ABSTRACT
Acinetobacter baumannii is an important pathogen in hospital acquired infections. Although tigecycline currently remains a potent antibiotic for treating infections caused by multidrug resistant A. baumannii (MDRAB) strains, reports of tigecycline resistant isolates have substantially increased. The resistance mechanisms to tigecycline in A. baumannii are far more complicated and diverse than what has been described in the literature so far. Here, we characterize in vitro-selected MDRAB strains obtained by increasing concentrations of tigecycline. We have identified mutations in adeS, rrf and rpoB that result in reduced susceptibility to tigecycline. Using in situ complementation experiments, we confirm that mutations in rrf, rpoB, and two types of mutations in adeS correlate with tigecycline resistance. By Western blot and polysome profile analysis, we demonstrate that the rrf mutation results in decreased expression of RRF, which affects the process of ribosome recycling ultimately leading to increased tigecycline tolerance. A transcriptional analysis shows that the mutated rpoB gene plays a role in regulating the expression of the SAM-dependent methyltransferase (trm) and transcriptional regulators, to confer moderate tigecycline resistance. This study provides direct in vitro evidence that mutations in the adeS, rpoB and rrf are associated with tigecycline resistance in A. baumannii.
KEYWORDS: Multidrug-resistant A. baumannii, tigecycline resistance, adeS, rpoB, rrf
Introduction
Acinetobacter baumannii has emerged as an important nosocomial pathogen worldwide that is primarily associated with infections such as ventilator-associated pneumonia, meningitis, bacteremia, and urinary tract infections [1]. Multidrug resistant A. baumannii (MDRAB) is considered a major public health threat and strains that are carbapenem-resistant have been declared the top priority by the World Health Organization (WHO) for new antimicrobials [2]. Treatment options for infections by such strains are extremely limited due to multidrug resistance (MDR), including last resort drugs such as colistin and tigecycline [3].
Tigecycline is a glycylcycline antibiotic with a broad-spectrum antimicrobial activity that binds to the ribosomal A site of the 30S subunit and interferes with translation [4]. The 9-t-butyl-glycylamido side chain in tigecycline prevents the main tetracycline resistance mechanism (ribosomal mutations), conferring this tetracycline derivative a significant activity in inactivating a broad range of antibiotic-resistant bacteria, including MDRAB [5]. However, tigecycline resistance in A. baumannii is increasingly observed and highly concerning [6]. To oppose the action of tigecycline, bacteria have evolved different resistance strategies. In most of the cases, resistance stems from the constitutive expression of resistance-nodulation-division (RND) efflux pumps, most often AdeABC and AdeFGH, and to a lesser extent AdeIJK, which are controlled by the transcriptional regulators AdeRS, AdeL, and AdeN, respectively [7]. In A. baumannii, the most extensively studied RND efflux system is the AdeABC system, and mutations in the two-component regulatory system AdeRS lead to decreased susceptibility to tigecycline by increasing expression of the AdeABC pump [8–10]. Other mechanisms have also been proposed for tigecycline resistance, including mutations in certain enzymes (i.e. trm and plsC) and acquired tigecycline-resistant determinants (such as tetX3, tetX4, tetX5 and tetA variants) [6,11–15]. Clearly, the resistance mechanisms of tigecycline are complex and more research is required to understand how bacteria can inactivate or remove the antibiotic compound [7].
Protein synthesis occurs on ribosomes in four steps which include initiation, elongation, termination, and finally ribosome recycling. As a crucial component of protein synthesis, the ribosome recycling factor (RRF), a product of the rrf gene, is involved in the release of the polypeptide from the ribosome as part of the translational post-termination complex, initiating a new round of translation [16]. In concert with the elongation factor EF-G, RRF drives the dissociation of the two ribosomal subunits after reaching a stop codon, or if a ribosome stalls during translation [17]. Previously, an antibiotic resistance mechanism to lincomycin and erythromycin in Listeria monocytogenes was described which is mediated by the hflXr gene that encodes a heat shock protein for the rescue of stalled ribosomes by separating their two subunits [18]. Another study showed that a hypermutating tigecycline resistant strain containing an inactivated mutS, resulted in multiple mutations in the rrf gene, suggesting that the rrf gene may play a role in tigecycline resistance [19]. However, whether the rrf gene is connected to tigecycline resistance in A. baumannii, as well as the exact mechanism of tigecycline resistance potentially mediated by rrf, remained to be determined.
The β-subunit of the bacterial DNA-dependent RNA polymerase, which is encoded by the rpoB gene, is evolutionarily conserved among all cellular organisms [20]. More than 95% of the mutations resulting in resistance to rifampicin are found in the rpoB gene, mutations that are usually present within the rifampicin resistance-determining region (RRDR) [21]. Previous studies have demonstrated that some mutations in the rpoB gene alter susceptibility not only to rifampicin, but also to other last-resort antibiotics such as vancomycin and daptomycin in Staphylococcus aureus [22]. However, mutations in the rpoB gene have never been reported in the context of tigecycline resistance in A. baumannii.
In this study, we characterized in vitro-selected MDRAB strains that have been obtained by exposing the bacteria to increasing concentrations of tigecycline. We identified mutations in adeS, rrf and rpoB that result in reduced susceptibility to tigecycline. We then verified that two types of mutations in adeS which we observed, were indeed responsible for tigecycline resistance by reconstructing the mutations in situ. In addition, we investigated the effects of the mutations in the genes rrf and rpoB in detail by analysing the transcriptome and the protein expression levels, in order to determine the molecular basis of the novel tigecycline resistance mechanism in A. baumannii.
Methods
Bacterial isolates and antimicrobial susceptibility testing
The A. baumannii strain MDR-ZJ06 was isolated from the bloodstream of a patient in Hangzhou, China in 2006 and used as the parental isolate [23]. All isolates mentioned in this study were cultured in Mueller–Hinton (MH) agar plates or broth (Oxoid, Hampshire, UK) and Luria–Bertani (LB) broth (Sangon Biotech, Shanghai, China) at 37°C overnight. The MIC of tigecycline was determined using the broth microdilution method with cation-adjusted MH broth (CAMHB) (Oxoid, Hampshire, UK). Because there is no tigecycline breakpoint for Acinetobacter, the MICs were interpreted following the guidelines of the US Food and Drug Administration for Enterobacterales (with MICs <=2 µg/mL denoting susceptibility and >=8 µg/mL denoting resistance). Other antibiotic MICs were determined using the agar plate dilution method: cefoperazone/sulbactam (2:1), imipenem, meropenem, ceftazidine, cefepime, amikacin, gentamicin and ciprofloxacin. The MIC values were interpreted according to the manufacturer’s instructions. The results were interpreted according to the guidelines recommended by the Clinical and Laboratory Standards Institute (CLSI M100-S29) [24].
In vitro selection of tigecycline mutants with reduced susceptibility
Four independent single colonies of A. baumannii MDR-ZJ06 were grown overnight at 37°C. The in vitro serial passage experiments were performed using three methods. (i) the bacteria were streaked on MH agar plates containing 10 µg/mL tigecycline and incubated overnight 37°C. Then, the bacteria were serially passaged for 21 days in the presence of 24 µg/mL tigecycline and another 40 days in the presence of 50 µg/mL tigecycline. (ii) the bacteria were streaked on MH agar plates containing 10 µg/mL tigecycline once each day for 22 days. (iii) two independent single colonies were inoculated in MH broth and the cultures were exposed to serially increasing concentrations of tigecycline, starting from 1 µg/mL (1/2 MIC of MDR-ZJ06) to 256 µg/mL. The overnight cultures were stored at −80°C and the MIC of tigecycline in selected isolates were determined using the broth microdilution method.
