Abstract
In this commentary, we present the premise that, in Canada, mental illness research specific to eating disorders is underfunded, and many Canadians are suffering the consequences of this underinvestment. We highlight three critical aspects of eating disorders: 1) the increasingly common yet potentially life-threatening nature of eating disorders, with an onset usually during adolescence; 2) the challenges and costs to treating eating disorders, with a discussion of current hospital-related costs across Canada; and 3) the glaring discrepancy between the money spent on eating disorder diagnoses/treatment and the funding dollars granted for eating disorder research in Canada (i.e. only $0.70 per affected Canadian in 2018). Research funding per affected individual for other psychiatric and neurodevelopmental conditions are used as comparisons (e.g. $50.17 per affected Canadian with schizophrenia). We suggest that it is time to revolutionize treatment for individuals with eating disorders and use our resources in a more efficient and effective manner, using current neuroimaging and neuromodulation methods as promising examples. We conclude by emphasizing the need for increased research funding in the field of eating disorders in Canada, as the current research-related investments hinder progress in developing neuroscientifically-sound treatments for these populations.
Keywords: anorexia nervosa, eating disorders, healthcare costs, research funding
Résumé
Dans ce commentaire, nous présentons la prémisse selon laquelle, au Canada, la recherche en maladie mentale propre aux troubles alimentaires est sous-financée, et nombre de Canadiens souffrent des conséquences de ce sous-investissement. Nous soulignons trois aspects essentiels des troubles alimentaires: 1) la nature de plus en plus répandue et pourtant potentiellement mortelle des troubles alimentaires, qui débutent habituellement à l’adolescence; 2) les défis et les frais de traiter les troubles alimentaires, et une présentation des coûts actuels en milieu hospitalier au Canada; et 3) l’écart flagrant entre les sommes dépensées pour le traitement/diagnostic des troubles alimentaires et le financement accordé à la recherche sur les troubles alimentaires au Canada (c.-à-d., seulement 0,70 $ par Canadien touché en 2018). Le financement de la recherche par personne touchée par d’autres troubles psychiatriques et neurodéveloppementaux sert de comparaison (p. ex., 50,17$ par Canadien touché par la schizophrénie). Nous suggérons qu’il est temps de révolutionner le traitement pour les personnes souffrant de troubles alimentaires et d’utiliser nos ressources de façon plus efficiente et efficace, en nous servant de la neuroimagerie actuelle et des méthodes de neuromodulation, soit des exemples prometteurs. Nous concluons en mettant l’accent sur le besoin d’un financement accru de la recherche dans le domaine des troubles alimentaires au Canada, car les investissements actuels dans la recherche freinent le progrès du développement de traitements neuroscientifiquement efficaces pour ces populations.
Mots clés: anorexie mentale, troubles alimentaires, coûts des soins de santé, financement de la recherche
Here, we will present the premise that, in Canada, mental illness research specific to eating disorders is underfunded, and many Canadian youth, families and communities are suffering the consequences of this underinvestment.
First, eating disorders are common and potentially life threatening. It is estimated that more than 1.7 million Canadians suffer from an eating disorder at any given time (Galmiche et al., 2019). A large majority of these individuals are female adolescents and emerging adults, with most first-time cases occurring before the age of 25 (Volpe et al., 2016; Ward et al., 2019). If not treated early, eating disorders persist into/throughout adulthood (e.g., in approximately 33% of anorexia and bulimia nervosa patients in a 22-year follow-up study; (Eddy et al., 2017)), and often have long-term physical and psychological consequences (Keski-Rahkonen & Mustelin, 2016; O’Brien et al., 2017; Vall & Wade, 2015). Anorexia nervosa (AN), for example, is one of the deadliest psychiatric conditions (Arcelus et al., 2011), with a standardized mortality ratio of 5.86 (across all age groups) compared to a reference group. Among deaths among individuals with AN, an estimated 1 in 5 were the result of suicide (Arcelus et a., 2011). There is a relationship between the standardized mortality ratio and age of diagnosis, with a ratio of 10 for persons diagnosed between the ages of 15 and 19 and a ratio of 18, if diagnosed between the ages of 20–29 (Arcelus et al., 2011). Standardized mortality ratios for other common eating disorders follow closely, such as bulimia nervosa at 1.93 and eating disorder – not otherwise specified at 1.92 (Arcelus et al., 2011). In Canada, it is estimated that approximately 1000 – 1500 individuals die from AN or bulimia nervosa each year (Woodside, 2013). This is not considering other eating disorders, or deaths due to secondary complications of an eating disorder.
