Abstract
Introduction:
The prevalence of induced abortion among women with children has been estimated indirectly by projections derived from survey research. However, an empirically derived, population-based conclusion on this question is absent from the published literature.
Objective:
The objective of this study was to describe the period prevalence of abortion among all other possible pregnancy outcomes within the reproductive histories of Medicaid-eligible women in the U.S.
Methods:
A retrospective, cross-sectional, longitudinal analysis of the pregnancy outcome sequences of eligible women over age 13 from the 17 states where Medicaid included coverage of most abortions, with at least one identifiable pregnancy between 1999 and 2014. A total of 1360 pregnancy outcome sequences were grouped into 8 categories which characterize various combinations of the 4 possible pregnancy outcomes: birth, abortion, natural loss, and undetermined loss. The reproductive histories of 4,884,101 women representing 7,799,784 pregnancy outcomes were distributed into these categories.
Results:
Women who had live births but no abortions or undetermined pregnancy losses represented 74.2% of the study population and accounted for 87.6% of total births. Women who have only abortions but no births constitute 6.6% of the study population, but they are 53.5% of women with abortions and have 51.5% of all abortions. Women with both births and abortions represent 5.7% of the study population and have 7.2% of total births.
Conclusion:
Abortion among low-income women with children is exceedingly uncommon, if not rare. The period prevalence of mothers without abortion is 13 times that of mothers with abortion.
Keywords: pregnancy outcomes, induced abortion, pregnancy loss, Medicaid, fertility intentions
Introduction
A comprehensive description and analysis of the reproductive history of a population, i.e. the number and outcome of each pregnancy for every woman, has never appeared in the peer-reviewed science. Since the number and outcomes of pregnancies experienced by a woman are consequential determinants of her health status, the lack of a method to operationalize the patterning of pregnancy outcome sequences has limited the conduct of empirical research in this domain. The focus of interest of this research is the prevalence of induced abortion among the universe of pregnancies, and in particular, the extent to which abortion has been utilized by women to time and space their children. We found no empirically derived estimates of the prevalence of abortion in women with children in the published literature.
Various surveys report that 60% of women seeking an abortion have not completed their childbearing, and that 59% of women who have an abortion also have one or more children. 1,2 Analysis of more recent survey results from women obtaining abortions indicates that 16% were not sure if they wanted to have children, while 39% intended to have children, including 20% who wanted to delay a first birth and 19% who wanted to delay a second or higher order birth. 3 These survey results have a fundamental limitation as a measurement of fertility intentions: they describe a woman’s intention or motivation at a specific point in her reproductive history and, often, for only a single pregnancy outcome. A woman’s plans for future pregnancies, and her ability to achieve those plans, may change based on a myriad of influencing factors, including the trajectory of her reproductive history, prior pregnancy outcomes, and perceptions of pregnancy wantedness. 4,5
While these surveys attempt to represent motivation or intention to behave in a certain way, they do not provide any actual data on the number and type of pregnancy outcomes actually experienced by women. Nor do they deal more broadly with women who have abortions without births or women who have births but no abortions. A comprehensive population-based accounting of pregnancy outcome sequences, or the specific combination of pregnancy outcomes for each woman, may provide the data to estimate certain fertility or abortion intentionality behaviors. In previous research we were able to conclude that only about 1% of Medicaid enrolled women of childbearing age who had at least one pregnancy between 1999-2014 had spaced live births with an intervening induced abortion. 6 The objective of this research was to extend the concept of pregnancy outcome sequencing (POS) by defining mutually exclusive categories of sequences which could comprehensively describe patterns of a woman’s reproductive history. The subsequent distribution of women into these categories provides, for the first time in the literature, an empirically derived population-based estimate of the role of abortion in postponing, ending, or avoiding childbearing. The construct of POS provides an important methodology by which to quantify and characterize reproductive history, and the results inform reproductive epidemiology.
