Abstract
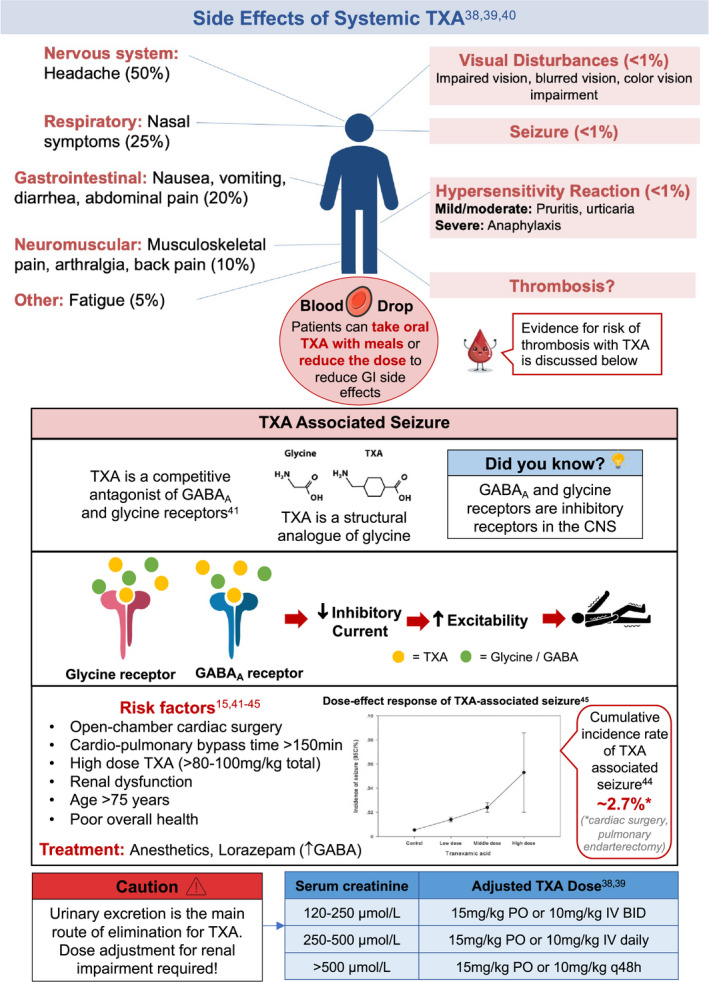
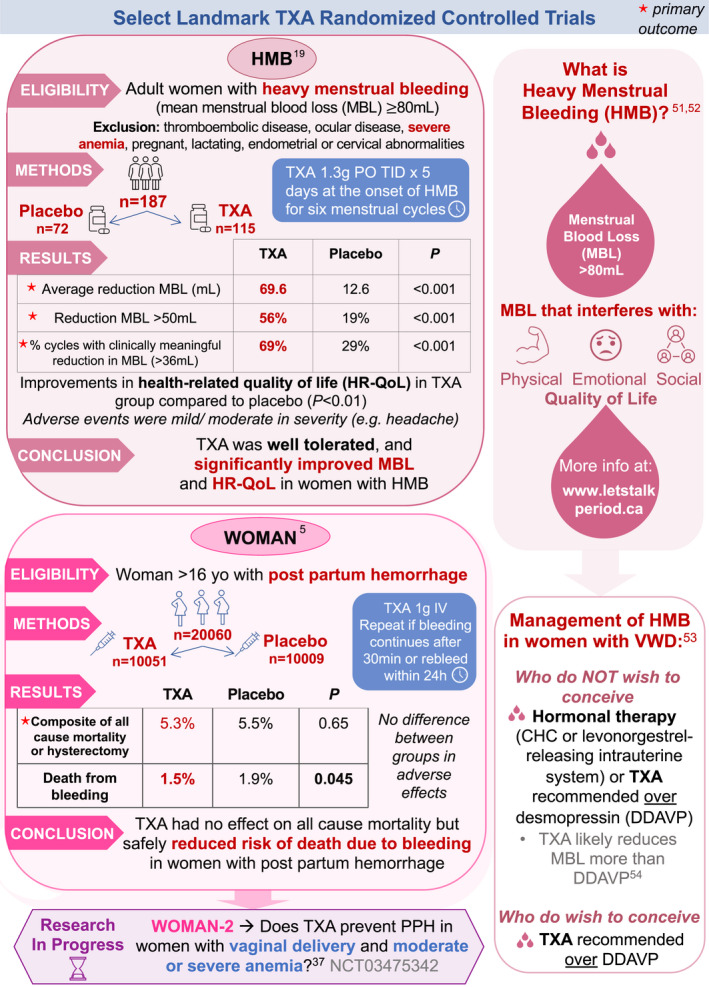
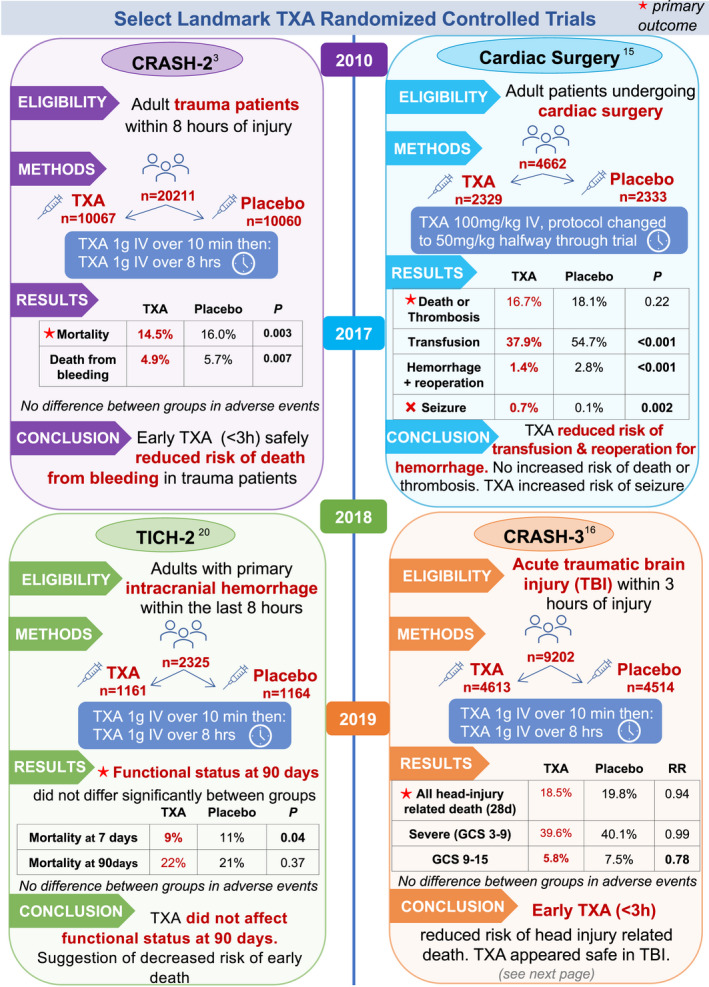
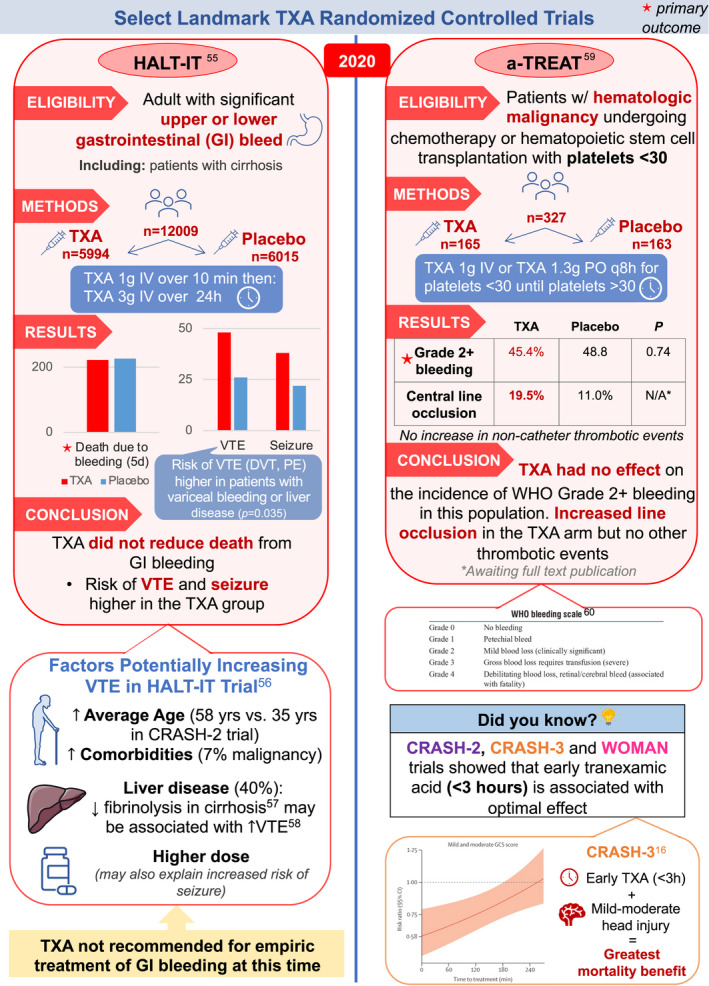
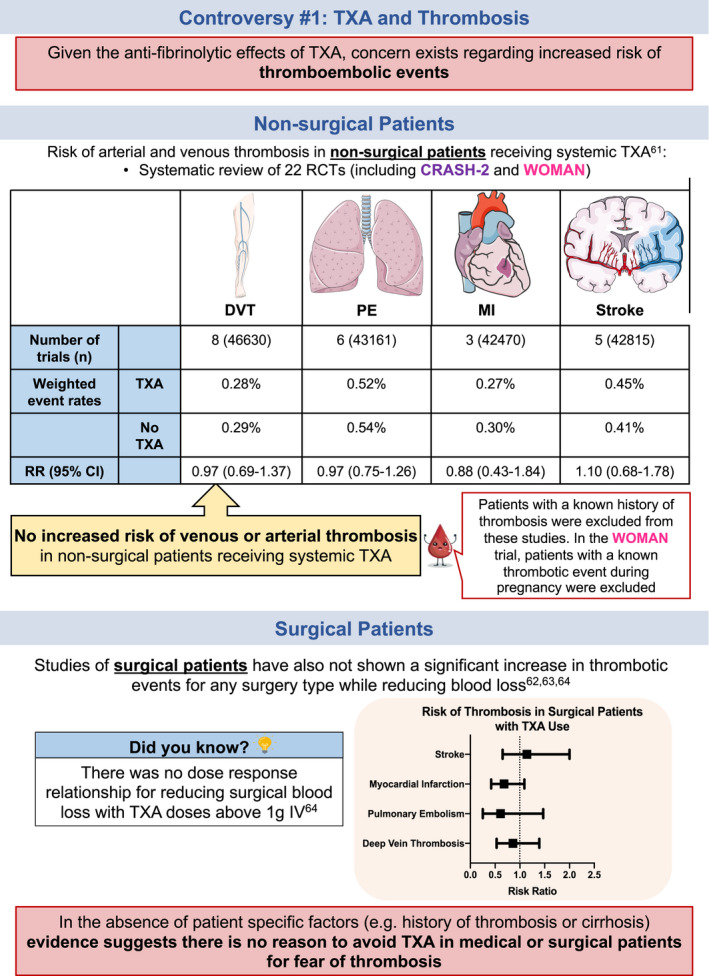
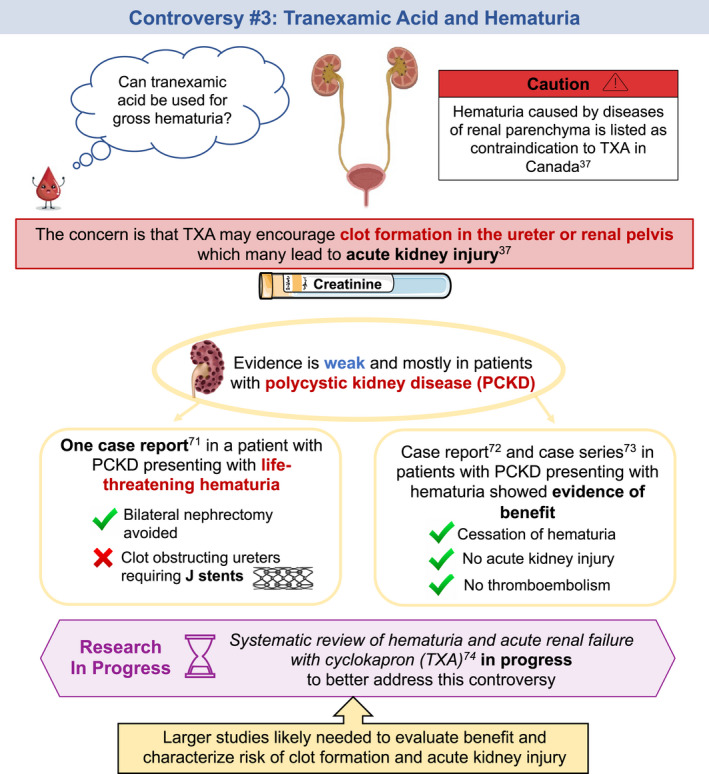
Tranexamic acid (TXA) is an antifibrinolytic agent commonly used for the treatment or prevention of bleeding. Indications for TXA are diverse, including heavy menstrual bleeding, trauma, postpartum hemorrhage, traumatic brain injury, and surgical site bleeding. Despite decades of use and a robust body of evidence, hesitancy using