Genomic DNA sequencing and analysis
Bacteria from a single colony were cultured overnight at 37°C in MH broth. The genomic DNA was extracted using QIAamp DNA mini kit (Qiagen, Valencia, CA, USA) following the manufacturer’s recommendations, and was sequenced at Zhejiang Tianke (Hangzhou, China) on an Illumina Hiseq™ 2000 (Illumina. San Diego, CA, USA) using the 2 × 100 bp pair-end protocol. Mapping and putative mutations detection were performed using breseq v0.33.0 [25], referenced to the original genome of MDR-ZJ06 (GenBank accession CP001937.2). Further PCR amplifications were performed on those predicted mutations followed by Sanger sequencing to confirm the predicted mutations.
Reconstruction of mutations
Reconstruction experiments were implemented to evaluate the contribution of the confirmed mutations in laboratory-evolved strains to their decreased susceptibility to tigecycline according to Amin et al. [26], with slight modifications. Briefly, upstream and downstream sequences of target gene were amplified from mutants and purified PCR products were cloned into the pMo130-HygR vector using ClonExpress® MultiS One Step Cloning Kit (Vazyme biotech Co, Nanjing, China) via BamHI and XbaІ restriction sites. The primers used are listed in Supplementary Table 1. The recombinant plasmids were then introduced into the chromosome of MDR-ZJ06 via electroporation and selected on MH agar containing 300 µg/mL hygromycin. 0.45 mol/L catechol solution was sprayed on the surface of the plate, and yellow clones were picked for PCR identification. The second selection was then performed by culturing bacteria in MH broth with 10% sucrose, incubated overnight at 37°C to identify sucrose-resistant sensitive clones (white clones), then analysed by PCR and Sanger sequencing to confirm that the target gene was excised, resulting in a markless mutation.
Growth rate determination
Four independent cultures of A. baumannii MDR-ZJ06, XH354 (adeS::ISAba1, 50 kb dup) and reconstructed mutants were grown overnight, diluted to 1:100 in MH broth containing 0, 0.25, 0.5, 1 and 2 µg/mL tigecycline, and then 200 µl aliquots placed into a flat-bottom100-well plate in three replicates. The plate was incubated at 37°C with agitation. The OD600 of each culture was determined every 5 min for 24 h using a Bioscreen C MBR machine (Oy Growth Curves Ab Ltd., Finland). The growth rate was estimated based on OD600 curves using an R script, as previously described [27]. And values returning a P value of <0.05 from a Student t-test were taken as significant.
Acquisition and analysis of single-cell Raman spectra
Four strains of A. baumannii MDR-ZJ06, XH1457 (MDR-ZJ06 rrf H33P), XH1458 (MDR-ZJ06 rpoB G136D) and XH1454 (XH354 adeS ΔISAba1) were cultured on MH plates at 37°C overnight. The colony suspension was adjusted to 0.5 McFarland. Cells were sub-cultured with serial concentrations of tigecycline (0, 1 × MIC, 2 × MIC, 4 × MIC) and 30% heavy water (v/v) as previously described [28]. Cells was sampled after an 8-hour incubation for Raman spectra measurement. Cell pretreatment and SCRS acquisition were performed using Clinical Antimicrobial Susceptibility Test Ramanometry system (CAST-R, Qingdao Single-cell Biotech, China) and parameters were set as described previously [28]. About 100 single cells of each group were randomly selected and measured. All spectra raw data had background noise subtracted, and the baseline corrected and normalized using Q-specs (Qingdao Single-cell Biotech, China). The C-D ratio, an index to quantify the substitution of D atom in C–H bond and the metabolism degree of single cells, was calculated by dividing the integrated area intensity of C-D band (2040–2300 cm−1) by the sum of C-D band and C–H band (2800-3100 cm−1) via Ramanome Explorer (RamEX, Qingdao Single-cell Biotech, China). All experiments were conducted in triplicate. Statistical analysis was performed by SPSS statistical package (SPSS 13.0 for Windows; SPSS, Inc., Chicago, IL, USA).
Transcriptome analysis of A. baumannii MDR-ZJ06 and the rpoB and rrf mutants
To investigate the role of rpoB and rrf in tigecycline resistance, RNA-seq of A. baumannii MDR-ZJ06, XH1457 and XH1458 were performed as previously described [29]. Briefly, A. baumannii MDR-ZJ06, XH1457 and XH1458 were cultured overnight at 37°C in LB broth. Strains were diluted in 1:100 in fresh LB broth and grown at 37°C for 2 h. The 100 ml cells were collected at 4°C by centrifugation (5000 rpm,10 min). Total RNA was extracted using TRIZOL Reagent (Invitrogen, Carlsbad, CA, USA) after liquid nitrogen grinding. Both wild type and mutants were prepared in bio-triplicate. Bacteria mRNA sequence library construction and sequencing were performed by staff at Zhejiang Tianke (Hangzhou, China). The sequenced reads were mapped to MDR-ZJ06 genome using Rockhopper version 2.0.3 [30]. The raw read count in output of Rockhopper was analysed by edgeR package [31], and ggplot2 was used for figure generation [32].
Growth rate under iron limitation
Due to its low aqueous solubility, ferrous iron chelator 2,2′-dipyridyl (DIP) was prepared with 40% (v/v) of ethanol and kept refrigerated and protected from light until use. Precultures were prepared by inoculating four single colonies of the strains A. baumannii MDR-ZJ06, XH354 and reconstructed mutants harvested from fresh MH agar plates and grown overnight at 37°C in MH broth. The 0.5 M DIP stock solution was diluted in MH broth to a concentration of 100, 200 and 300 μM 2,2′-dipyridyl. Precultures were diluted to 1:100 in MH broth and the iron-chelated MH medium (100, 200 and 300 μM DIP). The subsequent steps were the same as described in the Growth rate determination.
Western blot analysis
Cell lysates were solubilized by ultrasonication and the protein concentrations were determined using the BCA protein assay kit (Thermo, Waltham, MA, USA). Proteins in SDS-loading buffer were run on 10% SDS-PAGE gels. Proteins were transferred onto a PVDF membrane followed by blocking with skimmed milk for 1 h, then incubated with anti-RRF and anti-RpoB primary antibodies at 4°C overnight. The membrane strips then were washed and incubated in HRP-conjugated goat anti-rabbit antibodies (Fdbio, Hangzhou, China) (dilution 1:5000) for 2 h at 25°C. The signal was revealed using ECL Prime according to the manufacturer’s instructions and subsequently detected in a chemiluminator. Protein bands were quantified via ImageJ. All primary antibodies were generated in rabbits and purchased from GenScript (Nanjing, China) and anti-GroEL was used as a loading control.
Polysome profile analysis
Bacteria were grown overnight in LB broth at 37°C while shaking at 200 rpm. Overnight cultures were diluted 1:100 in fresh LB and grown at 37°C. Tigecycline (MDR-ZJ06: 1 µg/mL; XH1457: 2 µg/mL) was added or not (untreated condition) at OD600 = 1 and the cells were grown for 1 h. Bacteria were then pelleted by centrifugation (30 min at 28,000 g), washed in 1 mM chloramphenicol, and flash-frozen in liquid nitrogen. Pellets were resuspended in lysis buffer (20 mM Hepes-KOH pH 7.5, 100 mM NH4Cl, 50 mM Mg(OAc)2, 1.0 mM DTT, 0.5 mM EDTA) and the cells were lysed using a high pressure homogenizer machine at 1000 bar, repeated 4 times. The lysates were cleared of cell debris by centrifugation at 4°C using an SW-32 rotor at 30,000 g for 1 h. The crude ribosomes were pelleted by centrifugation at 100,000 g (28,800 rpm) for 16 h in a sucrose cushion buffer (22:15). The precipitates were resuspended in tight couples buffer (20 mM Hepes-KOH pH 7.5, 50 mM NH4Cl, 6 mM Mg(OAc)2, 1.0 mM DTT, 0.5 mM EDTA) and the crude ribosome pellets were resuspended in ribosome buffer (20 mM Hepes-KOH pH 7.5, 150 mM NH4Cl, 10 mM Mg(OAc)2, 1.0 mM DTT, 0.5 mM EDTA), and centrifuged at 12,000 g for 20 min. Equal amounts (OD260) of cell lysates were loaded on a sucrose gradient (10%–40%) and separated by ultra-centrifugation at 85,000 g (30,000 rpm) for 4 h at 4°C using the SW-41 rotor. Samples were collected at a speed of 6 mL/min using the Density Gradient Fractionation System, and absorbance was read at 260 nm. Raw data were exported, the zero was set according to the inflexion point, and values were normalized according to the area under the curve.
