Abstract
Hyaluronic acid injection is becoming a popular way for penile augmentation. However, only few studies and follow-ups have investigated the various complications of hyaluronic acid injection and their corresponding management. In this study, a total of 230 patients who had penile augmentation with hyaluronic acid injection from January 2018 to December 2019 were examined on follow-up for penile girth, complications, and their corresponding management. At 1-month, 3-month, and 6-month postoperative follow-ups, the penile circumference had increased by 2.66 ± 1.24 cm, 2.28 ± 1.02 cm, and 1.80 ± 0.83 cm, respectively. During the entire 6-month follow-up, 4.3% had complications such as subcutaneous bleeding, subcutaneous nodules, and infection. There were no systemic or local allergic reactions among all the patients. All complications were treated accordingly, and no further deterioration or severe sequelae were observed. Although complications of hyaluronic acid injections are mild and rare, these may affect the patient's satisfaction postoperatively. Preoperative redundant prepuce may increase the incidence of penile edema or postoperative gel migration. Standardization of the surgery protocol and elucidation of the effects of other injection parameters are still lacking. Nevertheless, it still highlights the importance of preoperative preparation and surgical technique.
Keywords: complications, hyaluronic acid injection, penile augmentation
INTRODUCTION
Penile size is an important index for the measurement of sexual development in men. It is perceived as a symbol of health, sexual performance, and masculinity.1,2 According to some studies, penile size is related to self-esteem, and men who underestimate their size may have a stronger tendency to exaggerate physiological defects and express psychological distress.3,4 As a result, they are prone to feeling depressed.5 The tendency of men to exaggerate women's penile size preference appears to drive anxiety and sexual dissatisfaction.6,7 Girth is considered more important than length.6 Due to all the reasons stated above, more and more men are consulting about penile augmentation (PA) and looking for ways to increase sexual attraction and satisfaction.
As the soft-tissue filling surgery becomes safer, it is also becoming more popular and accepted as a micro-invasive procedure for soft-tissue augmentation.8 Hyaluronic acid (HA) injection was considered to be safe in PA and can significantly improve psychological distress from small penis syndrome, a disorder where a person becomes anxious about having a small penis in the presence of a clinically normal penile size.9,10 However, few complications of the surgery were described. To our knowledge, though the adverse effects of the HA injection are usually mild, if any, at the least, these may cause negative psychological effects on the patients. In this article, we discussed the common complications after HA injections for PA and present our management after them.
PATIENTS AND METHODS
This is a retrospective study involving patients who underwent PA with HA injection in Beijing Eden Hospital (Beijing, China) and Chengdu Kowloon Hospital (Chengdu, China) between January 2018 and December 2019. The study was approved by the review board institution of Beijing Eden Hospital (No. S2017011) and Chengdu Kowloon Hospital (No. An0012). The inclusion criteria were adult males who (1) wanted to improve their quality of sex life, (2) were dissatisfied with their penile size, and (3) were willing to undergo surgery. The exclusion criteria were patients who (1) were over 65 years of age, (2) had coagulopathy, and (3) had to take long-term anticoagulants. A total of 230 patients (average age: 30.34 years) were selected. All patients have been informed of the study and have approved the collection of patient data. Photographs were taken before the operation and at the 1st, 3rd, and 6th month of follow-up. Penile girth, self-reported satisfaction, and postsurgical discomfort were assessed. All data were analyzed using descriptive statistics (SPSS statistics version 20, IBM, New York, NY, USA). The results were expressed as mean ± standard deviation (s.d.). All participants received previous counseling and signed informed consent.
The surgery was done by an experienced genital reconstructive surgeon (XWZ) under local anesthesia with lidocaine. An 18G cannula was used to establish an injection tunnel at the root of the penis. HA (Martifill, Wuhao Biological Technology, Shanghai, China) was injected through the tunnel between the penile superficial fascia and Buck's fascia. The total amount of HA injected ranged from 13 ml to 25 ml (mean ± s.d.: 16.30 ± 2.46 ml) depending on the size of the patient's penis. After injection, the doctor sutured the injection point with 4-0 Vicryl absorbable thread. The penis was dressed with elastic bandages for 14–21 days. Meanwhile, patients were taught to massage the penis to make the HA distributed evenly under the skin. Patients were asked to abstain from sexual intercourse for the first 4 weeks post-surgery.
RESULTS
At the 1st, 3rd, and 6th month follow-up, the penile circumference had increased by 2.66 ± 1.24 cm, 2.28 ± 1.02 cm, and 1.80 ± 0.83 cm (mean ± s.d.), respectively (Table 1). During the 6-month follow-up, 4.3% (10/230) of the patients experienced complications, most of which were mild, namely, subcutaneous bleeding (1.3%), subcutaneous nodules (2.2%), and infection (0.9%). There were no systemic or local allergic reactions among all the patients.
