Abstract
Sleep disruption is common among older adults. Non-pharmacological interventions involving music has emerged as a promising approach to address sleep disruption. The purpose of this systematic review was to examine the effects of music interventions on sleep outcomes among older adults (age ≥ 50). We searched five databases through May 2020 and found 16 eligible studies focused on two types of music interventions: music listening (n=11) and multi-component (n=5). We found mixed evidence in the efficacy of music interventions to improve sleep outcomes in older adults, which included sleep quality, objective and subjective sleep characteristics. Music listening interventions contained relaxing music with research teams personalizing music choice based on participants’ preferences. Multi-component interventions included listening to music in addition to one other approach, such as massage, tai chi, and nature scenes. Future higher-quality studies should provide a detailed description of music interventions and tailor music selections to older adults’ preferences.
Introduction
Sleep serves important restorative functions in the body, yet changes as we age.1 Sleep changes in older adults include shorter total sleep time, low sleep efficiency, longer sleep latency, and greater wake after sleep onset.2 Compared to younger adults, older adults experience a higher percentage of lighter sleep (stages N1 and N2) and spend less time in deeper stages of sleep (REM and slow wave sleep, SWS).3 Furthermore, older adults experience several circadian rhythm changes with aging, which include a decline in the amplitude of circadian markers (i.e., core body temperature, melatonin and cortisol), and a decrease in melatonin secretion at night.1 Between 15% and 65% of older adults report sleep disruption (nighttime sleep fragmentation, decreased sleep efficiency) and increased rates of nonrestorative sleep.3 Common sleep disorders in older adults include insomnia (difficulty falling asleep or waking up too early), sleep disordered breathing, restless leg syndrome and REM sleep behavior disorder.2,4
Treatment for sleep disorders among older adults involves both pharmacological and non-pharmacological approaches. For example, antidepressants, such as trazodone, can be used in low doses to treat insomnia in older adults.2 Pharmacological interventions, however, should not be the first line of treatment due to high risk of falls, daytime sedation, worsening of agitation, and cardiac-related mortality.4–8 In addition, many older adults have negative perceptions of sleep medication, as evidenced by their desire to fall asleep naturally and notions that sleep medication will lead to grogginess and addiction.9 Nonpharmacological interventions provide an alternative to pharmacological treatments to address sleep symptoms in older adults associated with sleep disorders. Promising nonpharmacological approaches include cognitive behavioral therapy for insomnia (CBT-I), light therapy,10 increased daytime physical activity,11 improved sleep hygiene such as reducing caffeine intake and changes in the immediate environment (such as quiet bedroom and avoiding blue light emitting devices prior to bedtime), or a combination of these approaches.12 Listening to relaxing music at bedtime has also demonstrated sleep benefits in prior studies of older adults.13
Engaging in music is a common activity among older adults and may help promote sleep. Older adults are frequent music listeners14 and report engaging in other music arts, such as singing in a choir.15 Musical properties may elicit benefits for older adults struggling with sleep disturbances. For example, relaxing and sedative music may improve sleep quality in older adults by promoting deep sleep,16 decreasing stress,17 and encouraging relaxation.18 Dickson and Schubert proposed several mechanisms by which music can aid in sleep including distraction, entrainment, masking, enjoyment, and cultural expectation.19 Music can distract listeners by changing their focal point of attention from stressful thoughts to relaxing music. Entrainment refers to the “synchronization of the listener’s low-frequency neural activity or heart rate to the rhythmic structure or tempo of an auditory stimulus” (p. 148). Masking occurs when external, often noxious, background noise is minimized by the music. Those who listen to music before going to sleep report enhanced mood thus contributing to the enjoyable experience.20 In addition, individuals may find certain music to be sleep-inducing because of its cultural connection.19
Given the adverse effects of pharmacological treatment for sleep in older adults,4–8 non-pharmacological approaches such as music may offer safer alternatives in improving sleep outcomes in this population. Music interventions have shown promising results in improving sleep among older adults.21–23 However, previous reviews of music interventions primarily focused on all adults (18 years old or greater)13,24 and did not examine the impact of music interventions specifically on older adults, who often report sleep complaints. We defined music intervention broadly as music that is being delivered with the intention of improving health outcomes for older adults, whether it is being delivered alone (such as listening to music), as part of therapy (i.e., music therapy) or in conjunction with other non-pharmacological approaches (such as exercise).25 The purpose of this systematic review is to examine music intervention characteristics and determine whether music interventions improve sleep outcomes in older adults. By identifying music intervention characteristics that are more likely to exert a positive effect on sleep outcomes in older adults, researchers in future studies can tailor their music selections to increase the strength of their interventions.
