Abstract
The gut microbiota—the community of microorganisms in the gut—has been implicated in many physical and mental disorders in addition to intestinal diseases. Diets are the most studied and promising factors for altering it. Indeed, certain dietary interventions that increase fiber intake rapidly change levels of certain nutrients that can modify the composition of the microbiota, promoting richness and diversity. Recent intriguing evidence from several human clinical trials suggested that the composition and diversity of patients’ gut microbiotas at baseline can influence their responses to cancer immunotherapy. If the factors that influence the gut microbiota were fully understood, it is conceivable that manipulating them could boost therapeutic responses in cancer patients. In this review, we investigate the possibility of using fruits, vegetables, or whole grains to enhance response to cancer therapies in humans, as current evidence suggests that these dietary components can manipulate and enhance diversity of the gut microbiota. Accordingly, dietary interventions with locally available fruits, vegetables, and whole grains might be an affordable and safe approach to enhancing the diversity of the gut microbiota before immunotherapy, in turn improving patients’ responses to their treatments.
Keywords: Fruits and vegetables, whole grains, gut microbiota, cancer immunotherapy, human clinical trials
1. INTRODUCTION
Alterations in the gut microbiota—the community of microorganisms in the gut—associate with functional gastrointestinal disorders, such as inflammatory bowel disease, gastroenteric infections, irritable bowel syndrome, and colorectal cancer [1]. However, they are also linked to genitourinary malignancies, including bladder, kidney, and prostate cancers [2], and their involvement in other cancers is being investigated. For example, Breast Cancer and Its Relationship With the Microbiota (MICROMA, NCT03885648) is an ongoing clincial trial to evaluate contributions to the risk of breast cancer of bacteria, archaea, viruses, fungi, and alterations in those communities by environmental contaminants [3]. In addition, gut microbes have been linked to responses to HIV vaccination [4], Helicobacter pylori eradication success rate [5], metabolic syndrome and obesity, liver diseases, allergic diseases, and neurological diseases such as autism [1], etc.
Recent intriguing evidence from several human clinical trials has suggested that the composition and diversity of the gut microbiota at baseline influences response to cancer immunotherapy [6]. Accordingly, once the factors that influence the gut microbiota are fully understood, it is highly likely that manipulating them could boost therapeutic responses in cancer patients. Diets are the most studied and promising factors that can alter the gut microbiota. Indeed, certain dietary interventions (such as increasing fiber intake) that induce rapid changes in levels of certain nutrients can modify the microbiota’s composition, promoting richness and diversity [7]. Whereas Western diets are high in fat, refined carbohydrates, and animal protein, Eastern diets are based on carbohydrates derived from plants, vegetables, rice, and fruits [8,9]. These two diets lead to different gut microbiota: Eastern populations have a higher prevalence of Prevotella spp. rather than Bacteriodes spp. than Western populations. Furthermore, animal sources of protein and fat associate with a greater number of Bacteriodes spp., while simple carbohydrates and fiber associate mostly with more Prevotella spp. These findings may provide a fundamental explanation for why populations that consume Western diets are at higher risk for cancers such as colon cancer than those that consume Eastern diets.
For the current systematic review, we used the terms fruits, vegetables, whole grains, gut microbiota, human clinical trials, and cancer therapy to search PubMed, Web of science, Sciencedirect and Scopus, because we wanted to explore the possibility that those diets could enhance patients’ response to cancer therapy by manipulating the gut microbiota. In addition to using animal models to investigate the effects of foods on gut microbiota that has been summarized elsewhere [10-12], the approach of in vitro gastrointestinal digestion of food components was also widely used [13,14]. Focusing on humans, the current findings suggest that the gut microbiota’s composition and diversity at baseline can predict response to cancer immunotherapy and that its diversity can be enhanced by fruits and vegetables. Accordingly, these dietary interventions could be used before chemotherapy to enhance response.
2. EVIDENCE FROM CLINICAL TRIALS THAT FRUITS, VEGETABLES, OR WHOLE GRAINS ALTER THE GUT MICROGIOTA
Fruit, vegetables, whole grains, and other edible plants that are sources of carbohydrates that stimulate the growth of various indigenous gut bacteria in humans are called prebiotics [15,16]. Some artificially produced prebiotics, such as inulin, have similar effects [15,16].
The incidence of obesity, Type 2 Diabetes Mellitus (T2DM), and many cancers is rapidly increasing globally [17]. It has been suggested that obesity increases the risks of both T2DM and certain cancers, and cancer patients with obesity and/or T2DM are commonly seen in clinics [17]. Accordingly, several human clincial trials have targeted overweight/obese populations to investigate if dietary interventions modulate the gut microbiota and alter clinical parameters in such patients.
3. HEALTHY INDIVIDUALS
The ability of diets to modulate the gut microbiota in healthy individuals has been investigated (Table 1). Dietary patterns play a major role in shaping the composition of the gut microbiota and its metabolites [18]. Adherence to a Mediterranean diet—high consumption of cereals, fruits, vegetables, and legumes—was investigated for its impact on the gut microbiota and associated metabolome [18]. That trial, which included 153 individuals habitually following omnivore, vegetarian, or vegan diets showed that vegetable-based diets (the Mediterranean diet) increased levels of fecal short chain fatty acid (SCFAs), Prevotella, and some fiber-degrading Firmicutes.
Table 1 ∣.