Methods
Data were obtained from the enrollee-level Medicaid Analytic eXtract (MAX) files licensed through the Centers for Medicare and Medicaid Services (CMS) Chronic Condition Data Warehouse’s (CCW) Medicaid data. The study population is comprised of enrollees from the 17 states whose official policies applied state funds to most abortions not covered by federal Medicaid during the period 1999 through 2014. Not all states funded abortion consistently or to the same extent during the study period. Despite their official policies, Arizona and Illinois funded relatively few abortions during this period, and Alaska experienced a short interruption to its abortion coverage. 7 Not all states had provided claims data through 2014 due to differing reporting timeframes. The latest year of data relative to each state was 2012 for Alaska, Illinois, Maryland, Montana, and New Mexico; 2013 for Arizona, Connecticut, Hawaii, Massachusetts, New York, Oregon, and Washington; and 2014 for California, Minnesota, New Jersey, Vermont, and West Virginia.
The study population was made up of enrollees over 13 years of age with at least one identifiable pregnancy outcome from 1999 through the latest year of data available for each state. For each beneficiary, all unique pregnancy outcomes were identified using International Classification of Diseases, Ninth Revision (ICD9) codes. Additionally, Current Procedural Terminology, 4th Edition (CPT4) and Healthcare Common Procedure Coding System (HCPCS) codes were used to confirm pregnancy outcomes.
These codes were used to allocate all pregnancy outcomes into 4 categories: live birth (ICD9 V27.0, V27.2, and V27.5), natural loss (ICD9 V27.1, V27.4, V27.7, 630, 631, 633, 634), induced abortion (ICD9 635.xx, CPT4 59840, 59841, 59850, 59851, 59852, 59855, 59856, 59857, and HCPCS: S0199, S2260, S2265, S2266, S2267, X7724, X7726, S0190, S0191), and undetermined loss. The category “undetermined loss” includes cases coded as illegally induced abortion (ICD9 636), unspecified abortion (ICD9 637), and failed attempted abortion (ICD9 638). In order to identify each unique pregnancy, multiple diagnostic or treatment codes within 30 days of a pregnancy loss (natural, induced, or undetermined) or within 180 days of a live birth were counted as a single pregnancy outcome using the first date associated with that series of Medicaid claims. Twins and higher order gestations that resulted in a combination of live birth and fetal loss were excluded from the analysis. The study has been exempted from IRB review pursuant to the U.S. Department of Health and Human Services (DHHS) Policy for Protection of Human Research Projects at C.F.R. 46.101(b). 8
The analytic strategy was composed of 3 phases. First, we identified all possible combinations of pregnancy outcomes within up to 5 pregnancies. Less than 1% of women in our study population had more than 5 pregnancies. Any given pregnancy can have 4 possible mutually exclusive outcomes: (1) live birth, (2) induced abortion, (3) natural loss, or (4) a loss of undetermined nature (unable to determine if induced or spontaneous loss). A single pregnancy can thus have 4 outcomes. Two pregnancies have a possible 4 times 4 or 16 possible sequences (1-1, 1-2, 1-3, 1-4, 2-1, 2-2, 2-3, etc.). Similarly, 3 pregnancies have 4 to the third power combinations (64); 4 pregnancies 4 to the fourth power (256); and 5 pregnancies 4 to the fifth power (1024). For a data set consisting of women who had at least one pregnancy, the total number of combinations for up to 5 pregnancies is thus 4 + 16 + 64 + 256 + 1024 = 1364 unique sequences. Of these 1364 possible combinations, 1360 were observed in the selected data set.
Second, we grouped the 1360 sequences by defining 5 mutually exclusive pregnancy behaviors as follows:
Group A: Abortion and natural losses only. This group includes sequences with undetermined losses and at least one confirmed abortion, but no live births.
Group B: Live births and natural losses only. This group has no abortions and hence no undetermined losses.
Group C: Live births and abortions combined. This group includes undetermined losses because a sequence includes both a confirmed live birth and an abortion.
