Abstract
Objective
To develop and implement criteria for description of post COVID syndrome based on analysis of patients presenting for evaluation at Mayo Clinic Rochester between November 2019 and August 2020.
Methods
A total of 465 patients with a history of testing positive for COVID-19 were identified and their medical records reviewed. After a thorough review, utilizing the DELPHI methods by an expert panel, 42 (9%) cases were identified with persistent central sensitization (CS) symptoms persisting after the resolution of acute COVID-19, herein referred to as Post COVID syndrome (PoCoS). In this report we describe the baseline characteristics of these PoCoS patients.
Results
Among these 42 PoCoS patients, the mean age was 46.2 years (median age was 46.5 years). Pain (90%), fatigue (74%), dyspnea (43%), and orthostatic intolerance (38%) were the most common symptoms. The characteristics of an initial 14 patients were utilized for the development of clinical criteria via a modified Delphi Method by a panel of experts in central sensitization disorders. These criteria were subsequently applied in the identification of 28 additional cases of suspected PoCoS. A 2-reviewer system was used to analyze agreement with using the criteria, with all 28 cases determined to be either probable or possible cases by the reviewers. Inter-reviewer agreement using these proposed defining criteria was high with a Cohen’s alpha of .88.
Conclusions
Here we present what we believe to be the first definitional criteria for Post COVID syndrome. These may be useful in clinical phenotyping of these patients for targeted treatment and future research.
Keywords: COVID-19, central sensitization, post-covid syndrome, fibromyalgia, postural orthostatic tachycardia syndrome
Introduction
The COVID-19 pandemic was first described in December 2019, with the United States recognizing its first case in mid-January 2020. 1 Much attention has been focused on the acute and subacute manifestations of COVID-19 that have left hospitals dealing with multiple waves of the infection, creating shortages of personal protective equipment, intensive care unit (ICU) beds, and ventilators. 2 However, as the pandemic has progressed, there has been national recognition of a chronic post-infectious syndrome associated with COVID-19 termed post acute sequelae of SARS-CoV-2 infection (PASC), similar to post-ICU syndrome in critically ill patients.3,4 However, persistent symptoms following infection with COVID may occur even in the absence of ICU admission. A recent study in post-hospital discharge patients from Italy followed 143 patients, of which only 5% received invasive ventilation and 15% received non-invasive ventilation. 5 Of these patients, 87.4% had persistent symptoms at day 60 with the most common symptoms being fatigue, dyspnea, joint pain, and chest pain. In a telephone survey of 582 patients 3 weeks after testing positive for COVID-19, 35% of the 274 respondents had not yet returned to their usual state of health. 6 One of the largest symptom reports comes from an online community of COVID-19 patients experiencing post-infectious symptoms, Survivor Corps. 7 This report again identified fatigue, pain, and dyspnea as predominant symptoms, but also introduced several previously unreported symptoms including difficulty concentrating or focusing, difficulty sleeping, and exercise intolerance. This symptom constellation was also confirmed by clinicians from a large public health system in France. 8 and a large academic center in the US. 9 These additional symptoms are notably consistent with other post-infectious syndromes.
The phenomenon of patients developing persistent symptoms after infectious illnesses is well-established. Prolonged post-infectious syndromes have been reported following infections by highly inflammatory agents such as Epstein-Barr virus, West Nile virus, Zika, Chikununga, Severe Acute Respiratory Syndrome (SARS), and Borrelia spp. These syndromes may involve persistent fatigue, unrefreshing sleep, nausea, headaches, and cognitive dysfunction, among other symptoms that may differ from the presentation of the original acute illness.10-21 These symptoms persist far beyond 6 months in many cases, and patients eventually meet criteria for chronic fatigue syndrome (CFS) or another central sensitization syndrome (CSS), wherein perception of severity of sensory stimuli are enhanced. One consistent finding noted on neuroimaging in this patient population is persistent central nervous system (CNS) inflammation, particularly of the thalamus and midbrain.22,23 Laboratory abnormalities include increased proinflammatory cytokines such as TNF-α and IL-6, suppressed ACTH, and T cell dysregulation.14,20,24-30 Based upon our current knowledge, SARS-CoV-2 appears to be highly immunogenic, and indeed the putative mechanisms of many of the cardiovascular and pulmonary complications have also been determined to be immune-mediated. 31 It therefore stands to reason that SARS-CoV-2 has the potential to incite a significant post-viral syndrome with central sensitization, which we refer to as Post COVID syndrome (PoCoS), which is one of the clinical phenotypes seen in PASC.