Method
Eligibility Criteria
The purpose of this systematic review was to collate results from published studies to examine the characteristics of music interventions and its effects on sleep outcomes in older adults. We used the following inclusion criteria for the studies: experimental (RCTs, cross-over RCTs) and quasi-experimental designs (pre/post); focused on older adults (defined as age 50 and older); published in English; subjective or objective sleep measure as an outcome, published before May 2020. We chose 50 as cut-off age because we included studies globally; the World Health Organization’s Study on Global AGEing and adult health (SAGE) defines older adults as those over the age of 50.26 Furthermore, we excluded qualitative studies because the focus of this review was on quantitative intervention outcomes, rather than qualitative explorations of intervention effect or mechanism.
Information Sources and Search Strategy
We conducted a review following the Cochrane Handbook for Systematic Reviews of Interventions (Version 6.1), the official guide that provides details on how to prepare and conduct a systematic review.27 In addition, we used the PRISMA-P (Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols) 2015 checklist to structure our systematic review.28 We searched five databases to find potential articles to include in this systematic review: CINAHL, Embase, PsycINFO, PubMed, and Scopus. We consulted with the university librarian to select search terms and used a combination of MESH terms and keywords: (music OR music therapy OR music perception) AND (sleep OR sleep wake disorders OR sleep disorder) AND (aged OR elderly OR older OR senior OR aging). All searches were conducted in May 2020.
Study Selection and Data Extraction
After completing the database searches, we imported all potentially eligible studies into reference management software (Endnote X9) and removed duplicates. Two authors independently screened the titles and abstracts of all searched results. We asked a third author to make a final decision for any discrepancy that arose between the two authors. The authors then read the full texts of the potential studies using previously identified inclusion/exclusion criteria. The two authors independently extracted data from full text articles, which included first author and year, study design, participant description, number of participants, mean age and standard deviation, intervention description, music used, intervention duration, control group, sleep measures and sleep outcomes. The authors met to discuss any discrepancy in the extraction forms and third author was asked to make a final decision for any discrepancy. Both authors reviewed the abstract, data tables, and procedural portions of each full-text study. A meta-analysis was not appropriate for this review because of the heterogeneity in the types of interventions and sleep outcomes.
Quality Assessment
We used the Joanna Briggs Institute (JBI) Checklist for Randomized Control Trials and Quasi-Experimental Trials to evaluate the quality of the studies because these are comprehensive quality assessments that can be used for both RCTs and quasi-experimental studies.29 The JBI RCT checklist contains 13 questions to evaluate credibility, transparency, and validity of each study. The JBI Quasi-Experimental checklist follows a similar format but utilizes 9 questions. These questions were either answered with a Y (yes), N (no), U (unclear), or NA (not applicable). Total scores were computed by adding the Y responses for each study assessment, with higher scores indicating higher quality. In addition, we assessed the overall quality of the included studies as a whole (i.e. low, moderate, high) based on the total score. For all the included studies, the first and second author independently reviewed and scored these studies based on the checklist. Any disagreements regarding scores were resolved between the authors with further discussion.27
Results
Search outcomes
We identified 624 studies after removing duplicates. Five hundred and thirty-seven articles were excluded based on titles and abstract screening, leaving 87 articles for full-text review. Next, 71 articles were excluded for the following reasons: study did not include older adults (n=28); no sub analysis for older adults was performed (n=24); study did not include pre and post measures (n=9); no sleep outcome (n=6); full-text was not available (n=1); duplicate study (n=1), study not in English (n=1) and other (n=1). Therefore, we included 16 studies in this systematic review. We illustrate the flow of studies through the systematic review in Figure 1.
