Abstract
Background
Despite the need for a common definition of severe and enduring anorexia nervosa (SE-AN) with the overarching goal to optimize treatments, this definition still is being debated. Therefore, in this study we conducted an in-depth investigation of the history of AN and its clinical outcomes on inpatients with AN to ascertain the eventual “profiles” for individuals with varying durations of the illness (DOI).
Methods
We recruited 169 inpatients with AN, grouping them according to DOI: <3 years (short duration, SD-AN); 3–6.99 years (medium duration, MD-AN); and ≥7 years (long duration, LD-AN). We then performed a self-report and interview-based investigation of AN history, clinical data, eating, and general psychopathology, including personality, premorbid traits, stage of change, and quality of life. We measured the clinical outcomes for hospitalization as well.
Results
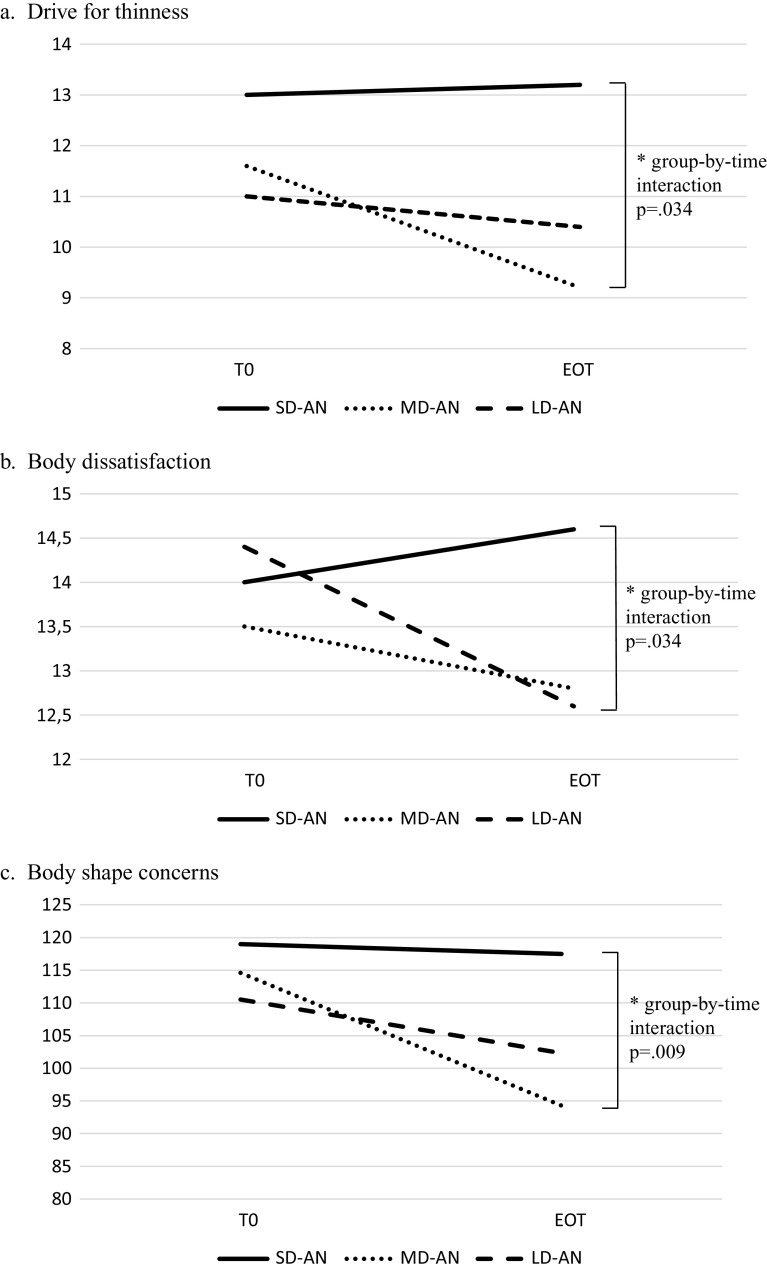
The majority of the measures did not differ across groups. Those with LD-AN were older and diagnosed mostly with the binge-purging AN subtype, failed more previous AN-related treatments, reported a lower lifetime body mass index, and trended toward a younger age at onset when compared to the other groups. All patients responded equally well to hospitalization, but patients with SD-AN improved less in drive for thinness and body-related concerns.
Conclusions
We did not find the “enduringness” of AN to be a specifier of severity. Hospitalization was effective for those with LD-AN and MD-AN, while interventions for the core cognitive aspects of over-evaluation of body shape should be offered to patients with SD-AN.
Keywords: eating disorders, hospitalization, quality of life, severe-enduring, stages of change
Introduction
Only 60% of patients with anorexia nervosa (AN) fully recover over the long-run [1] while a substantial number of patients develop a severe and enduring course (SE-AN). If this is the case, patient clinical history is characterized by relevant medical and psychological comorbidities, poor quality of life (QOL), and treatment resistance [1,2]. Importantly, a prolonged duration of illness (DOI) entails interpersonal and behavioral consequences coupled with chronic stress, thus constituting a maintaining factor [3].
Recent research has authoritatively highlighted the need for “data to clarify the nature and boundaries of SE-AN” [4]. The definitions and cutoffs for AN are challenging [5] and studies have proposed that DOI cannot be a specifier of severity because some patients need many years to recover [6,7]. Only a few studies have tried to classify SE-AN by comparing patients with different DOI or treatment responses. Data from Wildes et al. [8] did not support patients’ DOI and body mass index (BMI) as “defining” SE-AN, suggesting instead a role for eating disorder behaviors and QOL. More recently, Ambwani et al. [9] have found that patients with AN with different DOI had no differences in BMI or eating psychopathology after receiving outpatient treatment, but those with a longer DOI reported lower improvement in work or social adjustment.
However, the issue is more complicated when patients with SE-AN need to be hospitalized because of acute illness. In fact, those requiring hospitalization usually battle myriad medical, relational, and psychiatric needs [4], leading to a five times increased mortality risk [10]. Therefore, other severity indexes have been proposed, including QOL, motivation to recover, and number of previous treatment attempts [11]. Several different DOI cutoffs have been proposed for defining SE-AN, including 3 [5], 5 [12], 7 [7,9,13], 10 [14], and more than 20 years [15] with a recent review finding a mode of 7 years [11].
