Abstract
As pregnant women are at high risk of severe SARS-CoV-2 infection and COVID-19 vaccines are available in Switzerland, this study aimed to assess the willingness of Swiss pregnant and breastfeeding women to become vaccinated. Through a cross-sectional online study conducted after the first pandemic wave, vaccination practices and willingness to become vaccinated against SARS-CoV-2 if a vaccine was available were evaluated through binary, multi-choice, and open-ended questions. Factors associated with vaccine willingness were evaluated through univariable and multivariable analysis. A total of 1551 women responded to questions related to the primary outcome. Only 29.7% (153/515) of pregnant and 38.6% (400/1036) of breastfeeding women were willing to get vaccinated against SARS-CoV-2 if a vaccine had been available during the first wave. Positive predictors associated with SARS-CoV-2 vaccine acceptance were an age older than 40 years, a higher educational level, history of influenza vaccination within the previous year, having an obstetrician as the primary healthcare practitioner, and being in their third trimester of pregnancy. After the first pandemic wave, Switzerland had a low SARS-CoV-2 vaccination acceptance rate, emphasizing the need to identify and reduce barriers for immunization in pregnant and breastfeeding women, particularly among the youngest and those with a lower educational level.
Keywords: SARS-CoV-2, coronavirus, COVID-19, pregnancy, breastfeeding, vaccine willingness
1. Introduction
In 2020, the outbreak of a novel coronavirus, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was declared a pandemic with more than 166 million confirmed cases worldwide. In Switzerland, more than 680,000 people tested positive with more than 10,000 deaths reported [1].
Pregnant women are considered a vulnerable population for SARS-CoV-2 infection. Current evidence suggests that they are up to 70% more susceptible to infection. If infected, they are also at greater risk of developing complications [2,3,4] such as admission to an intensive care unit, mechanical ventilation, and death [5,6]. Increased risk of caesarian section, iatrogenic prematurity, post-partum hemorrhage, preeclampsia, and miscarriage have also been reported [7,8,9,10,11].
Currently, two SARS-CoV-2 mRNA vaccines approved by Swissmedic (the Swiss authority for the utilization and surveillance of therapeutic products) are used in the vaccine campaign in Switzerland [12]. However, vaccines cannot curb epidemics without widespread acceptance. The World Health Organization (WHO) has listed vaccine hesitancy as one of the top ten threats to global health [13], especially for populations at risk. In Switzerland, as in many countries, vaccination programs have already been established to protect pregnant women and their infants from serious infections such as influenza and pertussis. Both influenza and pertussis vaccines have proven to be effective in protecting mothers and their newborns [14,15]. However, immunization rates for influenza and pertussis have been disappointingly low in Switzerland [16] mainly due to a lack of adequate promotion and compliance [17]. Low uptake of vaccination in pregnancy has been reported worldwide [18,19] with several studies identifying inadequate knowledge about the disease threat; doubts about vaccine safety, efficacy, and benefits; and the lack of recommendations from vaccine providers, as the main obstacles among pregnant women [20,21,22]. Maternal characteristics may also play a role. Unemployment, younger age (<25 years old), and high perceived stress have been associated with lower vaccination rates during pregnancy, whereas a history of depression increased the likelihood of being vaccinated [23].
SARS-CoV-2 vaccination has recently been recommended in Switzerland for pregnant women who have additional risk factors or are at high risk of exposure through their work. This vaccination strategy may represent a barrier to the successful vaccination of all members of this high-risk group, especially when compared to some countries where pregnant women are routinely vaccinated or considered a priority group. This is a glaring example of the need to better understand the many factors influencing the acceptance of and access to vaccination, especially among more vulnerable populations such as pregnant women to develop targeted information campaigns.
Thus, in a cross-sectional survey during the first wave of the pandemic, we investigated COVID-19 vaccine willingness among Swiss pregnant and breastfeeding women if a vaccine was available, as well as the factors contributing to their acceptance or hesitancy.
2. Materials and Methods
2.1. Study Population and Data Collection
This Swiss cross-sectional online study is part of a European multi-center study conducted in several countries (Belgium, Ireland, Norway, The Netherlands, United Kingdom) and approved by the Ethics Committee Research of UZ/KU Leuven (id: S63966). The questionnaire used in Switzerland was available in German, French, and Italian. The goal was to examine the overall impact of the SARS-CoV-2 pandemic on pregnant and breastfeeding women (i.e., pregnancy/breastfeeding experience, life and professional habits, mental health status, relationship with the healthcare system, medication use, and vaccine perceptions during pregnancy/breastfeeding) [24]. The COVID-19 vaccine willingness of pregnant and breastfeeding women included in the multi-center study has already been published [25], and the Swiss rate was among the lowest, hence the need to investigate the factors associated with vaccine acceptance in a Swiss-specific study.
In Switzerland, the online questionnaire was accessible from 18 June to 12 July 2020 through websites, forums, and social media (www.letsfamily.ch, www.swissmom.ch, www.medela.ch, www.chuv.ch). All data were collected and processed anonymously. All participants provided online informed consent prior to survey initiation.
2.2. Study Population
To be eligible, Swiss women needed to be at least 18 years old and be pregnant at the time of the survey or have breastfed within the past three months.
2.3. Variables
We collected information on sociodemographic characteristics (i.e., age, primary language, marital status, working status, education level), medical history (i.e., gravidity, parity, co-morbidities, smoking during pregnancy, main practitioner for the pregnancy follow-up, clinical course of the neonate for breastfeeding mothers), exposure to SARS-CoV-2 or presence in an at-risk setting (i.e., symptoms potentially related to COVID-19, hospitalization related to COVID-19, testing by RT-PCR, serology or computed tomography, living with someone who tested positive, co-habiting with an elderly person (>65 years old)). The negative impact of the SARS-CoV-2 pandemic on the pregnancy/breastfeeding experience, life habits, and work was assessed through participants graded answers: “yes” or “rather yes”, grouped as “negative impact of the SARS-CoV-2 pandemic”; and “rather no” or “no”, grouped as “no negative impact of the SARS-CoV-2 pandemic”. Mental health status was assessed using validated screening tests including the Edinburgh Postnatal Depression Scale for depression [26,27], the Generalized Anxiety Disorder 7-item Scale for anxiety [28], and the Perceived Stress Scale for stress [29,30]. Information on vaccination practices was obtained through a dichotomic question on vaccination against influenza within the past year (yes or no) and multi-choice questions assessing their opinion on influenza vaccine usefulness during pregnancy and breastfeeding, the fear of maternal and fetal/neonatal side effects, and overall vaccination acceptance.
