Abstract
Background:
The 3 Wishes Project (3WP) promotes a personalized dying experience by eliciting and facilitating individualized terminal wishes for patients, families and the clinicians caring for them. We aimed to evaluate the adaptability of the 3WP to a community intensive care unit (ICU), and to describe the patients cared for with this palliative approach, as well as local implementation strategies.
Methods:
The 3WP was implemented in a 15-bed community hospital ICU in southern Ontario from 2017 to 2019. In this observational, descriptive study, we invited adult patients (≥ 18 yr) whose risk of death was deemed to be 95% or greater by the attending physician, or patients undergoing withdrawal of life-support to participate. We abstracted patient data from medical records, as well as the type, timing and cost of each wish, which person or service made and facilitated each wish, and if and why wishes were completed or not. We summarized data both narratively and quantitatively.
Results:
The 3WP helped to realize 479 (99.2%) of 483 terminal wishes for 101 dying patients. This initiative was introduced as an interprofessional intervention and championed by nursing staff who were responsible for most patient enrolment and wish facilitation. Wishes included humanizing the ICU environment for the patient with belongings and blankets, musical performances, smudging and bathing ceremonies, and keepsakes. The cost was $5.39 per patient (standard deviation $22.40), with 430 (89.8%) wishes incurring no cost. Wishes made directly by patients accounted for 30 (6.2%) of wishes; those from family members and ICU staff accounted for 236 (48.9%) and 238 (49.3%) of wishes, respectively. The program comforted patients and their loved ones, motivating clinicians to sustain this end-of-life intervention.
Interpretation:
We documented successful implementation of the 3WP in a community hospital, showing program adaptability and uptake outside of academic centres at relatively low cost. The lack of strict protocolization and personalized design of this intervention underscores its inherent flexibility, with potential to promote individualized end-of-life care in nonacademic hospital wards, homes or hospice.
Death and dying are undoubtedly sacred processes, valued and experienced differently across cultures. In some Buddhist traditions, the last thought at the moment of death determines the character of the next reincarnation. For the First Nations Ojibway people, the time of death is a spiritual transcendence, where Mother Earth reclaims the physical form, and the Creator father carries the spirit to its origin place.1 Despite its sanctity, most deaths in Canada occur in hospital,2 guided by clinicians and often without an individualized approach.
In the intensive care unit (ICU), technology deployed for monitoring and treatment can render the setting impersonal, noisy and sterile for critically ill patients who are dying. End-of-life care is ideally congruent with the goals of the patient, sometimes expressed in written or verbal advanced directives, but often expressed by family members in real time during serious illness. Despite the high mortality rate of patients who are critically ill or injured, optimal strategies for providing personalized care to dying patients, and methods to help families navigate the dying and grieving processes, remain understudied in the ICU setting.
The 3 Wishes Project (3WP) was developed in an academic teaching hospital with the goal of bringing peace to a patient’s final days and comforting families. This program aims to honour the individual, promote patient legacy, support families, and enrich relationships among patients, families and clinicians — all integral to patient-and family-centred end-of-life care3–5 — by eliciting and facilitating terminal wishes for dying patients, their loved ones and the clinicians caring for them. Wishes range from enhancing the clinical environment with personal belongings, to life celebrations, pet visitation, religious ceremonies and musical performances.4 Multicentred program evaluation in 4 North American academic centres showed that the 3WP is a valued, affordable and sustainable program that honours the inherent dignity of each patient.4
However, the transferability of this program to a community setting is uncertain and may be challenging, given a potentially less diverse multidisciplinary team of caregivers, fewer general house-staff to elicit and implement wishes and less available funding. In Canada, ICUs in community hospitals historically have not been as engaged in data collection for research and quality improvement, and many lack dedicated research staff.
The overall objective of this study was to evaluate the adaptability of the 3WP to a community hospital ICU, and to describe the patients cared for with this palliative approach and local program implementation strategies. By studying adaptability outside of academic centres, we assess whether this program can be successfully introduced and accepted, as judged by patient enrolment, staff participation and costs.
Methods
Setting and design
We implemented the 3WP between January 2017 and December 2019 in a level 3, 15-bed ICU at Brantford General Hospital, a community hospital in southern Ontario that is affiliated with McMaster University. The 3WP begins as a conversation that allows the bedside team to learn about the dying patient as a person, namely their interests, values and aspects of their life that are important to them.3–5 The team helps to elicit and facilitate individualized wishes made by patients and their families, with additional acts of compassion from clinicians representing additional wishes. We evaluated the program using descriptive analysis.
