Abstract
Background and Objectives
Existing studies typically explore the factor structure of coping strategies among dementia caregivers. However, this approach overlooks the fact that caregivers often use different coping strategies simultaneously. This study aims to explore the coping patterns of primary informal dementia caregivers in Singapore, examine their significant correlates, and investigate whether different patterns would affect the depressive symptoms of caregivers.
Research Design and Methods
Two hundred eighty-one primary informal caregivers of persons with dementia (PWD) were assessed. Coping strategies were measured by the Brief Coping Orientation to Problem Experienced inventory. A latent class analysis was performed to explore caregivers’ coping patterns, followed by logistic regressions to identify the significant correlates and the relationships between coping patterns and caregiver depression.
Results
The latent class analysis suggested a three-class solution that was featured by the frequency and variety of coping strategies used by caregivers—high coping (36.3%), medium coping (37.7%), and low coping (26.0%). Factors influencing the coping patterns of our sample were mainly related to caregivers’ individual resources such as personal characteristics and caregiving stressors like PWD’s problematic behaviors and caregiving burden. Compared to caregivers in the low coping group, those in the medium coping group had significantly higher risks of potential depression.
Discussion and Implications
The current study confirmed that there are distinct coping patterns among primary informal dementia caregivers, and caregivers with the low coping pattern had fewer depressive symptoms. Future research is needed to explore if coping patterns from our sample are generalizable to dementia caregivers elsewhere.
Keywords: Coping strategies, Dementia, Informal caregiving, Latent class analysis, Quantitative research methods
Background
Persons with dementia (PWD) require an increasing level of care and assistance with daily activities as a result of their progressive deterioration. Such care is usually provided by informal caregivers such as family members and friends (Ciccarelli & Van Soest, 2018). Informal caregivers often experience positive feelings while taking care of PWD, such as a sense of satisfaction or fulfillment from caring for a loved one (Mehta, 2005; Tremont, 2011). However, they are also likely to be affected by negative stressors that might increase their subjective burden and psychological stress leading to a decrease in quality of life (Metzelthin et al., 2017).
Coping is very important in the process of caregiver stress (Gilhooly et al., 2016). The transactional model of stress and coping (Lazarus & Folkman, 1984) is commonly used to understand the stress experienced by dementia caregivers (Hawken et al., 2018; Tremont, 2011). According to this model, stress is a transaction between individuals and their environment (Lazarus, 1991). More specifically, psychological stress is defined as “a relationship with the environment that individuals appraise as significant for his or her well-being in which the demands tax or exceed available coping resources” (Lazarus & Folkman, 1986, p. 63). Coping refers to the efforts made by individuals to manage these demands either cognitively or behaviorally (Lazarus & Folkman, 1984). The transactional model proposes that individuals go through a two-stage appraisal process to determine whether the situations or experiences are stressful, and in particular, options for coping are considered during the secondary appraisal (Lazarus & Folkman, 1984); and different coping strategies used might lead to different health outcomes (Folkman et al., 1986). In short, this model posits coping as one of the central mediators within the person–environment transaction (Krohne, 2001). However, coping might play an even more extensive role in this process. Pearlin et al. (1990) proposed in their stress process model that coping not only influences the effects of primary stressors such as care recipients’ problematic behavior, daily dependency, and perceived overload on health outcomes, it may also affect the extent to which primary stressors affect secondary stressors such as role strain and intrapsychic strains. Hence, given that dementia and its associated stressors are chronic and enduring, once caregivers get used to their caregiving role and start to learn more about the condition, they may gradually become less emotionally sensitive through their adaptations and adjustments (Pozzebon et al., 2016). As such, they may become inured to some of the stressors that would have affected them previously. In other words, coping might also affect the stress appraisals of individuals.
Coping strategies are usually measured with self-reported scales, such as the Brief Coping Orientation to Problems Experienced (Brief COPE) inventory (Carver, 1997) and the Ways of Coping Scale (Folkman & Lazarus, 1980). Although studies suggested that people tend to use a variety of coping strategies simultaneously in various settings such as parenting (Kistin et al., 2014), caring for the mentally ill (Azman et al., 2017), older adults (Lin & Wu, 2014), or even PWD (Folkman & Lazarus, 1980), a traditional variable-centered approach (i.e., factor analysis) still dominates the research on coping including coping among dementia caregivers (Gilhooly et al., 2016; Taylor et al., 2015). This approach focuses on explaining relationships between the variables of interest in a population (Howard & Hoffman, 2018), and it often assumes a homogeneous pattern of coping, thus overlooking the possibility that people might combine coping strategies in different ways (Lin & Wu, 2014). On the other hand, researchers realized that this approach failed to capture the diverse nature of the population which might lead to less accurate and over-generalized conclusions about the study samples (von Eye & Bergman, 2003). Therefore, to overcome these limitations, a person-centered analytical approach (i.e., latent class analysis; Scotto Rosato & Baer, 2012) is proposed in the current study, to explore the unobserved coping patterns of caregivers (latent classes). This approach could provide more specificity compared to the traditional variable-centered approach, as multiple subpopulations with different coping patterns will be described (Howard & Hoffman, 2018). We hypothesize that there are distinct coping patterns among dementia caregivers. Compared to specific coping strategies, coping patterns are a better indicator of caregivers’ overall preferences in how they deal with caregiving stressors. In addition, we also expect that coping patterns would affect the health outcomes such as depression among dementia caregivers.
Coping patterns might be affected by different factors. Although no study has investigated the coping pattern of dementia caregivers and their correlates so far, previous studies on caregivers of other older adults might provide clues. For example, Lin and Wu (2014) in their study among caregivers of frail older adults found that coping patterns of caregivers were affected by stressors and caregivers’ social resources. Given the similarity in caring for PWD and caring for frail older adults, the two aforementioned factors may affect the coping pattern of dementia caregivers as well.
The current study aims to (1) characterize the latent subtypes of the coping patterns among primary informal dementia caregivers in Singapore through a person-centered analytical approach, (2) examine the significant correlates of these coping patterns, and (3) investigate the relationships between the coping patterns and caregiver depression. Our hypotheses were as follows:
There would be distinct coping patterns among informal dementia caregivers while facing caregiving stressors.
Predictors of coping patterns would include factors related to caregiving stressors and caregiver’s social resources.
Coping patterns would affect the depressive symptoms of caregivers.
Methods
Participants and Procedures
Primary informal caregivers of PWD (informal caregivers who were most involved in the care management of the dementia patient) were recruited from the outpatient and satellite clinics of the Institute of Mental Health and a geriatric clinic in Changi General Hospital in Singapore. A recruitment advertisement was also put up in a Voluntary Welfare Organization that serves local caregivers. Eligible participants of this study were Singapore residents (including Singapore citizens and permanent residents) aged 21 years and older, primary informal caregiver to a patient who has been formally diagnosed with dementia, and able to communicate in either English, Mandarin, or Malay. Caregivers were excluded if they had difficulty understanding the informed consent or if they failed to visit the PWD on a weekly basis. More information about this study has been published in an earlier article (Yuan et al., 2020).
Participants were approached by the study team members or referred by the collaborating clinicians. Data from eligible caregivers who were interested in the study were collected by the study team member through an interviewer-administered questionnaire to ensure that the participants understood the questionnaires correctly. The choice of the language for administration was based on the participant’s preference. In total, 282 caregivers were interviewed between January 2017 and December 2018. After excluding one participant who refused to answer a few questions on coping strategies, the total sample included in the current study was 281.
The study was approved by the National Healthcare Group Domain Specific Review Board in Singapore (reference number: 2016/00921). Written informed consent was obtained from all participants.