Electrophoretic mobility shift assay (EMSA)
The EMSA was performed as previously described with some modifications [33]. The putative promoter regions of adeABC, rrf and rpoB were PCR-amplified from MDR-ZJ06 genomic DNA and purified by using a DNA Clean & Concentrator kit (Zymo Research, Orange County, CA, USA). The reaction mixtures (20 μl) consisted of 150 mM NaCl, 20 mM Tris–HCl pH 8.0, 0.1 mg/ml bovine serum albumin, 10% glycerol, 50 nM DNA probe and purified AdeR protein (0, 1, 2 and 4 μM) were incubated at 37°C for 30 min. Then, samples were separated on a 6% native polyacrylamide gel in 0.5 × TBE buffer. The gel was stained with GelRed nucleic acid staining solution for 15 min, and then the DNA bands were visualized by gel exposure to 260-nm UV light.
Results
Selection of A. baumannii mutants with reduced susceptibility to tigecycline: in vitro evolution experiments
In order to understand the evolution of tigecycline resistance and underlying molecular mechanisms, we performed a series of experiments to isolate A. baumannii mutants that display a decreased susceptibility to tigecycline. To this end, we performed an in vitro evolution experiment, creating a high selection pressure by slowly increasing the tigecycline concentration using the wild-type MDR-ZJ06 strain as the parental strain. For each step, the tigecycline MICs of the isolates were determined by the broth microdilution method. The MICs of the plate selected isolates increased most after the first day of selection. Surprisingly, the MICs of the selected isolates did not change significantly with the number of passages, with each passage having the amount of antibiotic doubled (Supplementary Figure 1). The final MIC values were established to be between 8 and 32 µg/mL. In the broth selection method, we measured the MICs of the final isolates from single colonies of two lineages. The MICs of the two lineages increased significantly, with final values between 16 and 32 µg/mL, while all other lineages evolved from tigecycline sensitive to resistant if using the Enterobacterales breakpoint.
Identification of genetic mutations associated with decreased susceptibility to tigecycline
Whole Genome Sequencing (WGS) was performed on the final isolates from single colonies of each lineage in order to identify mutations that possibly result in tigecycline resistance. Subsequently, the genomic differences between the selected isolates and wild-type strain (MDR-ZJ06) were determined. Four mutations were confirmed by sequencing PCR products of the regions containing the putative mutation site, that included three SNPs and one insertion (Supplementary Table 1). Two types of mutations were observed in one gene, adeS (ABZJ_02007). One mutation resulted in a substitution in amino acid number 51, changing a negatively charged glutamic acid to a positively charged lysine. Aside from the AdeS E51K, an insertion by the insertion sequence (IS) element ISAba1 was observed (371/1074). In addition, one SNP each was observed in rpoB (ABZJ_00330, G136D) and rrf (ABZJ_02277, H33P), respectively. We performed Sanger sequencing to confirm the mutations we identified in the other selected isolates and we found that all tigecycline resistance strains (MIC > = 8 µg/mL) contained the above mentioned putative resistance mutations (adeS E51K or adeS::ISAba1) (Table 1).
Table 1.
Description of bacterial strains used in this study.
| Strain | Line-age | Selection days | Parental strain | Selective MIC (µg/mL) | Description | Tigecycline MIC (µg/mL) | Relative growth rate |
|---|---|---|---|---|---|---|---|
| MDR-ZJ06 | NA | NA | NA | NA | Multidrug-resistant A. baumannii, wild type strain | 2 | 1.00 |
| Selected isolates | |||||||
| XH289 | 1 | 1 | MDR-ZJ06 | 10 | Plate selected isolates, adeS::ISAba1 | 8 | 0.90 |
| XH293 | 1 | 14 | XH289 | 10 | adeS::ISAba1 | 8 | 0.88 |
| XH297 | 1 | 7 | XH293 | 10 | adeS::ISAba1 | 8 | 0.88 |
| XH301 | 2 | 14 | XH289 | 24 | adeS::ISAba1 | 16 | 0.78 |
| XH305 | 2 | 7 | XH301 | 24 | adeS::ISAba1 | 16 | 0.80 |
| XH309 | 2 | 20 | XH305 | 50 | adeS::ISAba1 | 16 | 0.78 |
| XH313 | 2 | 20 | XH309 | 50 | adeS::ISAba1 | 16 | 0.77 |
| XH354 | 2 | NA | XH313 | NA | single clony of XH313, adeS::ISAba1, 50 kb dup | 16 | 0.93 |
| XH290 | 3 | 1 | MDR-ZJ06 | 10 | Plate selected isolates, adeS::ISAba1 | 8 | 0.81 |
| XH294 | 3 | 14 | XH290 | 10 | adeS::ISAba1 | 16 | 0.76 |
| XH298 | 3 | 7 | XH294 | 10 | adeS::ISAba1 | 8 | 0.79 |
| XH302 | 4 | 14 | XH290 | 24 | adeS::ISAba1 | 32 | 0.77 |
| XH306 | 4 | 7 | XH302 | 24 | adeS::ISAba1 | 8 | 0.83 |
| XH310 | 4 | 20 | XH306 | 50 | adeS::ISAba1, ATPase F287L | 32 | 0.75 |
| XH314 | 4 | 20 | XH310 | 50 | adeS::ISAba1, ATPase F287L | 32 | 0.76 |
| XH380 | 4 | NA | XH314 | NA | single clony of XH314, adeS::ISAba1, ATPase F287L, 6952 bp del | 32 | 0.78 |
| XH291 | 5 | 1 | MDR-ZJ06 | 10 | Plate selected isolates, adeS E51K | 8 | 0.89 |
| XH295 | 5 | 14 | XH291 | 10 | adeS E51K | 16 | 0.86 |
| XH299 | 5 | 7 | XH295 | 10 | adeS E51K | 16 | 0.91 |
| XH303 | 6 | 14 | XH291 | 24 | adeS E51K | 16 | 0.76 |
| XH307 | 6 | 7 | XH303 | 24 | adeS E51K | 16 | 0.73 |
| XH311 | 6 | 20 | XH307 | 50 | adeS E51K | 16 | 0.74 |
| XH315 | 6 | 20 | XH311 | 50 | adeS E51K | 16 | 0.75 |
| XH381 | 6 | NA | XH315 | NA | single clony of XH315, adeS E51K | 8 | 0.75 |
| XH292 | 7 | 1 | MDR-ZJ06 | 10 | Plate selected isolates, adeS::ISAba1 | 16 | 0.84 |
| XH296 | 7 | 14 | XH292 | 10 | adeS::ISAba1 | 8 | 0.81 |
| XH300 | 7 | 7 | XH296 | 10 | adeS::ISAba1 | 8 | 0.84 |
| XH304 | 8 | 14 | XH292 | 24 | adeS::ISAba1 | 8 | 0.78 |
| XH308 | 8 | 7 | XH304 | 24 | adeS::ISAba1 | 8 | 0.74 |
| XH312 | 8 | 20 | XH308 | 50 | adeS::ISAba1 | 8 | 0.80 |
| XH316 | 8 | 20 | XH312 | 50 | adeS::ISAba1 | 16 | 0.81 |
| XH382 | 8 | NA | XH316 | NA | single clony of XH313, adeS::ISAba1, 50 kb dup, ABZJ_02002 1965bp del | 8 | 0.81 |
| XH351 | 9 | 9 | MDR-ZJ06 | 1–256 | liquid selected isolates, adeS::ISAba1, rpoB G136D, rrf H33P | 16 | 0.72 |
| XH355 | 9 | NA | XH351 | NA | single clony of XH351, adeS::ISAba1, rpoB G136D, rrf H33P | 32 | 0.61 |
| XH352 | 10 | 9 | MDR-ZJ06 | 1–256 | liquid selected isolates, adeS::ISAba1, rrf H33P | 16 | 0.66 |
| XH383 | 10 | NA | XH352 | NA | single clony of XH352, adeS::ISAba1, rrf H33P | 16 | 0.70 |
| Reconstructed mutants | |||||||
| XH1454 | NA | NA | XH354 | NA | XH354 adeS ΔISAba1 | 4 | 1.10 |
| XH1455 | NA | NA | MDR-ZJ06 | NA | MDR-ZJ06 adeS::ISAba1 | 16 | 1.05 |
| XH1456 | NA | NA | MDR-ZJ06 | NA | MDR-ZJ06 adeS E51K | 8 | 0.98 |