2.4. Main Outcomes
COVID-19 vaccine willingness of pregnant and breastfeeding women if a vaccine had been available was evaluated through participants’ graded answers: “fully agree”, “rather agree”, “rather disagree”, or “fully disagree”. Participants who “fully agree” or “rather agree” were grouped as “willing to get vaccinated against SARS-CoV-2” and those who “rather disagree” or “fully disagree” were grouped as “not willing to get vaccinated against SARS-CoV-2” in the analysis.
2.5. Statistical Analysis
Baseline and medical characteristics, SARS-CoV-2 exposure (SARS-CoV-2 testing, symptoms, and hospitalization), fears, impacts of the pandemic, mental health symptoms, and vaccination habits were presented using descriptive statistics for both pregnant and breastfeeding women. The prevalence of participants willing to get vaccinated against COVID-19 was calculated.
The associations between variables of interest and the willingness to get vaccinated against SARS-CoV-2 was measured by univariate and multivariate logistic regression and were presented as crude odds ratios (OR) and adjusted odds ratios (aORs) with 95% confidence intervals (95% CI). Variables with p > 0.10 in the univariate analysis were not included in the multivariate model. The variables of interest were maternal age >40 years old, educational level (dichotomized as higher than high school or not), professional activity (dichotomized as active or not), primary language (French, German, Italian), maternal co-morbidities (grouped into a single “any maternal co-morbidity” variable), testing positive for SARS-CoV-2 infection (either by RT-PCR, serology, or CT-scan, grouped into a single “tested positive for SARS-CoV-2” variable), living with someone >65 years old, having a negative impact by the pandemic on the pregnancy/breastfeeding experience, life habits, and work, experiencing symptoms of severe depression (EDS ≥ 13), anxiety (GAD-7 ≥ 15), or high stress perceived (PSS ≥ 27) (grouped into a single variable), being vaccinated against influenza in the past year, previous history of declining vaccination, and fear of side effects related to vaccines (for the mother and the fetus/neonate). Variables specific to pregnant women (pregnancy practitioner, current trimester of gestation, and fear of an adverse fetal outcome in case of maternal SARS-CoV-2 infection) were studied in a supplementary multivariate model including only pregnant participants.
2.6. Missing Values
Maternal comorbidities were considered as absent if not reported, based on the assumption that severe comorbidities are normally documented. Based on the hypothesis of missing variables completely at random (MCAR), multiple imputations with chained equations (10 replications) were performed to increase the power of comparisons for missing values.
3. Results
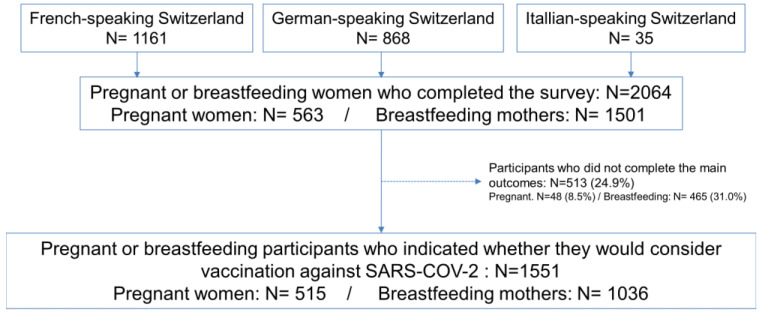
A total of 2064 respondents participated in the survey (1161 using the French questionnaire, 868 using the German questionnaire, and 35 using the Italian questionnaire) including 1501 breastfeeding and 563 pregnant women. Among them, 513 (24.9%) did not answer the question relating to whether they were willing to get vaccinated against SARS-CoV-2 if a vaccine was available. Thus, 75.1% (n = 1551) contributed to the analyses addressing the primary aim of the study (1036 breastfeeding mothers and 515 pregnant women) (Figure 1).
Figure 1.
Flow chart.
3.1. Baseline Characteristics
Baseline characteristics are presented in Table 1. The median age of respondents was 33 years and the majority were married or cohabiting (79.8%; 1237/1551). A significant proportion of women were healthcare providers (20.4%; 317/1551) or homemakers (9.0%; 139/1551). A high proportion of participants (46.5%; 721/1551) had an education level above high school. Overall, 9.7% (151/1551) reported having co-morbidities.
Table 1.
Baseline characteristics and medical history of participants. Abbreviations: ENT, ear nose throat; IQR, interquartile range; NICU, neonatal intensive care unit, HCP, healthcare provider.
