Abstract
Objectives
Adolescents and young adults with chronic medical conditions report higher distress and lower wellbeing than their physically healthy peers. Previous research suggests that self-compassion is negatively correlated with distress and positively correlated with wellbeing among healthy young people, as well as adults with chronic medical conditions. The current study aimed to extend these findings to a sample of adolescents and young adults with chronic medical conditions. This study also aimed to replicate findings observed in other populations by testing emotion regulation difficulties as a mediator of this relationship.
Methods
Adolescents and young adults aged 16 to 25 with chronic physical medical conditions (N = 107) completed an online survey including measures of self-compassion, emotion-regulation, wellbeing, and distress. Two mediation models were tested using the PROCESS macro in SPSS, with distress and wellbeing as outcomes.
Results
Self-compassion had a significant direct negative association with distress and a significant direct positive association with wellbeing. While self-compassion and emotion regulation difficulties explained a large amount of variance in both wellbeing, R2 = .31, p < .001, and distress, R2 = .46, p < .001, no support was found for the mediating role of emotion regulation difficulties between self-compassion and wellbeing. However, emotion regulation difficulties mediated the relationship between self-compassion and distress.
Conclusions
These findings suggest that an emotion regulation model of self-compassion may be applicable to young people with chronic medical conditions. Future research within this population may evaluate programs that develop self-compassion and emotion regulation skills.
Keywords: Self-compassion, Emotion regulation, Chronic illness, Adolescents, Young adults, Wellbeing
Chronic medical conditions (CMCs) are diseases which persist for at least three months and require ongoing medical treatment; for example, asthma, cancer, diabetes, and arthritis (Mokkink et al., 2008). While the experience of living with a CMC varies according to an individual’s diagnosis, common challenges include disruptions to daily functioning due to physical symptoms or treatment regimens, and worries about the future (Compas et al., 2012; Pinto-Gouveia et al., 2014). Population estimates in the USA suggest that 11 to 27% of adolescents experience at least one CMC (Van Cleave et al., 2010). This wide range of prevalence estimates reflects, at least in part, differences in which conditions are included under the CMC umbrella across studies and jurisdictions (Van Cleave et al., 2010).
In addition to physical health concerns, many young people with CMCs experience comorbid mental health conditions. While prevalence estimates vary depending on how mental health outcomes are measured, a recent systematic review of anxiety disorders in children and adolescents with chronic conditions reported that approximately 20 to 50% were affected (Cobham, et al., 2020). Further, a US population-based study found that young people with CMCs were 51% more likely to experience mental illness than their physically healthy peers (Adams et al., 2019). This may be due to activity limitations and the challenges of managing their illness alongside the developmental challenges of adolescence and young adulthood (Adams et al., 2019). For example, many adolescents place a high value on being able to conform with their peers (Kraaij & Garnefski, 2012). Illness-related tasks such as taking medication may be perceived as a point of difference from their peers, threatening adolescents’ ability to conform (Kraaij & Garnefski, 2012). Similarly, physical symptoms or the need to attend appointments may impact adolescents’ ability to participate in school or social activities (Adams et al., 2019). Accordingly, social consequences may be a cause of distress beyond illness management tasks themselves (Adams et al., 2019).
The challenges of managing a CMC may continue into young or “emerging” adulthood (Richter et al., 2015). This period describes the transition from adolescence to adulthood that occurs between 18 and 26 years of age (Tanner & Arnett, 2011). It is considered developmentally distinct from adulthood due the rapid and numerous changes in education, career, and relationships that young adults experience during this time (Tanner & Arnett, 2011). These changes present a unique challenge for young adults with CMCs, who may need to re-adjust the management of their condition to adapt to new environments, such as transitioning from university to the workforce (Richter et al., 2015). The demands of managing a CMC during both adolescence and young adulthood place young people aged 16 to 25 with CMCs in a position that is unique from both adults with CMCs, as well as their healthy peers (Garnefski et al., 2009). As a result, there is a need for targeted research with this population.
The majority of research regarding the psychological impacts of CMCs has used negative indicators of mental health such as distress (e.g., Kraaij & Garnefski, 2012; McCarthy et al., 2016). However, the psychological impact of CMCs may be usefully examined through the lens of positive psychology (Macaskill, 2016). The positive psychology movement is based on the philosophy that psychological treatment should support individuals to reach an optimal level of functioning (Seligman & Csikszentmihalyi, 2000). Positive psychology moves beyond a “deficit” model, focusing on factors rendering a person vulnerable to psychopathology, to a “strengths” model, which emphasizes both an individual’s inborn strengths and capacity for growth (Keyes et al., 2012). In the context of research, it is therefore important to identify correlates of wellbeing in addition to identifying correlates of distress (Macaskill, 2016). A positive psychology framework appears well-suited to research involving young people with CMCs, as it highlights the value of protective factors that promote wellbeing even in the presence of adversity (Keyes et al., 2012).
Self-compassion may be a potential target for interventions designed to promote wellbeing and protect against distress among young people with CMCs (e.g., Marsh et al., 2018; Zessin et al., 2015). Self-compassion is an adaptive way of relating to oneself with kindness in times of difficulty, similar to the warmth one would offer a close friend (Neff, 2003a). According to Neff (2003a), self-compassion includes three components: “Self-kindness” involves responding to failure and personal challenges with care and understanding; “mindfulness” involves maintaining an objective awareness of painful emotions without becoming overwhelmed by them; and “common humanity” involves recognizing that negative experiences are not a personal failure, but an inevitable part of being human. Self-compassionate individuals may experience less distress in adverse circumstances, particularly those over which they have minimal control (Neff, 2009). Accordingly, self-compassion appears to be relevant to the experience of CMCs, whereby individuals may face challenges that are ongoing and unpredictable (Brion et al., 2014).
Neff and Germer (2013) noted that mindfulness in the context of self-compassion is narrower than mindfulness as it is generally conceptualized. Mindfulness is traditionally defined as paying attention to present thoughts, feelings, and sensations with a mindset of openness, curiosity, and acceptance (Bishop et al., 2004). These internal experiences may be positive, neutral, or negative (Bishop et al., 2004). In contrast, the mindfulness component of self-compassion focuses on maintaining a balanced awareness of negative stimuli related to the experience of suffering (Neff & Germer, 2013). It also emphasizes an acceptance of the “self” as the person who is experiencing the negative thoughts, feelings, or sensations, beyond simply attending to the experience itself (Neff & Germer, 2013). This mindful focus on the self is closely linked with common humanity and self-kindness: by being aware that they are experiencing suffering, an individual is able to respond with gentleness and reassure themselves that such hardships are also experienced by others (Neff & Germer, 2013).
An alternative definition of self-compassion has been proposed by Gilbert (2014), who described compassion as arising from an evolved affect regulation system (the “soothing system”). Individuals are motivated to seek affiliation with others and, as a result, experience feelings of contentment (Gilbert & Procter, 2006). Activation of the soothing system is associated with down-regulation of the sympathetic nervous system, stimulation of the parasympathetic nervous system, and the release of oxytocin (Gilbert & Procter, 2006). Gilbert (2014) suggested that these physiological responses to comfort from others also occur when compassion is directed towards the self. The theories of Neff (2003a) and Gilbert (2014) can be considered complementary, as Neff (2003a) described components of self-compassion that can be accessed at a conscious, intentional level, while Gilbert (2014) accounted for the autonomic processes underlying the compassion response.