| XH1457 | NA | NA | MDR-ZJ06 | NA | MDR-ZJ06 rrf H33P | 4 | 0.96 |
| XH1458 | NA | NA | MDR-ZJ06 | NA | MDR-ZJ06 rpoB G136D | 4 | 0.92 |
Investigation of the role of mutated genes in tigecycline resistance
After identifying the four mutations in the three genes adeS, rpoB and rrf, the impact of each individual mutation on the strain with regards to tigecycline resistance was investigated. We first introduced four mutations into the genome of the parental strain MDR-ZJ06 and created four mutant strains containing the above mutation in an otherwise wild-type strain. The effect of each mutation, the three point mutations and the one insertion, were determined by measuring their susceptibility to tigecycline. The reconstruction of the putative target mutations with a wild-type background confirmed that the individual mutations in all three genes, adeS, rpoB and rrf, played important roles in the reduced susceptibility to tigecycline, as all mutants displayed elevated MICs compared to the wild type (Table 1). The strain containing the ISAba1 insertion in adeS, subsequently called XH1455 (adeS::ISAba1) and the adeS E51K mutant strain, subsequently referred to as XH1456, showed an increased tolerance from initially 2 µg/mL (wild-type) to 16 and 8 µg/mL, respectively. This observation suggested that both types of adeS alteration ultimately lead to a decrease in tigecycline susceptibility.
Out of a total of 10 lineages, the adeS::ISAba1 mutation appeared in almost all selected strains, with the exception of lineage 5 and 6. In order to further confirm the role of ISAba1 in adeS in the resistance to tigecycline, we constructed an ISAba1 knockout strain in XH354 (MDR-ZJ06 adeS::ISAba1, 50 kb dup); the resulting strain was subsequently referred to as XH1454. In contrast to the strain that contains the IS, the knockout strain XH1454 displayed susceptibility to tigecycline, with MIC values decreasing from 16 to 4 µg/mL. This demonstrated that the insertion of ISAba1 into the adeS gene indeed correlated with tigecycline resistance. We then investigated the other two genes in which mutations occurred. Compared to the parental strain MDR-ZJ06, the tigecycline MIC of strain XH1457 doubled when we introduced the rrf H33P mutation, as did the MIC of strain XH1458, which contains the rpoB G136D mutation. This demonstrated that the single point mutation in the respective genes indeed confer reduced susceptibility to tigecycline, albeit not dramatically. To test whether any of the mutations also alter antibiotic susceptibility to other compounds, we determined the MICs to other antimicrobial drugs. We could not identify any significant change in MICs of the strains, with the exception to a dramatically increased susceptibility to cefoperazone/sulbactam in XH1455 (Supplementary Table 2).
Since the increase of the MIC values in the rrf and rpoB mutants was rather small (from 2 to 4 µg/mL), we aimed to investigate the mechanism of increased tolerance towards tigecycline further. Therefore, we performed antimicrobial susceptibility testing of single bacterial cells using Raman spectrometry. The Raman result showed that the relative C-D ratios of the XH1457 and XH1458 cells treated with 4 µg/mL tigecycline were significantly greater (p < 0.01) than that of the wild-type (Supplementary Figure 2). The results provided strong evidence that the resistant phenotype was directly linked to survival in the presence of inhibiting concentrations of tigecycline, corroborating the results obtained in the broth microdilution tests.
Do mutations that confer tigecycline resistance result in reduced fitness?
The expression of antibiotic resistance determinants is often associated with a fitness cost. To investigate this aspect, the relative growth rates of the in vitro-selected isolates and reconstructed mutants were measured and compared with the wild-type strain MDR-ZJ06 in the absence of antibiotics. All of the laboratory-selected strains exhibited slower growth than the parental strain, indicating reduced fitness, with reductions in growth rates of 7% to 39% (Table 1). Since we demonstrated that in vitro-selected adeS, rrf and rpoB mutants were involved in tigecycline resistance, we therefore sought to investigate if the reconstructed mutants also exhibited reduced growth (Figure 1(a)). Only the strain XH1458, containing the rpoB mutation, exhibited relative slower growth, indicating that this mutation was associated with reduced fitness compared with its parental strain. The other mutants showed no decreased fitness under the tested laboratory conditions. Therefore, the mutations in the adeS and rrf genes do not appear to have an impact on fitness.
Figure 1.
Fitness cost of A. baumannii MDR-ZJ06, XH354 and reconstructed mutants. (a) Histogram of relative growth rates of the wild type strain and mutant strains without tigecycline. (b) Point plot of the relative growth rates of the wild type strain and mutant strains at different concentrations of tigecycline. The experiment was repeated in triplicate. Representative results of four independent experiments are shown, and the data are the mean ± SD. *P < 0.05 (Student t test).
To investigate the effect of the mutated genes on growth under the stress, i.e. in presence of tigecycline, we determined the relative growth rate of A. baumannii MDR-ZJ06, XH354 and the reconstructed mutants at different concentrations of tigecycline (Figure 1(b)). We observed significant differences in the growth rates of the wild-type strain and the three adeS mutants (XH1455, XH1456 and XH354), as the three mutants had faster growth in antibiotic environments compared to the wild-type. The concentrations of antibiotics were chosen to be just below the MIC values of the respective strains. Our observations indicated that the mutations in adeS resulted in tigecycline resistance, facilitating faster growth in media containing antibiotic. The strains XH1457 (rrf H33P) and XH1458 (rpoB G136D) exhibited slightly higher growth rate compared to the wild-type in presence of antibiotic, although no difference was observed at 2 µg/mL of tigecycline. The ISAba1 knockout strain XH1454 (adeS ΔISAba1 in XH354) showed significantly slower growth than XH354 in presence of antibiotic, demonstrating that the insertion of ISAba1 in adeS was involved in tigecycline resistance. The results we observed correlated with the observations we obtained from measuring tigecycline MIC values of the reconstructed mutants and their parental strains.