Group D: Natural losses only. This group has no live births, abortions, or undetermined losses.
Group U: Remaining undetermined losses. This group includes births and natural losses, but no confirmed abortions.
All possible sequences which could be included in each of the 5 major categories were identified. The number of pregnancy outcome sequences (POS) which compose each category appears in the bottom row of Table 1. For each category, we sorted through our sample of Medicaid-eligible women with at least one pregnancy outcome to identify each woman who had a matching sequence. The assignment was based on the entire 15 year cumulative history with no analyses attempted of the transitional probabilities of each subsequent pregnancy.
Table 1.
Five Medicaid Reproductive History Patterns Composed of 1360 Pregnancy Outcome Sequences (POS).
| Counts/values | Abortions, no births (A) | Births, no abortions (B) | Births & abortions (C) | Natural loss only (D) | Remaining undetermined (U) | Grand total |
|---|---|---|---|---|---|---|
| Women (patients) (%) | 321,571 (6.6) | 3,623,191 (74.2) | 279,871 (5.7) | 272,485 (5.6) | 386,983 (7.9) | 4,884,101 |
| Births (%) | 0 | 4,960,803 (87.6) | 405,102 (7.2) | 0 | 296,181 (5.2) | 5,662,087 |
| per woman | 0 | 1.37 | 1.44 | 0 | .76 | 1.16 |
| Abortions (%) | 459,030 (51.6) | 0 | 431,271 (48.4) | 0 | 0 | 890,301 |
| per woman | 1.43 | 0 | 1.54 | 0 | 0 | .18 |
| Natural losses (%) | 26,751 (3.5) | 291,271 (38.0) | 41,163 (5.4) | 317,070 (41.3) | 90,450 (11.8) | 766,705 |
| per woman | .08 | .08 | .15 | 1.16 | .23 | .16 |
| Undetermined (%) | 19,910 (4.1) | 0 | 28,938 (6.0) | 0 | 431,843 (89.8) | 480,691 |
| per woman | .06 | 0 | .10 | 0 | 1.12 | .10 |
| Pregnancies (%) | 505,691 (6.5) | 5,252,074 (67.3) | 906,475 (11.6) | 317,070 (4.0) | 818,474 (10.5) | 7,799,784 |
| per woman | 1.57 | 1.45 | 3.24 | 1.16 | 2.11 | 1.60 |
| # Pregnancy outcome sequences (POS) | 298 | 57 | 699 | 5 | 301 | 1360 |
Third, we identified 3 subgroups within the major category Group C in order to estimate the period prevalence of defined pregnancy outcome sequences which are proxy measures of motivation or intention of abortion in the context of childbearing:
I: Abortion that delays a first birth. One or more abortions followed by a subsequent live birth.
II: Abortion that spaces children. Any form of the sequence birth-abortion-birth.
III: Abortion that ends childbearing. Last pregnancy outcome was an abortion, with at least one preceding live birth.
The process of matching sequences in each Group C subgroup was similar to that described for the major categories except that the subgroups are not unique; that is, a woman may have a sequence which matches more than a single subgroup and would be counted in both subcategories. For example, she may have had both an abortion that delayed a first birth and an abortion that spaced 2 live births. The overlapping cumulative counts provide the most accurate indication of period prevalence for these patterns.
Findings
The study population of 4,884,101 women accounted for a total of 7,799,784 pregnancy outcomes: 5,662,087 births (72.6%); 890,301 induced abortions (11.4%); 766,705 miscarriages (9.8%) and 480,691 undetermined (6.2%).
There were 321,571 women with abortions but no births (Group A), 6.6% of the study population (Table 1). Group A accounts for 459,030 abortions or 51.6% of total abortions and 1.43 abortions per woman. The group also accounts for 26,751 (3.5%) miscarriages and 19,910 (4.1%) undetermined outcomes. Overall, Group A women had 505,691 pregnancies (6.5%) and 1.57 pregnancies per woman.