Over the last decade, the epigenetics of fibromyalgia and other related central sensitization syndromes (disorders involving increased responsivity of the central nervous system to sensory stimuli) have become better elucidated. In fibromyalgia in particular, several candidate genes have been identified. 32 These genes are thought to be dormant at birth but can be activated via multiple epigenetic pathways during prolonged stressful circumstances—such as social, economic, or physical stressors, including major medical illness. Once activated, these genes allow for enhanced CNS sensitivity to a variety of stimuli including pain, fatigue, and sensation including vision, hearing, smell, and touch. 32 Individuals affected by central sensitization disorders often struggle with a significant symptom burden with very few positive clinical tests. Definitive treatment of these patients is difficult and as they almost always require a multi-modal approach to management.
The Mayo Clinic General Internal Medicine (GIM) division offers evaluation and treatment programs for individuals experiencing central sensitization, including those of post-infectious etiologies. Patients may directly request or be referred for evaluation at Mayo Clinic in Rochester for these concerns. Patient-reported symptoms are collected prior to appointment scheduling to facilitate consolidated appointment itineraries. Not surprisingly, GIM has seen an increase in requests for consultation from patients with unexplained symptoms following acute infection with COVID-19. Our team’s initial experience with long-term associated symptoms in COVID-19 is summarized below as we attempt to better define this new post-infectious syndrome.
Methods
Patient appointment request documentation submitted to GIM at Mayo Clinic Rochester from 11/15/2019 through 8/5/2020 were screened using a Boolean search for the keywords: “COVID,” “coronavirus,” “virus,” or “viral.” A total of 305 potential cases were initially identified, and their appointment request forms were deidentified and then manually reviewed. Cases that described new symptoms developing after a viral illness could potentially be consistent with PoCoS and were then submitted to a group of experts in fibromyalgia, postural orthostatic tachycardia syndrome (POTS), and CFS. Patients whose symptoms were not temporally related to their viral illness were excluded. A modified Delphi technique was implemented to determine criteria for case definition. The Delphi method, also known as the estimate-talk-estimate technique (ETE), is a systematic and qualitative method of forecasting by collecting opinions from a group of experts through several rounds of questions. 33 For this project, cases were reviewed independently by each reviewer and then graded into 1 of 3 categories with respect to their likelihood of having Post COVID syndrome—probable, possible, and unlikely. After circulating the combined assessment of patient classification, a meeting was held to discuss possible clinical and diagnostic criteria for identification of the Post COVID syndrome.
Subsequently, 160 new cases obtained between 11/15/2019 and 08/05/2020 were examined by 1 reviewer with determination of 28 possible or probable cases of Post COVID syndrome based on the developed criteria. The cases were then divided and distributed to the remaining 4 reviewers for a total of 40 new cases reviewed by each for concordance. A third reviewer was involved for cases in which there was disagreement between the first and second reviewer. A second Delphi round was held to determine whether the definitional criteria was reproducible and consistent.
Results
Patient Characteristics
Of the total 465 cases reviewed, 42 (9%) met criteria for PoCoS. Among the 42 patients, 14 (33.3%) patients identified as male and 28 (66.6%) female. Ages ranged from 21 to 74 with median and mean ages of 46.5 and 46.2 years, respectively. COVID testing was positive in 15 patients (35.7%), negative in 15 patients (35.7%), and was not reported or unavailable for 12 patients (28.6%).
The predominant symptoms reported were pain (90.2%), fatigue (73.8%), dyspnea (42.9%), and orthostatic intolerance (38.1%). Paresthesias and chest pain tended to be more common in men than women, while headache, anorexia, and joint pain were more common in women. Data was available for duration of symptoms on 38 of 42 patients, which ranged from 4 to 22 weeks with an average duration of 11 weeks. Patient level clinical data is presented in Table 1 and summarized in Table 2.
Table 1.