| Pregnant Women | Breastfeeding Mothers | Total | |||||
|---|---|---|---|---|---|---|---|
| n = 515 | (%) | n = 1036 | (%) | n = 1551 | (%) | ||
| Baseline characteristics | |||||||
| Maternal age (years)—median (IQR) | 33 | (31–35) | 33 | (31–35) | 33 | (31–35) | |
| >40 years | 19 | (3.7) | 63 | (6.1) | 82 | (5.3) | |
| Marital status | |||||||
| Married/cohabiting | 422 | (81.9) | 815 | (78.7) | 1237 | (79.8) | |
| Single/divorced/others | 4 | (0.8) | 9 | (0.9) | 13 | (0.8) | |
| Unknown | 89 | (17.3) | 212 | (20.5) | 301 | (19.4) | |
| Working status | |||||||
| Health care provider | 122 | (23.7) | 195 | (18.8) | 317 | (20.4) | |
| Employed other than HCP | 257 | (49.9) | 465 | (44.9) | 722 | (46.6) | |
| Student | 3 | (0.6) | 7 | (0.7) | 10 | (0.6) | |
| Housewife | 21 | (4.1) | 118 | (11.4) | 139 | (9.0) | |
| Job seeker | 12 | (2.3) | 23 | (2.2) | 35 | (2.3) | |
| Unknown | 100 | (19.4) | 228 | (22.0) | 328 | (21.1) | |
| Educational level | |||||||
| Less than high school | 9 | (1.8) | 20 | (1.9) | 29 | (1.9) | |
| High school | 75 | (14.6) | 212 | (20.5) | 287 | (18.5) | |
| More than high school | 257 | (49.9) | 464 | (44.8) | 721 | (46.5) | |
| Unknown | 174 | (33.8) | 340 | (32.8) | 514 | (33.0) | |
| Primary language | |||||||
| French | 217 | (42.1) | 418 | (40.4) | 635 | (40.9) | |
| German | 183 | (35.5) | 322 | (31.1) | 505 | (32.6) | |
| Italian | 8 | (1.6) | 23 | (2.2) | 31 | (2.0) | |
| Other | 18 | (3.5) | 61 | (5.8) | 79 | (5.1) | |
| Unknown | 89 | (17.3) | 212 | (20.5) | 301 | (19.4) | |
| Maternal co-morbidities | |||||||
| Any comorbidity | 51 | (9.9) | 100 | (9.7) | 151 | (9.7) | |
| Pulmonary | 14 | (2.7) | 28 | (2.7) | 42 | (2.7) | |
| Cardio-vascular | 6 | (1.2) | 11 | (1.1) | 17 | (1.1) | |
| Pregestational diabetes | 5 | (1.0) | 9 | (0.9) | 14 | (0.9) | |
| Thyroid dysfunction | 12 | (2.3) | 27 | (2.6) | 39 | (2.5) | |
| Oncologic | 1 | (0.2) | 2 | (0.2) | 3 | (0.2) | |
| Hematologic | 2 | (0.4) | 0 | (0.0) | 2 | (0.1) | |
| Auto-immune | 2 | (0.4) | 4 | (0.4) | 6 | (0.4) | |
| Neurologic | 3 | (0.6) | 4 | (0.4) | 7 | (0.5) | |
| Psychic | 3 | (0.6) | 6 | (0.6) | 9 | (0.6) | |
| Digestive | 3 | (0.6) | 7 | (0.7) | 10 | (0.7) | |
| Uro-genital tract | 6 | (1.2) | 15 | (1.4) | 21 | (1.4) | |
| Cutaneous | 2 | (0.4) | 4 | (0.4) | 6 | (0.4) | |
| ENT | 0 | (0.0) | 1 | (0.1) | 1 | (0.1) | |
| Smoking | 69 | (13.4) | 149 | (14.4) | 218 | (14.1) | |
| Actual pregnancy or breastfeeding | |||||||
| Practitioner: | Obstetrician | 468 | 90.9 | / | |||
| Midwife | 13 | 8.3 | |||||
| Family physician | 4 | 0.8 | |||||
| Gestation | 1 | 240 | 46.6 | / | |||
| >1 | 275 | 53.4 | |||||
| Parity | 0 | 20/274 | 7.3 | / | |||
| 1 | 204/274 | 74.4 | |||||
| >1 | 50/274 | 18.2 | |||||
| Planned pregnancy | 483 | 93.8 | / | ||||
| Gestational age—median (IQR) | 28 | (18-34) | / | ||||
| 1st Trimester | 79 | (15.0) | |||||
| 2nd Trimester | 194 | (40.7) | |||||
| 3rd Trimester | 241 | (44.3) | |||||
| Neonate hospitalized in NICU | / | 29 | (2.8) | ||||
Among the pregnant participants, the median gestational age was 28 weeks’ gestation at the time of survey completion. Half of them were multigravida (275/515), among which 74.4% (204/274) and 18.2% (50/274) had one or more previous children respectively. More than 90% (468/515) were under the care of an obstetrician. Among the breastfeeding participants, 2.8% (29/1036) had their neonates hospitalized in an intensive care unit.
3.2. SARS-CoV-2 Exposure, Fears, and Beliefs
Data on SARS-CoV-2 exposure, fears, and beliefs are presented in Table 2. Almost 55% (850/1551) of participants reported having experienced symptoms potentially related to SARS-CoV-2 within the 3 months preceding the survey. Only 10.9% (170/1551) of the women had been tested for SARS-CoV-2 infection, among which 10.5% had a positive result (18/170) through a PCR-based nasopharyngeal swab, serology, or CT-scan. Less than 1.0% (9/1551) reported having been hospitalized due to COVID-19. Only 1.2% (18/1551) of participants reported living with someone older than 65 years old. Participants reported that the COVID-19 pandemic had a negative impact on their pregnancy or breastfeeding experience in 35.3% (97/275) and 8.0% (41/512) of cases, respectively. According to their responses, 11.0% (170/1551) of them experienced symptoms of severe depression (EDS ≥ 13), anxiety (GAD-7 ≥ 15), or high stress (PSS ≥ 27) over the last four weeks. More than half of pregnant women (53.4%; 275/515) declared that they feared an adverse fetal outcome in case of maternal infection.
Table 2.
SARS-CoV-2 exposure, fears, and beliefs. Abbreviations: PCR, polymerase chain reaction.
