Abstract
Jaw lesions are a wide array of benign, malignant, and locally aggressive lesions. On radiography, they can appear radiolucent, mixed, or radioopaque. The imaging appearances of radiolucent jaw lesions are markedly overlapping. The role of the radiologist is to formulate a narrow differential diagnosis based on imaging characteristics and aid appropriate management decisions. The aim of this pictorial review is to familiarize the reader with the imaging approach to radiolucent jaw lesions, which form the bulk of jaw lesions in clinical practice.
Keywords: computed tomography, magnetic resonance imaging, orthopantomogram, radiolucent jaw lesions
Introduction
Jaw lesions comprise a broad spectrum of odontogenic and nonodontogenic lesions. They may be cysts, tumors, or tumor-like lesions. Clinical presentation of this vast spectrum of pathology is nonspecific. On imaging, they may be classified as radiolucent, mixed, or radioopaque. Based on this broad categorization of imaging appearances and few specific imaging characteristics if present, it may be possible to diagnose a particular jaw lesion or at least reach a narrow differential diagnosis. With the increasing use of advanced imaging techniques in the evaluation of jaw lesions, the role of radiologist has increased tremendously not only in diagnosis but also in guiding the management of jaw lesions.
This article aims to discuss the imaging findings of radiolucent jaw lesions to aid the radiologist to formulate a differential diagnosis for this vast spectrum of jaw lesions with overlapping clinical and imaging appearances.
Imaging Modalities
Radiographs
Conventional radiographs form the backbone of jaw imaging. Intraoral radiographs and orthopantomogram (OPG) are usually the first investigation when a jaw lesion is suspected clinically. While intraoral radiographs give detailed information from a small region, OPG gives us a broad view of the entire jaw. Intraoral radiographs cannot depict the entire extent of lesions larger than 3 cm. In case of larger lesions, OPG helps visualize the relationship of these lesions to adjacent structures and teeth. However, the spatial resolution of OPG is inferior to that of intraoral radiography. 1
Since radiographs convert three-dimensional information into a two-dimensional image, lesion size, margins, and extent cannot be accurately assessed on radiography. Further imaging is required to assess the detailed morphological characteristics of the lesion. Few small jaw lesions like radicular cysts, however, do not need any further imaging and can be diagnosed on radiographs alone.
Computed Tomography
Thin section computed tomography (CT) can delineate the osseous, as well as the soft-tissue extent of the lesion. Reconstruction on the bone window gives excellent detail of lesion size, margins, matrix, and relationship to the inferior alveolar canal. Panoramic reconstruction on multidetector CT (MDCT) helps to obtain OPG-like image that can better evaluate the relationship of the lesion to adjacent teeth whether they are merely displaced or eroded ( Fig. 1 ). It also helps to ascertain the lesion relationship with the alveolar canal and maxillary antra. Orthoradial reconstructions of the jaw are used for preoperative implant assessment. Contrast administration and evaluation of soft-tissue window settings are useful in jaw infections and tumors. 1
Fig. 1.
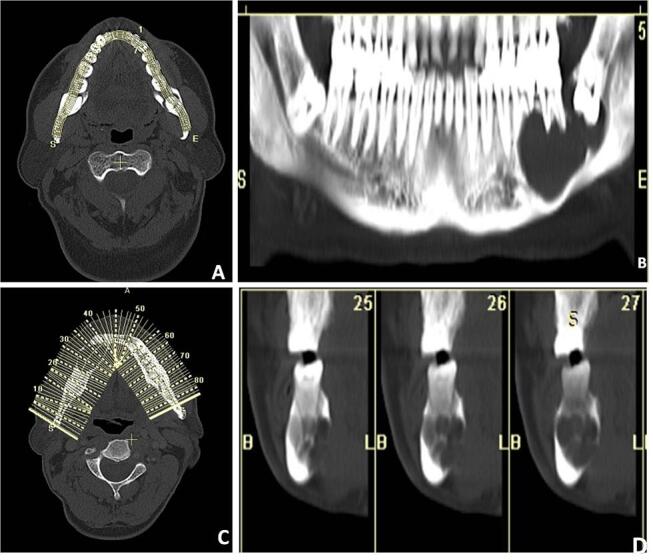
( A–D ) Panoramic reconstruction: the images are reconstructed using a dental computed tomography (CT) application where multiple dots are deposited along the curve of the jaw starting from one end of the jaw to the other end ( A ). Then the program connects these dots to form a smooth curved line that is superimposed to form a panoramic image ( B ). Orthoradial reconstruction. The same dental CT application can also be used to create para-axial views where the application creates multiple perpendicular lines along the smooth curved line ( C ) to give a series of paraxial views along each corresponding tooth ( D ).
Cone beam CT is a low dose technique that can exquisitely depict the osseous lesion with high spatial resolution. However, the time required to acquire the lesion is higher, in the range of 20 to 40 seconds. Extra osseous details are not provided by this technology.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is a complementary tool that helps better characterization of soft-tissue components of the lesion, enhancement pattern, wall thickness, and nodularity, as well as extraosseous soft-tissue involvement. As contrast enhancement is better picked up on MR, it is a more sensitive modality to differentiate cysts from tumors. MR also shows marrow involvement better than CT, while CT is more useful for cortical involvement and detection of calcification. Diffusion-weighted (DW) MR imaging is another technique that has shown promising results in differentiating cysts from tumors. It has been found to be especially useful in differentiating odontogenic keratocyst (OKC) from cystic ameloblastoma. 2
Radiolucent lesions involving the jaw can be further categorized as lesions with well-defined or ill-defined borders with subtypes ( Table 1 ).
Table 1. Radiolucent lesions of the jaw.
| Well-defined margins | ||||
|---|---|---|---|---|
| Odontogenic | Non-odontogenic | |||
| Cystic | Radicular cyst Residual cyst Dentigerous cyst Odontogenic keratocyst |
Stafne cyst/ static bone cavity Simple bone cyst Nasopalatine cyst |
||
| Solid | Ameloblastoma | Central giant cell granuloma Venous malformation Langerhan cell histiocytosis |
||
| Ill-defined margins | ||||
| Malignant odontogenic tumors ▪ Odontogenic carcinoma ▪ Odontogenic carcinosarcoma ▪ Odontogenic sarcoma |
Osteomyelitis Osteonecrosis Malignant non-odontogenic tumors ▪ Squamous cell carcinoma of the oral cavity invading the jaw ▪ Metastases ▪ Hematological malignancy ▪ Sarcoma (osteosarcoma/chondrosarcoma/fibrosarcoma) ▪ Malignant transformation of intraosseous salivary epithelial tumor |
|||
Odontogenic versus Nonodontogenic Lesions
Odontogenic lesions usually occur in relation to one tooth or a component of tooth. For example, radicular cysts develop around the tooth apex while dentigerous cysts surround the tooth crown. Nonodontogenic lesions usually have either no relation with teeth or may involve a large part of the bone in close proximity to two or more teeth. While odontogenic lesions usually are seen above the level of the alveolar canal, lesions below the level of the canal are nonodontogenic in origin ( Fig. 2 ). 3
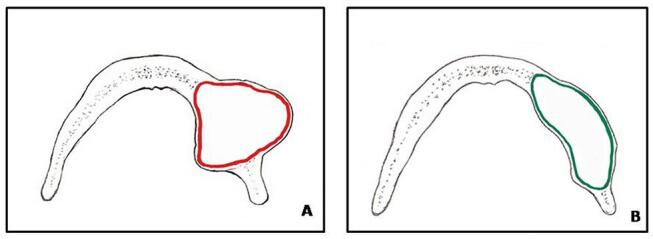
Fig. 2.
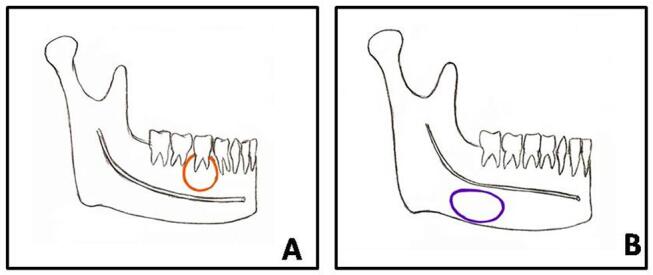
( A, B ) Schematic diagram of odontogenic vs non-odontogenic lesion. ( A ) It depicts an odontogenic lesion seen in relation to one tooth/component of tooth and located above the mandibular canal, while a nonodontogenic lesion and ( B ) is seen below the mandibular canal either in no relationship to the tooth as seen here or in relation to multiple teeth.
This review aims to describe the radiolucent lesions of the jaw as enumerated in Table 1 with an emphasis on their key diagnostic features.
Radiolucent Lesion with Well-Defined Margins
Odontogenic Cysts
Radicular Cyst
Radicular cyst is the most common odontogenic cyst, seen in relation to the root of a nonvital tooth. The peak incidence is in the third to fifth decade of life. It is usually asymptomatic and mostly less than 1 cm in size.
Tooth caries lead to infection spreading to the pulp of the tooth which results in the formation of periapical granuloma and abscess. This necrotic cavity can get epithelialized by odontogenic epithelium, the rests of Malassez, forming the radicular cyst ( Fig. 3 ). A thin sclerotic rim around the cyst helps differentiate it from apical periodontitis due to endodontal disease. There may be mild accompanying tooth resorption and displacement of adjacent roots if the cyst is large. Treatment options include endodontic treatment with extraction and cyst wall enucleation. 4
Fig. 3.