Second, eating disorders are challenging and costly to treat. Response and remission rates to current treatment approaches for eating disorders is only approximately 50% (Hughes et al., 2019), with 50% of cases becoming severe and enduring (Treasure et al., 2015). Annually, eating disorder diagnoses and treatments are a costly endeavor for Canada. For context, in 2017/2018, Canada spent an average of $24,017 per individual affected with an eating disorder, 1.79 times more than what was spent on schizophrenia (Canadian Institute of Health Information, 2020). These costs were specific only to hospital services. In the same year, the average length of stay in a hospital for someone with an eating disorder was 33.5 days. In Alberta alone (where our research teams resides), $14 million per year is spent on treating and diagnosing eating disorders (Alberta Health Services, 2017). Nearly 50% (~$6.5 million) of that total is towards pediatric cases (<18 years of age)(Alberta Health Services, 2017). In Ontario, the average cost per patient (across all age groups, 5 – 65+ years old) was $10,022 in 2012 (de Oliveira et al., 2017). In the same dataset, for pediatric cases only (5–19 years), the average cost per patient was $19,857, nearly three times that of an adult 20–39 years old (de Oliveira et al., 2017). These costs have only increased in recent years (e.g. $21,128 in 2017–2018; Canadian Institute of Health Information, 2020). Using British Columbia as a final example, a 2003 study estimated long-term disability costs for a person with Anorexia nervosa in the province could range from $2.5 million to $101.7 million (calculated using a senstivity analysis; Su & Birmingham, 2003). Notably, where a patient fit within this large range was estimated based on the duration of their current illness, their gender, which provincial disability benefit level they qualified for, their insurance provider, and the number of years of long-term disability required. Importantly, the current costs of eating disorder in Canada are calculated based on diagnosed cases of eating disorders; the indirect costs of sub-clinical and undiagnosed cases are crucial to consider as well. For example, costs related to hospital stays for reasons related to diagnosed co-morbidities, visits to the clinic that resulted in a missed diagnosis, or even lost workdays and decreased productivity in the workplace in those suffering in silence (Trautmann et al., 2016).
Third, the money spent on research into eating disorders at a federal level does not reflect its impact on society. While millions are being spent on eating disorder diagnoses and treatment every year in Canada, the amount spent on research dollars for eating disorders is much more underwhelming. In 2019, the Canadian Institutes of Health Research (CIHR) support for eating disorder research equated to approximately $0.61 research dollars spent per affected individual, taking a conservative estimate of 1.7 million Canadians with a diagnosed eating disorder. In 2018, it was $0.59 per affected individual. Social Sciences and Humanities Research Council of Canada (SSHRC) support for eating disorder research in that same year equated to approximately $0.11 per affected individual (2019 numbers have not yet been made public). Averaged from 2014–2019, SSHRC support was $0.08 per affected individual. CIHR research funding averaged over the past 5 years was $0.65 per affected individual. Total CIHR funding in 2019–2020 for projects (that included “eating disorder” as a key word) equated to $1,065,131. These numbers are in stark contrast to the funding provided for other psychiatric or neurodevelopment disorders that year, such as schizophrenia ($16,926,811; approximately $47.01 per affected individual) and bipolar disorder ($4,245,604; approximately $7.78 per affected individual), and autism ($20,168,663; approximately $53.22 per affected individual). Total SSHRC funding for 2019–2020 have not yet been made public but see table 1 for total funding from 2014–2019 for each aforementioned disorder. Murray, Pila, Griffiths, and Le Grange (2017) observed that research dollar funding for eating disorders in the United States was $0.73 USD per affected individual. Reasons for these low funding rates are not known. We hypothesize that they could be due to several (non-mutually exclusive) factors, such as 1) gender biases (i.e. biases towards women, who are often disproportionately affected by (certain) eating disorders compared to men (Hoek, 2006; Smink et al., 2012), alongside male biases in the perception of eating disorder severity (Mond & Arrighi, 2011)), 2) priorities on who is available to review (fewer researchers in the field mean fewer expert reviewers for funding applications), 3) the chronic and obstinate nature of eating disorders (limited progress in treatment leads to limited funding and vice versa), and 4) implicit biases in perception (i.e. the perception that eating disorders are not “real” disorders) combined with lack of education on the factors that contribute to eating disorders (Blodgett Salafia et al., 2015; Mond & Hay, 2008). Thus, whether low funding rates for eating disorder research are attributable to these reasons would be an interesting area for future research.