TXA persists in many clinical settings. This illustrated review describes the history, pharmacology, and practical considerations of TXA use. We also describe the major landmark randomized controlled trials of TXA and their implications. Finally, we review the evidence around common controversies surrounding TXA such as the risk of thrombosis, prescription along with combined hormonal contraceptives, and use in patients with gross hematuria.
Keywords: antifibrinolytic agents, blood coagulation, contraceptive agents, thrombosis, tranexamic acid
Essentials.
Tranexamic acid (TXA) decreases the risk of bleeding and often the risk of death from bleeding.
In general, TXA does not increase the risk of blood clots.
Consider shared decision making in patients taking TXA and combined hormonal contraceptives.
It is unknown if TXA causes harm in patients with blood in the urine.
TXA ILLUSTRATED REVIEW
Reference citations 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74





RELATIONSHIP DISCLOSURE
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
NR and MS conceived and designed the manuscript. NR, NLJC, and MS wrote the paper.
ACKNOWLEDGMENTS
Select images in this review were taken from https://smart.servier.com and are licensed under a Creative Commons Attribution 3.0 Unported License. Blood drop image (pages 1, 4‐5, 9‐11) was purchased from shutterstock (stock vector ID: 641207020)
Relke N, Chornenki NLJ, Sholzberg M. Tranexamic acid evidence and controversies: An illustrated review. Res Pract Thromb Haemost. 2021;5:e12546. 10.1002/rth2.12546
Handling Editor: Alisa Wolberg.
Contributor Information
Nicole Relke, Email: nrelke@qmed.ca, @NicoleRelke.
Nicholas L. J. Chornenki, @NicholasJC95.
Michelle Sholzberg, @sholzberg.
