Purpose of review
Insight into body composition is of great value in the ICU. Bioelectric impedance analysis (BIA) is the most applicable bedside technique. However, bioimpedance has not been validated in the critically ill, and the interpretation of the measurements poses challenges. This review discusses the potential clinical applications of BIA and explores caveats and solutions to its use in the intensive care setting.
Recent findings
A correlation is repeatedly found between raw impedance parameters, fluid ratios, overhydration, and adverse outcome of critical illness. However, cut-off and reference values remain elusive. Experience with BIA-guided fluid management in the ICU is limited. BIA-derived muscle mass appears a promising biomarker for sarcopenia, correlating well with CT-analysis. Body cell mass and fat-free mass provide potential use in estimation of metabolic rate, protein requirements and pharmacokinetics. Several methods of reducing bias in BIA parameters in critical illness require validation.
Summary
There are currently too many uncertainties and discrepancies regarding interpretation of bioimpedance in critical illness, to justify therapeutic consequences. However, there are several promising areas of research, concerning some of the most urgent clinical problems in intensive care, emphasizing the need to evaluate further the use and interpretation of bioimpedance in the intensive care setting.
Keywords: bioelectric impedance, bioimpedance, body composition, critical illness, phase angle
INTRODUCTION
Body composition describes the relative contribution of fat, muscle, bone and water to an individual's body volume. In the ICU, real-time knowledge of body composition is advantageous to the individualization and optimization of fluid balances, nutrition regimes and medication dosing. Several body composition techniques are available, based on assumptions of weight (hydrostatic weighing), water content (isotope dilution), volume (air displacement plethysmography), energy attenuation (Dual-Energy X-Ray Absorptiometry; DXA), and imaging techniques like computer tomography (CT) and MRI. Although extensively validated, all techniques have limitations when applied during critical illness, because of costs, impracticality or radiation exposure.
Bioelectric impedance analysis (BIA) is quick, noninvasive and relatively inexpensive, making it ideal for bedside use. However, BIA assumes static ratios, most notably a fixed hydration of tissues, which often do not apply to critically ill patients, making interpretation less straightforward. Nevertheless, it is worth exploring potential applications, as BIA currently seems the most feasible body composition measurement technique in the ICU.
Angles for future research will be indicated throughout this manuscript with an asterix (∗) and are summarized in Table 1.
Table 1.
Suggestions for future research angles concerning bioelectric impedance analysis in critical care
| Subject | Research angle |
| Internal validity | Influence of overhydration and rapid hydration shifts on BIA measurements |
| Influence of overhydration and rapid hydration shifts on predictive value of BIA parameters | |
| Influence of body temperature on BIA measurements | |
| Influence of osmotic shifts on BIA measurements | |
| External validity | Reference values for BIA measurements in (subgroups of) critically ill patients |
| Cut-off values for outcome predictive qualities of BIA measurements in (subgroups of) critically ill patients | |
| Validation of overhydration adjustment of derived parameters in (subgroups of) critically ill patients | |
| Safety | Possible interference of BIA electrical current with electrical implants other than internal ICDs |
| Clinical use | Development and validation of predictive scoring systems including raw BIA parameters for (subgroups of) critically ill patients |
| Assessment of predictive qualities of BIA measurements for malnutrition | |
| Development and validation of BIA-derived metabolic rate equations with gold-standard methods | |
| External validation of method to predict glomerular filtration rate based on BIA-derived body cell mass (BIA-eGFR) | |
| Pharmacokinetic models using BIA-eGFR and effect on outcome parameters | |
| Pharmacokinetic models using BIA-derived body composition and effect on outcome parameters | |
| Development and validation of equation for protein dosing to BIA-FFM and effect on outcome parameters | |
| Exploring options to calculate derived BIA parameters omitting body weight and possibly height | |
| Effect of BIVA/BIA-guided fluid management on ICU patient-centered outcomes |
BIA, bioelectric impedance analysis; BIVA, bioelectrical impedance vector analysis; FFM, fat-free mass; ICD, implantable cardioverter defibrillator.
Box 1.

no caption available
PRINCIPLES OF BIOIMPEDANCE ANALYSIS
Impedance is the vector analysis of resistance, the opposition to flow of a current, and reactance, the opposition to a current change because of a material's capacitance. When an electrical current is sent through the body, tissues present varying resistance levels. Electrolyte-rich body water is highly conductive; therefore, muscles, having a higher water content, will encounter less resistance than relatively anhydrous tissues, such as fat. Conversely, reactance increases proportionally to cell numbers and their integrity, because of membrane capacitance.
Single-frequency BIA devices (SF-BIA) use a single frequency (usually 50 kHz) to measure impedance. However, low-frequency currents will not penetrate cell membranes, and thus will only measure extracellular water (ECW) impedance. Total body water (TBW) is then estimated through proportional equations. High-frequency currents will go through cells. This impedance reflects combined ICW and ECW : TBW (Fig. 1).
FIGURE 1.
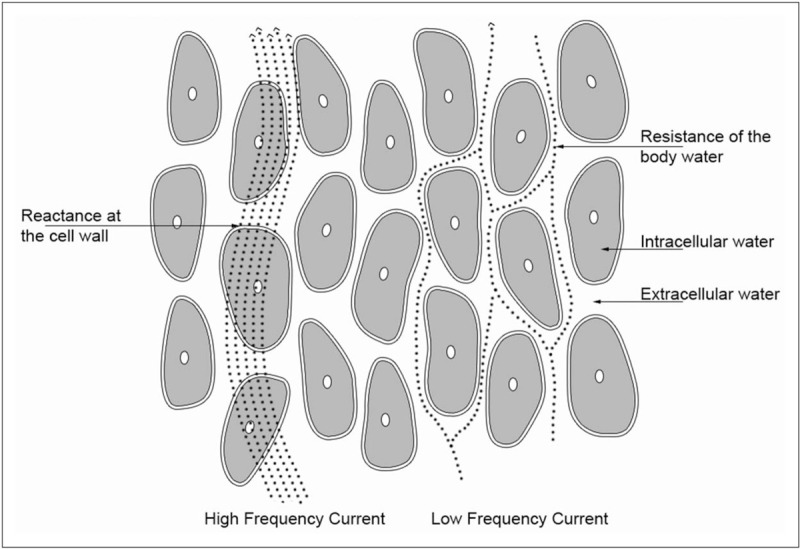
Low-frequency currents will not penetrate cell membranes, and as such will measure extracellular water impedance. High-frequency currents will go through cells, at which point the impedance reflects total body water (TBW).