Most self-compassion research has been conducted using Neff’s (2003b) Self-Compassion Scale. Extensive literature documents the association between self-compassion and psychopathology, with meta-analyses using general community samples (Macbeth & Gumley, 2012) and adolescent samples (Marsh et al., 2018) reporting strong negative relationships. Similar findings have been obtained in samples of adults with CMCs, such as human immunodeficiency virus (Brion et al., 2014), epilepsy (Clegg et al., 2019), diabetes (Kane et al., 2018), inflammatory bowel disease and arthritis (Sirois et al., 2015), and cancer (Pinto-Gouveia et al., 2014). In addition, a meta-analysis conducted by Zessin et al. (2015) found a significant positive association between self-compassion and wellbeing across general adult samples. In light of these findings, there is a need to understand the mechanisms underlying the relationship between self-compassion, wellbeing, and distress (Inwood & Ferrari, 2018). Emotion regulation capacities have been proposed as one such mechanism (Diedrich et al., 2014; Finlay-Jones, 2017; Krieger et al., 2013).
Emotion regulation describes the processes individuals use to modify the intensity, duration, and expression of emotion (Thompson, 1994). While there are many taxonomies of emotion regulation, according to Gratz and Roemer (2004), emotion regulation involves four skills: identifying and understanding emotions; accepting emotions instead of avoiding them; applying strategies in constructive ways to achieve a goal; and tailoring the use of emotion regulation strategies in response to situational demands. Following this, emotion regulation difficulties can be defined as the inability to utilize one or more of these skills (Gratz & Roemer, 2004). Emotion regulation skills are considered fundamental to healthy development, while emotion regulation difficulties are often highlighted as a transdiagnostic mechanism underlying psychopathology (Aldao et al., 2010).
Multiple studies have found evidence of a positive association between emotion regulation difficulties and distress among individuals with CMCs, such as arthritis (Garnefski et al., 2009) and inflammatory bowel disease (Trindade et al., 2017). Large, positive correlations have been observed between depression and the use of specific emotion regulation styles such as rumination and catastrophizing in a sample of adolescents with CMCs (Kraaij & Garnefski, 2012). This suggests that these strategies may be maladaptive for this population (Kraaij & Garnefski, 2012). Emotion regulation difficulties have also been examined in relation to wellbeing, with a meta-analysis of general community samples demonstrating that emotion regulation strategies such as cognitive reappraisal are positively associated with wellbeing, while the inverse is true for emotion regulation strategies such as suppression (Hu et al., 2014). However, these correlations were medium and small, respectively, suggesting that although present, the association between emotion regulation and wellbeing is not as strong as the association between emotion regulation and distress.
Recent studies have proposed an emotion regulation model of self-compassion (e.g., Finlay-Jones et al., 2015; Raes, 2010). According to this model, self-compassionate individuals experience greater wellbeing and less distress because a self-compassionate mindset facilitates the use of effective emotion regulation skills (Finlay-Jones, 2017). For example, the mindfulness component of self-compassion may facilitate emotional awareness, which has been identified as a necessary precursor of emotion regulation (Subic-Wrana et al., 2014). By exercising self-kindness, individuals may experience less negative affect and be less likely to engage in emotional suppression, as emotions are perceived as less threatening (Allen & Leary, 2010; Bluth et al., 2016a, b). Further, in recognizing that the experience of suffering is common to all people, individuals may feel less alienated by the experience of hardship and seek out social support (Allen & Leary, 2010). In addition, Gilbert (2014) described that the “threat system” is associated with activation of the limbic system and suppression of activity in the prefrontal cortex. Activation of the threat system may therefore suppress executive functions such as cognitive reappraisal (Beauchaine, 2015). By activating the soothing system through exercising self-compassion, resources may be made available for engaging in explicit cognitive emotion regulation strategies (Svendsen et al., 2016).
This thinking is supported by a growing body of empirical evidence (Inwood & Ferrari, 2018). Inwood and Ferrari’s (2018) systematic review found that emotion regulation difficulties mediated the relationship between self-compassion and symptoms of psychopathology, including post-traumatic stress disorder (Barlow et al., 2017); stress (Finlay-Jones et al., 2015); and depression (Diedrich et al., 2017). Specifically, rumination (Johnson & O’Brien, 2013) and cognitive and behavioral avoidance (Krieger et al., 2013) have been found to mediate the relationship between self-compassion and symptoms of depression. Rumination has also been identified as a mediator between self-compassion, depression, and anxiety in a young adult sample (Raes, 2010). However, this relationship has not yet been explored among young people with CMCs or with wellbeing as an outcome.
The aim of this study was to investigate the relationship between self-compassion, emotion regulation, wellbeing, and distress in a group of young people with CMCs. Specifically, we explored whether emotion regulation difficulties mediate the relationship between self-compassion and wellbeing and self-compassion and distress. Wellbeing and distress were examined in two separate models. In model one, it was hypothesized that, after controlling for gender and symptom severity: (1) there would be a significant direct negative association between self-compassion and emotion regulation difficulties, and there would be a significant negative association between self-compassion and distress, both (2) directly, and (3) indirectly via emotion regulation difficulties. In model two, it was hypothesized that, after controlling for gender and symptom severity: (4) there would be a significant direct negative association between self-compassion and emotion regulation difficulties, and there would be a significant positive association between self-compassion and wellbeing, both (5) directly, and (6) indirectly via emotion regulation difficulties.
Method
Participants
The sample consisted of 107 (21 male, 81 female, 5 transgender or gender-diverse) adolescents and young adults with a mean age of 21.27 (SD = 2.59). To meet inclusion criteria, participants needed to live in Australia, be aged 16–25, and self-identify as having a chronic physical medical condition. The most commonly reported CMCs were asthma (n = 33; 30.8%), chronic pain (n = 29; 27.1%), chronic fatigue syndrome/myalgic encephalomyelitis (n = 27; 25.2%), and allergies (n = 26; 24.3%), with 45.8% of participants reporting two or more CMCs. A complete list of CMCs reported by participants and the prevalence of these conditions in the sample is reported in Table 1. Table 2 displays participant characteristics including location, duration of illness, and the number of chronic medical conditions and mental health conditions reported per participant.
Table 1.
