar]
- 42.Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52(7):643–651. [DOI] [PubMed] [Google Scholar]
- 43.Riley WT, Rothrock N, Bruce B, et al. Patient-reported outcomes measurement information system (PROMIS) domain names and definitions revisions: further evaluation of content validity in IRT-derived item banks. Qual Life Res. 2010;19(9):1311–1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. [DOI] [PubMed] [Google Scholar]
- 45.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Glasgow RE, Toobert DJ, Barrera M, Strycker LA. The Chronic Illness Resources Survey: Cross-validation and sensitivity to intervention. Health Educ Res. 2005;20(4):402–409. doi: 10.1093/her/cyg140 [DOI] [PubMed] [Google Scholar]
- 47.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med (Baltim). 1987;16(6):825–836. [DOI] [PubMed] [Google Scholar]
- 48.Broadhead WE, Gehlbach SH, Gruy F V., Kaplan BH The Duke-UNC functional social support questionnaire: Measurement of social support in family medicine patients. Med Care. 1988;26(7):709–723. [DOI] [PubMed] [Google Scholar]
- 49.Estabrooks PA, Carron A V. The Physical Activity Group Environment Questionnaire: An instrument for the assessment of cohesion in exercise classes. Gr Dyn Theory, Res Pract. 2000;4(3):230. [Google Scholar]
- 50.Fleury J. The index of readiness: development and psychometric analysis. J Nurs Meas. 1994;2(2):143–154. [PubMed] [Google Scholar]
- 51.Resnick B, Jenkins LS. Testing the reliability and validity of the self-efficacy for exercise scale. Nurs Res. 2000;49(3):154–159. [DOI] [PubMed] [Google Scholar]
- 52.Mullen SP, Olson EA, Phillips SM, et al. Measuring enjoyment of physical activity in older adults: Invariance of the physical activity enjoyment scale (paces) across groups and time. Int J Behav Nutr Phys Act. 2011;8(1):103. doi: 10.1186/1479-5868-8-103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yeom H-A, Fleury J. Validity and Reliability of the Index of Self-Regulation Scale for Physical Activity in Older Korean Americans. Nurs Res Pract. 2011;2011:1–6. doi: 10.1155/2011/329534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mendoza T, Mayne T, Rublee D, Cleeland C. Reliability and validity of a modified Brief Pain Inventory short form in patients with osteoarthritis. Eur J Pain. 2006;10(4):353. [DOI] [PubMed] [Google Scholar]
- 55.Peel C, Baker PS, Roth DL, Brown CJ, Bodner E V, Allman RM. Assessing Mobility in Older Adults: The UAB Study of Aging Life-Space Assessment. Phys Ther. 2005;85(10):1008–1019. doi: 10.1093/ptj/85.10.1008 [DOI] [PubMed] [Google Scholar]
- 56.Leveille SG, Jones RN, Kiely DK, et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. Jama. 2009;302(20):2214–2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(suppl 2):ii37–ii41. [DOI] [PubMed] [Google Scholar]
- 58.Fitabase. Research Platform. Published 2015. http://www.fitabase.com/ [Google Scholar]
- 59.Buman MP, Hekler EB, Haskell WL, et al. Objective Light-Intensity Physical Activity Associations With Rated Health in Older Adults. Am J Epidemiol. 2010;172(10):1155–1165. doi: 10.1093/aje/kwq249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cain KL, Geremia CM. Accelerometer Data Collection and Scoring Manual. Published online 2011. [Google Scholar]
- 61.Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer Data Collection and Processing Criteria to Assess Physical Activity and Other Outcomes: A Systematic Review and Practical Considerations. Sport Med. 2017;47(9):1821–1845. doi: 10.1007/s40279-017-0716-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schwenk M, Lauenroth A, Stock C, et al. Definitions and methods of measuring and reporting on injurious falls in randomised controlled fall prevention trials: a systematic review. BMC Med Res Methodol. 2012;12(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hauer K, Lamb SE, Jorstad EC, Todd C, Becker C. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing. 2006;35(1):5–10. [DOI] [PubMed] [Google Scholar]
- 64.Markland D, Tobin V. A modification to the behavioural regulation in exercise questionnaire to include an assessment of amotivation, Journal of Sport and Exercise Psychology 26 (4) (2004) 191–11196. [Google Scholar]
- 65.Glascow RE, Harden SM, Gaglio B, Rabin B, Smith ML, Porter GC, Ory MG, Estabrooks PA, RE-AIM Planning and Evaluation Framework: Adapting to New Science and Practice With a 20-Year Review. Front. public health 7 (64) (2019) 10.3389/fpubh.2019.00064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Miles MB, Huberman AM, Saldaña J. Qualitative Data Analysis : A Methods Sourcebook. 3rd ed.; 2013. [Google Scholar]
- 67.Dziak Collins LM, & Wagner ATJJ FactorialPowerPlan SAS macro suite users’ guide (Version 1.0). University Park: The Methodology Center, Penn State. Published 2013. http://methodology.psu.edu [Google Scholar]
- 68.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kugler KC, Trail JB, Dziak JJ, Collins LM. Effect coding versus dummy coding in analysis of data from factorial experiments. Methodol Center, Pennsylvania State Univ Univ; Park PA. Published online 2012. [Google Scholar]
- 70.MacKinnon DP, Pirlott AG. Statistical Approaches for Enhancing Causal Interpretation of the M to Y Relation in Mediation Analysis. Personal Soc Psychol Rev. 2015;19(1):30–43. doi: 10.1177/1088868314542878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Valeri L, VanderWeele TJ. Mediation analysis allowing for exposure–mediator interactions and causal interpretation: Theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rubenstein LZ, Josephson KR, Trueblood PR, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. Journals Gerontol Ser A Biol Sci Med Sci. 2000;55(6):M317–M321. [DOI] [PubMed] [Google Scholar]
- 73.Zubala A, MacGillivray Stephen, Frost Helen, Kroll Thilo, .Skelton DawnA, Gavine Anna, Gray NicolaM., Toma Madalina, Morris Jacqui, Promotion of physical activity interventions for community dwelling older adults: A systematic review of reviews PLoS ONE 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]