| Pregnant Women | Breastfeeding Mothers | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| n = 515 | (%) | n = 1036 | (%) | n = 1551 | (%) | |||
| SARS-COV-2 exposure | ||||||||
| Symptoms during the 3 last months | 296 | (57.5) | 554 | (53.5) | 850 | (54.8) | ||
| Hospitalized for COVID-19 | 2 | (0.4) | 7 | (0.7) | 9 | (0.6) | ||
| Tested for SARS-CoV-2 infection | 48 | (9.3) | 122 | (11.8) | 170 | (10.9) | ||
| PCR on nasopharyngeal swab | 39 | (7.6) | 112 | (108.0) | 151 | (9.7) | ||
| positive | 5/39 | (12.8) | 6/112 | (5.3) | 11/151 | (7.3) | ||
| negative | 33/39 | (84.6) | 103/112 | (92.0) | 136/151 | (90.1) | ||
| unknown | 1/39 | (2.6) | 3/112 | (2.7) | 4/151 | (2.7) | ||
| Serology | 7 | (1.4) | 21 | (2.0) | 28 | (1.8) | ||
| positive | 3/7 | (42.9) | 2/21 | (9.5) | 5/28 | (17.9) | ||
| negative | 3/7 | (42.9) | 16/21 | (76.2) | 19/28 | (67.9) | ||
| unknown | 1/7 | (14.2) | 3/21 | (14.3) | 4/28 | (14.3) | ||
| Scanner | 2 | (0.4) | 2 | (0.2) | 4 | (2.6) | ||
| positive | 2/2 | (100.0) | 0/2 | (0.0) | 2/4 | (50.0) | ||
| negative | 0/2 | (0.0) | 2/2 | (100.0) | 2/4 | (50.0) | ||
| Living with someone with symptoms | 82 | (15.9) | 220 | (21.2) | 302 | (19.5) | ||
| Living with someone tested positive | 4 | (0.8) | 10 | (1.0) | 14 | (0.9) | ||
| Living with someone > 65 years old | 6 | (1.2) | 12 | (1.2) | 18 | (1.2) | ||
| Negative impact of the COVID-19 pandemic on: | ||||||||
| Pregnancy or breastfeeding experience | 97 | (18.8) | 41 | (4.0) | 138 | (8.9) | ||
| unknown | 240 | (46.6) | 524 | (50.6) | 764 | (49.3) | ||
| Life habits | 350 | (68.2) | 700 | (67.6) | 1050 | (67.7) | ||
| unknown | 8 | (1.6) | 25 | (2.4) | 33 | (2.1) | ||
| Work | 295 | (57.3) | 394 | (38.0) | 689 | (44.4) | ||
| unknown | 100 | (19.4) | 320 | (30.9) | 420 | (27.1) | ||
| Fear of an adverse fetal outcome | 275 | (53.4) | / | |||||
| Symptoms of severe depression, anxiety or high stress perceived during the 1st wave | 53 | (10.3) | 117 | (11.3) | 170 | (11.0) | ||
3.3. Vaccination Practices and Beliefs
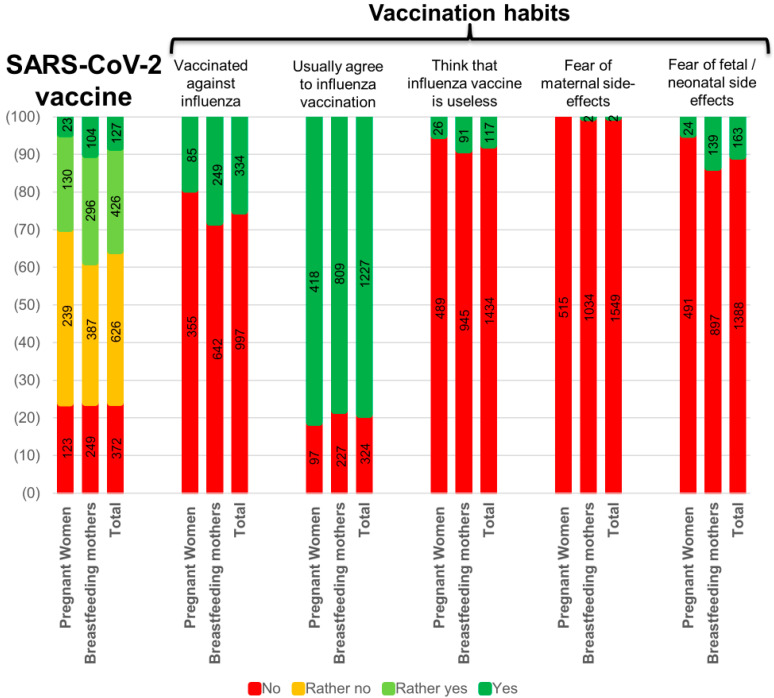
Only 19.3% (85/440) of pregnant and 28.0% (249/891) of breastfeeding women were vaccinated against influenza in the past year. Among the participants, 10.5% (163/1551) and 0.1% (2/1551) mentioned fear of potential consequences for their fetus/infant or themselves respectively resulting from vaccination during pregnancy or breastfeeding. More than 20% (324/1551) of them indicated usually declining influenza vaccination, and 7.5% (117/1551) think the influenza vaccine is not needed during pregnancy or breastfeeding (Figure 2).
Figure 2.
SARS-CoV-2 vaccine willingness among Swiss pregnant and breastfeeding women, and vaccination habits.
3.4. Willingness to Get the SARS-CoV-2 Vaccine
Only 29.7% (153/515) of pregnant and 38.6% (400/1036) of breastfeeding women were willing to get vaccinated against SARS-CoV-2 if a vaccine had been available during the first wave. More specifically, 8.1% (127/1551) fully agreed, 27.5% (426/1551) somewhat agreed, 40.4% (626/1551) somewhat disagreed, and 24% (372/1551) fully disagreed to get vaccinated (Figure 2 and Table S1).
3.5. Factors Associated with SARS-CoV-2 Vaccine Willingness
Potential predictors of SARS-CoV-2 vaccine acceptance are shown in Table 3. Sociodemographic factors such as a maternal age above 40 years old (aOR 1.8 [1.1–3.2]), an educational level higher than high school (aOR 1.5 [1.2–2.0]), and Italian as a primary language (aOR 3.3 [1.4–8.0]) were associated with a higher rate of vaccine acceptance. On the other hand, German-speaking participants were less likely to get vaccinated (aOR 0.7 [0.5–0.9]).
Table 3.
Factors associated with SARS-CoV-2 vaccine willingness among Swiss pregnant and breastfeeding women. Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; CT, computed tomography; OR, odds ratio; RT-PCR, reverse-transcriptase polymerase chain reaction; T, trimester of gestation.