Measurements
Coping strategies of the participants were measured by the Brief COPE inventory (Carver, 1997). This scale consists of 28 items measuring 14 different domains of coping, with two items for each domain. The 14 domains are (1) self-distraction (e.g., I’ve been turning to work other activities to take my mind off things), (2) active coping (e.g., I’ve been taking action to try to make the situation better), (3) denial (e.g., I’ve been saying to myself “this is not real”), (4) substance use (e.g., I’ve been using alcohol or other drugs to make myself feel better), (5) use of emotional support (e.g., I’ve been getting emotional support from others), (6) use of instrumental support (e.g., I’ve been getting help and advice from other people), (7) behavioral disengagement (e.g., I’ve been giving up trying to deal with it), (8) venting (e.g., I’ve been saying things to let my unpleasant feelings escape), (9) positive reframing (e.g., I’ve been trying to see it in a different light, to make it seem more positive), (10) planning (e.g., I’ve been trying to come up with a strategy about what to do), (11) humor (e.g., I’ve been making jokes about it), (12) acceptance (e.g., I’ve been accepting the reality of the fact that it has happened), (13) religion (e.g., I’ve been trying to find comfort in my religion or spiritual beliefs), and (14) self-blame (e.g., I’ve been criticizing myself). Caregivers were asked to indicate how often they used each coping strategy to deal with stressful caregiving events during the past month on a four-point Likert scale, ranging from 1—“I haven’t been doing this at all” to 4—“I’ve been doing this a lot” (Carver, 1997). This scale has been used among family caregivers of individuals with dementia in Singapore before (Lim et al., 2011). The internal reliability (Cronbach’s alpha) of this scale among the current sample was 0.88.
The Center for Epidemiologic Studies Depression Scale (CES-D) was used to screen for depressive symptoms among the primary caregivers (Radloff, 1977). Caregivers were asked how often they experienced symptoms associated with depression over the past week. This scale consists of 20 items with response options ranging from 0 to 3 for each item (0 = rarely or none of the time, 1 = some or little of the time, 2 = moderately or much of the time, and 3 = most or almost all the time). This scale has been widely used in epidemiological studies, and it has been validated in Singapore (Stahl et al., 2008). Its total score ranges from 0 to 60, with higher scores indicating more severe depressive symptoms. A CES-D score of 16 or higher indicates at risk for clinical depression (Lewinsohn et al., 1997). A previous study suggested that it has good validity and utility in detecting depression among family caregivers of PWD (Ying et al., 2019). The internal reliability of CES-D in the current study was 0.91.
The caregiver burden was assessed using the Zarit Burden Interview (ZBI; Zarit et al., 1980). ZBI consists of 22 items on the perception of caregiving, with the responses to each item coded on a scale from 0 (never) to 4 (nearly always). The total score of the scale ranges from 0 to 88, with higher scores indicating a higher perceived caregiver burden. Examples of questions include “do you feel that your relative asks for more help than he/she needs?” and “do you feel angry when you are around your relatives?” This scale has been validated locally in a previous study and it was found to possess very good internal reliability (Cronbach’s alpha = 0.93) and good test–retest reliability (r = 0.89; Seng et al., 2010). In the current study, the internal reliability of ZBI was 0.92.
Caregiving stressors mainly include the PWD’s functional dependence and problematic behaviors. The functional dependence of the PWD was measured using the Activities of Daily Living (ADL) scale (Katz et al., 1963) and the Instrumental Activities of Daily Living (IADL) scale (Lawton, 1969). Both ADL (Sien & Jung, 2014; Xie et al., 2006) and IADL (Ng et al., 2006) scales have been validated in Singapore. The ADL scale includes six items, covering patient disability in six basic self-care activities (i.e., bathing, dressing, toileting, transfer, continence, and feeding). The IADL has eight items, and it measures eight other higher-order self-care activities (i.e., ability to use the telephone, shopping, food preparation, housekeeping, laundry, mode of transportation, responsibility for own medication, and ability to handle finances). The number of endorsed ADLs and IADLs was summed up to get a total functional dependence score (Haley et al., 1996). The internal reliability of ADL and IADL in the current study was 0.82 and 0.74, respectively. The memory and behavior problems of PWD were assessed by the memory (seven items) and behavior disruption (eight items) domains of the Revised Memory and Behavior Problems Checklist (Teri et al., 1992). It has been used in Singapore before and has shown good internal reliability for both the memory (Cronbach’s alpha = 0.87) and behavior subscales (Cronbach’s alpha = 0.73; Østbye et al., 2013). In the current study, the internal reliability was 0.65 for the memory subscale, 0.71 for the behavior subscale, and 0.74 for the two subscales together.
Data on caregivers’ individual resources including their sociodemographic characteristics and caregiving-related variables were collected. Sociodemographic information included caregiver’s age, gender (male vs. female), ethnicity (Chinese vs. Malay vs. Indian and others), educational level (secondary or below vs. A-level, polytechnic and other diploma vs. degree or above), marital status (single vs. married/divorced/widowed), and employment status (employed vs. unemployed/retired/housewife). Caregiving-related variables such as caregiver’s relationship to the PWD (spouse vs. son vs. daughter vs. others), living arrangement (together with the PWD vs. separately from the PWD), duration of the care recipient being diagnosed with dementia, and weekly caregiving hours as well as caregivers’ social resources—having a domestic helper to support them (yes vs. no) were also collected.
Statistical Analysis
Latent Class Analysis (LCA) was conducted using PROC LCA in SAS 9.3 (Lanza et al., 2007) with all the 28 items of Brief COPE. The Akaike Information Criteria (AIC; Akaike, 1987), the Bayesian Information Criteria (BIC; Schwarz, 1978), the consistent Akaike Information Criteria (cAIC; Bozdogan, 1987), and the interpretability of competing solutions were considered while selecting the model with the optimal number of latent classes. Lower ICs indicate a better fit. Second, multinomial logistic regression was used to explore the significant correlates of the latent subtypes. Finally, logistic regression was used to explore the association between latent subtypes of coping strategy patterns and the potential depression among the caregivers (depressive = 1 if CES-D ≥16). The regression analyses were also performed through SAS 9.3 (SAS Institute Inc., 2011), and a two-sided p value less than .05 was considered as statistically significant.
Results
The sample characteristics are given in Table 1. The current sample comprised 281 primary informal dementia caregivers, with an average age of 55.6 years (SD = 11.8). The majority were female (75.1%), Chinese (82.9%), married/divorced/widowed (71.9%), and currently living with the PWD (70.1%). More than half were daughter caregivers, followed by son caregiver (17.1%) and spousal caregivers (15.0%). On average, the PWD had been diagnosed for 52.5 months; and their caregivers spent 55.1 h weekly to take care of them. According to the caregivers, the PWD they were caring for had a mean functional dependence score of 5.6, and the average number of memory and behavioral problems during the past week was reported as 6.9. The mean score of the caregiving burden reported by caregivers was 33.3, which was slightly higher than the suggested cutoff of 33 or above for severe caregiving burden (Hébert et al., 2000).
Table 1.