Table 1.
Canadian research funding for specified psychiatric and neurodevelopmental disorders (2014–2019)
| Funding agency | Year | Eating disorders | Schizophrenia | Bipolar disorder | Autism |
|---|---|---|---|---|---|
| CIHR | 2014 | $764,559 | $16,045,050 | $2,925,917 | $12,096,982 |
| 2015 | $1,161,122 | $14,774,889 | $2,555,932 | $15,237,926 | |
| 2016 | $1,589,391 | $15,089,923 | $3,162,220 | $18,936,469 | |
| 2017 | $790,031 | $16,310,910 | $3,043,827 | $15,176,843 | |
| 2018 | $1,024,224 | $17,848,051 | $3,994,919 | $18,889,692 | |
| 2019 | $1,065,131 | $16,926,811 | $4,245,604 | $20,168,663 | |
|
| |||||
| SSHRC | 2014 | $90,000 | $0 | $0 | $629,445 |
| 2015 | $107,500 | $17,500 | $35,000 | $593,836 | |
| 2016 | $105,000 | $52,500 | $35,000 | $1,699,272 | |
| 2017 | $172,500 | $70,000 | $35,000 | $2,008,386 | |
| 2018 | $195,000 | $212,500 | $0 | $2,829,176 | |
| 2019 | N/A | N/A | N/A | N/A | |
|
| |||||
| CIHR + SSHRC | Total (2014–2018) | $5,999,327.00 | $80,421,323.00 | $15,787,815.00 | $88,098,027.00 |
| Average/year | $1,199,865.40 | $16,084,264.60 | $3,157,563.00 | $17,619,605.40 | |
Note. Total funding was obtained from the CIHR and SSHRC’s public databases (2014–2019). Projects that included the name of the specific disorder (e.g. “eating disorder(s)” or “schizophrenia”) as a keyword or within the title of the funded project were included.
N/A: Not Available.
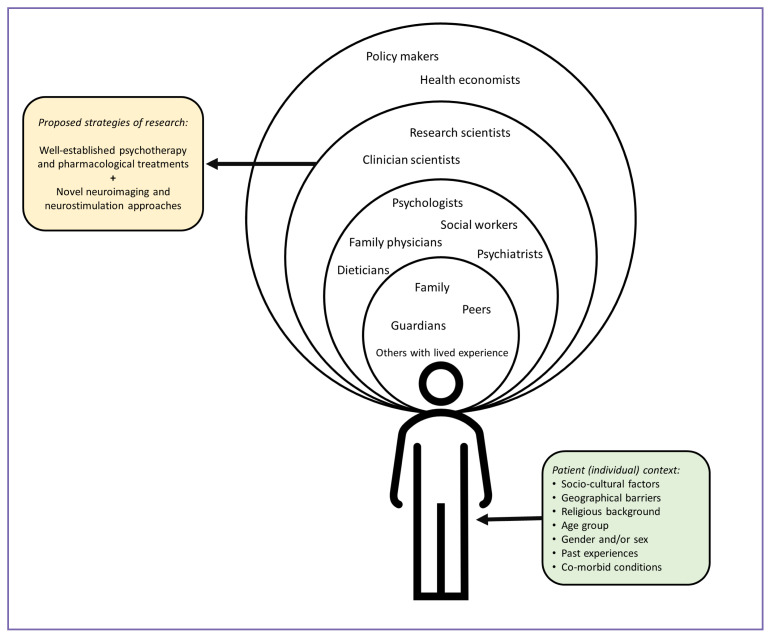
The combination of these factors with an urgent need for further research in this space presents an opportunity for the creation of collaborative groups across Canada (and internationally) focused on eating disorder research and treatment. It is time to revolutionize treatment for individuals with eating disorders and use our resources in a more efficient and effective manner, considering the individual’s immediate and extended support systems, as well as cultural, environmental, and social factors. Our suggestion is for the creation of a key stakeholder research group that brings together policy makers, providers, researchers from different fields, people with lived experience, and caregivers. We would like representation from key informants and stakeholders to ensure that there is an opportunity to generate new ideas for addressing the genetic to clinical issues. See figure 1 for a depiction of this.
