Abstract
South Asian (SA) individuals represent a large, growing population in a number of European countries. These individuals, particularly first-generation SA immigrants, are at higher risk of developing type 2 diabetes, atherogenic dyslipidaemia, and coronary heart disease than most other racial/ethnic groups living in Europe. SAs also have an increased risk of stroke compared to European-born individuals. Despite a large body of conclusive evidence, SA-specific cardiovascular health promotion and preventive interventions are currently scarce in most European countries, as well as at the European Union level. In this narrative review, we aim to increase awareness among clinicians and healthcare authorities of the public health importance of cardiovascular disease among SAs living in Europe, as well as the need for tailored interventions targeting this group – particularly in countries where SA immigration is a recent phenomenon. For this purpose, we review key studies on the epidemiology and risk factors of cardiovascular disease in SAs living in the United Kingdom, Italy, Spain, Denmark, Norway, Sweden, and other European countries. Building on these, we discuss potential opportunities for multi-level, targeted, tailored cardiovascular prevention strategies. Because lifestyle interventions often face important cultural barriers in SAs, particularly for first-generation immigrants, we also discuss features that may help maximise the effectiveness of those interventions. Finally, we evaluate knowledge gaps, currently available risk stratification tools such as QRISK-3, and future directions in this important field.
Keywords: cardiovascular disease, coronary heart disease, diabetes, physical activity, prevention, South Asian
Graphical Abstract
Introduction
According to the 2016 European Society of Cardiology (ESC) guidelines for cardiovascular disease (CVD) prevention, first-generation South Asian (SA) immigrants living in Europe should have their Systematic Coronary Risk Evaluation (SCORE) estimates multiplied by a 1.4 correction factor.1 Similarly, the American College of Cardiology and American Heart Association list SA ethnicity as a “risk enhancer” for 10-year CVD risk estimations.2
These recommendations are the result of a wealth of research studies published since the 1950s, conducted in South Asia as well as in groups of SA immigrants living across the globe, which have demonstrated a higher cardiovascular and particularly coronary heart disease (CHD) risk in SA individuals compared to most other racial/ethnic groups.3–25
In Europe, SAs represent one of the largest, fastest growing minority groups in a number of countries, including the United Kingdom (UK), Italy, Germany, France, Spain, Greece, Switzerland, the Scandinavian countries, and the Netherlands.26 Research in these countries has consistently described individuals of SA ethnicity as having a higher burden of type 2 diabetes (T2D) and CHD compared to other local racial/ethnic groups.11–25 Some studies have also demonstrated a higher risk of stroke in SAs compared to local Whites.12–14,18,22 Despite this large body of evidence and recent calls for action,27,28 SA-specific health promotion and preventive interventions are scarce in most European countries – as well as at the European Union level.
The aim of this narrative review is to increase awareness among clinicians and healthcare authorities of the importance of CVD in SA individuals living in Europe, as well as the need for aggressive preventive interventions targeting this group – particularly first-generation immigrants. For this purpose, we review European studies on the epidemiology of CVD in SAs, and discuss opportunities for prevention tailored to their unique risk profile. We also evaluate features that may maximise the effectiveness of those interventions in a context of cultural barriers. Finally, we evaluate knowledge gaps, currently available risk stratification tools such as QRISK-3, and future directions in this important field.
Demography of SA immigration to Europe
As of 2018, South Asia (i.e., India, Pakistan, Bangladesh, Sri Lanka, Nepal, Bhutan, and Maldives) accounted for 23% of the world’s population – approximately 1,750 million men and women.29 In addition, an estimated 20 million SAs live in other diaspora countries.30 This includes large communities in the United States (US), Canada, the Middle East, Malaysia, South Africa, Australia, and several European countries, among others.
According to EuroStat, more than 2.5 million first-generation SA immigrants lived in Europe as of 2011.26 The UK currently hosts the largest SA population living in Europe, with approximately 1.85 million first-generation SA immigrants registered in the national census of November 2018, and more than 3 million people of SA ethnicity.31 This is likely the consequence of longstanding colonial and post-colonial ties between the UK, India and Pakistan, together with the large diaspora that followed the partition of India in 1947.
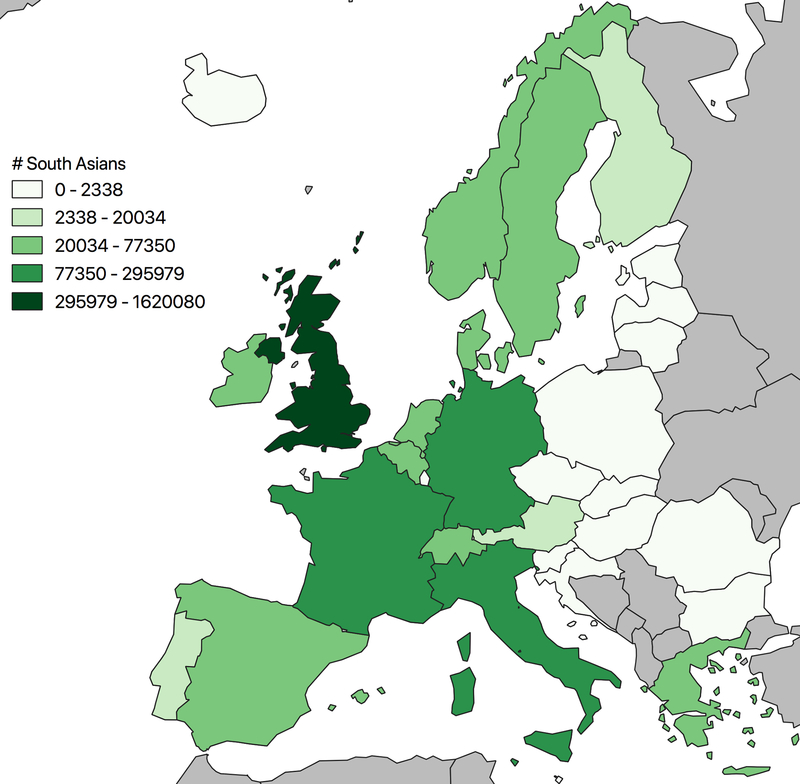
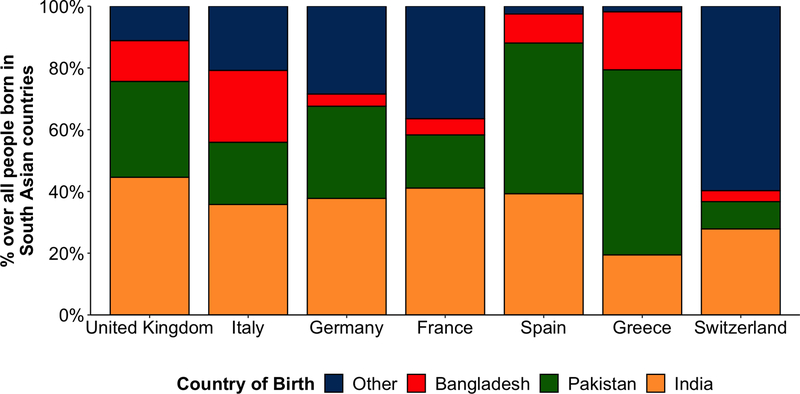
Besides the UK, large groups of SAs, mostly first-generation immigrants, live in many other European regions (Figure 1). India is the most frequent country of origin, followed by Pakistan (Figure 2). In countries such as Italy and Spain, where SA immigration is a relatively recent phenomenon, SAs represent a young, mostly male group.15,18,32 Conversely, in the UK, where this phenomenon has been occurring for almost a century, the SA population is closer to the local in terms of age/sex distribution.31
Figure 1.