Given the inadequacy of DOI to describe patients with SE-AN [8], it has been suggested that a putative definition should also include treatment resistance [5]. Similarly, a detailed description of treatment mechanisms coupled with a broad reconceptualization of outcomes has been advocated for eating disorders [16]. Consequently, the most recent definition of SE-AN reads as a persistent state of dietary restriction, being underweight, and overvaluation of weight and shape with functional impairment, coupled with at least 3 years of AN and exposure to at least two evidence-based treatments [5].
However, the relationship between SE-AN and treatment feasibility is complex and plagued by several issues. First, factual treatment options for patients with SE-AN range from medical palliative care [17] to neuromodulation [18], with an open debate on the most appropriate focus for psychological therapies [4]. Second, the failure of previous therapeutic attempts is a vague concept, with “nonresponse” (e.g., relapse after treatment) confused with “treatment resistance” (e.g., not improving after a certain therapy or refusing treatments). Third, certain labels can affect treatment availability for patients with SE-AN. An enduring course of AN could entail different (and sometimes poorer [19]) possibilities of access to care, according to each health care system. Therefore, a common definition of SE-AN is needed not only for patients and their families but also for clinicians and researchers.
Despite previous research efforts, data are still conflicting and largely lacking about inpatients with SE-AN. Therefore, we aimed to investigate both the history of AN (and AN-related treatments) and the outcomes of hospitalization using a large sample of inpatients with dissimilar DOI. We had a twofold aim: first, to precisely measure the “profile” of SE-AN by performing a comprehensive assessment of patients with different DOI (e.g., history of AN, clinical data, eating and general psychopathology, personality, premorbid traits, stage of change, and QOL). Second, we aimed to shed light on the potentially diverse clinical trajectories of hospitalization of patients with different DOI. As inpatients with AN might entail a different severity scenario than that mentioned in the findings reported so far, for those with a longer DOI, we expected to find a greater overall severity coupled with poorer outcomes on hospital discharge.
Methods
Participants
A total of 190 inpatients were consecutively enrolled at the Psychiatry Ward of the Eating Disorders Center of the “Città Della Salute e Della Scienza” Hospital of the University of Turin, Italy, from January 2016 to June 2020. All participants were Caucasian and voluntarily admitted. Inclusion criteria were: (a) diagnosis of AN as assessed on admission by an experienced psychiatrist using a structured interview [20]; (b) age range of 16–55 years; and (c) no history of psychotic-spectrum disorders, bipolar disorders, or substance use dependence. In our analyses, we used a patient’s first admission to our unit in cases of multiple hospitalizations.
Of the initial sample, five patients refused to provide their consent to participate in the study, and 16 returned incomplete assessments; therefore, the final sample was 169 inpatients. All patients provided written informed consent for this Ethical Committee-approved study (Approval No. 0036472).
To ensure data comparability, using the earlier literature [9,11] we divided the sample as follows: patients with short (SD-AN, <3 years), medium (MD-AN, 3–6.99 years), and long DOI (LD-AN, ≥7 years). During the admission interview, an experienced psychiatrist measured patients’ DOI, documenting the first onset of the eating disorder. No patients reported lifetime cross-over across diagnoses of eating disorders, so the data collected for our sample consistently referred to the DOI of AN.
Procedures
We collected the patients’ clinical characteristics at hospital admission (T0) and discharge (e.g., end of treatment [EOT]). An experienced psychiatrist performed a specific anamnestic investigation on patient DOI and previous treatments to disentangle nonresponse versus treatment resistance. We calculated BMI at both time points.
All patients completed the following assessments at T0 and EOT: the Eating Disorder Inventory-2 (EDI-2), Italian version [21], to measure eating disorder attitudes and behaviors (we included in our analysis the “core” subscales of this questionnaire, namely drive for thinness, bulimia, and body dissatisfaction); the Eating Disorder Examination Questionnaire (EDE-Q), Italian version [22], to assess eating psychopathology; the Body Shape Questionnaire (BSQ) [23], to estimate body image perception; the State–Trait Anxiety Inventory (STAI), Italian version [24], to assess state and trait anxiety; the Beck Depression Inventory (BDI) [25] to measure depressive symptoms; the Hamilton Rating Scale for Anxiety (HAM-A) [26] to assess severity of anxiety through symptom gradation; the Hamilton Depression Rating Scale (HAM-D) [27] to investigate depressive symptoms; and the EuroQoL Health Questionnaire/Visual Analogue Scale (EQ-5D) [28] to measure QOL.
All patients completed the following assessments at T0: the Anorexia Nervosa Stages of Change Questionnaire (ANSOCQ) [29] to evaluate the core features of AN and assess stages of change; the Temperament Evaluation of Memphis, Pisa, Paris and San Diego Autoquestionnaire (TEMPS-A), Italian version [30], to investigate affective temperaments; the Frost Multidimensional Perfectionism Scale (FMPS) [31] to evaluate multidimensional perfectionism; the Childhood Retrospective Perfectionism Questionnaire (CHIRP)-self-report version [32] to assess childhood AN-related traits; and the Premorbid Childhood Traits Questionnaire (PCT-Q) [33] to measure childhood harm avoidance, reward sensitivity, social phobia, alexithymia, achievement drive, interoceptive awareness, food obsessions, worry about future, and sleep problems.
At EOT all patients completed the Working Alliance Inventory-Short Revised (WAI-SR) [34] to evaluate therapeutic alliance.
Treatment
All participants were inpatients seeking treatment at the Eating Disorders Center of the University of Turin, Italy, with the vast majority admitted through the emergency room in an acute phase of AN. All treatment costs were covered by the National Health System, so no financial or insurance barriers existed for the patients. The treatment was delivered following international guidelines [35]. The intervention was “noneclectic”; it was integrated and focused on improving patients’ AN-related life-threatening conditions and managing eating symptoms. The intervention had the following aims: (a) to reduce patients’ clinical life-threatening conditions; (b) to foster patients’ motivation for the subsequent therapeutic steps; (c) to work with structured daily sessions on symptom management focusing on diet and body image; (d) to work psychologically to understand the possible causes that led to an emergency admission; and (e) to provide families with psychoeducation. We strictly monitored patients from a medical standpoint and provided psychological interventions informed by motivational interviewing to support patients’ daily efforts and to reinforce the next steps of treatment. No involuntary admissions are allowed at our unit nor are coercive methods used. Instead, we offer behavioral contracting for meals and eating symptoms.