The influence of rpoB and rrf mutations on the bacterial transcriptome
To determine if the mutations in the genes rpoB and rrf had an effect on the transcriptome of A. baumannii, RNA sequencing analyses were performed. To this end, total RNA was extracted from A. baumannii MDR-ZJ06, XH1457 (rrf H33P), and XH1458 (rpoB G136D). The sequence reads were then mapped to the genome sequence of A. baumannii MDR-ZJ06 to accommodate the genes present in A. baumannii MDR-ZJ06, XH1457 and XH1458. The number of differentially expressed genes were higher for XH1457 (n = 1105) compared to XH1458 (n = 817). The numbers of gene upregulated in XH1457 and XH1458 were 376 and 406, respectively. Down-regulation occurred in 729 and 411 genes in XH1457 and XH1458, respectively (Figure 2(a)). The changed expression affected genes that could be classified in a variety of functional categories (Figure 2(b)). The differentially expressed genes of XH1457 and XH1458 are listed in Supplementary Tables 3 and 4. For XH1457, a significant number of upregulated genes were involved in ribosome regulation, energy generation, biosynthesis, and transport functions, including multiple ribosome proteins, the ribosome-associated protein hpf, a heme biosysnthesis related gene (hemF), cystathionine-β-lyase (metC) and DUF2171, whereas Acinetobactin biosynthesis proteins and phage-related genes were downregulated (Figure 2(c)). For XH1458, multiple transcriptional regulators possibly involved in stress response and drug resistance were either upregulated or downregulated, but a number of genes related to drug resistance, motility, biosynthesis and genes of unknown function were also affected. For example, the antibiotic resistance genes blaADC-30 and blaOXA-23 were upregulated, as were the transcription elongation factor greA, the PQQ biosynthesis proteins (pqqABCDE), and fimbrial biogenesis genes. Two hypothetical proteins, the SAM-dependent methyltransferase (trm), and an AcrR/TetR regulated protein were downregulated (Figure 2(d)).
Figure 2.
Overview of the transcriptional differences of XH1457 and XH1458. (a) The number of genes differentially expressed and shared in XH1457 and XH1458. (b) The differentially expressed genes were organized per COG category (up: XH1457; down: XH1458) and were arranged according to their gene position in (c) XH1457 and (d) XH1458. The differential expression level is represented by (log2 transformed fold change) relative to MDR-ZJ06. The dots indicate the differential expression of all open reading frames and several differentially expressed genes are circled here, with COG pathway information given (see results).
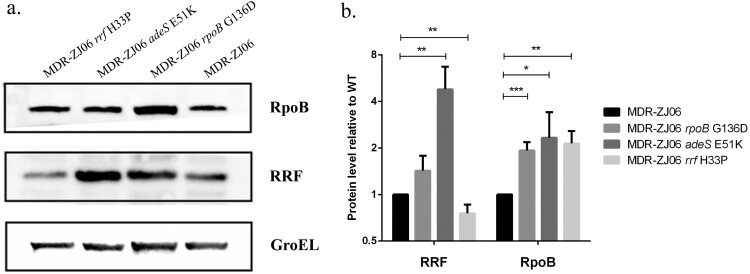
Expression levels of RRF are decreased in the rrf mutant
To investigate the contribution of the rrf and rpoB genes in reducing the susceptibility to tigecycline in more detail, we quantified the relative amount in protein expression of RpoB and RRF employing Western blot of all three reconstructed mutants (XH1456, XH1457 and XH1458). As seen in Figure 3, the expression levels of RpoB were higher in all three reconstructed mutants compared to the wild-type stain MDR-ZJ06. In the case of RRF, we observed a significantly higher expression level in strain XH1456 (adeS E51K) compared to the wild-type. Curiously, the rrf H33P mutation in strain XH1457 (rrf H33P) led to a reduction in RRF protein expression.
Figure 3.
Western blot analysis of A. baumannii MDR-ZJ06, XH1456, XH1457 and XH1458. (a) Comparison of protein levels between WT and mutants. Western blot analysis was performed for RpoB and RRF. GroEL was used as a loading control. (b) Quantification of immunoblots from four independent experiments using ImageJ software. Pixel intensity corresponds to protein levels. Asterisks indicate significant differences (*p < 0.05, **p < 0.01, ***p < 0.001) between compared groups using t test analysis.
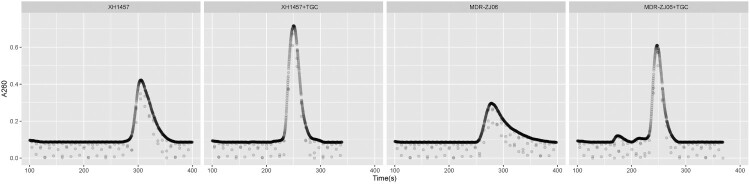
The RRF protein rescues stalled ribosomes by separating their two subunits. It might therefore be reasonable to assume with a reduction in RRF expression, the cells of strain XH1457 will experience an accumulation of 70S ribosomes compared to the wild-type. In order to test the hypothesis whether changes observed in RRF abundance were caused by ribosome stalling and recycling, we performed polysome profiling of wild-type and strain XH1457, grown in the presence or the absence of tigecycline. In our results, we observed a greater quantity of 70S ribosomes in XH1457 compared to the wild-type in the absence of tigecycline (Figure 4). This observation was consistent with the effects observed in the presence of tigecycline. Here, the difference was the quantity of 70S ribosomes being lower than in the presence of tigecycline. These data suggested that the mutation in rrf induced a reduction in expression of RRF which affected the process of ribosome recycling, resulting in increased tolerance towards tigecycline.
Figure 4.
Polysome profile analysis of A. baumannii MDR-ZJ06 and XH1457. The wild-type or rrf mutant was grown in the presence or absence of tigecycline and then analysed by sucrose density gradient centrifugation. The dots indicate the differential absorbance at 260 nm, with the x-axis representing the collection time.
AdeR binds to the promotors of rrf or rpoB
The regulator of the two-component system is able to bind to more than one site and thus can have an effect on more than one function in the cell [34]. As our Western blot assay showed that the level of RRF in the adeS mutant was significantly increased, we tested whether AdeRS is capable of binding to the rrf or rpoB promoter. The employed EMSA experiments used purified AdeR protein and dsDNA strands with the respective promotor regions for rrf and rpoB. We observed that AdeR caused a concentration dependent shift of the 316-bp rrf promoter DNA (Figure 5), while also binding (and shifting) a 439-bp rpoB promoter DNA element. The negative control adeABC* is a 168-bp predicted promoter sequence of adeABC but not the binding region of AdeR, as previously reported [34]. Taken together, these results suggested that the downstream genes of regulator AdeR included not only adeABC, but also rrf and rpoB genes.
Figure 5.
AdeR binds the rrf and rpoB promoter. The DNA binding capability of AdeR were evaluated by EMSAs. The promoter DNA fragments of rrf and rpoB were incubated with increasing amounts of purified AdeR. adeABC* was used in the EMSA as a negative control [34].
Discussion
Tigecycline resistance mechanisms in A. baumannii are more complex and diverse than what has so far been reported [7,19,35]. While the role of adeS in tigecycline susceptibility has been shown previously, in this study, we also found that additional mutations in rrf and rpoB played a significant role in reduced susceptibility to tigecycline in A. baumannii. The study examined the contributions of the individual mutations and investigated the molecular basis for the mechanism of tigecycline resistance.
Encoded by the adeS gene, AdeS is the sensor kinase of the two-component regulatory system AdeRS, that relays environmental stimuli to the response regulator AdeR for regulating AdeABC gene expression [7]. Previous studies indicated that base substitutions, insertions and deletions in the adeS gene could cause overexpression of the AdeABC efflux pump which resulted in removal of tigecycline, leading to decreased tigecycline susceptibility in A. baumannii [7,35,36]. In this study, we identified a new mutation, leading to an E51K substitution in the sensor domain of AdeS protein. The MIC of the reconstructed mutant XH1456 (adeS E51K) showed a twofold increase in MIC to tigecycline compared to the wild type. We also identified a transposon (ISAba1) insertion in adeS in our tigecycline resistant strains, and ISAba1 complementation and knockout experiments in situ demonstrated that the ISAba1 insertion in adeS played an important role in tigecycline resistance. The tigecycline MIC of XH1455 (adeS::ISAba1) can be as high as 16 µg/mL. To the best of our knowledge, this study includes the first in situ construction of an ISAba1 insertion adeS mutant in A. baumannii. Regarding the fitness of the strains, which we assessed by measuring their growth rates, we could establish that XH1455 and XH1456 displayed faster growth in antibiotic environments compared with the wild-type strain, which suggests that both types of mutations in adeS (adeS::ISAba1 and adeS E51 K) are associated with tigecycline resistance.