First generation SA immigrants living in Europe as of 2011.
Source: EuroStats 2011
Figure 2.
National origin among large SA communities in Europe.
Source: EuroStats 2011
Marked socioeconomic contrasts exist between individuals of Indian origin living in the UK, who have a high average household income33 (similarly to what has been reported in the US34), and Pakistanis and Bangladeshis living in the UK and other European countries, such as Spain, who face more adverse conditions.32,33
Epidemiology of CVD in SAs Living in Europe
A large number of studies have evaluated the importance of CVD and particularly CHD in individuals of SA ancestry. These include studies in South Asia, which have shown higher event and mortality rates than those reported in Western countries;3,4 multinational studies such as INTERHEART or Prospective Urban Rural Epidemiology (PURE), in which SA countries lead the incidence of CHD events worldwide, occurring almost a decade earlier than in other world regions;5,6 studies in non-European countries, where SA immigrants have higher CHD event rates and mortality than their local counterparts;7–10 and research conducted in Europe.11–25
A summary of some European cohort and population-based studies is presented in Table 1. For decades, the UK has led international research in this field. First-generation SA immigrants have the highest UK CHD death rates since the 1970s,11,12 with very high cerebrovascular death rates also reported in some subgroups, such as Bangladeshis.12 Also, landmark cohort studies have shown individuals of SA ethnicity to have the highest incidence of CVD among all racial/ethnic groups in the UK, particularly Pakistanis and Bangladeshi women.13 Importantly, in many of these studies such excess risk was independent of the established risk factors.
Table 1.
Example European studies on the epidemiology of CVD and CHD among SA immigrants.
| Country | Author | Pub. year | Area | Study period | Main findings | Ref. |
|---|---|---|---|---|---|---|
| Mortality | ||||||
| UK | McKeigue | 1988 | England, Wales | 1970–1972 | SA men and women had 50% higher CHD mortality than the national average | 11 |
| UK | Wild | 2007 | England, Wales | 2001–2003 | Standardised mortality rates for circulatory disease death in Bangladeshis were the highest of all 13 groups assessed. For CHD, men: local 96, Pakistani 162, Indian 131, Bangladeshi 175; women: 97, 174, 149 and 167 | 12 |
| Italy | Fedeli | 2015 | Veneto | 2008–2013 | SAs had the highest SMRs (compared to Italians) for CHD death of all 7 immigrant groups assessed: 2.53 for men, 4.53 for women | 14 |
| Spain | Regidor | 2009 | National data | 2001–2005 | SA men had the highest age-adjusted CVD mortality across Spaniards and 9 immigrant groups. Compared to Spaniards, MRRs for CHD were 2.8 for SAs men; for CeVD, 3.6 for SA men and 2.2 for women | 17 |
| Various | Ikram | 2016 | – | 1992–2007 | Pooling data from Denmark, England & Wales, France, the Netherlands, Scotland, and Spain, SA immigrants had a higher CVD mortality compared to European-borns | 25 |
| Prevalence and Incidence | ||||||
| UK | Hippisley-Cox | 2017 | England | 1998–2015 | Compared to local Whites, Pakistanis and Bangladeshi women had 70% higher CVD risk, Indians and Bangladeshi men 30% higher risk | 13 |
| Italy | Fedeli | 2018 | Veneto | 2015 | SAs had the highest risk of CHD compared to Italians and other immigrant groups | 15 |
| Spain | Cainzos-Achirica | 2019 | Catalonia | 2017 | SAs had the highest prevalence of CHD compared to Spaniards and other 4 immigrant groups. SA women ages 60–79 years had the highest prevalence of CeVD among women | 18 |
| Denmark | Hempler | 2011 | Capital, Central Regions | 1997–2000 | Pakistanis had a higher incidence of CVD and AMI than Danes, Turks, and Former Yugoslavians. Age- and socioeconomic status-adjusted RRs of CVD compared to Danes were 1.40 and 1.77 for Pakistani men and women, respectively | 20 |
| Norway | Rabanal | 2015 | National data | 1994–2009 | SAs had the highest risk of AMI/stroke hospitalization compared to locals and 13 immigrant groups. AMI SERs in men: Norwegians 386, SAs 812; women: Norwegians 98, SAs 216 | 22 |
| Sweden | Hedlund | 2007 | Stockholm County | 1977–1996 | Compared to Swedish-borns, age- and sex-adjusted RR of first AMI in SA was 1.50 for men, 2.06 for women | 23 |
Abbreviations: AMI, acute myocardial infarction; CHD, coronary heart disease; CeVD, cerebrovascular disease; CVD, cardiovascular disease; MRR, mortality rate ratio; RR, relative risk; SA, South Asian; SER, standardised event rate; SMR, standardised mortality ratio; UK, United Kingdom
Due to space limitations this list is not exhaustive but rather, presents a summary of cohort, population-based and mortality statistics studies from key European countries.
The second-largest European SA population lives in Italy.26 In this country, SAs have the highest cardiovascular mortality rates,14 prevalence of CHD15 and hospitalisation rates for acute myocardial infarction (AMI).16 SAs living in Italy also present a higher risk of stroke than the local population.14 Similar observations have been reported in Spain,17,18 where SAs hospitalised for a first AMI are in average younger and have more severe coronary atherosclerosis than their local counterparts.19
SA immigrants also lead the incidence of CHD/CVD in Denmark,20 Norway,21,22 and Sweden.23 In addition, studies pooling data from several European countries, including France and the Netherlands, confirm a higher CVD mortality among SA immigrants compared to European-born individuals.24,25
Why are SAs living in Europe at higher cardiovascular risk?
Although many epidemiological studies have considered SAs to be a single, homogeneous group, the SA ethnicity is actually highly heterogeneous.35 This may explain why almost every known cardiovascular risk factor has been described as potentially relevant to SAs, as well as some inconsistent observations regarding the importance of specific risk factors across studies. Additional heterogeneity must also be recognised within Europe, the UK accumulating several generations of progressively acculturated SAs, while most SAs living in Mediterranean Europe are first-generation immigrants.
