Abstract
Background:
Medical mistrust influences patients’ treatment seeking, adherence, health behaviors, and minority participation in research studies. However, medical mistrust remains understudied within neurological diseases like stroke despite disproportionately affecting minority populations.
Objective:
This study examines the relationship of medical mistrust with stroke knowledge among Black, Latino, Korean and Chinese-Americans.
Methods:
Subjects >60 years were enrolled from senior centers to test a culturally-tailored educational curriculum around stroke risk reduction in a randomized controlled trial. A Trust Physician Scale and a modified Trust of Medical Researchers Scale measured medical mistrust. The Stroke Action Test instrument measured stroke knowledge, focusing on intent to call 911 appropriately when presented with stroke symptoms.
Results:
Of 225 subjects, 69.5% were female (n=157) with an average age of 73.7 years (standard deviation 6.7). Blacks had highest trust scores of physicians relative to Latino/a, Korean or Chinese subjects (p<0.05). In multivariable analysis, decreased stroke knowledge was associated with decreased researcher trust at baseline (<0.05), but not physician trust, when controlling for covariates. Among Latino/a, Korean and Chinese groups, mainstream acculturation reduced the association between researcher trust and stroke knowledge. A mediation model showed no evidence of physician trust mediating researcher trust.
Conclusions:
Among minority seniors participating in an RCT, decreased trust of researchers, not physicians, was associated with low baseline knowledge of stroke symptoms. Those least acculturated to US culture may be a particular focus for trust building intervention. Future studies should examine whether researcher mistrust is disproportionately preventing those with the largest knowledge gaps from participating in trials.
Keywords: Stroke, Disparities, Health Education, Trust, Elderly, Minorities
INTRODUCTION
Patients’ mistrust of physicians and medical researchers acts as a barrier to patients’ optimal health status and participation in research studies. Previous studies have found that mistrust of physicians is a barrier to engaging in positive health behaviors like treatment initiation and adherence(1); engaging in preventive health behaviors like cancer or cholesterol screening(2,3); and having improved health outcomes and health-related quality of life(1,4). Mistrust of physicians has also been identified as one factor contributing to disparities in care among African Americans in particular(3).
Other studies suggest that mistrust of medical research is one reason for reduced participation in research studies among minorities, despite federal mandates to ensure inclusion of minorities in federally-funded research(5). The Tuskegee Study is one research study frequently linked to African Americans’ mistrust in medical researchers(5), one example in a longer history of racial exploitation and ethical misconduct in the context of clinical research in the United States(6). A widespread concern is that mistrust of research, connected to or independent of mistrust of physicians, will impede successful recruitment of African Americans into research studies and diminish generalizability of research findings.
Physician and researcher mistrust within other minority groups demonstrates a similar trend. Latino/a and Asian patients having higher mistrust of physicians than their white counterparts(7,8), with higher levels of acculturation or longer tenure in the U.S. associated with increased trust in healthcare providers(9,10). Participation in research trials is also lower among Latino/a and Asians(11,12), with mistrust identified as one reason for reduced participation involving concerns about informed consent and medical experimentation(11,13).
Medical mistrust represents one root cause of disparities, with potential significant distinctions between interpersonal and institutional physician, researcher, and healthcare system mistrust. In this paper, we focus on mistrust of physicians and researchers. These concepts remain particularly understudied in neurological disease, despite diseases like stroke disproportionately affecting minority populations and disparities evident in diagnosis, treatment, and prognosis(14). Poor knowledge of stroke symptoms and appropriate response to symptoms when they occur (calling 911) is one mechanism for disparities in stroke outcomes and has been a cardinal focus of community-level interventions to increase thrombolysis rates for acute ischemic stroke specifically(15,16). Trust is one component that facilitates the transfer of stroke knowledge and associated action(17), but requires further study to optimize stroke education interventions and address stroke-related disparities. One stroke prevention study found that recruitment of African American participants partly depended on the influence of participants’ primary physicians(18), suggesting a potential mediating effect of physician trust on, and engagement with, medical research.
As a first step towards addressing this possibility, this study aims to (1) describe levels of physician and researcher mistrust among African American, Latino, Korean and Chinese Americans in a cohort of seniors participating in a trial of a physical activity/stroke risk factor reduction intervention; (2) assess racial/ethnic differences of physician and researcher mistrust; (3) determine the relationship of physician and researcher mistrust with stroke knowledge, including potential moderation by acculturation; and (4) examine the potential mediating role of physician mistrust on researcher mistrust and stroke knowledge.