The tigecycline-resistant isolates obtained by the in vitro selection process contained at least one adeS mutation combined with additional mutations in rpsJ, rrf, msbA, and gnaA that may contribute to emerging tigecycline resistance mechanisms but remains to be clearly demonstrated [19]. Other previous studies had indicated that mutations in the genes rpsJ and gnaA correlated with a decrease in susceptibility to tigecycline in A. baumannii, while mutations in msbA might not be responsible for tigecycline resistance and only correlated with a decrease in fitness [11,37,38]. The gene rrf encodes the ribosome recycling factor (RRF), which plays an essential role in protein biosynthesis [16]. Recycling of the ribosome for a new round of translation initiation is an essential step of protein synthesis. In bacteria, post-termination 70S ribosome complexes fall apart into the individual 30S and 50S subunits facilitated by the concerted action of the RRF and EF-G [39]. It has been proposed that RRF is moved from the A site or P site to this second site with the help of EF-G, resulting in the release of tRNA from the ribosome [40]. Since tigecycline reversibly associates to the ribosome 30S subunit and interferes with the binding of the aminoacyl-tRNA in the ribosomal A site, RRF may play a role in dissociating tigecycline-bound ribosomes that appear to be stalled on the mRNA [19]. In our study, XH383 and XH355 were isogenic with MDR-ZJ06 and had increased tigecycline MIC during the serial passage experiment. The mutation in rrf (H33P) was observed in both XH383 and XH355 by whole genome comparison. After reconstruction of mutations in situ, the tigecycline MIC for the reconstructed mutant XH1457 was 4 µg/mL, doubling the antibiotic tolerance level compared with MDR-ZJ06. This MIC result was also confirmed by Raman micro-spectroscopy. These results both support that the rrf mutation correlates with decreased susceptibility to tigecycline.
RRF has been shown to strongly stimulate in vitro protein synthesis of Escherichia coli [41]. To assess the impact of the rrf mutation on protein synthesis, we determined the growth rates of XH1457 and MDR-ZJ06. The results showed that no or only a minimal significant difference between the two strains occurs, implying that the rrf mutation does not have a strong impact on cellular growth.
Surprisingly, the transcriptome analysis showed that XH1457 displayed lower expression levels of Acinetobactin biosynthesis protein compared with the wild-type strain. Acinetobactin is an iron chelator and is ubiquitously found in the majority of the A. baumannii isolates [42]. A. baumannii requires iron to successfully cause an infection and persist in the host, and therefore utilizes a high affinity siderophore-mediated acquisition system, with acinetobactin being a common trait to scavenge iron from the host [43,44]. We identified that the mutation in rrf led to an impairment of strain XH1457 in its ability to grow under iron-chelated conditions compared with wild-type strain (Supplementary Figure 3a). Based on these observations, it seems that the rrf mutation may affect cell growth by impairing iron acquisition, even though it does not significantly or only slightly affect the viability of this mutant under iron-rich conditions.
Ribosomal protection proteins (RPPs) like TetO and TetM that remove antibiotic compounds from the stalled ribosome, have previously been described, whereas tigecycline generally retains antibacterial activities in the presence of RPPs [45]. To the best of our knowledge, our description of the mechanism by which the ribosome is disassembled and recycled mediated by rrf is a so far unknown way to mediate tigecycline resistance. Hammerstrom et al. predicted that the mutations in rrf may decrease RRF function because they found that two mutations (rrf M1V and rrf N3N) are likely to decrease translation from the rrf mRNA, and the mutation (rrf R132C) was shown to decrease RRF-dependent disassembly of ribosomes in E. coli in an earlier study [19,46]. Our results confirm this prediction by Hammerstrom et al., as we found that the mutation in rrf resulted in a decrease of the RRF expression and the proportion of 70S ribosome decreased in XH1457 grown in the presence or absence of tigecycline, which we confirmed by the polysome profile. These observations allow us to propose that the tigecycline resistance mechanism mediated by the mutation in rrf is to reduce the expression level of RRF to affect the process of ribosome dissociation and recycling. In addition, since both RRF and tigecycline can bind to the A-site of the ribosome [40], and the structural similarities of RRF with tRNA [47], it is possible that the RRF structural modifications that are introduced by the mutation reduce the binding affinity of tigecycline to the A-site, causing a decrease in sensitivity to tigecycline. As these are multiple factors that may play a role in the resistance mechanism, to understand the interaction of RRF and tigecycline requires further studies.
RpoB is a well-known target of action of rifampin, and mutations in the RRDR are frequently associated with rifampin resistance [48]. When occurring outside of the RRDR, some missense rpoB mutations are not correlated with rifampin susceptibility [49]. Mutations in rpoB are also associated with alterations in vancomycin and daptomycin susceptibility in S. aureus [22,50]. Certain rpoB mutations have rather complex consequences and often lead to different physiological characteristics. Different mutations in the rpoB gene may induce biofilm formation, impair surface-associated motility, or reduce virulence together with an increase in fitness costs [51–53]. In this study, we confirmed the mutated rpoB (G136D) resulted in a decrease in susceptibility to tigecycline when investigating a genetically reconstructed strain containing the rpoB mutation only. To our knowledge, this is the first report of a rpoB mutation to be associated with tigecycline resistance. Growth rate experiments indicated that the mutated rpoB (G136D) conferred fitness costs to A. baumannii. In addition, the rpoB mutation induced a change in the transcriptional profile that might alter susceptibilities to other antibiotics [50]. Our transcriptional analysis showed that multiple transcriptional regulators were highly expressed, while some regulator proteins like the AcrR/TetR were present at statistically significant lower expression levels, which were often involved in the regulation of the expression of efflux systems by acting as repressors [54]. In addition, the SAM-dependent methyltransferase (trm) was downregulated in the rpoB mutant strain; previous studies suggested that a disruption of trm plays an important role in decreased susceptibility to tigecycline of A. baumannii [11,55]. Our observations might indicate a similar effect, that the mutated rpoB may be involved in the regulation of the trm expression and of transcriptional regulators such as AcrR/TetR, to confer moderate tigecycline resistance.
The two-component system AdeRS is associated with regulating the production of AdeABC efflux pump, but it has also been shown to affect biofilm formation and virulence in a strain-specific manner [56]. We demonstrated that AdeR is able to bind to the rrf and rpoB promoters, which stands in contrast to the interpretations of a previous study that adeABC genes might be the only downstream genes under control of the regulator AdeR [34]. In fact, a large number of two-component systems, such as BfmRS, BaeRS, SaeRS and ParRS have been demonstrated to have diverse effects to augment multidrug resistance, virulence and metabolic adaptations [57–60]. Since the rrf and rpoB promoter harbours a putative AdeR-binding motif, AdeRS may control a broader gene network, at least for the rrf and rpoB genes. However, the detailed effect of AdeR on the rrf or rpoB gene expression requires further experimental confirmation.
To summarize the findings of our work, we identified several dominant genetic mutations in adeS, rrf and rpoB, which result in reduced susceptibility to tigecycline in MDRAB. Using in situ complementation experiments, we verified that mutations in rrf, rpoB, and the two mutations in adeS correlate with resistance to the antibiotic. By employing Western blot and polysome profile analysis, we confirmed that the mutated rrf reduced the protein expression of RRF which affected the process of ribosome recycling, ultimately increasing the tolerance towards tigecycline. trm and multiple transcriptional regulators are possibly involved in tigecycline resistance which is mediated by a mutation in rpoB. Our study is the first to provide direct in vitro evidence that changes in the rrf and rpoB gene can lead to tigecycline resistance. The correlation between ribosome recycling and tigecycline resistance in A. baumannii is established for the first time.
Supplementary Material
Acknowledgements
We thank Prof. Yurong Wen (Xi’an Jiaotong University) for providing the purified AdeR protein in this study.