Despite this diversity, some factors have consistently been described as highly prevalent in almost all SA subgroups evaluated, particularly first-generation SA immigrants; both in Europe and elsewhere. Among them, glucose metabolism abnormalities and particularly T2D are almost ubiquitous.3,5–7,10,13,15,18,19,27,30,36,37 Not only is T2D highly prevalent in SAs living in Europe, but once diagnosed, average glycosylated haemoglobin levels tend to be higher in first-generation SAs than in other groups.38,39 Nonetheless, promising temporal trends have been reported in the UK in the management and outcomes of T2D in SAs,40 with appropriate treatment substantially attenuating SA’s excess CVD risk.40 Among SA national origins, Bangladeshis have the highest risk of developing T2D.41
Several underlying mechanisms have been proposed for the T2D epidemic in SAs, including lifestyle features, epigenetic signalling related to impaired beta-cell function, and body composition: for a given body mass index [BMI], SAs have less lean tissue, and higher proportions of fat mass and fat in abdominal deposits, than Whites40 – resulting in a higher prevalence of abdominal obesity and of T2D for a given BMI. This has led to the recommendation by the World Health Organization to use use lower BMI thresholds to define overweight (BMI ≥23kg/m2) and obesity (BMI ≥27.5kg/m2) in Asians.42 Among them, low levels of physical activity and low fitness5,6,10,27,30,37,40,43 appear as key preventable risk factors. Frequent intake of sugar-rich snacks and drinks may also play a role, at least in some SA subgroups.44,45
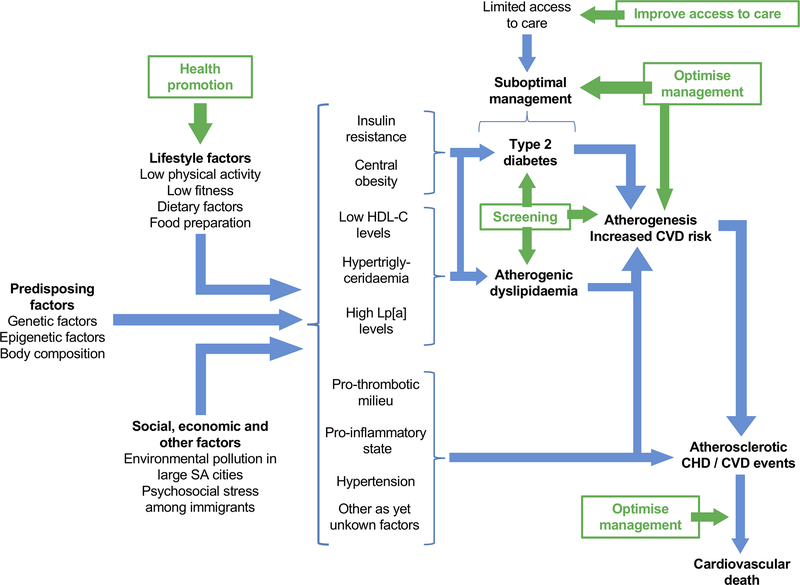
Other features proposed as potentially relevant to SAs’ cardiovascular risk include additional dietary factors, such as intake of foods rich in saturated/trans fats (e.g., ghee, a type of clarified butter, although this practice is lessening in many SA communities),27,39,40 high-heat food preparation,46 and reutilisation of cooking oil;46 atherogenic dyslipidaemia, with low levels of high density lipoprotein cholesterol, hypertriglyceridemia, and small dense low density lipoprotein particles;3,7,13,19,27,30,36,47 high levels of lipoprotein [a];7,27,48 obesity, particularly among women;18,49 pro-thrombotic/pro-inflammatory states;7,27,36,48 endothelial dysfunction;27,48 and social factors, including low birth weight50 and migration-associated stress; among others (Figure 3).27,30,48,51,52 Importantly, none of these factors is directly captured in usual risk scores,1,13 and to what extent any of these, either in isolation or collectively, help explain the excess risk in SAs is currently not fully established, and future collaborative efforts are needed to examine these issues.
Figure 3.
Factors potentially involved in excess CVD risk in SAs living in Europe, and opportunities for targeted interventions.
Abbreviations: CHD, coronary heart disease; CVD, cardiovascular disease; HDL-C, high density lipoprotein cholesterol; Lp[a], lipoprotein [a]; SA, South Asian
In green, opportunities for preventive/therapeutic interventions.
Regarding hypertension, published reports have yielded heterogeneous findings, likely due to differing risks in different SA subgroups.13,15,18,19,52–54 For toxic substances, most European research has described tobacco smoking being less relevant to the risk profile of SA immigrants than to that of local populations,13,18,19,53 although this may not be true for some subgroups of Bangladeshi men.55 Cocaine/substance abuse also seems more relevant as a risk factor for early AMI among some European populations, such as Spaniards, than in SAs.19,56 Finally, whether other factors, such as blood vessel size/morphology57,58 are also relevant to SAs’ excess risk should be examined further.
SAs in European CVD prevention guidelines
The size and growth of the SA population in some European regions represents a challenge for local healthcare systems which were designed for the care of lower-CVD-risk populations.1 It is therefore crucial to develop tailored health promotion and preventive interventions focused specifically on these individuals. Such interventions are likely not only to have large health benefits, but also to contribute to the sustainability of local healthcare systems.
Nonetheless, SA-specific recommendations for CVD prevention, risk assessment and management included in key ESC prevention documents are currently very few.1,59,60 These refer to 1) use of a crude 1.4 correction factor for SCORE risk estimations, and 2) tailored waist circumference thresholds (≥90cm in men, ≥80cm in women) when defining central obesity in SAs.
At the local level, although recommendations are also scarce in the National Institute for Health and Care Excellence (NICE) CVD prevention document,61 NICE guidelines for the management of specific cardiovascular risk factors, particularly T2D, include detailed guidance for individual- and group-level interventions targeting SAs.62 Conversely, in other European countries, SA-specific recommendations are, to our knowledge, currently very limited. We believe such omissions need to be corrected.
Opportunities for tailored CVD prevention interventions for SAs in Europe
The current scarcity of available guidance highlights the need for further national- and European-level efforts. Below we discuss some proposed multi-level, tailored interventions (Figure 3, in green). Although most of them are likely to be relevant to all racial/ethnic groups living in Europe, they may be particularly beneficial for SAs provided their unique risk profile. In a context of limited resources for public health interventions, governments may want to prioritise some of these interventions when designing SA-specific CVD prevention programs.
A first key intervention should be the aggressive, multi-level promotion of daily physical activity (Table 2), given its beneficial effects on fitness, prevention of T2D, lipid levels, blood pressure, and body weight.63–67 Importantly, regular physical activity has been associated with a 50% lower risk of CHD events even among individuals at high genetic CHD risk,68 and is also highly beneficial in individuals with established T2D.69–71 Sedentary jobs -such as shop clerks and car drivers- are very common among SA immigrant men,72 therefore, interventions promoting regular physical activity to travel to, or at the work place itself, may be particularly valuable.
Table 2.
Proposed multi-level approaches for the promotion of regular physical activity among SAs.