Clinical Characteristics of Patients with Probable Post-COVID Syndrome.
| Age | Gender | Duration of symptoms (weeks) | COVID PCR | Fatigue | Pain | Dyspnea | GI effects | Orthostatic intolerance | Palpitations | Cognitive Dysfunction | Paresthesia | Anorexia | Rash | Weakness | Edema | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chest | Joint | Myalgia | Headache | |||||||||||||||
| 53 | Female | 10 | Positive | Y | Y | Y | Y | |||||||||||
| 45 | Female | 10 | Positive | Y | Y | Y | Y | |||||||||||
| 44 | Male | 10 | Positive | Y | Y | Y | Y | |||||||||||
| 36 | Male | 10 | Negative | Y | Y | Y | ||||||||||||
| 46 | Female | 11 | N/A | Y | Y | Y | Y | Y | ||||||||||
| 52 | Female | 11 | Negative | Y | ||||||||||||||
| 69 | Female | 11 | Negative | Y | Y | |||||||||||||
| 63 | Female | 12 | N/A | Y | Y | Y | Y | Y | Y | |||||||||
| 47 | Female | 12 | N/A | Y | Y | |||||||||||||
| 68 | Male | 12 | N/A | Y | Y | Y | Y | Y | ||||||||||
| 32 | Female | 12 | Negative | Y | Y | Y | Y | |||||||||||
| 36 | Male | 12 | Positive | Y | Y | Y | Y | |||||||||||
| 30 | Female | 14 | Positive | Y | Y | Y | Y | Y | Y | Y | Y | Y | ||||||
| 67 | Female | 14 | Positive | Y | Y | Y | Y | Y | ||||||||||
| 52 | Male | 14 | Positive | Y | Y | Y | Y | |||||||||||
| 44 | Female | 15 | Positive | Y | Y | Y | ||||||||||||
| 29 | Male | 16 | N/A | Y | Y | Y | Y | Y | Y | Y | Y | Y | ||||||
| 45 | Male | 16 | Negative | Y | Y | Y | Y | |||||||||||
| 44 | Female | 18 | Negative | Y | Y | Y | Y | Y | Y | |||||||||
| 21 | Female | 18 | Positive | Y | Y | Y | Y | |||||||||||
| 43 | Male | 18 | Negative | Y | Y | Y | Y | Y | Y | Y | ||||||||
| 25 | Female | 18 | Positive | Y | Y | Y | Y | Y | ||||||||||
| 55 | Female | 19 | Positive | Y | Y | Y | Y | |||||||||||
| 42 | Female | 20 | Negative | Y | Y | Y | Y | Y | Y | Y | ||||||||
| 37 | Female | 20 | N/A | Y | Y | Y | Y | Y | ||||||||||
| 45 | Male | 20 | Negative | Y | Y | Y | Y | Y | Y | Y | ||||||||
| 49 | Male | 22 | Negative | Y | Y | Y | Y | Y | ||||||||||
| 69 | Female | 4 | Negative | Y | Y | Y | Y | Y | ||||||||||
| 60 | Female | 4 | N/A | Y | Y | Y | ||||||||||||
| 59 | Male | 4 | Negative | Y | ||||||||||||||
| 25 | Female | 6 | Negative | Y | Y | Y | ||||||||||||
| 55 | Female | 6 | Positive | Y | Y | Y | Y | Y | Y | |||||||||
| 55 | Male | 6 | N/A | Y | Y | |||||||||||||
| 55 | Male | 6 | N/A | Y | Y | Y | ||||||||||||
| 54 | Female | 7 | N/A | Y | Y | Y | Y | Y | Y | |||||||||
| 41 | Female | 8 | N/A | Y | Y | Y | ||||||||||||
| 66 | Female | 8 | Positive | Y | ||||||||||||||
| 53 | Female | 9 | N/A | Y | Y | Y | ||||||||||||
| 28 | Female | Undefined | Positive | Y | Y | Y | Y | Y | ||||||||||
| 45 | Male | Undefined | Positive | Y | Y | |||||||||||||
| 71 | Female | Undefined | Negative | Y | Y | Y | Y | Y | ||||||||||
| 74 | Male | Undefined | Negative | Y | Y | Y | Y | |||||||||||
Table 2.