METHODS
Design
This is a cross-sectional analysis of baseline data from “Worth the Walk,” a randomized controlled trial (RCT) aimed at increasing physical activity and stroke knowledge in order to reduce stroke risk among high-risk minority seniors in Los Angeles(19). This project was conducted using community-based participatory research principles(20).
The University of California Los Angeles institutional review board approved the study protocol.
Participants, Setting, and Data Collection
Participants were recruited and enrolled from four Los Angeles, senior-service organizations, serving African American, Latino, Korean, and Chinese American communities. To be eligible, participants had to be ≥ 60 years old, report a history of hypertension, and be able to walk and participate in group discussion sessions. Trained research associates using iPads and REDCap interviewed participants in their preferred language. All African American participants and three Latino participants completed interviews in English; other participants completed interviews in Spanish, Korean, or Mandarin Chinese.
Measures
Clinical and Social Demographics
Participants self reported race/ethnicity, age, and gender. Education was categorized as the highest grade completed: below 8th grade, high school/ GED, or higher education. Insurance status was categorized as dichotomous (yes/no). We used the Katz/Charlson comorbidity scale modified for self-administration to assess medical comorbidities for each participant(21). Sixteen diseases are included in this index, which was tested as a valid predictor of mortality due to comorbid conditions in a 10-year follow-up cohort study(22). This is included as people with chronic diseases have more chances to visit healthcare providers and develop trusting relationships with them. Acculturation was measured via the Vancouver Acculturation Index, a 20-item measure that distinguishes between acquisition of new host cultural tendencies and maintenance of heritage culture, with higher mainstream scores and lower heritage scores reflecting greater orientation toward American culture(23). The instrument was administered to Latino/a, Korean, and Chinese American participants, and not African American participants.
Stroke Knowledge
We used the Stroke Action Test (STAT) to assess stroke knowledge. STAT is a previously-tested instrument with good validity and reliability for assessing correct responses to individual stroke symptoms, consisting of 28 close-ended items(24). Twenty-one items describe stroke-warning signs and 7 describe non-stroke warning signs(24). For each item, there are 4 possible responses: call 911; go to the emergency room; wait 1-hour prior to deciding next action; and wait 1-day prior to deciding next action. The STAT is scored by counting how many times the respondent selected the correct answer for stroke symptoms and modeled as a continuous variable. In this study, the version of STAT contained 23 items that named or described a symptom, with 17 involving stroke symptoms. Like others who have used this instrument, we focused on correct responses to calling 911(25), as knowledge of stroke symptoms alone has not been consistently associated with intent to call 911(26). We created a STAT variable by calculating percent of correct responses to call 911 when presented with a stroke symptom.
Physician and Researcher Mistrust
The Trust in Physicians Scale (TPS) and a modified Trust in Medical Researchers (TMR) scale were used to gauge interpersonal participant trust of physicians and researchers, respectively(27–29). TPS is an 11-item, previously tested self-administered questionnaire with acceptable validity and reliability for measuring three dimensions of trust: physician dependability, confidence in physician knowledge and skills, and confidentiality and reliability of information received from the physician(27). Items are answered in a 5-point Likert format from 1 “strongly disagree” to 5 “strongly agree” and a summary measure of the responses is transformed to a 0–100 scale. Higher scores reflect greater trust(27). TPS scores are significantly correlated with continuity of care, adherence to prescribed medication, and overall satisfaction with care(27).
Our TMR was a 5-item questionnaire modified from two instruments(28,29), translated into the different languages, pre-tested and modified in iterative fashion to optimize comprehension. The Cronbach’s alpha in each group was as follows: 0.67 in Korean and Latino/a groups, 0.70 in the Chinese group, and 0.78 in the African American group. The Cronbach’s alpha was 0.70 across all groups, demonstrating adequate internal consistency reliability. Questions pertained to honesty about purpose of the research, participant safety, informed consent, and a global sense of trust in researchers. The questionnaire involves a 4-point Likert format from “1” strongly agree to “4” strong disagree; the unweighted mean of the responses is transformed to a 0–100 scale, with higher scores reflecting greater trust. For the multivariate models we constructed a categorical variable (<50, =50, and >50) for ease of interpretation.