| Approaches |
|---|
| Communicate |
| Importance of cardiovascular disease as cause of premature death and morbidity in SAs |
| Use appealing messages: Improving activity levels can be simple, fun, help socialise, reduce stress, and lower risk of diabetes and heart disease |
| Engage |
| Empower SAs as advocates of their own, family and community cardiovascular health |
| Community leaders, local SA organizations and media |
| Employers |
| Healthcare professionals |
| Cardiovascular scientific societies |
| Local governments, public health service providers, healthcare managers |
| Interventions at the work place |
| Physically active commute: walk, cycle or mixed mode – if not on a daily basis, 1–3 times/week |
| Minimise periods of sitting |
| Increase physical activity: go for short walks, walking meetings, walk during phone calls, active lunch breaks, use stairs |
| Interventions during leisure time |
| Allocate at least 45min/day at least 5 days/week for brisk walking, dancing, or other cardio |
| Maximise participation in physically active group activities, local sports and competitions |
| Interventions in SA communities |
| Group information sessions |
| Education interventions encouraging SA boys and girls to take an interest in sports |
| Interventions targeting women |
| Structural interventions in key neighbourhoods |
| Increase availability of safe green spaces and walkable areas |
| Affordable fitness centres |
| Motivational tools |
| Wearable devices to monitor daily physical activity |
| Information technologies facilitating peer communication and competition |
| Incentives at the work place |
| Research |
| Cultural practices/beliefs regarding sedentary behaviours |
| Cultural adaptations maximising acceptability of interventions |
| Evaluate adherence and effectiveness |
Abbreviations: SA, South Asian
Regarding diet, key sources of saturated fat (e.g., ghee) should be replaced with healthier fats. Low intake of sugar-rich foods should also be recommended, mirroring international recommendations for pre-diabetic and diabetic patients.70,71 In Spain, a Mediterranean diet with high intake of extra virgin olive oil or nuts reduced the incidence of CVD and T2D compared to a low-fat diet with a higher proportion of carbohydrates.73,74 In PURE, high carbohydrate intake was associated with higher CVD events and death, particularly in SAs.75
Early detection of T2D and dyslipidaemia should also be a priority among SAs, with lower age and BMI thresholds considered for screening. Accurate risk stratification and optimal, personalised therapeutic management should be pursued as well, including appropriate use of statins and glucose-lowering medications.40,76 For all these to happen, cardiovascular health information and other public health campaigns, improved access to care, and increased awareness within the medical community are likely to be key first steps to intervention.
Maximising the effectiveness of preventive efforts in SAs
Interventions may face important cultural barriers in SA communities, particularly among first-generation immigrants, and some adaptations may be necessary. Indeed, lifestyle change intervention studies in SAs living in industrialised countries have so far yielded modest results.77
First, interventions should be holistic and culturally adapted for SAs, making them understandable, acceptable, and relevant to their context and income. For this purpose, cultural mediators and community leaders should be involved, from the design phase to dissemination. Interventions may include, for example, promotion of healthy cooking methods; identification of local sources of affordable, healthy foods; or improved communication of cardiovascular prevention/screening programs available within the local public healthcare system.
Interventions at the individual level may face barriers derived from group values and traditions, and should be combined with community interventions. These may help identify and overcome some of those barriers, thus facilitating paradigm change at the group level;78 maximise dissemination of preventive initiatives within SA communities, and inform further cultural adaptations of individual-level interventions.
For women, who tend to have less access to the job market,72 household and community sessions as well as interventions within the primary care system may be more effective. Of note, because in many SA households, women take care of the nutrition of the entire family, healthy diet counselling for women may have multiplicative health benefits.
Finally, to maximise the effectiveness of the proposed interventions not only SA individuals, organisations and community leaders should be involved, but also key local stakeholders such as those listed in Table 2.
Acculturation and Healthcare Utilization: Opportunities to Further Improve the Cardiovascular Health of South Asians Living in Europe
Studies conducted in the UK show that second-generation individuals of SA ancestry living in the UK have incorporated some healthy behaviors compared to first-generation immigrants, particularly higher levels of frequent physical activity.79 This, together with increased provider awareness and improved access to / utilization of healthcare, which may result in the early detection of diabetes, the improved lifelong therapeutic management of diabetes and of other cardiovascular risk factors, and an optimised management of cardiovascular risk in second and subsequent generation immigrants, among other improvements have been proposed as potential mechanisms explaining the lower rates of CVD observed in contemporary SAs, most of which are second/third generation individuals.40 Indeed, evidence accumulated from studies spanning several decades suggest the excess mortality in SAs with diabetes compared to their white counterparts has been attentuating over time as have CVD morbidity patterns;40 but further work is needed to validate these changes.
In Southern Europe, where SA immigration is still a recent phenomenon, acculturation to the Mediterranean lifestyle, which includes not only the Mediterranean diet but also frequent physical activity,80 would be expected to result in improved cardiovascular health. Nevertheless, studies on second-generation SAs are currently lacking, and further research is needed to better understand the outcome of progressive Mediterranean acculturation in this ethnic group. Regarding healthcare access, recent epidemiological studies in countries such as Spain or Italy suggest that access of first-generation SA immigrants to some cardiovascular therapies is concerningly lower than among the local population. For example, in a recent population-based study conducted in Catalonia (Spain),18 despite having similar rates of dyslipidemia and much higher rates of diabetes than Catalans, the frequency of statin use among SAs was much lower. Use of antidiabetic medications has also been observed to be low among SAs living in Spain.39 Similarly, a recent study carried out in the Lombardia Region (Northern Italy, aprox. 10 million inhabitants) showed that South Asian immigrants with diabetes received fewer drugs for cardiovascular prevention (e.g. statins, ACE-inhibitors) than Italians; such indicators were more favourable among SAs with longer duration of stay in Italy.38 These and other studies stress the need for additonal efforts in Southern European countries, aimed at ensuring the optimal therapeutic and risk management of these individuals.
In the US, a country which has also been receiving SA immigrants for decades, studies suggest that SA acculturation to the US lifestyle has yielded improvements in some risk factors.81 Nevertheless, incorporation of deleterious habits such as high intake of red meat, sugar-rich drinks and processed foods has also occurred.27,82 In the MASALA study, bicultural SAs (those who adopt some American beliefs/behaviors and retain some SA ones) have the lowest carotid intima-media thickness and lower fasting glucose and 2-hour glucose.81 With regards to healthcare access and utilization, US studies describe very high rates of statin use among SAs.83
Next steps
Despite a large body of published literature, several knowledge gaps still remain in SAs living in Europe (Table 3). These include a better characterization of the potential genetic and epigenetic factors underlying the very high prevalence of diabetes and atherogenic dyslipidemia observed in SAs; as well as of the potential role —if any— of consanguineous marriages, which are highly frequent in some SA communities.84,85 A better characterization is also needed of the anatomical, cultural, dietary and metabolic factors underpinning their premature CVD, both overall as well as for specific subgroups. Finally, a better understanding of the effects of acculturation, duration of migration, and genetic mix warranted as well.
Table 3.
Knowledge gaps in SAs living in Europe.
| Further characterisation of |
|---|
| Factors underlying SAs’ excess cardiovascular risk |
| Predisposing polymorphisms |
| Epigenetic factors |
| Coronary artery diameter and tortuosity |
| SA dietary patterns |
| Other novel risk factors |
| Heterogeneity |
| National and cultural heterogeneity |
| Effect of immigrant duration |
| Cardiovascular risk in 2nd and 3rd generation SAs |
| Ethnically-mixed families |
| Differential effects of diabetes across SA subgroups |
| Other knowledge gaps |
| Subclinical atherosclerosis using imaging |
| Risk of heart failure |
| Pharmacokinetics of statins |
| Evaluation |
| Effectiveness of SA-specific preventive interventions |
| Benefits of Mediterranean diet subtypes |
Abbreviations: SA, South Asian
SA-targeted CVD prevention guidelines should be developed, particularly in countries where this group is large. Similarly, targeted policies are also needed. These should include provision of linguistically and culturally appropriate services, public awareness campaigns, ensure access to care, and allocation of sufficient research funds, among others. Besides local efforts, development of guidelines and policies at the European level will likely improve the dissemination, implementation and effectiveness of preventive interventions.
