Abstract
Caregivers of patients with bipolar disorder (BD) undergo a considerable amount of burden. In India, family caregivers are the primary source of support and care for their ill relatives. The burden faced by family members of patients with BD often results in physical and mental health consequences. This may lead to negative interaction patterns such as hostility, criticality, and overinvolvement, termed as expressed emotions (EE). Here, we report how we addressed the EE in family members, using a single-subject design that involved the family caregivers (n = 2) of two adults who presented with a diagnosis of BD with a current episode of mania. An assessment of family caregivers, using the family questionnaire, revealed high EE. Family focused therapy (FFT) of 12 sessions was delivered over 3–4 weeks on an inpatient basis, with positive outcomes of reductions in EE and family stress and improved psychosocial functioning in patient that were sustained over 9–10 months. FFT can be an important add on psychosocial therapy to reduce EE and stress and to facilitate functioning and communication.
Keywords: Bipolar disorder, family focused therapy, family caregiver, expressed emotions
Bipolar disorder (BD) is associated with a high level of disability in the patient and a marked level of distress in the caregivers. BD leads to significant anguish and occupational impairment and pose a considerable burden on the caregivers.1–4 In India, family caregivers are the primary source of support and care for their ill relatives.5 They provide care and support, including taking care of daily routine, monitoring medications, ensuring regular follow-up, and meeting the financial needs.6. This boundless involvement of families in care is driven both by choice as well as compulsion.7 The task of supervising the patient leads to emotional exhaustion in the caregiver.8 The negative interaction pattern, such as hostility, criticality, and overinvolvement, termed as EE, when used by the family members toward a patient, has been linked with relapse of symptoms in mental disorders.9, 10 The burden faced by family members of patients with BD often has physical and mental health consequences.11. Further, if caregivers such as the parents or the spouse have high-EE, the chance of recurrence is two to three times higher.12 Psychosocial treatments such as family focused therapy (FFT) has caused improvement in symptoms among patients with BD whose relatives showed high EE.13 However, to our knowledge, there are no Indian studies focusing on the effect of FFT on the EE of the caregiver. Hence, this study was planned to cater to family members of patients with BD using FFT in the Indian context and to examine its usefulness in reducing EE and stress.
Case Report #1
A 27-year-old married lady from a rural background, with higher secondary education, belonging to the lower socioeconomic status, with 5 years’ history of BD, presented with 3 months’ history of irritability, decreased need for sleep, increased energy, increased psychomotor activity, and aggressive and assaultive behavior. The symptoms caused significant distress and burden to the family, especially the mother who accompanied her in this visit. She had a previous history of three episodes (in 5 years), each episode lasting 2–3 months.
She was admitted to the female inpatient psychiatric unit of National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru. On assessment, the therapist noticed that the current symptoms were triggered by drug default (the patient had stopped taking medicine for more than 10 months). In addition, there were family problems, as well. The mother was 56 years old, had primary school education, was widowed, and was working in a private factory. Due to the aggressive and disinhibited behavior, the patient was brought by the mother and admitted to female inpatient unit. She was diagnosed to have BD, current episode Mania with psychotic symptoms.
An interview was conducted with the mother to understand the issues faced by her. An assessment of EE was done using the family questionnaire.14 The mother scored high on EE and also expressed her distress of caring for the patient. The mother underwent 12 tailor-made, face-to-face, thrice-weekly sessions of FFT15 (Table 1). The first four sessions focused on psychoeducation about the illness, explaining the stress diathesis model, the importance of medication adherence, sleep hygiene, and the warning signs of BD. The next four sessions concentrated on training on communication skills, with the help of video developed for the current study.