Frequency of chronic medical conditions
| Diagnosis | n | % |
|---|---|---|
| Asthma | 33 | 30.8 |
| Chronic pain | 29 | 27.1 |
| Chronic fatigue syndrome | 27 | 25.2 |
| Allergies | 26 | 24.3 |
| Chronic skin conditions | 9 | 8.4 |
| Arthritis | 7 | 6.5 |
| Inflammatory bowel disease | 7 | 6.5 |
| Cancer | 6 | 5.6 |
| Endometriosis | 6 | 5.6 |
| Alopecia | 5 | 4.7 |
| Burns | 5 | 4.7 |
| Ehlers-Danlos syndrome | 4 | 3.7 |
| Epilepsy | 4 | 3.7 |
| Postural orthostatic tachycardia syndrome | 4 | 3.7 |
| Type 1 diabetes | 4 | 3.7 |
| Cystic fibrosis | 3 | 2.8 |
| Cerebral palsy | 2 | 1.9 |
| Coeliac disease | 2 | 1.9 |
| Fibromyalgia | 2 | 1.9 |
| Joint hypermobility | 2 | 1.9 |
| Multiple sclerosis | 2 | 1.9 |
| Nemaline myopathy | 2 | 1.9 |
| Axial spondylitis | 1 | 0.9 |
| Bronchiectasis | 1 | 0.9 |
| Cystic fibrosis-related diabetes | 1 | 0.9 |
| Chiari malformation | 1 | 0.9 |
| Congenital heart disease | 1 | 0.9 |
| Connective tissue disorder | 1 | 0.9 |
| Functional neurological disorder | 1 | 0.9 |
| Gastroesophageal reflux disease | 1 | 0.9 |
| Hip dysplasia | 1 | 0.9 |
| Hyper IgE syndrome | 1 | 0.9 |
| Klippel-Feil syndrome | 1 | 0.9 |
| Migraine | 1 | 0.9 |
| Polycystic ovarian syndrome | 1 | 0.9 |
| Sickle cell disease | 1 | 0.9 |
| Supraventricular tachycardia | 1 | 0.9 |
| Type 2 diabetes | 1 | 0.9 |
Participants could select more than one condition
Table 2.
Medical, mental health, and geographic characteristics of participants
| Characteristic | n | % | ||
|---|---|---|---|---|
| Number of chronic medical conditionsa | ||||
| 1 | 58 | 54.2 | ||
| 2 | 20 | 18.7 | ||
| 3 | 13 | 12.1 | ||
| 4 | 12 | 11.2 | ||
| 5 | 3 | 2.8 | ||
| 7 | 1 | 0.9 | ||
| Number of mental health conditionsb | ||||
| 0 | 52 | 48.6 | ||
| 1 | 17 | 15.9 | ||
| 2 | 15 | 14.0 | ||
| 3 | 18 | 16.8 | ||
| 4 | 2 | 1.9 | ||
| 5 | 2 | 1.9 | ||
| 6 | 1 | 0.9 | ||
| Time since diagnosisc | ||||
| Less than 1 month | 1 | 0.9 | ||
| 1–3 months | 2 | 1.9 | ||
| 4–6 months | 3 | 2.8 | ||
| 7–11 months | 4 | 3.7 | ||
| 1–2 years | 12 | 11.2 | ||
| 3–4 years | 26 | 24.3 | ||
| More than 5 years | 58 | 54.2 | ||
| Not specified | 1 | 0.9 | ||
| Location | ||||
| Western Australia | 31 | 29.0 | ||
| Victoria | 28 | 26.2 | ||
| New South Wales | 22 | 20.6 | ||
| Queensland | 6 | 5.6 | ||
| South Australia | 5 | 4.7 | ||
| Australian Capital Territory | 5 | 4.7 | ||
| Tasmania | 3 | 2.8 | ||
| Not specified | 7 | 6.5 | ||
N = 107
aNumber of chronic medical conditions reported per participant
bNumber of mental health conditions reported per participant
cFor illness of longest duration reported by each participant
Procedure
Data were collected using an online survey hosted by Qualtrics (Qualtrics, Provo, UT). Participants were recruited via organizations representing young people with CMCs. Promotional materials containing the survey link were distributed through emailing lists, online newsletters, and social media posts. Participants followed the link directly to the survey. They were required to check a box indicating that they understood the information sheet and consented to participate in order to proceed. The survey took approximately 20–30 min to complete. Participation could be terminated at any time by exiting the survey. A $10 voucher for Big W or JB Hi Fi was offered to each participant upon completion. Data were collected between January and September 2020.
Measures
Demographic questions included age, gender, location, chronic medical diagnosis, mental health diagnosis, and time since diagnosis.
Self-Compassion Scale–Short Form
The Self-Compassion Scale–Short Form (SCS-SF; Raes et al., 2011) is a 12-item abbreviated form of Neff’s (2003b) 26-item Self-Compassion Scale (SCS). Participants responded to items such as, “When I’m feeling down I tend to obsess and fixate on everything that’s wrong” on a Likert scale ranging from 1 (almost never) to 5 (almost always). Some items were negatively worded and required reverse coding. The SCS-SF contains six subscales, with self-kindness, common humanity, and mindfulness reflecting compassionate self-responding and self-judgment, isolation, and over-identification reflecting uncompassionate self-responding. Responses from all items were summed and averaged to give a total mean self-compassion score (Raes et al., 2011). Possible scores range from 1 to 5, with a high score indicating that an individual is highly self-compassionate. Internal consistency in this sample was high, α = 0.91.
Difficulties in Emotion Regulation Scale–Short Form
The Difficulties in Emotion Regulation Scale–Short Form (DERS-SF; Kaufman et al., 2016) is an 18-item abbreviated form of Gratz and Roemer’s (2004) Difficulties in Emotion Regulation Scale. Participants responded to items such as, “I have difficulty making sense out of my feelings” on a Likert scale ranging from 1 (almost never) to 5 (almost always). The DERS-SF has six subscales labelled strategies, non-acceptance, impulse, goals, awareness, and clarity. The use of a total score reflecting global emotion regulation difficulties has been validated in multiple studies (e.g., Hallion et al., 2018). Three items required reverse coding. Responses from all items were summed to give a total score. Possible scores range from 18 to 90, with high scores indicating substantial emotion regulation difficulties. Internal consistency in this sample was high, α = 0.92.
World Health Organization Wellbeing Index
The World Health Organization Wellbeing Index (WHO-5; Bech, 1996) is a five-item unidimensional indicator of general wellbeing. Participants considered their feelings over the last 2 weeks and responded to items such as, “I have felt active and vigorous” on a Likert scale ranging from 5 (all of the time) to 0 (at no time). Scores were multiplied by four to give a total score out of 100. Possible scores range from zero, indicating the poorest wellbeing imaginable, to 100, indicating the best wellbeing imaginable. Internal consistency in this sample was high, α = 0.87.
Kessler Psychological Distress Scale
The Kessler Psychological Distress Scale (K-10; Kessler et al., 2002) is a 10-item measure of non-specific psychological distress, with items covering several domains including depression, anxiety, fatigue, and physical symptoms of arousal (Andrews & Slade, 2001). Participants were asked, “In the past 30 days how often…” and responded to items such as “did you feel nervous?” on a five-point Likert scale ranging from 5 (all of the time) to 1 (none of the time). Possible scores range from 10, indicating no distress, to 50, indicating severe distress. Internal consistency in this sample was high, α = 0.90.
Symptom Severity
Symptom severity was measured using a single item, “On a scale of 1–10, how severe would you say your current physical symptoms are?” Participants responded on a 10-point Likert scale ranging from 1 (not severe at all) to 10 (extremely severe). Lu et al. (2020) found that participants’ scores on a single item measuring headache severity were highly correlated with their total score on a six-item measure, r = 0.08, providing support for the validity of single-item measures. The use of a general, non-symptom-specific question was necessitated by the inclusion of many different diagnoses in the present study.