Figure 1:
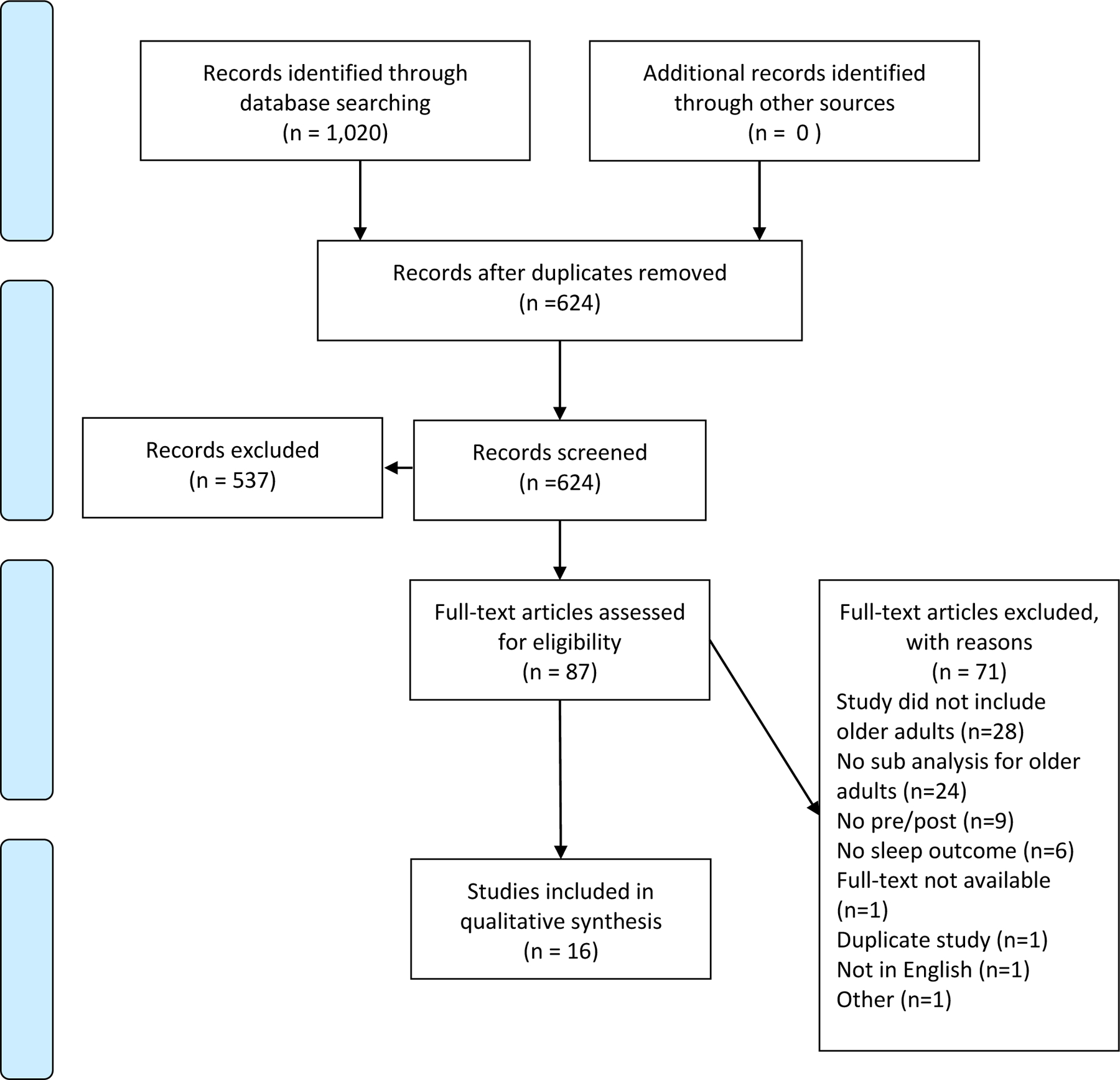
Flow Diagram of the Literature Search
Study characteristics
The research from 16 included studies took place in nine different countries: China,21 Israel,30 Germany,31 Hong Kong,32 Japan,33 Korea,34 Singapore,23,35,36 Taiwan,37–39 and United States.22,40–42 These studies were published between 200341 and 2020.31 Almost all (15/16) studies enrolled participants from the community; one study took place in a nursing home.31 Eleven out of 16 studies were RCTs,21–23,31–34,36,38,40,42 two were cross-over RCTs,37,39 and three studies used quasi-experimental pre/post one group design (Table 1).30,35,41
Table 1:
Characteristics of included studies.