Frequency of Post-COVID Symptoms by Gender and COVID PCR Status.
| Symptom | Female (n = 28) | Male (n = 14) | Relative risk (female) | COVID positive PCR (n = 15) | COVID negative or not available (n = 27) | Relative risk (COVID positive) |
|---|---|---|---|---|---|---|
| Anorexia | 3 | 0 | 3.6 (P = .38) | 0 | 3 | 0.25 (P = .35) |
| Edema | 3 | 1 | 1.5 (P = .71) | 1 | 3 | 0.60 (P = .65) |
| Paresthesia | 3 | 5 | 0.3 (P = .07) | 4 | 4 | 1.80 (P = .35) |
| Rash | 6 | 2 | 1.5 (P = .59) | 1 | 7 | 0.26 (P = .18) |
| Weakness | 4 | 4 | 0.5 (P = .27) | 2 | 6 | 0.60 (P = .50) |
| Cognitive dysfunction | 7 | 2 | 1.8 (P = .44) | 4 | 5 | 1.44 (P = .54) |
| Palpitations | 9 | 4 | 1.1 (P = .82) | 5 | 8 | 1.13 (P = .80) |
| GI effects | 11 | 3 | 1.8 (P = .28) | 5 | 9 | 1.00 (P = 1.00) |
| Orthostatic intolerance | 9 | 7 | 0.6 (P = .25) | 9 | 7 | 2.31 (P = .03) |
| Dyspnea | 10 | 8 | 0.6 (P = .17) | 6 | 12 | 0.90 (P = .78) |
| Fatigue | 19 | 12 | 0.8 (P = .17) | 9 | 22 | 0.74 (P = .18) |
| Any pain | 24 | 13 | 1.2 (P = .30) | 14 | 23 | 1.10 (P = .39) |
| Chest pain | 10 | 9 | 0.6 (P = .07) | 10 | 6 | 1.80 (P = .18) |
| Joint Pain | 6 | 1 | 3.2 (P = .26) | 1 | 4 | 0.45 (P = .46) |
| Myalgia | 7 | 4 | 0.9 (P = .80) | 4 | 2 | 3.60 (P = .11) |
| Headache | 9 | 2 | 2.3 (P = .25) | 3 | 5 | 1.08 (P = .91) |
Definitional Criteria Performance
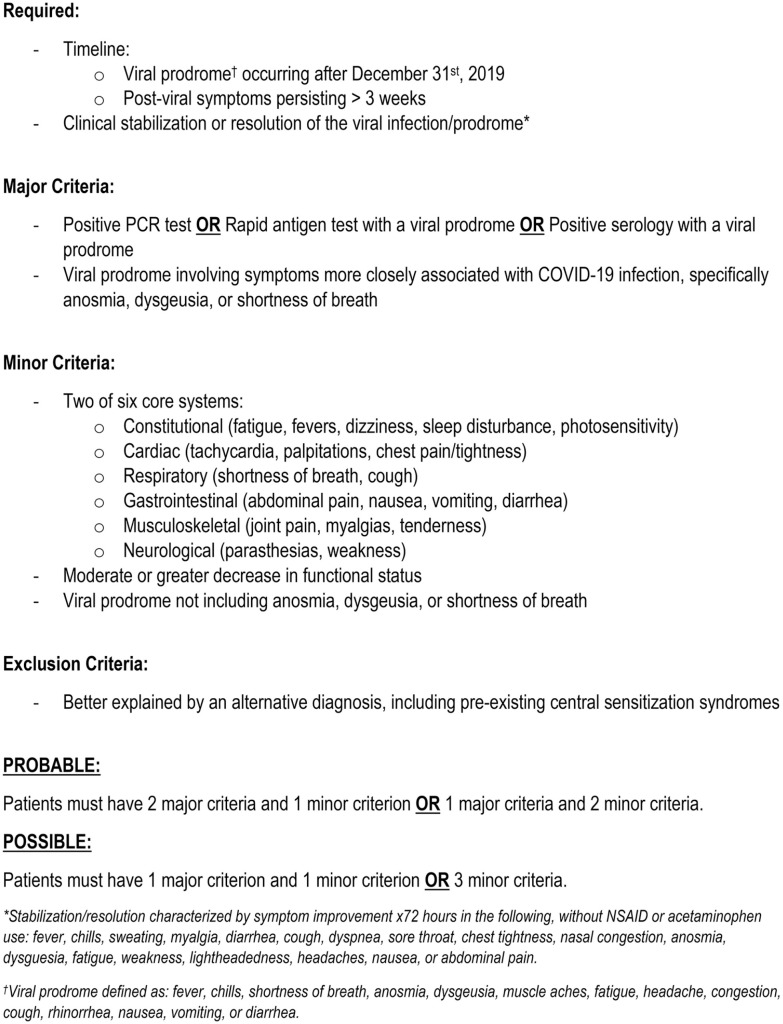
All 28 cases identified by the first reviewer were also characterized by the second reviewer as probable (very likely) or possible (potential but not likely) cases of PoCoS. Four of the remaining 132 cases were initially deemed unlikely but considered to be possible by the second reviewer and were therefore submitted to a third reviewer. The cases of disagreement were additionally examined by the group of experts to identify areas indicating potential improvement of the criteria. Of the disputed cases, 3 were ultimately classified as unlikely based on the established criteria, and 1 case demonstrated the need to specify the viral prodrome as occurring after December 31st, 2019 to be considered within the appropriate timeline for COVID-19 infection. The final consensus diagnostic criteria are shown in Figure 1. Cohen’s kappa was calculated as .88; reviewer concordance is detailed in Table 3.
Figure 1.
Proposed post-COVID syndrome diagnostic criteria.
Table 3.
Reviewer Concordance for Diagnosis of Post-COVID Syndrome.
| # of cases | Concordance | |
|---|---|---|
| Reviewer agreement | ||
| Probable/probable | 12 | |
| Possible/possible | 14 | |