Multifrequency BIA devices (MF-BIA), therefore, provide a more direct portrayal of water compartments, making them more reliable in case of altered hydration status or electrolyte imbalances. Bioimpedance spectroscopy (BIS) applies a more extensive frequency range than MF-BIA. The increase in information obtained from BIS potentially improves predictive power. However, it still requires extrapolation based on population references. Superiority of BIS to the SF-BIA and MF-BIA techniques has not been proven in nonhealthy populations [1–3,4▪].
The phase angle (PhA) shows the relationship between reactance and resistance (Fig. 2).
FIGURE 2.
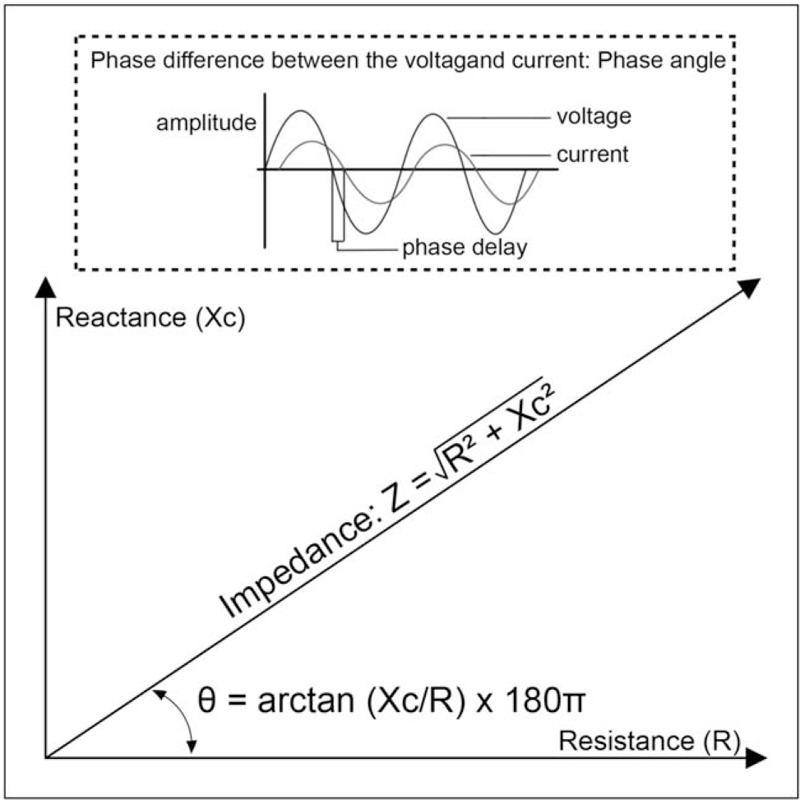
When an electric current passes a cell membrane, reactance causes a time delay, creating a phase shift between voltage and current. The phase angle describes this difference between the voltage and the current. A high-phase angle is, therefore, consistent with large quantities of intact cell membranes and body cell mass.
The greater the number of cell membranes the signal has to pass through, the greater the reactance, and therefore, the PhA. Thus, a large PhA is consistent with a large body cell mass (BCM) relative to ECW, as seen in healthy individuals, whereas ICU patients tend to have a lower PhA. A PhA greater than 6 is assumed normal in health, although PhA varies with sex (men↑) and age (↓because of loss of fat-free mass; FFM), and should ideally be related to a reference population, or converted to standardized PhA (SPhA) before comparing across populations [5,6]. PhA measured at 50 kHz is most frequently used, and most reference data are available for this frequency, as this is the frequency at which both resistance and maximum reactance are best measured [7,8].
Bio-electrical impedance vector analysis (BIVA) represents impedance as a vector of reactance and resistance in an x--y plot referring to reference population's tolerance ellipses (Fig. 3).
FIGURE 3.

Bioelectric impedance vector analysis relates the length and direction of the phase angle to that of a reference population, enabling a visual interpretation of the clinical relevance of the raw bioelectric impedance analysis values.
BIVA allows simultaneous interpretation of direction (phase) and length of the impedance vector; through which changes in tissue hydration and BCM can be appreciated, independent of regression equations, or body water.
DERIVED PARAMETERS
Reactance, resistance, impedance and PhA, are often referred to as ‘raw’ BIA parameters, that is, not reliant upon empirical modeling. BIA defines the water volumes using impedance and body height, upon which other body composition parameters are based. Earlier BIA devices regarded the body as one cylinder and extrapolated impedance measured on one side of the body. However, this simplification overlooks possible asymmetry and the proportional difference between the trunk and the limbs. Segmental BIA (SM-BIA) devices consider the body as five separate cylinders and use electrodes on all limbs, improving accuracy (Fig. 4).
FIGURE 4.
