Abstract
To address vaccine hesitancy based on concerns about fertility, this study assesses sperm parameters before and after mRNA vaccine administration.
Two mRNA vaccines, BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna), received Emergency Use Authorization from the US Food and Drug Administration. Despite high efficacy and few adverse events found in clinical trials, only 56% of individuals in the US reported wanting to receive the vaccine.1 One of the reasons for vaccine hesitancy is the potential negative effect on fertility.2 Because reproductive toxicity was not evaluated in the clinical trials and SARS-CoV-2 has been associated with decreases in sperm parameters,3 we assessed sperm parameters before and after mRNA vaccine administration.
Methods
This single-center prospective study at the University of Miami recruited healthy volunteers aged 18 to 50 years scheduled for mRNA COVID-19 vaccination through flyers posted throughout the university hospital and internal list-serve emails. The University of Miami institutional review board approved the study and written informed consent was obtained from all participants.
Men were prescreened to ensure they had no underlying fertility issues. Those with COVID-19 symptoms or a positive test result within 90 days were excluded. Participants provided a semen sample after 2 to 7 days of abstinence, prior to receiving the first vaccine dose and approximately 70 days after the second. Semen analyses were performed by trained andrologists per World Health Organization guidelines and included semen volume, sperm concentration, sperm motility, and total motile sperm count (TMSC).4 Individuals with oligospermia (sperm concentration <15 million/mL) were included. After calculating data distribution on normality test, medians and interquartile ranges (IQRs) were reported for all variables. The Wilcoxon rank sum test was used to compare pre- and postvaccination semen parameters. Change in TMSC is presented graphically. Statistical analysis was performed with SPSS version 24 (IBM). A 2-tailed P < .05 was considered statistically significant.
Results
Between December 17, 2020, and January 12, 2021, 45 men volunteered (median age, 28 years [IQR, 25-31]); follow-up samples were obtained at a median of 75 days (IQR, 70-86) after the second dose. The study ended on April 24, 2021. Baseline samples were obtained after a median abstinence period of 2.8 days (IQR, 2-3) and follow-up samples after a median of 3 days (IQR, 3-4). Of the 45 men, 21 (46.7%) received BNT162b2 and 24 (53.3%) received mRNA-1273. Baseline median sperm concentration and TMSC were 26 million/mL (IQR, 19.5-34) and 36 million (IQR, 18-51), respectively. After the second vaccine dose, the median sperm concentration significantly increased to 30 million/mL (IQR, 21.5-40.5; P = .02) and the median TMSC to 44 million (IQR, 27.5-98; P = .001). Semen volume and sperm motility also significantly increased (Table).
Table. Change in Semen Analysis Parameters Before and After COVID-19 Vaccination.
| Parameter | Normal value | Median (IQR) | P value | |
|---|---|---|---|---|
| Baseline | Follow-up | |||
| No. of participants | 45 | 45 | ||
| Volume, mL | >1.5 | 2.2 (1.5-2.8) | 2.7 (1.8-3.6) | .01 |
| Sperm concentration, million/mL | >15 | 26 (19.5-34) | 30 (21.5-40.5) | .02 |
| Total motility, % | >40 | 58 (52.5-65) | 65 (58-70) | .001 |
| TMSC, million | >9 | 36 (18-51) | 44 (27.5-98) | .001 |
Abbreviations: IQR, interquartile range; TMSC, total motile sperm count.
Eight of the 45 men were oligospermic before the vaccine (median concentration, 8.5 million/mL [IQR, 5.1-12]). Of these 8, 7 men had increased sperm concentration to normozoospermic range at follow-up (median concentration, 22 million/mL [IQR, 17-25.5]), and 1 man remained oligospermic. No man became azoospermic after the vaccine.
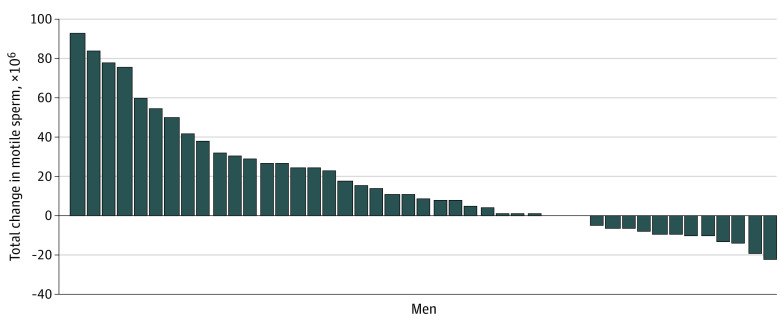
The waterfall plot shows the within-participant change in TMSC from baseline (range, −22 million to 93 million) for each man (Figure).
Figure. Waterfall Plot Showing Changes in Total Motile Sperm Count Parameters Within Participants Before and After COVID-19 Vaccination.
Each bar represents an individual participant.
Discussion
In this study of sperm parameters before and after 2 doses of a COVID-19 mRNA vaccine, there were no significant decreases in any sperm parameter among this small cohort of healthy men. Because the vaccines contain mRNA and not the live virus, it is unlikely that the vaccine would affect sperm parameters. While these results showed statistically significant increases in all sperm parameters, the magnitude of change is within normal individual variation and may be influenced by regression to the mean.5 Additionally, the increase may be due to the increased abstinence time before the second sample. Men with oligospermia did not experience further decline.
The limitations of the study include the small number of men enrolled; limited generalizability beyond young, healthy men; short follow-up; and lack of a control group. In addition, while semen analysis is the foundation of male fertility evaluation, it is an imperfect predictor of fertility potential. Despite this, the study’s time frame encompasses the full life cycle of sperm.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Szilagyi PGTK, Thomas K, Shah MD, et al. National trends in the US public’s likelihood of getting a COVID-19 vaccine: April 1 to December 8, 2020. JAMA. 2020;325(4):396-398. doi: 10.1001/jama.2020.26419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berry SD, Johnson KS, Myles L, et al. Lessons learned from frontline skilled nursing facility staff regarding COVID-19 vaccine hesitancy. J Am Geriatr Soc. 2021;69(5):1140-1146. doi: 10.1111/jgs.17136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Best JC, Kuchakulla M, Khodamoradi K, et al. Evaluation of SARS-CoV-2 in human semen and effect on total sperm number: a prospective observational study. World J Mens Health. 2021;39(e12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper TG, Noonan E, von Eckardstein S, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16(3):231-245. doi: 10.1093/humupd/dmp048 [DOI] [PubMed] [Google Scholar]
- 5.Keel BA. Within- and between-subject variation in semen parameters in infertile men and normal semen donors. Fertil Steril. 2006;85(1):128-134. doi: 10.1016/j.fertnstert.2005.06.048 [DOI] [PubMed] [Google Scholar]