REFERENCES
- 1. Watts G. Utako Okamoto (Obituary). Lancet. 2016;387:2286. [DOI] [PubMed] [Google Scholar]
- 2. Okamoto S, Okamoto U. Amino‐methyl‐cyclohexane‐carboxylic acid: AMCHA. A new potent inhibitor of fibrinolysis. Keio J Med. 1962;11:105‐115. [Google Scholar]
- 3. Olldashi F, Kerçi M, Zhurda T, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH‐2): a randomised, placebo‐controlled trial. Lancet. 2010;376:23‐32. [DOI] [PubMed] [Google Scholar]
- 4. WHO Expert Committee . The selection and use of essential medicines (including the 17th WHO model list of essential medicines). WHO Tech Rep Ser [Internet]. 2011;2011:1‐249. [Google Scholar]
- 5. Shakur H, Roberts I, Fawole B, et al. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post‐partum haemorrhage (WOMAN): an international, randomised, double‐blind, placebo‐controlled trial. Lancet. 2017;389:2105‐2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thibault GE. Women in academic medicine. Acad Med. 2016;91:1045‐1046. [DOI] [PubMed] [Google Scholar]
- 7. Mannucci PM. Hemostatic drugs. NEJM. 1998;339;245‐253. [DOI] [PubMed] [Google Scholar]
- 8. Chapin JC, Hajjar KA. Fibrinolysis and the control of blood coagulation. Blood Rev. 2015;29:17‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin H, Xu L, Yu S, Hong W, Huang M, Xu P. Therapeutics targeting the fibrinolytic system. Exp Mol Med. 2020;52:367‐379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Linkins LA, Takach LS. Review of D‐dimer testing: Good, Bad, and Ugly. Int J Lab Hematol. 2017;39:98‐103. [DOI] [PubMed] [Google Scholar]
- 11. Johnson ED, Schell JC, Rodgers GM. The D‐dimer assay. Am J Hematol. 2019;94:833‐839. [DOI] [PubMed] [Google Scholar]
- 12. Tengborn L, Blombäck M, Berntorp E. Tranexamic acid ‐ an old drug still going strong and making a revival. Thromb Res. 2015;135:231‐242. [DOI] [PubMed] [Google Scholar]
- 13. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924‐926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Novikova N, Hofmeyr GJ, Cluver C. Tranexamic acid for preventing postpartum haemorrhage. Cochrane Database Syst Rev. 2015;1‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Myles PS, Smith JA, Forbes A, et al. Tranexamic acid in patients undergoing coronary‐artery surgery. N Engl J Med. 2017;376:136‐148. [DOI] [PubMed] [Google Scholar]
- 16. Collaborators C‐3 trial . Effects of tranexamic acid on death, disability, vascular occlusive events and other morbidities in patients with acute traumatic brain injury (CRASH‐3): a randomised, placebo‐controlled trial. Lancet. 2019;394:1713‐1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ac B, Lethaby A, Farquhar C, Hickey M. Antifibrinolytics for heavy menstrual bleeding (Review). Cochrane Database Syst Rev. 2018;1‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. La S, Warner GT, Cope E. Treatment of menorrhagia with tranexamic acid. a double‐blind trial summary: a double‐blind trial. Br Med J. 1970;4:214‐216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lukes A, Moore K, Muse K, Gersten J. Tranexamic acid treatment for heavy menstrual bleeding. J Obstet Gynecol. 2010;116:865‐867. [DOI] [PubMed] [Google Scholar]
- 20. Sprigg N, Flaherty K, Appleton JP, et al. Tranexamic acid for hyperacute primary IntraCerebral Haemorrhage (TICH‐2): an international randomised, placebo‐controlled, phase 3 superiority trial. The Lancet. 2018;391:2107‐2115. 10.1016/S0140-6736(18)31033-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wand O, Guber E, Guber A, Epstein Shochet G, Israeli‐Shani L, Shitrit D. Inhaled tranexamic acid for hemoptysis treatment. Chest. 2018;154:1379‐1384. 10.1016/j.chest.2018.09.026 [DOI] [PubMed] [Google Scholar]