Figure 1.
Multifaceted approach to supporting eating disorder patients. Graphic depiction of a multifaceted approach to better support the patient and advance our understanding of eating disorders. Proposed teams are included in each bubble. The innermost bubble depicts the patient’s immediate contacts and support system. Remaining bubbles include supports that move from more direct to indirect connections with the patient. Ideally, teams from different bubbles will work together.
Current (common and well-established) treatments for eating disorders involve psychotherapies and/or medications. For example, family-based treatment (or FBT) is the most effective treatment available for adolescents with anorexia nervosa. FBT is a form of therapy wherein the parents/caregivers play a central role in the recovery process, and has been shown to be superior to individual therapy, particularly at 6–12 months posttreatment (Couturier et al., 2013; Lock et al., 2010). Aligned with this, FBT is strongly recommended by the recently developed Canadian practice guidelines for the treatment of children and adolescents with eating disorders (Couturier et al., 2020). However, clinical response rates to any one therapy (e.g., FBT with response rates of ~35–50%; (Hughes et al., 2019; Le Grange et al., 2014)) or cognitive behavioural therapy for adolescents with bulimia nervosa (Schmidt et al., 2007)), or medication alone are not 100%. How can we better improve response rates to current treatment approaches, such as FBT? Undoubtedly, novel work in multiple directions is needed.
Aligned with this, we know that methods in neuroscience and psychiatry have improved substantially in the past 20 years. For example, transcranial magnetic stimulation is a form of non-invasive brain stimulation that can change brain activity and function in parts of the brain (Klomjai et al., 2015). There is evidence for its effectiveness in individuals with treatment-resistant Major depressive disorder (Gaynes et al., 2014; McClintock et al., 2018) and is a promising treatment for many other psychiatric and neurodevelopmental disorders (Cirillo et al., 2019; Hsu et al., 2018; Lusicic et al., 2018). Thus, combining neuroimaging techniques (like magnetic resonance imaging and spectroscopy) with neurostimulation paradigms could transform our understanding of eating disorders. Such investigations are emerging in the field of eating disorders (Jáuregui-Lobera & Martínez-Quiñones, 2018; Van Den Eynde & Guillaume, 2013), but these investigations, particularly in Canada, are still limited, and perhaps not yet well enough supported by the evidence. We therefore could focus our efforts on funding research that combines current and well-established therapies, such as family-based treatment (Couturier et al., 2013; Doyle et al., 2010; Lock et al., 2010), with novel neurostimulation and neuroimaging techniques to potentially accelerate clinical response. Such opportunities will allow us to refine and strengthen current approaches, while also advancing our understanding of novel therapies. Ultimately, this could lead to the development of personalized treatment plans for individuals with eating disorders.
Thus, with increased funding opportunities, Canada could be at the forefront for uncovering these (still unknown) mechanisms that underlie eating disorders, and in the advancements of tailoring treatment approaches accordingly. Overall, it could better revolutionize care for the affected individuals, and their families alike. A recent Canada-wide survey on research priorities for eating disorders revealed that the top need was effective treatment options, including a better understanding of the biology of eating disorders and predictive elements of treatment (Obeid et al., 2020). Unfortunately, the current research-related investments hinder progress in that domain. The breakdown of these research-related investments by major granting agencies in Canada, by factors such as the age of the research population being studied (i.e., pediatric, young adults, older adults), is not readily available in the public datasets as they exist. Moreover, these granting agencies do not routinely (or publicly) publish which proposed projects do not receive funding each year. These pose limitations to the interpretation of this dissonance between research funding and healthcare utilization costs. As a call to action, we suggest these agencies publish aggregate data (as not to identify individual/team applicants) on the number of applications submitted to the granting agency, organized by funding status, proposed medical condition, and population type (e.g., age).