| First author, year, country | Study design | Participants | N, mean age±SD | Intervention(s) description | Music used | Intervention Duration | Control group | Sleep measure(s) | Sleep outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Music listening | |||||||||
| Chan (2010)32 Hong Kong |
RCT | Healthy older adults (60+) | N= 42 (IG 21; CG 21) 57.1% age 75+ | Listening to an MP3 player + relaxation instructions. | Meditative, Chinese classical, western classical, jazz; all were slow, flowing pieces at 60–80 BPM | 4 weeks, daily for 30 minutes | Uninterrupted rest period | PSQI | No significant differences between groups. |
| Huang (2016)39 Taiwan |
Cross-over RCT | Sedentary older adults (50+) with chronic insomnia | N=38 56.4±6.4 years old |
|
Three soothing Buddhist songs (Praise Buddha, Song of Praise Sambo, and Namo Shakyamuni Buddha), 60–80 BPM, minor tonalities, smooth melodies. | 1 week, 2 days for 30 mins | Participants served as their own control | EEG+ actigraphy Sleep quality: VAS |
|
| Innes (2016)22 United States |
RCT | Older adults (50+) with subjective cognitive decline or mild cognitive impairment | N=60 (KK 30, ML
30) 60.6±1.0 |
|
Relaxing instrumental music from each of 6 composers:Mozart, Bach, Vivaldi, Beethoven, Pachelbel, and Debussy | 12 minutes every day for 12 weeks | None | PSQI | No differences in sleep quality between groups at any time points |
| Innes (2018)40 United States |
RCT | Older adults (50+) with osteoarthritis pain | N= 22 (MM 11; ML
11) 58.5±1.4 |
|
Relaxing instrumental music from each of 6 composers: Mozart, Bach, Vivaldi, Beethoven, Pachelbel, and Debussy | 2 times a day for 15–20 mins for 8 weeks | None | PSQI | Relative to ML, the MM group showed significantly greater improvements in overall sleep quality (p=0.04) |
| Johns on (2003)41 United States |
Quasi-experimental pre/post one group | Older women (70+) with chronic insomnia | N=52 80.5 |
Music listening: listening to music in bed with an automatic shut-off. | Selections varied, participants were asked to choose music in the same category. Participants selected soothing classical music (64%), sacred music (19%) and new age music (17%) | 10 days every day, session length not reported | None | 1. SSS 2. Sleep log: sleep onset, number of awakenings |
|
| Lai (2005)38 Taiwan |
RCT | Healthy older (60+) adults with poor sleep | N=60 (IG 30, CG 30) | Music listening: listening to music + standardized relaxation instructions | 6 types of sedative music: 5 types western music (synthesizer, harp, piano, orchestra, slow jazz) and 1 type of Chinese music (orchestra folk). Sedative music - 60–80 BPM without accented beats, percussive characteristics or syncopation. | 3 weeks, 45 minutes every day | Participants were not given music | PSQI | Sleep quality: significant differences between groups. Compared to CG, sleep quality in IG improved (F(1,60), 86.49; p < 0.01). |
| Shum (2014)23 Singapore |
RCT | Older (55+) adults with poor sleep | N=60 (IG 28, CG 32) | Music listening: MP4 music player with earphones with constant music genre for the week + additional relaxation instructions. | Western classical (Bach, Mozart, Chopin), Chinese classical (Spring river in the moonlight, variation on yang pass), jazz (everlasting, Winter wonderland, in love in vain) and New Age (Shizuku, Lord of wind). All music was soft, instrumental slow music, 60–80 BPM with no lyrics. | 40 min session once per week for 6 weeks | Asked not to listen to music for 6 weeks | PSQI | Sleep quality: significant group differences in all weeks between groups. PSQI scores for IG decreased while CG scores remained the same (p values <0.001 – 0.018). |
| Wahbeh (2019)42 United States |
RCT | Older (55+) adults with depressive symptoms | N=29 (IG 15, CG 14) |