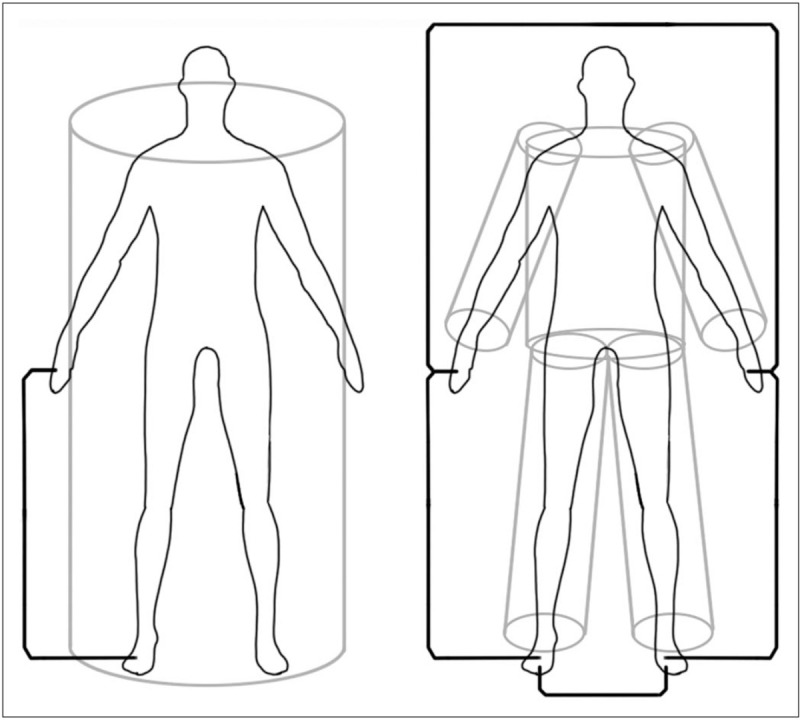
Earlier bioelectric impedance analysis devices regarded the body as one cylinder, calculating body water volumes based on whole-body impedance and body height. Segmental BIA devices consider the body as five separate cylinders and use electrodes on all limbs, improving accuracy. BIA, bioelectric impedance analysis.
Various body composition parameters are derived from thereon, using regression analyses with multiple variables obtained through reference measurements. Figure 5 provides an overview of the relationship between several frequently used parameters. SM-BIA can provide additional values, such as the appendicular skeletal muscle mass (ASMM), the sum of the four limbs’ muscle masses.
FIGURE 5.
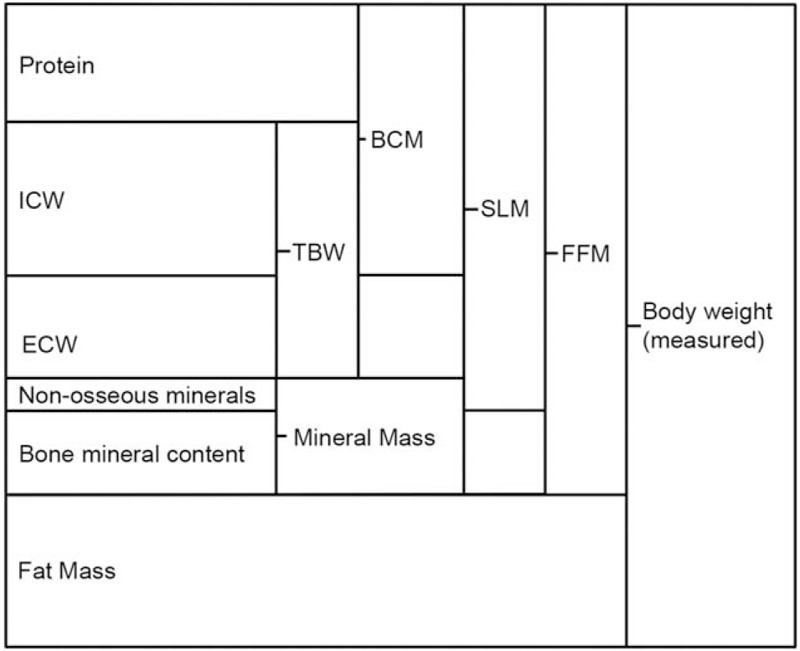
Overview of the relationship between several frequently used derived body composition parameters, based on a multicompartment body composition model. Definitions may vary slightly between sources and device manufacturers.
OUTCOME PREDICTION WITH BIOELECTRIC IMPEDANCE ANALYSIS
Several raw and BIA-derived body composition parameters have been validated as mortality and morbidity predictors in various patient groups and are now being researched as predictors of critical illness outcome [9,10].
Raw parameters
Diminished cell count, membrane integrity and altered hydration status in critical illness can lead to changes in reactance and resistance, thereby decreasing PhA compared with healthy individuals [11,12]. Decreased PhA at ICU admission has been associated with hospital, 28-day, 90-day and 12-month mortality [6,13–16]. Concordantly, PhA improved over the first 5 days of ICU stay in ICU survivors, while decreasing significantly in nonsurvivors [17]. Furthermore, negative correlations have been observed between admission PhA and the length of ward stay, ICU stay and hospital stay, mechanical ventilation duration the APACHE-II score, and recently with the severity of disease of coronavirus disease 2019 (COVID-19) [15,16,18▪–20▪].
However, the cut-off values for the predictive value of PhA vary across these studies∗. The heterogeneity of the ICU populations studied might in part explain these discrepancies. A study comparing sepsis patients with other critically ill patients found that PhA was negatively correlated with the APACHE-II score only in the nonsepsis group [21]. Additionally, in addition to the acute changes because of the current illness, PhA inherently also reflects poor underlying health, muscle wasting and frailty, which are independently associated with outcome.
One study using Segmental Multifrequency BIA (SMMF-BIA) found that impedance, reactance and PhA showed more predictive power for mortality than the SAPS, APACHE-II and SOFA severity scoring systems. Similarly, the landmark Phase Angle Project showed that a combined multivariable score improved the discriminative power in predicting mortality, compared with PhA alone [22]∗.
Hydration parameters
Overhydration in ICU patients is positively correlated with adverse outcomes but current methods to assess volume status [in-bed weighing, cumulative fluid balance (CFB), central venous pressure] have their limitations. Marked BIVA-OH on the first 5 days after ICU admission was shown in ICU and 60-day nonsurvivors [19▪,23,24]. Notably, BIVA predicted mortality better than CFB [23].