| Unlikely/unlikely | 128 | |
| Reviewer disagreement | ||
| Probable/possible | 2 | |
| Possible/unlikely | 4 | |
| Total cases | 160 | 154/160 = 96.3% |
| Cohen’s kappa = .88 | ||
Discussion
It is now well-documented that many patients infected with COVID-19 may have persistent symptoms even after resolution of the acute infection. These symptoms may be either specific to COVID itself or secondary to long-term hospitalizations including ICU and ventilator care. The most common symptoms reported with our PoCoS cases were fatigue, pain, orthostatic intolerance, dyspnea, and palpitations. Interestingly, these symptoms show remarkable similarity to other post-infectious syndromes such as those associated with EBV, West Nile virus, and Borrelia spp.9-14 We propose using the term PoCoS to describe the subset of PASC patients who present with a constellation of symptoms consistent with CSS after clinical recovery from acute COVID illness. Should these symptoms persist >6 months without significant apparent other underlying etiology, these patients may meet the clinical definition of one of the common CSS disorders—FM, CFS, or POTS.34-36
Clinical Criteria
While PASC has been recognized by the NIH, data are still limited on patient symptoms and the underlying etiology of PASC. We propose that PASC is heterogenous with several phenotypes, including those secondary to tissue damage, such as dyspnea, myocarditis, and anosmia, and those not secondary to identifiable tissue damage but rather to CSS (PoCoS).
Our demographics do seem to follow the traditional gender distribution of central sensitization syndromes with a 2:1 female to male preponderance, as well as a rough prevalence of around 10% of patients screened, which match published estimates.9,37 The symptoms reported by our patient population correlate positively with those reported to date by others with pain (90%), fatigue (74%), dyspnea (43%), orthostatic intolerance (38%), and GI effects (33%) being the most common symptoms. This constellation of symptoms correlates with that seen in other post-infectious syndromes.
The proposed definitional criteria allow an entry point for patients who did not have a positive PCR or antibody test. This decision was initially made secondary to the lack of widespread availability of appropriate testing initially in the COVID-19 pandemic which was the period of time during which many of our sample patients experienced symptoms. This particular criterion should be considered by each center based upon local availability of COVID-19 testing.