Table 1.
Characteristics of all patients
| Variables | All patients (n=230) |
|---|---|
| Age (year) | 30.30±5.23 |
| BMI (kg m−2) | 23.70±3.17 |
| HA dosage (ml) | 16.30±2.46 |
| Penile girth (cm) | |
| Preoperation | 8.20±2.01 |
| Growth at 1-month follow-up | 2.66±1.24 |
| Growth at 3-month follow-up | 2.28±1.02 |
| Growth at 6-month follow-up | 1.80±0.83 |
All data are presented as mean±s.d. s.d.: standard deviation; BMI: body mass index; HA: hyaluronic acid
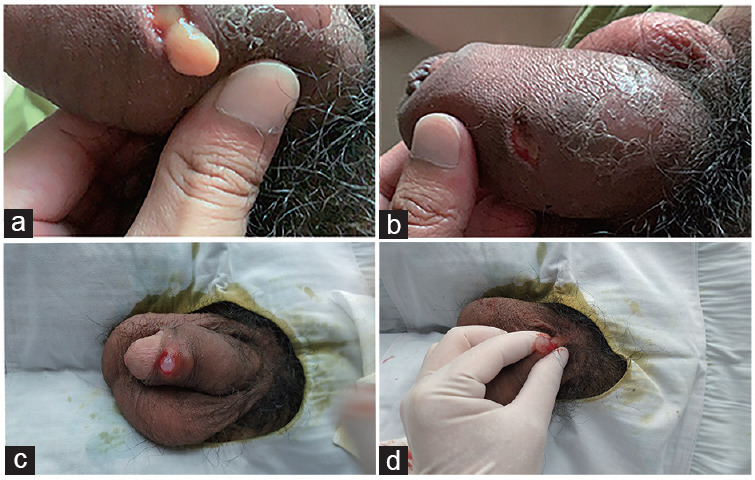
Subcutaneous bleeding manifested as a darkened skin on the penis, often causing panic in patients (Figure 1). Subcutaneous nodules presented as masses with diameters larger than 1 cm. Because nodules smaller than 1 cm can be managed by massaging for several days, only the large nodules have to be removed surgically. Nonetheless, all of the nodules were painless, visible, and palpable (Figure 1). Infection always occurred in the unhealed wound, presenting as a sudden warm penile swelling with redness (Figure 2). The symptoms are often found by the patients themselves. After confirmation by the surgeon, the complications were managed by their corresponding treatment.
Figure 1.

Subcutaneous bleeding and subcutaneous nodule. (a) The front view of a patient who developed subcutaneous bleeding characterized by skin darkening on the 3rd day postoperation. (b) The side view of this patient. (c) The front view of a patient who developed subcutaneous nodules on the 17th day postoperation. (d) The side view picture shows that the patient had multiple subcutaneous nodules.
Figure 2.

Infection in penis postoperation. The patient developed skin infection on the 50th day postoperation. The entire hyaluronic acid layer was infected, presenting as a total penile swelling.
DISCUSSION
HA is a key component of the extracellular matrix, found naturally in the human body. Because of the small chemical structure and similarity among all species, HA seldom causes implant rejection or allergic reactions.10,11 Previous studies have shown that HA injection is a feasible and safe micro-invasive surgery for PA.12,13 Although injected HA gel is gradually degraded after 6 months, causing a 15% decrease in the maximal circumference after 5 years, it is still a long-term effective method for PA.14,15
To our knowledge, there are no follow-up studies to identify the complications of PA using HA injection due to the low incidence. Based on the current classifications,16 the complications of filler surgery can be classified into three types, namely, (1) basic health status of patients, (2) surgical problems, and (3) filler properties. Because many studies have confirmed the safety of HA injection in penile surgery, our study mainly focused on the first two types.
This study has found that the complications of PA with HA injection were subcutaneous nodule, penile edema, and infection. The timeline of these complications is summarized in Figure 3.
Figure 3.