Statistical analysis
We used the SPSS 26.0 statistical software package (IBM SPSS Statistics for Windows, version 26.0; IBM Corp., Armonk, NY) for data analysis. We split the sample into three groups according to the aforementioned criteria (SD-AN, <3 years; MD-AN, 3–6.99 years; LD-AN, ≥7 years). Subsequently, we conducted an analysis of variance (ANOVA), followed by the Sheffè post hoc test, to ascertain differences across groups in the continuous variables. For categorical parameters we used Fisher’s exact test with correction for multiple comparisons. To investigate hospitalization outcomes and differences across groups over time, we performed a repeated-measures ANOVA. We measured effect size using eta-squared (η 2) according to Cohen’s work [36] on effect sizes: small, η 2 = 0.01–0.06; moderate, η 2 = 0.06–0.14; or large, η 2 > 0.14.
Results
Sociodemographic and clinical characteristics
Patients with LD more frequently were married and unemployed than were those with SD and MD (Table 1). Patients with MD and LD were more often diagnosed with AN-BP than were patients with SD but also reported more diagnostic cross-over. Age significantly differed across groups, with patients with SD being younger than those with MD, who in turn were younger than those LD. Also, the SD group reported a lowest lifetime BMI significantly higher than the LD group; however, comparisons between the SD and MD groups and the MD and LD groups did not differ from each other. Similarly, patients with SD reported a significantly lower number of AN-related hospitalizations than did those with LD; however, comparisons between patients with SD and MD and with MD and LD did not differ from each other. Those with LD also showed a trend toward a significantly earlier age at onset when compared to those with SD. In contrast, the groups did not differ in gender distribution, current BMI, medications at admission, family history of psychiatric disorders (including AN), and past sexual abuse and suicide attempts.
Table 1.
Differences in sociodemographic and clinical data for patients with short, medium, and long duration of illness.
| Total sample inpatients with AN n = 169 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| <3 years | ≥3 and <7 years | ≥7 years | Test statistics | ||||||
| Short duration (SD-AN) n = 76 | Medium duration (MD-AN) n = 47 | Long duration (LD-AN) n = 46 | |||||||
| Mean (SD) | N (%) | Mean (SD) | N (%) | Mean (SD) | N (%) | F | p | Sheffè post hoc | |
| Age, years | 19.6 (4.9) | 23.1 (7.5) | 31.7 (9.4) | 41.75 | <0.001 | SD-AN < MD-AN < LD-AN | |||
| Gender | 0.735 a | ||||||||
| Female | 71 (93.4) | 43 (91.5) | 44 (95.7) | ||||||
| Male | 5 (6.6) | 4 (8.5) | 2 (4.3) | ||||||
| Status | 0.001 a | ||||||||
| Single | 66 (86.8)b | 40 (85.1)b | 27 (58.7)c | ||||||
| In a relationship/married | 10 (13.2)b | 7 (14.9)b | 17 (37)c | ||||||
| Divorced | 0 (0)b | 0 (0)b | 2 (4.3)b | ||||||
| Employment | <0.001 a | ||||||||
| Student | 34 (44.7)b | 19 (40.4)b | 5 (10.9)b | ||||||
| Employed | 33 (43.4)b | 18 (38.3)b | 23 (50)b | ||||||
| Unemployed | 9 (11.9)b | 10 (21.3)b,c | 18 (39.1)c | ||||||
| Subtype of AN | 0.006 a | ||||||||
| AN-R | 65 (85.5)b | 31 (66)c | 29 (63)c | ||||||
| AN-BP | 11 (14.5)b | 16 (34)c | 17 (37)c | ||||||
| Diagnostic cross-over in the past | 3 (4)b | 7 (14.9)b,c | 9 (20)c | 0.014 a | |||||
| Age at onset, years | 18.3 (5.2) | 18.9 (7.5) | 15.8 (4.1) | 3.159 | 0.046 | SD-AN = MD-AN | |||
| MD-AN = LD-AN | |||||||||
| SD-AN > LD-AN d | |||||||||
| Body mass index | 14.4 (1.9) | 14.4 (1.7) | 14.3 (2.1) | 0.007 | 0.993 | – | |||
| Lowest lifetime BMI | 14.1 (2) | 13.7 (1.6) | 12.8 (1.9) | 5.91 | 0.003 | SD-AN = MD-AN | |||
| MD-AN = LD-AN | |||||||||
| SD-AN > LD-AN | |||||||||
| Previous AN-related hospitalizations | 21 (31.3)b | 23 (48.9)c | 29 (63)c | <0.001 a | |||||
| Number of previous hospitalizations | 0.4 (.8) | 1.1 (1.6) | 2.6 (3.2) | 17.91 | <0.001 | SD-AN = MD-AN | |||
| MD-AN = LD-AN | |||||||||
| SD-AN < LD-AN | |||||||||
| Use of medications upon admission | 44 (57.9) | 31 (66) | 30 (65.2) | 0.585 a | |||||
| Ineffective therapeutic strategies before admission | |||||||||
| Medications | 14 (18.4)b | 14 (30.4)c | 25 (54.3)c | 0.001 a | |||||
| Psychotherapy | 24 (31.6)b | 27 (57.4)c | 29 (63)c | 0.002 a | |||||
| History of sexual abuse | 4 (5.3) | 6 (12.8) | 6 (13) | 0.212 a | |||||
| Family history of psychiatric disorders | 22 (28.9) | 14 (30.4) | 17 (37) | 0.688 a | |||||
| Family history of eating disorders | 11 (14.5) | 9 (19.1) | 8 (17.4) | 0.805 a | |||||
| History of previous suicide attempts | 13 (17.1) | 13 (27.7) | 10 (21.7) | 0.359 a | |||||
p-value of the Fisher’s exact test.
p-value = 0.066.
The sample included 33.7% diagnosed with major depression, with no differences across groups. Anxiety disorders were present in 9.5% of the sample, with those with LD showing significantly more anxious comorbidity than did those with SD (SD, 5.3%; MD, 6.4%; LD, 19.6%; p = 0.030).
Eating and general psychopathology, stages of change, and QOL
For eating and general psychopathology, the three groups differed only on the EDI-2 bulimia subscale, with the SD group reporting the lowest scores. No differences emerged for anxiety and depression, self-esteem, AN stages of change, and QOL (Table 2).
Table 2.