There were 3,623,191 women who had live births but no abortions (Group B). This large group of women represented 74.2% of the study population and accounted for 4,960,803 births, or 87.6% of the total, i.e. 1.4 births per woman. The B group accounted for 291,271 (38.0%) of the miscarriages and 5,252,074 (67.3%) of total pregnancies; 1.45 pregnancies per woman.
Women who had both births and abortions (Group C) totaled 279,871 or 5.7% of the study population. Group C women accounted for 431,271 (48.4%) abortions or 1.5 abortions per woman; 405,102 (7.2%) births or 1.4 births per woman; and 41,163 (5.4%) miscarriages. This group had 906,474 (11.6%) of the pregnancies or 3.2 per woman.
Within this group, the distribution of patients into 3 specific patterns of abortion placement relative to birth sequences, a proxy measure of “intentionality,” was as follows (Table 2):
Abortion that delays a first birth, 107,868 (38.5%);
Abortion that spaces births, 49,996 (17.9%);
Abortion that ends childbearing, 146,321 (52.3%).
Table 2.
Women With Births and Abortions in 3 Non-Discrete and Non-Comprehensive Categories.
| I (%)* | II (%) | III (%) | Unique | |
|---|---|---|---|---|
| Patients | 107,868 (38.5) | 49,996 (17.9) | 146,321 (52.3) | 279,871 |
| Births | 135,338 (33.4) | 117,608 (29.0) | 191,112 (47.2) | 405,102 |
| Abortions | 183,115 (42.5) | 77,660 (18.0) | 247,479 (57.4) | 431,271 |
| # POS | 349 | 120 | 220 | 699 |
I: Abortion to delay first birth.
II: Abortion to space birth.
III: Abortion to end childbearing.
* Is of unique patients and outcomes.
Unlike the 5 major categories in Table 1, which are discrete and non-overlapping, the values in Table 2 for the subgroups of major group C (births and abortions) are non-discrete, non-comprehensive and overlapping. This is because women, births, abortions, and pregnancy outcome sequences can appear in more than one subgroup and, in Table 2, not all possible subgroups are shown.
There were 272,485 (5.6%) women who experienced natural losses only, with no undetermined pregnancy outcomes (Group D). This group experienced 317,070 (41.3%) natural losses and 4% of the total pregnancies.
Finally, the remaining group of women (Group U), which did not fit into any of the previous 4 categories had 89.8%, 431,843, of the total of undetermined outcomes, and also 296,181 (5.2%) births and 90,450 (11.8%) natural losses. Group U had a total of 818,474 (10.5%) pregnancies, or 2.1 per woman.
Discussion
Influential private foundations and professional associations have consistently promoted induced abortion as an integral part of family planning. 9 -11 Based entirely upon survey data, some researchers have concluded that abortion is common among women with children. Media coverage has claimed that “women who are already mothers have more abortions than anyone else” and that “the typical abortion patient is a mother.” 12 This assertion has been expanded to further assert that there are no differences between “‘women who have abortions’ on one side and ‘women who are mothers’ on another; these groups are often the same.” 13 How valid are these assertions when they are subjected to empirical analysis?
Women who have both births and abortions represent only 5.7% of the study population (Figure 1). Women who have only abortions but no births constitute a larger group, 6.6% of the study population; and women with only births but no abortions represent 74.2% of the study population. So, the assertion that women with abortions and births “are often the same” is demonstrably false—among the larger population of women who have experienced pregnancy, women with both abortions and births are decidedly uncommon if not rare. Note also that women without abortions have 92.8% of the total births compared to only 7.2% represented by women who have also had abortions (Figure 2). Further note that among our study population, only 12.3% of women experience an abortion, including both those with and without children (Figure 3). Although they are not directly comparable, this number is half the estimate of the often-reported lifetime abortion incidence (24%), also derived from projections based on survey data. 14
Figure 1.