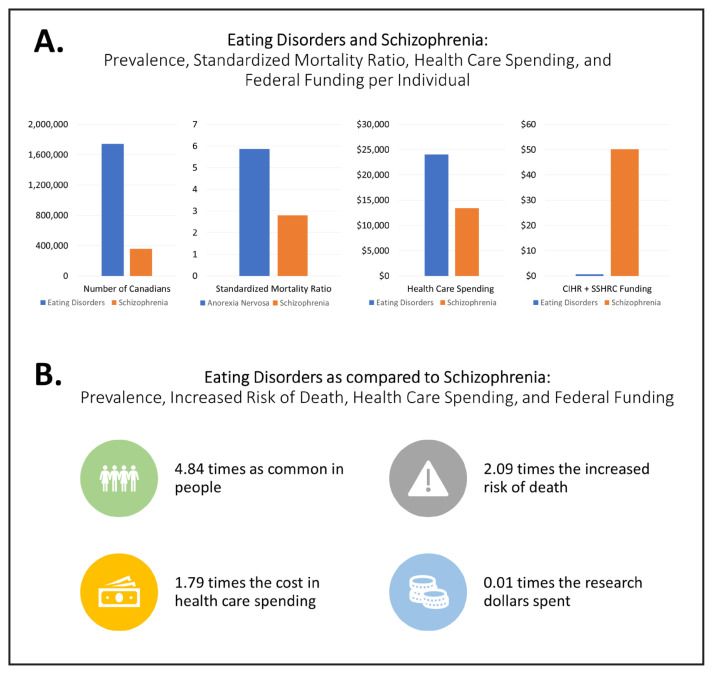
In conclusion, by every measure, the cost to society, impact on the individual, and risk of death from eating disorders is on par with serious mental illnesses like schizophrenia, but the level of research investment pales in comparison (see figure 2). So, we must ask ourselves: what is lost when we consider the current cost of eating disorders?
Figure 2.
A) Eating Disorders and Schizophrenia: Prevalence, Standardized Mortality Ratio, Health Care Spending, and Federal Funding. From left to right, bar graphs depicting prevalence, increased risk of death (standardized mortality ratio), health care spending per individual (hospital costs, calculated by CIHI 2017–2018), and CIHR plus SSHRC funding dollars per affected individual in 2018–2019. Blue bars represent eating disorders (or anorexia nervosa in second graph from left); orange bars represent schizophrenia B) Eating disorders as compared to schizophrenia. Visualization of the increased prevalence, risk of death, health care spending, as well as the proportion of research dollars spent on eating disorders compared to schizophrenia.
Footnotes
Conflicts of Interest
The authors declare that they have no conflicts of interest to disclose.
Funding Source
Behavior and the Developing Brain Seed Grant with the Alberta Children’s Hospital Research Institute
References
- Alberta Health Services. Alberta Visit Rates, Diagnosis Rates, and Costs. Alberta Health Services; 2017. https://www.albertahealthservices.ca/about/Page13342.aspx. [Google Scholar]
- Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Archives of General Psychiatry. 2011;68(7):724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- Blodgett Salafia EH, Jones ME, Haugen EC, Schaefer MK. Perceptions of the causes of eating disorders: a comparison of individuals with and without eating disorders. Journal of Eating Disorders. 2015;3(1):32. doi: 10.1186/s40337-015-0069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Institute of Health Information. Patient Cost Estimator. 2020. https://www.cihi.ca/en/patient-cost-estimator.