Data Analysis
Descriptive statistics were calculated overall, and unadjusted regression models tested whether physician and research mistrust differed by race/ethnicity. Pair-wise comparisons with a Sidak adjustment identified which groups differed from one another. We subsequently developed a regression model to examine the association between physician and researcher mistrust and correct endorsement of calling 911. The model adjusted for age, gender, race/ethnicity, insurance status, educational attainment and medical comorbidity, which have been previously identified to influence medical mistrust. A parallel model was done in the sample of Latino, Chinese and Korean Americans, adding acculturation to the model to test whether exposure related to correct endorsement of calling 911 for stroke symptoms over and above mistrust measures. Acculturation was not included in the full-sample model because the acculturation measure was not administered to African American participants. Test of physician trust as a mediator between researcher mistrust and correct endorsement of calling 911 was assessed using the Sobel-Goodman criteria for mediation(30). We used 0.05 as the statistical significance level and data analysis was performed using STATA version 15.1.
RESULTS
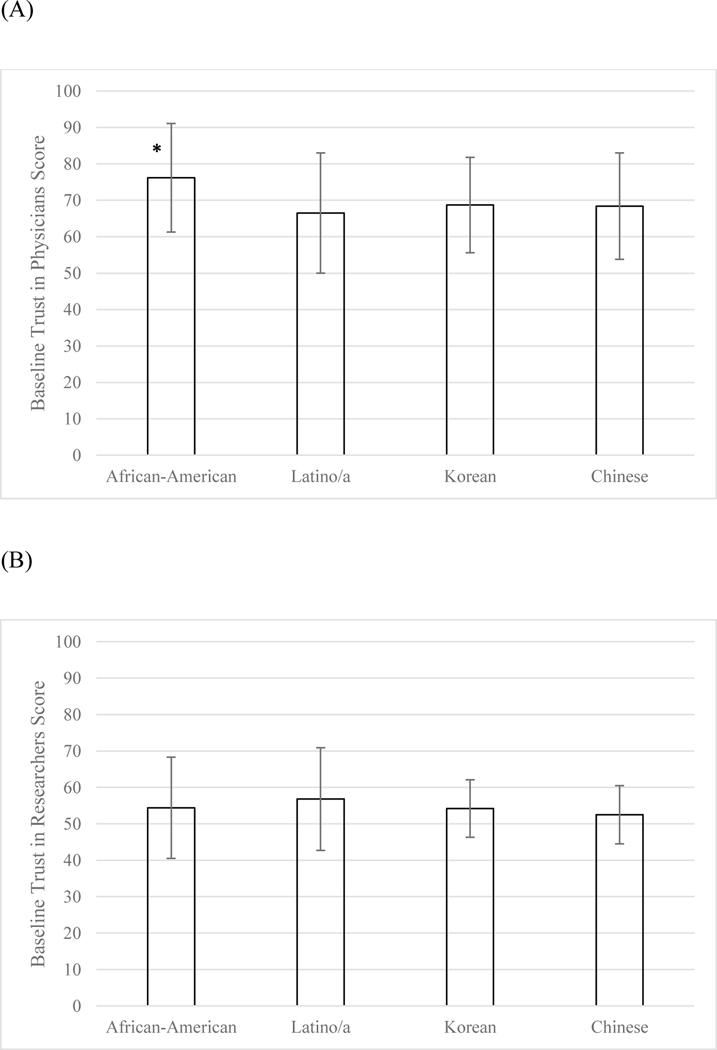
There were 233 participants enrolled in the study. Eight participants were excluded for missing data on the TPS and/or TMR measures. Of the remaining 225 participants, 69.3% were female (n=156) with an average age of 73.9 years (standard deviation 6.7) (Table 1). The cohort was largely insured (92%, n=207) and the African American group was the highest educated group, with 61.5% (n=32) having at least some college education. Both TPS and TMR measures were negatively skewed, with less than <15% of the sample having scores of <50 in either measure. For example, in the TPS measure, 85% of the sample agreed or strongly agreed with the statement, “I trust my doctor’s judgments about my medical care” and 72% agreed or strongly agreed with the statement, “I trust my doctor to tell me if a mistake was made about my treatment.” The mean TPS score was 69.9 (SD=15.2) with a range of 14–100. In unadjusted analysis of the TPS scores, scores differed across racial/ethnic groups (p=0.001), with the African American group having highest physician trust on the TPS scale (76.2 points, SD=14.9). Follow-up pairwise comparisons using Sidak adjustments for multiple comparisons indicated African Americans had greater mean trust in physicians than Latino/a, Korean and Chinese participants (p’s ≤ .05; Figure 1; Table 1). Latino/a, Korean, and Chinese American participants did not have statistically significant differences in their reported mean trust in physicians.
Table 1.