Fluid distribution can also be assessed by BIA-derived ECW/TBW ratio. A healthy ECW/TBW ratio varies slightly between sources and device manufacturers but ranges from 0.36 to 0.40. An ECW/TBW ratio of more than 0.40 is considered indicative of overhydration of the extracellular compartment∗. ECW/TBW-ratio is higher among ICU nonsurvivors and correlates with a longer mechanical ventilation duration [25]. Slobod et al. found that a SF-BIA ECW/TBW-ratio greater than 0.39 on ICU-day 1, associated with an increased number of ventilation days, independent of the APACHE-II score [26▪]. In CRRT ICU patients, a cut-off for SMMF-BIA ECW/TBW-ratio of 0.413 predicted 28-day mortality, with 71.4% sensitivity and 70.6% specificity [27].
On the basis of the assumption that excess volume accumulates primarily as ECW, the quantity of overhydration can be calculated as the difference between expected ECW, based on the euvolemic ECW/TBW ratio, and the measured ECW [28,29]. On ICU days 1 and 3, BIS-OH (>1l) associated significantly with hospital mortality in 140 ICU patients with 23 nonsurvivors. Day 3 volume status correlated with the duration of ventilation and ICU stay. More ICU-free and ventilator-free days were observed among patients with normal hydration status on day 3 (OH <1 to 1 l) [30▪]. We showed increased SMMF-BIA-OH, and ECW/TBW ratio were associated with mortality in COVID-19 [20▪].
Muscle mass
Determining muscle mass is essential in distinguishing the sarcopenic, from the nonsarcopenic obese, as the former are at higher risk of adverse outcome in the ICU. Furthermore, rapid wasting of muscle mass is a major clinical conundrum, as it is a strong independent predictor for morbidity, mortality, physical functioning and quality of life. PhA is often considered a proxy for LBM. Indeed, two studies found that low BIA/BIS-PhA corresponded to low CT- muscle mass (CT-MM) and muscle density in the critically ill [31▪▪,32▪▪]. Additionally, BIA provides several derived muscle parameters, including FFM, soft lean mass (SLM), LBM, SMM, SMM index (SMI) and segmental values. Two groups studied agreement between CT-MM and BIA-SMM in the ICU. One used the SMM automatically generated by the SMMF-BIA software, and found a high correlation, regardless of patients’ sex, or edema status [33▪]. Another group calculated SMM, ASMM and total muscle mass based on raw SF-BIA measurements, using three different equations, and found that although the BIA and CT measurements correlated significantly, the agreement was low, with increasing overestimation of muscle mass by BIA at higher CT-MM. However, BIA did correctly identify patients with low CT-MM [31▪▪]. Therefore, BIA might be clinically useful to identify sarcopenic patients at risk for adverse outcome. However, there was a time difference between the BIA and CT evaluation in these studies, potentially inducing bias. Furthermore, increased muscle mass in ICU patients should not be interpreted as muscle mass of good quality, as intramuscular edema will be classified as muscle mass by both BIA and CT analysis. However, a recent pilot-study comparing CT-MM at ICU admission and BIS-FFM adjusted for overhydration, using an algorithm developed for dialysis patients, found significant correlations and good agreements between the two techniques [32▪▪]∗. The unadjusted BIS-FFM correlated with CT-MM but performed poorly in classifying muscularity status [32▪▪].
NUTRITION MANAGEMENT
Critically ill patients are at increased risk of malnutrition. Several BIA parameters can potentially provide information on nutrition status and requirements.
Body cell mass
BCM is the metabolically active part of FFM, in contrast to bone and ECW. As such, a decrease of BCM resulting from critical illness is a marker for malnutrition. Logically, increased ECW is associated with a lower BCM/FFM-ratio. A study comparing BIA measurements before and after hemodialysis in AKI patients (mean weight loss 3.8 kg), suggested hydration shifts have little effect on the BCM measurement, theoretically making it more reliable in critically ill patients [34,35]∗.
Raw parameters
PhA inherently reflects BCM. In 89 ICU patients, a PhA less than less than 5.5° showed an accuracy of 79% in identifying patients at high nutrition risk (NUTRIC score ≥5) [19▪]. In renal replacement therapy patients, a PhA cut-off of 4.6° has been shown to predict malnutrition, defined by protein--energy wasting [36,37]. A study comparing the accuracy of BIVA, versus the definition according to ESPEN in hospitalized patients, in predicting malnutrition, found that BIVA might be the superior method [38].
Fat-free mass
Assessment of muscularity by BIA is recommended by the Global Leadership Initiative on Malnutrition (GLIM) [39]. A prospective study among 60 ventilated ICU patients found that a cumulative energy-deficit during ICU stay was independently associated with loss of BIS-FFM between inclusion and ICU discharge, as well as with ICU-acquired weakness [40▪▪]. In a retrospective post hoc analysis, including this study, these associations disappeared [41▪]. However, raw parameters remained related to muscle weakness [41▪]∗.
FFM is closely related to energy expenditure, and some BIA devices offer options to estimate basal metabolic rate (BMR), using FFM-based equations (e.g. Cunningham, or Katch--McArdle). However, based upon derived FFM, these calculations are subject to caveats and have proven to be inferior to indirect calorimetry in several populations, albeit still more accurate than weight-based equations [42,43].
Potentially, BIA-FFM could facilitate targeted protein dosing. Protein targets are usually set to measured actual weight or calculated FFM∗. However, these methods do not incorporate changes in body composition and weight gain because of overhydration, as such masking the decrease of FFM during ICU stay.
FLUID MANAGEMENT
BIA is commonly used in dialysis patients to guide fluid management by calculating dry weight goals [11,44]. Likewise, in critical illness PhA, ECW/TBW ratio and overhydration could be used to monitor the effect of fluid management strategies. A prospective, clinician-blinded study was conducted to assess the feasibility and validity of BIVA as a measure of hydration in critically ill patients. The study showed that clinicians blinded to the BIVA results, achieved a mean CFB that was concordant with the prior BIVA classification (i.e. positive for patients’ BIVA classified as dehydrated, negative for overhydrated patients and neutral for normally hydrated patients), proving feasibility [45]. Moreover, directional BIVA changes correlated with directional changes in fluid balance. However, the study showed that vector length increased in parallel with 2.4-l fluid loss, suggesting BIVA might be insensitive to smaller changes [45]. The effect of BIVA/BIA-guided fluid management on patient-centered outcomes has not yet been researched∗.