Eating and general psychopathology, stages of change, and quality of life across groups of patients with anorexia nervosa (AN) showing short, medium, or long duration of illness.
| Total sample inpatients with AN n = 169 | ||||||
|---|---|---|---|---|---|---|
| <3 years | ≥3 and <7 years | ≥7 years | Test statistics | |||
| Short duration (SD-AN) n = 76 | Medium duration (MD-AN) n = 47 | Long duration (LD-AN) n = 46 | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | F | p | Sheffè post hoc | |
| EDI-2 | ||||||
| Drive for thinness | 12.8 (7.9) | 10.8 (7.9) | 11.4 (7.9) | 0.86 | 0.426 | – |
| Bulimia | 2.2 (3.5) | 3.3 (4.9) | 5.1 (6.6) | 4.2 | 0.017 | SD-AN = MD-AN |
| MD-AN = LD-AN | ||||||
| SD-AN < LD-AN | ||||||
| Body dissatisfaction | 13.7 (6.7) | 13.4 (6.9) | 14.5 (7) | 0.29 | 0.75 | – |
| EDE-Q | ||||||
| Restraint | 3.3 (1.9) | 2.7 (2) | 3.1 (2.2) | 0.91 | 0.407 | – |
| Eating concern | 3.1 (1.5) | 2.7 (1.6) | 2.7 (1.9) | 0.81 | 0.447 | – |
| Shape concern | 3.9 (1.7) | 4.1 (1.7) | 3.7 (1.8) | 0.54 | 0.585 | – |
| Weight concern | 3.5 (1.8) | 5.6 (1.6) | 3.2 (1.9) | 0.37 | 0.694 | – |
| Total | 3.4 (1.6) | 3.2 (1.6) | 3.2 (1.8) | 0.38 | 0.68 | – |
| BSQ | 102 (43.7) | 113.6 (42.7) | 113.3 (54.1) | 0.35 | 0.702 | – |
| STAI | ||||||
| State | 54.3 (14.8) | 53.7 (13.9) | 54.4 (13.7) | 0.03 | 0.968 | – |
| Trait | 55.9 (15.3) | 58.6 (11.4) | 59.7 (11.9) | 1.1 | 0.338 | – |
| HAM-A | 19.9 (7.2) | 17.8 (6.6) | 18.8 (6.4) | 1.198 | 0.305 | |
| BDI | 16.2 (8.4) | 16.8 (7.3) | 15.2 (8.1) | 0.39 | 0.681 | – |
| HAM-D | 20.3 (7.4) | 18.5 (7.5) | 17.7 (7.5) | 1.718 | 0.183 | |
| ANSOCQ | 2.6 (0.9) | 2.7 (0.7) | 2.6 (0.8) | 0.24 | 0.788 | – |
| EQ-5D | ||||||
| Index | 0.4 (0.5) | 0.5 (0.4) | 0.4 (0.6) | 0.46 | 0.630 | – |
| EQ5D-VAS | 53.9 (24.7) | 46.7 (20.1) | 44.8 (24.6) | 2.1 | 0.132 | – |
Abbreviations: ANSOCQ, Anorexia Nervosa Stages of Change Questionnaire; BDI, Beck Depression Inventory; BSQ, Body Shape Questionnaire; EDE-Q, Eating Disorders Examination-Questionnaire; EDI-2, Eating Disorder Inventory-2; EQ-5D, EuroQoL Health Questionnaire/Visual Analogue Scale; HAM-A, Hamilton Anxiety Rating Scale; HAM-D, Hamilton Depression Rating Scale; STAI, State Trait Anxiety Inventory.
Personality and premorbid traits
All patient groups did not differ in personality and premorbid traits (Table 3).
Table 3.
Personality, temperament, and premorbid traits of patients with short, medium, and long duration of anorexia nervosa (AN).
| Total sample inpatients with AN n = 169 | ||||||
|---|---|---|---|---|---|---|
| <3 years | ≥3 and <7 years | ≥7 years | Test statistics | |||
| Short duration (SD-AN) n = 76 | Medium duration (MD-AN) n = 47 | Long duration (LD-AN) n = 46 | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | F | p | Sheffè post hoc | |
| TEMPS-A | ||||||
| Depressive | 12.2 (4.1) | 12.7 (4.1) | 13.2 (3.8) | 0.74 | 0.480 | – |
| Cyclothymic | 9.9 (4.8) | 9.6 (4.7) | 9.9 (5.1) | 0.01 | 0.916 | – |
| Hyperthymic | 6.9 (3.8) | 6.1 (3.8) | 7.8 (4.7) | 1.7 | 0.187 | – |
| Irritable | 6.7 (3.9) | 7 (3.6) | 7.2 (4.3) | 0.20 | 0.816 | – |
| Anxious | 12.8 (5.4) | 13.8 (5.7) | 13.8 (5.1) | 0.55 | 0.577 | – |
| FMPS | 111.4 (25.8) | 106.6 (27.3) | 110 (26.3) | 0.42 | 0.658 | – |
| CHIRP | ||||||
| Global perfectionism | 2.8 (2.2) | 2.8 (2.2) | 3 (1.9) | 0.08 | 0.919 | – |
| Inflexibility | 3.2 (1.4) | 3.2 (1.4) | 3.1 (1.1) | 0.13 | 0.877 | – |
| Need for order and symmetry | 1.3 (1.5) | 1.2 (1.3) | 1.5 (1.5) | 0.38 | 0.684 | – |
| PCT-Q | ||||||
| Harm avoidance | 4.3 (2.9) | 4.1 (2.7) | 3.8 (3.2) | 0.42 | 0.657 | – |
| Alexithymia | 2.5 (2.3) | 2.9 (2.6) | 2.3 (2.3) | 0.78 | 0.460 | – |
| Interoceptive awareness | 2.7 (2.5) | 2.6 (2.4) | 2.5 (2.7) | 0.14 | 0.866 | – |
| Social phobia | 1.8 (1.8) | 2.3 (1.9) | 1.9 (1.9) | 1.11 | 0.330 | – |
| Food obsessions | 0.8 (1.2) | 1 (1.3) | 1.3 (1.6) | 1.85 | 0.159 | – |
Abbreviations: CHIRP, Childhood Retrospective Perfectionism Questionnaire; FMPS, Frost Multidimensional Perfectionism Scale; PCT-Q, Premorbid Childhood Traits Questionnaire; TEMPS-A, Temperament Evaluation of Memphis, Pisa, Paris, and San Diego Autoquestionnaire.
Clinical outcomes of hospitalization
The mean duration of hospitalization was 35.8 ± 17.1 days, with no differences across the groups (F = 2.03; p = 0.13), and all patients significantly improved after hospitalization on all measures except the EDI-2 body dissatisfaction subscale (Table 4).
Table 4.