Descriptive Statistics of the Study Participants (n = 281)
| Mean/ Frequency | SD/% | |
|---|---|---|
| Caregiver characteristics | ||
| Age | 55.6 | 11.8 |
| Gender | ||
| Male | 70 | 24.9 |
| Female | 211 | 75.1 |
| Ethnicity | ||
| Chinese | 233 | 82.9 |
| Malay | 29 | 10.3 |
| Indian and others | 19 | 6.8 |
| Education level | ||
| Secondary or below (include N/O level) | 119 | 42.4 |
| A-level, polytechnic and other diploma | 73 | 25.9 |
| Degree or above | 89 | 31.7 |
| Marital status | ||
| Single | 79 | 28.1 |
| Married/divorced/widowed | 202 | 71.9 |
| Employment status | ||
| Unemployed/retired/housewife | 120 | 42.7 |
| Employed | 161 | 57.3 |
| Caregiving-related variables | ||
| Relationship to the PWD | ||
| Spouse | 42 | 15.0 |
| Son | 48 | 17.1 |
| Daughter | 156 | 55.5 |
| Others | 35 | 12.5 |
| Living arrangement | ||
| Together with the PWD | 197 | 70.1 |
| Separately from the PWD | 84 | 29.9 |
| Have a domestic helper | ||
| Yes | 161 | 57.3 |
| No | 120 | 42.7 |
| Duration of illness (months) | 52.5 | 53.8 |
| Weekly caregiving hours | 55.1 | 53.0 |
| Functional dependence of PWD | 5.6 | 3.5 |
| Memory and behavioral problems of PWD | 6.9 | 3.0 |
| Caregiving burden | 33.3 | 16.0 |
Note: PWD = persons with dementia.
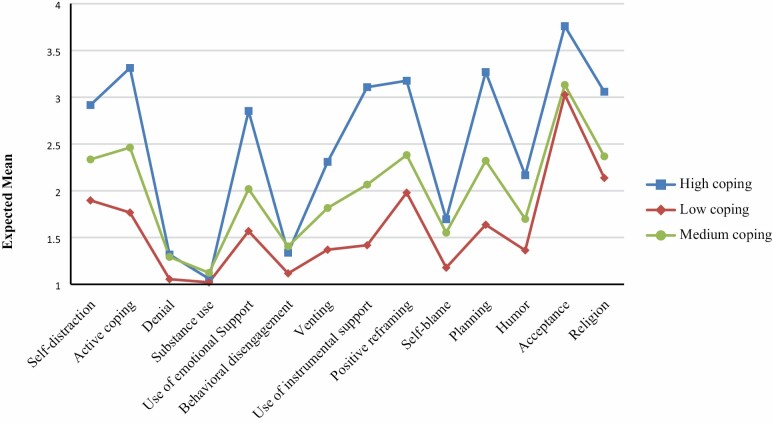
Model fit indices of the LCA models are given in Supplementary Table 1. Comparisons of fit indices across models showed the AIC reached its lowest value in the five-class solution, whereas the BIC and cAIC favored the three-class solution. In this case, solutions from three to five classes were all considered. Considering the interpretability of the model, and the fact that BIC tends to have better performance across the ICs (Nylund et al., 2007), the three-class model was selected as the final model. Table 2 includes the item response probability for each latent class. Class 1 (36.3%) was characterized with the highest probability of adopting a variety of coping strategies very frequently (i.e., active coping, self-distraction, and use of emotional support) when facing caregiving stressors such as PWD’s problematic behaviors compared to the other two coping patterns. As a result, this class was named the “high use of coping skills” group (referred to as “high coping” group hereafter). For Class 2 (26.0%)—most of the caregivers under this group tended to rely on acceptance while having a low probability of usage of other coping strategies. On items such as “I’ve been giving up trying to deal with it” and “I’ve been giving up the attempt to cope,” this group had the highest probability of reporting not using such strategies at all. As such, this class was named as the “low coping” group. For Class 3 (37.7%)—it had a similar pattern as that of Class 1, but they had relatively less frequent usage of different coping skills, and slightly higher usage of some maladaptive coping skills such as substance use and behavioral disengagement. As a result, this class was named as the “medium coping” group. Figure 1 shows the expected means of the domains of Brief COPE.
Table 2.
Rho Statistic (Item Response Probability) of the Latent Class Analysis
| High coping | Medium coping | Low coping | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Not at all | A little bit | A medium amount | A lot | Not at all | A little bit | A medium amount | A lot | Not at all | A little bit | A medium amount | A lot | ||
| Self-distraction | 1. I’ve been turning to work or other activities to take my mind off things. | .174 | .218 | .229 | .378 | .201 | .45 | .271 | .078 | .572 | .208 | .123 | .097 |
| 19. I’ve been doing something to think about it less, such as going to movies, watching TV, reading, daydreaming, sleeping, or shopping. | .139 | .127 | .315 | .419 | .102 | .445 | .356 | .097 | .423 | .302 | .072 | .203 | |
| Active coping | 2. I’ve been concentrating my efforts on doing something about the situation I’m in. | .031 | .178 | .308 | .482 | .106 | .533 | .289 | .072 | .622 | .241 | .069 | .069 |
| 7. I’ve been taking action to try to make the situation better. | .051 | .06 | .343 | .547 | .065 | .369 | .48 | .086 | .408 | .327 | .156 | .109 | |
| Denial | 3. I’ve been saying to myself “this isn’t real.” | .812 | .077 | .072 | .039 | .767 | .171 | .054 | .01 | .957 | .016 | .027 | 0 |
| 8. I’ve been refusing to believe that it has happened. | .832 | .069 | .06 | .039 | .812 | .104 | .085 | 0 | .973 | .014 | .014 | 0 | |
| Substance use | 4. I’ve been using alcohol or other drugs to make myself feel better. | .961 | .01 | .029 | 0 | .896 | .095 | 0 | .01 | 1 | 0 | 0 | 0 |
| 11. I’ve been using alcohol or other drugs to help me get through it. | .971 | .01 | .02 | 0 | .896 | .095 | 0 | .01 | .986 | 0 | 0 | .014 | |
| Use of emotional support | 5. I’ve been getting emotional support from others. | .175 | .233 | .319 | .274 | .273 | .534 | .193 | 0 | .659 | .204 | .028 | .109 |
| 15. I’ve been getting comfort and understanding from someone. | .12 | .151 | .35 | .378 | .194 | .49 | .297 | .019 | .644 | .203 | .108 | .046 | |
| Behavioral disengagement | 6. I’ve been giving up trying to deal with it. | .725 | .157 | .089 | .029 | .588 | .338 | .074 | 0 | .912 | .061 | .014 | .014 |
| 16. I’ve been giving up the attempt to cope. | .833 | .099 | .049 | .02 | .736 | .217 | .038 | .01 | .917 | .056 | .027 | 0 | |
| Venting | 9. I’ve been saying things to let my unpleasant feelings escape. | .331 | .263 | .23 | .176 | .425 | .475 | .1 | 0 | .714 | .179 | .08 | .027 |
| 21. I’ve been expressing my negative feelings. | .288 | .244 | .302 | .167 | .247 | .534 | .209 | .01 | .771 | .174 | .029 | .026 | |
| Use of instrumental support | 10. I’ve been getting help and advice from other people. | .049 | .165 | .405 | .382 | .216 | .56 | .196 | .028 | .685 | .221 | .081 | .014 |
| 23. I’ve been trying to get advice or help from other people about what to do. | .075 | .19 | .304 | .431 | .218 | .497 | .248 | .037 | .686 | .22 | .094 | 0 | |
| Positive reframing | 12. I’ve been trying to see it in a different light, to make it seem more positive. | .097 | .137 | .259 | .506 | .056 | .484 | .421 | .04 | .397 | .3 | .084 | .219 |
| 17. I’ve been looking for something good in what is happening. | .099 | .11 | .318 | .474 | .104 | .492 | .382 | .022 | .517 | .231 | .139 | .113 | |
| Self-blame | 13. I’ve been criticizing myself. | .592 | .202 | .147 | .059 | .505 | .42 | .066 | .01 | .876 | .07 | .041 | .014 |
| 26. I’ve been blaming myself for things that happened. | .575 | .198 | .15 | .078 | .626 | .254 | .102 | .019 | .903 | .055 | .013 | .028 | |
| Planning | 14. I’ve been trying to come up with a strategy about what to do. | .079 | .141 | .392 | .388 | .141 | .46 | .386 | .013 | .559 | .316 | .031 | .095 |
| 25. I’ve been thinking hard about what steps to take. | .03 | .085 | .296 | .588 | .124 | .453 | .35 | .072 | .583 | .253 | .12 | .044 | |
| Humor | 18. I’ve been making jokes about it. | .362 | .193 | .232 | .213 | .388 | .409 | .183 | .019 | .737 | .139 | .095 | .03 |
| 28. I’ve been making fun of the situation. | .464 | .181 | .218 | .137 | .6 | .261 | .11 | .029 | .795 | .122 | .057 | .027 | |
| Acceptance | 20. I’ve been accepting the reality of the fact that it has happened. | .02 | .029 | .09 | .861 | .02 | .101 | .474 | .406 | .081 | .237 | .122 | .561 |
| 24. I’ve been learning to live with it. | .02 | .01 | .192 | .779 | .02 | .187 | .57 | .224 | .203 | .182 | .142 | .473 | |
| Religion | 22. I’ve been trying to find comfort in my religion or spiritual beliefs. | .181 | .073 | .193 | .552 | .29 | .19 | .305 | .216 | .586 | .089 | .097 | .229 |
| 27. I’ve been praying or meditating. | .175 | .126 | .215 | .484 | .305 | .3 | .199 | .196 | .436 | .143 | .11 | .311 |
Figure 1.