GLOMERULAR FILTRATION RATE AND PHARMACOKINETICS
Adequate dosing of renally excreted drugs is challenging in critically ill patients because of changes in kidney function. Most equations to estimate glomerular filtration rate are based on serum creatinine measurement. However, significant limitations arise when these formulas are applied to patients with altered body composition, like low muscle mass [9,10–13]. A Dutch group recently developed and validated a formula to predict creatinine/urea clearance based on 24 h urine collection (currently the gold-standard in ICU) using serum creatinine and MF-BIA-BCM and ECW/TBW ratio, with good results [46▪▪]∗.
BIA also provides interesting theoretical ways for pharmacokinetic characterization and medication dosing through real-time appreciation of the changing body composition and volumes of distribution [47]. However, no recent attempts for predictive pharmacokinetic models using BIA in the ICU have been published∗.
CAVEATS
One main drawback of BIA is the incorporation of reference population values, for all but the raw parameters, which might not apply to the individual patient or population. Although they are validated against standard methods (usually MRI and DXA), the exact equations used by BIA software are rarely released by manufacturers, impairing judgment of applicability [48]∗. Several other caveats impair routine use of BIA in the ICU, such as use of inexact input parameters, the lack of ICU reference and cut-off values, and the possible bias introduced by a rapidly changing clinical status. Evidence regarding other considerations to use and interpretation of BIA in the ICU setting are summarized in Table 2.
Table 2.
Caveats to the use and interpretation of bioelectric impedance analysis with potential clinical relevance to the ICU setting∗
| Caveats∗ | Evidence |
| Input parameters, such as body height and weight are difficult to measure accurately in the ICU setting | Proxy measurements, such as ulna length, can be used to estimate height [40▪▪]. |
| Ideal body weight (IBW) cannot replace measured body weight as BIA input parameter [49]. | |
| The Biasioli equation to calculate total body weight is based upon height but not weight and can be used to avoid the need for weighing [9,50▪]. | |
| BIA is not validated in patients undergoing large and swift hydration shifts | Changes in TBW determine changes in phase angle (PhA) during ICU days 1–3, suggesting that overhydration (OH) significantly influences PhA [50▪]. |
| BIA might be most reliable at ICU admission (before fluid resuscitation) or after ICU discharge when hydration status has stabilized [14]. | |
| Altered BIA raw parameters because of hydration shifts do not devaluate their prognostic value [50▪]. | |
| Overhydration distorts the normal distribution of water in the intracellular and extracellular space that is used to obtain derived BIA parameters and BIVA | A decline in PhA is related to the hydration score (TBW/FFM × 100%), whereas body cell mass (BCM) and muscle mass (MM) decrease, suggesting that OH is mainly related to the extracellular compartment [50▪]. |
| Decrease of MM might be underestimated, as in case of muscle edema, FFM estimates might overestimate MM, as a constant FFM hydration of 0.73 is usually assumed [33▪,41▪,51]. This is likely less problematic with (multifrequency) MF-BIA or BIS, where TBW can be measured [4▪]. | |
| Interstitial edema is interpreted by BIVA as a state of OH, even if there is a state of relative intravascular hypovolemia [24]. | |
| Derived values might be recalculated to a normalized ECW/TBW ratio, analogous to dialysis BIA software [20▪]. | |
| Ascites, pleural effusion and urine retention theoretically influence BIA measurements | Segmental BIA can distinguish apparent trunk OH because of peritoneal dialysate, without influencing the extremities’ measurements [52]. |
| In cirrhosis patients, PhA is positively correlated with CT-derived MM, irrespective of ascites’ presence [53]. | |
| Changing tissue electrolyte concentrations might influence raw BIA parameters | In chronic kidney disease patients, a 20% increase in Na+ as measured by 23Na-MRI, leads BIS to overestimate ECW by 1.2–2.4 l because of lower extracellular resistance [54]. |
| Fever might influence BIA measurements by reducing ECW | In ambulant Influenza persons, individuals (T ≥ 37.1 °C) show a tendency toward greater reactance and PhA than afebrile individuals [55]. |
| BIA could interfere with electrical implants, leading manufacturers to advise against use whenever one is present | Multiple studies show that BIA could be safely performed in patients with ICDs [56,57▪,58,59]. The same has not been researched for other electrical implants. |
BIA, bioelectric impedance analysis; BIVA, bioelectrical impedance vector analysis; ECW, extracellular water; FFM, fat-free mass; ICD, implantable cardioverter defibrillator; OH, overhydration.
CONCLUSION
There are several promising areas of BIA research concerning some of the most urgent clinical problems in intensive care. A correlation is repeatedly found between raw impedance parameter, fluid ratios, overhydration and adverse outcomes in critical illness. BIA-derived muscle mass appears a promising biomarker for sarcopenia, as it correlates well with CT-analysis. BCM and fat-free mass provide potential use in estimation of metabolic rate, glomerular filtration rate, protein needs and pharmacokinetics. Contrastingly, experience with BIA-guided fluid management is still limited and suggested methods of reducing bias in BIA-measurements in the critically ill require validation. There are currently too many uncertainties and discrepancies regarding the interpretation of BIA measurements in critical illness to justify large therapeutic consequences, emphasizing the need for further evaluation of the use and interpretation of bioelectric impedance in the ICU setting.
Acknowledgements
We thank C.S. Redshaw for the creation of all figures shown in this article.
Financial support and sponsorship
None.