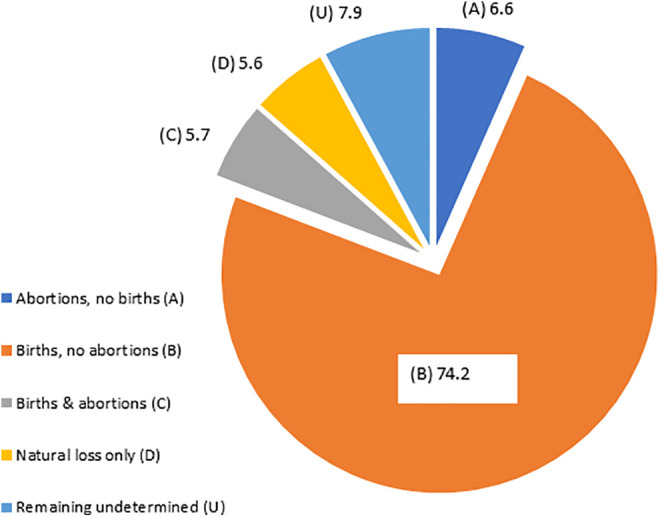
All women (4,884,101) by pregnancy outcome sequence categories (%).
Figure 2.
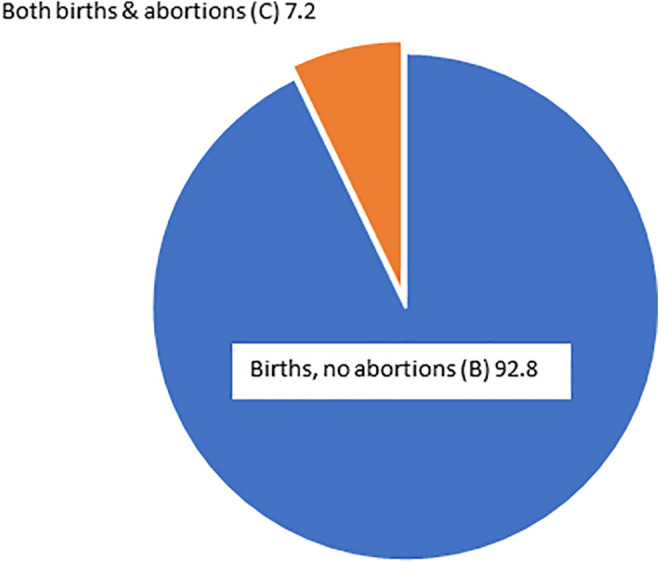
Abortion status of women with births (3,903,062) (%).
Figure 3.
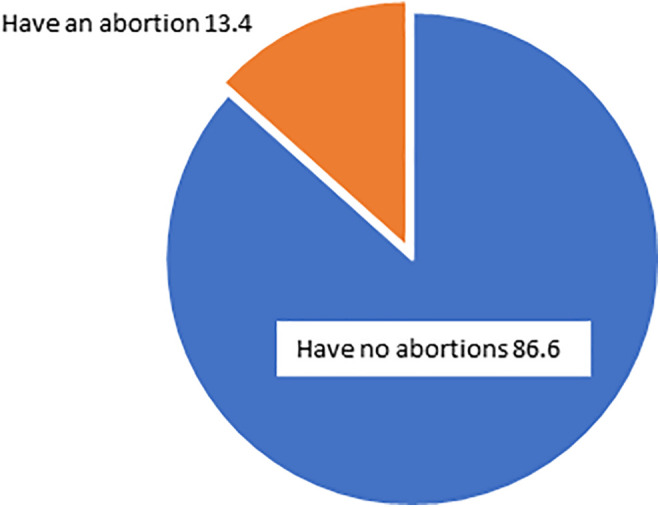
Women with all known outcomes (4,497,118), by abortion status (%).