Participants
Adult patients (≥ 18 yr) were eligible to participate if their risk of death in the ICU was deemed to be 95% or greater by the attending physician, or if withdrawal of life-sustaining technology was planned. Eligibility was determined via discussions with the most responsible physician or if the patient and family had already decided on palliative comfort measures, as per discussions with bedside nursing staff. Patients were excluded if the death was sudden or precipitous, occurring too quickly to initiate the 3WP.
Program implementation
We introduced the program to the hospital ICU after a multidisciplinary reverse site visit to the originating institution, St. Joseph’s Healthcare Hamilton, followed by an on-site presentation at grand medical rounds. The original 3WP team facilitated a 1-day workshop that addressed the goals and genesis of the 3WP, sharing examples of common wishes and suggested strategies for project initiation. Launch of the 3WP in the ICU at Brantford General Hospital was accomplished through the initiative of the local physician lead, support of other intensivists, the ICU Nurse Manager, the Spiritual Care team and a research coordinator. The local 3WP team comprised the nurse manager (B.L.), research coordinator (W.D.) and local lead investigator (B.R.).
A brief step-by-step guide to the 3WP program is provided in Appendix 1, available at www.cmajopen.ca/content/9/3/E757/suppl/DC1. This tool guided clinical staff on the process and logistical steps to help organize the 3WP and integrate it into their care path. It shows the flow of activities for wish elicitation and facilitation. This guide was distributed during the initial multicentre evaluation,4 to provide direction on early conversations and introduce the 3WP to families.
Clinical staff and volunteers helped with data collection, communicated openly with families of dying patients, and created individualized keepsakes through direct discussions with patients and their loved ones. Various community members also participated, including a group who donated hand-knitted blankets. Once the program was clearly established, the hospital foundation offered ongoing support to purchase any needed supplies.
At semiannual retreats organized by the original project management office (B.R., W.D., D.J.C., F.C.), Brantford General staff and other local and international groups shared their data and experiences with each other; key activities included grand rounds (D.J.C., F.C., B.R.) on Sept. 20, 2017. Social media was instrumental in promoting this program, generating interest from local businesses, including a coffee shop that supplied a coffee maker with ongoing replenishment of coffees, teas and condiments. Families who used the program often donated supplies, such as books, toys, toiletries, tissues and rhythm strip vials (i.e., patient electrocardiogram strips inserted in glass vials as a keepsake for the family).
The costs of this 2-year program were covered primarily through donations, fundraising (W.D., B.R., B.L.) and grant support (D.J.C.). Grant funding was used exclusively for partial salary of the research coordinator, including 8 hours/week for the first 6 months and about 3 hours/week thereafter. Momentum was sustained by a successful in-hospital fundraiser (W.D., B.R., B.L.). Thereafter, occasional additional fundraising and numerous donations of consumables fuelled the clinical aspect of the program. We also created a periodic multidisciplinary staff newsletter about the 3WP (W.D., B.L.).
Outcomes
We selected outcomes in accordance with previous studies evaluating the 3WP.4 Outcomes for this study included the type, timing and cost of each wish, which person or service made and facilitated each wish, and if and why the wish was successfully facilitated or not. Costs of wishes included direct costs of items purchased and consumables, such as materials for creating wishes, but did not include personnel time or other indirect costs, such as overhead. We also assessed patient enrolment and overall staff participation.
Data collection
The clinical team or research coordinator abstracted patient information from electronic and paper-based medical records onto pretested case report forms from the original 3WP,4 including demographics, admitting diagnosis, comorbidities, advanced life supports (including those administered, withheld and withdrawn), clinical course (i.e., length of stay in the ICU, time and location of death), clinician engagement, allied health services involved and family member presence at the time of death.