Effects of consuming fruits and vegetables and whole grains on the gut microbiota in healthy individuals
| Human populations | Fruits/vegetables/whole grains comsumed |
Gut microbiota altered | Other effects measured | Trial registration |
References |
|---|---|---|---|---|---|
| 153 healthy individuals | Omnivore, vegetarian, or vegan diets | Vegetable-based diets ↑ SCFAs, ↑ Prevotella, ↑ Fiber-degrading Firmicutes |
– |
ClinicalTrials.gov NCT02118857 |
[18] |
| 81 healthy men and healthy post-menopausal women | Whole grains for 6 weeks | ↑ Lachnospira ↓ Enterobacteriaceae |
↑ Stool frequency ↑ Acetate ↑ Total SCFAs |
ClinicalTrials.gov NCT01902394 |
[19] |
| 28 healthy subjects | Whole grains, brown rice or whole grains + brown rice for 4 weeks | All diets ↑ Microbial diversity, ↑ Firmicutes to Bacteroidetes ratio ↑ Abundance of the genus Blautia |
Whole grains + brown rice group ↓ IL-6, ↓ Peak postprandial glucose |
– | [20] |
| 46 healthy adults, habitual avoiders of whole grains | Whole grains for 6 weeks | No difference | ↑ Bowel movements |
ClinicalTrials.gov NCT01403857 |
[21] |
Also, a randomized trial investigated the consumption of whole grains for 6 weeks by 49 healthy men and 32 healthy postmenopausal women, looking at changes in the gut microbiota and inflammatory markers [19]. It showed that the whole-grain, but not refined-grain, group had increased levels of plasma alkyre-sorcinols (showing that they had complied with the diet) and also had increased stool weight and frequency and higher levels of stool acetate and SCFAs. These changes associated with increased levels of Lachnospira, which produces SCFAs, and decreased levels of Enterobacteriaceae, which are pro-inflammatory. Like whole grains, brown rice might beneficially modulate the gut microbiota [20]. For 4 weeks, 28 healthy humans consumed whole grains, brown rice, or the two combined in a randomized crossover trial that determined impacts on the fecal microbiota and blood markers of inflammation and glucose and lipid metabolism [20]. All the dietary groups showed increases in fecal microbial diversity, the Firmicutes/Bacteroidetes ratio, and the abundance of the genus Blautia. Furthermore, the whole grain group had higher levels of the genera Roseburia, Bifidobacterium, and Dialister and the species Eubacterium rectale, Roseburia faecis, and Roseburia intestinalis. Whole grains plus brown rice decreased IL-6 levels in the blood and lowered peak postprandial glucose. This study revealed that even short-term intake of whole grains and/or brown rice induced changes in the composition of the gut microbiota that coincided with improvements in the hosts’ physiological measures. In contrast, the composition of the fecal microbiota did not change in 46 healthy adults who had habitually eschewed whole grains and then consumed them for 6 weeks, though bowel movements became more frequent [21].
In summary, the majority of human intervention studies in healthy individuals using fruits, vegetables, and/or whole grains have found improvements in the diversity of the gut microbiota, gut health, and physiological measures. These results suggest that including such foods in the daily lives of healthy individuals might help manage multiple clinical conditions besides cancer because of the gut microbiota’s role in maintaining physical and mental health.
4. OVERWEIGHT OR OBESE SUBJECTS
The effects of fruits, vegetables, and whole grains on the gut microbiotas of overweight or obese subjects are controversial, as some trials have reported increased diversity in the gut microbiota whereas others have seen no changes (Table 2). One study investigated diet-induced weight loss and weight stabilization in 38 obese and 11 overweight individuals [22]. Individuals with low-grade inflammation and abnormal metabolism had a 40% reduction in gut microbial gene richness after dietary intervention. Six weeks after those subjects increased their consumption of fruits and vegetables, gene richness improved and blood levels of triglycerides decreased, as did those of C-reactive protein, a highly sensitive indicator of inflammation. In another study, 50 overweight men and postmenopausal women were randomly assigned to a 12-week intervention with either whole grain wheat or refined wheat [23]. Whole grain wheat increased gut bacterial diversity and postprandial triglyceride levels, which may protect against hepatic fat. A larger study supported this finding, as a whole grain-based diet consumed by 123 overweight/obese subjects for 9 weeks significantly reduced fecal levels of Enterobacteriaceae and Desulfovibrionaceae, which are endotoxin-producing pathogens. In contrast, levels of Bifidobacteriaceae, which protect the gut barrier, increased [24]. Levels of lipopolysaccharide-binding protein, TNF-α, and IL-6 decreased, and levels of adiponectin increased, suggesting that whole grain intake may ameliorate inflammatory and metabolic phenotypes. In a randomized crossover study of 20 normal weight individuals consuming whole grains for 10 weeks increased diversity in the gut microbiota and lowered obesity parameters such as body mass index, body fat mass, and body weight [25].
Table 2 ∣.