Table 1. Details of Family Focused Therapy Session Conducted for the Caregivers of Two Cases.
| Sessions | Case #1 | Case #2 |
|
Psychoeducation (1–4 sessions) |
Preassessments followed by an exploration of patient symptoms observed by the caregiver. Discussion on BD. Identification of relevant stressors. Writing an individualized mood behavior chart. Identification of coping followed by the caregiver. Discussion on the importance of medication adherence and the need for supervised medication intake was done with the mother and her doubts were clarified. Sleep hygiene and its role in triggering the symptoms was discussed with the patient. The mother was also suggested sleep hygiene techniques as she was not having adequate sleep. Taught the mother to follow the relaxation technique (deep breathing exercise, JPMR) |
Preassessments followed by an exploration of patient symptoms observed by the caregiver. Discussion on BD. Identification of relevant stressors. Writing an individualized mood behavior chart. Identification of coping skills followed by the father and the patient. Discussion done on the importance of medication adherence. The need for supervised medication intake was emphasized, with examples. Discussion on substance use and its ill effect was discussed with the patient, and future plans of the patient were also explored. Emphasized the role of family environment. |
| Communication enhancement training (5–8 sessions) |
Provided basic information on communication skills training. Evaluated the current communication style in the family. Discussed communication skills and demonstrated the skills through video demonstration. Subsequently, rehearsals, using their everyday life situation in their family, were done to follow the right communication skills. Symptoms of illness and the need for medication adherence, warning signs of BD to patients were explained. |
Provided basic information on communication skills training. Evaluated the current communication style in the family. Communication skills training was carried out through video demonstration, followed by rehearsal using their everyday life situations that caused negative interaction patterns. |
| Problem-solving skill training |
Identified specific problems Taught the problem-solving approach with examples. Explored the reason for conflict between the patient and her in-laws. A session was conducted for the father-in-law and husband regarding the illness and the current stressors were addressed. Facilitated discussion among them and the solutions were sought. |
Identified specific problems Taught the problem-solving approach with examples. Explored the reason for interpersonal issues. A telephonic session was conducted for the younger son, regarding the illness, for better understanding and enhanced support. The possible solutions of resolving the interpersonal issues were discussed with the father. |
BD: bipolar disorder, JPMR: Jacobson’s progressive muscular relaxation.
The last four sessions were about problem-solving techniques, as there were interpersonal issues between the patient and her in-laws, such as the illness of the patient and differences in opinion and arguments related to the asset. The mother was taught relaxation techniques of Jacobson’s progressive muscular relaxation and deep breathing exercises. She was instructed to practice them twice a day, to reduce the stress, and advised to continue that even after the discharge. The husband, the father-in-law, and the patient were asked to attend the session to resolve the conflicts among them. They were guided to sort out the family conflicts and find solutions themselves. The therapist functioned as a facilitator only. Once the acute symptoms subsided, the patient also attended the sessions and was provided psychoeducation on the illness.
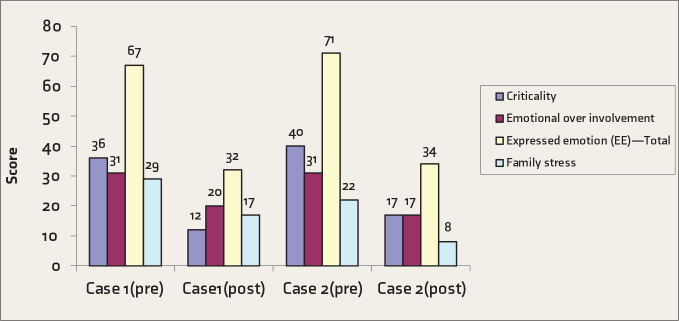
Postassessment carried out by a blind rater (blind to the therapy/intervention as well as timing of assessment), after the completion of FFT, showed a reduction in the level of EE both subjectively as well as objectively (Figure 1). On telephonic follow-ups at the 6th and 9th months after the termination of the therapy, the mother reported that the patient has been asymptomatic and that she was taking care of the children and involved in household work. The patient was taking medicine herself with the supervision of the mother. The mother’s subjective report revealed a reduction in the amount of burden vested on her.
Figure 1. Pre and Post-assessment Score on Expressed Emotions and Family Stress Among Primary Caregivers.
