Abstract
Objective:
Healthcare system distrust (HCSD) has been linked to poor breast cancer outcomes. Previous HSCD analyses have focused on Black-White disparities; however, focusing only on race ignores the complex set of factors that form identity. We quantified the contributions of race and sexual minority (SM) identity to HCSD among US women who had received breast cancer screening.
Methods:
This cross-sectional study used intersectionality decomposition methods to assess the degree to which racial and SM identity contributed to disparate responses to the validated 9-item HCSD Scale. The sample included online survey participants identifying as a Black or White woman living in the US, with a self-reported abnormal breast cancer screening result in the past 24 months and/or breast cancer diagnosis since 2011.
Results:
Of 649 participants, 49.4% of Black SM women (n = 85) were in the highest HCSD tertile, followed by 37.4% of White SM women (n = 123), 24.4% of Black heterosexual women (n = 156), and 19% of White heterosexual women. Controlling for age, 72% of the disparity in HCSD between Black SM women and White heterosexual women was due to SM status, 23% was due to racial identity, and 3% was due to both racial and SM identity.
Conclusions:
SM identity emerged as the largest driver of HCSD disparities; however, the combined racial and SM disparity persisted. Excluding sexual identity in HCSD studies may miss an important contributor. Interventions designed to increase the HCS's trustworthiness at the provider and system levels should address both racism and homophobia.
Keywords: African Americans, decomposition, intersectionality, Psycho-oncology, sexual and gender minorities, trust
1 ∣. BACKGROUND
Healthcare system distrust (HCSD) is a persistent challenge in breast cancer care in the United States.1 It has been linked to poor outcomes across the breast cancer continuum1 from screening, genetic testing, and counseling2-4 to treatment5,6 and survivorship.6,7 While HCSD is often thought of as a property of individuals, warranted distrust reflects properties of institutions that reinforce racism, homophobia and other forms of discrimination that make those institutions untrustworthy.8 Thus, understanding the characteristics of those at risk of experiencing HCSD is critical to cancer care.
Previous studies on HCSD differences focus on race,8,9 and find that (healthcare system) HCS untrustworthiness is a well-established barrier to care for Blacks compared to Whites 10-13; however, focusing only on racial minority identity ignores the complex set of factors that form identity. For example, previous studies suggest that HCSD among sexual minorities is high,9,14-16 and is often associated with fear of stigmatization due to sexual minority (SM) identity. Racial/ethnic minorities who are also sexual minorities may experience dual marginalization within healthcare due to being at the intersection of racism and homophobia,9 and may be at even greater risk of HCSD than those identifying as either a racial minority or SM.
Examination of the combined contributions of race and sexual identity to beliefs in the HCS’s trustworthiness is largely unexamined overall.1,14 The few studies on mistrust that have focused on both race and sexual identity9,14-16 have not been in breast cancer, where these identities clearly pattern care. Being Black is associated with diagnosis at later stages of breast cancer, longer time between mammograms, and lack of timely follow-up after abnormal mammograms17-19 than Whites, even among those who are insured.20 Being an SM is associated with low rates of screening, less timely screening,21-25 and delays after an abnormal screening.26 However, studies at the intersection of racial and sexual identity show a more complex trend: While a lower percentage of Black SM women use mammography than White SM women, White bisexual women have lower odds of mammography than White heterosexual women while Black bisexual women have higher odds of mammography than Black SM women.27 Disparities in the receipt of care by racial and SM identity may be attributed to the experiences of discrimination that racial or SM groups experience that signal untrustworthiness of the HCS. Our understanding of how identity relates to HCSD ratings in breast cancer is a gap that must be filled in order to address the roots of care disparities.
Both race and sexual identity are markers of differential treatment in society, such that the contributions of each reflect complex historical processes for which they are a proxy measure.28,29 New methods now enable us to assess the extent to which disparities in health outcomes and exposures related to various parts of identity: race, sexual identity, or the intersection of both race and sexual identity.30,31 Applying these new methods, this analysis sought to answer the question: To what extent does being a racial or SM contribute to HCSD among those seeking follow-up care after breast cancer screening?