Baseline Characteristics of Study Participants (N=225)
| Characteristic | Overall (n=225) | African-American (n=52) | Latino/a (n=62) | Korean (n=58) | Chinese (n=53) |
|---|---|---|---|---|---|
| Age, mean (SD)* | 73.9 (6.7) | 72.3 (7.2) | 72.6 (5.7) | 76.4 (6.7) | 74.3 (6.4) |
| Female, n (%) | 156 (69.3) | 40 (76.9) | 48 (77.4) | 35 (60.3) | 33 (62.3) |
| Education, n (%) ** | |||||
| </= 8th grade | 93 (41.3) | 12 (23.1) | 43 (69.4) | 15 (25.9) | 23 (43.4) |
| Completed HS | 47 (20.9) | 8 (15.4) | 8 (12.9) | 22 (37.9) | 9 (17.0) |
| At least some College | 85 (37.8) | 32 (61.5) | 11 (17.7) | 21 (36.2) | 21 (39.6) |
| No insurance, n (%) | 18 (8.0) | 3 (5.8) | 2 (3.2) | 8 (14.0) | 5 (9.4) |
| Charlson Comorbidity Index, mean (SD)* | 1.9 (2.2) | 2.1 (2.1) | 1.5 (2.4) | 1.5 (1.7) | 2.7 (2.3) |
| Maintenance of heritage culture, mean (SD) | N/A | 7.5 (1.2) | 7.0 (1.0) | 6.7 (0.8) | |
| Acculturation towards mainstream culture, mean (SD)** | N/A | 6.7 (1.6) | 5.1 (1.1) | 5.4 (1.3) | |
| Physician Trust (TPS), mean (SD)** | 69.8 (15.2) | 76.2 (14.9) | 66.5 (16.5) | 68.7 (13.1) | 68.4 (14.6) |
| Researcher Trust (TMR), mean (SD) | 54.6 (11.5) | 54.4 (13.9) | 56.8 (14.1) | 54.2 (7.9) | 52.5 (8.0) |
| Stroke Action Test, mean (SD)* | 46.4 (22.2) | 56.9 (20.8) | 49.2 (19.2) | 34.9 (23.3) | 45.5 (19.9) |
p-value <0.05
p-value <0.001
Figure 1.
Physician (A) and Researcher (B) Trust scores among Study Participants
In the TMR measure (mean score=54.8, SD 11.5; range 5–75), 89% of the sample agreed or strongly agreed with the statement, “if a medical researcher asked me to participate in a medical research study, I trust that he/she would provide me with a full explanation of the study”; 87% agreed or strongly agreed with the statement, “I completely trust doctors who do medical research.” Researcher trust did not demonstrate statistically significant differences across racial/ethnic groups (p =0.2) (Figure 1). The physician and research trust measures had a Spearman correlation coefficient of 0.3 (P<0.001).
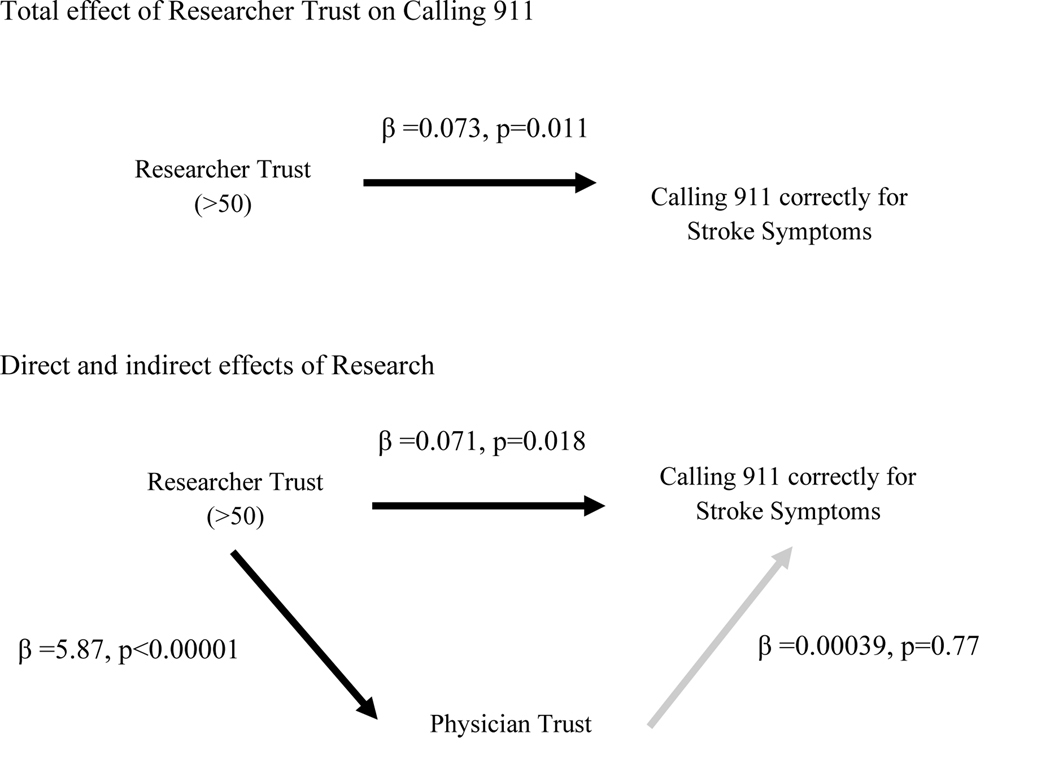
In unadjusted analyses, neither physician nor researcher trust were associated with correctly endorsing calling 911 (Table 2). In multivariable regression analysis (Table 2), higher researcher trust (>50 points), but not physician trust, was associated with correct endorsement of calling 911 when controlling for covariates. Researcher trust score of greater than 50 was associated with nearly a 14-point percentage higher likelihood of calling 911 when presented with stroke symptoms, compared to individuals with researcher trust less than 50 (Table 2). This relationship was moderated by mainstream acculturation among Latino/a, Korean and Chinese groups, such that the effect of researcher trust on calling 911 correctly increased with higher mainstream acculturation (β =0.14, p=<0.05). This interaction explains the discrepancy between unadjusted and adjusted models, where trust is associated with correct endorsement of calling 911 in the context of other factors like acculturation. In exploratory analyses assessing the relationship between physician and researcher trust and various demographic and social characteristics including acculturation, increased mainstream acculturation was associated with increased trust in both scales (p<0.05 for both, data not shown). Lastly, a mediation model did not show evidence of physician trust mediating researcher mistrust and correct endorsement of calling 911 with stroke warning signs (Figure 2).