Our brief descriptive study has several significant potential areas of bias including small sample size and self-selection of patients to apply for a consultative medicine appointment, which could select for those with more serious disease and a higher socioeconomic demographic. However, given the similarities in patient symptomatology and outcomes between our sample and that portrayed in previous literature, the syndrome description appears appropriate.5-7,9,38
Based on results from our modified Delphi, the proposed clinical criteria for diagnosis of PoCoS demonstrated strong inter-reviewer concordance with a Cohen’s kappa of .88. We also note that characterizations were made on patient appointment request documentation, which may provide limited information based on what the patient reports in their form; as such, we acknowledge that there may have been cases which may have been found to be consistent with PoCoS with additional inquiry by a provider. Given these limitations, it is likely that these criteria will in fact have greater sensitivity upon application to full clinical encounters.
Approach
The approach to the patient who has persistent symptoms after active COVID infection needs to be carefully conducted as these patients can have significant organ system dysfunction. We propose that these patients undergo a comprehensive evaluation for organ damage based on symptom constellation. If at the end of comprehensive evaluation there is no objective evidence of organ dysfunction, a diagnosis of PoCoS could be considered, and these patients should be treated with graded rehabilitation.
Future Directions
Based on our current knowledge, PoCoS can affect adults of any age and disease severity with variable penetrance.5-7,9,38 This implies that there are intrinsic patient factors that may play a role in pathogenesis of this syndrome. Patients who were asymptomatic in their acute exposure or those who demonstrated evidence of central sensitization syndromes prior to infection were notably excluded from this set of criteria in order to reduce confounding variables; however, we now know that asymptomatic patients may develop secondary symptoms, 9 and it is certainly a possibility that individuals with preexisting central sensitization may have new or worsening symptoms following infection with COVID-19. There is currently insufficient information to predict the anticipated severity and duration of this syndrome based on patient presentation. These topics will need to be elucidated further through further research, and we anticipate that these criteria may continue to be modified as we learn more about the COVID-19 virus and its long-term effects. Given its similarity to other post-infectious syndromes, such efforts may also provide useful understanding for these types of conditions as a whole.
Conclusion
The COVID-19 pandemic has already caused significant economic, social, and health-related global disruption with over 165 million infections and 3.4 million deaths as of May 20, 2021. 39 A portion of patients with PASC present with delayed and significantly prolonged symptoms even after clinical resolution of the virus. Better definition of the pathophysiology and treatment underlying PASC is needed in order to provide appropriate care to these patients in the clinical setting. We present a subset of PASC patients that have characteristics of central sensitization disorder and propose the nomenclature of Post COVID Syndrome, or PoCoS, for this subgroup. Given the similarities to other post-infectious syndromes, it is hopeful that the scientific progress we make on this front may be applicable not only to those afflicted with Post COVID syndrome, but also to the millions of other patients suffering from this spectrum of disorders.
Footnotes
Authors’ Contributions: DMB, CAA, SLG, BS, ITC, RTH, and RG made substantial contributions to the concept and design of the study, the interpretation of data, and the critical revision of the manuscript for important intellectual content, made substantial contributions to the acquisition of data, the analysis and interpretation of data, drafting of the manuscript, and substantial contributions to critical revision of the manuscript for important intellectual content.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Stephanie L. Grach  https://orcid.org/0000-0002-8337-6219
https://orcid.org/0000-0002-8337-6219
Ivana T. Croghan  https://orcid.org/0000-0003-3464-3525
https://orcid.org/0000-0003-3464-3525