2 ∣. METHODS
2.1 ∣. Sample
From June 2018 to October 2019, we recruited participants through targeted emails to specific breast cancer interest groups (i.e., Susan Love Research Army, the Pride Study, the Pride Study, the National Lesbian, Gay, Bisexual, Transgender (LGBT) Cancer Network, Living Beyond Breast Cancer), Facebook posts, social media promotion through breast cancer advocates (Ericka Hart), and via personal referrals. Our community partner, the National Organization of Black Lesbians on Aging (ZAMI NOBLA), boosted participation by Black SM women through recruitment at health fairs and churches affirming same gender-loving persons. Participants provided online informed consent prior to accessing the online survey questions.
An initial 2,798 individuals completed the survey's screening questions to determine eligibility, of which 852 were eligible for the survey based on screening questions. Eligibility for the survey included being aged 35 or older, assigned female at birth, currently identifying as a Black or White woman and with a self-reported abnormal clinical breast exam, mammogram, breast magnetic resonance imaging (MRI) , or breast ultrasound result in the past 24 months and/or diagnosed with breast cancer since 2011. Of all those eligible, 851 completed the survey yielding a 99.8% completion rate. Of the 851 women who completed the survey, 123 were excluded from this analysis for the following reasons: 94 women identified as a race other than Black or White and/or did not identify their sexual orientation; and 30 women were eligible based on responses to their screening question but were later deemed ineligible based on survey questions about breast cancer history. Among the 728 women remaining, 79 women did not provide complete information to calculate the HCSD variable. The final analytic sample was 649.
Survey items included self-reported demographics, behavioral questions about delays in care-seeking following breast cancer diagnosis or abnormal screening (results reported in26), and structural and psychosocial barriers to or facilitators of seeking care. The study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (protocol #00007908), and the study conforms to standards outlined in the Declaration of Helsinki and the US Federal Policy for the Protection of Human Subjects. Further details on survey development and recruitment are previously published.26
2.2 ∣. Measures
Intersectional identity: Race and SM status were self-reported. Patients not identifying as Black or White were excluded from analysis. Ethnicity was asked as a separate question. Regardless of ethnicity, all individuals who identified as Black were coded as Black. SM women were classified as those who self-identified as lesbian, gay, queer, bisexual, or same-gender loving, and were coded as SM. Women who identified as Straight/Heterosexual were coded as nonsexual minority (NSM). The sample was analyzed across four intersectional groups: White NSM, White SM, Black NSM, and Black SM women.
Sample characteristics: Participants self-reported current insurance and type of insurance. Experiences of discrimination were measured by the 13-item Intersectional Discrimination Index—Major (InDI-M) scale,32 with higher values representing greater discrimination during experiences with healthcare, housing, employment or interpersonal relationships (Cronbach's a = 0.81 in this sample). Charlson comorbidity score33 was included as a measure of the health of the patient based on the patient's self-reported number of diagnosed comorbid conditions.
Healthcare system trustworthiness: Participants completed the validated 9-item Health Care System Distrust scale34,35 which measures subdomains of: values distrust, which reflects the fidelity, honesty, and belief that the healthcare system will act in the best interest of the patient, and competence distrust, which reflects the perceptions of the healthcare system's ability and knowledge to perform in the expected way.36 Items focus on discrimination by race and insurance, beliefs about unethical experimentation by the HCS, and that the HCS prioritizes making money over healing patients. Item responses were on a 5-point agreement scale (1 = strongly disagree, 5 = strongly agree), with summary score ranges from 9 to 45. The measure has high internal consistency in the current sample, with a Cronbach's a = 0.88 for the overall sample, with scores of 0.86 for White NSM, 0.83 for White SM, 0.87 for Black NSM, and 0.91 for Black SM women subgroups.