We calculated the Acute Physiology and Chronic Health Evaluation (APACHE II) score6 using biochemical values (e.g., creatinine, electrolytes, white blood cell count) and clinical data (e.g., vitals, Glasgow Coma Scale score, oxygen requirements) retrieved from the patient’s medical chart. We did not abstract data in duplicate, given the clear nature of the data collected. No judgment was required. The research coordinator did, however, double-check the information recorded by bedside nurses, including information regarding implemented wishes and their cost. Although information was initially collected on paper for quick documentation (January 2017 to June 2017), this eventually moved to electronic medical records by bedside nurses, allowing for wishes to be recorded in real time. There was a 6-month interval between initiation of electronic record-keeping and paper documentation. The research coordinator collated the information from the case report forms and entered anonymized data using the encrypted software program REDCap.7
Statistical analysis
We performed all quantitative analyses using SAS Version 9.4. Descriptive statistics included means and standard deviations (SDs) for continuous variables, and absolute counts and percentages for categorical variables.
Ethics approval
This study was approved by the Brant Community Healthcare System Research Ethics Committee on Oct. 19, 2017. Approval for the original 3WP was under the Hamilton Integrated Research Ethics Board.3 This application was updated and approved in April 2017 to evaluate the 3WP.4 We used a waived consent model for quantitative data (i.e., basic characteristics and terminal wishes).
Results
We included 101 dying patients, with a mean age of 68.1 (SD 15.9) years; 56 (55.4%) were female (Table 1). Patients were predominantly White (n = 95, 94.1%); 5 (5.0%) patients were Indigenous. Patients generally presented directly to the ICU from the emergency department; 91 (90.1%) had medical admitting diagnoses, 7 (6.9%) had surgical conditions and 3 (3.0%) were admitted because of trauma. Life-support interventions were withdrawn immediately before death for all patients, including mechanical ventilation from 60 (59.4%) patients, and inotropes from 41 (40.6%) patients (Table 2). Throughout the dying period, patients received consultations from spiritual care (n = 38, 37.6%), palliative care (n = 16, 15.8%), social work (n = 53, 52.5%) and psychology (n = 1, 1.0%).
Table 1:
Patient baseline demographic characteristics
| Characteristic | No. (%) of patients* n = 101 |
|---|---|
| Age, yr, mean ± SD | 68.1 ± 15.9 |
| Sex, female | 56 (55.4) |
| Race | |
| White | 95 (94.1) |
| Indigenous | 5 (5.0) |
| Asian | 1 (1.0) |
| APACHE II score, mean ± SD | 24.9 ± 6.8 |
| Location before ICU | |
| Emergency department | 49 (48.5) |
| Hospital ward | 37 (36.6) |
| Operating room | 6 (5.9) |
| Other (inpatient rehabilitation ward) | 1 (1.0) |
| Other hospital (emergency department or ICU) | 8 (8.0) |
| ICU admitting diagnosis | |
| Cardiovascular or vascular | 20 (19.8) |
| Respiratory | 38 (37.6) |
| Gastrointestinal | 9 (8.9) |
| Neurologic | 10 (9.9) |
| Sepsis | 13 (12.9) |
| Other (e.g., trauma, metabolic) | 11 (11.0) |
| Admission category | |
| Medical | 91 (90.1) |
| Surgical | 7 (6.9) |
| Trauma | 3 (3.0) |
| Spiritual belief | |
| Anglican | 4 (4.0) |
| Baptist | 8 (7.9) |
| Buddhist | 1 (1.0) |
| Catholic | 14 (13.9) |
| Christian | 4 (4.0) |
| Eastern Orthodox | 1 (1.0) |
| Jehovah’s Witness | 1 (1.0) |
| Longhouse | 1 (1.0) |
| Lutheran | 2 (2.0) |
| Pentecostal | 1 (1.0) |
| Protestant | 7 (6.9) |
| United | 10 (9.9) |
| Unknown | 14 (13.9) |
| None indicated | 33 (32.7) |
Note: ICU = intensive care unit, SD = standard deviation.
Unless indicated otherwise.