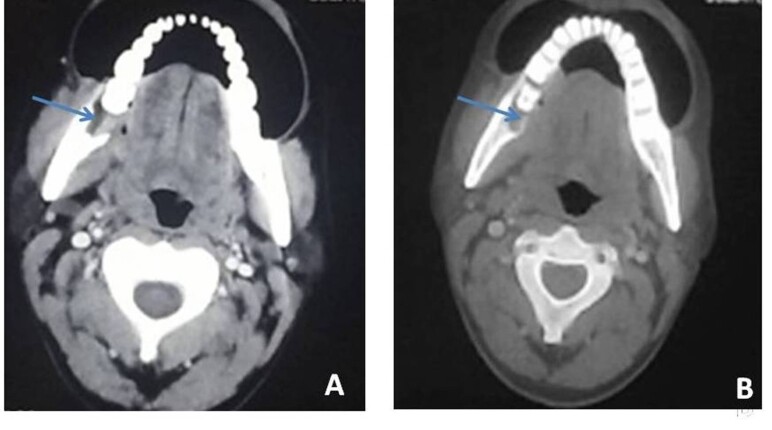
( A–C ) Radicular cyst: a 30-year-old-male with pain over the left lower jaw. Axial bone window algorithm ( A ) image shows small radiolucency around the left mandibular second molar tooth. Sagittal reformatted image ( B ) shows the periapical location of the lesion. Cyst shows a thin sclerotic rim (yellow arrow). Schematic diagram ( C ) shows the typical location of the periapical cyst (red circle) in relation to the root of the tooth. CECT, contrast-enhanced computed tomography.
Key Imaging Features
Well-defined cyst with a thin sclerotic rim around the root apex of a carious tooth, particularly upper lateral incisor.
Residual Cyst
A residual cyst is an inflammatory cyst that presents on a postextraction site. It is usually asymptomatic and is seen as a well-defined lesion, mostly measuring less than 1 cm in size.
Key Imaging Features
Well-defined cyst with a thin sclerotic rim with missing overlying tooth.
Dentigerous Cyst (Follicular Cyst)
Dentigerous cyst is the most common noninflammatory cystic lesion of the jaw. This is mostly seen in young adults and adolescents and is usually asymptomatic. It forms as a result of accumulation of fluid between the unerupted/impacted tooth and epithelium of the dental follicle that surrounds the tooth.
On imaging, it is seen as a well-defined unilocular round/ovoid cystic lesion with smooth margins with the crown of the tooth seen projecting within the cyst. The roots of the tooth are typically seen to lie outside the cyst. The most common location is around the crown of an unerupted third molar tooth ( Fig. 4 ). Cysts larger than 2 cm may cause bone expansion, although cortex is mostly preserved. There is no soft tissue or periosteal reaction. Larger cysts may have the potential to displace or resorb adjacent teeth. On MRI, dentigerous cysts are typically hypointense on T1-weighted (T1W) and hyperintense on T2W images. They usually show a thin enhancing rim. Proteinaceous contents within the cysts may increase signal intensity on T1W images ( Fig. 4C ). 5
Fig. 4.
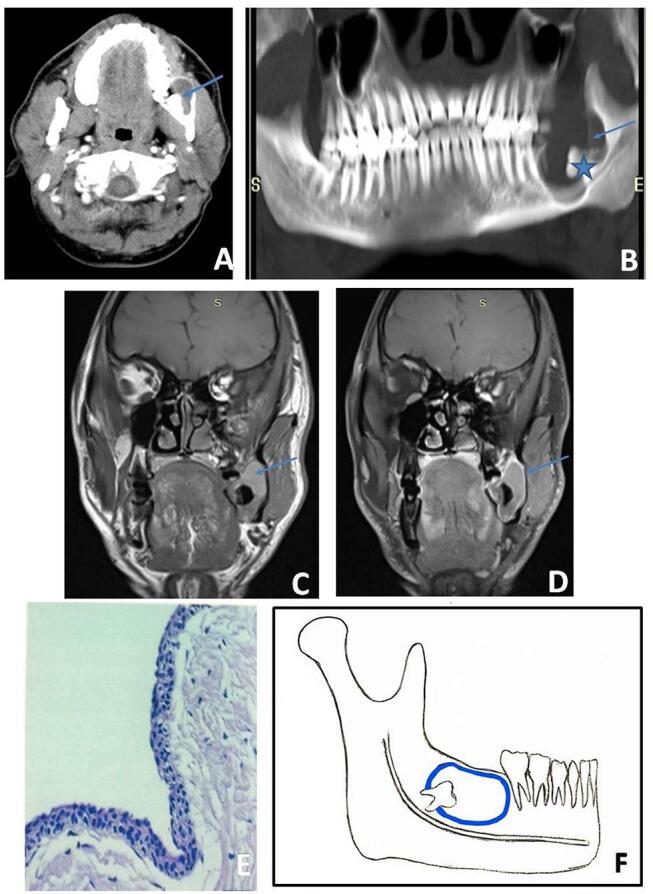
( A−E ) Dentigerous cyst: axial postcontrast ( A ) and panoramic reconstructed computed tomography (CT) images ( B ) show a well-defined, unilocular, lytic lesion (blue arrow) involving angle and ramus of left mandible with impacted third molar tooth (blue star). Coronal T1-weighted magnetic resonance (MR) image ( C ) shows a mildly hyperintense lesion with thin rim of enhancement (blue arrow) on contrast enhanced image ( D ). Microscopy ( E ) shows 2 to 4 cells layered nonkeratinizing enhanced odontogenic epithelium with a flattened interface. Schematic diagram ( F ) shows pericoronal relationship of dentigerous cyst (blue circle) with respect to impacted tooth.
These cysts are usually treated with enucleation and curettage with the extraction of the involved tooth. Complications include the development of mural ameloblastoma and rarely odontogenic carcinoma. Coexistence of unilocular cystic lesion with a crown of teeth within along with aggressive feature of bone erosion, enhancing nodules, or extension of mass into surrounding soft tissues may point toward ameloblastoma arising from a dentigerous cyst. However, histopathological examination is confirmatory. 4 6
Key Imaging Features
Well-defined unilocular round to ovoid cyst with smooth margins.
Surrounds the crown of unerupted/impacted tooth, usually the third molar.
Roots of the tooth project out of the lesion.
Odontogenic Keratocyst
The nomenclature of odontogenic keratocyst has been changed multiple times in the World Health Organization (WHO) classification of head and neck tumors. It was changed to keratocystic odontogenetic tumor (KCOT) in the third edition of WHO classification owing to presumed overlapping molecular phenotyping with jaw tumors. It has now been changed back to OKC in the latest fourth edition of WHO classification in 2017, because it is believed that there is insufficient evidence to support the neoplastic nature of this lesion. 7
OKC is lined with odontogenic para keratinizing squamous epithelium and thin fibrous wall with cheese-like contents within. This is most often seen in the second to fourth decades of life. It is more aggressive than other odontogenic cysts, as it shows basal layer budding and formation of daughter cysts that lie outside the primary cyst ( Fig. 5 ). Like dentigerous cysts, OKCs are also often associated with unerupted or impacted teeth. However, unlike dentigerous cysts, these cysts when large envelop the entire tooth and not just the crown. 8
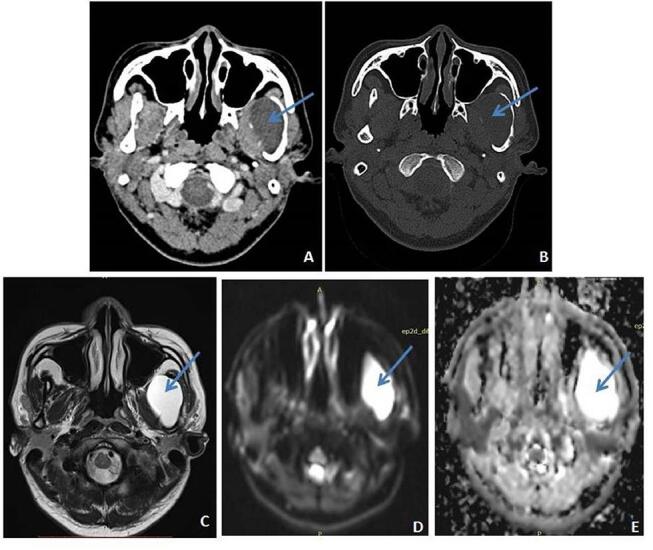
Fig. 5.