| Participants Willing to Get Vaccinated against COVID-19 | Participants Not Willing to Get Vaccinated against COVID-19 | OR | (95% CI) | p | aOR | (95% CI) | p | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | ||||||||
| 553 | (35.7) | 998 | (64.3) | ||||||||
| Baseline characteristics | |||||||||||
| Maternal age >40 years | 42 | (7.6) | 40 | (4.0) | 2.0 | (1.3–3.0) | 0.003 | 1.8 | (1.1–3.2) | 0.028 | |
| Educational level > highschool | 300 * | (75.9) | 421 * | (65.6) | 1.7 | (1.3–2.2) | <0.001 | 1.5 | (1.1–2.0) | 0.017 | |
| Professionally active | 387 * | (87.4) | 652 * | (83.6) | 1.4 | (1.0–1.9) | 0.007 | 1.0 | (0.7–1.5) | 0.919 | |
| Primary language | |||||||||||
| French | 238 | (52.8) | 397 | (49.7) | 1.1 | (0.9–1.4) | 0.295 | ||||
| German | 159 * | (35.3) | 346 * | (43.3) | 0.7 | (0.6–0.9) | 0.005 | 0.7 | (0.5–0.9) | 0.015 | |
| Italian | 19 * | (4.2) | 12 * | (1.5) | 2.9 | (1.4–6.0) | 0.005 | 3.3 | (1.4–8.0) | 0.007 | |
| Any maternal co-morbidity | 58 | (10.5) | 93 | (9.3) | 1.1 | (0.8–1.6) | 0.457 | ||||
| Impact of the SARS-COV-2 pandemic | |||||||||||
| Tested positive for SARS-COV-2 (RT-PCR, serology and/or CT) | 9 | (1.6) | 3 | (0.3) | 5.5 | (1.5–20.4) | 0.011 | 3.3 | (0.8–13.7) | 0.095 | |
| Living with someone >65 years old | 10 | (1.8) | 8 | (0.8) | 2.3 | (0.8–6.7) | 0.076 | 2.0 | (0.7–6.1) | 0.094 | |
| Negative impact of the pandemic on | |||||||||||
| Pregnancy | 52 | (19.9) | 86 | (16.3) | 1.1 | (1.0–1.2) | 0.215 | ||||
| Life habits | 398 * | (72.8) | 652 * | (67.2) | 1.3 | (1.0–1.7) | 0.023 | 1.0 | (0.8–1.4) | 0.822 | |
| Work | 244 | (60.1) | 445 | (61.4) | 1.0 | (0.7–1.2) | 0.672 | ||||
| Symptoms of severe depression, anxiety or high stress | 68 | (12.3) | 102 | (10.2) | 1.2 | (0.9–1.7) | 0.211 | ||||
| Vaccination habits and beliefs | |||||||||||
| Vaccinated against Influenza last year | 197 * | (41.1) | 137 * | (16.1) | 3.6 | (2.8–4.7) | <0.001 | 2.1 | (1.5–2.8) | <0.001 | |
| Usually decline vaccination | 30 | (5.4) | 294 | (29.5) | 0.1 | (0.1–0.2) | <0.001 | 0.2 | (0.1–0.3) | <0.001 | |
| Fear of side effects related to vaccines | 51 | (9.2) | 114 | (11.4) | 0.8 | (0.6–1.1) | 0.179 | ||||
| Supplementary model including pregnancy-related variables (tested only in pregnant women, N = 515) | N | (%) | N | (%) | OR | (95%CI) | p | aOR | (95%CI) | p | |
| 153 | (29.7) | 362 | (60.3) | ||||||||
| Follow-up by an obstetrician | 144 | (94.1) | 324 | (89.5) | 1.9 | (0.9–4.0) | 0.101 | 3.6 | (1.2–11.2) | 0.027 | |
| Gestational age | |||||||||||
| T1 | 25 | (16.3) | 54 | (15.0) | 1.1 | (0.7–1.9) | 0.691 | ||||
| T2 | 47 | (30.7) | 147 | (40.7) | 0.6 | (0.4–1.0) | 0.033 | 0.6 | (0.4–0.9) | 0.015 | |
| T3 | 81 | (52.9) | 160 | (44.3) | 1.4 | (1.0–2.0) | 0.074 | 1.8 | (1.1–2.7) | 0.018 | |
| Fear of an adverse fetal outcome in case of infection | 75 | (49.0) | 200 | (55.3) | 0.9 | (0.8–1.0) | 0.196 | ||||
* Multiple imputations on missing values.
Having had the influenza vaccination in the past year was a positive predictor for SARS-CoV-2 vaccine acceptance (aOR 2.1 [1.5–2.8]). Women who usually declined influenza vaccination were less likely to be willing to get the SARS-CoV-2 vaccine (aOR 0.2 [0.1–0.3]).
When assessing the impact of the SARS-CoV-2 pandemic, none of the variables showed statistically significant influence on the willingness to get vaccinated. However, a trend toward COVID-19 vaccine willingness can be observed among women having a positive diagnosis of SARS-CoV-2 (aOR 3.3 [0.8–13.7] and living with someone older than 65 years old (aOR 2.0 [0.7–6.1]).
Among the pregnant participants, those who had an obstetrician following their pregnancy (aOR 3.6 [1.2–11.2]) and who were in their third trimester of pregnancy (aOR 1.8 [1.1–2.7]) were more likely to be willing to receive the SARS-CoV-2 vaccine. On the other hand, being in their second trimester of pregnancy was associated with a higher SARS-CoV-2 vaccination refusal (aOR 0.6 [0.4–0.9]).
4. Discussion
Our results demonstrate that in Switzerland, only one-third (35.7%; 553/1551) of pregnant and breastfeeding women that participated in the survey were willing to get a SARS-CoV-2 vaccine during the first wave of the pandemic if one had been available. The positive predictors for SARS-CoV-2 vaccine acceptance among all participants were an age older than 40 years, a higher educational level, speaking Italian as their primary language, and having been vaccinated against influenza in the previous year. On the other hand, speaking German and usually declining influenza vaccination were negative predictors. Regarding pregnant participants, having an obstetrician following their pregnancy and being in their third trimester of pregnancy were two positive factors associated with the willingness to be vaccinated against SARS-CoV-2, whereas being in their second trimester of pregnancy was a negative predictor. No association was found between maternal co-morbidities and the participants’ willingness to get vaccinated.
4.1. Interpretation
Our study shows that despite Switzerland being among SARS-CoV-2 high incidence countries during the first wave with a particularly negative impact on pregnancy and breastfeeding experience [24], it has a low rate of SARS-CoV-2 vaccination acceptance. The results from our survey of Swiss women were among the lowest when compared to a recent survey conducted in 16 countries that showed a SARS-CoV-2 vaccine acceptance rate among pregnant women of 52.0%, with responses varying substantially between countries (28.8–84.4%) [31]. An American cross-sectional survey showed a rate of 41% of SARS-CoV-2 vaccine acceptance among pregnant women [32]. The low percentage of Swiss pregnant women willing to get the SARS-CoV-2 vaccine that we observed is consistent with the rather low influenza and pertussis immunization rates in Switzerland previously mentioned [16]. We also identified variability in SARS-CoV-2 vaccine acceptance between different regions of Switzerland. This has already been observed with Swiss-German women being more reluctant to get their children vaccinated [33,34]. In contrast, the part of Switzerland most affected by SARS-CoV-2, the Italian part, seems to have a higher rate of vaccine acceptance than the other parts of Switzerland, although fewer Italian speaking women were included, and these results should be interpreted with caution.
In this Swiss sub-analysis, the proportion of breastfeeding women willing to be vaccinated was higher than that of pregnant women (38.6% vs. 29.7%). This difference was also found in all countries included in the European study of which these data are a part, with a difference of up to +25% for the UK [25]. These results support that “vaccine hesitancy” may be even more common during pregnancy, which may be related to an overall greater reluctance to use medicines during pregnancy.