Table 2:
Patient clinical course characteristics
| Characteristic | No. (%) of patients* n = 101 |
|---|---|
| Advanced life supports at any time in ICU | |
| Mechanical ventilation | 67 (66.3) |
| Inotropes | 65 (64.4) |
| Dialysis | 4 (4.0) |
| Advanced life supports withdrawn just before death | |
| Mechanical ventilation | 60 (59.4) |
| Inotropes | 41 (40.6) |
| Dialysis | 0 (0.0) |
| Consults | |
| Spiritual care | 38 (37.6) |
| Palliative care | 16 (15.8) |
| Social work | 53 (52.5) |
| Psychology | 1 (1.0) |
| Organ donation coordinator | 24 (23.8) |
| Consent for donation† | |
| Yes, donation after cardiac death | 3 (12.5) |
| Yes, donation after neurologic death | 2 (8.3) |
| No donation made | 7 (29.2) |
| Patient ineligible for organ donation | 12 (50.0) |
| Patient death in hospital | |
| Yes | 98 (97.0) |
| No | 2 (2.0) |
| Still in palliative unit | 1 (1.0) |
| Enrolment in 3WP initiated by | |
| Principal investigator | 8 (7.9) |
| 3WP team | 5 (5.0) |
| Bedside nurse | 76 (75.2) |
| Spiritual care | 1 (1.0) |
| ICU attending physician | 4 (4.0) |
| Other | 7 (6.9) |
| Days from hospital admission to ICU admission, median (IQR) | 0 (0–3) |
| Days from ICU admission to death, median (IQR)‡ | 6 (3–10) |
| Days from hospital admission to death, median (IQR) | 9 (4–16) |
| Days from ICU admission to enrolment in 3WP, median (IQR) | 5 (2–9) |
| Days from enrolment in 3WP to death, median (IQR)‡ | 1 (0–1) |
Note: 3WP = 3 Wishes Project, ICU = intensive care unit, IQR = interquartile range.
Unless indicated otherwise.
Of 24 patients with a consult from organ donation coordinator.
For patients who did not die in hospital, the date of intensive care unit discharge was used to calculate days from hospital admission to death, days from intensive care unit admission to death, and days from enrolment in 3 Wishes to death.
The median length of stay in the ICU was 6 (interquartile range [IQR] 3–10) days. Enrolment in the 3WP was most often toward the end of ICU admission, with a median of 5 (IQR 2–9) days from ICU admission to enrolment in 3WP. Patients were introduced to the 3WP primarily by bedside nurses (n = 76, 75.2%); the 3WP team (local lead investigator, research coordinator and nurse manager), other ICU physicians and the spiritual care team also introduced patients to the program. Of 101 patients, 98 (97.0%) died in hospital, with 78 (79.6%) dying in the ICU; a designated palliative care bed was secured for 11 (11.2%) patients. At the time of death, 87 (88.8%) patients had family or friends present at the bedside. Of 12 patients deemed eligible for organ donation, organ donation was realized for 5 patients, including 3 after cardiac death and 2 after neurologic death.
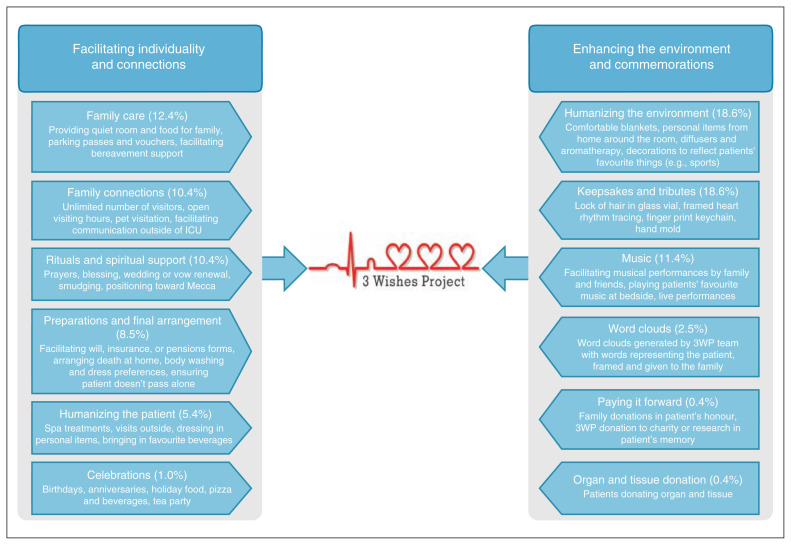
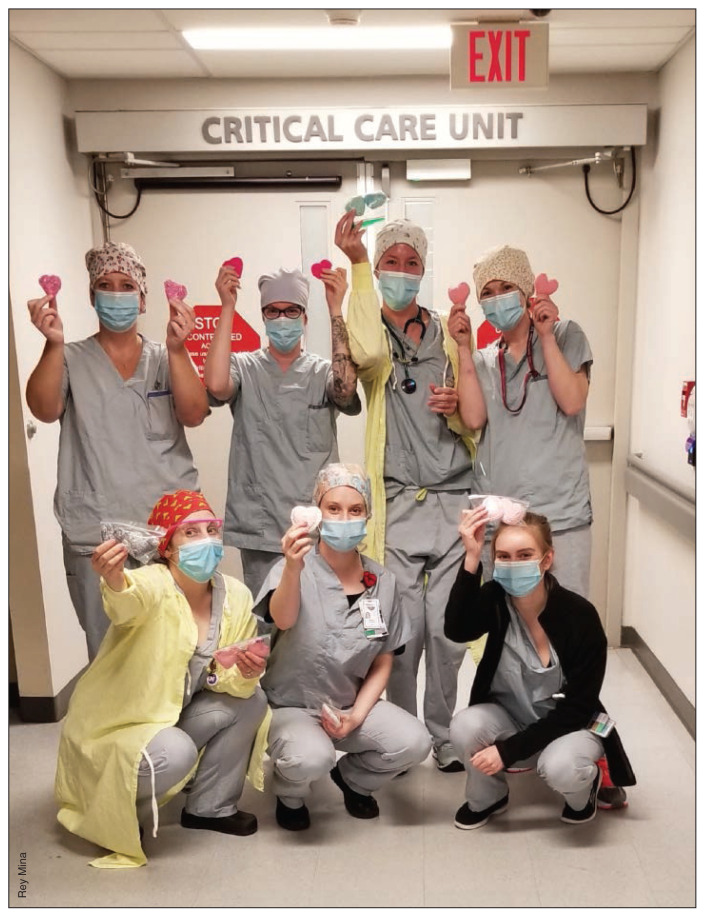
Description of wishes