Effects of consuming fruits and vegetables and whole grains on the gut microbiota in overweight and obese subjects
| Human populations | Fruits/vegetables/whole grains comsumed |
Gut microbiota altered | Other effects measured | Trial registration |
References |
|---|---|---|---|---|---|
| 38 obese and 11 overweight adults | Diet with increased fruits and vegetables for 6 weeks | Improved fecal bacterial gene richnesses | ↓ Triglycerides, ↓ Highly sensitive C-reactive protein |
ClinicalTrials.gov NCT01314690 |
[22] |
| 50 subjects (overweight men and post-menopausal women) | Whole grains for 12 weeks | ↑ Microbial diversity by whole grain diet | ↑ Post-prandial triglycerides |
ClinicalTrials.gov NCT02385149 |
[23] |
| 123 overweight or obese subjects | Whole grains for 9 weeks | ↓ Enterobacteriaceae and Desulfovibrionaceae, ↑ Bifidobacteriaceae |
↓ Lipopolysaccharide-binding protein, ↓ TNF-α, IL-6, ↑ Adiponectin |
– | [24] |
| 20 normal weight subjects | Whole grains for 10 weeks | ↑ Microbial diversity by whole grain diet | ↓ Obesity parameters (Body mass index, body fat mass, and body weight) |
ClinicalTrials.gov NCT01449383 |
[25] |
| 60 adults at risk of developing metabolic syndrome | Whole grains for 8 weeks | No change in fecal microbiota | ↓ Bodyweight, ↓ IL-6, ↓ C-reactive protein |
ClinicalTrials.gov NCT01731366 |
[26] |
| 70 overweight adults, habitual avoiders of whole grains | Whole grains for 6 weeks | No difference | ↑ Flatulence, ↑ Bowl movements, ↓ Bloating |
ClinicalTrials.gov NCT02358122 |
[27] |
| 49 overweight or obese subjects with low intake of fruits and vegetables and whole grains | – Fruits and vegetables (3 servings/day for 6 weeks) – Whole grains (3 servings/ day for 6 weeks) |
– No differences in fecal microbiota composition between groups of fruits and vegetables and whole grains – ↑ α-diversity in whole-grain group |
↓ Lipopolysaccharide-binding protein in both the fruits and vegetables and whole grain groups, ↓ IL-6 in fruits and vegetables group ↓TNF-α in whole-grain group |
ClinicalTrials.gov NCT02602496 |
[28] |
| 125 obese men and women (62 treated, 63 placebo) | Lactobacillus rhamnosus CGMCC1.3724 + oligofructose + inulin for 24 weeks | ↑ Fecal Lachnospiraceae family | ↓ Body weight only in women, ↓ Fat mass in women, ↓ Circulating leptin |
ClinicalTrials.gov NCT01106924 |
[31] |
In contrast, several trials found that consuming fruits, vegetables, and whole grains failed to alter the gut microbiota. For example, an 8-week randomized crossover trial investigated if a whole-grain-rich diet reduced body weight and inflammation in 60 adults who were at risk of developing metabolic syndrome [26]. The whole-grain group had higher alkylresorcinol levels in plasma than the refined-grain group, confirming compliance. Although whole-grain diet did not induce major changes in the gut microbiota, it decreased body weight and levels of IL-6 (particularly with rye intake) and C-reactive protein in the circulating blood. Similarly, in a randomized parallel trial, 70 healthy overweight adults consumed whole-grain rye, whole-grain wheat, or refined wheat for 6 weeks. None of the diets affected the gut microbiota’s composition, but the whole-grain groups had more flatulence and bowel movements and less bloating, suggesting that whole grains may be included in the diet to maintain gut health [27].
A head-to-head comparison of fruits and vegetables with whole grains on the impact of inflammatory markers and the gut microbiota’s composition was carried out in a randomized controlled trial with 49 overweight or obese subjects who habitually consumed few fruits, vegetables, or whole grains [28]. Individualized changes in microbiotic composition were observed, but differences among the groups were not identified except that α-diversity increased in the fruits and vegetables group. Lipopolysaccharide-binding protein was decreased in both groups. In addition, levels of IL-6 decreased in the fruits and vegetables group, whereas levels of TNF-α decreased in the whole-grain group. These data suggest that fruits and vegetables and whole grains exert anti-inflammatory effects through different mechanisms. Interestingly, their anti-inflammatory effects did not relate to changes in the gut microbiota’s composition; instead, they correlated with the microbiota’s composition at baseline.
Synbiotics—combinations of prebiotics and probiotics—are used to not only improve the survival of beneficial microorganisms added to the diet but also to stimulate the proliferation of specific native bacterial strains that inhabit the gastrointestinal tract [29]. However, the effects of synbiotics on metabolic health remain unclear, and they probably depend on the particular combination of probiotic and prebiotic [30]. Considering the huge number of possible combinations, application of synbiotics to modulate the intestinal microbiota in humans seems promising [30]. A study of 125 obese men and women investigated the effects of supplementation with Lactobacillus rhamnosus CGMCC1.3724 plus oligofructose and inulin on weight loss and maintenance [31]. This synbiotic intervention associated with weight loss only in the women, where it was accompanied by a significant reduction in fat mass and circulating leptin concentrations and increased abundance of bacteria in the Lachnospiraceae family in feces.
Despite some confusing results from human studies, the ability of fruits and vegetables and whole grains to modulate the gut microbiota in obese or overweight subjects and to have anti-inflammatory and other beneficial effects on gut health are consistent across studies. These results suggest that responses of the gut microbiotas of overweight or obese subjects to fruits and vegetables and whole grains are heterogeneous. Accordingly, it is reasonable to speculate that components of fruits, vegetables, and whole grains or their metabolites in the gut can suppress inflammation and improve gut health by modulating the immune system before changes in the gut microbiota become obvious. Also, the use of synbiotics for losing weight in overweight and obese subjects warrants further investigation.
5. FUNCTIONAL DISEASES OF THE GASTROINTESTINAL SYSTEM
It is not surprising that alterations in the gut microbiota have been associated with functional gastrointestinal diseases such as inflammatory bowel disease, gastroenteric infections, irritable bowel syndrome, and colorectal cancer [1]. In one study, 88 subjects at risk of developing colorectal cancer were recruited to a randomized dietary intervention trial of either a Mediterranean diet or healthy eating for 6 months [32] (Table 3). Both the diets, which doubled fruit and vegetable intake, failed to change the bacterial community in the colonic mucosa. Our group conducted an intervention trial using black raspberries where 20 colorectal cancer patients consumed freeze-dried black raspberry powder (60 g/day) for 1–9 weeks in a pre-surgical model [33]. Black raspberries significantly increased benzoate metabolites produced from the metabolism of polyphenols and anthocyanins by gut microbiota and were absorbed in the large intestine [34].
Table 3 ∣.