Of the total number of women who have abortions, 53.5% have no births and they account for 51.5% of total abortions (Figure 4). This finding stands in contrast to the idea of the “Mother Majority”; that is, that mothers account for more of the total abortions than do women without children. Of further note, women who have both abortions and births actually, on average, have more abortions than they have children (1.54 versus 1.44 per woman). In other words, in this group, a woman is actually more likely to be spacing abortions with a birth than spacing births with an abortion. Further, women with both abortions and births experience twice the average number of pregnancies per woman (3.24) than either women with only abortions (1.57) or only births (1.45). This finding is consistent with previous research which indicates that abortion results in a higher number of rapid repeat pregnancies which result in more abortions. 15,16
Figure 4.

Women with confirmed abortions (601,442) by birth status (%).
Within the group of women with both births and abortions, 38.5% had an abortion timed consistent with an attempt to delay a first birth, 17.9% had an abortion that spaced live births, and 52.3% had an abortion that could indicate a desire to end childbearing. The estimated period prevalence for each of these patterns is 2.2%, 1.0%, and 3.0% respectively. Therefore, abortion practiced possibly as a means to achieve any of these family planning objectives is rare. These prevalence estimates used the study population of Medicaid women with at least a single pregnancy (4,884,101) as the denominator. A prevalence estimate using all Medicaid-eligible women of childbearing age would yield a significantly lower incidence for each of these patterns.
In summary, these findings indicate that a woman who has both abortions and births is exceedingly uncommon, if not rare. Women without abortions account for nearly 93% of all births. Women with abortions and births have more abortions than births and double the number of pregnancies of any other group. Frequent abortion to achieve some family planning objective is largely unsupported by empirical evidence. Abortion is not a pregnancy outcome that typifies motherhood.
The use of Medicaid claims data has limitations. Medicaid-eligible beneficiaries are low income and do not represent the universe of U.S. women experiencing abortion, and the factors of race and financial status are likely to have both independent and joint impacts on the patterns of childbearing and abortion. While there is no research on the impact of a woman’s financial status on her likelihood to have both a birth and an abortion, there is some evidence that women who do not use insurance for an abortion (self-payers) appear less likely to have repeat abortions. 17 Pregnancy outcomes occurring before 1999 or after 2014 or during periods of ineligibility are not included in these claims data. Similarly, services received by Medicaid-eligible women but not funded by Medicaid (e.g., paid “out-of-pocket”) are not included. Administrative data may be affected by inconsistent and erroneous coding and the exclusion of codes considered unnecessary for billing, which may vary from state to state. 18,19 Our analysis used ICD codes to identify women who had abortions, which could result in an undercount from providers which do not use ICD codes to code abortions. However, any undercount would likely result from random variation over time in coding protocols and would be unlikely to impact the findings. The prevalence estimates derived are based solely on the counts of specific pregnancy outcome sequences absent any knowledge of motivation or intentionality.
Finally, it is worth noting that the U.S. lacks a national, all-pregnancy outcomes registry. Such a system would enable the analysis of the universe of pregnancy outcomes across all pay sources and states, and markedly inform the epidemiology of induced abortion.
Author Biographies
James Studnicki is currently the Vice President and Director of Data Analytics at the Charlotte Lozier Institute in Arlington, Virginia. Over a span of four decades, he held academic appointments at the Johns Hopkins University School of Hygiene and Public Health, the University of South Florida College of Public Health, and the University of North Carolina, Charlotte, where for ten years he served as the Irwin Belk Endowed Chair in Health Services Research. Dr. Studnicki holds Doctor of Science (ScD) and Master of Public Health (MPH) degrees from Johns Hopkins and a Master of Business Administration (MBA) from the George Washington University.
John W. Fisher is currently an Associate Scholar at the Charlotte Lozier Institute. Following a 22 year career as a nuclear submarine officer, he served as the Director of Life Support and engineering at the Florida Aquarium, Chief Financial Officer of Technology Transfer Services, and 10 years as an Assistant Professor at the University of North Carolina at Charlotte College of Health and Human Services. Dr. Fisher holds a PhD in Information Systems and Decision Sciences from the University of South Florida, a JD from Massachusetts School of Law, and Master's degrees from the Massachusetts Institute of Technology (Ocean Engineering), University of Notre Dame (Administration), Indiana University (Business Administration), and the United States Naval War College (National Security Policy). He is currently a member of the bar in New Hampshire and Massachusetts.