- 22. Calvo GS, De Granda‐Orive I, Padilla DL. Inhaled tranexamic acid as an alternative for hemoptysis treatment. Chest. 2016;149:604. 10.1016/j.chest.2015.10.016 [DOI] [PubMed] [Google Scholar]
- 23. Kagoma YK, Crowther MA, Douketis J, Bhandari M, Eikelboom J, Lim W. Use of antifibrinolytic therapy to reduce transfusion in patients undergoing orthopedic surgery: a systematic review of randomized trials. Thromb Res. 2009;123:687‐696. [DOI] [PubMed] [Google Scholar]
- 24. Wang Z, Zhang H. Comparative effectiveness and safety of tranexamic acid plus diluted epinephrine to control blood loss during total hip arthroplasty: a meta‐analysis. J Orthop Surg Res. 2018;13:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Morimoto Y, Yoshioka A, Sugimoto M, Imai Y, Kirita T. Haemostatic management of intraoral bleeding in patients with von Willebrand disease. Oral Dis. 2005;11:243‐248. [DOI] [PubMed] [Google Scholar]
- 26. Eghbali A, Melikof L, Taherahmadi H, Bagheri B. Efficacy of tranexamic acid for the prevention of bleeding in patients with von Willebrand disease and Glanzmann thrombasthenia: a controlled, before and after trial. Haemophilia. 2016;22:e423‐e426. [DOI] [PubMed] [Google Scholar]
- 27. Montroy J, Hutton B, Moodley P, et al. The efficacy and safety of topical tranexamic acid: a systematic review and meta‐analysis. Transfus Med Rev. 2018;32:165‐178. [DOI] [PubMed] [Google Scholar]
- 28. Zahed R, Mousavi Jazayeri MH, Naderi A, Naderpour Z, Saeedi M. Topical tranexamic acid compared with anterior nasal packing for treatment of epistaxis in patients taking antiplatelet drugs: randomized controlled trial. Acad Emerg Med. 2018;25:261‐266. [DOI] [PubMed] [Google Scholar]
- 29. Joseph J, Martinez‐Devesa P, Bellorini J, Burton MJ. Tranexamic acid for patients with nasal haemorrhage (epistaxis). Cochrane Database Syst Rev. 2018;2018:1‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Geisthoff UW, Seyfert UT, Kübler M, Bieg B, Plinkert PK, König J. Treatment of epistaxis in hereditary hemorrhagic telangiectasia with tranexamic acid ‐ a double‐blind placebo‐controlled cross‐over phase IIIB study. Thromb Res. 2014;134:565‐571. [DOI] [PubMed] [Google Scholar]
- 31. Shpilberg O, Blumenthal R, Sofer O, et al. A controlled trial of tranexamic acid therapy for the reduction of bleeding during treatment of acute myeloid leukemia. Leuk Lymphoma. 1995;19:141‐144. [DOI] [PubMed] [Google Scholar]
- 32. Avvisati G, Büller HR, Ten CJW, Mandelli F. Tranexamic acid for control of haemorrhage in acute promyelocytic leukaemia. Lancet. 1989;334:122‐124. [DOI] [PubMed] [Google Scholar]
- 33. Kim HJ, Moon SH, Cho SH, Lee JD, Kim HS. Efficacy and safety of tranexamic acid in melasma: a meta‐analysis and systematic review. Acta Derm Venereol. 2017;97:776‐781. [DOI] [PubMed] [Google Scholar]
- 34. Compels MM, Lock RJ. C1 inhibitor deficiency: management. Clin Exp Dermatol. 2005;30:737‐740. [DOI] [PubMed] [Google Scholar]
- 35. Sentilhes L, Winer N, Azria E, et al. Tranexamic acid for the prevention of blood loss after vaginal delivery. N Engl J Med. 2018;379:731‐742. [DOI] [PubMed] [Google Scholar]
- 36. Sentilhes L, Daniel V, Deneux‐Tharaux C. TRAAP2‐TRAnexamic Acid for Preventing postpartum hemorrhage after cesarean delivery: a multicenter randomized, doubleblind, placebo‐controlled trial‐a study protocol. BMC Pregnancy Childbirth. 2020;20:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ker K, Roberts I, Chaudhri R, et al. Tranexamic acid for the prevention of postpartum bleeding in women with anaemia: study protocol for an international, randomised, double‐blind, placebo‐controlled trial. Trials. 2018;19:1‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pfizer Canada . Product Monograph: Cyklokapron [Internet]; 2018. https://www.pfizer.ca/cyklokapron‐tranexamic‐acid (accessed December 16, 2020). [Google Scholar]