Conflicts of interest
H.P.F.X.M. has no conflicts of interest to disclose. A.R.H.V.Z. reported that he had received honoraria for advisory board meetings, lectures and travel expenses from Abbott, Amomed, Baxter, Cardinal Health, Danone-Nutricia, DIM-3, Fresenius Kabi, Lyric, Mermaid and Nestle-Novartis. Inclusion fees for patients in nutrition trials were paid to the local ICU research foundation.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Seoane F, Abtahi S, Abtahi F, et al. Mean expected error in prediction of total body water: a true accuracy comparison between bioimpedance spectroscopy and single frequency regression equations. Biomed Res Int 2015; 2015:656323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kyle UG, Bosaeus I, De Lorenzo AD, et al. Bioelectrical impedance analysis--part I: review of principles and methods. Clin Nutr 2004; 23:1226–1243. [DOI] [PubMed] [Google Scholar]
- 3.Martinoli R, Mohamed EI, Maiolo C, et al. Total body water estimation using bioelectrical impedance: a meta-analysis of the data available in the literature. Acta Diabetol 2003; 40: Suppl 1: S203–S206. [DOI] [PubMed] [Google Scholar]
- 4▪.Mundi MS, Patel JJ, Martindale R. Body composition technology: implications for the ICU. Nutr Clin Pract 2019; 34:48–58. [DOI] [PubMed] [Google Scholar]; A review of clinical relevance, discussing the most commonly available clinical technology for assessment of body composition, including data from trials in critically ill patients highlighting the benefits and weaknesses of each modality.
- 5.Barbosa-Silva MC, Barros AJ, Wang J, et al. Bioelectrical impedance analysis: population reference values for phase angle by age and sex. Am J Clin Nutr 2005; 82:49–52. [DOI] [PubMed] [Google Scholar]
- 6.Thibault R, Makhlouf AM, Mulliez A, et al. Phase Angle Project Investigators. Fat-free mass at admission predicts 28-day mortality in intensive care unit patients: the international prospective observational study Phase Angle Project. Intensive Care Med 2016; 42:1445–1453. [DOI] [PubMed] [Google Scholar]
- 7.Kumar S, Dutt A, Hemraj S, et al. Phase angle measurement in healthy human subjects through bio-impedance analysis. Iran J Basic Med Sci 2012; 15:1180–1184. [PMC free article] [PubMed] [Google Scholar]
- 8.Hui D, Dev R, Pimental L, et al. Association between multifrequency phase angle and survival in patients with advanced cancer. J Pain Symptom Manage 2017; 53:571–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lukaski HC, Kyle UG, Kondrup J. Assessment of adult malnutrition and prognosis with bioelectrical impedance analysis: phase angle and impedance ratio. Curr Opin Clin Nutr Metab Care 2017; 20:330–339. [DOI] [PubMed] [Google Scholar]
- 10.Kyle UG, Bosaeus I, De Lorenzo AD, et al. Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr 2004; 23:1430–1453. [DOI] [PubMed] [Google Scholar]
- 11.Malbrain ML, Huygh J, Dabrowski W, et al. The use of bio-electrical impedance analysis (BIA) to guide fluid management, resuscitation and deresuscitation in critically ill patients: a bench-to-bedside review. Anaesthesiol Intensive Ther 2014; 46:381–391. [DOI] [PubMed] [Google Scholar]
- 12.Berbigier MC, Pasinato VF, Rubin BA, et al. Bioelectrical impedance phase angle in septic patients admitted to intensive care units. Rev Bras Ter Intensiva 2013; 25:25–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuchnia A, Earthman C, Teigen L, et al. Evaluation of bioelectrical impedance analysis in critically ill patients: results of a multicenter prospective study. JPEN J Parenter Enteral Nutr 2017; 41:1131–1138. [DOI] [PubMed] [Google Scholar]
- 14.Stapel SN, Looijaard WGPM, Dekker IM, et al. Bioelectrical impedance analysis-derived phase angle at admission as a predictor of 90-day mortality in intensive care patients. Eur J Clin Nutr 2018; 72:1019–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.do Amaral Paes TC, de Oliveira KCC, de Carvalho PP, Peres WAF. Phase angle assessment in critically ill cancer patients: relationship with the nutritional status, prognostic factors and death. J Crit Care 2018; 44:430–435. [DOI] [PubMed] [Google Scholar]
- 16.Buter H, Veenstra JA, Koopmans M, Boerma CE. Phase angle is related to outcome after ICU admission; an observational study. Clin Nutr ESPEN 2018; 23:61–66. [DOI] [PubMed] [Google Scholar]
- 17.Ellegard LH, Petersen P, Öhrn L, Bosaeus I. Longitudinal changes in phase angle by bioimpedance in intensive care patients differ between survivors and nonsurvivors. Clin Nutr ESPEN 2018; 24:170–172. [DOI] [PubMed] [Google Scholar]
- 18▪.Jansen AK, Gattermann T, da Silva FJ, et al. Low standardized phase angle predicts prolonged hospitalization in critically ill patients. Clin Nutr ESPEN 2019; 34:68–72. [DOI] [PubMed] [Google Scholar]; Methodologically thorough longitudinal, dual-center, prospective study evaluating the predictive validity of standardized Pha for adverse outcome critically ill patients.
- 19▪.Razzera EL, Marcadenti A, Rovedder SW, et al. Parameters of bioelectrical impedance are good predictors of nutrition risk, length of stay, and mortality in critically ill patients: a prospective cohort study. JPEN J Parenter Enteral Nutr 2020; 44:849–854. [DOI] [PubMed] [Google Scholar]; One of the first prospective studies evaluating the predictive validity of standardized phase angle for malnutrition and prolongued stay in critically ill patients.
- 20▪.Moonen HPFX, van Zanten FJL, Driessen L, et al. Association of bioelectric impedance analysis body composition and disease severity in COVID-19 hospital ward and ICU patients: the BIAC-19 study. Clin Nutr 2020; 40:2328–2336. [DOI] [PMC free article] [PubMed] [Google Scholar]; One of the first studies evaluating the association between BIA-derived body composition and disease severity in COVID-19, showing the relevance of PhA as prediction marker for this population.