Effects of consuming fruits and vegetables and whole grains on gut microbiotas of subjects with functional gastrointestinal diseases
| Human populations | Fruits/vegetables/whole grains comsumed |
Gut microbiota altered | Other effects measured | Trial registration |
References |
|---|---|---|---|---|---|
| 88 healthy individuals at increased risk of colon cancer | Doubled fruit and vegetable intake with either a Mediterranean diet or Healthy Eating diet | No change in bacterial community | – |
ClinicalTrials.gov NCT00475722 |
[32] |
| 20 patients with colorectal cancer | Freeze-dried black raspberries for 1–9 weeks | ↑ Benzoate metabolites produced by gut microbiota metabolisms | – | – | [34] |
| 20 patients with an ileal pouch-anal anastomosis | Inulin for 3 weeks | ↓ Bacteroides fragilis | ↑ Fecal butyrate, ↓ Fecal pH, ↓ Fecal secondary bile acids |
– | [35] |
| 10 patients with active ileocolonic Crohn’s | Fructo-oligosaccharides for 3 weeks | ↑ Fecal Bifidobacteria | ↓ Harvey Bradshaw index, ↑ IL-10-, TLR2-, or TLR4-expressing dendritic cells |
– | [36] |
| 37 colon cancer patients and 43 polypectomized patients | Oligofructose-enriched inulin + Lactobacillus rhamnosus GG + Bifidobacterium lactis Bb12 for 12 weeks | ↑ Fecal Bifidobacterium and Lactobacillus, ↓ Fecal Clostridium perfringens | ↓ Colorectal proliferation, ↑ Epithelial barrier function, ↓ IL-2 secretion, ↑ IFN-γ secretion |
– | [37] |
| 15 colorectal cancer patients | Bifidobacterium lactis Bl-04 + Lactobacillus acidophilus NCFM + inulin for 8–78 days | ↑ Microbiota diversity, Fusobacterium, Selenomonas and Peptostreptococcus in tumor, ↑ Butyrate-producing bacteria, especially Faecalibacterium and Clostridiales spp. in the tumor, non-tumor mucosa and fecal microbiota |
– |
ClinicalTrials.gov NCT03072641 |
[38] |
| 120 ulcerative colitis patients | – Probiotic (Bifidobacterium longum) – Prebiotic (Psyllium) – Synbiotic (Bifidobacterium longum + Psyllium) |
– | UC patients on synbiotic therapy experienced greater quality of life than those on probiotic or prebiotic treatment. | – | [39] |
In patients with ileal pouch-anal anastomosis, inflammation in the ileal reservoir is a constant finding [35]. In healthy subjects, inulin, a dietary fiber, is fermented to SCFAs, which lower pH and change fecal flora [35]. The effects of dietary supplementation with inulin for 3 weeks on inflammation of the ileal reservoir was investigated in 20 patients with ileal pouch-anal anastomosis in a randomized, double-blind, crossover trial [35]. Inulin increased levels of butyrate, lowered pH, decreased numbers of Bacteroides fragilis, and decreased levels of secondary bile acids in feces. Endoscopic and histological findings showed reduced mucosal inflammation of the ileal reservoir. In another study, fructo-oligosaccharides increased fecal and mucosal Bifidobacteria in healthy volunteers: 10 patients with active ileocolonic Crohn’s disease who received fructo-oligo-saccharides for 3 weeks showed a decrease in the Harvey Bradshaw index and increased fecal Bifidobacteria concentrations [36]. Also, numbers of IL-10-, TLR2- (toll-like receptor), and TLR4-positive dendritic cells were increased by fructo-oligosaccharides, suggesting immunoregulatory effects. A 12-week randomized, double-blind, placebo-controlled trial determined the effects of a synbiotic preparation of oligofructose-enriched inulin plus L. rhamnosus GG and Bifidobacterium lactis Bb12 in 37 colon cancer patients and 43 polypectomized patients [37]. The synbiotic intervention significantly changed the fecal flora: abundances of Bifidobacterium and Lactobacillus increased, while those of Clostridium perfringens decreased. Synbiotic consumption also decreased colorectal proliferation, increased epithelial barrier function, and decreased IL-2 in the polypectomized patients and increased interferon (IFN)-γ in the colon cancer patients. These results suggest that synbiotic intervention can be beneficial to colon cancer patients and polypectomized patients. In another trial, 15 patients with colorectal cancer were treated with inulin and probiotics containing strains of Lactobacillus acidophilus and B. lactis for 8–78 days, depending on the time to surgery [38]. This synbiotic intervention increased the abundance of butyrate-producing bacteria (particularly Faecalibacterium and other Clostridiales) within the tumor, its associated non-tumor colonic mucosa, and stool [38].
Although most studies have focused on the use of probiotics or prebiotics for treating ulcerative colitis patients, a randomized controlled head-to-head comparison investigated whether synbiotic, probiotic, or prebiotic supplements could improve quality of life for such patients [39]. One hundred twenty ulcerative colitis patients were randomly assigned to three groups of 40 for probiotic (Bifidobacterium longum), prebiotic (psyllium), or synbiotic (B. longum + psyllium) therapy for 4 weeks. Intriguingly, better quality of life was reported by the ulcerative colitis patients who received the synbiotic therapy than those on either the probiotic or prebiotic intervention. These data suggest that adding synbiotic therapy to standard therapy might be a promising approach to improving the quality of life in ulcerative colitis patients.
The current findings suggest that prebiotics such as inulin and fructo-oligosaccharides and probiotics such as L. rhamnosus GG, B. lactis Bb12, and B. longum can improve gut health in functional diseases of the gastrointestinal tract. We argue that the combination of prebiotics and probiotics that constitutes synbiotics likely will produce even better protective effects because they provide the appropriate food source for the bacteria. This concept was supported by the ulcerative colitis trial in which synbiotics improved quality of life better than prebiotics or probiotics alone [39]. Therefore, synbiotic approaches warrant further investigation in patients with functional and other gastrointestinal diseases.