Funding Statement
This work was supported by the grants from the National Natural Science Foundation of China [grant number: 32011530116, 82002175, 31970128, 81861138054, 31770142], and the Zhejiang Province Medical Platform [grant number: 2020RC075].
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The complete genome sequences of the tigecycline resistant A. baumannii MDR-ZJ06 isolates were deposited in GenBank under BioProject No. PRJNA669209. The RNA-seq data of A. baumannii MDR-ZJ06, XH1457 and XH1458 were deposited in GenBank under BioProject no. PRJNA669292.
References
- 1.Harding CM, Hennon SW, Feldman MF.. Uncovering the mechanisms of Acinetobacter baumannii virulence. Nat Rev Microbiol. 2018 Feb;16(2):91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tacconelli E, Carrara E, Savoldi A, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018 Mar;18(3):318–327. [DOI] [PubMed] [Google Scholar]
- 3.Ni W, Han Y, Zhao J, et al. Tigecycline treatment experience against multidrug-resistant Acinetobacter baumannii infections: a systematic review and meta-analysis. Int J Antimicrob Agents. 2016;47(2):107–116. [DOI] [PubMed] [Google Scholar]
- 4.Olson MW, Ruzin A, Feyfant E, et al. Functional, biophysical, and structural bases for antibacterial activity of tigecycline. Antimicrob Agents Chemother. 2006 Jun;50(6):2156–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gordon NC, Wareham DW.. A review of clinical and microbiological outcomes following treatment of infections involving multidrug-resistant Acinetobacter baumannii with tigecycline. J Antimicrob Chemother. 2009 Apr;63(4):775–780. [DOI] [PubMed] [Google Scholar]
- 6.He T, Wang R, Liu D, et al. Emergence of plasmid-mediated high-level tigecycline resistance genes in animals and humans. Nat Microbiol. 2019 Sep;4(9):1450–1456. [DOI] [PubMed] [Google Scholar]
- 7.Gerson S, Nowak J, Zander E, et al. Diversity of mutations in regulatory genes of resistance-nodulation-cell division efflux pumps in association with tigecycline resistance in Acinetobacter baumannii. J Antimicrob Chemother. 2018 Jun 1;73(6):1501–1508. [DOI] [PubMed] [Google Scholar]
- 8.Ruzin A, Keeney D, Bradford PA.. AdeABC multidrug efflux pump is associated with decreased susceptibility to tigecycline in Acinetobacter calcoaceticus–Acinetobacter baumannii complex. J Antimicrob Chemother. 2007;59(5):1001–1004. [DOI] [PubMed] [Google Scholar]
- 9.Sun JR, Perng CL, Chan MC, et al. A truncated AdeS kinase protein generated by ISAba1 insertion correlates with tigecycline resistance in Acinetobacter baumannii. PLoS One. 2012;7(11):e49534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang YS, Chen HY, Hsu WJ, et al. Overexpression of AdeABC efflux pump associated with tigecycline resistance in clinical Acinetobacter nosocomialis isolates. Clin Microbiol Infect. 2019 Apr;25(4):512.e1–512.e6. [DOI] [PubMed] [Google Scholar]
- 11.Chen Q, Li X, Zhou H, et al. Decreased susceptibility to tigecycline in Acinetobacter baumannii mediated by a mutation in trm encoding SAM-dependent methyltransferase. J Antimicrob Chemother. 2014 Jan;69(1):72–76. [DOI] [PubMed] [Google Scholar]
- 12.Li X, Liu L, Ji J, et al. Tigecycline resistance in Acinetobacter baumannii mediated by frameshift mutation in plsC, encoding 1-acyl-sn-glycerol-3-phosphate acyltransferase. Eur J Clin Microbiol Infect Dis. 2015 Mar;34(3):625–631. [DOI] [PubMed] [Google Scholar]
- 13.Wang L, Liu D, Lv Y, et al. Novel plasmid-mediated tet(X5) gene conferring resistance to tigecycline, eravacycline and omadacycline in clinical Acinetobacter baumannii. Antimicrob Agents Chemother. 2019 Dec 20;64(1):e01326–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Linkevicius M, Sandegren L, Andersson DI.. Potential of tetracycline resistance proteins to evolve tigecycline resistance. Antimicrob Agents Chemother. 2016 Feb;60(2):789–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Foong WE, Wilhelm J, Tam HK, et al. Tigecycline efflux in Acinetobacter baumannii is mediated by TetA in synergy with RND-type efflux transporters. J Antimicrob Chemother. 2020 May 1;75(5):1135–1139. [DOI] [PubMed] [Google Scholar]
- 16.Ma Z, Tao L, Bechthold A, et al. Overexpression of ribosome recycling factor is responsible for improvement of nucleotide antibiotic-toyocamycin in streptomyces diastatochromogenes 1628. Appl Microbiol Biotechnol. 2014 Jun;98(11):5051–5058. [DOI] [PubMed] [Google Scholar]
- 17.Vivanco-Dominguez S, Bueno-Martinez J, Leon-Avila G, et al. Protein synthesis factors (RF1, RF2, RF3, RRF, and tmRNA) and peptidyl-tRNA hydrolase rescue stalled ribosomes at sense codons. J Mol Biol. 2012 Apr 13;417(5):425–439. [DOI] [PubMed] [Google Scholar]
- 18.Duval M, Dar D, Carvalho F, et al. Hflxr, a homolog of a ribosome-splitting factor, mediates antibiotic resistance. Proc Natl Acad Sci U S A. 2018 Dec 26;115(52):13359–13364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hammerstrom TG, Beabout K, Clements TP, et al. Acinetobacter baumannii repeatedly evolves a hypermutator phenotype in response to tigecycline that effectively surveys evolutionary trajectories to resistance. PLoS One. 2015;10(10):e0140489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Campbell EA, Korzheva N, Mustaev A, et al. Structural mechanism for rifampicin inhibition of bacterial rna polymerase. Cell. 2001 Mar 23;104(6):901–912. [DOI] [PubMed] [Google Scholar]
- 21.Zaw MT, Emran NA, Lin Z.. Mutations inside rifampicin-resistance determining region of rpoB gene associated with rifampicin-resistance in mycobacterium tuberculosis. J Infect Public Health. 2018 Sep–Oct;11(5):605–610. [DOI] [PubMed] [Google Scholar]
- 22.Cui L, Isii T, Fukuda M, et al. An RpoB mutation confers dual heteroresistance to daptomycin and vancomycin in Staphylococcus aureus. Antimicrob Agents Chemother. 2010 Dec;54(12):5222–5233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou H, Zhang T, Yu D, et al. Genomic analysis of the multidrug-resistant Acinetobacter baumannii strain MDR-ZJ06 widely spread in China. Antimicrob Agents Chemother. 2011 Oct;55(10):4506–4512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.CLSI . Performance standards for antimicrobial susceptibility testing. 29th ed. Wayne (PA): Clinical and Laboratory Standards Institute. 2019. CLSI supplement M100. p. 1–282.