Tessa Longbons is a research associate with the Charlotte Lozier Institute. Her research focuses on abortion statistics at the state and national levels and the changing landscape of abortion policy, provision, and access in the United States. She received her B.A. from Thomas Edison State University.
David C. Reardon is the director of Elliot Institute, a biomedical ethicist, and a lead author on numerous studies and books examining the risk factors and effects of pregnancy loss on women and families.
Donna J. Harrison, M.D. dip ABOG received her M.D. from the University of Michigan and completed ObGyn residency at a University of Michigan Affiliate hospital (St. Joseph Mercy Hospital). She is currently CEO of the American Association of Pro-Life Obstetricians and Gynecologists.
Christopher Craver is an independent health services researcher affiliated with the Charlotte Lozier Institute focused on the use of secondary healthcare data sources in population based scientific research. He is widely published in many healthcare topics including cancer treatment, rare disease populations, and the efficacy of surgical services.
Maka Tsulukidze, MD, PhD, MPH, is an Assistant Professor at the Florida Gulf Coast University, Marieb College of Health & Human Services. Before joining FGCU, Dr. Tsulukidze was a Postdoctoral Fellow at the Dartmouth Center for Health Care Delivery Science. She has earned a Ph.D. degree from the University of North Carolina at Charlotte and MD from Tbilisi Medical Academy. Previously Dr. Tsulukidze was a UNICEF National Consultant to the Parliament of Georgia, Short-Term Consultant at PAHO/WHO and Senior Expert at the Parliament of Georgia, Committee on Health and Social Issues. She has also worked as a Deputy Chair/Project Manager for the Task Force for Prevention of Micronutrient Malnutrition and Food Fortification Initiatives established under the Parliament of Georgia, Committee on Health and Social Issues.
Ingrid Skop, M.D., F.A.C.O.G. has been a practicing obstetrician-gynecologist in San Antonio, Texas for 24 years. She received her Bachelor of Science in physiology from Oklahoma State University and her medical doctorate from Washington University School of Medicine. She completed her residency in obstetrics and gynecology at the University of Texas Health Science Center at San Antonio. Dr. Skop is a Fellow of the American College of Obstetrics and Gynecology, a Charlotte Lozier Institute Associate Scholar and Chairman of the American Association of Pro-Life Obstetricians and Gynecologist's Maternal Mortality Committee. She is the Board Chairman of Any Woman Can Pregnancy Resource Center-which specializes in free mental health counseling and is a board member of The Source for Women-a consortium of holistic women's health care centers in Texas. Dr. Skop is married to a physician and is the proud mother of two sons and a daughter.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Charlotte Lozier Institute.