6. THE GUT MICROBIOTA AT BASELINE AFFECTS RESPONSES TO CANCER IMMUNOTHERAPY
Studies of radiation-induced gastrointestinal mucositis have suggested that the gut microbiota plays a major role in maintaining intestinal homoeostasis and integrity during chemotherapy [40]. Patients receiving cytotoxic and radiation therapy exhibit marked changes in the intestinal microbiota, most frequently with decreases in Bifidobacterium, Clostridium cluster XIVa, and Faecalibacterium prausnitzii and increases in Enterobacteriaceae and Bacteroides. These modifications may contribute to the development of features of mucositis, particularly diarrhea and bacteremia [40]. Whether the gut microbiota affects patients’ responses to chemotherapy or radiation therapy warrants investigation.
On the other hand, multiple human clinical trials have suggested that the composition of the gut microbiota at baseline might affect response to cancer immunotherapy (Table 4). Ipilimumab, an immune checkpoint inhibitor that targets cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), prolonged survival in a subset of patients with metastatic melanoma [41]. However, it also induced immune-related adverse events, including enterocolitis. One trial of ipilimumab studied 26 metastatic melanoma patients, comparing those whose guts were enriched with the Faecalibacterium genus and other Firmicutes at baseline with those who were enriched in Bacteroides. The former had longer progression-free survival and overall survival as well as more frequent colitis induced by ipilimumab. In a trial with 34 metastatic melanoma patients treated with ipilimumab, the presence of fecal bacteria in the phylum Bacteroidetes correlated with resistance to ipilimumab-induced colitis and changes in metabolomic pathways, such as polyamine transport and B vitamin biosynthesis, that is associate with increased risk of colitis [42]. Also, a trial with 39 metastatic melanoma patients studied the effects of pretreatment with gut microbiota and metabolites on responses to various immunotherapies: ipilimumab, nivolumab, ipilimumab plus nivolumab, or pembrolizumab. At baseline, the gut microbiota of all the responders was enriched in Bacteroides caccae and had higher anacardic acid levels [43]. Among the responders treated with ipilimumab plus nivolumab, it was enriched in F. prausnitzii, Bacteroides thetaiotamicron, and Holdemania filiformis. Among the responders treated with pembrolizumab, the microbiota was enriched for Dorea formicogenerans.
Table 4 ∣.
Baseline gut microbiota affect responses to cancer immunotherapies
| Cancer patients | Immunotherapy | Gut microbiota | Clinical trial registration |
References |
|---|---|---|---|---|
| 26 patients with metastatic melanoma | Ipilimumab | Baseline Faecalibacterium and other Firmicutes –respond better to ipilimumab –enterocolitis phenotype –increased regulatory T cells |
– | [41] |
| 34 metastatic melanoma patients | Ipilimumab | Baseline increased Bacteroidetes phylum → resistant to Ipilimumab-induced colitis | – | [42] |
| 39 metastatic melanoma patients | Ipilimumab, nivolumab, ipilimumab plus nivolumab, or pembrolizumab | Responders to all the therapies were enriched in fecal Bacteroides caccae at baseline. | – | [43] |
| 112 melanoma patients | Anti-PD1 immunotherapy | –Responders had higher α diversity in fecal bacteria and Ruminococcaceae family at baseline. –Responders had enriched anabolic pathways at baseline. |
– | [44] |
| 34 metastatic melanoma patients | Anti-PD1 immunotherapy | Responders had more fecal Bifidobacterium longum, Collinsella aerofaciens, and Enterococcus faecium at baseline. | – | [45] |
| 60 non-small-cell lung cancer and 40 renal cell carcinoma patients | Anti-PD1 immunotherapy | ↑ Akkermansia muciniphila in responders at baseline | – | [46] |
A few other studies have investigated relationships between the gut microbiota and responses to immunotherapy that suppresses Programmed Cell Death 1 Protein (PD1). One such trial included 112 melanoma patients treated with anti-PD1 immunotherapy [44]. Responders had increased alpha diversity and abundant Ruminococcaceae family members in their gut microbiotas. Their anabolic pathways were upregulated, and their systemic and antitumor immunity was enhanced [44]. Likewise, when 34 metastatic melanoma patients were treated with anti-PD1 immunotherapy, there was a significant association between commensal microbial composition at baseline and clinical response: B. longum, Collinsella aerofaciens, and Enterococcus faecium were more abundant in the responders at baseline [45]. Besides these studies with melanoma patients, the only trial that investigated the gut microbiota and efficacy of anti-PD1 immunotherapy against epithelial tumors, non-small-cell-lung cancer, and renal cell carcinoma suggested that antibiotics inhibited the clinical benefits of anti-PD1 therapy [46]. However, there was a positive correlation between the relative abundance of Akkermansia and clinical responses to such therapy in these patients [46].
7. DIETS, GUT MICROBIOTAS, AND RESPONSES TO CANCER IMMUNOTHERAPY
Several ongoing clinical trials are manipulating the gut microbiota through intensive lifestyle changes (diet, exercise, and psychosocial factors) or by administering probiotics or synbiotics, or by fecal transplantation to improve responses to cancer therapy [44]. As stated above, human clinical trials suggest that fruits and vegetables, whole grains, probiotics, or synbiotics can affect several bacterial groups and their downstream metabolites. This has important implications for cancer therapy, particularly immunotherapy [44,47]. Therefore, understanding how diets and their nutrients and their metabolites affect bacterial composition and dynamic functions and how microbes interact with the innate and adaptive human immune systems is not only urgently needed research but also could provide the opportunity to enhance responses to cancer immunotherapy [48].