Results
Preliminary Analyses
As there is a lack of consensus in the literature surrounding the factor structure of the SCS-SF (e.g., Neff et al., 2018) and DERS-SF (e.g., Moreira et al., 2020), factor analyses were conducted to determine the appropriateness of using a total score. Principal axis factoring with Promax rotation supported a single-factor structure for the SCS-SF. A single-factor model using principal axis factoring with Promax rotation produced high factor loadings for all items of the DERS-SF except 1, 4, and 6, which form the “awareness” subscale. The literature commonly reports low reliability and poor factor loadings for the awareness subscale in both adolescent (e.g., Neumann et al., 2010) and young adult (e.g., Bardeen et al., 2012; Tull et al., 2007) populations, to the extent that several papers recommended that the subscale is excluded from the total score (e.g., Hallion et al., 2018; Moreira et al., 2020). Consistent with previous research, items 1, 4, and 6 in the present study had low initial and extracted communalities, and internal reliability of the total scale was higher without these items. These items were removed, and a second analysis using principal axis factoring with Promax rotation supported a single-factor structure. As such, subsequent analyses were conducted using a total score comprised of the 15 retained items.
Pearson’s correlations between each measure are reported in Table 3, alongside the mean, standard deviation, and Cronbach’s alpha.
Table 3.
Bivariate correlations, means, standard deviations, and Cronbach’s alpha for symptom severity and measures in mediation models
| 1 | 2 | 3 | 4 | M (SD) | α | |
|---|---|---|---|---|---|---|
| Symptom severity | − .10 | .20* | − .23* | .24* | 5.66 (2.02) | |
| 1. SCS-SFa | - | 2.71 (0.80) | .91 | |||
| 2. DERS-SFb | − .70** | - | 40.54 (12.04) | .92 | ||
| 3. WHO-5c | .46** | − .47** | - | 39.66 (20.75) | .87 | |
| 4. K10d | − .61** | .62** | − .74** | - | 27.04 (8.18) | .90 |
N = 107
aSelf-Compassion Scale–Short Form (Raes et al., 2011)
bDifficulties in Emotion Regulation Scale–Short Form (Kaufman et al., 2016)
cWorld Health Organization Wellbeing Index (Bech, 1996)
dKessler Psychological Distress Scale (Kessler et al., 2002)
*Correlation is significant at the .05 level (2-tailed)
**Correlation is significant at the .01 level (2-tailed)
Two simple mediation models were analyzed using the PROCESS macro (Hayes, 2013) for SPSS (IBM Corp., 2019). PROCESS conducts path analysis using ordinary least squares regression (Hayes, 2013). Model 4 was selected with a 95% confidence interval and 10, 000 bias-corrected bootstrap samples. Gender and symptom severity were included as control variables in both models.
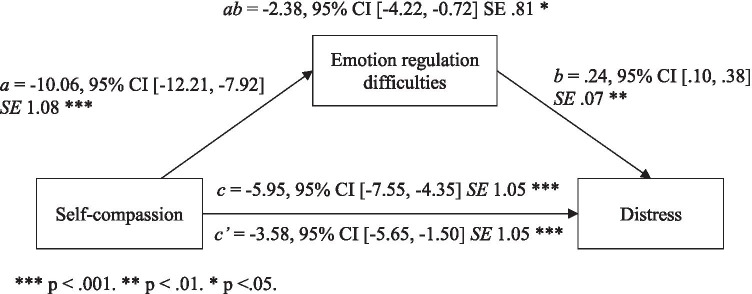
Model One: Self-Compassion, Emotion Regulation, and Distress
Unstandardized (B) regression coefficients, 95% CI, and standard error estimates for model one are presented in Fig. 1. Self-compassion and emotion regulation difficulties in combination accounted for a statistically significant proportion of unique variance in distress, R2 = 0.46, F(4, 101) = 21.83, p < 0.001. This is a large effect according to Cohen’s (1988) conventions (f2 = 0.85). Hypothesis one was supported, with self-compassion predicting a significant proportion of unique variance in emotion regulation difficulties, a = − 10.06, LLCI/ULCI 0, p < 0.001. Emotion regulation difficulties also predicted a significant proportion of unique variance in distress, b = 0.24, LLCI/ULCI 0, p < 0.05. Hypothesis two was supported, with evidence of a significant direct negative association between self-compassion and distress, c’ = − 3.58, LLCI/ULCI 0, p < 0.01. Hypothesis three was also supported, with the indirect effect of self-compassion via emotion regulation difficulties predicting a significant proportion of unique variance in distress, ab = − 2.38, LLCI/ULCI 0, p < 0.05. The total effect of the model was also significant, c = − 5.95, LLCI/ULCI 0, p < 0.001. Effect size was determined by calculating the ratio of indirect effect to total effect (Hayes, 2013). The indirect pathway accounted for 40% of the total effect of self-compassion on distress.
Fig. 1.
Statistical diagram of mediation model one: distress (K10) as outcome
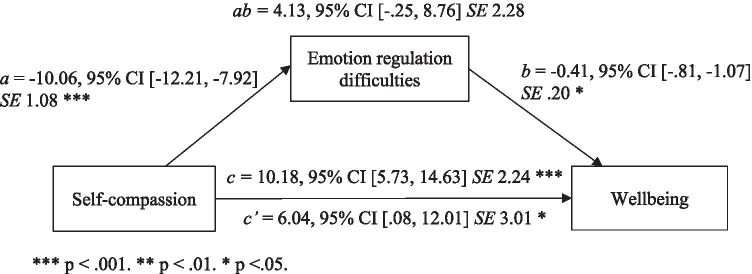
Model Two: Self-Compassion, Emotion Regulation, and Wellbeing
Unstandardized (B) regression coefficients, 95% CI, and standard error estimates for model two are presented in Fig. 2. Self-compassion and emotion regulation difficulties in combination accounted for a statistically significant proportion of unique variance in wellbeing, R2 = 0.31, F(4, 101) = 11.47, p < 0.001. This is a large effect according to Cohen’s (1988) conventions (f2 = 0.45). Hypothesis four was supported, with self-compassion predicting a significant proportion of unique variance in emotion regulation difficulties, a = − 10.06, LLCI/ULCI 0, p < 0.001. Hypothesis five was supported, as the direct path between self-compassion and wellbeing was significant, c’ = 6.04, LLCI/ULCI 0, p < 0.05. Emotion regulation difficulties also predicted a significant proportion of unique variance in wellbeing, b = − 0.41, LLCI/ULCI 0, p < 0.05. Hypothesis six was not supported as the unstandardized coefficient for the indirect effect was non-significant, ab = 4.13, LLCI/ULCI 0, p > 05.
Fig. 2.