2.3 ∣. Analysis
We calculated descriptive statistics on the overall sample, and each of four identity-based subsamples: White NSM women, White SM women, Black NSM women, and Black SM women. For continuous variables mean values across groups were compared with one-way ANOVA. For categorical variables, values across groups were compared with Pearson's chi-squared tests.
To complete the intersectional analysis, we used decomposition methods developed by Jackson and colleagues30,31 to separate out how much race and SM status contributed to HCSD. This method uses a linear regression model to calculate four different metrics1: the joint disparity, or the overall difference between someone who is Black and SM and someone who is White and not an SM2; the referent race disparity, in our case, the contribution that being Black makes to HCSD3; the referent sexual identity disparity, in our case, the contribution that SM status makes to HCSD; and the4 excess intersectional disparity, or the additional contribution that being both Black and SM makes to HCSD, above and beyond the sum of the racial and sexual identity disparity. We calculated the percentage of disparity attributable to specific identities as the percentage of the joint disparity explained by each of the decomposed component (referents and excess intersectional) disparities.
Our linear regression model adjusted only for age due to differential risk for breast cancer by age and that Black women are more likely to have a breast cancer diagnosis at a younger age than White women, and because differences in comorbidities were predicted by age. The decomposition method used is rooted in a causal inference perspective, meaning that additional sociodemographic covariates such as insurance, education, or income would need to be modeled as mediators between intersectional identity and HCSD. Even if we had modeled these factors as mediators, their contributions would still be driven by the intersectional identity exposure, which absorbs their influence. Thus, ultimately, we opted not to include these variables in the decomposition analysis. We also did not include stigma or discrimination because the distrust measure already includes items about discrimination, raising issues of endogeneity. We report these variables only to characterize each subsample.
3 ∣. RESULTS
Six hundred and fourty-nine women responded to the HCSD question and were classified as either Black or White. The mean age across the sample was 55, and the majority of participants had health insurance (Table 1), though SM women and Black women groups all had lower rates of health insurance that White NSM women. Black and White SM women reported the highest experiences of discrimination, followed by Black NSM and White NSM. Black SM reported highest rates of HCSD untrustworthiness, followed by White SM, Black NSM, and then White NSM.
TABLE 1.
Demographics of White or Black sexual minority (SM) or nonsexual minority (NSM) respondents to the healthcare system distrust scale (N = 649)
| Mean (SD) | All N = 649 (100%) |
White NSM n = 285 (43.9%) |
White SM n = 123 (19%) |
Black NSM n = 156 (24%) |
Black SM n = 85 (13.1%) |
p |
|---|---|---|---|---|---|---|
| Agea | 55 (11) | 58 (10) | 54 (12) | 55 (11) | 50 (9.7) | 0.15 |
| College educationb (n, %) | 575 (88.6%) | 266 (93.3%) | 118 (95.9%) | 119 (76.3%) | 72 (84.7%) | <0.001 |
| Annual income >$50,000c (n, %) | 441 (68%) | 228 (80%) | 90 (73.2%) | 80 (51.3%) | 43 (50.6%) | <0.001 |
| Insurancea (n, %) | 626 (96%) | 285 (100%) | 119 (96.8%) | 144 (92.3%) | 78 (91.8%) | <0.001 |
| Experiences of discriminationc (range: 13–34) | 17 (4) | 16 (4) | 19 (5) | 17 (4) | 19 (5) | <0.001 |
| Comorbiditiesa (range: 0–16) | 2 (1) | 2 (1) | 3 (2) | 2 (1) | 2 (1) | <0.001 |
| Distrust scorea (range: 9–45) | 27 (7) | 25 (6) | 29 (6) | 27 (7) | 31 (8) | <0.001 |
Zero observations missing for this variable.
<5% of observations missing for this variable.
<10% of observations missing for this variable.