Table 2.
Characteristics Associated with Higher Stroke Knowledge
| Variable | Unadjusted Coefficient (p-value) | Adjusted Coefficient (p-value) |
|---|---|---|
| Physician Trust (TPS) | 0.0017 (0.17) | 0.078 (0.41) |
| Researcher Trust (TPR) | ||
| TPR=50 | −0.012 (0.85) | 0.098 (0.13) |
| TPR>50 | 0.076 (0.24) | 0.14 (0.03) |
TPR<50 as reference
Adjusted for ethnicity, gender, age, insurance, education, Charlson Comorbidity Index
Figure 2.
Mediation model
*Adjusted for ethnicity, gender, age, insurance, education, Charlson Comorbidity Index
DISCUSSION
Our study involved a sample of seniors across four racial/ethnic groups in Los Angeles participating in a randomized controlled trial, who generally trusted physicians and researchers. Mean physician trust levels were higher among the African American group than the Latino/a and Asian subgroups in this cohort, highlighting the importance of understanding group-specific factors contributing to medical mistrust in different contexts and among racial/ethnic minority groups more broadly. For example, in this study, the difference could have related to senior centers’ prior experiences with research teams, varying levels of involvement among senior center staff, and differing recruitment strategies at the senior centers. Previous literature demonstrates that African Americans report higher trust of research when they feel that their participation will benefit the African American community, which underscores the importance of tailored communication strategies during recruitment(31). Other facilitators to research participation include familiarity with the research recruiter and inclusion of community leaders or trusted intermediaries in the recruitment process(32,33). Factors influencing trust appear therefore to be both context-specific (e.g. according to type of institution and staff at the institution) in addition to being contingent upon the racial/ethnic population involved and language of the instruments.
Our study also demonstrates that researcher trust, but not physician trust, is associated with lower baseline stroke action knowledge (correct endorsement of calling 911 for stroke symptoms). Though we may have been underpowered to detect associations between physician trust and stroke knowledge in this exploratory analysis, this finding of the association between researcher trust and stroke knowledge is new, potentially important, and warrants further investigation, For our Latino/a, Korean, and Chinese participants, acculturation to mainstream American culture positively moderated the effect of trust on calling 911 correctly for stroke symptoms. This builds on findings from prior studies that have shown higher acculturation or longer tenure in the United States as associated with higher trust in healthcare providers(9,10). This could be due to acculturation increasing familiarity with the U.S. healthcare system broadly speaking, increasing ability to communicate with healthcare providers, and adaptation to a system that more strongly emphasizes individuality, autonomy, and assertiveness in clinical encounters. Notably, however, the literature remains scant on the acculturation and trust relationship among Latino/a and Asian groups in particular, as most studies focus on African Americans and Whites.