Overall, a mean of 4.7 (SD 1.6) terminal wishes were facilitated for each patient (total range of 3–11 wishes/patient). The 479 total terminal wishes facilitated in this study represented a 99.2% completion rate; only 4 were not realized because of logistical or medical reasons (Table 3). Facilitated wishes represented each of the wish categories described in the original 3WP study (Figure 1). Humanizing the environment included decorating a patient’s room with memorabilia, such as emblems of the patient’s birthplace region. Celebrations included a New Year’s cheer, and arranging for an antique car show outside a patient’s hospital window. Spiritual wishes included smudge ceremonies, a cedar bath, last rites, a wedding and bedside baptism. Keepsakes included paired crochet hearts, one to pin on a patient’s chest and an identical heart as a family memento (Figure 2); another involved arranging a bedside ultrasound of a patient’s partner to visualize their unborn child. Music included playing the patient’s favourite songs on tablets or phones, and live performances with family and friends. For family connections, unlimited visiting hours and pet visits were arranged.
Table 3:
Summary of wishes from the 3 Wishes Project
| Characteristic | No. (%) of wishes n = 483 |
|---|---|
| Wish category | |
| Family care | 60 (12.4) |
| Family connections | 50 (10.4) |
| Rituals and spiritual support | 50 (10.4) |
| Preparations and final arrangements | 41 (8.5) |
| Humanizing the patient | 26 (5.4) |
| Celebrations | 5 (1.0) |
| Humanizing the environment | 90 (18.6) |
| Keepsakes and tributes | 90 (18.6) |
| Music | 55 (11.4) |
| Word clouds | 12 (2.5) |
| Paying it forward | 2 (0.4) |
| Organ and tissue donation | 2 (0.4) |
| Who made the wish* | |
| Patient | 30 (6.2) |
| Family | 236 (48.9) |
| Intensive care unit | 238 (49.3) |
| 3WP team | 0 (0.0) |
| Other (friends, Trillium Gift of Life Network staff, research staff) | 14 (2.9) |
| Wish made | |
| Antemortem | 472 (97.7) |
| Postmortem | 11 (2.3) |
| Wish elicited by* | |
| Patient | 7 (1.4) |
| Family | 103 (21.3) |
| Intensive care unit | 363 (75.2) |
| 3WP team | 17 (3.5) |
| Other (chaplain, friends, Trillium Gift of Life Network staff research staff) | 13 (2.7) |
| Wish completed | |
| Yes | 479 (99.2) |
| No | 4 (0.8) |
More than 1 option can be chosen for a single wish; therefore, total is more than 100%.
Figure 1:
Visual pictograph outlining wish categories from the 3 Wishes Project (3WP), with a summary of examples. The percentages reported reflect the representation of wish categories among the 483 wishes documented during the study period. Note: ICU = intensive care unit. Categories were generated from a qualitative analysis during the original implementation of the 3 Wishes Project at St. Joseph’s Healthcare Hamilton.