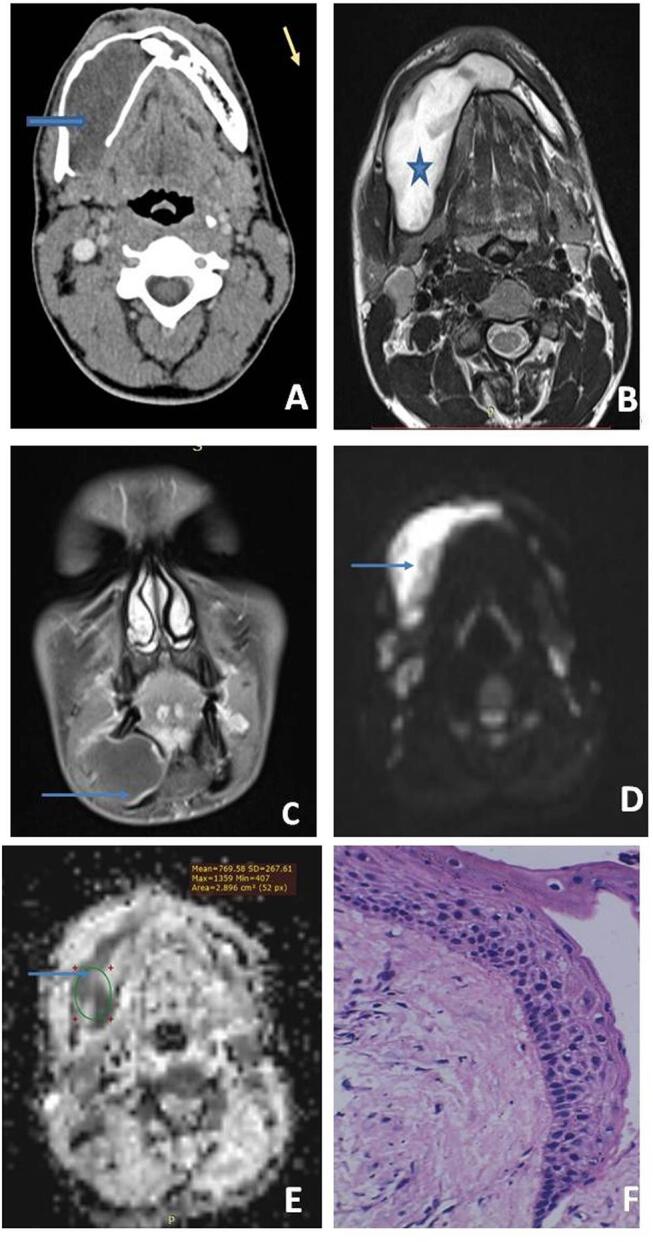
( A–F ) Odontogenic keratocyst: axial postcontrast computed tomography (CT) image ( A ) shows a well-defined, unilocular, nonenhancing, expansile lytic lesion (blue arrow) with predominant anteroposterior expansion, focal areas of cortical breach, and impacted tooth within (yellow arrow). The lesion (arrow) appears hyperintense on axial T2-weighted magnetic resonance (MR) image ( B ) with peripheral thin rim of enhancement on contrast-enhanced image ( C ) and restricted diffusion (blue arrow) on diffusion-weighted (DW) images ( D, E ). Microscopy ( F ) shows parakeratinized odontogenic epithelium of 6 to 8 cell layers with foci of palisading nuclei at the basal layer.
These are unilocular or multilocular cystic lesions, mostly seen in the posterior body and ramus of the mandible. They are usually well defined and corticated. A characteristic pattern of growth of OKCs is expansion along the axis of the mandible with relatively little expansion along the buccolingual axis ( Fig. 5A ). These cysts bear scalloped margins reflecting unequal rates of growth of different parts of the lesion. There may be accompanying cortical thinning and teeth displacement/resorption. Alveolar margin breach can lead to secondary infection of OKC with oral cavity flora. Underlying expansion of the involved jaw by the cyst can help differentiate it from primary osteomyelitis of the jaw.
On MRI, these cysts can show heterogeneous intermediate-to-high signal on T1W images and low-to-high signal on T2W images owing to keratinaceous contents within. Thin or thick rim enhancement may be seen on postcontrast images. Diffusion restriction of the proteinaceous contents of the cyst is a feature characteristically seen in OKC ( Fig. 5B-E ). 2 8 9
Multiple OKCs are seen with basal cell nevus syndrome (Gorlin–Goltz syndrome).
Since these are aggressive cysts with daughter cysts outside the primary lesion, enucleation with wide bony margin resection is the method of treatment. Enucleation and curettage may result in a higher recurrence rate. Breach of the cortex with soft-tissue extension into orbit/masticator space can be extremely difficult to remove surgically. 8
Key Imaging Features
Unilocular or multilocular well-defined cyst with scalloped margins.
Characteristic anteroposterior expansion.
If associated with unerupted tooth, it can envelop the entire tooth when large including the roots.
Intermediate-to-high signal on T1W MRI and low-to-high signal on T2W MRI with restriction of diffusion.
Thin or thick rim enhancement.
Nonodontogenic Cysts
Stafne Cyst/Static Bone Cavity
Stafne cyst is a pseudocyst of the mandible with a typical location at the angle of the jaw, posterior to the third molar tooth. This results from aberrant submandibular gland or fat resulting in bowing and remodeling of lingual cortex at this characteristic location. This may have a thin sclerotic rim all around the cyst. As it is a nonodontogenic cystic lesion, it typically lies below the level of the inferior alveolar canal. This cyst is usually an incidental finding and requires no treatment. 10
Key Imaging Features
Unilocular cyst at angle of mandible behind the third molar tooth below the inferior alveolar canal that contains aberrant submandibular salivary gland/fat.
Simple Bone Cyst
Simple bone cyst (SBC) is also known as solitary/traumatic/hemorrhagic bone cyst. This is a pseudocyst with no epithelial lining. It is an uncommon cyst that is proposed to result from intramedullary hemorrhage from trauma which results in the formation of a cavity within the jaw. This is usually picked up incidentally in an asymptomatic individual, usually before 20 years of age and shows a female predominance.
The typical location of SBC is the posterior mandible, where it is seen as a unilocular cyst that may have expansile, scalloped margins. It is seen to characteristically extend between the roots of adjacent teeth resulting in superior scalloped margins with preservation of lamina dura ( Fig. 6 ). CT and MR can depict the hemorrhagic contents. No enhancement is seen on contrast administration. 3 10
Fig. 6.
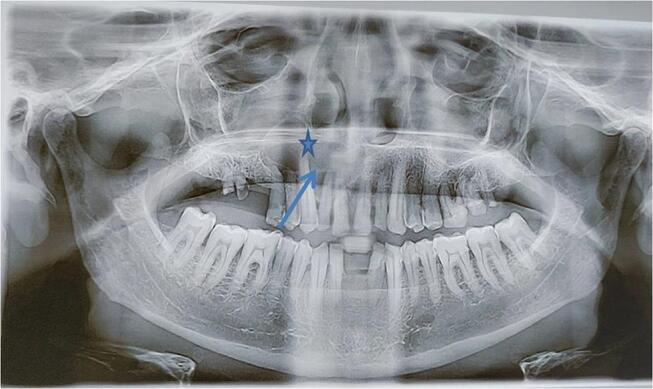
Simple bone cyst: a 19-year-old boy with upper jaw swelling. Orthopantogram shows a well-defined radiolucent lesion (blue star) seen involving right maxilla extending between the roots of the right maxillary lateral incisor and canine (blue arrow). No obvious root resorption seen.
Treatment is usually by curettage. When it cannot be distinguished from other cysts like OKC, surgical exploration may be necessary.
Key Imaging Features
Unilocular cyst extending between the roots of adjacent teeth resulting in superior scalloped margins with preservation of lamina dura.
Nasopalatine Duct Cyst
Nasopalatine duct cyst originates from the remnant epithelium of the nasopalatine duct, a primitive organ of smell, which usually regresses in fetal life. Other names for this cyst include midline maxillary cyst, anterior midline palatine cyst, or incisive canal cyst. It is mostly seen in men in their fourth and fifth decades of life. Although mostly asymptomatic, patients may present with pain and discharge if the cyst gets infected.
On imaging, the cyst is round to ovoid well-defined corticated lesion above the roots of the central incisors resulting in divergence of these roots. Owing to the presence of the nasal spine in the center, it may assume a “heart shape” in some cases. Although mostly it is placed symmetrically, sometimes it may be asymmetrically positioned. Adjacent teeth are vital. Treatment is usually by enucleation if the cyst is symptomatic. 11
Key Imaging Features
Midline maxillary round to ovoid cyst above the roots of the maxillary incisors diverging the roots with vital teeth with preserved lamina dura and periodontal ligament space.