Previous studies have also shown that trust of researchers is influenced by negative encounters with healthcare providers(31); however, given that the relationship between trust and stroke action knowledge was not mediated by physician trust in this study, our results suggest that addressing researcher trust may be an important but distinct effort from strategies focused on addressing physician trust alone. Rather than playing a mediating role, patients may view physician trust as independent of their trust of researchers, and/or differentiate between institutional and interpersonal trust related to a specific physician. Other instruments measure a related concept of trust in the healthcare system(34), highlighting the need for further understanding the distinction between these concepts of trustworthiness in healthcare. Addressing trust of researchers, as separate from trust of physicians, offers potential promise as a mechanism to increase recruitment of minority seniors in clinical research, including in behavioral/ educational trials that pose minimal risk for physical adverse effects and exposure to unsafe treatments.
Overall, physicians and researchers must take responsibility for earning patients’ trust in order to include diverse groups in health education and research efforts(35). In fact, business management leaders have increasingly viewed trustworthiness as a teachable leadership competency that can be made an explicit objective to focus on and improve, as emphasized in Steve Covey’s popular layperson press book “The Speed of Trust”(36); behaviors of high-trust leaders include demonstrating respect, creating transparency, and clarifying expectation, among others(36). Establishing trust may therefore benefit from explicit instruction and discussion in medical education, with opportunities for incorporation into existing medical curricula about professionalism, cultural competency, or communication skills training. Few interventions have been developed specifically to improve physician-trust building skills, yielding mixed results(37). None of these interventions focused on improving trust of researchers. Thus, future efforts could explore the impact of specific training on patients’ trust, including efforts targeted toward addressing physician and researcher trust.
Limitations and Strengths
The study findings should be interpreted with consideration of several limitations. First, the cross-sectional nature makes it impossible to establish a causal relationship between mistrust and stroke action knowledge. Second, both trust measures have not been tested in other languages or cultural contexts, an important consideration in our linguistically and ethnically diverse population. Third, study outcomes were measured using self-reports, which introduces social desirability bias as participants may report positive attitudes to study interviewers to gain approval. Further, while all study survey instruments were front and back-translated, and pilot tested in all the communities for understanding, it is possible that there remained lack of clarity around certain concepts, like the concept of a “researcher.” Fourth, unmeasured variables that may have played a role include duration of relationship between patient and physician and physician-patient race concordance; these factors have been shown to play a role in perceptions of physician trust, although not yet elucidated in the researcher trust context(38–40). This was not a population-based sample and included participants who trusted researchers at least enough to enroll in the clinical trial; results cannot be extrapolated as representative of all older adults from these racial/ethnic groups.
However, a major strength of this study remains the inclusion of participants from different ethnic minority groups in an urban clinical setting. In addition, this is one of few studies to examine medical mistrusts’ role in stroke action knowledge, stroke representing one of several neurological diseases with significant persisting disparities.
Conclusion
Among minority seniors participating in a community intervention trial, greater mistrust of researchers, not physicians, was associated with low baseline knowledge of stroke action knowledge, or correct endorsement of calling 911 with stroke warning signs. Mainstream acculturation among Latino/a, Korean and Chinese subgroups moderated the trust and stroke action knowledge relationship. Future studies should examine whether researcher mistrust is disproportionately preventing those with the largest knowledge gaps from participating in trials, with trust facilitating health information exchange and transfer. Community-tailored strategies for overcoming higher levels of mistrust are warranted and may involve active trust building through deliberate outreach and education rather than assumptions around trust developing passively as consequence of personal interactions. Those least acculturated to mainstream US culture may be a particular focus for trust building interventions. Education on stroke signs and symptoms, linkage of stroke recognition with an immediate need to call 911, and understanding barriers to activating emergency services needs to happen concurrently with efforts to establish trust with the healthcare system more broadly.
Acknowledgement
The authors acknowledge Ms. Phyllis Willis from the project’s Community Advisory Board for her assistance with recruitment, enrollment, and suggestions on an early version of this manuscript. This research was supported by: NIH/NINDS Los Angeles Stroke Prevention/Intervention Research Program in Health Disparities (1U54NS081764), NIH/NIA Mid-Career Award in Patient-Oriented Research (1K24AGO47899), NIH/NIA UCLA Resource Center for Minority Aging Research/Center for Health Improvement of Minority Elders (RCMAR/CHIME) (2P30AG081684), NIH National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number (UL1TR001881).