Outcome of hospitalization of patients with short, medium, and long duration of anorexia nervosa (AN).
| Total sample inpatients with AN n = 169 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <3 years | ≥3 and <7 years | ≥7 years | Test statistics | ||||||||||||
| Short duration (SD-AN) n = 76 | Medium duration (MD-AN) n = 47 | Long duration (LD-AN) n = 46 | Main effect of group | Main effect of time | Time × group effect | ||||||||||
| T0 | EOT | T0 | EOT | T0 | EOT | F | p | η 2 | F | p | η 2 | F | p | η 2 | |
| BMI | 14.4 (1.9) | 15.1 (1.6) | 14.4 (1.7) | 15.1 (1.6) | 14.3 (2.1) | 15.1 (2.1) | 0.008 | 0.992 | <0.001 | 124.53 | <0.001 | 0.436 | 0.12 | 0.888 | 0.001 |
| EDE-Q total score | 3.4 (1.6) | 2.9 (1.6) | 3.4 (1.6) | 2.3 (1.5) | 3.2 (1.8) | 2.5 (1.7) | 0.47 | 0.623 | 0.008 | 58.82 | <0.001 | 0.327 | 2.8 | 0.065 | 0.044 |
| EDI-2 | |||||||||||||||
| DT | 13 (7.8) | 13.2 (7.6) | 11.6 (8) | 9.2 (7.8) | 11 (8) | 10.4 (8.2) | 1.6 | 2.1 | 0.027 | 5.1 | 0.026 | 0.043 | 3.5 | 0.034 | 0.059 |
| B | 2.2 (3.5) | 1.4 (2.6) | 3.7 (5) | 1.8 (3.7) | 4.7 (6.3) | 2.3 (3.2) | 2.2 | 0.113 | 0.038 | 28.42 | <0.001 | 0.202 | 2.7 | 0.073 | 0.046 |
| BD | 14 (7.5) | 14.6 (7.6) | 13.5 (7) | 12.8 (6.4) | 14.4 (6.8) | 12.6 (7.1) | 0.319 | 0.728 | 0.006 | 2.43 | 0.122 | 0.021 | 3.48 | 0.034 | 0.059 |
| BDI | 15.9 (8.5) | 11.5 (7.7) | 15.8 (7.3) | 8.8 (6.8) | 14.5 (8.2) | 11.5 (9.1) | 0.38 | 0.685 | 0.006 | 55.5 | <0.001 | 0.322 | 2.9 | 0.60 | 0.047 |
| STAI-state | 54.9 (15.2) | 52.4 (15.5) | 53.7 (14.2) | 47.2 (15.4) | 55.1 (13.5) | 51.8 (14.4) | 0.614 | 0.543 | 0.010 | 13.55 | <0.001 | 0.101 | 1.3 | 0.284 | 0.021 |
| BSQ | 119 (46.7) | 117.5 (47.2) | 114.6 (42.3) | 94.3 (41.1) | 110.5 (52.9) | 102.3 (45.6) | 1.13 | 0.327 | 0.021 | 15.9 | <0.001 | 0.129 | 4.9 | 0.009 | 0.084 |
| EQ-5D | |||||||||||||||
| INDEX | 0.42 (0.53) | 0.65 (0.25) | 0.54 (0.41) | 0.69 (0.34) | 0.43 (0.66) | 0.6 (0.28) | 0.66 | 0.517 | 0.012 | 14.88 | <0.001 | 0.121 | 0.33 | 0.717 | 0.006 |
| VAS | 53.5 (26) | 67.2 (19.8) | 51.7 (17.2) | 55.4 (24.8) | 45.7 (23.3) | 57.3 (21.8) | 2.2 | 0.119 | 0.043 | 14.97 | <0.001 | 0.134 | 1.5 | 0.230 | 0.030 |
| HAM-A | 19.9 (7.3) | 15.4 (6.9) | 17.9 (6.7) | 14.2 (6.1) | 19 (6.1) | 12.7 (6.1) | 1.4 | 0.248 | 0.019 | 102.47 | <0.001 | 0.414 | 2.2 | 0.116 | 0.029 |
| HAM-D | 20.3 (7.5) | 14.4 (6.8) | 18.9 (7.1) | 13.8 (6.9) | 17.9 (7) | 13.6 (6.6) | 1.9 | 0.156 | 0.025 | 143.83 | <0.001 | 0.498 | 0.4 | 0.673 | 0.005 |
Abbreviations: B, bulimia; BD, body dissatisfaction; BDI, Beck Depression Inventory; BMI, Body Mass Index; BSQ, Body Shape Questionnaire; DT, drive for thinness; EDE-Q, Eating Disorders Examination-Questionnaire; EDI-2, Eating Disorder Inventory-2; EQ-5D/VAS, EuroQoL Health Questionnaire/Visual Analogue Scale; HAM-A, Hamilton Rating Scale for Anxiety; HAM-D, Hamilton Depression Rating Scale; STAI, State Trait Anxiety Inventory.
The three groups did not differ at baseline but showed different trajectories for drive for thinness and body dissatisfaction subscales of the EDI-2 and for body shape concerns on the BSQ. Those with SD improved poorly on the aforementioned parameters (see Figure 1). In contrast, no differences emerged across groups during hospitalization with respect to BMI, EDE-Q total score, EDI-2 bulimia subscale, depressive and anxiety symptoms (self-reported or interview-based), and QOL (Table 4).
Figure 1.
Trajectory of change during ehospitalization between admission (T0) and end of treatment (EOT) for patients with short (SD-AN: <3 years), medium (MD-AN: 3–6.99 years), and long (LD-AN: ≥7 years) duration of anorexia nervosa with respect to: (A) drive for thinness (as measured by the Eating Disorders Inventory-2); (B) body dissatisfaction (as measured by the Eating Disorders Inventory-2); and (C) body shape concerns (as measured by the Body Shape Questionnaire).
Also, all three groups did not differ in therapeutic alliance at EOT (WAI-SR total SD, 67.4 ± 13.5; MD, 67.9 ± 12.9; LD, 70.8 ± 11.4; F = 0.76; p = 0.47).
When discharged, the groups did not differ in their stepping-down plans (p = 0.395; see Supplementary Material). Only three patients required a switch from voluntary to involuntary care.
Discussion
Given the cogent need for a common definition of SE-AN to optimize treatment, we thoroughly compared patients with different AN durations to ascertain “profiles” of illness and hospitalization outcomes. After grouping patients according to their DOI, two main findings emerged. First, few differences were found across groups. Those with ≥7 years of AN were older, diagnosed mostly with AN-BP, and failed a higher number of AN-related treatments. Furthermore, those with a longer DOI reported a lower lifetime BMI and a trend toward a younger age at onset. Second, all patients responded equally well to the hospitalization; notably, patients with <3 years of AN improved less in drive for thinness and body-related concerns. Different from our a priori hypothesis, these novel and somehow unexpected findings show that DOI is an inadequate specifier for AN.