SA-specific CVD risk estimators should also be developed, accurately informing their risk management. In the UK, functions such as ETHRISK and QRISK-3 allow accounting for ethnicity.86,13 Moreover, QRISK3 also accounts for within-SA heterogeneity by country and sex, using 1.7 risk multipliers in Pakistanis and Bangladeshi women, and 1.3 factors for Indians and Bangladeshi men.13 In Norway, NORRISK 2 does not capture ethnicity, but a 1.5 multiplication factor is recommended in individuals of SA origin.87 Conversely, SA-specific functions are currently not available in other countries, such as Spain or Italy. Local risk estimators in such low-risk European countries would likely underestimate risk in SA immigrants, consequently, local development of SA-specific functions should be prioritised. Alternatively, adaptation and validation of ETHRISK or QRISK-3 to non-UK countries should also be considered. Until those tools are available, current ESC recommendations for CVD risk assessment in SAs1 should be implemented systematically.88
Conclusions
SAs living in Europe represent a large, growing population. A wealth of European epidemiological studies have shown SA immigrants to be at high risk of T2D, early coronary atherosclerosis, and CVD. Although further studies are warranted, there is currently conclusive evidence of the need for effective prevention interventions targeting this group. These should pay special attention to the promotion of regular physical activity and healthy diets, as well as to the screening and aggressive management of cardiovascular risk factors, particularly T2D. Interventions should involve all key stakeholders and be multi-level, culturally adapted, appealing, and easy to incorporate. Accurate CVD risk assessment and management in SAs should also be prioritised, using relevant risk scores where available or appropriate adjustment factors. Implementation of these recommendations at both the local and European level will likely have large health benefits, contribute to the sustainability of local healthcare systems, and benefit our Society as a whole.
HIGHLIGHTS.
South Asian (SA) individuals represent a large, growing population in a number of European countries
SAs, particularly first-generation immigrants, are at higher risk of developing type 2 diabetes, atherogenic dyslipidaemia, and coronary heart disease than most other racial/ethnic groups living in Europe
SA-specific cardiovascular health promotion and preventive interventions are currently scarce in most European countries, as well as at the European Union level
In this review we aim to increase awareness among clinicians and healthcare authorities of the public health importance of cardiovascular disease among SAs living in Europe
We discuss potential opportunities for multi-level, targeted, tailored cardiovascular prevention strategies
Acknowledgments
The authors would like to thank Drs. Josepa Mauri, Montse Cleries, Fernando García, and Emili Vela, for their critical review and valuable input on the present manuscript.
ABBREVIATIONS AND ACRONYMS
- AMI
acute myocardial infarction
- BMI
body mass index
- CHD
coronary heart disease
- CVD
cardiovascular disease
- ESC
European Society of Cardiology
- NICE
National Institute for Health and Care Excellence
- PURE
Prospective Urban Rural Epidemiology
- SA
South Asian
- SCORE
Systematic Coronary Risk Evaluation
- T2D
type 2 diabetes
- UK
United Kingdom
- US
United States
Abbreviations:
- CHD
coronary heart disease
- CVD
cardiovascular disease
Footnotes
Conflicts of Interest
The authors declare that they have no conflicts of interest relevant to the content of this manuscript.
REFERENCES
- 1.Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corrà U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Løchen ML, Löllgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM, Binno S; ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J. 2016;37:2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC Jr, Sperling L, Virani SS, Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018. November 8. pii: S0735–1097(18)39034-X. doi: 10.1016/j.jacc.2018.11.003. [Epub ahead of print] [DOI] [Google Scholar]
- 3.Mohan V, Deepa R, Rani SS, Premalatha G; Chennai Urban Population Study (CUPS No.5). Prevalence of coronary artery disease and its relationship to lipids in a selected population in South India: The Chennai Urban Population Study (CUPS No. 5). J Am Coll Cardiol. 2001;38:682–7. [DOI] [PubMed] [Google Scholar]
- 4.Soman CR, Kutty VR, Safraj S, Vijayakumar K, Rajamohanan K, Ajayan K; PROLIFE Study Group. All-cause mortality and cardiovascular mortality in Kerala state of India: results from a 5-year follow-up of 161,942 rural community dwelling adults. Asia Pac J Public Health. 2011;23:896–903. [DOI] [PubMed] [Google Scholar]
- 5.Yusuf S, Hawken S, Ounpuu S, on behalf of the INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. [DOI] [PubMed] [Google Scholar]
- 6.Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, Bo J, Lou Q, Lu F, Liu T, Yu L, Zhang S, Mony P, Swaminathan S, Mohan V, Gupta R, Kumar R, Vijayakumar K, Lear S, Anand S, Wielgosz A, Diaz R, Avezum A, Lopez-Jaramillo P, Lanas F, Yusoff K, Ismail N, Iqbal R, Rahman O, Rosengren A, Yusufali A, Kelishadi R, Kruger A, Puoane T, Szuba A, Chifamba J, Oguz A, McQueen M, McKee M, Dagenais G; PURE Investigators. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371:818–27. [DOI] [PubMed] [Google Scholar]
- 7.Anand SS, Yusuf S, Vuksan V, Devanesen S, Teo KK, Montague PA, Kelemen L, Yi C, Lonn E, Gerstein H, Hegele RA, McQueen M. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE). Lancet. 2000;356:279–84. [DOI] [PubMed] [Google Scholar]
- 8.Hajra A, Li Y, Siu S, Udaltsova N, Armstrong MA, Friedman GD, Klatsky AL. Risk of coronary disease in the South Asian American population. J Am Coll Cardiol. 2013;62:644–5. [DOI] [PubMed] [Google Scholar]
- 9.Danaraj TJ, Acker MS, Danaraj W, Wong HO, Tan BY. Ethnic group differences in coronary heart disease in Singapore: an analysis of necropsy records. Am Heart J. 1959;58:516–26. [DOI] [PubMed] [Google Scholar]
- 10.Tuomilehto J, Ram P, Eseroma R, Taylor R, Zimmet P. Cardiovascular diseases and diabetes mellitus in Fiji: analysis of mortality, morbidity and risk factors. Bull World Health Organ. 1984;62:133–43. [PMC free article] [PubMed] [Google Scholar]
- 11.McKeigue PM, Marmot MG. Mortality from coronary heart disease in Asian communities in London. BMJ. 1988;297:903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wild SH, Fischbacher C, Brock A, Griffiths C, Bhopal R. Mortality from all causes and circulatory disease by country of birth in England and Wales 2001–2003. J Public Health (Oxf). 2007;29:191–8. [DOI] [PubMed] [Google Scholar]