When assessing factors influencing SARS-CoV-2 vaccine willingness among pregnant women, our results are consistent with another study identifying older age and higher educational level as positive predictors [31]. The same observations have been made for acceptance of the pertussis and influenza vaccines [23,31]. The positive correlation that we observed between SARS-CoV-2 vaccine willingness and having received the influenza vaccine during the previous season has also been found in a recent study evaluating pregnant women [32]. In addition, we identified that being in the second trimester of pregnancy might be a negative predictor for SARS-CoV-2 vaccine acceptance, suggesting a potential fear for induced fetal malformations. This is consistent with several studies identifying fear for any potential harmful side effects of the vaccine on their fetus or infant as well as concerns regarding safety and effectiveness as major reasons for vaccine reluctance [22,31,32]. Concerns about teratogenicity would be more likely in the first trimester, as second trimester exposures do not cause embryopathy. Here, patients who responded to the survey as being in the second trimester correspond to those who were in the first trimester at the time of the first wave, so our results may suggest that their fear of teratogenicity may be higher in early pregnancy and not necessarily in the second trimester. In contrast, we did not find an association between having experienced symptoms of severe depression, anxiety, or high stress in the weeks prior to the survey and the willingness to get the SARS-CoV-2 vaccine. This is not in line with a previous study where pregnant women with a history of major depressive disorder and moderate anxiety were significantly more likely to get influenza and pertussis vaccines [23]. However, at the time of the survey, no SARS-CoV-2 vaccine was yet available, and thus, no information was available regarding its safety or effectiveness in general and in the pregnant population, which may explain the reluctance of anxious or depressed women who may need safety information before accepting the vaccine. This might also have influenced participants who did not answer the question about SARS-CoV-2 vaccination acceptance, as the ambivalence toward this vaccine is still very strong. It is also interesting to note that while most participants showed acceptance of influenza vaccines, a much smaller percentage actually received it. This might question the access of Swiss breastfeeding and pregnant women to vaccines and how healthcare workers might play a role in it.
Our observations suggest that more than a specific reluctance toward the SARS-CoV-2 vaccine, it is one’s personal opinion on vaccination during pregnancy in general that might prevent Swiss pregnant and breastfeeding women from getting vaccinated. Hence, it is our hypothesis that SARS-CoV-2 and influenza or pertussis vaccines are avoided for similar reasons: mainly the lack of recommendation by healthcare professionals and the lack of compliance by pregnant women. Until the end of May 2021, Switzerland has made access to vaccines challenging, even for women that might want to be vaccinated, which could represent a barrier for vaccine acceptance. Furthermore, the ongoing debates over SARS-CoV-2 vaccines may have a negative influence on the willingness of pregnant women to become vaccinated. This emphasizes the need to improve access to vaccination for pregnant women as well as knowledge and acceptance of immunization during pregnancy among healthcare workers and pregnant/breastfeeding women.
4.2. Strengths and Limitations
In terms of temporality, our study explored the experience of Swiss pregnant women during the first wave of the SARS-CoV-2 pandemic. Our study included a large number of participants from different parts of Switzerland, was conducted in three official languages, and is the first to address the question of SARS-CoV-2 vaccine willingness in the country. Selection bias might have occurred as the proportion of participants who are professionally active and highly educated was higher than the general population of Swiss pregnant women [35,36]. This could have led to an increased vaccination acceptance rate, as highly educated women tend to have a higher acceptance of vaccination, which would mean that the vaccine willingness in the overall perinatal population might be even lower than that reported here. The survey was conducted online and, although most Swiss women have good access to the internet, those that rely more on online resources may have come across the online survey more often when looking for information about their pregnancy or breastfeeding. Women hospitalized or severely ill might not have had the opportunity to participate. This could have biased the association between SARS-CoV-2 exposure and the participants’ willingness to get vaccinated toward the null. In addition, as only 5% of women declared speaking another language in our survey, we might have an under representation of the immigrant population.
Another limitation might be the overrepresentation of French-speaking participants, which could be explained by the CHUV (Centre Hospitalier Universitaire Vaudois, university hospital of the largest French-speaking canton) leading the present study. Since some studies have shown an increased vaccination acceptance among the French-speaking part of Switzerland, this could have overestimated the rate of SARS-CoV-2 vaccine willingness in our study. Overestimation of SARS-CoV-2 vaccination acceptance could have also happened since a high percentage of participants were healthcare workers, more likely to be exposed to SARS-CoV-2 positive patients, and thus, more prone to being immunized.
Factors reported to be associated with SARS-CoV-2 vaccine willingness, considered in other studies, were not measured [31,32]. Those include socioeconomic status; perceived risk of SARS-CoV-2 (likelihood of infection, self or infant); opinion on the importance to public health to get a vaccine and for the majority of people to get vaccinated; compliance with preventive measures; monitoring of SARS-CoV-2 news and updates; trust and satisfaction with health authorities; as well as trust in science. Further surveys including those variables would be needed to better specify the factors influencing SARS-CoV-2 vaccination acceptance among Swiss pregnant women.
Finally, this survey was conducted at a time when no SARS-CoV-2 vaccine had yet been accepted by Swissmedic nor recommended for pregnant women. This could represent an important bias, since participants were asked if they would accept a potential vaccine without information about its efficiency and safety. Since this survey, the first randomized controlled trial of SARS-CoV-2 vaccination in pregnancy has been initiated [37]. Additionally, following the example of several other countries, the Swiss Society for Gynecology and Obstetrics (SSGO) along with the Federal Public Health Office (OFSP) has recommended, up until the end of May 2021, SARS-CoV-2 vaccination during the second and third trimester for pregnant women at high risk of developing complications or at high risk of exposure [38]. Recent studies also showed robust immune responses and efficient passage of antibodies to newborns after SARS-CoV-2 vaccination of pregnant women [39,40], unlike transplacental immunization through infected mothers, which seems to be less effective [41]. As new guidelines and more data on vaccinated pregnant women become available every day [42], willingness to become vaccinated might evolve, and new studies are urgently needed.
5. Conclusions
Our study suggests disappointing SARS-CoV-2 vaccine willingness among Swiss pregnant and breastfeeding women, emphasizing the need to identify and reduce barriers toward immunization. Inclusion of pregnant women in clinical trials, improving access to vaccines, and providing tailored information for pregnant and breastfeeding women, especially for those of younger age with a lower educational level, are crucially needed to protect them from SARS-CoV-2 and other viral threats ahead.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/v13071199/s1, Table S1: Raw data presented in Figure 2.