- 21.da Silva TK, Berbigier MC, Rubin BA, et al. Phase angle as a prognostic marker in patients with critical illness. Nutr Clin Pract 2015; 30:261–265. [DOI] [PubMed] [Google Scholar]
- 22.Lee YH, Lee JD, Kang DR, et al. Bioelectrical impedance analysis values as markers to predict severity in critically ill patients. J Crit Care 2017; 40:103–107. [DOI] [PubMed] [Google Scholar]
- 23.Samoni S, Vigo V, Reséndiz LI, et al. Impact of hyperhydration on the mortality risk in critically ill patients admitted in intensive care units: comparison between bioelectrical impedance vector analysis and cumulative fluid balance recording. Crit Care 2016; 20:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Basso F, Berdin G, Virzì GM, et al. Fluid management in the intensive care unit: bioelectrical impedance vector analysis as a tool to assess hydration status and optimal fluid balance in critically ill patients. Blood Purif 2013; 36:192–199. [DOI] [PubMed] [Google Scholar]
- 25.Lee Y, Kwon O, Shin CS, Lee SM. Use of bioelectrical impedance analysis for the assessment of nutritional status in critically ill patients. Clin Nutr Res 2015; 4:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26▪.Slobod D, Yao H, Mardini J, et al. Bioimpedance-measured volume overload predicts longer duration of mechanical ventilation in intensive care unit patients. Can J Anaesth 2019; 66:1458–1463. [DOI] [PubMed] [Google Scholar]; Prospective study evaluating repeated BIA measurements in critically ill patients; indicating that early volume overload, defined as an increased admission ECW/TBW ratio, is associated with prolonged ventilation time.
- 27.Park KH, Shin JH, Hwang JH, Kim SH. Utility of volume assessment using bioelectrical impedance analysis in critically ill patients receiving continuous renal replacement therapy: a prospective observational study. Korean J Crit Care Med 2017; 32:256–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Myatchin I, Abraham P, Malbrain MLNG. Bio-electrical impedance analysis in critically ill patients: are we ready for prime time? J Clin Monit Comput 2020; 34:401–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lopot F, Nejedlý B, Novotná H, et al. Age-related extracellular to total body water volume ratio (Ecv/TBW)--can it be used for ‘dry weight’ determination in dialysis patients? Application of multifrequency bioimpedance measurement. Int J Artif Organs 2002; 25:762–769. [DOI] [PubMed] [Google Scholar]
- 30▪.Yang SF, Tseng CM, Liu IF, et al. Clinical significance of bioimpedance spectroscopy in critically ill patients. J Intensive Care Med 2019; 34:495–502. [DOI] [PubMed] [Google Scholar]; Prospective observational study assessing predictive value of repeated BIS-derived overhydration and adverse outcome in critically ill patients.
- 31▪▪.Looijaard WGPM, Stapel SN, Dekker IM, et al. Identifying critically ill patients with low muscle mass: agreement between bioelectrical impedance analysis and computed tomography. Clin Nutr 2020; 39:1809–1817. [DOI] [PubMed] [Google Scholar]; The first prospective study comparing BIA-PhA and CT measurements of the muscle compartment. It demonstrates that BIA can identify the same population with low SMA. The correlation between PhA and skeletal muscle density, and the finding that low PhA, as defined by nutritional risk-related cut-off points and mortality-related cut-off points, corresponded to low CT-derived muscle area and CT-derived muscle density are new and provide future research perspectives.
- 32▪▪.Lambell KJ, Earthman CP, Tierney AC, et al. How does muscularity assessed by bedside methods compare to computed tomography muscle area at intensive care unit admission? A pilot prospective cross-sectional study. J Hum Nutr Diet 2020; 34:345–355. [DOI] [PubMed] [Google Scholar]; In this pilot study, a unique BIS-derived FFM variable using an equation that accounts for fluid overload was significantly correlated to CT muscle area and was able to correctly classify all the participants with low CT muscle area at ICU admission.
- 33▪.Kim D, Sun JS, Lee YH, et al. Comparative assessment of skeletal muscle mass using computerized tomography and bioelectrical impedance analysis in critically ill patients. Clin Nutr 2019; 38:2747–2755. [DOI] [PubMed] [Google Scholar]; Retrospective study comparing the SMM automatically generated in their SMMF-BIA device and CT measurement of skeletal muscle area, correcting for edema status.
- 34.Fiaccadori E, Morabito S, Cabassi A, Regolisti G. Body cell mass evaluation in critically ill patients: killing two birds with one stone. Crit Care 2014; 18:139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ismael S, Savalle M, Trivin C, et al. The consequences of sudden fluid shifts on body composition in critically ill patients. Crit Care 2014; 18:R49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leal Escobar G, Osuna Padilla IA, Cano Escobar KB, et al. Phase angle and mid arm circumference as predictors of protein energy wasting in renal replacement therapy patients. Nutr Hosp 2019; 36:633–639. [DOI] [PubMed] [Google Scholar]
- 37.Tan RS, Liang DH, Liu Y, et al. Bioelectrical impedance analysis-derived phase angle predicts protein-energy wasting in maintenance hemodialysis patients. J Ren Nutr 2019; 29:295–301. [DOI] [PubMed] [Google Scholar]
- 38.Dehesa-López E, Martínez-Felix JI, Ruiz-Ramos A, Atilano-Carsi X. Discordance between bioelectrical impedance vector analysis and the new ESPEN definition of malnutrition for the diagnosis of hospital malnutrition. Clin Nutr ESPEN 2017; 18:44–48. [DOI] [PubMed] [Google Scholar]
- 39.Cederholm T, Jensen GL, Correia MITD, et al. GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. J Cachexia Sarcopenia Muscle 2019; 10:207–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40▪▪.Fetterplace K, Beach LJ, MacIsaac C, et al. Associations between nutritional energy delivery, bioimpedance spectroscopy and functional outcomes in survivors of critical illness. J Hum Nutr Diet 2019; 32:702–712. [DOI] [PubMed] [Google Scholar]; Fetterplace et al. prospectively investigate association between cummulative energy deficit, loss of BIS-FFM and relate these to funcional outcomes in ventilated ICU patients, an important, patient-centered outcome.