Case Report #2
A 28-year-old single man with a diploma in engineering, from a rural background and a nuclear middle socioeconomic status family, with a duration of illness of 10 years, presented with a one-month history of irritability, sleeplessness, increased talk, singing, ideas of grandiosity, increased psychomotor activity, and aggressiveness. The current episode was precipitated by drug default (the patient refused to take medicines and has not been on medication for 1 year). The episode significantly affected the psychosocial functioning of the patient and the family environment. He had a history of 5–6 past episodes, each lasting about 2 months. He was brought by the father to psychiatric emergency services and later was admitted for inpatient care.
Interview with the father (primary care provider) revealed that the patient had frequent changes of job due to his poor performance, such as not going regularly for the job, not completing work, frequent leaves, etc., in many companies. For the last 1 year, the patient was not working and wished to act in films and demanded money. He would also force the father to buy new clothes and a motorbike.
The assessment of the father revealed significant EE, increased stress, poor knowledge regarding the illness, and interpersonal conflicts with wife over the patient’s behavior. The age of the father was 58 years. He had studied up to 8th standard and had agriculture as the main occupation. He underwent 12 tailor-made sessions of face to face FFT (Table 1).
A brief telephonic session was conducted for the younger siblings regarding the illness, with an emphasis on family support, since the father reported that the younger son had frequent fights with the patient due to poor knowledge of the illness, which made him think that the behavior of the patient as purposeful.
After discharge, they were followed up in the OPD every 2 months and a telephonic follow-up was done at the 10th month. According to the report of the father, the patient had maintained well, was compliant to medication, and was helping the father in agricultural work. Father’s subjective report indicated that he felt better with respect to caregiver burden. He was now able to concentrate on his work and also supervise the medication intake by the patient. These improvements were sustained up to 10 months after the discharge.
Discussion
It is a single subject design that involves caregivers of two adult patients. Both the patients were diagnosed to have BD with a current episode of mania. The nature of the illness and the severity of the symptoms affected the social and occupational functioning of the patients as well as the family, which led to high EE and increased stress due to a poor understanding of the illness and an inability to manage the patients who were not adherent to medications. The same was reflected in objective measures of EE by family questionnaire, which was administered by a blind rater (a trained nursing professional) at both pre- and post-assessment (Figure 1). The tailor-made FFT sessions involving the family member and the patient improved the understanding about the nature of illness in the family caregivers.
Education about illness would have majorly contributed to reduced EE and psychoeducation along the rest of the therapy components would have contributed to reduction in stress. This was maintained for 9 and 10 months, respectively, in the two patients after discharge, as reported by the caregivers. Both the caregivers did not receive any additional intervention during the follow-up period, and according to the caregivers, the patients adhered to the medications advised by the doctor. Similar results were found from the previous study where a reduction in symptoms and rapid recovery and low EE after FFT were noticed.16 FFT plays an important adjunctive role in treating persons with BD. Implementation of psychoeducational treatments such as FFT for families of persons with BD appears to hold promise and are reported to lead to a greater reduction in relapse rates than other psychosocial treatments.17 However, the effect of FFT on EE in family members has not been adequately examined. Thus, these case reports provide preliminary evidence for the effectiveness of FFT on EE as well as stress experienced by the caregivers. To suit the Indian setup, the frequency of the sessions was increased, and the video on communications skills was taken to suit the cultural and the patients’ family context. Since the literature on the role of FFT in the Indian subcontinent is sparse, these early findings suggest that it may be a useful adjunct to the treatment of patients with BD. Reduction in EE may indirectly have a favorable impact on the course of BD, as seen in the two patients described here. Some of the limitations of the study are using a single tool for assessing EE, not focusing on the other family dynamics, and not assessing the functioning using objective measures.
Conclusion
FFT may be a good initiative, especially in the Indian context, to improve the caregivers’ understanding of BD, which in turn reduces EE and stress and improves the communication pattern in the family, thereby leading to better interpersonal relationships, drug compliance, and relapse prevention.