Statistical diagram of mediation model two: wellbeing (WHO-5) as outcome
Discussion
The aim of the current study was to examine the relationship of self-compassion to distress and wellbeing. A further aim was to extend findings of an emotion regulation model of self-compassion to a population of young people with CMCs. The participants’ average distress rating is considered “high” against population norms (Australian Bureau of Statistics, 2012), as well as in comparison to samples of young people with CMCs, such as adolescents and young adults with cancer, who reported a mean K10 score of 19.2 (McCarthy et al., 2016). Participants also reported wellbeing considerably lower than the mean WHO-5 score of 63.38 observed in a sample of adolescents with type 1 diabetes (de Wit et al., 2007). The high distress and low wellbeing reported by this sample highlights the importance of identifying correlates of distress and wellbeing for adolescents and young adults with CMCs.
Self-Compassion, Emotion Regulation Difficulties, and Distress
Self-compassion and emotion regulation difficulties together accounted for nearly half of the unique variance in distress. This is consistent with findings from a hierarchical multiple regression that self-compassion and emotion regulation, alongside age, gender, insulin use, and symptom severity, predicted 38.5% of the variance in diabetes-related distress in adults with type 2 diabetes (Kane et al., 2018).
There was a significant direct negative association between self-compassion and emotion regulation difficulties. This was expected in light of previous research linking self-compassion and emotion regulation (e.g., Bluth et al., 2016a, b; Raes, 2010). There was a significant direct positive association between emotion regulation difficulties and distress. This is consistent with previous literature suggesting that adolescents (Garnefski et al., 2009; Kraaij & Garnefski, 2012) and adults (Trindade et al., 2017) with CMCs who experience high levels of emotion dysregulation experience greater distress. As predicted, there was a significant direct negative association between self-compassion and distress. This is consistent with findings from meta-analyses using general community samples (Macbeth & Gumley, 2012) and adolescent samples (Marsh et al., 2018) which suggest that individuals high in self-compassion are likely to experience less distress than individuals with an uncompassionate style of self-responding.
Findings from the current study further contribute to an understanding of the mechanism through which self-compassion is related to distress. As has been observed in previous samples of psychologists (Finlay-Jones et al., 2015), adults with depression (Diedrich et al., 2017; Krieger et al., 2013), and young adults (Barlow et al., 2017; Johnson & O’Brien, 2013; Raes, 2010), a significant negative indirect association was found between self-compassion and distress, operating via emotion regulation difficulties. This suggests that emotion regulation difficulties mediate the relationship between self-compassion and distress. Of note, this pathway accounted for 40% of the total effect of self-compassion on distress. This large effect is comparable to that observed in a sample of adults with depression, where the indirect pathway between self-compassion and depression symptoms via emotion regulation accounted for 46.63% of the total effect (Diedrich et al., 2017). These findings further strengthen support for an emotion regulation model of self-compassion (e.g., Finlay-Jones, 2017; Finlay-Jones et al., 2015), whereby self-compassion is related to lower distress by facilitating the use of adaptive emotion regulation strategies. The contribution of this study is to extend these findings to adolescents and young adults with CMCs.
Self-Compassion, Emotion Regulation Difficulties, and Wellbeing
The current study also aimed to explore whether a meaningful relationship exists between self-compassion, emotion regulation, and wellbeing. Overall, the model accounted for nearly a third of the unique variance in wellbeing, suggesting that self-compassion and emotion regulation difficulties are relevant to the experience of positive psychological outcomes in young people with CMCs. As expected, there was a significant positive direct effect of self-compassion on wellbeing, suggesting that individuals who are self-compassionate are more likely to experience high wellbeing than individuals who are less self-compassionate. This was expected, given the positive correlations previously observed in a meta-analysis using general community samples (Zessin et al., 2015).
A significant direct negative association was observed between emotion regulation difficulties and wellbeing, confirming our expectation that individuals with greater emotion regulation difficulties would experience lower wellbeing. However, no support was found for an indirect effect of self-compassion on wellbeing via emotion regulation difficulties. No previous research has investigated this relationship using wellbeing as an outcome. However, literature suggests that the bivariate correlations between self-compassion and wellbeing (e.g., Zessin et al., 2015), and emotion regulation difficulties and wellbeing (e.g., Hu et al., 2014), are smaller than their respective correlations with distress (e.g., Kraaij & Garnefski, 2012; Marsh et al., 2018). Given these findings, it is possible that an indirect effect exists but is smaller than the indirect effect observed in the distress model. The current study may have been underpowered to detect an effect of this size.
Additional explanations may relate to the measure of wellbeing that was used. According to Diener (1984), subjective wellbeing consists of affective wellbeing, such as the experience of positive emotions, and cognitive wellbeing, such as experiencing a state of satisfaction with life. It is logical that emotion regulation difficulties are most closely related to affective wellbeing. With only two items, “I have felt cheerful and in good spirits” and “I have felt calm and relaxed,” that may relate to affective wellbeing, it is possible that the WHO-5 (Bech, 1996), was not sensitive enough to detect this relationship.
Alternatively, emotion regulation difficulties may not act as a mediator between self-compassion and wellbeing. Emotion regulation may be more closely related to distress, due to its role in modulating the intensity and duration of negative affect (Thompson, 1994). The presence of decreased negative affect relative to positive affect may, over time, facilitate increased wellbeing (Diener, 1984). As such, the pathway between self-compassion and wellbeing may be more complex than what the simple mediation model used in the current study can explain. This possibility is consistent with the absence of an indirect effect, but presence of significant direct effects and significant unique variance explained by the model. Other variables within positive psychology such as hope (e.g., Yang et al., 2016) and self-efficacy (e.g., Sirois, 2015) may also be involved in the relationship between self-compassion and wellbeing in this population.
Theoretical Implications
These findings provide support for an emotion regulation model of self-compassion and its application among young people with CMCs. This is encouraging, as self-compassion and emotion regulation may meaningfully relate to the daily challenges experienced by this population. For example, Neff (2003a) described how self-compassion may buffer against negative affect when receiving negative self-relevant information. Young people with CMCs may frequently encounter negative self-relevant information related to their health status. For example, a young person with type 1 diabetes required to test their blood glucose several times a day may frequently receive readings outside their target range.
While the direction and causal nature of this relationship cannot be concluded from the current study, the hypothetical interaction of self-compassion, emotion regulation difficulties, and distress in a chronic illness population can be illustrated using the above situation as an example. In responding to this blood glucose reading with self-kindness, an individual may acknowledge that such experiences are stressful and reassure themselves that it is unrealistic to expect perfect readings every time. They may then find it easier to engage in positive emotion regulation strategies such as cognitive re-framing, reminding themselves that they have a plan to address such occurrences. From the perspective of common humanity, they may recognize that they are not alone in struggling with their illness management and reach out to sources of social support such as friends and family members.
Supporting both the self-compassion and emotion regulation skills of this population may be a beneficial focus for future intervention. Increases in self-compassion and wellbeing, and decreases in distress, have been observed following self-compassion training in healthy adolescent (Bluth et al., 2016a, b) and adult chronic illness populations (Friis et al., 2016). A meta-analysis by Kılıç et al. (2020) found a medium to large effect size of self-compassion interventions across adult samples with CMCs. Given these findings, it is promising that the efficacy of an online self-compassion program for young people with CMCs is under investigation (Finlay-Jones et al., 2020).