Ravindra Ganesh  https://orcid.org/0000-0002-6877-1712
https://orcid.org/0000-0002-6877-1712
References
- 1. Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929-936. doi: 10.1056/NEJMoa2001191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ranney ML, Griffeth V, Jha AK. Critical supply shortages – the need for ventilators and personal protective equipment during the covid-19 pandemic. N Engl J Med. 2020;382(18):e41. doi: 10.1056/NEJMp2006141 [DOI] [PubMed] [Google Scholar]
- 3. Jaffri A, Jaffri UA. Post-intensive care syndrome and COVID-19: crisis after a crisis? Heart Lung. 2020;49(6):883-884. doi: 10.1016/j.hrtlng.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jiang DH, McCoy RG. Planning for the post-COVID syndrome: how payers can mitigate long-term complications of the pandemic. J Gen Intern Med. 2020;35(10):3036-3039. doi: 10.1007/s11606-020-06042-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute covid-19. JAMA. 2020;324(6):603-605. doi: 10.1001/jama.2020.12603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network – United States, March-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(30):993-998. doi: 10.15585/mmwr.mm6930e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lambert N, Corps S, El-Azab SA, et al. COVID-19 survivors’ reports of the timing, duration, and health impacts of post-acute sequelae of SARS-CoV-2 (PASC) infection. BMJ 2021. doi: 10.1101/2021.03.22.21254026 [DOI] [Google Scholar]
- 8. Davido B, Seang S, Tubiana R, de Truchis P. Post-COVID-19 chronic symptoms: a postinfectious entity? Clin Microbiol Infect. 2020;26(11):1448-1449. doi: 10.1016/j.cmi.2020.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Logue JK, Franko NM, McCulloch DJ, et al. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw Open. 2021;4(2):e210830. doi: 10.1001/jamanetworkopen.2021.0830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cook RL, Xu X, Yablonsky EJ, et al. Demographic and clinical factors associated with persistent symptoms after West Nile virus infection. Am J Trop Med Hyg. 2010;83(5):1133-1136. doi: 10.4269/ajtmh.2010.09-0717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Duvignaud A, Fianu A, Bertolotti A, et al. Rheumatism and chronic fatigue, the two facets of post-chikungunya disease: the TELECHIK cohort study on Reunion island. Epidemiol Infect. 2018;146(5):633-641. doi: 10.1017/S0950268818000031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Islam MF, Cotler J, Jason LA. Post-viral fatigue and COVID-19: lessons from past epidemics. Fatigue. 2020;8(2):61-69. doi: 10.1080/21641846.2020.1778227 [DOI] [Google Scholar]
- 13. Kristiansen MS, Stabursvik J, O’Leary EC, et al. Clinical symptoms and markers of disease mechanisms in adolescent chronic fatigue following Epstein-Barr virus infection: an exploratory cross-sectional study. Brain Behav Immun. 2019;80:551-563. doi: 10.1016/j.bbi.2019.04.040 [DOI] [PubMed] [Google Scholar]
- 14. Leis AA, Grill MF, Goodman BP, et al. Tumor necrosis factor-alpha signaling may contribute to chronic west Nile virus post-infectious proinflammatory state. Front Med. 2020;7:164. doi: 10.3389/fmed.2020.00164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011;11:37. doi: 10.1186/1471-2377-11-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pedersen M, Asprusten TT, Godang K, et al. Predictors of chronic fatigue in adolescents six months after acute Epstein-Barr virus infection: a prospective cohort study. Brain Behav Immun. 2019;75:94-100. doi: 10.1016/j.bbi.2018.09.023 [DOI] [PubMed] [Google Scholar]
- 17. Pedersen M, Asprusten TT, Godang K, et al. Fatigue in Epstein-Barr virus infected adolescents and healthy controls: a prospective multifactorial association study. J Psychosom Res. 2019;121:46-59. doi: 10.1016/j.jpsychores.2019.04.008 [DOI] [PubMed] [Google Scholar]
- 18. Rodriguez-Morales AJ, Simon F. Chronic chikungunya, still to be fully understood. Int J Infect Dis. 2019;86:133-134. doi: 10.1016/j.ijid.2019.07.024 [DOI] [PubMed] [Google Scholar]
- 19. Sejvar JJ, Curns AT, Welburg L, et al. Neurocognitive and functional outcomes in persons recovering from West Nile virus illness. J Neuropsychol. 2008;2(2):477-499. doi: 10.1348/174866407x218312 [DOI] [PubMed] [Google Scholar]