Patients’ current BMI was comparable across groups with different DOI, in line with previous research on outpatients [8,9], questioning a correlation between enduringness and severity of symptoms. Those with longer DOI (MD and LD) were diagnosed more frequently with BP-AN. However, patients’ phenotype cannot be an early severity index, since literature shows that many of those currently diagnosed with BP-AN tend to report a diagnostic cross-over from R-AN to BP-AN [37]. Also, patients with LD reported a trend toward a younger onset of AN; however, this finding did not survive post hoc correction so, although interesting, further studies are needed to confirm this result. In contrast with current BMI, participants’ lifetime BMI was lowest for those with LD when compared to those with SD. Therefore, despite current BMI, clinical and research attention should be paid to patients reaching a very low weight; in fact, duration and degree of severity of extreme emaciation during the course of AN should be investigated more. However, lowest lifetime BMI could be a time-dependent variable. In fact, as it is well-known that low weight is an unfavorable prognostic factor [38] our data highlight the relevance of working hard in treatment to avoid extremely low weights, as suggested by other data on evidence-based treatments for eating disorders [7].
Our data showed that all groups failed earlier interventions and, in keeping with other research showing patients with longer DOI as being frequent utilizers of the health care system [39] those with LD reported a higher number of previous hospitalizations. Furthermore, both MD and LD groups had greater therapeutic attempts using both medications and psychotherapy. Therefore, this finding adds to earlier literature a more detailed characterization of the failure of previous treatments. In fact, our data show not only that patients sought treatments on multiple occasions but also that they were offered (and then failed) these recommended treatments [35]. However, it should be borne in mind that the differences in health care systems across countries (i.e., availability of specialized centers, economic or insurance barriers) may affect these issues.
Interestingly, no differences in the severity of eating psychopathology emerged across groups, except for the bulimia subscale scores on the EDI-2, which were higher in those with a longer DOI who were also more frequently diagnosed with AN-BP. To this end, our findings are in line with earlier data on inpatients [7] while data on outpatients yields a contrasting result [9]. However, the same nonsignificant trend emerged also for anxiety and depressive symptomatology, in keeping with former studies [7,9]. This interesting finding fulfills a gap in the literature because we conducted a broad (i.e., clinician-based) assessment. Therefore, the current AN acute phase could level patients’ scores, and also a state-independent perspective could be adopted. In fact, depressive and anxious traits are putative vulnerability factors in AN [40,41] and may be independent of DOI. In line with earlier data [4] in our study those with LD showed a higher comorbidity profile; however, we confirmed this trend only for anxiety disorders. Given recent research on this topic [42], also comorbidity may be explored in the debate on specifiers in AN.
QOL is known to be severely impaired in inpatients with AN [43] and also has been proposed as potentially discriminating SE-AN [8,9]. Interestingly, our data do not seem to support the aforementioned findings, but a relevant caveat exists: Our sample was composed of patients in an acute phase of the disorder, so this characteristic may be similar for all patients independent of their clinical history. Moreover, different assessments may yield incomparable results.
We also designed this study to investigate stages of change and premorbid traits in SE-AN, which are important and emaciation-independent aspects. The former refers to the Stages of Change Model proposed by Prochaska and DiClemente [44] and assesses how prone patients with AN are to change various aspects of their symptomatology, entailing precontemplation, contemplation, preparation, action, or maintenance stages. The questionnaire on premorbid traits [33] investigated harm avoidance, social phobia, alexithymia, interoceptive awareness, and food obsessions as they appeared before the onset of AN. In line with the overall lack of differences across groups found in this study, the patients did not report differences in their AN stages of change, as also reported earlier [45]. Given the design of our study, we cannot rule out that patients fluidly shift into different stages of change according to their phase of AN; however, these data seem to indicate that acutely ill patients show similar stages of change.
In addition, as has been suggested previously [46], we focused on the analysis of premorbid characteristics but no temperament traits or premorbid conditions (including inflexibility and interoceptive awareness) differed across groups, suggesting the difficulty of early identification of individuals potentially at risk for developing SE-AN. This is even more true if we consider that groups did not differ in familiarity with psychiatric disorders, history of sexual abuse, and suicide attempts. Therefore, future research might shift focus from vulnerability factors to resilience skills.
Interestingly, our findings also suggest that patients with a longer DOI can respond equally well to acute treatments when anxiety, depression, and body-related concerns are included as outcomes. Follow-up data are needed to complete this picture; however, this finding is important because, in some countries, a label of SE-AN could hamper treatment delivery for patients [4] who could, according to our data, respond well (at least as much as could those with a shorter DOI) to intensive treatment. Furthermore, this data could illuminate how responsive those with a longer DOI can be to structured and short-term treatments, as other research has suggested [4,19]. In keeping with earlier research from our group [47] patients with LD showed a therapeutic alliance comparable to that of the younger ones. Interestingly, those with a shorter DOI improved less in the drive for thinness and body shape concerns, mirroring a network analysis showing patients with a shorter DOI reporting overvaluation of weight or shape as key elements [48].
Altogether, our data suggest that patients with a longer DOI were not “simply” more severe than were patients with a shorter history of AN. In agreement with studies advocating a broader investigation of patients with AN [9,16], we assessed a wide spectrum of dimensions, but still no differences emerged. In fact, DOI, psychometric assessments, and failure of previous treatments did not seem to sufficiently differentiate AN severity. Possibly, a clinimetric approach [49] may be required to make a shift from psychometric tests and “clinical wisdom” [50] to a more individualized and fine-grained evaluation. We hypothesize that clinicians may catch nuances that psychometric tests do not fully capture, eventually in line with other fields of medicine (e.g., Apgar scores are clinician based). Still, we raise the possibility that biologically informed measures may become available in the future era of precision psychiatry [51].
This study has some strengths, including the use of validated and widely applied self-report and interview-based assessments. However, some limitations exist. The sample was composed of inpatients in an acute phase of AN (thus eventually contributing to the lack of differences in symptom severity), and we applied a cross-sectional design. Taken together, findings from this study support the need for other “empirical tests to clarify the best-defining features of SE-AN” [5], eventually informed by the clinimetric approach. Notwithstanding, should these data be confirmed by larger studies, some clinical implications could be surmised, because we did not find “enduringness” to be a specifier of severity. Moreover, the effectiveness of hospitalization for patients with longer DOI was supported, while specific interventions on the core cognitive aspects of over-evaluation of body shape could be offered to patients with a shorter DOI.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/j.eurpsy.2021.2218.
click here to view supplementary material
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that there are no conflicts of interest.