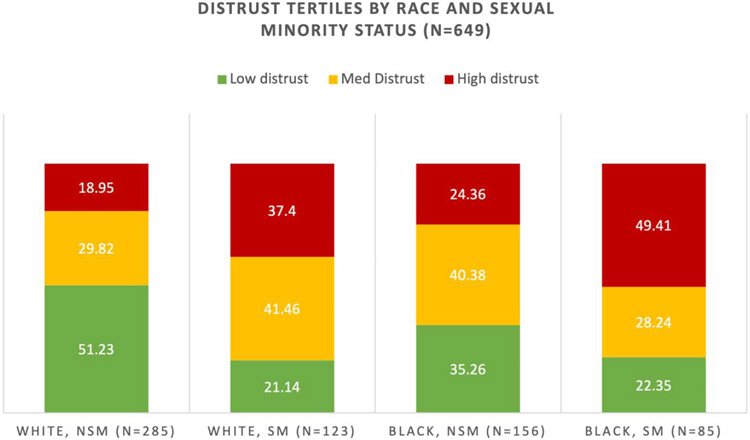
Figure 1 reports high, medium, and low tertiles of distrust by intersectional identity group. Nearly half (49.4%) of Black SM women were in the highest tertile of HCSD, followed by over one-third (37.4) of White SM women, and one-quarter (24.4%) of Black NSM women.
FIGURE 1.
Distrust tertiles by race and sexual minority status for women receiving breast cancer screening or follow-up care; SM, sexual minority; NSM, nonsexual minority
Table 2 shows the contributions of each identity to HCSD. The overall difference in HCSD scores between White NSM and Black SM (joint disparity) was 4.67 (−0.14, 9.48). This value could be decomposed into contributions due to Black race (referent race disparity) of 1.12 (−0.14, 2.38), or SM status (referent sexual identity disparity), 3.40 (2.03, 4.77). Above and beyond being a racial or sexual minority, the additional contribution of being both a racial and sexual minority (excess intersectional disparity) was 0.15 (−2.03, 2.33).
TABLE 2.
Results of healthcare system distrust intersectional decomposition by racial minority and sexual minority identity
| Absolute difference (95% CI) |
Interpretation | Percent of joint disparity |
|
|---|---|---|---|
| Joint disparity | 4.67 (−0.14, 9.48) | Difference in average healthcare system distrust score between Black SMW & White NSMW | -- |
| Referent race disparity | 1.12 (−0.14, 2.38) | Difference in average health system distrust on the basis of race alone | 24% |
| Referent sexual identity disparity | 3.40 (2.03, 4.77) | Difference in average healthcare system distrust score on the basis of sexual minority status alone | 72% |
| Excess intersectional disparity | 0.15 (−2.03, 2.33) | Difference in average healthcare system distrust score on the basis of interaction between race and sexual minority identity | 3% |
The disparity in HCSD, controlling for age, between Black SM women (avg HCSD score = 33.5) and White heterosexual women (avg HCSD score = 28.8) was primarily due to SM status ((1.12/4.7) × 100 = 72.3%). A smaller proportion of the difference was due to racial identity ((3.40/4.7) × 100 = 23.8%). An even smaller proportion was due to the intersection between SM status and racial identity ((0.15/4.7) × 100 = 3.19%).
4 ∣. DISCUSSION
Our results suggest that in a sample of racial and SM women with a history of breast cancer or abnormal breast cancer screening, most of the differences in HCSD was due to being an SM or being a racial minority, but no elevation of distrust due to being at the intersection of a racial and sexual minority. The sexual identity referent disparity was the only disparity measure that was statistically significant. This finding combined with the proportion of the joint disparity that is attributed to differences in SM status suggests that SM identity may be driving the difference in HCSD between Black SM women and White heterosexual women. Even though the excess intersectional disparity is neither statistically significant nor a large proportion of the joint disparity, this simply means that the contributions of race and SM identity are additive rather than multiplicative in determining HCSD. The fact that the combined racial and SM disparity exists at all remains important given the possible impact of HCSD on health behaviors and outcomes. These findings suggest that excluding sexual identity in studies of HCSD may miss an important contributor to HCSD that has not been previously captured.