As stated above, several clinical trials, particularly in melanoma patients, have repeatedly shown that the composition and diversity of the gut microbiota at baseline influences responses to cancer immunotherapy [41-46]. Supplementation with Akkermansia [43] or feeding certain foods that increase the abundance of Akkermansia, such as red pitaya (Hylocereus polyrhizus) betacyanins [49] or freeze-dried black raspberries [50]. These approaches warrant testing in non-small-cell lung cancer and renal cell carcinoma patients.
The safety, affordability, and accessibility of dietary interventions make them attractive for manipulating the gut microbiota and downstream immune responses in cancer patients [6]. For example, The Beans to Enrich the Gut Microbiome vs. Obesity’s Negative Effects trial (ClinicalTrials.gov: NCT02843425) was designed to investigate fiber supplementation in cancer patients. It is examining shifts in gut bacterial populations after cancer patients add half a cup of beans per day to their normal diets [6]. Another example is The Role of Lifestyle Factors in Breast Cancer-Related Outcomes (ClinicalTrials.gov: NCT02079662), a randomized trial that comprehensively overhauls the lifestyle of patients with stage III breast cancer who are starting radiation therapy. The subjects receive dietary counseling and meal delivery along with exercise programs and psychosocial services [6]. Another ongoing trial is investigating whether exercise impacts the composition of the gut microbiota in men undergoing androgen deprivation therapy for prostate cancer [51].
8. CONCLUSION
Dietary interventions that increase consumption of fruits and vegetables and whole grains to manipulate the gut microbiota in different human populations have reported discrepant findings. In general, these foods change the gut microbiota in healthy individuals and alter gut health and physiological measures. Conflicting data have been obtained from obese or overweight subjects, however, as these foods increased the diversity of gut microbes in some studies but failed to change it in others despite their consistently anti-inflammatory effects across all the studies. For functional gastrointestinal diseases, studies have focused on therapeutic approaches such as prebiotics (e.g., inulin and fructo-oligosaccharides) and probiotics (e.g., L. rhamnosus GG, B. lactis Bb12, and B. longum). These prebiotic and protbiotic approaches have improved gut health in patients with functional gastrointestinal diseases. Dietary approaches are yet to be studied in this population.
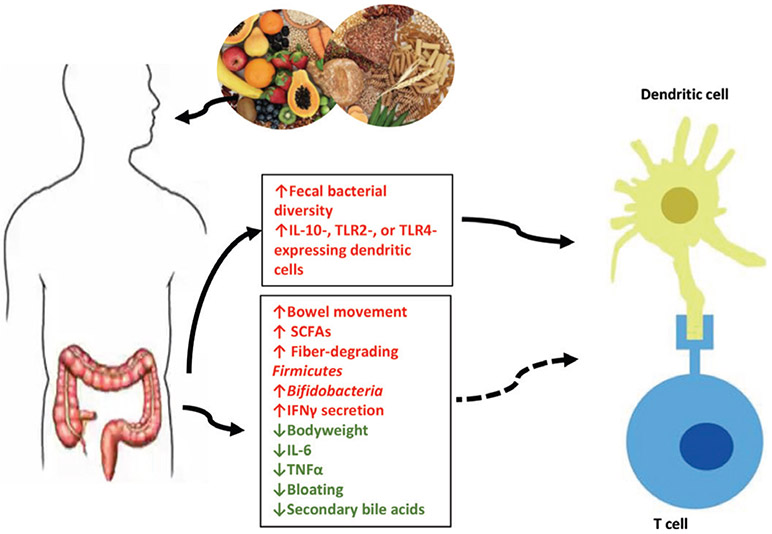
As evidence from several clinical trials suggests that baseline gut microbiota can predict responses to cancer immunotherapy, improving the composition of the gut microbiota before the onset of immunotherapy might favor patients’ responses. Dietary intervention using locally available fruits and vegetables and whole grains could be an affordable and safe strategy (Figure 1).
Figure 1 ∣.
Hypothetical scheme of the effects of consumption of fruits and vegetables and whole grains on cancer immunity. Evidences suggest that those foods enhance the diversity of gut microbiotas and other parameters, and together they might impact cancer immunity. Dashed line indicates the possible impact of these other parameters on cancer immunity.
Acknowledgments
FUNDING
This work was supported by NIH grants CA148818 and USDA/ NIFA 2020-67017-30843 (to L.-S. Wang), and CA185301, AI129582 and NS106170 (to J. Yu).