- Cirillo P, Gold AK, Nardi AE, Ornelas AC, Nierenberg AA, Camprodon J, Kinrys G. Transcranial magnetic stimulation in anxiety and trauma-related disorders: A systematic review and meta-analysis. Brain and Behavior. 2019. p. e01284. [DOI] [PMC free article] [PubMed]
- Couturier J, Isserlin L, Norris M, Spettigue W, Brouwers M, Kimber M, McVey G, Webb C, Findlay S, Bhatnagar N, Snelgrove N, Ritsma A, Preskow W, Miller C, Coelho J, Boachie A, Steinegger C, Loewen R, Loewen T, Pilon D. Canadian practice guidelines for the treatment of children and adolescents with eating disorders. Journal of Eating Disorders. 2020;8(1):1–80. doi: 10.1186/s40337-020-0277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couturier J, Kimber M, Szatmari P. Efficacy of family-based treatment for adolescents with eating disorders: A systematic review and meta-analysis. International Journal of Eating Disorders. 2013;46(1):3–11. doi: 10.1002/eat.22042. [DOI] [PubMed] [Google Scholar]
- de Oliveira C, Colton P, Cheng J, Olmsted M, Kurdyak P. The direct health care costs of eating disorders among hospitalized patients: A population-based study. International Journal of Eating Disorders. 2017;50(12):1385–1393. doi: 10.1002/eat.22797. [DOI] [PubMed] [Google Scholar]
- Doyle PM, Le Grange D, Loeb K, Doyle AC, Crosby RD. Early response to family-based treatment for adolescent anorexia nervosa. International Journal of Eating Disorders. 2010;43(7):659–662. doi: 10.1002/eat.20764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddy KT, Tabri N, Thomas JJ, Murray HB, Keshaviah A, Hastings E, Edkins K, Krishna M, Herzog DB, Keel PK, Franko DL. Recovery From Anorexia Nervosa and Bulimia Nervosa at 22-Year Follow-Up. The Journal of Clinical Psychiatry. 2017;78(02):184–189. doi: 10.4088/JCP.15m10393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galmiche M, Déchelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. The American Journal of Clinical Nutrition. 2019;109(5):1402–1413. doi: 10.1093/ajcn/nqy342. [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Lloyd SW, Lux L, Gartlehner G, Hansen RA, Brode S, Jonas DE, Evans TS, Viswanathan M, Lohr KN. Repetitive transcranial magnetic stimulation for treatment-resistant depression: A systematic review and meta-analysis. Journal of Clinical Psychiatry. 2014;75(5):477–489. doi: 10.4088/JCP.13r08815. [DOI] [PubMed] [Google Scholar]
- Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and other eating disorders. Current Opinion in Psychiatry. 2006;19(4):389–394. doi: 10.1097/01.yco.0000228759.95237.78. Curr Opin Psychiatry. [DOI] [PubMed] [Google Scholar]
- Hsu C-W, Wang L-J, Lin P-Y. Efficacy of repetitive transcranial magnetic stimulation for Tourette syndrome: A systematic review and meta-analysis. 2018 doi: 10.1016/j.brs.2018.06.002. [DOI] [PubMed] [Google Scholar]
- Hughes EK, Sawyer SM, Accurso EC, Singh S, Le Grange D. Predictors of early response in conjoint and separated models of family-based treatment for adolescent anorexia nervosa. European Eating Disorders Review. 2019;27(3):283–294. doi: 10.1002/erv.2668. [DOI] [PubMed] [Google Scholar]
- Jáuregui-Lobera I, Martínez-Quiñones JV. Neuromodulation in eating disorders and obesity: a promising way of treatment? Neuropsychiatric Disease and Treatment. 2018;14:2817–2835. doi: 10.2147/NDT.S180231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keski-Rahkonen A, Mustelin L. Epidemiology of eating disorders in Europe: Prevalence, incidence, comorbidity, course, consequences, and risk factors. Current Opinion in Psychiatry. 2016;29(6):340–345. doi: 10.1097/YCO.0000000000000278. [DOI] [PubMed] [Google Scholar]
- Klomjai W, Katz R, Lackmy-Vallée A. Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS) Annals of Physical and Rehabilitation Medicine. 2015;58(4):208–213. doi: 10.1016/j.rehab.2015.05.005. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Accurso EC, Lock J, Agras S, Bryson SW. Early Weight Gain Predicts Outcome in Two Treatments for Adolescent Anorexia Nervosa NIH Public Access. International Journal of Eating Disorders. 2014;47(2):124–129. doi: 10.1002/eat.22221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, Jo B. Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Archives of General Psychiatry. 2010;67(10):1025–1032. doi: 10.1001/archgenpsychiatry.2010.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lusicic A, Schruers KR, Pallanti S, Castle DJ. Transcranial magnetic stimulation in the treatment of obsessive-compulsive disorder: current perspectives. Neuropsychiatric Disease and Treatment. 