Solid Tumors
Odontogenic
Ameloblastoma
Ameloblastoma is a benign but locally aggressive odontogenic tumor that arises from the enamel forming cells of odontogenic epithelium and less commonly from the lining of a dentigerous cyst. The peak age of incidence is fourth to sixth decades of life with no sex predilection. It may present as a painless jaw swelling or even be picked up incidentally. Ameloblastoma is the most common odontogenic tumor amounting for nearly 10% of such tumors. 6 WHO 2017 fourth edition classification of head and neck tumors classifies ameloblastoma into ameloblastoma, unicystic ameloblastoma, extraosseous/peripheral type, and metastasizing ameloblastoma. 7
The typical location of ameloblastoma is the posterior mandible (posterior body and ramus). On radiographic imaging, the lesion is radiolucent and may be unilocular or multilocular. The septations within the lesion can give rise to “honeycomb” or “soap bubble” appearance. The lesion usually shows marked buccolingual expansion with cortical thinning/breach ( Fig. 7 ). There may be accompanying teeth displacement and resorption. 1
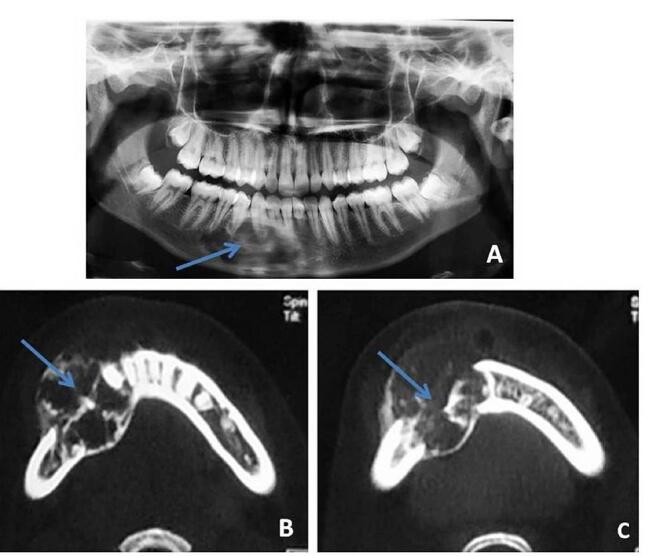
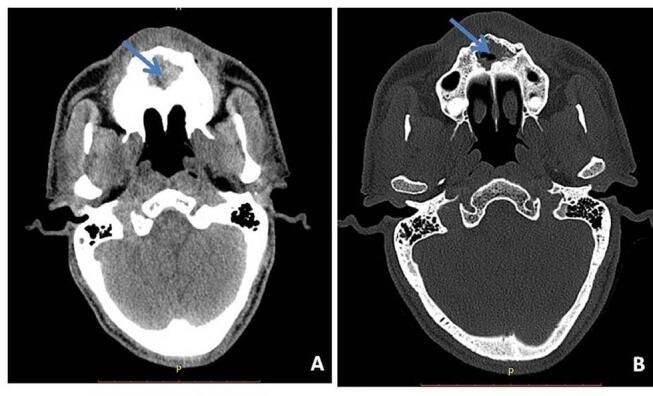
Fig. 7.
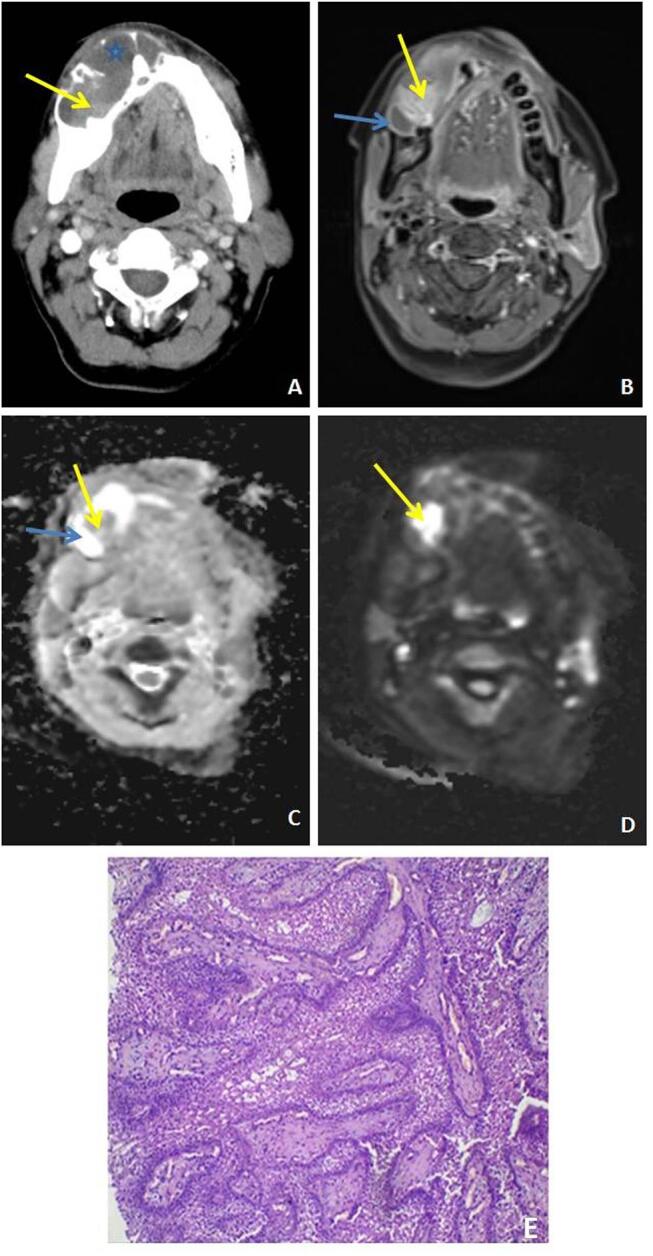
( A–E ) Ameloblastoma: axial postcontrast computed tomography (CT) ( A ) image shows a well-defined lytic lesion with predominantly buccolingual expansion. Nonenhancing cystic and enhancing solid component (yellow arrow) is seen within the lesion on CT ( A ) and postcontrast T1weighted magnetic resonance (MR) image ( B ) shows large peripherally enhancing cystic component (yellow arrow) with an enhancing solid component (blue arrow) within. The solid component of the lesion shows restricted diffusion ( C, D ). Microscopy ( E ) shows proliferating odontogenic epithelium with tall columnar peripheral cells and stellate central cells.
CT and MRI are useful in delineating internal cystic and solid components, cortical breach, soft-tissue extension, relationship to inferior alveolar canal, and enhancement of solid component/septations ( Fig. 7 ). Enhancement of the solid component and buccolingual expansion are features that help to differentiate ameloblastoma from OKC ( Fig. 8 ). MR signal characteristics and diffusion-weighted (DW) imaging are also helpful to distinguish it from OKC. The cystic component of ameloblastoma shows low T1 and bright T2 signal, unlike OKC which shows intermediate to bright T1 signal and low to high T2 signal. On DW images, the solid component of ameloblastoma shows restricted diffusion, while the cystic component has facilitated diffusion. The cystic component of OKC, on the other hand, has reduced diffusion owing to its viscous contents. An apparent diffusion coefficient (ADC) value of 2 × 10 −3 mm/s has been proven to be a useful cut-off to differentiate between the two. 9 12
Fig. 8.
( A, B ) Expansion pattern of ameloblastoma and odontogenic keratocyst (OKC). Schematic diagrams ( A, B ) show typical difference between the expansion pattern of ameloblastoma ( A ) and OKC ( B ) respectively. Ameloblastoma shows buccolingual expansion (red color), while OKC (green color) shows characteristic anteroposterior expansion with scalloping of the overlying margins.
The unicystic variant of ameloblastoma has a relatively benign biological behavior and affects the younger age group, mostly in the second decade of life. On imaging, it is seen as a cystic lesion with or without luminal or mural solid enhancing component ( Fig. 9 ). Extraosseous/peripheral ameloblastoma is a rare tumor and can be seen involving buccal mucosa, lips, palate, floor of mouth, or tongue base. It is a diagnosis that is only made on histology and not clinically or on imaging. Metastasizing/malignant ameloblastoma, on the other hand, refers to the tumor which shows distant metastases but is histologically benign. Both the primary lesion and metastases show histological features of benign ameloblastoma. 13 Histopathology is essential to distinguish it from an ameloblastomic carcinoma with well-defined margins.
Fig. 9.
( A–E ) Unicystic ameloblastoma: a 35-year-old female patient with swelling over left jaw. Axial postcontrast soft tissue ( A ) and bone window ( B ) images show expansile, nonenhancing hypodense lesion (blue arrow) involving body and ramus of left-side mandible with areas of cortical breach and marked cortical thinning (yellow arrow). Axial T2-weighted image ( C ) shows lesion (arrow) with high signal intensity. Axial diffusion-weighted image ( D ) shows hyperintense signal (white arrow) with no signal drop on corresponding ADC maps ( E ) suggestive of facilitated diffusion.
The treatment of ameloblastoma is surgical resection. Careful follow-up is recommended, as recurrence rates are high.
Key Imaging Features
Unilocular/multilocular radiolucent lesion with marked buccolingual expansion.
Cortical breach, root resorption, and soft-tissue extension due to aggressiveness of the lesion.
Enhancement of solid component on CT and MR.
Cystic component with low T1W and high T2W signal.
Diffusion restriction of solid component.
Nonodontogenic
Central Giant Cell Granuloma
Central giant cell granuloma is believed to result from a reactive process secondary to hemorrhage within the mandible. Histologically, there are areas of hemorrhage, fibrous tissue, and osteoclast-like giant cells in the lesion. Some authors believe it to be a benign tumor. It is most often seen in young women in their second and third decades of life. Characteristic location is anterior mandible or maxilla with a tendency to cross the midline. 4
Giant cell reparative cyst or giant cell granuloma are the other names used to describe this lesion. Patients may present with swelling and pain. On imaging, the lesion is most often a well-defined, multilocular radiolucent lesion. Less often, it may be seen as a unilocular lesion. The lesion can show expansion and cortical thinning and remodeling. Internal septations can give rise to “honeycomb” appearance. There may be displacement or even resorption of the teeth when the lesion is larger. Scalloped borders may result from uneven growth ( Fig. 10 ). 4
Fig. 10.