- 13.Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ. 2017;357:j2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fedeli U, Ferroni E, Pigato M, Avossa F, Saugo M. Causes of mortality across different immigrant groups in Northeastern Italy. PeerJ. 2015;3:e975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fedeli U, Avossa F, Ferroni E, Schievano E, Bilato C, Modesti PA, Corti MC. Diverging patterns of cardiovascular diseases across immigrant groups in Northern Italy. Int J Cardiol. 2018;254:362–367. [DOI] [PubMed] [Google Scholar]
- 16.Fedeli U, Cestari L, Ferroni E, Avossa F, Saugo M, Modesti PA. Ethnic inequalities in acute myocardial infarction hospitalization rates among young and middle-aged adults in Northern Italy: high risk for South Asians. Intern Emerg Med. 2018;13:177–182. [DOI] [PubMed] [Google Scholar]
- 17.Regidor E, Astasio P, Calle ME, Martínez D, Ortega P, Domínguez V. The association between birthplace in different regions of the world and cardiovascular mortality among residents of Spain. Eur J Epidemiol. 2009;24:503–12. [DOI] [PubMed] [Google Scholar]
- 18.Cainzos-Achirica M, Vela E, Cleries M, Bilal U, Mauri J, Pueyo MJ, Rosas A, Enjuanes C, Blaha MJ, Kanaya AM, Comin-Colet J. 2019. February 28. pii: heartjnl-2018–314436. doi: 10.1136/heartjnl-2018-314436. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Caínzos-Achirica M, García-García C, Elosua R, Piulats N, Recasens L, Bruguera-Cortada J. Myocardial infarction in South Asian immigrants in Catalonia. Results from the ASIAM Study. Rev Esp Cardiol (Engl Ed). 2013;66:405–7. [DOI] [PubMed] [Google Scholar]
- 20.Hempler NF, Larsen FB, Nielsen SS, Diderichsen F, Andreasen AH, Jørgensen T. A registry-based follow-up study, comparing the incidence of cardiovascular disease in native Danes and immigrants born in Turkey, Pakistan and the former Yugoslavia: do social inequalities play a role? BMC Public Health. 2011;11:662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rabanal KS, Meyer HE, Tell GS, Igland J, Pylypchuk R, Mehta S, Kumar B, Jenum AK, Selmer RM, Jackson R. Can traditional risk factors explain the higher risk of cardiovascular disease in South Asians compared to Europeans in Norway and New Zealand? Two cohort studies. BMJ Open. 2017;7:e016819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rabanal KS, Selmer RM, Igland J, Tell GS, Meyer HE. Ethnic inequalities in acute myocardial infarction and stroke rates in Norway 1994–2009: a nationwide cohort study (CVDNOR). BMC Public Health. 2015;15:1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hedlund E, Lange A, Hammar N. Acute myocardial infarction incidence in immigrants to Sweden. Country of birth, time since immigration, and time trends over 20 years. Eur J Epidemiol. 2007;22:493–503. [DOI] [PubMed] [Google Scholar]
- 24.Ikram UZ, Mackenbach JP, Harding S, Rey G, Bhopal RS, Regidor E, Rosato M, Juel K, Stronks K, Kunst AE. All-cause and cause-specific mortality of different migrant populations in Europe. Eur J Epidemiol. 2016;31:655–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rafnsson SB, Bhopal RS, Agyemang C, Fagot-Campagna A, Harding S, Hammar N, Hedlund E, Juel K, Primatesta P, Rosato M, Rey G, Wild SH, Mackenbach JP, Stirbu I, Kunst AE. Sizable variations in circulatory disease mortality by region and country of birth in six European countries. Eur J Public Health. 2013;23:594–605. [DOI] [PubMed] [Google Scholar]
- 26.Eurostat. Population by country of birth at national level. Available at: http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=cens_11cob_n&lang=en (Accessed February 7, 2019)
- 27.Volgman AS, Palaniappan LS, Aggarwal NT, Gupta M, Khandelwal A, Krishnan AV, Lichtman JH, Mehta LS, Patel HN, Shah KS, Shah SH, Watson KE; American Heart Association Council on Epidemiology and Prevention; Cardiovascular Disease and Stroke in Women and Special Populations Committee of the Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; and Stroke Council. Atherosclerotic Cardiovascular Disease in South Asians in the United States: Epidemiology, Risk Factors, and Treatments: A Scientific Statement From the American Heart Association. Circulation. 2018;138:e1–e34. [DOI] [PubMed] [Google Scholar]
- 28.Wong ND. Appreciating Cardiovascular Disease Risk in South Asians: The Time is Now. Available at: https://professional.heart.org/professional/ScienceNews/UCM_501317_Appreciating-Cardiovascular-Disease-Risk-in-South-Asians-The-Time-is-Now.jsp (Accessed February 7, 2019)
- 29.The World Bank. Total Population. Available at: https://data.worldbank.org/indicator/SP.POP.TOTL (Accessed February 7, 2019)
- 30.Ahmed ST, Rehman H, Akeroyd JM, Alam M, Shah T, Kalra A, Virani SS. Premature Coronary Heart Disease in South Asians: Burden and Determinants. Curr Atheroscler Rep. 2018;20:6. [DOI] [PubMed] [Google Scholar]
- 31.Office for National Statistics. Statistical bulletin: Migration Statistics Quarterly Report: February 2018. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/internationalmigration/bulletins/migrationstatisticsquarterlyreport/november2018 (Accessed February 7, 2019)
- 32.Generalitat de Catalunya. La població de nacionalitat pakistanesa a Catalunya. Available at: http://treballiaferssocials.gencat.cat/web/.content/03ambits_tematics/05immigracio_refugi/dades_immigracio/immigracio_en_xifres/La_immigracio_en_xifres_09-Pakistan.pdf (Accessed February 7, 2019)
- 33.GOV.UK. Household income. Ethnicity facts and figures. Available at: https://www.ethnicity-facts-figures.service.gov.uk/work-pay-and-benefits/pay-and-income/household-income/latest (Accessed February 7, 2019)
- 34.Pew Research Center. 5 facts about Indian Americans. Available at: http://www.pewresearch.org/fact-tank/2014/09/30/5-facts-about-indian-americans/ (Accessed February 7, 2019)
- 35.Bhopal R, Unwin N, White M, Yallop J, Walker L, Alberti KG, Harland J, Patel S, Ahmad N, Turner C, Watson B, Kaur D, Kulkarni A, Laker M, Tavridou A. Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: cross sectional study. BMJ. 1999;319:215–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chambers JC, Eda S, Bassett P, Karim Y, Thompson SG, Gallimore JR, Pepys MB, Kooner JS. C-Reactive Protein, Insulin Resistance, Central Obesity, and Coronary Heart Disease Risk in Indian Asians From the United Kingdom Compared With European Whites. Circulation 2001;10;145–150. [DOI] [PubMed] [Google Scholar]
- 37.Jenum AK, Diep LM, Holmboe-Ottesen G, Holme IM, Kumar BN, Birkeland KI. Diabetes susceptibility in ethnic minority groups from Turkey, Vietnam, Sri Lanka and Pakistan compared with Norwegians - the association with adiposity is strongest for ethnic minority women. BMC Public Health. 2012;12:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marzona I, Avanzini F, Tettamanti M, Vannini T, Fortino I, Bortolotti A, Merlino L, Genovese S, Roncaglioni MC. Prevalence and management of diabetes in immigrants resident in the Lombardy Region: the importance of ethnicity and duration of stay. Acta Diabetol. 2018;55:355–362. [DOI] [PubMed] [Google Scholar]