Expected mean of each domain of the Brief Coping Orientation to Problem Experienced inventory.
The multinomial logistic regression results suggested that compared to the high coping group, male caregivers (odds ratio [OR] = 7.17, 95% confidence interval [CI] 1.25–41.05, p = .027; vs. female caregivers) and those caring for PWD with more memory and behavioral problems (OR = 1.16, 95% CI 1.01–1.33, p = .038) were significantly more likely to be in the low coping group, whereas those with diploma level education (OR = 0.29, 95% CI 0.11–0.79, p = .016; vs. degree or above) and with higher caregiving burden (OR = 0.91, 95% CI 0.88–0.94, p < .0001) were significantly less likely to be in the low coping group. Male (OR = 5.91, 95% CI 1.10–31.70, p = .038; vs. female caregivers) and unemployed caregivers (OR = 2.09, 95% CI 1.04–4.21, p = .038; vs. employed caregivers) were significantly more likely to be in the medium coping group as compared to the high coping group. Lastly, compared to the medium coping group, caregivers with diploma level education (OR = 0.27, 95% CI 0.10–0.70, p = .007; vs. degree or above), other relationship to the PWD (OR = 0.15, 95% CI 0.03–0.86, p = .033; vs. spouse), and higher caregiving burden (OR = 0.91, 95% CI 0.88–0.94, p < .0001) were significantly less likely in the low coping group. Table 3 provides the detailed multinomial logistic regression results.
Table 3.
Multinomial Logistic Regression of the Latent Coping Pattern Subtypes
| Low coping vs. High coping | Medium coping vs. High coping | Low coping vs. Medium coping | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | P | |
| Caregiver characteristics | |||||||||
| Age | 1.01 | 0.96–1.05 | .788 | 0.98 | 0.95–1.02 | .341 | 1.02 | 0.98–1.07 | .281 |
| Gender | |||||||||
| Male | 7.17 | 1.25–41.05 | .027 | 5.91 | 1.10–31.70 | .038 | 1.21 | 0.27–5.40 | .801 |
| Female | Ref | Ref | |||||||
| Ethnicity | |||||||||
| Chinese | Ref | ||||||||
| Malay | 0.93 | 0.27–3.17 | .910 | 0.52 | 0.18–1.50 | .225 | 1.80 | 0.51–6.35 | .358 |
| Indian and others | 0.81 | 0.19–3.47 | .776 | 0.31 | 0.08–1.19 | .088 | 2.58 | 0.47–14.22 | .277 |
| Education level | |||||||||
| Secondary or below (include N/O level) | 0.41 | 0.17–1.02 | .055 | 0.64 | 0.30–1.34 | .235 | 0.65 | 0.27–1.57 | .338 |
| Diploma (including A-level and polytechnic) | 0.29 | 0.11–0.79 | .016 | 1.09 | 0.50–2.37 | .830 | 0.27 | 0.10–0.70 | .007 |
| Degree or above | Ref | ||||||||
| Marital status | |||||||||
| Single | 1.05 | 0.43–2.55 | .920 | 0.55 | 0.27–1.11 | .097 | 1.90 | 0.78–4.63 | .161 |
| Married/divorced/widowed | Ref | ||||||||
| Employment status | |||||||||
| Unemployed (including retired and housewife) | 1.63 | 0.70–3.82 | .261 | 2.09 | 1.04–4.21 | .038 | 0.78 | 0.34–1.80 | .557 |
| Employed | Ref | Ref | |||||||
| Caregiving-related variables | |||||||||
| Relationship to the PWD | |||||||||
| Spouse | Ref | ||||||||
| Son | 0.16 | 0.02–1.12 | .065 | 0.46 | 0.08–2.80 | .400 | 0.34 | 0.06–1.85 | .213 |
| Daughter | 0.77 | 0.19–3.17 | .718 | 2.41 | 0.60–9.66 | .214 | 0.32 | 0.07–1.57 | .160 |
| Others | 0.34 | 0.07–1.80 | .206 | 2.28 | 0.49–10.71 | .296 | 0.15 | 0.03–0.86 | .033 |
| Living arrangement | |||||||||
| Together with the PWD | 1.05 | 0.41–2.66 | .920 | 1.78 | 0.83–3.81 | .139 | 0.59 | 0.24–1.46 | .253 |
| Separately from the PWD | Ref | ||||||||
| Have a domestic helper | |||||||||
| Yes | 1.93 | 0.86–4.31 | .111 | 1.44 | 0.73–2.87 | .295 | 1.33 | 0.60–2.97 | .481 |
| No | Ref | ||||||||
| Duration of illness (months) | 1.00 | 0.99–1.01 | .690 | 1.00 | 0.99–1.00 | .222 | 1.00 | 1.00–1.01 | .476 |
| Weekly caregiving hours | 1.00 | 0.99–1.01 | .443 | 0.99 | 0.99–1.00 | .065 | 1.00 | 0.99–1.01 | .471 |
| Functional dependence of PWD | 0.95 | 0.85–1.06 | .339 | 1.01 | 0.92–1.12 | .772 | 0.93 | 0.84–1.04 | .222 |
| Memory and behavioral problems of PWD | 1.16 | 1.01–1.33 | .038 | 1.07 | 0.96–1.19 | .223 | 1.08 | 0.94–1.24 | .269 |
| Caregiving burden | 0.91 | 0.88–0.94 | <.0001 | 1.00 | 0.98–1.02 | .837 | 0.91 | 0.88–0.94 | <.0001 |
Note: CI = confidence interval; OR = odds ratio; PWD = persons with dementia.
The descriptive statistics of CES-D scores by different coping pattern groups suggested that the low coping group had the lowest CES-D score compared to the other two coping pattern groups (Table 4). After controlling for the confounding variables including sociodemographic information and caregiving-related variables, logistic regression exploring the relationship between caregivers’ latent coping patterns and potential depression suggested that compared to the low coping group, the medium coping group showed significantly higher odds of reporting potential depression (OR = 3.69, 95% CI 1.40–9.71, p = .008). However, the difference between the high coping group and the low coping group was not statistically significant (OR = 1.94, 95% CI 0.73–5.16, p = .186; Table 5).
Table 4.