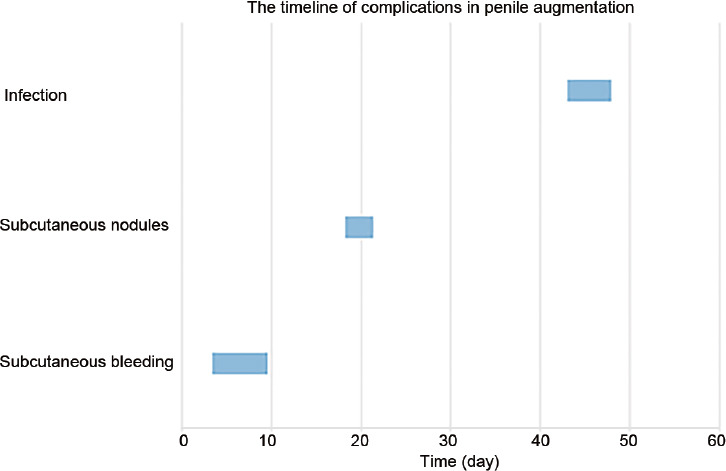
The timeline of complications in penile augmentation. The average time of appearance and duration of the complications.
Penile subcutaneous nodule
The most common complication of HA injection among patients is penile subcutaneous nodule (total incidence of 2.2%), usually occurring 2 weeks post-surgery. The nodules we described are related to the accumulation of HA in one area.15 Because HA requires a certain period of time for redistribution and shaping, elastic bands and penile massage may be used to evenly disperse HA. However, when HA is injected too fast, it may not distribute evenly. This may result in the development of nodules refractory to penile massage therapy after 1–2 weeks. Although these nodules tend to be painless, they can last for a long time if not managed.16 Moreover, due to the thin skin of the penis, subcutaneous nodules larger than 1 cm usually become noticeable and palpable. As a result, patients may feel discomfort and depression during sex. Moreover, these nodules cannot resolve spontaneously.
Treatment options include surgery17 (Figure 4) and hyaluronidase therapy.18,19 Surgery, however, may undermine PA as local HA is removed as well. On the other hand, hyaluronidase therapy is done by fine-needle injection of an appropriate amount (usually 30 units) of hyaluronidase depending on the size of the nodule. It usually takes about 3 days to take effect, and patients would not have to undergo another surgery. The disadvantage is that results are not instant – additional one or two treatments may be required to completely eradicate a nodule.
Figure 4.
Nodule removal and purulent fluid and hyaluronic acid gel in the infected penile skin. (a) Purulent fluid and hyaluronic acid gel discharge following incision. (b) Three days after debridement. (c) Incision of a nodule from the penile skin. (d) Removal of the subcutaneous nodule.
These nodules, however, can be prevented by making HA distribution more uniform. To do this, we made two adjustments, specifically, the use of (1) low HA dose (about 0.3 ml each) and (2) multi-point fan technique.
Subcutaneous bleeding
In the present study, subcutaneous bleeding occurred in 1.3% of all the patients. It mainly happens 2–5 days after surgery and peaks at the first week. The main mechanism of subcutaneous bleeding in HA injection is direct vascular puncture. Although HA injection is a micro-invasive surgery, use of anti-thrombotic drugs prior to treatments must be halted to decrease the risk of bleeding. Furthermore, the use of cannulas rather than needle has been shown to help decrease its risk.11 Reports have also shown that the use of thicker needle tubes to establish a cannula may reduce the incidence of subcutaneous bleeding. To prevent it, we used an 18G cannula to create a skin tunnel for HA injection. Subcutaneous bleeding, if any, can spontaneously resolve in a transient period. The most important thing the doctors can do is to reassure patients.
Infection
Infection is a common complication in any surgical procedure. However, the incidence of infection following soft-tissue injection is low.20 In the present study, only two patients were reported to have infection, both of whom are diabetic and had sexual intercourse 1–2 months post-surgery.
There are four main elements that can contribute to infection: (1) patient characteristics, (2) intercourse, (3) injection factors, and (4) HA gel features. Patient characteristics such as diabetes and immunodeficiency increase the risk of developing infections, particularly in the genital region. Intercourse can also contribute to infection. Bacteria, present abundantly in the vagina and pubic hair, may enter the unhealed wound during intercourse and cause infection.
Injection factors such as cannula size and injection site have a crucial role in infection. Unlike the results of Jeong et al.12 and Kwak et al.,14 complications such as subcutaneous nodule and infection are more frequent in our study. In the study of Kim et al.,21 initial and supplemental HA injections at 2 weeks were done via cannulation with sizes of 27G and 30G, respectively, based on the HA gel used. Moreover, HA gel injection was done in the glans penis without suturing. In our study, we found that injecting the root of the penis using an 18G cannula provides ease for the even distribution of HA. However, a disadvantage is that in some of the patients, the injection sites do not heal spontaneously, which may be sites for infection from the pubic hair flora in the absence of skin preparation. As a result, suturing of injection site was done.