Figure 2:
Community volunteers created pairs of crochet hearts, one to pin on a patient’s chest and an identical heart for a family memento, as shown by bedside nurses. Top, left to right: Amy Warwick RN, Karyn Way RN, Danielle DeVries RN, Stephanie Ackland RN. Bottom, left to right: Alyssa Forler RN, Marin de Beer RN, Kara Jonas RN.
Image courtesy of Rey Mina
Most wishes were elicited while patients were still alive (97.7%, 472 wishes), with only 2.3% (11 wishes) elicited in the postmortem period by families and friends. The ICU team elicited most wishes (n = 363 wishes, 75.2%), followed by family members (n = 103, 21.3%) and the 3WP team (n = 17, 3.5%). Wishes made directly by patients accounted for only 6.2% of wishes (n = 30), reflecting their critical illness; thus, family members and ICU staff wished for 238 (48.9%) and 236 (49.3%) wishes, respectively.
The mean cost per wish was $1.14 (SD $10.41); notably, 430 (89.8%) of the 483 wishes elicited were at no cost to the program. The total cost of all 479 wishes facilitated for 101 patients was estimated to be $5.39 per patient (SD $22.40).
Local program implementation
Over the study period, all physicians and nurses, as well as other staff designated to the ICU (i.e., spiritual care clinicians, social workers, recreational therapists, pharmacists and dietitians) became aware of the 3WP. We estimate that 70%–80% of the staff were personally involved in either eliciting or implementing a terminal wish. Staff reported that the step-by-step guide to implementing the 3WP was instrumental in its sustained uptake.
Interpretation
In this study, we documented successful implementation of the 3WP in the ICU of a community hospital. The program helped to realize 99% of 483 terminal wishes in 101 dying, critically ill patients. Our findings illustrate how interprofessional clinicians can work synergistically to provide compassionate, individualized care for dying patients, including those who may have difficulty advocating for themselves.
On average, 5 terminal wishes per patient were facilitated. In this study, staff were more often involved than in the original 3WP report,4 accounting for close to half of the wishes made, in contrast to the 5% of wishes made by staff as reported in the original 3WP multisite program evaluation. 4 Despite a similar proportion of about 90% of patients dying with family or close friends at the bedside in this community hospital and in the recent multicentre evaluation,4 the high proportion of wishes facilitated by ICU clinicians in this study reflects strong staff engagement.
Bedside nurses were not only responsible for enrolling 75% of patients, but they also facilitated 75% of the wishes, reflecting strong patient advocacy. Acknowledging that the provision of compassionate end-of-life care and facilitation of terminal wishes is not novel to nursing care, the formalization of this process through the 3WP helped to create norms, whereby compassionate acts are prevalent, approached with the means and structure to enable more consistent implementation. The 3WP emerged as a successful, nurse-championed hospital initiative, similar to rapid response critical care teams,8,9 smoking cessation clinics,10 diabetes education11 and hospital admission avoidance initiatives for older adults.12 Many nursing-led projects are cost-effective,11 are sustainable8 and favourably affect organizational culture, promoting effective communication between teams and patients.13
Although patients in this study appear to be less racially diverse than in the multicentre report, (94.1% v. 70.0% White), there was greater representation of Indigenous people (5.0% v. 2.7%).4 The uptake of a palliative care program among First Nations communities is important, considering barriers to end-of-life care, such as isolation from families, limited access to public transportation, and cultural insensitivity to optimal end-of-life care for First Nations people.14 Trauma-informed care requires acknowledgement of the historic effects of colonialism, including organization-level discrimination and intergenerational trauma.14 It aims to prevent the perpetuation of discriminatory care stemming from Western misconceptions about First Nations culture.14,15 Wishes elicited from patients and families in this study aligned with trauma-informed care, fostering relationships with clinicians in the wish generation process. Moreover, the 3WP is a primarily patient- and family-led initiative, promoting the unique and culturally informed needs of all dying patients.