Descriptive Statistics of ZBI and CES-D Scores by Different Coping Pattern Groups
| High coping (n = 102) | Medium coping (n = 106) | Low coping (n = 73) | ||||
|---|---|---|---|---|---|---|
| Mean | Mean | Mean | Mean | Mean | SD | |
| ZBI | 37.3 | 36.8 | 22.6 | 22.6 | 36.8 | 13.9 |
| CES-D | 16.0 | 17.1 | 7.9 | 7.9 | 17.1 | 9.8 |
Note: CES-D = Center for Epidemiologic Studies Depression Scale; ZBI = Zarit Burden Interview.
Table 5.
Logistic Regression of Coping Subtypes on Potential Caregiver Depression
| OR | 95% CI | P | |
|---|---|---|---|
| High coping (Class 1) | 1.94 | 0.73–5.16 | .186 |
| Medium coping (Class 3) | 3.69 | 1.40–9.71 | .008 |
| Low coping (Class 2) | Ref |
Notes: Controlled for caregiver characteristics including age, gender, ethnicity, education level, marital status, and employment status; and caregiving-related variables including relationship to the PWD, living arrangement, having a domestic helper or not, duration of illness, weekly caregiving hours, functional dependence of PWD, memory and behavioral problems of PWD, and caregiving burden. CI = confidence interval; OR = odds ratio; PWD = persons with dementia.
Discussion
Through a person-centered analytical approach, the current study confirmed that there are three mutually exclusive underlying coping patterns among primary informal dementia caregivers in Singapore—high, medium, and low coping. These patterns are different from the unpatterned, emotional, and hybrid coping patterns identified among caregivers of frail older adults (Lin & Wu, 2014). Such differences might be due to the differences of the care recipients of the two studies (the current study is on caregivers of PWD and the other being caregivers of frail older adults) or due to the differences of the assessment tools used (we used the Brief COPE and the other study used a self-developed list of coping strategies). Informal caregivers in the high coping group used a variety of coping strategies including self-distraction, active coping, emotional/instrumental support, venting, positive reframing, planning, humor, acceptance, and religion quite frequently. Caregivers in this group were less likely to be male as compared to the other two coping groups and more likely to have a diploma-level education (vs. degree or above) as compared to the low coping group. Caregivers in the medium coping group used similar coping strategies as those in the high coping group, but with much lower frequencies. They also had slightly higher dependence on maladaptive coping strategies such as behavioral disengagement compared to the other two coping patterns. This group tended to be male and unemployed compared to the high coping group. They were more likely to have a diploma-level education (vs. degree or above) and a nonchild and nonspousal relationship with the PWD (vs. spouse) in comparison with the low coping group. Lastly, caregivers in the low coping group relied mainly on acceptance coping strategies and very minimally on any other coping strategies. Furthermore, this was also the group with the highest probability of not using coping strategies of behavioral disengagement and denial at all. This group was more likely to comprise male caregivers and those taking care of PWD with more memory and behavioral problems compared to the high coping group.
Factors influencing the coping patterns of our sample were mainly related to caregivers’ individual resources such as personal characteristics and caregiving stressors such as the PWD’s problematic behavior and caregiving burden. Caregivers’ social resources, such as having a domestic helper to assist in caregiving, did not affect their coping patterns. This is slightly different from the previous study on coping patterns of caregivers of frail older adults that suggested the importance of stressor and caregivers’ social resources (Lin & Wu, 2014). There are two possibilities. On the one hand, this could be due to the differences between social resources measured in the two studies—in our study, only information on the availability of a domestic helper was collected, whereas the previous study measured the number of informal caregivers, perceived social support, and family disagreement over caregiving (Lin & Wu, 2014). On the other hand, this might be due to the differences in caring for normal frail older adults and PWD. Caring for frail older adults mostly entails providing physical support to the older adults on their functioning needs such as ADL and IADL, while caring for PWD also requires dealing with more severe behavioral problems of PWD and uncertainties about the future. These uncertainties are less likely to be attenuated by caregivers’ social resources such as social support (Pozzebon et al., 2016; van Wijngaarden et al., 2018).
The multinomial logistic regression found that male caregivers were more likely to be in the low coping or medium coping groups than in the high coping group compared to female caregivers. Compared to the other two coping groups, the high coping group is characterized by the highest usage of different coping skills. Previous studies on gender and stress suggested that women suffered from more stress than men (Kelly et al., 2008; Matud, 2004). This also seems to be true in the caregiving setting. For instance, a previous meta-analysis suggested that compared to male caregivers, female caregivers spent more time in caregiving, were involved in more caregiving duties, and experienced higher caregiver burden and depression (Pinquart & Sorensen, 2006). Higher perceived stress might trigger more coping efforts among female caregivers, resulting in a pattern of high coping in our study. Other than gender, education was also found to affect coping patterns, with caregivers with a relatively higher education level (i.e., degree or above vs. diploma level) more likely to be in the low coping than the other two groups. As the deterioration caused by dementia is irreversible, and evidence suggests that individuals who make active efforts to eliminate problems that cannot be solved are at higher risk of depression (Isaacowitz & Seligman, 2002), a more advisable coping pattern would be to adjust and adapt to the condition. Once they are used to their caregiving role, fewer coping efforts might be triggered. Higher education might be helpful for caregivers to understand the disease better both in terms of the symptoms and the chronicity and enable them to be better adapted in their caregiving role.
Another interesting finding from the multinomial regression analysis was that caregivers with higher caregiving burden were less likely to be categorized into a low coping group (vs. high coping and medium coping groups). There are two potential explanations. First, as suggested previously, caregivers in the low coping group tended to rely on acceptance coping strategies compared to other coping strategies. It is possible that caregivers in this group have a better understanding of dementia and can adapt themselves better to their caregiving roles. Such understanding and adaptation would enable them to adjust their expectations against the PWD and avoid getting too frustrated and emotional during caregiving. Consequently, they would be more likely to overcome the daily caregiving challenges and to continue with life (Nakamura & Orth, 2005). In this case, stressors that affect other caregivers might not necessarily be perceived as stressful to them, resulting in lower perceived caregiving burden and less stress. Coping patterns could thus affect the appraisals within the transaction model of stress and coping (Lazarus & Folkman, 1984), that is, with an increasing level of threshold among caregivers in the low coping group, fewer events would be categorized as stressful in their primary appraisal. As a result, neither secondary appraisal nor other coping responses will be initiated. The other explanation is related to the level of caregiving burden. Conceivably, different levels of caregiving burden trigger different types of coping responses. When the caregiving burden is low, it is easier for caregivers to overcome it, by accepting or coming to terms with their situation. On the other hand, when the level of caregiving burden is high, the caregiver would possibly be in a greater state of distress (Del-Pino-Casado et al., 2019; Tremont, 2011). Thus, they are more likely to react with more coping responses to deal with their stress. These two explanations are divergent. Because the current study is cross-sectional in nature, we were unable to establish the causal relationship, and there is a need to conduct future longitudinal studies to determine the validity of these two explanations.
Findings from this study also extend the traditional transactional model of stress and coping in other ways. First of all, although previous studies suggested that individuals who endorse coping strategies such as emotional support seeking, problem-solving, and acceptance-based coping tend to have better health outcomes (Li et al., 2012), those who endorse more wishful thinking, avoidance, and denial coping are associated with worse health (Gilhooly et al., 2016; Li et al., 2012; Taylor et al., 2015); in reality, individuals rely on multiple coping strategies, and these strategies could cover both functional and dysfunctional coping strategies or both problem-solving and emotional coping strategies. Second, when multiple coping strategies are used, the traditional findings of the relationship between one specific coping strategy and health outcomes might no longer be applicable, indicating there might be potential research gaps here and more research is thus needed. Third, our finding suggests the possibility that coping patterns might affect the appraisals of individuals. And other than the different effects of coping strategies, coping patterns of individuals might also affect the health outcomes while facing stressors. In our study, informal dementia caregivers with low coping pattern had the lowest CES-D scores as compared to caregivers with the other two coping patterns. However, due to the cross-sectional nature of this study, future longitudinal studies are still needed to further test this hypothesis.