ORCID iDs: James Studnicki  https://orcid.org/0000-0003-2958-7493
https://orcid.org/0000-0003-2958-7493
Tessa Longbons  https://orcid.org/0000-0003-0479-9166
https://orcid.org/0000-0003-0479-9166
References
- 1. Finer LB, Frohwirth LF, Dauphinee LA, Singh S, Moore AM. Reasons U.S. women have abortions: quantitative and qualitative perspectives. Perspect Sex Reprod Health. 2005;37(3):110–118. doi:10.1363/psrh.37.110.05 [DOI] [PubMed] [Google Scholar]
- 2. Kortsmit K, Jatlaoui TC, Mandel MG, et al. Abortion surveillance—United States, 2018. MMWR Surveill Summ. 2020;69(7):1–29. doi:http://dx.doi.org/10.15585/mmwr.ss6907a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jones RK, Foster DG, Biggs AM. Fertility intentions and recent births among U.S. abortion patients. Contraception. 2021;103(2):75–79. doi:10.1016/j.contraception.2020.11.007 [DOI] [PubMed] [Google Scholar]
- 4. Preis H, Tovim S, Mor P, Grisaru-Granovsky S, Samueloff A, Benyamini Y. Fertility intentions and the way they change following birth—a prospective longitudinal study. BMC Pregnancy Childbirth. 2020;20(1):228. doi:10.1186/s12884-020-02922-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Biggs MA, Neilands TB, Kaller S, Wingo E, Ralph LJ. Developing and validating the psychosocial burden among people seeking abortion scale (PB-SAS). PLoS One. 2020;15(12):e0242463. doi:10.1371/journal.pone.0242463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Studnicki J, Fisher JW, Longbons T, Reardon DC, Craver C, Harrison DJ. Estimating the period prevalence of publicly funded abortion to space live births, 1999-2014. J Prim Care Community Health. 2021;12. doi:10.1177/21501327211012182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. New MJ. Hyde @ 40: Analyzing the Impact of the Hyde Amendment. Charlotte Lozier Institute; On Point Series 12. 2016. Accessed November 23, 2020. https://s27589.pcdn.co/wp-content/uploads/2016/09/OP_hyde_9.28.3.pdf [Google Scholar]
- 8. IRB. ID 7269. www.sterlingirb.com
- 9. American Board of Obstetrics and Gynecology. Proposal for the ACGME accreditation of a new fellowship program in the subspecialty of complex family planning. Published 2018. Accessed June 9, 2020. https://www.acgme.org/Portals/0/PFAssets/ProposalReviewandComment/Complex_Family_Planning_LOIandProposal.pdf
- 10. American Public Health Association. APHA Policy Statement 20103: Protecting Abortion Coverage in Health Reform. American Public Health Association; 2010. Accessed June 9, 2020. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2014/07/24/10/48/protecting-abortion-coverage-in-health-reform [Google Scholar]
- 11. Bill and Melinda Gates Foundation. Family Planning: Strategy Overview. Gates Foundation. https://www.gatesfoundation.org/What-We-Do/Global-Development/Family-Planning Accessed June 9, 2020. [Google Scholar]
- 12. Sander L. The mother majority. SLATE. Published 2011. Accessed June 2, 2021. https://slate.com/human-interest/2011/10/most-surprising-abortion-statistic-the-majority-of-women-who-terminate-pregnancies-are-already-mothers.html
- 13. Filipovic J. I’m a mother, and I had an abortion. Cosmopolitan. Published 2014. Accessed June 2, 2021. https://www.cosmopolitan.com/politics/news/a7061/mothers-abortion/
- 14. Jones RK, Jerman J. Population group abortion rates and lifetime incidence of abortion: United States, 2008-2014. Am J Public Health. 2017;107(12):1904–1909. doi:10.2105/AJPH.2017.304042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Studnicki J, Fisher JW, Reardon DC, Craver C, Longbons T, Harrison DJ. Pregnancy outcome patterns of Medicaid-eligible women, 1999-2014: a national prospective longitudinal study. Health Serv Res Manag Epidemiol. 2020;7. doi:10.1177/2333392820941348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Reardon DC, Craver C. Intervals and outcomes of first and second pregnancies in low income women: a record linkage longitudinal prospective cohort study. Med Sci Monit. 2021;27:e931596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jones R, Jerman J, Ingerick M. Which abortion patients have had a prior abortion? Findings from the 2014 U.S. abortion patient survey. J Womens Health (Larchmt). 2018;27(1):58–63. doi:10.1089/jwh.2017.6410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hicks J. The Potential of Claims Data to Support the Measurement of Health Care Quality [dissertation]. RAND; 2003. [Google Scholar]
- 19. Romano PS. Using administrative data to identify associations between implanted medical devices and chronic diseases. Ann Epidemiol. 2000;10(4):197–199. doi:10.1016/s1047-2797(00)00041-7 [DOI] [PubMed] [Google Scholar]