- 39.Franch-Nadal J, Martínez-Sierra MC, Espelt A, Sagarra-Busquets E, Patitucci-Gómez F, Goday-Arno A; redGDPS. The diabetic immigrant: cardiovascular risk factors and control. Contributions of the IDIME study. Rev Esp Cardiol (Engl Ed). 2013;66:39–46. [DOI] [PubMed] [Google Scholar]
- 40.Johns E, Sattar N. Cardiovascular and Mortality Risks in Migrant South Asians with Type 2 Diabetes: Are We Winning the Battle? Curr Diab Rep. 2017;17:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hippisley-Cox J, Coupland C, Robson J, Sheikh A, Brindle P. Predicting risk of type 2 diabetes in England and Wales: prospective derivation and validation of QDScore. BMJ. 2009;338:b880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. [DOI] [PubMed] [Google Scholar]
- 43.Ghouri N, Purves D, McConnachie A, Wilson J, Gill JM, Sattar N. Lower cardiorespiratory fitness contributes to increased insulin resistance and fasting glycaemia in middle-aged South Asian compared with European men living in the UK. Diabetologia. 2013;56:2238–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Simmons D, Williams R. Dietary practices among Europeans and different South Asian groups in Coventry. Br J Nutr. 1997;78:5–14. [DOI] [PubMed] [Google Scholar]
- 45.Emadian A, England CY, Thompson JL. Dietary intake and factors influencing eating behaviours in overweight and obese South Asian men living in the UK: mixed method study. BMJ Open. 2017;7:e016919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kakde S, Bhopal RS, Bhardwaj S, Misra A. Urbanized South Asians’ susceptibility to coronary heart disease: The high-heat food preparation hypothesis. Nutrition. 2017;33:216–224. [DOI] [PubMed] [Google Scholar]
- 47.Menon AS, Kotwal N, Singh Y, Girish R. Statins: Cholesterol guidelines and Indian perspective. Indian J Endocrinol Metab. 2015;19:546–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gupta M, Brister S. Is South Asian ethnicity an independent cardiovascular risk factor? Can J Cardiol 2006;22:193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shah A, Hernandez A, Mathur D, Budoff MJ, Kanaya AM. Adipokines and body fat composition in South Asians: results of the Metabolic Syndrome and Atherosclerosis in South Asians Living in America (MASALA) study. Int J Obes (Lond). 2012;36:810–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Margetts BM, Mohd Yusof S, Al Dallal Z, Jackson AA. Persistence of lower birth weight in second generation South Asian babies born in the United Kingdom. J Epidemiol Community Health. 2002;56:684–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Oxford Books. 2019. Bhopal RS. Epidemic of Cardiovascular Disease and Diabetes: Explaining the Phenomenon in South Asians Worldwide. [Google Scholar]
- 52.Agyemang C, van den Born BJ. Non-communicable diseases in migrants: an expert review. J Travel Med. 2018. October 20. doi: 10.1093/jtm/tay107. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 53.Cappuccio FP, Cook DG, Atkinson RW, Strazzullo P. Prevalence, detection, and management of cardiovascular risk factors in different ethnic groups in south London. Heart. 1997;78:555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Valerio L, Milozzi J, Figueredo A, Reina MD, Martínez-Cuevas O, Pérez-Quilez O. Prevalence of diabetes mellitus in young asian indian immigrants in Santa Coloma de Gramenet (Spain). Med Clin (Barc) 2006;126:53–6. [DOI] [PubMed] [Google Scholar]
- 55.Karlsen S, Millward D, Sandford A. Investigating ethnic differences in current cigarette smoking over time using the health surveys for England. Eur J Public Health. 2012;22:254–6. [DOI] [PubMed] [Google Scholar]
- 56.Andrés E, León M, Cordero A, Magallón Botaya R, Magán P, Luengo E, Alegría E, Casasnovas JA. Cardiovascular risk factors and lifestyle associated with premature myocardial infarction diagnosis. Rev Esp Cardiol. 2011;64:527–9. [DOI] [PubMed] [Google Scholar]
- 57.Makaryus AN, Dhama B, Raince J, Raince A, Garyali S, Labana SS, Kaplan BM, Park C, Jauhar R. Coronary artery diameter as a risk factor for acute coronary syndromes in Asian-Indians. Am J Cardiol. 2005;96:778–80. [DOI] [PubMed] [Google Scholar]
- 58.Tillin T, Dhutia H, Chambers J, Malik I, Coady E, Mayet J, Wright AR, Kooner J, Shore A, Thom S, Chaturvedi N, Hughes A. South Asian men have different patterns of coronary artery disease when compared with European men. Int J Cardiol. 2008;129:406–13. [DOI] [PubMed] [Google Scholar]
- 59.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 60.Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, Hoes AW, Jennings CS, Landmesser U, Pedersen TR, Reiner Ž, Riccardi G, Taskinen MR, Tokgozoglu L, Verschuren WMM, Vlachopoulos C, Wood DA, Zamorano JL, Cooney MT; ESC Scientific Document Group. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur Heart J. 2016;37:2999–3058. [DOI] [PubMed] [Google Scholar]
- 61.National Institute for Health and Care Excellence (NICE). Cardiovascular disease: risk assessment and reduction, including lipid modification. Available at: https://www.nice.org.uk/guidance/cg181 (Accessed February 7, 2019)
- 62.National Institute for Health and Care Excellence (NICE). Type 2 diabetes prevention: population and community-level interventions. Available at: https://www.nice.org.uk/guidance/ph35 (Accessed February 7, 2019)
- 63.Aune D, Norat T, Leitzmann M, Tonstad S, Vatten LJ. Physical activity and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis. Eur J Epidemiol. 2015;30:529–42. [DOI] [PubMed] [Google Scholar]
- 64.Kelley GA, Kelley KS. Vu Tran Z. Aerobic exercise, lipids and lipoproteins in overweight and obese adults: a meta-analysis of randomized controlled trials. Int J Obes (Lond) 2005;29: 881–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503. [DOI] [PubMed] [Google Scholar]
- 66.Ashor AW, Lara J, Siervo M, Celis-Morales C, Oggioni C, Jakovljevic DG, Mathers JC. Exercise modalities and endothelial function: a systematic review and dose-response meta-analysis of randomized controlled trials. Sports Med. 2015;45:279–96. [DOI] [PubMed] [Google Scholar]
- 67.Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, Bauman A, Lee IM; Lancet Physical Activity Series 2 Executive Committe; Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388:1302–10. [DOI] [PubMed] [Google Scholar]