Limitations and Future Research Directions
Several considerations should be made when interpreting the findings of this study. Firstly, data was collected during the COVID-19 pandemic. Research suggests that young people with CMCs experienced decreased wellbeing during this period, potentially related to high susceptibility to the virus and uncertainty surrounding treatment delivery (Košir et al., 2020). This may be an alternative explanation for the low wellbeing and high distress observed in this sample. An additional consideration is that medical diagnoses were self-reported by participants. To increase sampling rigor, future research may involve medical practitioners in the recruitment phase. The use of a non-specific measure of symptom severity, while facilitating the inclusion of young people with a range of CMCs, may have decreased its validity as a control variable. An individual’s perception of symptom severity may be influenced by the nature of their condition and whether this report reflected their physical symptoms as a whole or a specific primary complaint. Future research may utilize a measure with multiple items, more specific guidance for respondents, or involve medical practitioners in the assessment of symptom severity. Further, the use of several self-report measures in this study introduced the possibility of common methods bias (Mackenzie & Podsakoff, 2012). This bias describes the artificial inflation of correlations between constructs completed by the same respondent in a single survey, due to priming effects, social desirability, and personal response styles (Mackenzie & Podsakoff, 2012). Accordingly, it should be noted that the true correlations between the variables in this study may be lower than those observed using this data collection method.
A limitation of this study is that reduced item fit of the awareness subscale of the DERS-SF necessitated the deletion of these items. This limits our ability to link the mindfulness component of self-compassion with increased emotional awareness, as proposed in our theoretical model. Further, we remain unable to provide support for the argument that emotional awareness is a mechanism through which self-compassion is related to distress. Reduced item fit of the awareness subscale may be due to methodological limitations associated with negatively worded items, as it is the only subscale that requires reverse coding (Moreira et al., 2020). Alternatively, it has been suggested that awareness is not assessing the same underlying construct as the other subscales (Bardeen et al., 2012). This is consistent with findings from Subic-Wrana et al. (2014) that awareness is a precursor to emotion regulation, rather than an emotion regulation strategy (Bardeen et al., 2012). Future research may use an alternative measure of emotional awareness such as the Levels of Emotional Awareness Subscale (Lane et al., 1990), alongside the DERS-SF, to explore the relationship between the mindfulness component of self-compassion, emotional awareness, and emotion regulation difficulties.
As the research design is correlational, it is not possible to infer causation from these findings. Randomized control trials implementing self-compassion programs for young people with CMCs are therefore required. It is also recommended that future intervention studies include emotion regulation difficulties as an outcome measure to further evaluate its role as a mediator between self-compassion, wellbeing, and distress. In addition, future studies investigating emotion regulation may benefit from using a wellbeing measure such as the Positive and Negative Affect Schedule (Watson et al., 1988), which may be more closely aligned with the affective dimension of subjective wellbeing. Finally, replication with a larger sample could investigate whether an indirect effect between self-compassion and wellbeing was not detected due to insufficient power. Replication following the COVID-19 pandemic is also required to evaluate the extent to which the findings can be generalized to other samples of young people with CMCs.
Author Contribution
KP designed and executed the study, assisted with recruitment of participants, conducted data analysis, and wrote the paper. CS collaborated with the design of the study and editing of the paper. AFJ collaborated with the design of the study, recruited participants, conducted data cleaning, and edited the paper.
Declarations
Ethics Approval
This study was performed according to the National Statement on Ethical Conduct in Research (2018) and received ethics approval from the University of Western Australia (RA/4/20/5896) and Curtin University (HRE2020-0197).
Informed Consent
All participants viewed the information sheet and consent form prior to participation. They were required to check a box indicating that they had read, understood, and consented in order to proceed with the survey.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Adams JS, Chien AT, Wisk LE. Mental illness among youth with chronic physical conditions. Pediatrics. 2019;144:1–11. doi: 10.1542/peds.2018-1819. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30(2):217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Allen AB, Leary MR. Self-compassion, stress, and coping. Social and Personality Psychology Compass. 2010;4(2):107–118. doi: 10.1111/j.1751-9004.2009.00246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G, Slade T. Interpreting scores on the Kessler psychological distress scale (K10) Australian and New Zealand Journal of Public Health. 2001;25(6):494–497. doi: 10.1111/j.1467-842X.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics. (2012). Information paper: Use of the Kessler psychological distress scale in ABS health surveys, Australia, 2007–2008. (No. 4817.0.55.001). https://www.abs.gov.au/Ausstats/abs@.nsf/mf/4817.0.55.001
- Bardeen JR, Fergus TA, Orcutt HK. An examination of the latent structure of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2012;34(3):382–392. doi: 10.1007/s10862-012-9280-y. [DOI] [Google Scholar]
- Barlow MR, Goldsmith Turow RE, Gerhart J. Trauma appraisals, emotion regulation difficulties, and self-compassion predict posttraumatic stress symptoms following childhood abuse. Child Abuse & Neglect. 2017;65:37–47. doi: 10.1016/j.chiabu.2017.01.006. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP. Future directions in emotion dysregulation and youth psychopathology. Journal of Clinical Child & Adolescent Psychology. 2015;44(5):875–896. doi: 10.1080/15374416.2015.1038827. [DOI] [PubMed] [Google Scholar]
- Bech P. The Bech, Hamilton and Zung scales for mood disorders: Screening and listening (2nd ed.) Springer; 1996. [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Segal ZV, Abbey S, Speca M, Velting D, Devins G. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice. 2004;11(3):230–241. doi: 10.1093/clipsy.bph077. [DOI] [Google Scholar]