2018;14:1721–1736. doi: 10.2147/NDT.S121140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClintock SM, Reti IM, Carpenter LL, McDonald WM, Dubin M, Taylor SF, Cook IA, O’Reardon J, Husain MM, Wall C, Krystal AD, Sampson SM, Morales O, Nelson BG, Latoussakis V, George MS, Lisanby SH National Network of Depression Centers rTMS Task Group & American Psychiatric Association Council on Research Task Force on Novel Biomarkers Treatments. Consensus Recommendations for the Clinical Application of Repetitive Transcranial Magnetic Stimulation (rTMS) in the Treatment of Depression. The Journal of Clinical Psychiatry. 2018;79(1):35–48. doi: 10.4088/JCP.16cs10905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mond JM, Arrighi A. Gender differences in perceptions of the severity and prevalence of eating disorders. Early Intervention in Psychiatry. 2011;5(1):41–49. doi: 10.1111/j.1751-7893.2010.00257.x. [DOI] [PubMed] [Google Scholar]
- Mond JM, Hay PJ. Public perceptions of binge eating and its treatment. International Journal of Eating Disorders. 2008;41(5):419–426. doi: 10.1002/eat.20512. [DOI] [PubMed] [Google Scholar]
- Murray SB, Pila E, Griffiths S, Le Grange D. When illness severity and research dollars do not align: are we overlooking eating disorders? World Psychiatry. 2017;16(3):321. doi: 10.1002/wps.20465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien KM, Whelan DR, Sandler DP, Hall JE, Weinberg CR. Predictors and long-term health outcomes of eating disorders. PLoS ONE. 2017;12(7) doi: 10.1371/journal.pone.0181104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obeid N, McVey G, Seale E, Preskow W, Norris ML. Cocreating research priorities for anorexia nervosa: The Canadian Eating Disorder Priority Setting Partnership. International Journal of Eating Disorders. 2020;53(5):392–402. doi: 10.1002/eat.23234. [DOI] [PubMed] [Google Scholar]
- Schmidt U, Lee S, Beecham J, Perkins S, Treasure J, Yi I, Winn S, Robinson P, Murphy R, Keville S, Johnson-Sabine E, Jenkins M, Frost S, Dodge L, Berelowitz M, Eisler I. A randomized controlled trial of family therapy and cognitive behavior therapy guided self-care for adolescents with bulimia nervosa and related disorders. American Journal of Psychiatry. 2007;164(4):591–598. doi: 10.1176/ajp.2007.164.4.591. [DOI] [PubMed] [Google Scholar]
- Smink FRE, Van Hoeken D, Hoek HW. Epidemiology of eating disorders: Incidence, prevalence and mortality rates. Current Psychiatry Reports. 2012;14(4):406–414. doi: 10.1007/s11920-012-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su JC, Birmingham CL. Anorexia nervosa: The cost of long-term disability. Eating and Weight Disorders. 2003;8(1):76–79. doi: 10.1007/BF03324993. [DOI] [PubMed] [Google Scholar]
- Trautmann S, Rehm J, Wittchen H. The economic costs of mental disorders. EMBO Reports. 2016;17(9):1245–1249. doi: 10.15252/embr.201642951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treasure J, Cardi V, Leppanen J, Turton R. New treatment approaches for severe and enduring eating disorders. Physiology and Behavior. 2015;152:456–465. doi: 10.1016/j.physbeh.2015.06.007. [DOI] [PubMed] [Google Scholar]
- Vall E, Wade TD. Predictors of treatment outcome in individuals with eating disorders: A systematic review and meta-analysis. International Journal of Eating Disorders. 2015;48(7):946–971. doi: 10.1002/eat.22411. [DOI] [PubMed] [Google Scholar]
- Van Den Eynde F, Guillaume S. Neuromodulation techniques and eating disorders. International Journal of Eating Disorders. 2013;46(5):447–450. doi: 10.1002/eat.22100. [DOI] [PubMed] [Google Scholar]
- Volpe U, Tortorella A, Manchia M, Monteleone AM, Albert U, Monteleone P. Eating disorders: What age at onset? Psychiatry Research. 2016;238:225–227. doi: 10.1016/j.psychres.2016.02.048. [DOI] [PubMed] [Google Scholar]
- Ward ZJ, Rodriguez P, Wright DR, Austin SB, Long MW. Estimation of Eating Disorders Prevalence by Age and Associations With Mortality in a Simulated Nationally Representative US Cohort. JAMA Network Open. 2019;2(10):e1912925. doi: 10.1001/jamanetworkopen.2019.12925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodside B. Evidence - FEWO (41-2) Standing Committee on the Status of Women - No. 5- House of Commons of Canada. 2013. https://www.ourcommons.ca/DocumentViewer/en/41-2/FEWO/meeting-5/evidence.