Several HA gel features have been implicated in infections and subcutaneous nodules. In our study, a mono-phasic and synthetic HA was used. Aseptic technique was strictly followed to reduce the possibilities of infection.
The two patients that had infection during the follow-up underwent incision and drainage (I&D). Incision was made on the penile skin with swelling. Due to the high internal pressure, HA and purulent fluid were discharged and drained from the incision point (Figure 4). After I&D, intravenous antibiotics were administered for 3–5 days. Both healed without further progression and discomfort. This indicates that although HA injection is safe for most of the patients, diabetics and immunocompromised patients have a higher risk for infection.
Penile edema is characterized by swelling of the penile skin (Figure 5). Interestingly, all the 21 patients who had penile edema after PA with HA injection had the problem of redundant prepuce and did not underwent preoperative circumcision. Redundant prepuce may cause distal accumulation of the injected HA gel and lead to lymphatic compression.22 Penile edema can be relieved by using elastic bandage for 2 weeks without severe adverse effects.
Figure 5.

Penile edema in a 33-year-old patient with redundant prepuce. The patient developed penile edema on the 35th day postoperation following sexual intercourses.
This study is limited by patient variability, sample size, and temporal constraints, which must be addressed in future studies.
Differences among patients (e.g., redundant prepuce before injection) must be standardized in the succeeding studies. Our results have shown that the patients who had penile edema after the operation had redundant prepuce. In a randomized controlled trial by Abdallah et al.23 where all the patients were circumcised prior to HA gel injection, no penile edema was reported. Although there is no study explaining the role of redundant prepuce on the incidence of complications, we hypothesized that the distal migration of the injected HA contributes to its pathogenesis. Thus, we strongly recommend circumcision before operation.
Second, the low number of cases and short follow-up period hindered the detection of rare and late-onset complications. In future, longer follow-up time must be implemented to yield more convincible results on penile girth, complications, and satisfaction of the patients.
CONCLUSIONS
This article mainly discussed the complications and management of PA with HA injection. We aimed to provide some effective treatment ideas for the complications of HA injection. According to the existing statistics, the overall complication rate of this method is acceptable. Furthermore, most of the complications can resolve spontaneously without further side effects. If complications are diagnosed, prognosis is satisfactory after treatment. Although standardization of surgical protocols and elucidation of the effects of several HA parameters are still lacking, it is sufficient to conclude that HA injection is an effective and safe method for PA.
AUTHOR CONTRIBUTIONS
YQ participated in the surgery and follow-up and drafted the manuscript. ZRG made the main follow-up work and recorded the complications. XD arranged the data and made the statistics. LK helped to draft the manuscript. MZ participated in the arrangement of figures and tables. QL and TX participated in the study design. XWZ participated in the surgeries, guided the study, and made the managements of all the complications. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
ACKNOWLEDGMENTS
This study was supported by Beijing Municipal Natural Science Foundation (No. 7194327).
REFERENCES
- 1.Wang YN, Zeng Q, Xiong F, Zeng Y. Male external genitalia growth curves and charts for children and adolescents aged 0 to 17 years in Chongqing, China. Asian J Androl. 2018;20:567–71. doi: 10.4103/aja.aja_51_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wylie KR, Eardley I. Penile size and the 'small penis syndrome'. BJU Int. 2007;99:1449–55. doi: 10.1111/j.1464-410X.2007.06806.x. [DOI] [PubMed] [Google Scholar]
- 3.Veale D, Miles S, Read J, Bramley S, Troglia A, et al. Relationship between self-discrepancy and worries about penis size in men with body dysmorphic disorder. Body Image. 2016;17:48–56. doi: 10.1016/j.bodyim.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Vardi Y, Lowenstein L. Penile enlargement surgery–fact or illusion? Nat Clin Pract Urol. 2005;2:114–5. doi: 10.1038/ncpuro0120. [DOI] [PubMed] [Google Scholar]