Based on our study findings in a sample of racial and sexual minorities, sexual identity had a greater influence than racial identity on reports of low HCS trustworthiness. These findings may be related to the higher rates of discrimination reported by White SM women than any other group in our sample. There may be several reasons for this finding. White SM women in this study were older and had more comorbidities, which may have resulted in greater need for engagement with the HCS than other groups, thus more opportunities to experience discrimination by the HCS. Another explanation based on previous studies is that Whites may be more likely to perceive discrimination compared with Blacks, despite evidence that they are less likely to experience discrimination.37,38 The racial majority privilege that White women experience may be overshadowed by the SM status for White SM women, contributing to high reports of discrimination.
These findings might also be related to disclosure of SM status. Unlike racial minority status, SM status may not be apparent to healthcare provider teams unless the patient discloses it. Healthcare teams may be able to visibly assess when a patient is a racial minority and may be careful to act in trustworthy ways. Providers may even have participated in racial bias training. However, providers may not be able to tell if someone is an SM, and the “white-washing” of lesbian, gay, biseuxal, transgender, or queer (LGBTQ) communities39 may mean that providers assume that Black patients are not sexual minorities. An SM patient may feel the need to protect their SM identity if they believe that the HCS cannot be trusted to do right by them otherwise. Therefore, the lack of training and competence (hence, warranted distrust) in serving SM patients may be observed by the patient.
4.1 ∣. Study limitations
While our study advances our understanding of how identity contributes to HCSD, and helps refine in which populations interventions should focus, our results must be considered in light of its limitations. Populations who are most stigmatized or for whom the HCS is least trustworthy may not be engaged in care at all, and our study circumvents that challenge by focusing only on a population that is already engaged in care and has access to healthcare. This enables us to further isolate the causal influences of race and sexual identity. Our study focused on a sample of women over age 35 seeking breast cancer care and may not represent the full spectrum of SM women or age groups; however, rates of breast cancer screening in the United States are high and rising, thus targeting a breast cancer-related sample would be expected to include a broad sample. Additionally, perspectives of HCS trustworthiness by those identifying both as racial and sexual minorities in cancer care is lacking, so our study is an anchor contribution in an understudied area.
4.2 ∣. Clinical implications
In addition to interactions with providers, sexual minorities may be discriminated against by the HCS itself. For example, from our team's previous qualitative work with Black SM women one breast cancer patient expressed frustration that there was a breast cancer support group specifically geared toward male but not female partners of breast cancer survivors.40 Altogether, these results and examples suggest an increased need for interventions at the provider and healthcare system levels in cancer screening and care to regain trust among racial and SM patients.
5 ∣. CONCLUSION
HCS untrustworthiness has been linked to poor outcomes across the breast cancer continuum (1) and our analysis adds the importance of the role of intersectional identity in HCSD distrust. While previous studies suggested high rates of HCSD for Black racial/ethnic minorities, our analysis suggests even higher HCSD by SM status which supercedes that associated with racial identity alone. Nonetheless, greater attribution of HCSD disparities to sexual identity than racial identity does not minimize the race difference of HCSD, but rather, shows that for those at the intersection of race and SM, discrimination due to SM status may be a greater concern to patients. Toward eliminating breast cancer disparities, institutions within the healthcare system, from insurance to clinics to provider-patient dyads, need multilevel interventions to address homophobia and racism that lead to HCS untrustworthiness.
ACKNOWLEDGEMENTS
We gratefully acknowledge our many community partners who made this research study possible. They include ZAMI National Organization of Black Lesbians on Aging (NOBLA), the Susan Love Research Army, the Pride Study, the National LGBT Cancer Network, Living Beyond Breast Cancer, and Ericka Hart—Black queer breast cancer survivor and advocate. Funding was provided by the Johns Hopkins Bloomberg School of Public Health Faculty Innovation Fund. Dr. Dean's efforts were supported by the National Cancer Institute grant K01CA184288 and the Sidney Kimmel Cancer Center grant P30CA006973. Dr. Greene was supported by NCI National Research Service Award T32 CA009314. Dr. Tredway is supported by an NCI T-32 award in Cancer Epidemiology, Prevention, and Control NIH/NCI 5T32CA009314-37.