- 39. Tranexamic acid. FDA. [Internet]; 2019. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/212020lbl.pdf (accessed January 25, 2021). [Google Scholar]
- 40. Muse K, Lukes AS, Gersten J, Waldbaum A, Mabey RG, Trott E. Long‐term evaluation of safety and health‐related quality of life in women with heavy menstrual bleeding treated with oral tranexamic acid. Women’s Heal. 2011;7:699‐707. [DOI] [PubMed] [Google Scholar]
- 41. Lecker I, Wang DS, Whissell PD, Avramescu S, Mazer CD, Orser BA. Tranexamic acid‐associated seizures: causes and treatment. Ann Neurol. 2016;79:18‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gofton TE, Chu MWA, Norton L, et al. A prospective observational study of seizures after cardiac surgery using continuous EEG monitoring. Neurocrit Care. 2014;21:220‐227. [DOI] [PubMed] [Google Scholar]
- 43. Manji RA, Grocott HP, Leake J, et al. Seizures following cardiac surgery: the impact of tranexamic acid and other risk factors. Can J Anesth. 2012;59:6‐13. [DOI] [PubMed] [Google Scholar]
- 44. Kalavrouziotis D, Voisine P, Mohammadi S, Dionne S, Dagenais F. High‐dose tranexamic acid is an independent predictor of early seizure after cardiopulmonary bypass. Ann Thorac Surg [Internet]. 2012;93:148‐154. 10.1016/j.athoracsur.2011.07.085 [DOI] [PubMed] [Google Scholar]
- 45. Lin Z, Xiaoyi Z. Tranexamic acid‐associated seizures: a meta‐analysis. Seizure [Internet]. 2016;36:70‐73. 10.1016/j.seizure.2016.02.011 [DOI] [PubMed] [Google Scholar]
- 46. Baharoglu MI, Germans MR, Rinkel GJE, et al. Antifibrinolytic therapy for aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev. 2013;2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Imbesi S, Nettis E, Minciullo PL, et al. Hypersensitivity to tranexamic acid: a wide spectrum of adverse reactions. Pharm World Sci. 2010;32:416‐419. [DOI] [PubMed] [Google Scholar]
- 48. Li PH, Trigg C, Rutkowski R, Rutkowski K. Anaphylaxis to tranexamic acid—a rare reaction to a common drug. J Allergy Clin Immunol Pract [Internet]. 2017;5:839‐841. 10.1016/j.jaip.2016.12.014 [DOI] [PubMed] [Google Scholar]
- 49. Connolly ES, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012;43:1711‐1737. [DOI] [PubMed] [Google Scholar]
- 50. Post R, Germans MR, Tjerkstra MA, et al. Ultra‐early tranexamic acid after subarachnoid haemorrhage (ULTRA): a randomised controlled trial. Lancet. 2020;6736:1‐7. [DOI] [PubMed] [Google Scholar]
- 51. Hallberg L, Högdahl AM, Nilsson L, Rybo G. Menstrual blood loss—a population study. Variation at different ages and attempts to define normality. Obstet Gynecol Surv. 1967;22:653‐654. [DOI] [PubMed] [Google Scholar]
- 52. Heavy menstrual bleeding clinical guideline 2007. National Collaborating Centre for Women’s and Children’s Health. NICE; 2007. [Google Scholar]
- 53. Connell NT, Flood VH, Brignardello‐Petersen R, et al. ASH ISTH NHF WFH 2021 guidelines on the management of von Willebrand disease. Blood Adv. 2021;5:301‐325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kouides PA, Byams VR, Philipp CS, et al. Multisite management study of menorrhagia with abnormal laboratory haemostasis: a prospective crossover study of intranasal desmopressin and oral tranexamic acid. Br J Haematol. 2009;145:212‐220. [DOI] [PubMed] [Google Scholar]
- 55. Roberts I, Shakur‐Still H, Afolabi A, et al. Effects of a high‐dose 24‐h infusion of tranexamic acid on death and thromboembolic events in patients with acute gastrointestinal bleeding (HALT‐IT): an international randomised, double‐blind, placebo‐controlled trial. Lancet. 2020;395:1927‐1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Roberts LN. Tranexamic acid in acute gastrointestinal bleeding – a cautionary tale. J Thromb Haemost. 2020;18:2440‐2443. [DOI] [PubMed] [Google Scholar]