(A–C) Central giant cell granuloma: a 17-year-old lady with lower jaw swelling. Orthopantomogram (OPG) ( A ) shows multilocular, expansile radiolucent lesion (blue arrow) seen involving right side of mandible reaching the midline. Axial computed tomography (CT) images ( B, C ) at bone window settings show expansile, lytic lesion (blue arrow) seen involving right side of mandible with multiple trabeculae within the lesion.
Cross-sectional imaging can help assess bony involvement and cortical thinning better. On MR, the lesion shows intermediate signal on T1W and T2W images with moderate to marked contrast enhancement. T2 shortening reflects the presence of hemorrhage and giant cells within the lesion.
Although radiographic appearances can be overlapping with odontogenic cysts and ameloblastoma, characteristics demographic features and location can be a clue to the diagnosis. These are also very similar to brown tumors on imaging, as well as histopathology, when patient’s age and laboratory findings can point toward the correct diagnosis. 1 4
Typical slow-growing lesions can be treated with conservative methods like intralesional steroid injection, calcitonin injections, and radiotherapy. However, definitive treatment requires enucleation and curettage; surgical resection may be done in aggressive cases. 14
Key Imaging Features
Young patients in the second to third decade; female predominance.
Multilocular expansile lesion in the anterior jaw, with a tendency to cross midline.
Intraosseous Venous Malformation
Intraosseous venous malformation is a rare lesion of the jaw with a varied appearance It is often incorrectly labelled as ‘hemangioma’ in the literature.
Intraosseous venous malformation is most often seen in women in the second to fifth decades of life. Mostly asymptomatic, it may present as painless jaw swelling. Mobile teeth, pain, and paraesthesia may also be encountered occasionally.
It is the body of the mandible which is most commonly affected. Radiological findings are varied. It could present as a unilocular cyst, cyst with ill-defined borders or sclerotic rim, multilocular expansile lesion with honeycomb appearance resulting from fine trabeculae within the lesion, “sunburst” appearance with radiating bone spicules, and soap bubble/tennis racquet appearance in an expansile lesion with septations ( Fig. 11 ). Due to varied and inconsistent appearances, definite diagnosis on imaging can be difficult.
Fig. 11.
( A–D ) Intraosseous venous malformation: a 75-year-old male patient with pain over right lower face region. Panoramic radiograph ( A ) reveals well-defined lytic lesion (star) involving right mandibular body. Sagittal reformatted CT image ( B ) shows involvement of right mandibular canal by the lesion (blue arrow).Magnetic resonance (MR) images show the hyperintense lesion (blue arrow) on short tau inversion recovery (STIR) ( C ) with postcontrast enhancement (D).
The involved bone and developing teeth may enlarge which may erupt earlier. The mandibular canal and mental foramen can get enlarged. Adjacent teeth may be displaced, as well as resorbed. MR imaging can show variable signal intensity reflecting blood of various ages with marked enhancement.
There are multiple imaging mimics of this lesion. Sunburst appearance may mimic an osteosarcoma. Osteosarcoma is seen as a lucent, mixed, or sclerotic lesion with ill-defined margins. 15 Tennis racquet appearance may also simulate odontogenic myxoma. However, it is believed that bony spicules extending into the lesion forming right angles to the bone with surrounding intact bone are characteristic of venous malformation. Loculations of giant cell granuloma are generally thicker and larger compared with the fine fibrillar pattern of venous malformation. 4 A high index of suspicion for this diagnosis is important on imaging as the lesion can have catastrophic bleeding. Needle aspiration should precede biopsy when this suspicion is raised.
Treatment includes steroid therapy, sclerosing agents, radiotherapy, and surgical excision depending on the size and location of the lesion. Surgical intervention is generally accepted as the definitive treatment where the surgeon needs to be prepared to handle brisk intraoperative bleeding. 16
Langerhan Cell Histiocytosis
Langerhan cell histiocytosis (LCH) is a disease characterized by abnormal proliferation of Langerhan cells of the reticuloendothelial system. The three forms of LCH are unifocal or localized form seen in 70% cases, multifocal unisystem or chronic recurring form in 20%, and multifocal multisystem or fulminant form seen in 10%. Localized form presents between 5 and 15 years of age with involvement of a single or few bones, and may also involve the lung. Chronic recurring form involves multiple bones and also the reticuloendothelial system (i.e., liver, spleen, and lymph nodes). These cases present earlier at approximately 1 to 5 years of age. The most severe fulminant form presents in the first 2 years of life, and there is widespread involvement of the reticuloendothelial system. This form is often fatal. 17
The mandible is the second most common bone to be involved after skull. Symptoms range from pain, swelling, loosening of teeth, and limitation of mouth opening. On imaging, the lesion is lytic in nature with ill-defined borders in the early stage to well defined and sclerotic margins in the late phase of the disease. There may be accompanying cortical breach and periosteal reaction. The involvement of the alveolar crest can give rise to “scooped out” appearance. “Floating teeth” appearance results from destruction of the alveolar bone selectively. On MRI, the lesion appears hypointense on T1W and hyperintense on T2W images with marked contrast enhancement. Softtissue extension can be better visualized on MRI. When aggressive features like ill-defined margins, cortical breach, and soft-tissue extension are seen, it may be difficult to differentiate from osteomyelitis and malignant lesions. 18 DW imaging can aid in differentiation from malignant pathology. Apparent diffusion coefficient values have been proposed to be slightly higher in LCH than in malignant tumors (1.2 × 10 −3 mm 2 /s vessels vs. 1.0×10 −3 mm/s). 1
Treatment options include surgery, radiotherapy, chemotherapy, and intralesional injection of corticosteroids depending on the number, size, and location of lesions.
Key Imaging Features
Presentation in childhood/adolescence.
Lytic lesion, usually with well-defined borders.
”Scooped out” or “floating teeth appearance.”
Cortical breach, soft-tissue extension, and marked enhancement can be seen on cross-sectional imaging.
Radiolucent Lesions with Ill-Defined Margins
Odontogenic
Malignant Odontogenic Tumors
These are rare tumors that include odontogenic carcinoma, odontogenic carcinosarcoma, and odontogenic sarcomas as per 2017 WHO classification of odontogenic lesions. Odontogenic carcinomas include ameloblastic carcinoma, primary intraosseous carcinoma not otherwise specified (NOS), sclerosing odontogenic carcinoma, clear cell odontogenic carcinoma, and ghost cell odontogenic carcinoma. These are more common in men in their sixth to eighth decades. 13
Irregular ill-defined radiolucent lesion is the typical presentation. Aggressive features that point toward malignancy include ill-defined margins, cortical destruction, soft-tissue extension, and solid enhancing components that show restricted diffusion on MRI. Atypical features like well-defined smooth margins or a sclerotic rim may be seen. 5
Nonodontogenic
Osteomyelitis
Osteomyelitis is more often seen to affect the mandible than the maxilla. Causes include pulpal or periodontal infection, trauma, foreign body, or a prior surgical procedure. Osteomyelitis may be acute or chronic. While acute osteomyelitis presents with severe pain, fever, swelling, trismus, paraesthesias, or even pathological fracture, chronic cases are usually more indolent in presentation.
On radiography, there are changes of indistinct cortex which become obvious only 1 to 2 weeks after onset of infection. Subsequently, ill-defined lytic lesions in bone, permeative bone destruction, and periosteal reaction are seen. Chronic osteomyelitis may be associated with sequestrate, seen as dense necrotic bone. CT and MR can show the extent of involvement in adjacent soft tissues which show loss of intervening fat planes in contrast to neoplasia where fat planes are displaced ( Fig. 12 ). MR is more sensitive than CT in delineating marrow and soft-tissue changes. On contrast administration, there is variable enhancement of involved bone and adjacent soft tissues. Rim-enhancing abscesses can be seen. Treatment consists of antibiotics and surgical debridement. 4 10
Fig. 12.
( A, B ) Osteomyelitis: a 65-year-old male patient with pain and swelling over midfacial region following tooth extraction. Axial computed tomography (CT) image on soft tissue ( A ) and bone window settings ( B ) reveal ill-defined soft tissue attenuation lesion (blue arrow) involving maxillary alveolus in the midline with destruction of maxillary alveolus and increased adjacent soft tissue with blurred fat planes.
Key Imaging Features
Clinical setting of odontogenic infection/trauma/surgery.
Ill-defined lytic lesion with periosteal reaction and focus of carious tooth.
Loss of surrounding soft-tissue fat planes with rim enhancing abscesses.
Osteonecrosis
Osteonecrosis of the mandible may occur as a result of radiation (osteoradionecrosis) or medication that may have antiangiogenic/bone remodeling suppression effects (medication-related osteonecrosis of jaw [MRONJ]). The latter include bisphosphonates used in the treatment of osteoporosis and malignancy and immunosuppressant-like tyrosine kinase inhibitors or vascular endothelial growth factor (VEGF) inhibitors. MRONJ has been previously called bisphosphonate-related osteonecrosis of the jaw (BRONJ) but MRONJ is now the preferred term as bisphosphonates are not the only implicated agent.
The diagnosis of MRONJ is based on three criteria as follows:
Area of exposed bone not healing for more than 8 weeks.