Footnotes
Conflict of Interest Disclosure Statement: The authors (A.S., A.Y.K., J.A.M, C.A.C, C.E.R., and C.A.S.) have nothing to disclose.
References
- 1.Birkhäuer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner C, et al. Trust in the health care professional and health outcome: A meta-analysis. PLOS ONE. 2017. February 7;12(2):e0170988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Musa D, Schulz R, Harris R, Silverman M, Thomas SB. Trust in the Health Care System and the Use of Preventive Health Services by Older Black and White Adults. Am J Public Health. 2009. July 1;99(7):1293–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hammond WP, Matthews D, Mohottige D, Agyemang A, Corbie-Smith G. Masculinity, Medical Mistrust, and Preventive Health Services Delays Among Community-Dwelling African-American Men. J Gen Intern Med. 2010. December;25(12):1300–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corbie-Smith G, Ford CL. Distrust and Poor Self-Reported Health. J Gen Intern Med. 2006. April;21(4):395–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shavers VL, Lynch CF, Burmeister LF. Knowledge of the Tuskegee study and its impact on the willingness to participate in medical research studies. J Natl Med Assoc. 2000. December;92(12):563–72. [PMC free article] [PubMed] [Google Scholar]
- 6.Byrd WM, Clayton LA. Race, medicine, and health care in the United States: a historical survey. J Natl Med Assoc. 2001. March;93(3 Suppl):11S–34S. [PMC free article] [PubMed] [Google Scholar]
- 7.Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/Ethnic Differences in Physician Distrust in the United States. Am J Public Health. 2007. July;97(7):1283–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ngo-Metzger Q, Legedza ATR, Phillips RS. Asian Americans’ Reports of Their Health Care Experiences. J Gen Intern Med. 2004. February;19(2):111–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simon MA, Zhang M, Dong X. Trust in Physicians Among U.S. Chinese Older Adults. J Gerontol A Biol Sci Med Sci. 2014. November;69(Suppl 2):S46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hong HC, Lee H, Collins EG, Park C, Quinn L, Ferrans CE. Factors affecting trust in healthcare among middle-aged to older Korean American women. BMC Womens Health [Internet]. 2018. December [cited 2018 Dec 3];18(1). Available from: https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-018-0609-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Limkakeng A, Phadtare A, Shah J, Vaghasia M, Wei DY, Shah A, et al. Willingness to Participate in Clinical Trials among Patients of Chinese Heritage: A Meta-Synthesis. PLoS ONE [Internet]. 2013. January 17 [cited 2019 Mar 27];8(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3547937/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004. June 9;291(22):2720–6. [DOI] [PubMed] [Google Scholar]
- 13.George S, Duran N, Norris K. A Systematic Review of Barriers and Facilitators to Minority Research Participation Among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health. 2014. February;104(2):e16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics−−2015 update: a report from the American Heart Association. Circulation. 2015. January 27;131(4):e29–322. [DOI] [PubMed] [Google Scholar]
- 15.Skolarus LE, Zimmerman MA, Bailey S, Dome M, Murphy JB, Kobrossi C, et al. Stroke Ready Intervention: Community Engagement to Decrease Prehospital Delay. J Am Heart Assoc Cardiovasc Cerebrovasc Dis [Internet]. 2016. May 20 [cited 2019 Mar 27];5(5). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4889198/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malek AM, Adams RJ, Debenham E, Boan AD, Kazley AS, Hyacinth HI, et al. Patient Awareness and Perception of Stroke Symptoms and the Use of 911. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc. 2014. October;23(9):2362–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mackintosh JE, Murtagh MJ, Rodgers H, Thomson RG, Ford GA, White M. Why People Do, or Do Not, Immediately Contact Emergency Medical Services following the Onset of Acute Stroke: Qualitative Interview Study. PLOS ONE. 2012. October 4;7(10):e46124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gorelick PB, Harris Y, Burnett B, Bonecutter FJ. The recruitment triangle: reasons why African Americans enroll, refuse to enroll, or voluntarily withdraw from a clinical trial. An interim report from the African-American Antiplatelet Stroke Prevention Study (AAASPS). J Natl Med Assoc. 1998. March;90(3):141–5. [PMC free article] [PubMed] [Google Scholar]