- 57. Blasi A, Patel VC, Adelmeijer J, et al. Mixed fibrinolytic phenotypes in decompensated cirrhosis and acute‐on‐chronic liver failure with hypofibrinolysis in those with complications and poor survival. Hepatology. 2020;71:1381‐1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lisman T, De Groot PG, Meijers JCM, Rosendaal FR. Reduced plasma fibrinolytic potential is a risk factor for venous thrombosis. Blood. 2005;105:1102‐1105. [DOI] [PubMed] [Google Scholar]
- 59. Gernsheimer T, Brown SP, Triulzi DJ, et al. Effects of tranexamic acid prophylaxis on bleeding outcomes in hematologic malignancy: the a‐TREAT trial. Blood. 2020;136:1‐2.32430499 [Google Scholar]
- 60. Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer. 1981;47:207‐214. [DOI] [PubMed] [Google Scholar]
- 61. Chornenki NLJ, Um KJ, Mendoza PA, et al. Risk of venous and arterial thrombosis in non‐surgical patients receiving systemic tranexamic acid: a systematic review and meta‐analysis. Thromb Res [Internet]. 2019;179:81‐86. 10.1016/j.thromres.2019.05.003 [DOI] [PubMed] [Google Scholar]
- 62. Taeuber I, Weibel S, Herrmann E, et al. Association of intravenous tranexamic acid with thromboembolic events and mortality. A systematic review, meta‐analysis, and meta‐regression . JAMA Surg. 2021;156;1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ker K, Edwards P, Perel P, Shakur H, Roberts I. Effect of tranexamic acid on surgical bleeding: systematic review and cumulative meta‐analysis. BMJ. 2012;344:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ker K, Prieto‐Merino D, Roberts I. Systematic review, meta‐analysis and meta‐regression of the effect of tranexamic acid on surgical blood loss. Br J Surg. 2013;100:1271‐1279. [DOI] [PubMed] [Google Scholar]
- 65. Thorne JG, James PD, Reid RL. Heavy menstrual bleeding: is tranexamic acid a safe adjunct to combined hormonal contraception? Contraception [Internet]. 2018;98:1‐3. 10.1016/j.contraception.2018.02.008 [DOI] [PubMed] [Google Scholar]
- 66. Heinemann LAJ, Dinger JC. Range of published estimates of venous thromboembolism incidence in young women. Contraception. 2007;75:328‐336. [DOI] [PubMed] [Google Scholar]
- 67. Reid RL, Westhoff C, Mansour D, et al. Oral contraceptives and venous thromboembolism: consensus opinion from an international workshop held in Berlin, Germany in December 2009. J Fam Plan Reprod Heal Care. 2010;36:117‐122. [DOI] [PubMed] [Google Scholar]
- 68. Iacobellis G, Iacobellis G. Combined treatment with tranexamic acid and oral contraceptive pill causes coronary ulcerated plaque and acute myocardial infarction. Cardiovasc Drugs Ther. 2004;18:239‐240. [DOI] [PubMed] [Google Scholar]
- 69. Klok FA, Schreiber K, Stach K, et al. Oral contraception and menstrual bleeding during treatment of venous thromboembolism: expert opinion versus current practice. Thromb Res. 2017;153:101‐107. [DOI] [PubMed] [Google Scholar]
- 70. Meschino D, Sholzberg M. Evaluating the combined effect of anti‐fibrinolytics and estrogen on the risk of thromboembolism: a scoping review. Available from: osf.io/edj28
- 71. Vujkovac B, Sabovic M. A successful treatment of life‐threatening bleeding from polycystic kidneys with antifibrinolytic agent tranexamic acid. Blood Coagul Fibrinolysis. 2006;17:589‐591. [DOI] [PubMed] [Google Scholar]
- 72. AlAmeel T, West M. Tranexamic acid treatment of life‐threatening hematuria in polycystic kidney disease. Int J Nephrol. 2011;2011:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Peces R, Aguilar A, Vega C. Medical therapy with tranexamic acid in autosomal dominant polycystic kidney disease patients with severe haematuria. Nefrologia. 2012;32:160‐165. [DOI] [PubMed] [Google Scholar]
- 74. Lee S, Fralick M, Sholzberg M, et al. Systematic‐review of Hematuria and Acute Renal‐failure with cycloKapron (SHARK); 2020. [DOI] [PubMed]