- Bluth K, Gaylord S, Campo R, Mullarkey M, Hobbs L. Making friends with yourself: A mixed methods pilot study of a mindful self-compassion program for adolescents. Mindfulness. 2016;7(2):479–492. doi: 10.1007/s12671-015-0476-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluth K, Roberson P, Gaylord S, Faurot K, Grewen K, Arzon S, Girdler S. Does self-compassion protect adolescents from stress? Journal of Child and Family Studies. 2016;25(4):1098–1109. doi: 10.1007/s10826-015-0307-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brion JM, Leary MR, Drabkin AS. Self-compassion and reactions to serious illness: The case of HIV. Journal of Health Psychology. 2014;19(2):218–229. doi: 10.1177/1359105312467391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clegg S, Sirois F, Reuber M. Self-compassion and adjustment in epilepsy and psychogenic nonepileptic seizures. Epilepsy & Behavior. 2019;100:1–6. doi: 10.1016/j.yebeh.2019.106490. [DOI] [PubMed] [Google Scholar]
- Cobham VE, Hickling A, Kimball H, Thomas HJ, Scott JG, Middeldorp CM. Systematic review: Anxiety in children and adolescents with chronic medical conditions. Journal of the American Academy of Child & Adolescent Psychiatry. 2020;59(5):595–618. doi: 10.1016/j.jaac.2019.10.010. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences (2nd ed.) Erlbaum; 1988. [Google Scholar]
- Compas BE, Jaser SS, Dunn MJ, Rodriguez EM. Coping with chronic illness in childhood and adolescence. Annual Review of Clinical Psychology. 2012;8(1):455–480. doi: 10.1146/annurev-clinpsy-032511-143108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit M, Pouwer F, Gemke R, Waal H, Snoek F. Validation of the WHO-5 well-being index in adolescents with type 1 diabetes. Diabetes Care. 2007;30:2003–2006. doi: 10.2337/dc07-0447. [DOI] [PubMed] [Google Scholar]
- Diedrich A, Burger J, Kirchner M, Berking M. Adaptive emotion regulation mediates the relationship between self-compassion and depression in individuals with unipolar depression. Psychology and Psychotherapy: Theory, Research and Practice. 2017;90(3):247–263. doi: 10.1111/papt.12107. [DOI] [PubMed] [Google Scholar]
- Diedrich A, Grant M, Hofmann SG, Hiller W, Berking M. Self-compassion as an emotion regulation strategy in major depressive disorder. Behaviour Research and Therapy. 2014;58:43–51. doi: 10.1016/j.brat.2014.05.006. [DOI] [PubMed] [Google Scholar]
- Diener E. Subjective well-being. Psychological Bulletin. 1984;95(3):542–575. doi: 10.1037/0033-2909.95.3.542. [DOI] [PubMed] [Google Scholar]
- Finlay-Jones, A. L. (2017). The relevance of self-compassion as an intervention target in mood and anxiety disorders: A narrative review based on an emotion regulation framework. Clinical Psychologist, 21, 90–103. 10.1111/cp.12131
- Finlay-Jones, A. L., Rees, C. S., & Kane, R. T. (2015). Self-compassion, emotion regulation and stress among Australian psychologists: Testing an emotion regulation model of self-compassion using structural equation modelling. PLOS ONE, 10(7), e0133481. 10.1371/journal.pone.0133481 [DOI] [PMC free article] [PubMed]
- Finlay-Jones A, Boyes M, Perry Y, Sirois F, Lee R, Rees C. Online self-compassion training to improve the wellbeing of youth with chronic medical conditions: Protocol for a randomised control trial. BMC Public Health. 2020;20(1):1–10. doi: 10.1186/s12889-020-8226-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friis AM, Johnson MH, Cutfield RG, Consedine NS. Kindness matters: A randomized controlled trial of a mindful self-compassion intervention improves depression, distress, and HbA1c among patients with diabetes. Diabetes Care. 2016;39(11):1963–1971. doi: 10.2337/dc16-0416. [DOI] [PubMed] [Google Scholar]
- Garnefski N, Koopman H, Kraaij V, Cate R. Brief report: Cognitive emotion regulation strategies and psychological adjustment in adolescents with a chronic disease. Journal of Adolescence. 2009;32:449–454. doi: 10.1016/j.adolescence.2008.01.003. [DOI] [PubMed] [Google Scholar]
- Gilbert P. The origins and nature of compassion focused therapy. British Journal of Clinical Psychology. 2014;53(1):6–41. doi: 10.1111/bjc.12043. [DOI] [PubMed] [Google Scholar]
- Gilbert P, Procter S. Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy. 2006;13(6):353–379. doi: 10.1002/cpp.507. [DOI] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Hallion, L. S., Steinman, S. A., Tolin, D. F., & Diefenbach, G. J. (2018). Psychometric properties of the difficulties in emotion regulation scale (DERS) and its short forms in adults with emotional disorders. Frontiers in Psychology, 9(539). 10.3389/fpsyg.2018.00539 [DOI] [PMC free article] [PubMed]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression‐based approach. Guildford Press; 2013. [Google Scholar]
- Hu T, Zhang D, Wang J, Mistry R, Ran G, Wang X. Relation between emotion regulation and mental health: A meta-analysis review. Psychological Reports. 2014;114(2):341–362. doi: 10.2466/03.20.PR0.114k22w4. [DOI] [PubMed] [Google Scholar]
- IBM Corp. (2019). IBM SPSS Statistics for Macintosh. IBM Corp.
- Inwood E, Ferrari M. Mechanisms of change in the relationship between self-compassion, emotion regulation, and mental health: A systematic review. Applied Psychology. 2018;10(2):215–235. doi: 10.1111/aphw.12127. [DOI] [PubMed] [Google Scholar]
- Johnson E, O'Brien K. Self-compassion soothes the savage ego-threat system: Effects on negative affect, shame, rumination, and depressive symptoms. Journal of Social and Clinical Psychology. 2013;32(9):939–963. doi: 10.1521/jscp.2013.32.9.939. [DOI] [Google Scholar]
- Kane NS, Hoogendoorn CJ, Tanenbaum ML, Gonzalez JS. Physical symptom complaints, cognitive emotion regulation strategies, self-compassion and diabetes distress among adults with type 2 diabetes. Diabetic Medicine. 2018;35(12):1671–1677. doi: 10.1111/dme.13830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman EA, Xia M, Fosco G, Yaptangco M, Skidmore CR, Crowell SE. The difficulties in emotion regulation scale short form (DERS-SF): Validation and replication in adolescent and adult samples. Journal of Psychopathology and Behavioral Assessment. 2016;38(3):443–455. doi: 10.1007/s10862-015-9529-3. [DOI] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S-LT, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Keyes CLM, Fredrickson BL, Park N. Positive psychology and the quality of life. In: Land KC, Michalos AC, Sirgy MJ, editors. Handbook of social indicators and quality of life research (pp. 99–112) Springer Netherlands; 2012. [Google Scholar]
- Kılıç A, Hudson J, McCracken LM, Ruparelia R, Fawson S, Hughes LD. A systematic review of the effectiveness of self-compassion-related interventions for individuals with chronic physical health conditions. Behavior Therapy. 2020;52(3):607–625. doi: 10.1016/j.beth.2020.08.001. [DOI] [PubMed] [Google Scholar]
- Košir U, Loades M, Wild J, Wiedemann M, Krajnc A, Roškar S, Bowes L. The impact of COVID-19 on the cancer care of adolescents and young adults and their well-being: Results from an online survey conducted in the early stages of the pandemic. Cancer. 2020;126(19):4414–4422. doi: 10.1002/cncr.33098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraaij V, Garnefski N. Coping and depressive symptoms in adolescents with a chronic medical condition: A search for intervention targets. Journal of Adolescence. 2012;35(6):1593–1600. doi: 10.1016/j.adolescence.2012.06.007. [DOI] [PubMed] [Google Scholar]