Past or current treatment with medications that can cause MRONJ.
No radiation therapy to head and neck regain.
MRONJ has been reported to occur between 6 and 60 months of treatment. 19
Osteoradionecrosis can occur as a complication of radiation therapy for head and neck cancer, seen in 2 to 22% of these patients. Most cases of osteoradionecrosis are reported to occur within 4 months to 2 years, although delayed presentation after many years has also been reported. Risk factors include tumor burden and stage, high dose of radiation therapy, concurrent chemoradiation, injury or dental extraction, infection, immunosuppression, bad nutritional status, and poor oral hygiene. 20
Early stages may be asymptomatic and picked up only on imaging. Patients usually present late with exposed necrotic bone and ulcerated mucosa. Other features include pain, pus discharge, trismus, halitosis, paraesthesias, and fever.
Imaging findings include ill-defined lytic areas, permeative bone destruction, and sclerotic foci in the early stage of the disease, while sequestration, fragmentation, areas of gas attenuation, cortical destruction, periosteal reaction, and pathological fractures may be seen in the advanced stage of the disease ( Fig. 13 ). The involvement of the inferior alveolar canal may also be demonstrated on cross-sectional imaging. Bilateral involvement can also occur in osteoradionecrosis. On MR, variable signal intensity can be seen on both T1W and T2W images with variable contrast enhancement depending on the stage of the disease. Marrow edema, marrow sclerosis, and sequestrum, all have different signal intensities. 5 20
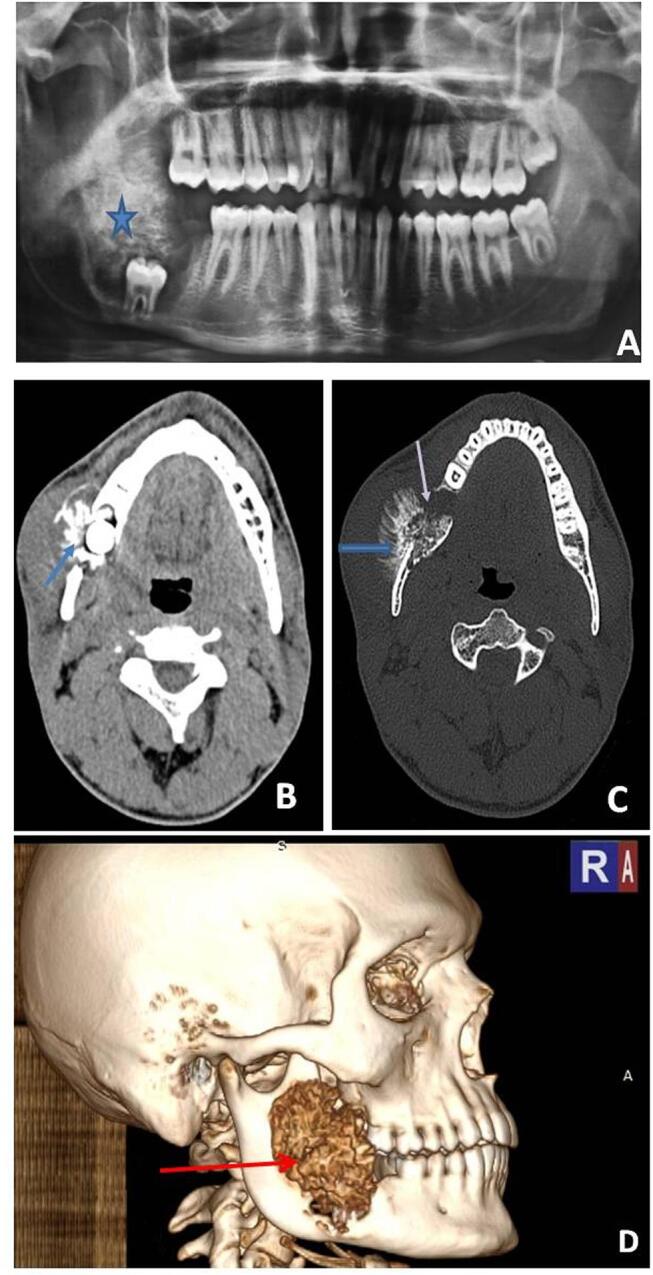
Fig. 13.
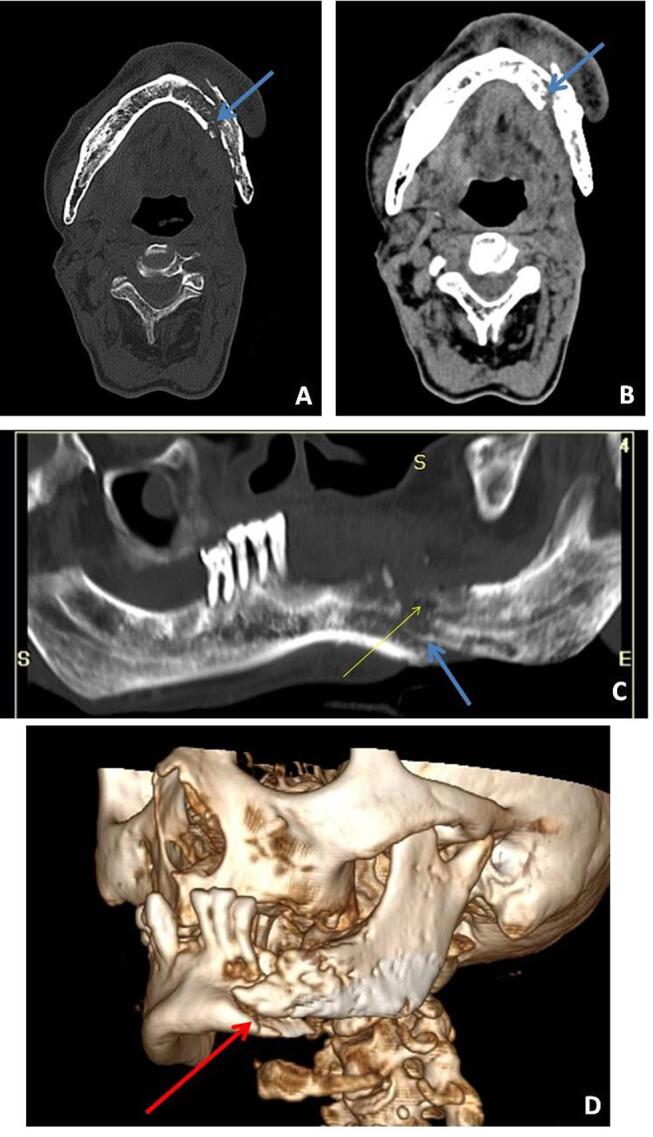
( A–D ) Osteonecrosis: a 70-year-old male patient with pain over left lower jaw and history of prior radiotherapy for oral cancer. Axial images ( A, B ) in bone window and soft tissue settings show ill-defined lytic destruction (blue arrow) of the body of mandible on left side with pathological fracture of the same. Panoramic reformatted image ( C ) shows ill-defined lytic areas with pathological fracture (blue arrow) and few air foci within (yellow arrow). Volume rendered image ( D ) shows pathological fracture (red arrow) with cortical irregularity along the body of left side mandible.
The diagnosis is primarily clinical but differential diagnosis includes osteomyelitis and malignant involvement by primary or secondary neoplasm. Osteoradionecrosis is also frequently complicated by superimposed infection. Appropriate clinical setting and clinical examination findings are the mainstay of differentiation. The presence of abscess is indicative of superimposed infection. DW imaging can also aid in the differentiation of osteonecrosis from neoplastic pathology. 1 20
Treatment is mainly conservative with oral care, treatment of superadded infection, and pain control. Surgery may be done in nonresponsive cases and is usually not the primary treatment method, as it may aggravate necrosis. 21
Malignant Nonodontogenic Tumors
Nonodontogenic tumors: these are mostly extensions from squamous cell carcinoma of the oral cavity. Other nonodontogenic malignant lesions to affect the jaw include the following:
Metastases.
Hematological malignancies.
Sarcomas from osseous, cartilaginous, or neuroectodermal elements.
Malignant transformation of intraosseous salivary epithelial remnants.
Squamous Cell Carcinoma of the Oral Cavity Invading the Jaw
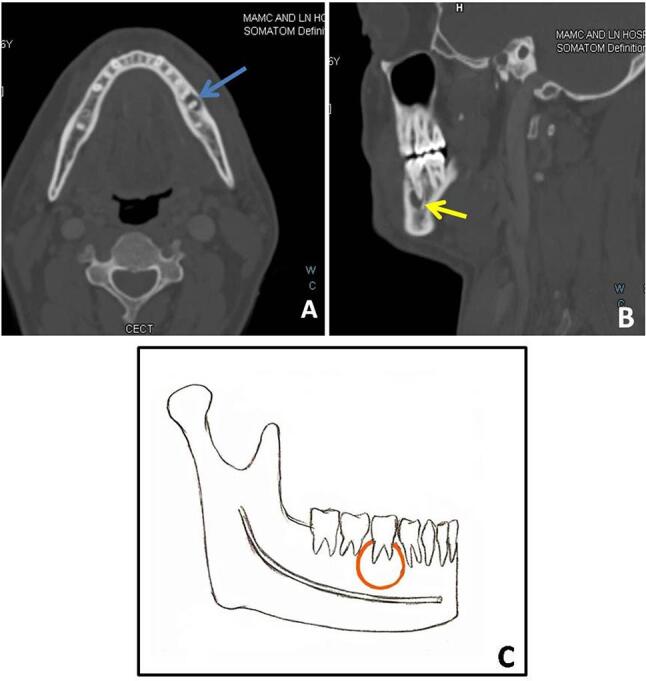
Squamous cell carcinoma (SCC) of the oral cavity mostly affects men above the age of 50 years. In advanced stages, mandibular involvement can occur. Radiologically, it is seen as an ill-defined lytic lesion involving the bone adjacent to the mass ( Fig. 14 ). The inferior alveolar canal can also get involved leading to paresthesia along mandibular nerve distribution. Imaging plays an important role in the evaluation of the extent of malignancy and nodal, as well as distant metastases.