Author Contributions
M.C., H.N. and A.P. conceived and designed the study. M.S., U.W., D.B. and A.P. translated and promoted the study in Switzerland. S.S., G.F., E.G., V.L., A.P. and L.P. wrote the first version of the report and did the literature review. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by EC Research UZ/KU Leuven; S63966; 10 April 2020.
Informed Consent Statement
All participants provided online informed consent prior to survey initiation.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.FOPH Status Report, Switzerland and Liechtenstein. [(accessed on 1 May 2021)]; Available online: https://www.covid19.admin.ch/
- 2.Favre G., Pomar L., Baud D. Coronavirus Disease 2019 during Pregnancy: Do not Underestimate the Risk of Maternal Adverse Outcomes. Am. J. Obstet. Gynecol. MFM. 2020;2:100160. doi: 10.1016/j.ajogmf.2020.100160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jering K.S., Claggett B.L., Cunningham J.W., Rosenthal N., Vardeny O., Greene M.F., Solomon S.D. Clinical Characteristics and Outcomes of Hospitalized Women Giving Birth With and Without COVID-19. JAMA Intern. Med. 2021;181:714. doi: 10.1001/jamainternmed.2020.9241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lokken E.M., Taylor G.G., Huebner E.M., Vanderhoeven J., Hendrikson S., Coler B., Sheng J.S., Walker C.L., McCartney S.A., Kretzer N.M., et al. Higher SARS-CoV-2 Infection Rate in Pregnant Patients. Am. J. Obstet. Gynecol. 2021 doi: 10.1016/j.ajog.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zambrano L.D., Ellington S., Strid P., Galang R.R., Oduyebo T., Tong V.T., Woodworth K.R., Nahabedian J.F., III, Azziz-Baumgartner E., Gilboa S.M., et al. Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status-United States, January 22–October 3, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1641–1647. doi: 10.15585/mmwr.mm6944e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allotey J., Stallings E., Bonet M., Yap M., Chatterjee S., Kew T., Debenham L., Llavall A.C., Dixit A., Zhou D., et al. Clinical Manifestations, Risk Factors, and Maternal and Perinatal Outcomes of Coronavirus Disease 2019 in Pregnancy: Living Systematic Review and Meta-Analysis. BMJ. 2020;370:m3320. doi: 10.1136/bmj.m3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khalil A., Kalafat E., Benlioglu C., O’Brien P., Morris E., Draycott T., Thangaratinam S., Doare K.L., Heath P., Ladhani S., et al. SARS-CoV-2 Infection in Pregnancy: A Systematic Review and Meta-Analysis of Clinical Features and Pregnancy Outcomes. EClinicalMedicine. 2020;25:100446. doi: 10.1016/j.eclinm.2020.100446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martínez-Perez O., Vouga M., Melguizo S.C., Acebal L.F., Panchaud A., Muñoz-Chápuli M., Baud D. Association Between Mode of Delivery Among Pregnant Women With COVID-19 and Maternal and Neonatal Outcomes in Spain. JAMA. 2020;324:296–299. doi: 10.1001/jama.2020.10125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khalil A., Von Dadelszen P., Draycott T., Ugwumadu A., O’Brien P., Magee L. Change in the Incidence of Stillbirth and Preterm Delivery During the COVID-19 Pandemic. JAMA. 2020;324:705. doi: 10.1001/jama.2020.12746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hcini N., Maamri F., Picone O., Carod J.F., Lambert V., Mathieu M., Carles G., Pomar L. Maternal, Fetal and Neonatal Outcomes of Large Series of SARS-CoV-2 Positive Pregnancies in Peripartum Period: A Single-Center Prospective Comparative Study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021;257:11–18. doi: 10.1016/j.ejogrb.2020.11.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baud D., Greub G., Favre G., Gengler C., Jaton K., Dubruc E., Pomar L. Second-Trimester Miscarriage in a Pregnant Woman With SARS-CoV-2 Infection. JAMA. 2020;323:2198–2200. doi: 10.1001/jama.2020.7233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swissmedic [(accessed on 1 May 2021)]; Available online: https://www.swissmedic.ch/swissmedic/fr/home/news/coronavirus-covid-19/dritten-impfstoff-gegen-covid-19-erkrankung.html.
- 13.WHO Ten Threats. [(accessed on 1 May 2021)]; Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 14.Blanchard-Rohner G., Siegrist C.-A. Vaccination during Pregnancy to Protect Infants Against Influenza: Why and Why Not? Vaccine. 2011;29:7542–7550. doi: 10.1016/j.vaccine.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 15.Reuman P.D., Ayoub E.M., Small P.A. Effect of Passive Maternal Antibody on Influenza Illness in Children: A Prospective Study of Influenza A in Mother-Infant Pairs. Pediatr. Infect. Dis. J. 1987;6:398–403. doi: 10.1097/00006454-198704000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Blanchard-Rohner G., Eberhardt C. Review of Maternal Immunisation during Pregnancy: Focus on Pertussis and Influenza. Swiss Med. Wkly. 2017;147:w14526. doi: 10.4414/smw.2017.14526. [DOI] [PubMed] [Google Scholar]
- 17.Erb M.L., Erlanger T.E., Heininger U. Child-Parent Immunization Survey: How Well are National Immunization Recommendations Accepted by the Target Groups? Vaccine X. 2019;1:100013. doi: 10.1016/j.jvacx.2019.100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Healy C.M., Rench M.A., Montesinos D.P., Ng N., Swaim L.S. Knowledge and Attitiudes of Pregnant Women and their Providers Towards Recommendations for Immunization during Pregnancy. Vaccine. 2015;33:5445–5451. doi: 10.1016/j.vaccine.2015.08.028. [DOI] [PubMed] [Google Scholar]