Funding information
Division of Cancer Prevention, National Cancer Institute; Johns Hopkins Bloomberg School of Public Health Faculty Innovation Fund
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.Mouslim MC, Johnson RM, Dean LT. Healthcare system distrust and the breast cancer continuum of care. Breast Cancer Res Treat. 2020:180(1):33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson HS, Valdimarsdottir HB, Jandorf L, Redd W. Perceived disadvantages and concerns about abuses of genetic testing for cancer risk: differences across African American, Latina and Caucasian women. Patient Educ Couns. 2003;51(3):217–227. [DOI] [PubMed] [Google Scholar]
- 3.Hann KE, Freeman M, Fraser L, et al. Awareness, knowledge, perceptions, and attitudes towards genetic testing for cancer risk among ethnic minority groups: a systematic review. BMC Publ Health. 2017;17(1):503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheppard VB, Mays D, LaVeist T, Tercyak KP. Medical mistrust influences black women's level of engagement in BRCA 1/2 genetic counseling and testing. J Natl Med Assoc. 2013;105(1):17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bickell NA, Weidmann J, Fei K, Lin JJ, Leventhal H. Underuse of breast cancer adjuvant treatment: patient knowledge, beliefs, and medical mistrust. J Clin Oncol. 2009;27(31):5160–5167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dean LT, Moss SL, McCarthy AM, Armstrong K. Healthcare system distrust, physician trust, and patient discordance with adjuvant breast cancer treatment recommendations. Cancer Epidemi Prev Biomarker. 2017;26(12):1745–1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cavanagh BM, Wakefield CE, McLoone JK, Garvey G, Cohn RJ. Cancer survivorship services for indigenous peoples: where we stand, where to improve? A systematic review. J Canc Survivo. 2016;10(2):330–341. [DOI] [PubMed] [Google Scholar]
- 8.Jaiswal J, Halkitis PN. Towards a more inclusive and dynamic understanding of medical mistrust informed by science. Behav Med. 2019;45(2):79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benkert R, Cuevas A, Thompson HS, Dove-Meadows E, Knuckles D. Ubiquitous yet unclear: a systematic review of medical mistrust. Behav Med. 2019;45(2):86–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Armstrong K, McMurphy S, Dean LT, et al. Differences in the patterns of health care system distrust between Blacks and whites. J General Intern Med. 2008;23(6):827–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boulware L, Cooper L, Ratner L, LaVeist TA, Powe N. Race and trust in the health care system. Publ Health Rep. 2003;118:358–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brandon DT, Isaac LA, LaVeist TA. The legacy of Tuskegee and trust in medical care: is Tuskegee responsible for race differences in mistrust of medical care? J Natl Med Assoc. 2005;97(7):951. [PMC free article] [PubMed] [Google Scholar]
- 13.LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health ServRes. 2009;44(6):2093–2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brenick A, Romano K, Kegler C, Eaton LA. Understanding the influence of stigma and medical mistrust on engagement in routine healthcare among black women who have sex with women. LGBT Health. 2017;4(1):4–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eaton LA, Driffin DD, Kegler C, et al. The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. Am J Publ Health. 2015;105(2):e75–e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dean L, Meyer IH, Robinson K, et al. Lesbian, gay, bisexual, and transgender health: findings and concerns. J Gay Lesbian Med Assoc. 2000;4(3):102–151. [Google Scholar]
- 17.McCarthy AM, Kim JJ, Beaber EF, et al. Follow-up of abnormal breast and colorectal cancer screening by race/ethnicity. Am J Prev Med. 2016;51(4):507–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gorin SS, Heck JE, Cheng B, Smith SJ. Delays in breast cancer diagnosis and treatment by racial/ethnic group. Archives Intern Med. 2006;166(20):2244–2252. [DOI] [PubMed] [Google Scholar]