- Krieger T, Altenstein D, Baettig I, Doerig N, Holtforth MG. Self-compassion in depression: Associations with depressive symptoms, rumination, and avoidance in depressed outpatients. Behavior Therapy. 2013;44(3):501–513. doi: 10.1016/j.beth.2013.04.004. [DOI] [PubMed] [Google Scholar]
- Lane RD, Quinlan DM, Schwartz GE, Walker PA, Zeitlin SB. The levels of emotional awareness scale: A cognitive-developmental measure of emotion. Journal of Personality Assessment. 1990;55:124–134. doi: 10.1080/00223891.1990.9674052. [DOI] [PubMed] [Google Scholar]
- Lu, L. H., Bowles, A. O., Kennedy, J. E., Eapen, B. C., & Cooper, D. B. (2020). Single-item versus multiple-item headache ratings in service members seeking treatment for brain injury. Military Medicine, 185(2), 43–46. 10.1093/milmed/usz173 [DOI] [PubMed]
- Macaskill A. Review of positive psychology applications in clinical medical populations. Healthcare. 2016;4(66):1–11. doi: 10.3390/healthcare4030066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacBeth A, Gumley A. Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review. 2012;32(6):545–552. doi: 10.1016/j.cpr.2012.06.003. [DOI] [PubMed] [Google Scholar]
- Mackenzie SB, Podsakoff PM. Common method bias in marketing: Causes, mechanisms, and procedural remedies. Journal of Retailing. 2012;88(4):542–555. doi: 10.1016/j.jretai.2012.08.001. [DOI] [Google Scholar]
- Marsh IC, Chan SWY, MacBeth A. Self-compassion and psychological distress in adolescents: A meta-analysis. Mindfulness. 2018;9:1011–1027. doi: 10.1007/s12671-017-0850-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy MC, McNeil R, Drew S, Dunt D, Kosola S, Orme L, Sawyer SM. Psychological distress and posttraumatic stress symptoms in adolescents and young adults with cancer and their parents. Journal of Adolescent and Young Adult Oncology. 2016;5(4):322–329. doi: 10.1089/jayao.2016.0015. [DOI] [PubMed] [Google Scholar]
- Mokkink LB, van der Lee JH, Grootenhuis MA, Offringa M, Heymans HAS. Defining chronic diseases and health conditions in childhood (ages 0–18 years of age): National consensus in the Netherlands. European Journal of Pediatrics. 2008;167:1441–1447. doi: 10.1007/s00431-008-0697-y. [DOI] [PubMed] [Google Scholar]
- Moreira, H., Gouveia, M. J., & Canavarro, M. C. (2020). A bifactor analysis of the difficulties in emotion regulation scale - short form (DERS-SF) in a sample of adolescents and adults. Current Psychology. Advance online publication. 10.1007/s12144-019-00602-5
- Neff K. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity. 2003;2(2):85–101. doi: 10.1080/15298860309032. [DOI] [Google Scholar]
- Neff KD. The development and validation of a scale to measure self-compassion. Self and Identity. 2003;2(3):223–250. doi: 10.1080/15298860309027. [DOI] [Google Scholar]
- Neff KD. The role of self-compassion in development: A healthier way to relate to oneself. Human Development. 2009;52(4):211–214. doi: 10.1159/000215071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology. 2013;69(1):28–44. doi: 10.1002/jclp.21923. [DOI] [PubMed] [Google Scholar]
- Neff KD, Long P, Knox MC, Davidson O, Kuchar A, Costigan A, Williamson Z, Rohleder N, Tóth-Király I, Breines JG. The forest and the trees: Examining the association of self-compassion and its positive and negative components with psychological functioning. Self and Identity. 2018;17(6):627–645. doi: 10.1080/15298868.2018.1436587. [DOI] [Google Scholar]
- Neumann A, van Lier PAC, Gratz KL, Koot HM. Multidimensional assessment of emotion regulation difficulties in adolescents using the difficulties in emotion regulation scale. Assessment. 2010;17(1):138–149. doi: 10.1177/1073191109349579. [DOI] [PubMed] [Google Scholar]
- Pinto-Gouveia J, Duarte C, Matos M, Fráguas S. The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic and in cancer patients. Clinical Psychology and Psychotherapy. 2014;21(4):311–323. doi: 10.1002/cpp.1838. [DOI] [PubMed] [Google Scholar]
- Raes F. Rumination and worry as mediators of the relationship between self-compassion and depression and anxiety. Personality and Individual Differences. 2010;48(6):757–761. doi: 10.1016/j.paid.2010.01.023. [DOI] [Google Scholar]
- Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the self-compassion scale. Clinical Psychology and Psychotherapy. 2011;18:250–255. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- Richter D, Koehler M, Friedrich M, Hilgendorf I, Mehnert A, Weißflog G. Psychosocial interventions for adolescents and young adult cancer patients: A systematic review and meta-analysis. Critical Reviews in Oncology / Hematology. 2015;95(3):370–386. doi: 10.1016/j.critrevonc.2015.04.003. [DOI] [PubMed] [Google Scholar]
- Seligman MEP, Csikszentmihalyi M. Positive psychology: An introduction. American Psychologist. 2000;55(1):5–14. doi: 10.1037/0003-066X.55.1.5. [DOI] [PubMed] [Google Scholar]
- Sirois FM. A self-regulation resource model of self-compassion and health behavior intentions in emerging adults. Preventive Medicine Reports. 2015;2:218–222. doi: 10.1016/j.pmedr.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirois FM, Molnar D, Hirsch JK. Self-compassion, stress and coping in the context of chronic illness. Self and Identity. 2015;14(3):334–347. doi: 10.1080/15298868.2014.996249. [DOI] [Google Scholar]
- Subic-Wrana C, Beutel ME, Brähler E, Stöbel-Richter Y, Knebel A, Lane RD, Wiltink J. How is emotional awareness related to emotion regulation strategies and self-reported negative affect in the general population? Plos One. 2014;9(3):Article e91846. doi: 10.1371/journal.pone.0091846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svendsen JL, Osnes B, Binder P-E, Dundas I, Visted E, Nordby H, Schanche E, Sørensen L. Trait self-compassion reflects emotional flexibility through an association with high vagally mediated heart rate variability. Mindfulness. 2016;7(5):1103–1113. doi: 10.1007/s12671-016-0549-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner, J. L., & Arnett, J. J. (2011). Presenting “emerging adulthood”: What makes it developmentally distinctive? In J. J. Arnett, L. B. Henry, M. Kloep & J. L. Tanner (Eds.), Debating emerging adulthood: Stage or process (pp. 13–30). Oxford University Press.
- Thompson RA. Emotion regulation: A theme in search of definition. Monographs of the Society for Research in Child Development. 1994;59(2–3):25–52. doi: 10.2307/1166137. [DOI] [PubMed] [Google Scholar]
- Trindade IA, Ferreira C, Moura-Ramos M, Pinto-Gouveia J. An 18-month study of the effects of IBD symptomatology and emotion regulation on depressed mood. International Journal of Colorectal Disease. 2017;32(5):651–660. doi: 10.1007/s00384-017-2774-z. [DOI] [PubMed] [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy. 2007;38(3):303–313. doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. Journal of the American Medical Association. 2010;303(7):623–630. doi: 10.1001/jama.2010.104. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Yang Y, Zhang M, Kou Y. Self-compassion and life satisfaction: The mediating role of hope. Personality and Individual Differences. 2016;98:91–95. doi: 10.1016/j.paid.2016.03.086. [DOI] [Google Scholar]
- Zessin U, Dickhäuser O, Garbade S. The relationship between self-compassion and well-being: A meta-analysis. Applied Psychology: Health and Well-Being. 2015;7(3):340–364. doi: 10.1111/aphw.12051. [DOI] [PubMed] [Google Scholar]