Fig. 14.
( A, B ) Squamous cell carcinoma of retromolar trigone invading jaw: axial soft tissue ( A ) and bone algorithm ( B ) images show ill-defined soft tissue lesion (blue arrow) in right retromolar trigone causing destruction of adjacent ramus of right side mandible (blue arrow).
Metastases
These are seen to involve the mandible more often than maxilla in the ratio 4:1. Maxillary metastases are less common owing to the paucity of red bone marrow. 10
The posterior body and angle of the mandible are the most common sites likely due to the predominant red marrow in these regions. The most common primary malignances to involve the jaw are lung, prostate, kidney, breast, gastrointestinal, and thyroid cancers ( Fig. 15 ).
Fig. 15.
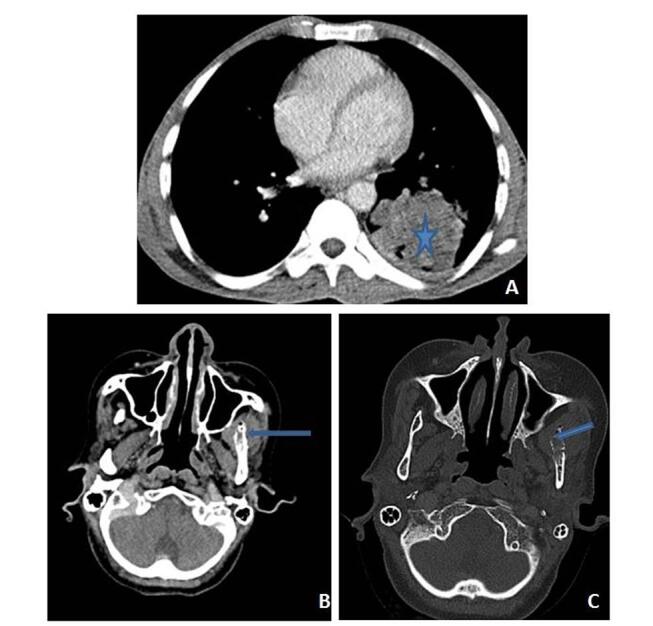
( A–C ) Metastases: a 55-year-old female patient with left lung mass. Contrast-enhanced axial ( A ) computed tomography (CT) image reveals irregularly marginated, heterogeneously enhancing mass lesion (star) in left lower lobe. Axial CT image in soft tissue window ( B ) and bone window algorithm ( C ) settings show ill-defined lytic lesion (blue arrow) with cortical destruction and associated soft tissue component involving ramus of left side of mandible.
These lesions may present with pain, swelling, and paraesthesias but may also be asymptomatic. At times, they may be the first presentation from an occult primary tumor.
On imaging, ill-defined lytic lesions are usually seen with no accompanying periosteal reaction. Sclerotic metastases may be seen with prostate carcinoma. Expansile metastases can be encountered in renal and thyroid malignancy. Metastases from kidney malignancy may also be hypervascular. Treatment is usually palliative as metastases are usually widespread when jaw metastases have occurred. 5 22
Key Imaging Features
Ill-defined lytic lesions with no periosteal reaction.
Should be considered in the differential of a nonodontogenic jaw lesion in a case of known primary malignancy.
Hematological Malignancies
Leukemia and lymphoma can also rarely involve the jaws. Primary jaw lymphoma is usually Non-Hodgkin lymphoma. On imaging, these can be seen as ill-defined permeative lesions. Sometimes, the findings may also be limited to minor lysis, loss of lamina dura, or enlarged mandibular canal. On MR, marrow infiltration and involvement of soft tissues may be far more striking than cortical involvement. It is seen as a low-to-intermediate signal mass on T1W and T2W images with homogeneous contrast enhancement. Multiple accompanying enlarged nodes support the diagnosis of lymphoma. 1
Multiple myeloma can present as a single lesion, multiple punched out lesions with no rim, ill-defined permeative pattern of bone destruction, or large area of bone destruction ( Fig. 16 ). On MRI, a low–to-intermediate signal is seen on T1W images and a high signal is seen on T2W images. 22
Fig. 16.
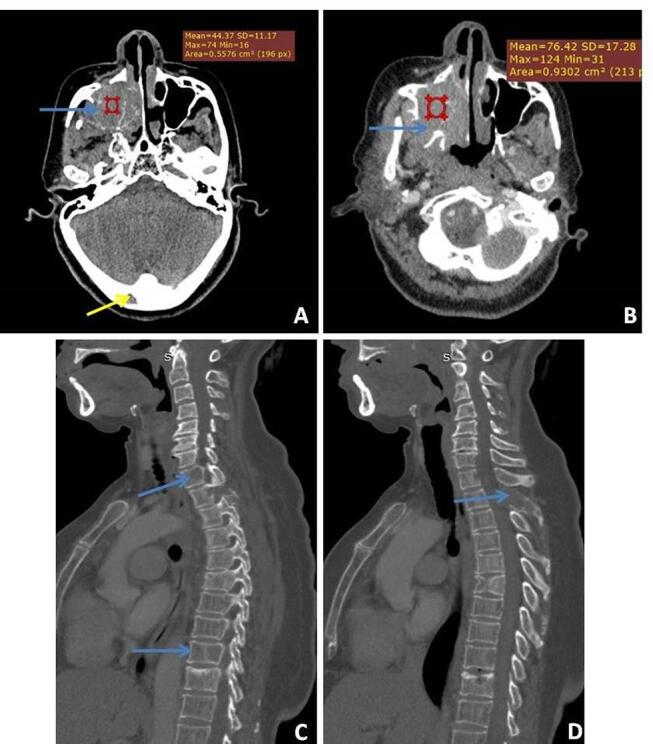
( A–D ) Multiple myeloma: a 55-year-old male with right-sided facial swelling. Axial precontrast and corresponding post contrast ( A, B ) computed tomography (CT) images show an enhancing aggressive mass involving the right maxilla with significant osseous destruction with another small lytic lesion (yellow arrow) also seen in right occipital bone. Biopsy of the larger mass revealed multiple myeloma. Evaluation of the spine ( C, D ) shows diffuse osteopenia with multiple lytic lesions involving D1, D9 vertebral bodies and posterior element of D2 vertebral body (blue arrow).
Sarcomas
Sarcomas of the jaw include osteosarcoma, chondrosarcoma, fibrosarcoma, and Ewing sarcoma. Among these, osteosarcoma is the commonest. Primary osteosarcoma of the jaw occurs slightly later than other long bones, peak incidence being in the third and fourth decades of life. Osteosarcoma may also occur secondary to radiation therapy of the head and neck region. It is most often seen to involve the posterior mandible.
On imaging, it may appear as a lytic, sclerotic, or mixed lesion. The lytic lesion is generally ill-defined with no new bone formation. The sclerotic and mixed forms may have the characteristic “sunburst” periosteal reaction with cortical destruction ( Fig. 17 ). On MRI, it appears heterogeneous in signal intensity depending on the extent of the mineralized matrix. 5
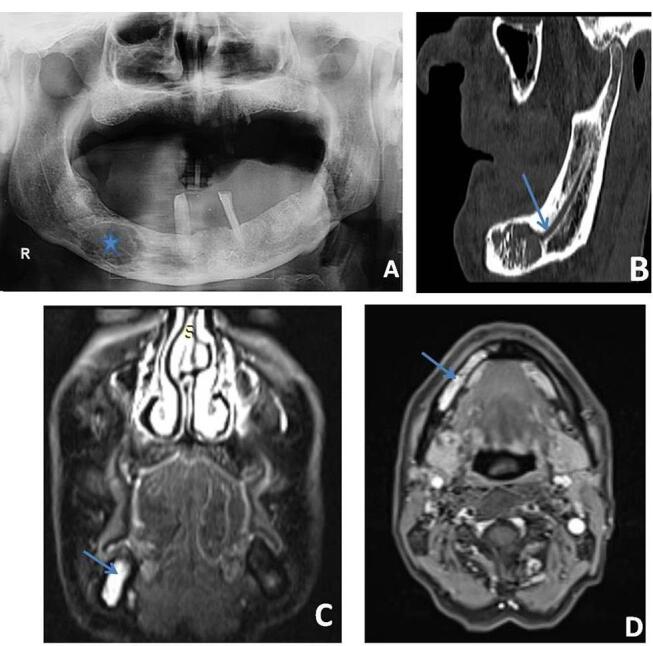
Fig. 17.