Footnotes
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
REFERENCES
- [1].Ianiro G, Bibbò S, Gasbarrini A, Cammarota G. Therapeutic modulation of gut microbiota: current clinical applications and future perspectives. Curr Drug Targets 2014;15:762–70. [DOI] [PubMed] [Google Scholar]
- [2].Markowski MC, Boorjian SA, Burton JP, Hahn NM, Ingersoll MA, Vareki SM, et al. The microbiome and genitourinary cancer: a collaborative review. Eur Urol 2019;75:637–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Plaza-Díaz J, Álvarez-Mercado AI, Ruiz-Marín CM, Reina-Pérez I, Pérez-Alonso AJ, Sánchez-Andujar MB, et al. Association of breast and gut microbiota dysbiosis and the risk of breast cancer: a case-control clinical study. BMC Cancer 2019;19:495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Cram JA, Fiore-Gartland AJ, Srinivasan S, Karuna S, Pantaleo G, Tomaras GD, et al. Human gut microbiota is associated with HIV-reactive immunoglobulin at baseline and following HIV vaccination. PLoS One 2019;14:e0225622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Oh B, Kim BS, Kim JW, Kim JS, Koh SJ, Kim BG, et al. The effect of probiotics on gut microbiota during the Helicobacter pylori eradication: randomized controlled trial. Helicobacter 2016;21:165–74. [DOI] [PubMed] [Google Scholar]
- [6].Gopalakrishnan V, Helmink BA, Spencer CN, Reuben A, Wargo JA. The influence of the gut microbiome on cancer, immunity, and cancer immunotherapy. Cancer Cell 2018;33:570–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Aron-Wisnewsky J, Clément K. The gut microbiome, diet, and links to cardiometabolic and chronic disorders. Nat Rev Nephrol 2016;12:169–81. [DOI] [PubMed] [Google Scholar]
- [8].Rajilić-Stojanović M, Jonkers DM, Salonen A, Hanevik K, Raes J, Jalanka J, et al. Intestinal microbiota and diet in IBS: causes, consequences, or epiphenomena? Am J Gastroenterol 2015;110:278–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol 2015;12:205–17. [DOI] [PubMed] [Google Scholar]
- [10].Zitvogel L, Ma Y, Raoult D, Kroemer G, Gajewski TF. The microbiome in cancer immunotherapy: diagnostic tools and therapeutic strategies. Science 2018;359:1366–70. [DOI] [PubMed] [Google Scholar]
- [11].Thomas RM, Jobin C. Microbiota in pancreatic health and disease: the next frontier in microbiome research. Nat Rev Gastroenterol Hepatol 2020;17:53–64. [DOI] [PubMed] [Google Scholar]
- [12].Catalkaya G, Venema K, Lucini L, Rocchetti G, Delmas D, Daglia M, et al. Interaction of dietary polyphenols and gut microbiota: microbial metabolism of polyphenols, influence on the gut microbiota, and implications on host health. Food Front 2020;1:109–33. [Google Scholar]
- [13].Cianciosi D, Forbes-Hernández TY, Giampieri F, Zhang J, Ansary J, Pacetti M, et al. Effect of in vitro gastrointestinal digestion on the bioaccessibility of phenolic compounds and antioxidant activity of manuka honey. eFood 2019;1:85–93. [Google Scholar]
- [14].Zhang L, Shi M, Tian M, Wang X, Ji J, Liao X, et al. Guidelines for absolute quantitative real-time PCR for microbial determination in in vitro gastrointestinal digestion. Food Front 2020;1:200–4. [Google Scholar]
- [15].Markowiak P, Ślizewska K. Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients 2017;9:1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Chung WSF, Walker AW, Louis P, Parkhill J, Vermeiren J, Bosscher D, et al. Modulation of the human gut microbiota by dietary fibres occurs at the species level. BMC Biol 2016;14:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Klil-Drori AJ, Azoulay L, Pollak MN. Cancer, obesity, diabetes, and antidiabetic drugs: is the fog clearing? Nat Rev Clin Oncol 2017;14:85–99. [DOI] [PubMed] [Google Scholar]
- [18].De Filippis F, Pellegrini N, Vannini L, Jeffery IB, La Storia A, Laghi L, et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 2016;65:1812–21. [DOI] [PubMed] [Google Scholar]
- [19].Vanegas SM, Meydani M, Barnett JB, Goldin B, Kane A, Rasmussen H, et al. Substituting whole grains for refined grains in a 6-wk randomized trial has a modest effect on gut microbiota and immune and inflammatory markers of healthy adults. Am J Clin Nutr 2017;105:635–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Martínez I, Lattimer JM, Hubach KL, Case JA, Yang J, Weber CG, et al. Gut microbiome composition is linked to whole grain-induced immunological improvements. ISME J 2013;7:269–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Cooper DN, Kable ME, Marco ML, De Leon A, Rust B, Baker JE, et al. The effects of moderate whole grain consumption on fasting glucose and lipids, gastrointestinal symptoms, and microbiota. Nutrients 2017;9:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Cotillard A, Kennedy SP, Kong LC, Prifti E, Pons N, Le Chatelier E, et al. Dietary intervention impact on gut microbial gene richness. Nature 2013;500:585–8. [DOI] [PubMed] [Google Scholar]
- [23].Schutte S, Esser D, Hoevenaars FPM, Hooiveld GJEJ, Priebe MG, Vonk RJ, et al. A 12-wk whole-grain wheat intervention protects against hepatic fat: the Graandioos study, a randomized trial in overweight subjects. Am J Clin Nutr 2018;108:1264–74. [DOI] [PubMed] [Google Scholar]
- [24].Xiao S, Fei N, Pang X, Shen J, Wang L, Zhang B, et al. A gut microbiota-targeted dietary intervention for amelioration of chronic inflammation underlying metabolic syndrome. FEMS Microbiol Ecol 2014;87:357–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Foerster J, Maskarinec G, Reichardt N, Tett A, Narbad A, Blaut M, et al. The influence of whole grain products and red meat on intestinal microbiota composition in normal weight adults: a randomized crossover intervention trial. PLoS One 2014;9:e109606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Roager HM, Vogt JK, Kristensen M, Hansen LBS, Ibrügger S, Msrkedahl RB, et al. Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: a randomised cross-over trial. Gut 2019;68:83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Vuholm S, Nielsen DS, Iversen KN, Suhr J, Westermann P, Krych L, et al. Whole-grain rye and wheat affect some markers of gut health without altering the fecal microbiota in healthy overweight adults: a 6-week randomized trial. J Nutr 2017;147:2067–75. [DOI] [PubMed] [Google Scholar]