Data Availability Statement
Data are not publicly available.
References
- [1]. Eddy KT, Tabri N, Thomas JJ, Murray HB, Keshaviah A, Hastings E, et al. Recovery from anorexia nervosa and bulimia nervosa at 22-year follow-up. J Clin Psychiatry. 2017;78:184–9. doi: 10.4088/JCP.15m10393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. Abbate-Daga G, Amianto F, Delsedime N, De-Bacco C, Fassino S. Resistance to treatment in eating disorders: a critical challenge. BMC Psychiatry. 2013;13:282. doi: 10.1186/1471-244X-13-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Treasure J, Willmott D, Ambwani S, Cardi V, Clark Bryan D, Rowlands K, et al. Cognitive interpersonal model for anorexia nervosa revisited: the perpetuating factors that contribute to the development of the severe and enduring illness. J Clin Med. 2020;9:630. doi: 10.3390/jcm9030630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Wonderlich SA, Bulik CM, Schmidt U, Steiger H, Hoek HW. Severe and enduring anorexia nervosa: update and observations about the current clinical reality. Int J Eat Disord. 2020;53:1303–12. doi: 10.1002/eat.23283. [DOI] [PubMed] [Google Scholar]
- [5]. Hay P, Touyz S. Classification challenges in the field of eating disorders: Can severe and enduring anorexia nervosa be better defined? J Eat Disord. 2018;6:41. doi: 10.1186/s40337-018-0229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Abbate-Daga G, Marzola E, De-Bacco C, Buzzichelli S, Brustolin A, Campisi S, et al. Day hospital treatment for anorexia nervosa: a 12-month follow-up study. Eur Eat Disord Rev. 2015;23:390–8. doi: 10.1002/erv.2369. [DOI] [PubMed] [Google Scholar]
- [7]. Calugi S, el Ghoch M, Dalle Grave R. Intensive enhanced cognitive behavioural therapy for severe and enduring anorexia nervosa: a longitudinal outcome study. Behav Res Ther. 2017;89:41–8. doi: 10.1016/j.brat.2016.11.006. [DOI] [PubMed] [Google Scholar]
- [8]. Wildes JE, Forbush KT, Hagan KE, Marcus MD, Attia E, Gianini LM, et al. Characterizing severe and enduring anorexia nervosa: an empirical approach. Int J Eat Disord. 2017;50:389–97. doi: 10.1002/eat.22651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Ambwani S, Cardi V, Albano G, Cao L, Crosby RD, Macdonald P, et al. A multicenter audit of outpatient care for adult anorexia nervosa: symptom trajectory, service use, and evidence in support of “early stage” versus “severe and enduring” classification. Int J Eat Disord. 2020;53:1337–48. doi: 10.1002/eat.23246. [DOI] [PubMed] [Google Scholar]
- [10]. van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of slife, and family burden. Curr Opin Psychiatry. 2020;33:521–7. doi: 10.1097/YCO.0000000000000641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. Broomfield C, Stedal K, Touyz S, Rhodes P. Labeling and defining severe and enduring anorexia nervosa: a systematic review and critical analysis. Int J Eat Disord. 2017;50:611–23. doi: 10.1002/eat.22715. [DOI] [PubMed] [Google Scholar]
- [12]. Andries A, Frystyk J, Flyvbjerg A, Støving RK. Dronabinol in severe, enduring anorexia nervosa: a randomized controlled trial. Int J Eat Disord. 2014;47:18–23. doi: 10.1002/eat.22173. [DOI] [PubMed] [Google Scholar]
- [13]. Gaudiani JL, Brinton JT, Sabel AL, Rylander M, Catanach B, Mehler PS. Medical outcomes for adults hospitalized with severe anorexia nervosa: an analysis by age group. Int J Eat Disord. 2016;49:378–85. doi: 10.1002/eat.22437. [DOI] [PubMed] [Google Scholar]
- [14]. Calugi S, Dalle Grave R, Marchesini G. Longstanding underweight eating disorder: associated features and treatment outcome. Psychother Res. 2013;23:315–23. doi: 10.1080/10503307.2012.717308. [DOI] [PubMed] [Google Scholar]
- [15]. Robinson PH, Kukucska R, Guidetti G, Leavey G. Severe and enduring anorexia nervosa (SEED-AN): a qualitative study of patients with 20+ years of anorexia nervosa. Eur Eat Disord Rev. 2015;23:318–. doi: 10.1002/erv.2367. [DOI] [PubMed] [Google Scholar]
- [16]. Murray SB, Loeb KL, le Grange D. Treatment outcome reporting in anorexia nervosa: Time for a paradigm shift? J Eat Disord. 2018;6:10. doi: 10.1186/s40337-018-0195-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17]. Kaplan A, Buchnan S. Is there a role for palliative care in the management of treatment resistant chronic anorexia nervosa? The international conference on eating disorders, Austin, TX; 2012. [Google Scholar]
- [18]. Dalton B, Foerde K, Bartholdy S, McClelland J, Kekic M, Grycuk L, et al. The effect of repetitive transcranial magnetic stimulation on food choice-related self-control in patients with severe, enduring anorexia nervosa. Int J Eat Disord. 2020;53:1326–36. doi: 10.1002/eat.23267. [DOI] [PubMed] [Google Scholar]
- [19]. Guarda AS, Wonderlich S, Kaye W, Attia E. A path to defining excellence in intensive treatment for eating disorders. Int J Eat Disord. 2018;51:1051–5. doi: 10.1002/eat.22899. [DOI] [PubMed] [Google Scholar]
- [20]. American Psychiatric Association. DSM-5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- [21]. Rizzardi M, Trombini E, Trombini G. Manuale EDI-2. Florence, Italy: O.S. Organizzazioni Speciali; 1995. [Google Scholar]
- [22]. Calugi S, Milanese C, Sartirana M, el Ghoch M, Sartori F, Geccherle E, et al. The eating disorder examination questionnaire: reliability and validity of the Italian version. Eat Weight Disord. 2017;22:509–14. doi: 10.1007/s40519-016-0276-6. [DOI] [PubMed] [Google Scholar]
- [23]. Cooper P, Taylor M, Cooper Z, & Fairburn CG. The development and validation of the Body Shape Questionnaire. International Journal of Eating Disorders. 1987;6:485–494. [Google Scholar]
- [24]. Lazzari R, Pancheri P. Questionario di Valutazione dellAnsia di Stato e di Tratto. Florence, Italy: Organizzazioni Speciali; 1980. [Google Scholar]