The current findings provide valuable new information on coping among informal dementia caregivers, and these findings have meaningful implications. First of all, unlike existing studies focused on specific coping strategies (Gilhooly et al., 2016; Rodríguez-Pérez et al., 2017), our study suggests that informal dementia caregivers combine a variety of coping strategies in different ways and have distinct coping patterns while facing caregiving stressors. We are uncertain whether these coping patterns also exist among dementia caregivers elsewhere, as dementia caregivers at different places have different characteristics. For instance, compared to a representative sample of dementia caregivers in the United States, our study has a higher proportion of child caregivers (i.e., son and daughters of PWD) 72.6% versus 50.4–52.8% among the U.S. study depending on the PWD having substantial disabilities or not (Riffin et al., 2017). Second, our study suggests that caregivers with medium coping pattern suffered from a higher risk of depression. As such, it is necessary to understand the motivators behind such a coping pattern and to develop tailored interventions to improve it. Third, studies on acceptance therapy suggest that it might be particularly helpful to situations that involve aspects that are unchangeable, such as chronic pain (Esteve et al., 2007; McCracken & Eccleston, 2003), loss of psychological function in aging (Wetherell et al., 2011), and parenting children with autism (Blackledge & Hayes, 2006). Our study might further expand this possibility as caregivers in the low coping group showed a clear reliance on acceptance coping strategies (vs. other coping strategies) and had relatively fewer depressive symptoms. Acceptance and commitment therapy (ACT) is an evidence-based psychotherapy that targets the struggles with symptoms that may be most salient and disruptive in chronic disorders (Wetherell et al., 2011). It aims to facilitate detachment from self-critical thoughts and promote psychological flexibility (Collins & Kishita, 2018; Hayes et al., 1999). In fact, there is preliminary evidence suggesting that ACT seems to be a viable and effective treatment for dementia caregivers (Collins & Kishita, 2018; Losada et al., 2015). However, because most of these studies had a relatively small sample size and were conducted in western countries (Collins & Kishita, 2018; Losada et al., 2015), more research is still needed to further test the effectiveness of ACT (especially culturally specific ACT) among dementia caregivers.
To the best of our knowledge, this is one of the first few studies—also the first in Asia—that used a person-centered analytical approach to explore the coping pattern among primary informal dementia caregivers. There was another study that had used similar analytical strategies among dementia caregivers; however, its focus was on the caregiving style which is about how caregivers manage the PWD (Hong et al., 2013). The advantage of such an approach is that it is able to capture the heterogeneity of the study sample, and as a result, it provides additional insights that traditional variable-centered approaches fail to do (Nurius & Macy, 2008; Scotto Rosato & Baer, 2012). From this point of view, a person-centered analytical approach could be a good supplement to the traditional variable-centered approach, and such a combination would give a more objective picture of the study population. Increasingly, researchers are starting to combine the use of these two approaches to understand a single issue (Meeusen et al., 2018). For future studies, researchers could investigate the generalizability of the coping patterns among informal dementia caregivers elsewhere and the rationale behind each coping pattern.
There are some limitations to the current study. First, the study focused on primary informal dementia caregivers in Singapore and participants were self-selected, which might limit the generalizability of the study findings. Nonetheless, researchers could use the same analytical strategies to investigate coping patterns of dementia caregivers elsewhere. Second, although the interviewer-administered questionnaire could ensure the quality of the data collected, it might also cause social desirability bias (Bowling, 2005), especially questions related to substance use. Third, because self-reported measures were used, there might be recall bias in the data collection. More specifically, the results of the brief COPE might be affected by the type of stressors caregivers experienced and remembered at the time of administration. Fourth, due to the relatively small sample of our study, multinomial logistic regression was run outside the LCA modeling, which might lead to less accurate predictions of the associations (Bolck et al., 2004). Additionally, although brief COPE is a widely used assessment tool for coping strategies, this inventory was not validated in Singapore. Nevertheless, the previous application of this scale among dementia caregivers in Singapore showed that it had good reliability (Lim et al., 2011). Lastly, the current study used a cross-sectional design, which precluded us from drawing a conclusion on causal relationships (e.g., caregiving burden and coping patterns). It is also possible that the level of caregiving burden and depression might affect the types of coping strategies used by caregivers. Future longitudinal studies are needed to further verify the relationships between coping patterns, caregiving burden, and caregiver health outcomes.
Conclusions
The current study confirmed that there are three distinct coping patterns among primary informal dementia caregivers in Singapore while facing stressful events from caregiving, namely, high coping, medium coping, and low coping. These coping patterns are featured by the frequency and variety of coping strategies used by caregivers, and different coping patterns could lead to different health outcomes. Informal dementia caregivers with the low coping pattern had fewer depressive symptoms. Factors influencing coping patterns mainly fall under caregivers’ individual resources (e.g., gender and education) and caregiving stressors (e.g., PWD’s problematic behaviors). Going forward, researchers should investigate the underlying reasons for different coping patterns, further test the relationships between coping patterns, caregiving burden, and PWD’s health outcomes, and examine whether an acceptance-based intervention would be helpful for informal dementia caregivers.
Funding
The study was funded by the Singapore Ministry of Health’s National Medical Research Council under the Center Grant Programme (Grant No.: NMRC/CG/004/2013) and the Institute of Mental Health Bridging Fund (CRC ref No.: 545-2016). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors have declared that no competing interests exist.