Beyond the favourable influence that the 3WP has for patients, family members and health care professionals,5 this study shows strong engagement of a community hospital in a combined clinical and research project. Community centres deliver most health care in Canada, accounting for 80% of the inpatient beds in Ontario, and 49%–100% in other provinces.16 However, community centres are typically underrepresented in research generation,17 as most studies are designed and tested exclusively in academic settings.18 Previous work suggested that hospitals participating in research have improved outcomes for patients compared to hospitals that do not participate, 18 including increased adherence to guidelines,19 higher nursing and physician satisfaction, and better employee retention.20 Anticipating the barriers to research in the community setting, such as the delivery-focused model of care and their relatively fewer resources compared with academic centres, 17 we documented successful uptake of the 3WP, strong staff partnership and program sustainability beyond the research period. Our findings align with a perceived paradigm shift to increased research participation and academic contributions from community hospitals.17,18,21
Our work has shown the 3WP to function as a successfully and well-received, compassionate end-of-life program. Specifically, we showed that the program tapped into a desire for families to demonstrably honour the passing of loved ones, which may not have been realized before the invitation was given in the form of this program. The 3WP was a vehicle for enhanced recognition of each patient’s inherent dignity, and a means to show compassion for patients and families while also individualizing care. Strengths include the realization of nearly all terminal wishes, achieving personalized, affordable, end-of-life interventions in this setting. Other differences from the original study3 and multicentre evaluation4 include nursing-led project implementation and early support from community agencies in our study.
Limitations
This study lacks qualitative interviews of patients, families and clinicians to draw on their experiences, which could have informed our understanding of the drivers of successful uptake of the 3WP and potential challenges to address. We did not perform duplicate data collection and entry for this study, so cannot exclude the possibility of mistakes, but these data are generally clear and not prone to error. We did not seek important measures of end-of-life quality in this study. Direct costs included only actual costs of wishes, not including costs of donated items.
Conclusion
The 3 Wishes Project is a patient- and family-centred palliative care initiative, successfully adapted to this community hospital at relatively low cost. The lack of strict protocolization and personalized design of this intervention underscores its inherent flexibility, with the potential to promote individualized end-of-life care in nonacademic hospital wards, homes or hospice. For consideration in other rural or remote venues, participatory research and more intentional cultural adaptation are needed.
Appendix
Acknowledgements
The authors thank the patients and their loved ones for whom they had the honour of caring. The authors are grateful to the bedside nurses in the Critical Care Unit of the Brantford General Hospital, in addition to the physicians and other multidisciplinary colleagues who were instrumental in initiating and sustaining this program, including Ms. Tomoko Okomura (representing music therapy, Ms. Rachel Brown (representing recreation therapy), the Brant Community Healthcare System Foundation (led by Ms. Kari Wilson) and Mr. Tim Staffen, who manages the Tim Hortons. Additional leadership from ICU nurses, Ms. Laura Roth and Ms. Marin de Beer, and from Dr. Anna Rozenberg has been invaluable. The authors thank colleagues from the 3 Wishes Network for their assistance, especially the spiritual care clinician, Ms. Feli Toledo.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Brenda Reeve, William Dechert, Barbara Longo, France Clarke, John Arthur and Deborah Cook contributed to the conception and design of the work. William Dechert collected data, which all of the authors interpreted. Brenda Reeve and Brittany Dennis drafted the manuscript, and all authors revised it critically for important intellectual content, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Funding: The research component was supported by the Canadian Institutes for Health Research (Foundation Grant 143243, Deborah Cook), which had no role in study design and conduct of the study, data collection, management, analysis, interpretation, or the preparation, review, or approval of the manuscript.
Data sharing: Summary data that support the findings of this study are available on request from the corresponding author. Individual patient data are not publicly available due to the identifying nature of some of the wishes.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/9/3/E757/suppl/DC1.