Acknowledgments
The authors would like to acknowledge Dr K. Muralidharan, Professor, Department of Psychiatry, NIMHANS for his support and comments on the manuscript.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Depp CA, Davis CE, Mittal D. et al. Health-related quality of life and functioning of middle-aged and elderly adults with bipolar disorder. J Clin Psychiatry; 2006; 67(2): 215–221. [DOI] [PubMed] [Google Scholar]
- 2.Goossens PJJ, Van Wijngaarden B, Knoppert-Van Der Klein EAM. et al. Family caregiving in bipolar disorder: caregiver consequences, caregiver coping styles, and caregiver distress. Int J Soc Psychiatry; 2008; 54(4): 303–316. [DOI] [PubMed] [Google Scholar]
- 3.Ostacher MJ, Nierenberg AA, Iosifescu DV. et al. Correlates of subjective and objective burden among caregivers of patients with bipolar disorder. Acta Psychiatr Scand; 2008; 118(1): 49–56. [DOI] [PubMed] [Google Scholar]
- 4.Roth GA, Abate D, Abate KH. et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet; 2018; 392(10159): 1736–1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chadda RK. Caring for the family caregivers of persons with mental illness. Indian J Psychiatry; 2014; 56(3): 221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sadath A, Muralidhar D, Varambally S. et al. Caregiving and help seeking in first episode psychosis: a qualitative study. J Psychosoc Rehabil Ment Health; 2014; 1(2): 47–53. [Google Scholar]
- 7.Chakrabarti S. Research on family caregiving for mental illness in India and its impact on clinical practice: are we doing enough to help families? Indian J Soc Psychiatry; 2016; 32(1): 19. [Google Scholar]
- 8.Chaturvedi SK, Ranjan S. Family distress and expressed emotions in caregivers of mentally ill. Indian J Soc Psychiatry; 2006; 22: 25–34. [Google Scholar]
- 9.Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry; 1998; 55(6): 547–552. [DOI] [PubMed] [Google Scholar]
- 10.Amaresha AC, Venkatasubramanian G. Expressed emotion in schizophrenia: an overview. Indian J Psychol Med; 2012; 34(1): 12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heru AM, Ryan CE. Burden, reward and family functioning of caregivers for relatives with mood disorders: 1-year follow-up. J Affect Disord; 2004. December; 83(2–3): 221. [DOI] [PubMed] [Google Scholar]
- 12.Miklowitz DJ. The role of family systems in severe and recurrent psychiatric disorders: a developmental psychopathology view. Dev Psychopathol; 2004. September; 16(3): 667–688. [DOI] [PubMed] [Google Scholar]
- 13.Miklowitz DJ, Chung B. Family-focused therapy for bipolar disorder: reflections on 30 years of research. Family Process; 2016. September; 55(3): 483-499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wiedemann G, Rayki O, Feinstein E. et al. The family questionnaire: development and validation of a new self-report scale for assessing expressed emotion. Psychiatry Res; 2002; 109(3): 265–279. [DOI] [PubMed] [Google Scholar]
- 15.Miklowitz DJ, O’Brien MP, Schlosser DA. et al. Clinicians’ treatment manual for family-focused therapy for early-onset youth and young adults (FFT-EOY). Los Angeles: University of California, 2012. [Google Scholar]
- 16.Miklowitz DJ, Schneck CD, Singh MK. et al. Early intervention for symptomatic youth at risk for bipolar disorder: a randomized trial of family-focused therapy. J Am Acad Child Adolesc Psychiatry; 2013; 52(2): 121–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miklowitz DJ, Simoneau TL, George EL. et al. Family-focused treatment of bipolar disorder: 1-year effects of a psychoeducational program in conjunction with pharmacotherapy. Biol Psychiatry; 2000; 48(6): 582–592. [DOI] [PubMed] [Google Scholar]