- 19.Warner ET, Tamimi RM, Hughes ME, et al. Time to diagnosis and breast cancer stage by race/ethnicity. Breast Canc Res Treat. 2012;136(3):813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Selove R, Kilbourne B, Fadden MK, et al. Time from screening mammography to biopsy and from biopsy to breast cancer treatment among black and white, women Medicare beneficiaries not participating in a health maintenance organization. Women's Health Issues. 2016;26(6):642–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cochran SD, Mays VM, Bowen D, et al. Cancer-related risk indicators and preventive screening behaviors among lesbians and bisexual women. Am J Publ Health. 2001;91(4):591–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lacombe-Duncan A, Logie CH. Correlates of clinical breast examination among lesbian, gay, bisexual, and queer women. Can J Public Health. 2016;107(4-5):e467–e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark MA, Bonacore L, Wright SJ, Armstrong G, Rakowski W. The cancer screening project for women: experiences of women who partner with women and women who partner with men. Women Health. 2003;38(2):19–33. [DOI] [PubMed] [Google Scholar]
- 24.Brown JP, Tracy JK. Lesbians and cancer: an overlooked health disparity. Canc Causes Contr. 2008;19(10):1009. [DOI] [PubMed] [Google Scholar]
- 25.Hart SL, Bowen DJ. Sexual orientation and intentions to obtain breast cancer screening. J Women's Health. 2009;18(2):177–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Poteat T, Adams MA, Malone J, et al. Delays in breast cancer care by race and sexual orientation: results from a national survey with diverse women in the United States. Cancer; 2021. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agénor M, Pérez AE, Tabaac AR, et al. Sexual orientation identity disparities in mammography among White, Black, and Latina U.S. women. LGBT Health. 2020.7(6):312–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.VanderWeele TJ, Robinson WR. On causal interpretation of race in regressions adjusting for confounding and mediating variables. Epidemiol. 2014;25(4):473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herek GM, Chopp R, Strohl D. Sexual Stigma: Putting Sexual Minority Health Issues in Context. The Health of Sexual Minorities. Boston, MA: Springer; 2007:171–208. [Google Scholar]
- 30.Jackson JW, VanderWeele TJ. Intersectional decomposition analysis with differential exposure, effects, and construct. Soc Sci Med. 2019;226:254–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jackson JW, Williams DR, VanderWeele TJ. Disparities at the intersection of marginalized groups. Soc psychiatry psychiatric Epidemiol. 2016;51(10):1349–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.AI Scheim, Bauer GR. The Intersectional Discrimination Index: development and validation of measures of self-reported enacted and anticipated discrimination for intercategorical analysis. Soc Sci Med. 2019;226:225–235. [DOI] [PubMed] [Google Scholar]
- 33.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 34.Shea JA, Micco E, Dean LT, McMurphy S, Armstrong K. Development of a revised health care system distrust scale. J General Intern Med. 2008;23(6):727–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rose A, Peters N, Shea J, Armstrong K. Development and testing of the health care system distrust scale. J Gen Intern Med. 2004;19(1):57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hovland C, Janis I, Kelley H. Communication and Persuasion. New Haven, CT: Yale University Press; 1953. [Google Scholar]
- 37.Coleman MG, Darity WA Jr, Sharpe RV. Are reports of discrimination valid? Considering the moral hazard effect. Am J Econ Sociol. 2008;67(2):149–175. [Google Scholar]
- 38.Mayrl D, Saperstein A. When white people report racial discrimination: the role of region, religion, and politics. Soc Sci Res. 2013;42(3):742–754. [DOI] [PubMed] [Google Scholar]
- 39.Ramirez JL, Gonzalez KA, Galupo MP. “Invisible during my own crisis”: responses of LGBT people of color to the Orlando shooting. J Homosex. 2018;65(5):579–599. [DOI] [PubMed] [Google Scholar]
- 40.Greene N, Malone J, Adams MA, Dean LT, Poteat T. “This is some mess right here”: exploring interactions between Black sexual minority women and health care providers for breast cancer screening and care. Cancer. 2020;127(1):74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.