- 5.Son H, Lee H, Huh JS, Kim SW, Paick JS. Studies on self-esteem of penile size in young Korean military men. Asian J Androl. 2003;5:185–9. [PubMed] [Google Scholar]
- 6.Francken AB, van de Wiel HB, van Driel MF, Weijmar Schultz WC. What importance do women attribute to the size of the penis? Eur Urol. 2002;42:426–31. doi: 10.1016/s0302-2838(02)00396-2. [DOI] [PubMed] [Google Scholar]
- 7.Prause N, Park J, Leung S, Miller G. Women's preferences for penis size: a new research method using selection among 3d models. PLoS One. 2015;10:e0133079. doi: 10.1371/journal.pone.0133079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Urdiales-Gálvez F, Delgado NE, Figueiredo V, Lajo-Plaza JV, Mira M, et al. Treatment of soft tissue filler complications: expert consensus recommendations. Aesthetic Plast Surg. 2018;42:498–510. doi: 10.1007/s00266-017-1063-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang DY, Ko K, Lee SH, Lee WK. A comparison of the efficacy and safety between hyaluronic acid and polylactic acid filler injection in penile augmentation: a multicenter, patient/evaluator-blinded, randomized trial. J Sex Med. 2019;16:577–85. doi: 10.1016/j.jsxm.2019.01.310. [DOI] [PubMed] [Google Scholar]
- 10.Friedman PM, Mafong EA, Kauvar AN, Geronemus RG. Safety data of injectable nonanimal stabilized hyaluronic acid gel for soft tissue augmentation. Dermatol Surg. 2002;28:491–4. doi: 10.1046/j.1524-4725.2002.01251.x. [DOI] [PubMed] [Google Scholar]
- 11.Ahn ST, Il Kwak T, Park KS, Kim JJ, Moon DG. Complications of glans penis augmentation. Int J Impot Res. 2019;31:245–55. doi: 10.1038/s41443-018-0097-4. [DOI] [PubMed] [Google Scholar]
- 12.Jeong HG, Ahn ST, Kim JW, Seo KK, Lee DS, et al. Practice patterns among Korean urologists for glans penis augmentation using hyaluronic acid filler in the management of premature ejaculation. Sex Med. 2018;6:297–301. doi: 10.1016/j.esxm.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moon du G, Kwak TI, Kim JJ. Glans penis augmentation using hyaluronic acid gel as an injectable filler. World J Mens Health. 2015;33:50–61. doi: 10.5534/wjmh.2015.33.2.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kwak TI, Jin MH, Kim JJ, Moon DG. Long-term effects of glans penis augmentation using injectable hyaluronic acid gel for premature ejaculation. Int J Impot Res. 2008;20:425–8. doi: 10.1038/ijir.2008.26. [DOI] [PubMed] [Google Scholar]
- 15.Kim JJ, Kwak TI, Jeon BG, Cheon J, Moon DG. Effects of glans penis augmentation using hyaluronic acid gel for premature ejaculation. Int J Impot Res. 2004;16:547–51. doi: 10.1038/sj.ijir.3901226. [DOI] [PubMed] [Google Scholar]
- 16.Daines SM, Williams EF. Complications associated with injectable soft-tissue fillers: a 5-year retrospective review. JAMA Facial Plast Surg. 2013;15:226–31. doi: 10.1001/jamafacial.2013.798. [DOI] [PubMed] [Google Scholar]
- 17.Fukuda H, Endo H, Katsuzaki J, Mukai H. Development of nodules on the glans penis due to hyaluronic acid filler injection. Eur J Dermatol. 2016;26:416–7. doi: 10.1684/ejd.2015.2600. [DOI] [PubMed] [Google Scholar]
- 18.Weber GC, Buhren BA, Schrumpf H, Wohlrab J, Gerber PA. Clinical applications of hyaluronidase. Adv Exp Med Biol. 2019;1148:255–77. doi: 10.1007/978-981-13-7709-9_12. [DOI] [PubMed] [Google Scholar]
- 19.Landau M. Hyaluronidase caveats in treating filler complications. Dermatol Surg. 2015;41(Suppl 1):S347–53. doi: 10.1097/DSS.0000000000000555. [DOI] [PubMed] [Google Scholar]
- 20.Ferneini EM, Beauvais D, Aronin SI. An overview of infections associated with soft tissue facial fillers: identification, prevention, and treatment. J Oral Maxillofac Surg. 2017;75:160–6. doi: 10.1016/j.joms.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 21.Kim JJ, Kwak TI, Jeon BG, Cheon J, Moon DG. Human glans penis augmentation using injectable hyaluronic acid gel. Int J Impot Res. 2003;15:439–43. doi: 10.1038/sj.ijir.3901044. [DOI] [PubMed] [Google Scholar]
- 22.Cox SE, Adigun CG. Complications of injectable fillers and neurotoxins. Dermatol Ther. 2011;24:524–36. doi: 10.1111/j.1529-8019.2012.01455.x. [DOI] [PubMed] [Google Scholar]
- 23.Abdallah H, Abdelnasser T, Hosny H, Selim O, Al-Ahwany A, et al. Treatment of premature ejaculation by glans penis augmentation using hyaluronic acid gel: a pilot study. Andrologia. 2012;44(Suppl 1):650–3. doi: 10.1111/j.1439-0272.2011.01244.x. [DOI] [PubMed] [Google Scholar]