- 41▪.Baldwin CE, Fetterplace K, Beach L, et al. Early detection of muscle weakness and functional limitations in the critically ill: a retrospective evaluation of bioimpedance spectroscopy. JPEN J Parenter Enteral Nutr 2020; 44:837–848. [DOI] [PubMed] [Google Scholar]; A post hoc analysis of BIS measurements and functional outcomes, comparing data of multiple centers and highlighting the importance of standardization of practise in BIA use, to promote pooling of data and further research in this important area.
- 42.Hashizume N, Tanaka Y, Yoshida M, et al. Resting energy expenditure prediction using bioelectrical impedance analysis in patients with severe motor and intellectual disabilities. Brain Dev 2019; 41:352–358. [DOI] [PubMed] [Google Scholar]
- 43.Zanella PB, Ávila CC, de Souza CG. Estimating resting energy expenditure by different methods as compared with indirect calorimetry for patients with pulmonary hypertension. Nutr Clin Pract 2018; 33:217–223. [DOI] [PubMed] [Google Scholar]
- 44.Tian N, Yang X, Guo Q, et al. Bioimpedance guided fluid management in peritoneal dialysis: a randomized controlled trial. Clin J Am Soc Nephrol 2020; 15:685–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jones SL, Tanaka A, Eastwood GM, et al. Bioelectrical impedance vector analysis in critically ill patients: a prospective, clinician-blinded investigation. Crit Care 2015; 19:290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46▪▪.de Jong LAA, Otten-Helmers AG, Spronk PE, van Kan HJM. Bioelectrical impedance measurements for assessment of kidney function in critically ill patients. Crit Care Med 2019; 47:e984–e992.31609770 [Google Scholar]; De Jong et al. developed an innovative new method of predicting creatinine/urea clearance in critically ill patients based on BIA-derived body composition, which, if externally validated, will be far quicker than the current gold-standard technique based on 24-h urine collection values.
- 47.Zarowitz BJ, Robert S, Mlynarek M, et al. Determination of gentamicin pharmacokinetics by bioelectrical impedance in critically ill adults. J Clin Pharmacol 1993; 33:562–567. [DOI] [PubMed] [Google Scholar]
- 48.Beaudart C, Bruyère O, Geerinck A, et al. Belgian Aging Muscle Society (BAMS). Equation models developed with bioelectric impedance analysis tools to assess muscle mass: A systematic review. Clin Nutr ESPEN 2020; 35:47–62. [DOI] [PubMed] [Google Scholar]
- 49.Dewitte A, Carles P, Joannes-Boyau O, et al. Bioelectrical impedance spectroscopy to estimate fluid balance in critically ill patients. J Clin Monit Comput 2016; 30:227–233. [DOI] [PubMed] [Google Scholar]
- 50▪.Denneman N, Hessels L, Broens B, et al. Fluid balance and phase angle as assessed by bioelectrical impedance analysis in critically ill patients: a multicenter prospective cohort study. Eur J Clin Nutr 2020; 74:1410–1419. [DOI] [PubMed] [Google Scholar]; Important study investigating the controversial influence hydration status on raw BIA, emphasizing the need for a more nuanced interpretation of BIA measurements in the critically ill population.
- 51.Chamney PW, Wabel P, Moissl UM, et al. A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr 2007; 85:80–89. [DOI] [PubMed] [Google Scholar]
- 52.Davenport A. Does peritoneal dialysate affect body composition assessments using multifrequency bioimpedance in peritoneal dialysis patients? Eur J Clin Nutr 2013; 67:223–225. [DOI] [PubMed] [Google Scholar]
- 53.Ruiz-Margáin A, Xie JJ, Román-Calleja BM, et al. Phase angle from bioelectrical impedance for the assessment of sarcopenia in cirrhosis with or without ascites. Clin Gastroenterol Hepatol 2020; Sep 2:S1542-3565(20)31225-8. doi: 10.1016/j.cgh.2020.08.066. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 54.Mitsides N, McHugh D, Swiecicka A, et al. Extracellular resistance is sensitive to tissue sodium status; implications for bioimpedance-derived fluid volume parameters in chronic kidney disease. J Nephrol 2020; 33:119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marini E, Buffa R, Contreras M, et al. Effect of influenza-induced fever on human bioimpedance values. PLoS One 2015; 10:e0125301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Meyer P, Makhlouf AM, Mondouagne Engkolo LP, et al. Safety of bioelectrical impedance analysis in patients equipped with implantable cardioverter defibrillators. JPEN J Parenter Enteral Nutr 2017; 41:981–985. [DOI] [PubMed] [Google Scholar]
- 57▪.Garlini LM, Alves FD, Kochi A, et al. Safety and results of bioelectrical impedance analysis in patients with cardiac implantable electronic devices. Braz J Cardiovasc Surg 2020; 35:169–174. [DOI] [PMC free article] [PubMed] [Google Scholar]; Innovative study design that draws attention to a possible association between osmotic shifts and BIA measurements, not yet previously appreciated.
- 58.Buch E, Bradfield J, Larson T, Horwich T. Effect of bioimpedance body composition analysis on function of implanted cardiac devices. Pacing Clin Electrophysiol 2012; 35:681–684. [DOI] [PubMed] [Google Scholar]
- 59.Chabin X, Taghli-Lamallem O, Mulliez A, et al. Bioimpedance analysis is safe in patients with implanted cardiac electronic devices. Clin Nutr 2019; 38:806–811. [DOI] [PubMed] [Google Scholar]