- [25]. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- [26]. Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- [27]. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28]. EuroQol Group. EuroQol – a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- [29]. Rieger E, Touyz S, Schotte D, Beumont P, Russell J, Clarke S, et al. Development of an instrument to assess readiness to recover in anorexia nervosa. Int J Eat Disord. 2000;28:387–96. doi:. [DOI] [PubMed] [Google Scholar]
- [30]. Pompili M, Girardi P, Tatarelli R, Iliceto P, de Pisa E, Tondo L, et al. TEMPS-A (Rome): psychometric validation of affective temperaments in clinically well subjects in mid- and South Italy. J Affect Disord. 2008;107:63–75. doi: 10.1016/j.jad.2007.07.031. [DOI] [PubMed] [Google Scholar]
- [31]. Frost RO, Marten P, Lahart C, Rosenblate R. The dimensions of perfectionism. Cogn Ther Res. 1990;14:449–68. doi: 10.1007/BF01172967. [DOI] [Google Scholar]
- [32]. Southgate L, Tchanturia K, Collier D, Treasure J. The development of the childhood retrospective perfectionism questionnaire (CHIRP) in an eating disorder sample. Eur Eat Disord Rev. 2008;16:451–62. doi: 10.1002/erv.870. [DOI] [PubMed] [Google Scholar]
- [33]. Marzola E, Fassino S, Migliaretti G, Abbate-Daga G, Kaye WH. Development and validation of the premorbid childhood traits questionnaire (PCT-Q) in eating disorders. Eat Weight Disord. 2019;24:815–23. doi: 10.1007/s40519-019-00748-y. [DOI] [PubMed] [Google Scholar]
- [34]. Hatcher RL, Gillaspy JA. Development and validation of a revised short version of the working alliance inventory. Psychother Res. 2006;16:12–25. doi: 10.1080/10503300500352500. [DOI] [Google Scholar]
- [35]. National Institute for Health and Care Excellence (NICE). Eating disorders: recognition and treatment NICE guideline. London, UK: National Institute for Health and Care Excellence; 2017. [Google Scholar]
- [36]. Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, MI: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- [37]. Castellini G, lo Sauro C, Mannucci E, Ravaldi C, Rotella CM, Faravelli C, et al. Diagnostic crossover and outcome predictors in eating disorders according to DSM-IV and DSM-V proposed criteria: a 6-year follow-up study. Psychosom Med. 2011;73:270–9. doi: 10.1097/PSY.0b013e31820a1838. [DOI] [PubMed] [Google Scholar]
- [38]. Fichter MM, Quadflieg N, Crosby RD, Koch S. Long-term outcome of anorexia nervosa: results from a large clinical longitudinal study. Int J Eat Disord. 2017;50:1018–30. doi: 10.1002/eat.22736. [DOI] [PubMed] [Google Scholar]
- [39]. Hay P, Chinn D, Forbes D, Madden S, Newton R, Sugenor L, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Aust N Z J Psychiatry. 2014;48:977–1008. doi: 10.1177/0004867414555814. [DOI] [PubMed] [Google Scholar]
- [40]. Klump KL, Strober M, Bulik CM, Thornton L, Johnson C, Devlin B, et al. Personality characteristics of women before and after recovery from an eating disorder. Psychol Med. 2004;34:1407–18. doi: 10.1017/S0033291704002442. [DOI] [PubMed] [Google Scholar]
- [41]. Marzola E, Porliod A, Panero M, De-Bacco C, Abbate-Daga G. Affective temperaments and eating psychopathology in anorexia nervosa: Which role for anxious and depressive traits? J Affect Disord. 2020;266:374–80. doi: 10.1016/j.jad.2020.01.142. [DOI] [PubMed] [Google Scholar]
- [42]. van Alsten SC, Duncan AE. Lifetime patterns of comorbidity in eating disorders: an approach using sequence analysis. Eur Eat Disord Rev. 2020;28:709–23. doi: 10.1002/erv.2767. [DOI] [PubMed] [Google Scholar]
- [43]. Abbate-Daga G, Facchini F, Marzola E, Delsedime N, Giovannone C, Amianto F, et al. Health-related quality of life in adult inpatients affected by anorexia nervosa. Eur Eat Disord Rev. 2014;22:285–91. doi: 10.1002/erv.2302. [DOI] [PubMed] [Google Scholar]
- [44]. Prochaska JO, di Clemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychotherapy. 1982;19:276–88. doi: 10.1037/h0088437. [DOI] [Google Scholar]
- [45]. Abd Elbaky GB, Hay PJ, le Grange D, Lacey H, Crosby RD, Touyz S. Pre-treatment predictors of attrition in a randomised controlled trial of psychological therapy for severe and enduring anorexia nervosa. BMC Psychiatry. 2014;14. doi: 10.1186/1471-244X-14-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46]. Kaplan AS, Strober M. Severe and enduring anorexia nervosa: Can risk of persisting illness be identified, and prevented, in young patients? Int J Eat Disord. 2019;52:478–80. doi: 10.1002/eat.23019. [DOI] [PubMed] [Google Scholar]
- [47]. Marzola E, Albini E, Delsedime N, Fassino S, Abbate-Daga G. Therapeutic alliance in inpatients with severe anorexia nervosa. Eur Eat Disord Rev. 2019;27:671–81. doi: 10.1002/erv.2687. [DOI] [PubMed] [Google Scholar]
- [48]. Christian C, Williams BM, Hunt RA, Wong VZ, Ernst SE, Spoor SP, et al. A network investigation of core symptoms and pathways across duration of illness using a comprehensive cognitive-behavioral model of eating-disorder symptoms. Psychol Med. 2021;51:815–24. doi: 10.1017/S0033291719003817. [DOI] [PubMed] [Google Scholar]
- [49]. Fava GA, Carrozzino D, Lindberg L, Tomba E. The clinimetric approach to psychological assessment: a tribute to per Bech, MD (1942–2018). Psychother Psychosom. 2018;87:321–6. doi: 10.1159/000493746. [DOI] [PubMed] [Google Scholar]
- [50]. Zhu J, Yang Y, Touyz S, Park R, Hay P. Psychological treatments for people with severe and enduring anorexia nervosa: a mini review. Front Psych. 2020;11:206. doi: 10.3389/fpsyt.2020.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51]. Passos IC, Ballester P, Rabelo-da-Ponte FD, Kapczinski F. Precision psychiatry: the future is now. Can J Psychiatr. 2021; 24:706743721998044. doi: 10.1177/0706743721998044. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/j.eurpsy.2021.2218.
click here to view supplementary material
Data Availability Statement
Data are not publicly available.