Supplementary Material
References
- Akaike, H. (1987). Factor analysis and AIC. Psychometrika, 52(3), 317–332. doi: 10.1007/BF02294359 [DOI] [Google Scholar]
- Azman, A., Jamir Singh, P. S., & Sulaiman, J. (2017). Caregiver coping with the mentally ill: A qualitative study. Journal of Mental Health (Abingdon, England), 26(2), 98–103. doi: 10.3109/09638237.2015.1124395 [DOI] [PubMed] [Google Scholar]
- Blackledge, J. T., & Hayes, S. C. (2006). Using acceptance and commitment training in the support of parents of children diagnosed with autism. Child & Family Behavior Therapy, 28(1), 1–18. doi: 10.1300/J019v28n01_01 [DOI] [Google Scholar]
- Bolck, A., Croon, M., & Hagenaars, J. (2004). Estimating latent structure models with categorical variables: One-step versus three-step estimators. Political Analysis, 12(1), 3–27. doi: 10.1093/pan/mph001 [DOI] [Google Scholar]
- Bowling, A. (2005). Mode of questionnaire administration can have serious effects on data quality. Journal of Public Health (Oxford, England), 27(3), 281–291. doi: 10.1093/pubmed/fdi031 [DOI] [PubMed] [Google Scholar]
- Bozdogan, H. (1987). Model selection and Akaike’s information criterion (AIC): The general theory and its analytical extensions. Psychometrika, 52(3), 345–370. doi: 10.1007/bf02294361 [DOI] [Google Scholar]
- Carver, C. S. (1997). You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine, 4(1), 92–100. doi: 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Ciccarelli, N., & Van Soest, A. (2018). Informal caregiving, employment status and work hours of the 50+ population in Europe. De Economist, 166(3), 363–396. doi: 10.1007/s10645-018-9323-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins, R. N., & Kishita, N. (2018). The effectiveness of mindfulness- and acceptance-based interventions for informal caregivers of people with dementia: A meta-analysis. The Gerontologist, 59(4), e363–e379. doi: 10.1093/geront/gny024 [DOI] [PubMed] [Google Scholar]
- Del-Pino-Casado, R., Rodríguez Cardosa, M., López-Martínez, C., & Orgeta, V. (2019). The association between subjective caregiver burden and depressive symptoms in carers of older relatives: A systematic review and meta-analysis. PLoS One, 14(5), e0217648. doi: 10.1371/journal.pone.0217648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esteve, R., Ramírez-Maestre, C., & López-Marínez, A. E. (2007). Adjustment to chronic pain: The role of pain acceptance, coping strategies, and pain-related cognitions. Annals of Behavioral Medicine, 33(2), 179–188. doi: 10.1007/BF02879899 [DOI] [PubMed] [Google Scholar]
- von Eye, A., & Bergman, L. R. (2003). Research strategies in developmental psychopathology: Dimensional identity and the person-oriented approach. Development and Psychopathology, 15(3), 553–580. doi: 10.1017/s0954579403000294 [DOI] [PubMed] [Google Scholar]
- Folkman, S., & Lazarus, R. S. (1980). An analysis of coping in a middle-aged community sample. Journal of Health and Social Behavior, 21(3), 219–239. doi: 10.2307/2136617 [DOI] [PubMed] [Google Scholar]
- Folkman, S., Lazarus, R. S., Dunkel-Schetter, C., DeLongis, A., & Gruen, R. J. (1986). Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology, 50(5), 992–1003. doi: 10.1037//0022-3514.50.5.992 [DOI] [PubMed] [Google Scholar]
- Gilhooly, K., Gilhooly, M., Sullivan, M., McIntyre, A., Wilson, L., Harding, E., Woodbridge, R., & Crutch, S. (2016). A meta-review of stress, coping and interventions in dementia and dementia caregiving. BMC Geriatrics, 16, 106. doi: 10.1186/s12877-016-0280-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley, W. E., Roth, D. L., Coleton, M. I., Ford, G. R., West, C. A., Collins, R. P., & Isobe, T. L. (1996). Appraisal, coping, and social support as mediators of well-being in black and white family caregivers of patients with Alzheimer’s disease. Journal of Consulting and Clinical Psychology, 64(1), 121–129. doi: 10.1037//0022-006x.64.1.121 [DOI] [PubMed] [Google Scholar]
- Hawken, T., Turner-Cobb, J., & Barnett, J. (2018). Coping and adjustment in caregivers: A systematic review. Health Psychology Open, 5(2), 2055102918810659. doi: 10.1177/2055102918810659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. Guilford Press. [Google Scholar]
- Hébert, R., Bravo, G., & Préville, M. (2000). Reliability, validity and reference values of the Zarit Burden Interview for assessing informal caregivers of community-dwelling older persons with dementia. Canadian Journal on Aging, 19(4), 494–507. doi: 10.1017/S0714980800012484 [DOI] [Google Scholar]
- Hong, S. I., Luo, N., & Yap, P. (2013). Maximizing a nurturing care style for persons with dementia: A person-centered analysis. The American Journal of Geriatric Psychiatry, 21(10), 987–998. doi: 10.1016/j.jagp.2013.01.034 [DOI] [PubMed] [Google Scholar]
- Howard, M. C., & Hoffman, M. E. (2018). Variable-centered, person-centered, and person-specific approaches: Where theory meets the method. Organizational Research Methods, 21(4), 846–876. doi: 10.1177/1094428117744021 [DOI] [Google Scholar]
- Isaacowitz, D. M., & Seligman, M. E. (2002). Cognitive style predictors of affect change in older adults. International Journal of Aging & Human Development, 54(3), 233–253. doi: 10.2190/J6E5-NP5K-2UC4-2F8B [DOI] [PubMed] [Google Scholar]
- Katz, S., Ford, A. B., Moskowitz, R. W., Jackson, B. A., & Jaffe, M. W. (1963). Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA, 185, 914–919. doi: 10.1001/jama.1963.03060120024016 [DOI] [PubMed] [Google Scholar]
- Kelly, M. M., Tyrka, A. R., Price, L. H., & Carpenter, L. L. (2008). Sex differences in the use of coping strategies: Predictors of anxiety and depressive symptoms. Depression and Anxiety, 25(10), 839–846. doi: 10.1002/da.20341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kistin, C. J., Radesky, J., Diaz-Linhart, Y., Tompson, M. C., OʼConnor, E., & Silverstein, M. (2014). A qualitative study of parenting stress, coping, and discipline approaches among low-income traumatized mothers. Journal of Developmental and Behavioral Pediatrics, 35(3), 189–196. doi: 10.1097/DBP.0000000000000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krohne, H. W. (2001). Stress and coping theories. In Smelser N. J. & Baltes P. B. (Eds.), International encyclopedia of the social & behavioral sciences (pp. 15,163–15,170). Pergamon. [Google Scholar]
- Lanza, S. T., Collins, L. M., Lemmon, D. R., & Schafer, J. L. (2007). PROC LCA: A SAS procedure for latent class analysis. Structural Equation Modeling, 14(4), 671–694. doi: 10.1080/10705510701575602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton, M. P. (1969). Supportive services in the context of the housing environment. The Gerontologist, 9(1), 15–19. doi: 10.1093/geront/9.1.15 [DOI] [PubMed] [Google Scholar]
- Lazarus, R. S. (1991). Emotion and adaptation. Oxford University Press. [Google Scholar]
- Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. Springer. [Google Scholar]
- Lazarus, R. S., & Folkman, S. (1986). Cognitive theories of stress and the issue of circularity. In Appley M. H. & Trumbull R. (Eds.), Dynamics of stress: Physiological, psychological and social perspectives (pp. 63–80). Springer US. [Google Scholar]
- Lewinsohn, P. M., Seeley, J. R., Roberts, R. E., & Allen, N. B. (1997). Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging, 12(2), 277–287. doi: 10.1037//0882-7974.12.2.277 [DOI] [PubMed] [Google Scholar]
- Li, R., Cooper, C., Bradley, J., Shulman, A., & Livingston, G. (2012). Coping strategies and psychological morbidity in family carers of people with dementia: A systematic review and meta-analysis. Journal of Affective Disorders, 139(1), 1–11. doi: 10.1016/j.jad.2011.05.055 [DOI] [PubMed] [Google Scholar]
- Lim, J., Griva, K., Goh, J., Chionh, H. L., & Yap, P. (2011). Coping strategies influence caregiver outcomes among Asian family caregivers of persons with dementia in Singapore. Alzheimer Disease and Associated Disorders, 25(1), 34–41. doi: 10.1097/WAD.0b013e3181ec18ae [DOI] [PubMed] [Google Scholar]