- 20. Sepulveda N, Carneiro J, Lacerda E, Nacul L. Myalgic encephalomyelitis/chronic fatigue syndrome as a hyper-regulated immune system driven by an interplay between regulatory T cells and chronic human herpesvirus infections. Front Immunol. 2019;10:2684. doi: 10.3389/fimmu.2019.02684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shikova E, Reshkova V, Kumanova capital AC, et al. Cytomegalovirus, Epstein-Barr virus, and human herpesvirus-6 infections in patients with myalgic encephalomyelitis/chronic fatigue syndrome. J Med Virol. 2020;92:3682-3688. doi: 10.1002/jmv.25744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fujii H, Sato W, Kimura Y, et al. Altered structural brain networks related to adrenergic/muscarinic receptor autoantibodies in chronic fatigue syndrome. J Neuroimaging. 2020;30(6):822-827. doi: 10.1111/jon.12751 [DOI] [PubMed] [Google Scholar]
- 23. Maksoud R, du Preez S, Eaton-Fitch N, et al. A systematic review of neurological impairments in myalgic encephalomyelitis/ chronic fatigue syndrome using neuroimaging techniques. PLoS One. 2020;15(4):e0232475. doi: 10.1371/journal.pone.0232475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Agliari E, Barra A, Vidal KG, Guerra F. Can persistent Epstein-Barr virus infection induce chronic fatigue syndrome as a Pavlov reflex of the immune response? J Biol Dyn. 2012;6:740-762. doi: 10.1080/17513758.2012.704083 [DOI] [PubMed] [Google Scholar]
- 25. Banfi G, Diani M, Pigatto PD, Reali E. T cell subpopulations in the physiopathology of fibromyalgia: evidence and perspectives. Int J Mol Sci. 2020;21(4):1186. doi: 10.3390/ijms21041186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Harvey JM, Broderick G, Bowie A, et al. Tracking post-infectious fatigue in clinic using routine Lab tests. BMC Pediatr. 2016;16:54. doi: 10.1186/s12887-016-0596-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ji RR, Nackley A, Huh Y, Terrando N, Maixner W. Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology. 2018;129(2):343-366. doi: 10.1097/aln.0000000000002130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Morris G, Maes M, Berk M, Puri BK. Myalgic encephalomyelitis or chronic fatigue syndrome: how could the illness develop? Metab Brain Dis. 2019;34(2):385-415. doi: 10.1007/s11011-019-0388-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ramos S, Brenu E, Broadley S, et al. Regulatory T, natural killer T and gammadelta T cells in multiple sclerosis and chronic fatigue syndrome/myalgic encephalomyelitis: a comparison. Asian Pac J Allergy Immunol. 2016;34(4):300-305. doi: 10.12932/AP0733 [DOI] [PubMed] [Google Scholar]
- 30. Theoharides TC, Tsilioni I, Bawazeer M. Mast cells, neuroinflammation and pain in fibromyalgia syndrome. Front Cell Neurosci. 2019;13:353. doi: 10.3389/fncel.2019.00353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Azkur AK, Akdis M, Azkur D, et al. Immune response to SARS-CoV-2 and mechanisms of immunopathological changes in COVID-19. Allergy. 2020;75(7):1564-1581. doi: 10.1111/all.14364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. D’Agnelli S, Arendt-Nielsen L, Gerra MC, et al. Fibromyalgia: genetics and epigenetics insights may provide the basis for the development of diagnostic biomarkers. Mol Pain. 2019;15:1744806918819944. doi: 10.1177/1744806918819944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. CFI. What is the Delphi method? Accessed May 20, 2021, https://corporatefinanceinstitute.com/resources/knowledge/other/delphi-method/
- 34. Committee on the Diagnostic Criteria for Myalgic Encephalomyelitis/Chronic Fatigue S, Board on the Health of Select P, Institute of M. The National Academies Collection: Reports funded by National Institutes of Health. Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness. National Academies Press; 2015. [Google Scholar]
- 35. Raj SR, Guzman JC, Harvey P, et al. Canadian cardiovascular society position statement on postural orthostatic tachycardia syndrome (POTS) and related disorders of chronic orthostatic intolerance. Can J Cardiol. 2020;36(3):357-372. doi: 10.1016/j.cjca.2019.12.024 [DOI] [PubMed] [Google Scholar]
- 36. Wolfe F, Clauw DJ, Fitzcharles MA, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46(3):319-329. doi: 10.1016/j.semarthrit.2016.08.012 [DOI] [PubMed] [Google Scholar]
- 37. Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370:m3026. doi: 10.1136/bmj.m3026 [DOI] [PubMed] [Google Scholar]
- 38. Halpin SJ, McIvor C, Whyatt G, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J Med Virol. 2021;93:1013-1022. doi: 10.1002/jmv.26368 [DOI] [PubMed] [Google Scholar]
- 39. Coronavirus Research Center. Johns Hopkins University & Medicine. Accessed May 20, 2021, https://coronavirus.jhu.edu/