- 19.Abu-Raya B., Maertens K., Edwards K.M., Omer S.B., Englund J.A., Flanagan K.L., Snape M.D., Amirthalingam G., Leuridan E., Van Damme P., et al. Global Perspectives on Immunization During Pregnancy and Priorities for Future Research and Development: An International Consensus Statement. Front. Immunol. 2020;11:1282. doi: 10.3389/fimmu.2020.01282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacDougall D.M., Halperin S.A. Improving Rates of Maternal Immunization: Challenges and Opportunities. Hum. Vaccines Immunother. 2016;12:857–865. doi: 10.1080/21645515.2015.1101524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilson R.J., Paterson P., Jarrett C., Larson H.J. Understanding Factors Influencing Vaccination Acceptance during Pregnancy Globally: A Literature Review. Vaccine. 2015;33:6420–6429. doi: 10.1016/j.vaccine.2015.08.046. [DOI] [PubMed] [Google Scholar]
- 22.Lutz C.S., Carr W., Cohn A., Rodriguez L. Understanding Barriers and Predictors of Maternal Immunization: Identifying gaps through an Exploratory Literature Review. Vaccine. 2018;36:7445–7455. doi: 10.1016/j.vaccine.2018.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mohammed H., Roberts C.T., Grzeskowiak L.E., Giles L., Leemaqz S., Dalton J., Dekker G., Marshall H.S. Psychosocial Determinants of Pertussis and Influenza Vaccine Uptake in Pregnant Women: A Prospective Study. Vaccine. 2020;38:3358–3368. doi: 10.1016/j.vaccine.2020.02.020. [DOI] [PubMed] [Google Scholar]
- 24.Ceulemans M., Foulon V., Ngo E., Panchaud A., Winterfeld U., Pomar L., Lambelet V., Cleary B., O’Shaughnessy F., Passier A., et al. Mental Health Status of Pregnant and Breastfeeding Women during the COVID-19 Pandemic-A Multinational Cross-Sectional Study. Acta Obstet. Gynecol. Scand. 2021 doi: 10.1111/aogs.14092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ceulemans M., Foulon V., Panchaud A., Winterfeld U., Pomar L., Lambelet V., Cleary B., O’Shaughnessy F., Passier A., Richardson J., et al. Vaccine Willingness and Impact of the COVID-19 Pandemic on Women’s Perinatal Experiences and Practices—A Multinational, Cross-Sectional Study Covering the First Wave of the Pandemic. Int. J. Environ. Res. Public Health. 2021;18:3367. doi: 10.3390/ijerph18073367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cox J.L., Holden J.M., Sagovsky R. Detection of Postnatal Depression. Development of the 10-Item Edinburgh Post-Natal Depression Scale. Br. J. Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 27.Bergink V., Kooistra L., Berg M.P.L.-V.D., Wijnen H., Bunevicius R., van Baar A., Pop V. Validation of the Edinburgh Depression Scale during Pregnancy. J. Psychosom. Res. 2011;70:385–389. doi: 10.1016/j.jpsychores.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 29.Cohen S., Kamarck T., Mermelstein R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983;24:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 30.Taylor J.M. Psychometric Analysis of the Ten-Item Perceived Stress Scale. Psychol. Assess. 2015;27:90–101. doi: 10.1037/a0038100. [DOI] [PubMed] [Google Scholar]
- 31.Skjefte M., Ngirbabul M., Akeju O., Escudero D., Hernandez-Diaz S., Wyszynski D.F., Wu J.W. COVID-19 Vaccine Acceptance among Pregnant Women and Mothers of Young Children: Results of a Survey in 16 Countries. Eur. J. Epidemiol. 2021;36:197–211. doi: 10.1007/s10654-021-00728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ashley N., Battarbee M.S.S., Varner M., Newes-Adeyi G., Daugherty M., Gyamfi-Bannerman C., Tita A., Vorwaller K., Vargas C., Subramaniam A., et al. Attitudes Toward COVID-19 Illness and COVID-19 Vaccination among Pregnant Women: A Cross-Sectional Multicenter Study during August–December 2020. [(accessed on 1 May 2021)]; doi: 10.1055/s-0041-1735878. Pre-print.2021. Available online: https://www.medrxiv.org/content/10.1101/2021.03.26.21254402v1. [DOI] [PubMed]
- 33.Lang P., Zimmermann H., Piller U., Steffen R., Hatz C. The Swiss National Vaccination Coverage Survey, 2005–2007. Public Health Rep. 2011;126:97–108. doi: 10.1177/00333549111260S212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Les Suisses Sceptiques à L'égard des Vaccins. [(accessed on 1 May 2021)]; Available online: https://www.pharmapro.ch/news/les-suisses-sceptiques-a-l-egard-des-vaccins-0222.htm.
- 35.Niveau de Formation de la Population-Données de L’indicateur. [(accessed on 1 May 2021)]; Available online: https://www.bfs.admin.ch/bfs/fr/home/statistiques/situation-economique-sociale-population/egalite-femmes-hommes/formation/niveau-formation.assetdetail.12527179.html.
- 36.Situation Professionnelle Selon le Sexe et la Situation Familiale. [(accessed on 1 May 2021)]; Available online: https://www.bfs.admin.ch/bfs/fr/home/statistiques/catalogues-banques-donnees/tableaux.assetdetail.13108456.html.
- 37.Pfizer-BioNTech Study to Evaluate the Safety, Tolerability, and Immunogenicity of SARS CoV-2 RNA Vaccine Candidate (BNT162b2) Against COVID-19 in Healthy Pregnant Women 18 Years of Age and Older. U.S in National Library of Medicine. [(accessed on 1 May 2021)];2021 Available online: https://clinicaltrials.gov/ct2/show/NCT04754594.
- 38.SGGG [(accessed on 1 May 2021)]; Available online: https://www.sggg.ch/fr/nouvelles/detail/1/infection-a-coronavirus-covid-19-et-grossesse/
- 39.Harvard Gazette [(accessed on 1 May 2021)]; Available online: https://news.harvard.edu/gazette/story/2021/03/study-shows-covid-19-vaccinated-mothers-pass-antibodies-to-newborns/
- 40.Gilbert P.D., Rudnick C.A. Newborn Antibodies to SARS-CoV-2 Detected in Cord Blood after Maternal Vaccination. medRxiv. 2021 doi: 10.1101/2021.02.03.21250579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Atyeo C., Pullen K.M., Bordt E.A., Fischinger S., Burke J., Michell A., Slein M.D., Loos C., Shook L.L., Boatin A.A., et al. Compromised SARS-CoV-2-Specific Placental Antibody Transfer. Cell. 2021;184:628–642.e10. doi: 10.1016/j.cell.2020.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shimabukuro T.T., Kim S.Y., Myers T.R., Moro P.L., Oduyebo T., Panagiotakopoulos L., Marquez P.L., Olson C.K., Liu R., Chang K.T., et al. Preliminary Findings of mRNA Covid-19 Vaccine Safety in Pregnant Persons. N. Engl. J. Med. 2021 doi: 10.1056/NEJMoa2104983. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author.