- Lin, I. F., & Wu, H. S. (2014). Patterns of coping among family caregivers of frail older adults. Research on Aging, 36(5), 603–624. doi: 10.1177/0164027513513271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losada, A., Márquez-González, M., Romero-Moreno, R., Mausbach, B. T., López, J., Fernández-Fernández, V., & Nogales-González, C. (2015). Cognitive-behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for dementia family caregivers with significant depressive symptoms: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 83(4), 760–772. doi: 10.1037/ccp0000028 [DOI] [PubMed] [Google Scholar]
- Matud, M. P. (2004). Gender differences in stress and coping styles. Personality and Individual Differences, 37(7), 1401–1415. doi: 10.1016/j.paid.2004.01.010 [DOI] [Google Scholar]
- McCracken, L. M., & Eccleston, C. (2003). Coping or acceptance: What to do about chronic pain? Pain, 105(1–2), 197–204. doi: 10.1016/s0304-3959(03)00202-1 [DOI] [PubMed] [Google Scholar]
- Meeusen, C., Meuleman, B., Abts, K., & Bergh, R. (2018). Comparing a variable-centered and a person-centered approach to the structure of prejudice. Social Psychological and Personality Science, 9(6), 645–655. doi: 10.1177/1948550617720273 [DOI] [Google Scholar]
- Mehta, K. K. (2005). Stress among family caregivers of older persons in Singapore. Journal of Cross-Cultural Gerontology, 20(4), 319–334. doi: 10.1007/s10823-006-9009-z [DOI] [PubMed] [Google Scholar]
- Metzelthin, S. F., Verbakel, E., Veenstra, M. Y., van Exel, J., Ambergen, A. W., & Kempen, G. I. J. M. (2017). Positive and negative outcomes of informal caregiving at home and in institutionalised long-term care: A cross-sectional study. BMC Geriatrics, 17(1), 232. doi: 10.1186/s12877-017-0620-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura, Y. M., & Orth, U. (2005). Acceptance as a coping reaction: Adaptive or not? Swiss Journal of Psychology, 64(4), 281–292. doi: 10.1024/1421-0185.64.4.281 [DOI] [Google Scholar]
- Ng, T. P., Niti, M., Chiam, P. C., & Kua, E. H. (2006). Physical and cognitive domains of the Instrumental Activities of Daily Living: Validation in a multiethnic population of Asian older adults. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 61(7), 726–735. doi: 10.1093/gerona/61.7.726 [DOI] [PubMed] [Google Scholar]
- Nurius, P. S., & Macy, R. J. (2008). Heterogeneity among violence-exposed women: Applying person-oriented research methods. Journal of Interpersonal Violence, 23(3), 389–415. doi: 10.1177/0886260507312297 [DOI] [PubMed] [Google Scholar]
- Nylund, K. L., Asparouhov, T., & Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14(4), 535–569. doi: 10.1080/10705510701575396 [DOI] [Google Scholar]
- Østbye, T., Malhotra, R., Malhotra, C., Arambepola, C., & Chan, A. (2013). Does support from foreign domestic workers decrease the negative impact of informal caregiving? Results from Singapore survey on informal caregiving. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 68(4), 609–621. doi: 10.1093/geronb/gbt042 [DOI] [PubMed] [Google Scholar]
- Pearlin, L. I., Mullan, J. T., Semple, S. J., & Skaff, M. M. (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30(5), 583–594. doi: 10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Pinquart, M., & Sörensen, S. (2006). Gender differences in caregiver stressors, social resources, and health: An updated meta-analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 61(1), 33–45. doi: 10.1093/geronb/61.1.p33 [DOI] [PubMed] [Google Scholar]
- Pozzebon, M., Douglas, J., & Ames, D. (2016). Spouses’ experience of living with a partner diagnosed with a dementia: A synthesis of the qualitative research. International Psychogeriatrics, 28(4), 537–556. doi: 10.1017/S1041610215002239 [DOI] [PubMed] [Google Scholar]
- Radloff, L. S. (1977). The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Riffin, C., Van Ness, P. H., Wolff, J. L., & Fried, T. (2017). Family and other unpaid caregivers and older adults with and without dementia and disability. Journal of the American Geriatrics Society, 65(8), 1821–1828. doi: 10.1111/jgs.14910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Pérez, M., Abreu-Sánchez, A., Rojas-Ocaña, M. J., & del-Pino-Casado, R. (2017). Coping strategies and quality of life in caregivers of dependent elderly relatives. Health and Quality of life Outcomes, 15(1), 71. doi: 10.1186/s12955-017-0634-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. (2011). SAS® 9.3 software. SAS Institute Inc. [Google Scholar]
- Schwarz, G. (1978). Estimating the dimension of a model. The Annals of Statistics, 6(2), 461–464. doi: 10.1214/aos/1176344136 [DOI] [Google Scholar]
- Scotto Rosato, N., & Baer, J. C. (2012). Latent class analysis: A method for capturing heterogeneity. Social Work Research, 36(1), 61–69. doi: 10.1093/swr/svs006 [DOI] [Google Scholar]
- Seng, B. K., Luo, N., Ng, W. Y., Lim, J., Chionh, H. L., Goh, J., & Yap, P. (2010). Validity and reliability of the Zarit Burden Interview in assessing caregiving burden. Annals of the Academy of Medicine, Singapore, 39(10), 758–763. [PubMed] [Google Scholar]
- Sien, N. Y., & Jung, H. J. T.(2014). Assessment of the six activities of daily living in adults. The Singapore Family Physician, 40(4), 26–36. [Google Scholar]
- Stahl, D., Sum, C. F., Lum, S. S., Liow, P. H., Chan, Y. H., Verma, S., Chua, H. C., & Chong, S. A. (2008). Screening for depressive symptoms: Validation of the center for epidemiologic studies depression scale (CES-D) in a multiethnic group of patients with diabetes in Singapore. Diabetes Care, 31(6), 1118–1119. doi: 10.2337/dc07-2019 [DOI] [PubMed] [Google Scholar]
- Taylor, B. J., Irish, L. A., Martire, L. M., Siegle, G. J., Krafty, R. T., Schulz, R., & Hall, M. H. (2015). Avoidant coping and poor sleep efficiency in dementia caregivers. Psychosomatic Medicine, 77(9), 1050–1057. doi: 10.1097/PSY.0000000000000237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teri, L., Truax, P., Logsdon, R., Uomoto, J., Zarit, S., & Vitaliano, P. P. (1992). Assessment of behavioral problems in dementia: The revised memory and behavior problems checklist. Psychology and Aging, 7(4), 622–631. doi: 10.1037//0882-7974.7.4.622 [DOI] [PubMed] [Google Scholar]
- Tremont, G. (2011). Family caregiving in dementia. Medicine and Health, Rhode Island, 94(2), 36–38. [PMC free article] [PubMed] [Google Scholar]
- Wetherell, J. L., Afari, N., Ayers, C. R., Stoddard, J. A., Ruberg, J., Sorrell, J. T., Liu, L., Petkus, A. J., Thorp, S. R., Kraft, A., & Patterson, T. L. (2011). Acceptance and Commitment Therapy for generalized anxiety disorder in older adults: A preliminary report. Behavior Therapy, 42(1), 127–134. doi: 10.1016/j.beth.2010.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Wijngaarden, E., van der Wedden, H., Henning, Z., Komen, R., & The, A. M. (2018). Entangled in uncertainty: The experience of living with dementia from the perspective of family caregivers. PLoS One, 13(6), e0198034. doi: 10.1371/journal.pone.0198034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie, F., Li, S.-C., Roos, E. M., Fong, K.-Y., Lo, N.-N., Yeo, S.-J., Yang, K.-Y., Yeo, W., Chong, H.-C., & Thumboo, J. (2006). Cross-cultural adaptation and validation of Singapore English and Chinese versions of the Knee injury and Osteoarthritis Outcome Score (KOOS) in Asians with knee osteoarthritis in Singapore. Osteoarthritis and Cartilage, 14(11), 1098–1103. doi: 10.1016/j.joca.2006.05.005 [DOI] [PubMed] [Google Scholar]
- Ying, J., Yap, P., Gandhi, M., & Liew, T. M. (2019). Validity and utility of the center for epidemiological studies depression scale for detecting depression in family caregivers of persons with dementia. Dementia and Geriatric Cognitive Disorders, 47(4–6), 323–334. doi: 10.1159/000500940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan, Q., Tan, T. H., Wang, P., Devi, F., Ong, H. L., Abdin, E., Harish, M., Goveas, R., Ng, L. L., Chong, S. A., & Subramaniam, M. (2020). Staging dementia based on caregiver reported patient symptoms: Implications from a latent class analysis. PLoS One, 15(1), e0227857. doi: 10.1371/journal.pone.0227857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarit, S. H., Reever, K. E., & Bach-Peterson, J. (1980). Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist, 20(6), 649–655. doi: 10.1093/geront/20.6.649 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.