- [28].Kopf JC, Suhr MJ, Clarke J, Eyun SI, Riethoven JJM, Ramer-Tait AE, et al. Role of whole grains versus fruits and vegetables in reducing subclinical inflammation and promoting gastrointestinal health in individuals affected by overweight and obesity: a randomized controlled trial. Nutr J 2018;17:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Gourbeyre P, Denery S, Bodinier M. Probiotics, prebiotics, and synbiotics: impact on the gut immune system and allergic reactions. J Leukoc Biol 2011;89:685–95. [DOI] [PubMed] [Google Scholar]
- [30].de Vrese M, Schrezenmeir J. Probiotics, prebiotics, and synbiotics. Adv Biochem Eng Biotechnol 2008;111:1–66. [DOI] [PubMed] [Google Scholar]
- [31].Sanchez M, Darimont C, Drapeau V, Emady-Azar S, Lepage M, Rezzonico E, et al. Effect of Lactobacillus rhamnosus CGMCC1.3724 supplementation on weight loss and maintenance in obese men and women. Br J Nutr 2014;111:1507–19. [DOI] [PubMed] [Google Scholar]
- [32].Djuric Z, Bassis CM, Plegue MA, Ren J, Chan R, Sidahmed E, et al. Colonic mucosal bacteria are associated with inter-individual variability in serum carotenoid concentrations. J Acad Nutr Diet 2018;118:606.e3–16.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Wang LS, Arnold M, Huang YW, Sardo C, Seguin C, Martin E, et al. Modulation of genetic and epigenetic biomarkers of colorectal cancer in humans by black raspberries: a phase I pilot study. Clin Cancer Res 2011;17:598–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Pan P, Skaer CW, Stirdivant SM, Young MR, Stoner GD, Lechner JF, et al. Beneficial regulation of metabolic profiles by black raspberries in human colorectal cancer patients. Cancer Prev Res (Phila) 2015;8:743–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Welters CFM, Heineman E, Thunnissen FBJM, van den Bogaard AEJM, Soeters PB, Baeten CGMI. Effect of dietary inulin supplementation on inflammation of pouch mucosa in patients with an ileal pouch-anal anastomosis. Dis Colon Rectum 2002;45:621–7. [DOI] [PubMed] [Google Scholar]
- [36].Lindsay JO, Whelan K, Stagg AJ, Gobin P, Al-Hassi HO, Rayment N, et al. Clinical, microbiological, and immunological effects of fructo-oligosaccharide in patients with Crohn’s disease. Gut 2006;55:348–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Rafter J, Bennett M, Caderni G, Clune Y, Hughes R, Karlsson PC, et al. Dietary synbiotics reduce cancer risk factors in polypectomized and colon cancer patients. Am J Clin Nutr 2007;85:488–96. [DOI] [PubMed] [Google Scholar]
- [38].Hibberd AA, Lyra A, Ouwehand AC, Rolny P, Lindegren H, Cedgard L, et al. Intestinal microbiota is altered in patients with colon cancer and modified by probiotic intervention. BMJ Open Gastroenterol 2017;4:e000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Fujimori S, Gudis K, Mitsui K, Seo T, Yonezawa M, Tanaka S, et al. A randomized controlled trial on the efficacy of synbiotic versus probiotic or prebiotic treatment to improve the quality of life in patients with ulcerative colitis. Nutrition 2009;25:520–5. [DOI] [PubMed] [Google Scholar]
- [40].Touchefeu Y, Montassier E, Nieman K, Gastinne T, Potel G, Bruley des Varannes S, et al. Systematic review: the role of the gut microbiota in chemotherapy- or radiation-induced gastrointestinal mucositis - current evidence and potential clinical applications. Aliment Pharmacol Ther 2014;40:409–21. [DOI] [PubMed] [Google Scholar]
- [41].Chaput N, Lepage P, Coutzac C, Soularue E, Le Roux K, Monot C, et al. Baseline gut microbiota predicts clinical response and colitis in metastatic melanoma patients treated with ipilimumab. Ann Oncol 2017;28:1368–79. [DOI] [PubMed] [Google Scholar]
- [42].Dubin K, Callahan MK, Ren B, Khanin R, Viale A, Ling L, et al. Intestinal microbiome analyses identify melanoma patients at risk for checkpoint-blockade-induced colitis. Nat Commun 2016;7:10391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Frankel AE, Coughlin LA, Kim J, Froehlich TW, Xie Y, Frenkel EP, et al. Metagenomic shotgun sequencing and unbiased metabolomic profiling identify specific human gut microbiota and metabolites associated with immune checkpoint therapy efficacy in melanoma patients. Neoplasia 2017;19:848–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Gopalakrishnan V, Spencer CN, Nezi L, Reuben A, Andrews MC, Karpinets TV, et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science 2018;359:97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Matson V, Fessler J, Bao R, Chongsuwat T, Zha Y, Alegre ML, et al. The commensal microbiome is associated with anti-PD-1 efficacy in metastatic melanoma patients. Science 2018;359:104–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Routy B, Le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillere R, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science 2018;359:91–7. [DOI] [PubMed] [Google Scholar]
- [47].Shortt C, Hasselwander O, Meynier A, Nauta A, Fernández EN, Putz P, et al. Systematic review of the effects of the intestinal microbiota on selected nutrients and non-nutrients. Eur J Nutr 2018;57:25–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Ma N, Guo P, Zhang J, He T, Kim SW, Zhang G, et al. Nutrients mediate intestinal bacteria-mucosal immune crosstalk. Front Immunol 2018;9:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Song H, Chu Q, Yan F, Yang Y, Han W, Zheng X. Red pitaya betacyanins protects from diet-induced obesity, liver steatosis and insulin resistance in association with modulation of gut microbiota in mice. J Gastroenterol Hepatol 2016;31:1462–9. [DOI] [PubMed] [Google Scholar]
- [50].Pan P, Lam V, Salzman N, Huang Y-W, Yu J, Zhang J, et al. Black raspberries and their anthocyanin and fiber fractions alter the composition and diversity of gut microbiota in F-344 rats. Nutr Cancer 2017;69:943–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Newton RU, Christophersen CT, Fairman CM, Hart NH, Taaffe DR, Broadhurst D, et al. Does exercise impact gut microbiota composition in men receiving androgen deprivation therapy for prostate cancer? A single-blinded, two-armed, randomised controlled trial. BMJ Open 2019;9:e024872. [DOI] [PMC free article] [PubMed] [Google Scholar]