( A–D ) Osteosarcoma: panoramic radiograph ( A ) reveals ill-defined lytic sclerotic lesion (star) involving body and ramus of right side mandible with impacted tooth within. Axial computed tomography (CT) image ( B ) reveals ill-defined mixed density lesion (blue arrow) involving, angle, and ramus of right side mandible with extension into masticator space, cortical destruction (white arrow), and sunburst type of periosteal reaction (blue arrow) ( C ) volume rendered image ( D ) shows a lytic lesion (red arrow) involving the ramus and angle of mandible with cortical destruction and periosteal reaction.
Malignant Transformation of Intraosseous Salivary Epithelial Rests
Intraosseous mucoepidermoid carcinoma may arise from salivary epithelial rests within the jaw.
Mucoepidermoid carcinoma of the mandible is an extremely rare tumor. Women are nearly twice as commonly affected as men with a mean age of presentation in the fifth decade of life. On radiograph, it may be seen as a well-defined multilocular cystic mass or ill-defined lytic area, typically involving the angle or posterior body of mandible. Medullary bone destruction with intact cortex is characteristic of intraosseous mucoepidermoid carcinoma. Cortical breach and soft-tissue extension may, however, be present. CT and MR are superior in depicting cortical breakthrough and associated lymphadenopathy. On MR, the cystic component is bright on T2W images, while the solid component is of lower signal intensity on T2W images with restricted diffusion. 23
Conclusion
Lesions of the jaws are categorized into radiolucent, sclerotic, and mixed based on radiographic appearances. Various radiolucent jaw lesions have overlapping imaging appearances. Discerning odontogenic or nonodontogenic origin of these lesions is the first step to aid in narrowing the differential diagnosis. However, this distinction may not be possible in large lesions. An algorithmic approach to common radiolucent lesions of the jaw is suggested ( Fig. 18 ).
Fig. 18.
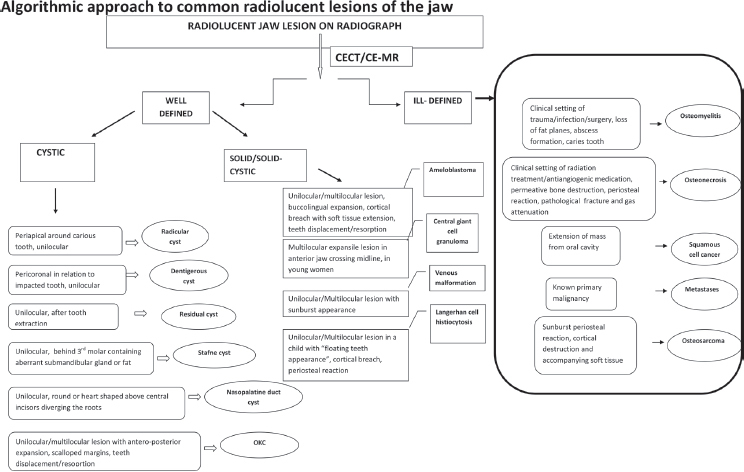
Algorithmic approach to common radiolucent lesions of the jaw. CECT, contrast-enhanced computed tomography; CE-MR, contrast-enhanced magnetic resonance; OKC, odontogenic keratocyst.
Funding Statement
Funding None.
Footnotes
Conflicts of interest None declared.
References
- 1.Avril L, Lombardi T, Ailianou A et al. Radiolucent lesions of the mandible: a pattern-based approach to diagnosis. Insights Imaging. 2014;5(01):85–101. doi: 10.1007/s13244-013-0298-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sumi M, Ichikawa Y, Katayama I, Tashiro S, Nakamura T. Diffusion-weighted MR imaging of ameloblastomas and keratocystic odontogenic tumors: differentiation by apparent diffusion coefficients of cystic lesions. AJNR Am J Neuroradiol. 2008;29(10):1897–1901. doi: 10.3174/ajnr.A1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neyaz Z, Gadodia A, Gamanagatti S, Mukhopadhyay S. Radiographical approach to jaw lesions. Singapore Med J. 2008;49(02):165–176, quiz 177. [PubMed] [Google Scholar]
- 4.Harmon M, Arrigan M, Toner M, O’Keeffe S A. A radiological approach to benign and malignant lesions of the mandible. Clin Radiol. 2015;70(04):335–350. doi: 10.1016/j.crad.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 5.Mosier K M. Magnetic resonance imaging of the maxilla and mandible: signal characteristics and features in the differential diagnosis of common lesions. Top Magn Reson Imaging. 2015;24(01):23–37. doi: 10.1097/RMR.0000000000000045. [DOI] [PubMed] [Google Scholar]
- 6.Cankurtaran C Z, Branstetter B F, IV, Chiosea S I, Barnes E L., Jr Best cases from the AFIP: ameloblastoma and dentigerous cyst associated with impacted mandibular third molar tooth. Radiographics. 2010;30(05):1415–1420. doi: 10.1148/rg.305095200. [DOI] [PubMed] [Google Scholar]
- 7.Wright J M, Vered M. Update from the 4th edition of the World Health Organization classification of head and neck tumours: Odontogenic and maxillofacial bone tumors. Head Neck Pathol. 2017;11(01):68–77. doi: 10.1007/s12105-017-0794-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mosier K M. Lesions of the jaw. Semin Ultrasound CT MR. 2015;36(05):444–450. doi: 10.1053/j.sult.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Srinivasan K, Seith B halla, A, Sharma R, Kumar A, Roychoudhury A, Bhutia O.Diffusion-weighted imaging in the evaluation of odontogenic cysts and tumours Br J Radiol 201285(1018)e864–e870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Özgür A, Kara E, Arpacı R et al. Nonodontogenic mandibular lesions: differentiation based on CT attenuation. Diagn Interv Radiol. 2014;20(06):475–480. doi: 10.5152/dir.2014.14143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Srivastava S, Misra N, Agarwal R, Pandey P. Nasopalatine canal cyst: often missed. BMJ Case Rep. 2013;2013:bcr2012007548. doi: 10.1136/bcr-2012-007548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bharatha A, Pharoah M J, Lee L, Tay K Y, Keller A, Yu E. Pictorial essay: cysts and cyst-like lesions of the jaws. Can Assoc Radiol J. 2010;61(03):133–143. doi: 10.1016/j.carj.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Speight P M, Takata T. New tumour entities in the 4th edition of the World Health Organization Classification of Head and Neck tumours: odontogenic and maxillofacial bone tumours. Virchows Arch. 2018;472(03):331–339. doi: 10.1007/s00428-017-2182-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pogrel A M. The diagnosis and management of giant cell lesions of the jaws. Ann Maxillofac Surg. 2012;2(02):102–106. doi: 10.4103/2231-0746.101325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elif B, Derya Y, Gulperi K, Sevgi B. Intraosseous cavernous hemangioma in the mandible: A case report. J Clin Exp Dent. 2017;9(01):e153–e156. doi: 10.4317/jced.52864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eliot C A, Castle J T. Intraosseous hemangioma of the anterior mandible. Head Neck Pathol. 2010;4(02):123–125. doi: 10.1007/s12105-010-0170-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zaveri J, La Q, Yarmish G, Neuman J. More than just Langerhans cell histiocytosis: a radiologic review of histiocytic disorders. Radiographics. 2014;34(07):2008–2024. doi: 10.1148/rg.347130132. [DOI] [PubMed] [Google Scholar]
- 18.Kim J E, Yi W J, Heo M S, Lee S S, Choi S C, Huh K H. Langerhans cell histiocytosis of the jaw, a mimicker of osteomyelitis on CT and MR images: A retrospective analysis. Medicine (Baltimore) 2019;98(27):e16331. doi: 10.1097/MD.0000000000016331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nicolatou-Galitis O, Schiødt M, Mendes R A et al. Medication-related osteonecrosis of the jaw: definition and best practice for prevention, diagnosis, and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;127(02):117–135. doi: 10.1016/j.oooo.2018.09.008. [DOI] [PubMed] [Google Scholar]
- 20.Deshpande S S, Thakur M H, Dholam K, Mahajan A, Arya S, Juvekar S. Osteoradionecrosis of the mandible: through a radiologist’s eyes. Clin Radiol. 2015;70(02):197–205. doi: 10.1016/j.crad.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 21.Rosella D, Papi P, Giardino R, Cicalini E, Piccoli L, Pompa G. Medication-related osteonecrosis of the jaw: clinical and practical guidelines. J Int Soc Prev Community Dent. 2016;6(02):97–104. doi: 10.4103/2231-0762.178742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meyer K A, Bancroft L W, Dietrich T J, Kransdorf M J, Peterson J J. Imaging characteristics of benign, malignant, and infectious jaw lesions: a pictorial review. AJR Am J Roentgenol. 2011;197(03):W412–21. doi: 10.2214/AJR.10.7225. [DOI] [PubMed] [Google Scholar]
- 23.Abt N B, Lawler M E, Zacharias J, Lahey E T. Primary intraosseous mucoepidermoid carcinoma of the mandible: radiographic evolution and clinicopathological features. BMJ Case Rep. 2019;12(04):e224612. doi: 10.1136/bcr-2018-224612. [DOI] [PMC free article] [PubMed] [Google Scholar]