- 25.Deatherage DE, Barrick JE.. Identification of mutations in laboratory-evolved microbes from next-generation sequencing data using breseq. Methods Mol Biol. 2014;1151:165–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amin IM, Richmond GE, Sen P, et al. A method for generating marker-less gene deletions in multidrug-resistant Acinetobacter baumannii. BMC Microbiol. 2013 Jul 13;13:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hua X, Zhang L, Moran RA, et al. Cointegration as a mechanism for the evolution of a KPC-producing multidrug resistance plasmid in proteus mirabilis. Emerg Microbes Infect. 2020 Dec;9(1):1206–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tao Y, Wang Y, Huang S, et al. Metabolic-Activity-Based assessment of antimicrobial effects by D(2)O-labeled single-cell Raman microspectroscopy. Anal Chem. 2017 Apr 4;89(7):4108–4115. [DOI] [PubMed] [Google Scholar]
- 29.Hua X, Liu L, Fang Y, et al. Colistin resistance in Acinetobacter baumannii MDR-ZJ06 revealed by a multiomics approach. Front Cell Infect Microbiol. 2017;7(45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McClure R, Balasubramanian D, Sun Y, et al. Computational analysis of bacterial RNA-Seq data. Nucleic Acids Res. 2013;41(14):e140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robinson MD, McCarthy DJ, Smyth GK.. Edger: a bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics. 2010 Jan 1;26(1):139–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wickham H. Ggplot2: elegant graphics for data analysis. New York: Springer-Verlag; 2016. [Google Scholar]
- 33.Cao Q, Wang Y, Chen F, et al. A novel signal transduction pathway that modulates rhl quorum sensing and bacterial virulence in Pseudomonas aeruginosa. PLoS Pathog. 2014 Aug;10(8):e1004340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chang TY, Huang BJ, Sun JR, et al. Ader protein regulates adeABC expression by binding to a direct-repeat motif in the intercistronic spacer. Microbiol Res. 2016 Feb;183:60–67. [DOI] [PubMed] [Google Scholar]
- 35.Xu Q, Hua X, He J, et al. The distribution of mutations and hotspots in transcription regulators of resistance-nodulation-cell division efflux pumps in tigecycline non-susceptible Acinetobacter baumannii in China. Int J Med Microbiol. 2020 Oct 24;310(8):151464. [DOI] [PubMed] [Google Scholar]
- 36.Shi Y, Hua X, Xu Q, et al. Mechanism of eravacycline resistance in Acinetobacter baumannii mediated by a deletion mutation in the sensor kinase adeS, leading to elevated expression of the efflux pump AdeABC. Infect Genet Evol. 2020 Jun;80:104185. [DOI] [PubMed] [Google Scholar]
- 37.Beabout K, Hammerstrom TG, Perez AM, et al. The ribosomal S10 protein is a general target for decreased tigecycline susceptibility. Antimicrob Agents Chemother. 2015 Sep;59(9):5561–5566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu Q, Chen T, Yan B, et al. Dual role of gnaA in antibiotic resistance and virulence in Acinetobacter baumannii. Antimicrob Agents Chemother. 2019 Oct;63(10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou D, Tanzawa T, Lin J, et al. Structural basis for ribosome recycling by RRF and tRNA. Nat Struct Mol Biol. 2020 Jan;27(1):25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Raj VS, Kaji H, Kaji A.. Interaction of RRF and EF-G from E. coli and T. thermophilus with ribosomes from both origins–insight into the mechanism of the ribosome recycling step. RNA. 2005 Mar;11(3):275–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ryoji M, Karpen JW, Kaji A.. Further characterization of ribosome releasing factor and evidence that it prevents ribosomes from reading through a termination codon. J Biol Chem. 1981 Jun 10;256(11):5798–5801. [PubMed] [Google Scholar]
- 42.Antunes LC, Imperi F, Towner KJ, et al. Genome-assisted identification of putative iron-utilization genes in Acinetobacter baumannii and their distribution among a genotypically diverse collection of clinical isolates. Res Microbiol. 2011 Apr;162(3):279–284. [DOI] [PubMed] [Google Scholar]
- 43.Penwell WF, Actis LA.. Isolation and Characterization of the Acinetobactin and baumannoferrin siderophores produced by Acinetobacter baumannii. Methods Mol Biol. 2019;1946:259–270. [DOI] [PubMed] [Google Scholar]
- 44.Zimbler DL, Penwell WF, Gaddy JA, et al. Iron acquisition functions expressed by the human pathogen Acinetobacter baumannii. Biometals. 2009 Feb;22(1):23–32. [DOI] [PubMed] [Google Scholar]
- 45.Jenner L, Starosta AL, Terry DS, et al. Structural basis for potent inhibitory activity of the antibiotic tigecycline during protein synthesis. Proc Natl Acad Sci U S A. 2013 Mar 5;110(10):3812–3816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ishino T, Atarashi K, Uchiyama S, et al. Interaction of ribosome recycling factor and elongation factor EF-G with E. coli ribosomes studied by the surface plasmon resonance technique. Genes Cells. 2000 Dec;5(12):953–963. [DOI] [PubMed] [Google Scholar]
- 47.Yoshida T, Uchiyama S, Nakano H, et al. Solution structure of the ribosome recycling factor from aquifex aeolicus. Biochemistry. 2001 Feb 27;40(8):2387–2396. [DOI] [PubMed] [Google Scholar]
- 48.Tupin A, Gualtieri M, Roquet-Banères F, et al. Resistance to rifampicin: at the crossroads between ecological, genomic and medical concerns. Int J Antimicrob Agents. 2010 Jun;35(6):519–523. [DOI] [PubMed] [Google Scholar]
- 49.Thapa B, Tribuddharat C, Rugdeekha S, et al. Rifampin resistance in carbapenem-resistant Acinetobacter baumannii in Siriraj hospital, Thailand. NMCJ. 2009 Dec;11(4):232–237. [PubMed] [Google Scholar]
- 50.Matsuo M, Hishinuma T, Katayama Y, et al. Mutation of RNA polymerase beta subunit (rpoB) promotes hVISA-to-VISA phenotypic conversion of strain Mu3. Antimicrob Agents Chemother. 2011 Sep;55(9):4188–4195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang C, Fang R, Zhou B, et al. Evolution of resistance mechanisms and biological characteristics of rifampicin-resistant Staphylococcus aureus strains selected in vitro. BMC Microbiol. 2019 Sep 18;19(1):220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou H, Zhang L, Xu Q, et al. The mismatch repair system (mutS and mutL) in Acinetobacter baylyi ADP1. BMC Microbiol. 2020 Feb 28;20(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pérez-Varela M, Corral J, Vallejo JA, et al. Mutations in the β-subunit of the RNA polymerase impair the surface-associated motility and virulence of Acinetobacter baumannii. Infect Immun. 2017 Aug;85(8):e00327–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ramos JL, Martinez-Bueno M, Molina-Henares AJ, et al. The TetR family of transcriptional repressors. Microbiol Mol Biol Rev. 2005 Jun;69(2):326–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Trebosc V, Gartenmann S, Royet K, et al. A novel genome-editing platform for drug-resistant Acinetobacter baumannii reveals an AdeR-unrelated tigecycline resistance mechanism. Antimicrob Agents Chemother. 2016 Dec;60(12):7263–7271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Richmond GE, Evans LP, Anderson MJ, et al. The Acinetobacter baumannii two-component system AdeRS regulates genes required for multidrug efflux, biofilm formation, and virulence in a strain-specific manner. mBio. 2016 Apr 19;7(2):e00430–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Geisinger E, Mortman NJ, Vargas-Cuebas G, et al. A global regulatory system links virulence and antibiotic resistance to envelope homeostasis in Acinetobacter baumannii. PLoS Pathog. 2018 May;14(5):e1007030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Leblanc SK, Oates CW, Raivio TL.. Characterization of the induction and cellular role of the BaeSR two-component envelope stress response of Escherichia coli. J Bacteriol. 2011 Jul;193(13):3367–3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sun F, Li C, Jeong D, et al. In the Staphylococcus aureus two-component system sae, the response regulator SaeR binds to a direct repeat sequence and DNA binding requires phosphorylation by the sensor kinase SaeS. J Bacteriol. 2010 Apr;192(8):2111–2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Muller C, Plésiat P, Jeannot K.. A two-component regulatory system interconnects resistance to polymyxins, aminoglycosides, fluoroquinolones, and β-lactams inPseudomonas aeruginosa. Antimicrob Agents Chemother. 2011 Mar;55(3):1211–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The complete genome sequences of the tigecycline resistant A. baumannii MDR-ZJ06 isolates were deposited in GenBank under BioProject No. PRJNA669209. The RNA-seq data of A. baumannii MDR-ZJ06, XH1457 and XH1458 were deposited in GenBank under BioProject no. PRJNA669292.