- 68.Khera AV, Emdin CA, Drake I, Natarajan P, Bick AG, Cook NR, Chasman DI, Baber U, Mehran R, Rader DJ, Fuster V, Boerwinkle E, Melander O, Orho-Melander M, Ridker PM, Kathiresan S. Genetic Risk, Adherence to a Healthy Lifestyle, and Coronary Disease. N Engl J Med. 2016;375:2349–2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, Horton ES, Castorino K, Tate DF. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care. 2016;39:2065–2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Authors/Task Force Members, Rydén L, Grant PJ, Anker SD, Berne C, Cosentino F, Danchin N, Deaton C, Escaned J, Hammes HP, Huikuri H, Marre M, Marx N, Mellbin L, Ostergren J, Patrono C, Seferovic P, Uva MS, Taskinen MR, Tendera M, Tuomilehto J, Valensi P, Zamorano JL; ESC Committee for Practice Guidelines (CPG), Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S; Document Reviewers, De Backer G, Sirnes PA, Ezquerra EA, Avogaro A, Badimon L, Baranova E, Baumgartner H, Betteridge J, Ceriello A, Fagard R, Funck-Brentano C, Gulba DC, Hasdai D, Hoes AW, Kjekshus JK, Knuuti J, Kolh P, Lev E, Mueller C, Neyses L, Nilsson PM, Perk J, Ponikowski P, Reiner Z, Sattar N, Schächinger V, Scheen A, Schirmer H, Strömberg A, Sudzhaeva S, Tamargo JL, Viigimaa M, Vlachopoulos C, Xuereb RG. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J. 2013;34:3035–87. [DOI] [PubMed] [Google Scholar]
- 71.American Diabetes Association. 4. Lifestyle Management: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41:S38–S50. [DOI] [PubMed] [Google Scholar]
- 72.Metropolitan. Barcelona’s Pakistani community. Available at: https://www.barcelona-metropolitan.com/features/report-barcelona-pakistani-community/ (Accessed February 7, 2019)
- 73.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al. ; PREDIMED Study Investigators. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N Engl J Med 2018;378:e34. [DOI] [PubMed] [Google Scholar]
- 74.Salas-Salvadó J, Bulló M, Babio N, Martínez-González MÁ, Ibarrola-Jurado N, Basora J, et al. Erratum. Reduction in the Incidence of Type 2 Diabetes With the Mediterranean Diet: Results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care 2011;34:14–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dehghan M, Mente A, Zhang X, Swaminathan S, Li W, Mohan V, Iqbal R, Kumar R, Wentzel-Viljoen E, Rosengren A, Amma LI, Avezum A, Chifamba J, Diaz R, Khatib R, Lear S, Lopez-Jaramillo P, Liu X, Gupta R, Mohammadifard N, Gao N, Oguz A, Ramli AS, Seron P, Sun Y, Szuba A, Tsolekile L, Wielgosz A, Yusuf R, Hussein Yusufali A, Teo KK, Rangarajan S, Dagenais G, Bangdiwala SI, Islam S, Anand SS, Yusuf S; Prospective Urban Rural Epidemiology (PURE) study investigators. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017;390:2050–2062. [DOI] [PubMed] [Google Scholar]
- 76.Yusuf S, Bosch J, Dagenais G, Zhu J, Xavier D, Liu L, Pais P, López-Jaramillo P, Leiter LA, Dans A, Avezum A, Piegas LS, Parkhomenko A, Keltai K, Keltai M, Sliwa K, Peters RJ, Held C, Chazova I, Yusoff K, Lewis BS, Jansky P, Khunti K, Toff WD, Reid CM, Varigos J, Sanchez-Vallejo G, McKelvie R, Pogue J, Jung H, Gao P, Diaz R, Lonn E; HOPE-3 Investigators. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374:2021–2031. [DOI] [PubMed] [Google Scholar]
- 77.Ballotari P, Ferrari F, Ballini L, Chiarenza A, Manicardi V, Giorgi Rossi P. Lifestyle-tailored interventions for South Asians with type 2 diabetes living in high-income countries: a systematic review. Acta Diabetol. 2017;54:785–794. [DOI] [PubMed] [Google Scholar]
- 78.Gómez-Pardo E, Fernández-Alvira JM, Vilanova M, Haro D, Martínez R, Carvajal I, Carral V, Rodríguez C, de Miguel M, Bodega P, Santos-Beneit G, Peñalvo JL, Marina I, Pérez-Farinós N, Dal Re M, Villar C, Robledo T, Vedanthan R, Bansilal S, Fuster V. A Comprehensive Lifestyle Peer Group-Based Intervention on Cardiovascular Risk Factors: The Randomized Controlled Fifty-Fifty Program. J Am Coll Cardiol. 2016;67:476–85. [DOI] [PubMed] [Google Scholar]
- 79.Bhatnagar P, Shaw A, Foster C. Generational differences in the physical activity of UK South Asians: a systematic review. Int J Behav Nutr Phys Act. 2015;12:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mediterranean Diet Foundation. Mediterranean Diet Pyramid: a lifestyle for today. Available at: https://dietamediterranea.com/piramidedm/piramide_INGLES.pdf (Accessed February 7, 2019)
- 81.Kanaya AM, Ewing SK, Vittinghoff E, Herrington D, Tegeler C, Mills C, Kandula NR. Acculturation and subclinical atherosclerosis among U.S. South Asians: Findings from the MASALA study. J Clin Exp Res Cardiol 2014;1:102. [PMC free article] [PubMed] [Google Scholar]
- 82.Talegawkar SA, Kandula NR, Gadgil MD, Desai D, Kanaya AM. Dietary intakes among South Asian adults differ by length of residence in the USA. Public Health Nutr 2015:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Al Rifai M, Cainzos-Achirica M, Kanaya AM, Kandula NR, Dardardi Z, Joshi PH, Patel J, Budoff M, Yeboah J, Guallar E, Blumenthal RS, Blaha MJ. Discordance between 10-year cardiovascular risk estimates using the ACC/AHA 2013 estimator and coronary artery calcium in individuals from 5 racial/ethnic groups: Comparing MASALA and MESA. Atherosclerosis. 2018;279:122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hussain R. Community perceptions of reasons for preference for consanguineous marriages in Pakistan. J Biosoc Sci. 1999;31:449–61. [DOI] [PubMed] [Google Scholar]
- 85.Saleheen D, Zaidi M, Rasheed A, Ahmad U, Hakeem A, Murtaza M, Kayani W, Faruqui A, Kundi A, Zaman KS, Yaqoob Z, Cheema LA, Samad A, Rasheed SZ, Mallick NH, Azhar M, Jooma R, Gardezi AR, Memon N, Ghaffar A, Fazal-ur-Rehman, Khan N, Shah N, Ali Shah A, Samuel M, Hanif F, Yameen M, Naz S, Sultana A, Nazir A, Raza S, Shazad M, Nasim S, Javed MA, Ali SS, Jafree M, Nisar MI, Daood MS, Hussain A, Sarwar N, Kamal A, Deloukas P, Ishaq M, Frossard P, Danesh J. The Pakistan Risk of Myocardial Infarction Study: a resource for the study of genetic, lifestyle and other determinants of myocardial infarction in South Asia. Eur J Epidemiol. 2009;24:329–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Brindle P, May M, Gill P, Cappuccio F, D’Agostino R Sr, Fischbacher C, Ebrahim S. Primary prevention of cardiovascular disease: a web-based risk score for seven British black and minority ethnic groups. Heart. 2006;92:1595–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Selmer R, Igland J, Ariansen I, Tverdal A, Njølstad I, Furu K, Tell GS, Klemsdal TO. NORRISK 2: A Norwegian risk model for acute cerebral stroke and myocardial infarction. Eur J Prev Cardiol. 2017;24:773–782. [DOI] [PubMed] [Google Scholar]
- 88.Volpe M, Tocci G, Accettura D, Battistoni A, Bellone S, Bellotti P, Bertolotti M, Borghi C, Casasco M, Consoli A, Coppini R, Corsini A, Costanzo G, Desideri G, Ferri C, Galanti G, Giada F, Icardi G, Lombardi N, Modena MG, Modesti PA, Monti G, Mugelli A, Orsi A, Parati G, Pedretti RF, Perseghin G, Pirro M, Ricotti R, Rizzoni D, Rotella C, Rubattu S, Salvetti G, Sarto P, Tassinari F, Trimarco B, de Kreutzenberg SV, Volpe R. Consensus document and recommendations for the prevention of cardiovascular disease in Italy - 2018. G Ital Cardiol (Rome). 2018;19:1S–95S. [DOI] [PubMed] [Google Scholar]