- 19.Menkin Josephine A, McCreath Heather E, Song Sarah Y, Carrillo Carmen A, Reyes Carmen E, Trejo Laura, et al. “Worth the Walk”: Culturally Tailored Stroke Risk Factor Reduction Intervention in Community Senior Centers. J Am Heart Assoc. 2019. March 19;8(6):e011088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kwon I, Choi S, Mittman B, Bharmal N, Liu H, Vickrey B, et al. Study protocol of “Worth the Walk”: a randomized controlled trial of a stroke risk reduction walking intervention among racial/ethnic minority older adults with hypertension in community senior centers. BMC Neurol [Internet]. 2015. June 15 [cited 2019 Mar 27];15. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4465734/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996. January;34(1):73–84. [DOI] [PubMed] [Google Scholar]
- 22.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. [DOI] [PubMed] [Google Scholar]
- 23.Ryder AG, Alden LE, Paulhus DL. Is Acculturation Unidimensional or Bidimensional? A Head-to-Head Comparison in the Prediction of Personality, Self-Identity, and Adjustment. :17. [DOI] [PubMed] [Google Scholar]
- 24.Billings-Gagliardi S, Mazor KM. Development and Validation of the Stroke Action Test. Stroke. 2005. May 1;36(5):1035–9. [DOI] [PubMed] [Google Scholar]
- 25.Caruso D, Akly MP, Costantini PD, Fridman S, Esnaola MM. Do Elderly Patients Call 911 When Presented with Clinical Scenarios Suggestive of Acute Stroke? A Cross-Sectional Study. Cerebrovasc Dis. 2015;39(2):87–93. [DOI] [PubMed] [Google Scholar]
- 26.Fussman C, Rafferty AP, Lyon-Callo S, Morgenstern LB, Reeves MJ. Lack of Association Between Stroke Symptom Knowledge and Intent to Call 911: A Population-Based Survey. Stroke. 2010. July;41(7):1501–7. [DOI] [PubMed] [Google Scholar]
- 27.Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the Trust in Physician Scale. The Stanford Trust Study Physicians. Med Care. 1999. May;37(5):510–7. [DOI] [PubMed] [Google Scholar]
- 28.Corbie-Smith G, Thomas SB, George DMMS. Distrust, Race, and Research. Arch Intern Med. 2002. November 25;162(21):2458–63. [DOI] [PubMed] [Google Scholar]
- 29.Hall MA, Camacho F, Lawlor JS, Depuy V, Sugarman J, Weinfurt K. Measuring trust in medical researchers. Med Care. 2006. November;44(11):1048–53. [DOI] [PubMed] [Google Scholar]
- 30.UCLA: Statistical Consulting Group. How to perform Sobel-Goodman mediation tests in Stata? [Internet]. [cited 2019 Apr 18]. Available from: https://stats.idre.ucla.edu/stata/faq/how-to-perform-sobel-goodman-mediation-tests-in-stata/
- 31.Scharff DP, Mathews KJ, Jackson P, Hoffsuemmer J, Martin E, Edwards D. More than Tuskegee: Understanding Mistrust about Research Participation. J Health Care Poor Underserved. 2010. August;21(3):879–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hughes TB, Varma VR, Pettigrew C, Albert MS. African Americans and Clinical Research: Evidence Concerning Barriers and Facilitators to Participation and Recruitment Recommendations. The Gerontologist. 2017. April 1;57(2):348–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.García AA, Zuñiga JA, Lagon C. A Personal Touch: The Most Important Strategy for Recruiting Latino Research Participants. J Transcult Nurs Off J Transcult Nurs Soc. 2017. July;28(4):342–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Armstrong K, McMurphy S, Dean LT, Micco E, Putt M, Halbert CH, et al. Differences in the patterns of health care system distrust between blacks and whites. J Gen Intern Med. 2008. June;23(6):827–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grob R, Darien G, Meyers D. Why Physicians Should Trust in Patients. JAMA. 2019. April 9;321(14):1347–8. [DOI] [PubMed] [Google Scholar]
- 36.Covey SM, Merril RR. The Speed of Trust: The one thing that changes everything. 7th ed. New York: Free Press; 2006. [Google Scholar]
- 37.Rolfe A, Cash-Gibson L, Car J, Sheikh A, McKinstry B. Interventions for improving patients’ trust in doctors and groups of doctors. Cochrane Database Syst Rev. 2014. March 4;(3):CD004134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the Medical Profession: Conceptual and Measurement Issues. Health Serv Res. 2002. October;37(5):1419–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pearson SD, Raeke LH. Patients’ Trust in Physicians: Many Theories, Few Measures, and Little Data. J Gen Intern Med. 2000. July;15(7):509–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118(4):358–65. [DOI] [PMC free article] [PubMed] [Google Scholar]