References
- 1.Anderson I. Indigenous perspectives on death and dying. Toronto: University of Toronto; 2020. [Google Scholar]
- 2.Menec VH, Nowicki SKA. Transfers to acute care hospitals at the end of life: do rural/remote regions differ from urban regions? [accessed 2017 June 1];Rural Remote Health. 2010 10:1281. Available: https://www.rrh.org.au/journal/article/1281. [PubMed] [Google Scholar]
- 3.Cook D, Swinton M, Toledo F, et al. Personalizing death in the intensive care unit: the 3 wishes project a mixed-methods study. Ann Intern Med. 2015;163:271–9. doi: 10.7326/M15-0502. [DOI] [PubMed] [Google Scholar]
- 4.Vanstone M, Neville TH, Clarke FJ, et al. Compassionate end-of-life care: mixed-methods multisite evaluation of the 3 wishes project. Ann Intern Med. 2020;172:1–11. doi: 10.7326/M19-2438. [DOI] [PubMed] [Google Scholar]
- 5.Neville TH, Agarwal N, Swinton M, et al. Improving end-of-life care in the intensive care unit: clinicians’ experiences with the 3 Wishes Project. J Palliat Med. 2019;22:1561–7. doi: 10.1089/jpm.2019.0135. [DOI] [PubMed] [Google Scholar]
- 6.Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 7.REDCap. Research Electronic Data Capture. Nashville: Vanderbilt University; 2004. [Google Scholar]
- 8.Mitchell A, Schatz M, Francis H. Designing a critical care nurse-led rapid response team using only available resources: 6 years later. Crit Care Nurse. 2014;34:41–55. doi: 10.4037/ccn2014412. quiz 56. [DOI] [PubMed] [Google Scholar]
- 9.McNeill MM, Archer S, Remsburg D, et al. Rapid response team-quality champion registered nurse: observations and perceptions. J Nurs Care Qual. 2019;34:325–9. doi: 10.1097/NCQ.0000000000000393. [DOI] [PubMed] [Google Scholar]
- 10.Byers MA, Wright P, Tilford JM, et al. Comparing smoking cessation outcomes in nurse-led and physician-led primary care visits. J Nurs Care Qual. 2018;33:272–8. doi: 10.1097/NCQ.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 11.Wilson M, Chen HS, Wood M. Impact of nurse champion on quality of care and outcomes in type 2 diabetes patients. Int J Evid-Based Healthc. 2019;17:3–13. doi: 10.1097/XEB.0000000000000156. [DOI] [PubMed] [Google Scholar]
- 12.Marsden E, Craswell A, Taylor A, et al. Nurse-led multidisciplinary initiatives to improve outcomes and reduce hospital admissions for older adults: The Care coordination through Emergency Department, Residential Aged Care and Primary Health Collaboration project. Australas J Ageing. 2018;37:135–9. doi: 10.1111/ajag.12526. [DOI] [PubMed] [Google Scholar]
- 13.Leach LS, Mayo AM. Rapid response teams: qualitative analysis of their effectiveness. Am J Crit Care. 2013;22:198–210. doi: 10.4037/ajcc2013990. [DOI] [PubMed] [Google Scholar]
- 14.Russell B, Fred DE, Brown C. Culturally safe end-of-life care for First Nations persons living on reserve. Rural Remote Health. 2018;18:4500. doi: 10.22605/RRH4500. [DOI] [PubMed] [Google Scholar]
- 15.Kelley ML, Prince H, Nadin S, et al. Developing palliative care programs in indigenous communities using participatory action research: a Canadian application of the public health approach to palliative care. Ann Palliat Med. 2018;7(Suppl 2):S52–S72. doi: 10.21037/apm.2018.03.06. [DOI] [PubMed] [Google Scholar]
- 16.Number of hospital beds staffed and in operation, 2016–2017. Ottawa: Canadian Institute for Health Information; 2018. [accessed 2020 Sept. 14]. Available: www.cihi.ca/en/access-data-reports/results?query=Hospital+Beds+Staffed+and+In+Operation%2C+2016-2017&Search+Submit= [Google Scholar]
- 17.Gehrke P, Binnie A, Chan SPT, et al. Fostering community hospital research. CMAJ. 2019;191:E962–6. doi: 10.1503/cmaj.190055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DiDiodato G, Didiodato JA, McKee AS. The research activities of Ontario’s large community acute care hospitals: a scoping review. BMC Health Serv Res. 2017;17:566. doi: 10.1186/s12913-017-2517-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luetz A, Balzer F, Radtke FM, et al. Delirium, sedation and analgesia in the intensive care unit: a multinational, two-part survey among intensivists. PLoS One. 2014;9:e110935. doi: 10.1371/journal.pone.0110935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hacker K, Bhuiya N, Pernice J, et al. Assessing research interest and capacity in community health centers. Clin Transl Sci. 2013;6:391–7. doi: 10.1111/cts.12046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Likumahuwa S, Song H, Singal R, et al. Building research infrastructure in community health centers: a Community Health Applied Research Network (CHARN) report. J Am Board Fam Med. 2013;26:579–87. doi: 10.3122/jabfm.2013.05.130025. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.