|
Favorite music | Two-day retreat followed by 6 weeks for at least 20 minutes daily use | None | PSQI | Sleep quality: significant group differences. Sleep quality significantly improved in the iRest mediation group compared to the music listening group (F=4.15, p=0.05) |
| Wang (2016)21 China |
RCT | Older (60+) adults with poor sleep | 64 (IG 32, CG 32) 69.4±5.5 (IG 66.9±5.0; CG 69.8±5.6) |
Music listening: instructions to music on an MP3 player + relaxation instructions | Chinese instrumental classic, Western classic, natural sounds music, and classical songs without lyrics. All music - soft and sedative with stable melodies at 60–80 BPM | 30–45 mins per night for 3 months | Sleep hygiene | PSQI | Compared to the CG, the IG achieved greater improvements in global PSQI score at each time point (p=0.020, 0.012, 0.001); greater improvements in sleep latency (p=0.041), daytime dysfunction (p=0.005); sleep latency (p=0.003); sleep duration (p=0.023), sleep efficiency (p=0.006). |
| Ziv (2008)30 Israel |
Quasi-experimental pre/post one group | Older adults (67+) with insomnia | N=15 |
|
Slow melody accompanied by minor harmony all played on piano with background violins and bells that develops for the first 10 mins | 40 mins per session for 1 week | N/A | 1. Actigraphy outcomes: sleep percentage,
sleep efficiency, time falling asleep 2. Mini sleep questionnaire and Technion long sleep questionnaire |
|
| Weise (2020)31 Germany |
RCT | Nursing home residents (73+) with a diagnosis of dementia | N=20 (IG 10, CG
10) 85.1±5.9 |
Music listening: Three individualized playlists on MP3 players with headphones. | Personally significant music based on own preferences and experiences | 30 mins every other day for 4 weeks | Wait-list | VAS | Compared to participants in the CG, participants in the IG had significantly better sleep quality (p=0.038, d=0.52) |
| Multi-component interventions | |||||||||
| Choi (2015)34 Korea |
RCT | Healthy women (60+) | N=72 (ML+HM 24; HM 25; CG 23) 68% age >66 years old |
|
Popular Korean songs to instrumental performances | Four weeks: 5 minutes, twice a week | Did not receive hand massage or music | Hours of sleep | No significant differences between groups |
| Lai (2015)37 Taiwan |
Cross-over RCT | Older adults (50+) with insomnia | N=38 59.6±6.7 |
Music videos: Seven peaceful religious videos showed nature scenes along with text comprising Buddha’s teaching and words of wisdom while the peaceful music was being played. | The musical tempos range from 60 to 85 beats/min (slow), and the music used minor tonalities and smooth melodies to achieve a relaxing effect | 30 mins per night for one night | Usual care | 1. VAS: ease of falling asleep, perceived
sleep quality, ease of awakening, daytime function 2. PSG: TST, SE, SOL, WASO, number of awakenings, N1, N2, N3, REM, sleep, arousal index |
|
| Rawtaer (2017)35 Singapore |
Quasi-experimental one-group pre/post | Older adults (60+) | N=189 69.3±5.7 |
Combination of tai chi exercise, mindfulness awareness practice, art therapy, music reminiscence therapy | Popular evergreen songs | 1 to 2 hours for 10 weeks, every 2 weeks for 18 weeks and monthly for the rest of the year | N/A | PSQI |
|
| Satoh (2015)33 Japan |
RCT | Older adults (68+) with probable Alzheimer’s Disease | N=20 (CG 10, IG 10) (IG 78.1±7.0; CG 77.0±6.1) |
Music therapy sessions | Favorite music, which was either popular in patients’ youth or very familiar ones of recent years | 1 hour per week for 6 months; at home 3x/week for 20 minutes | Neuropsychological assessments twice within the 6 month time period | Hours slept 2 weeks prior to assessment | Sleep time for patients in music therapy group increased from 7.5 hours per night at baseline to 8.2 hours per night post intervention (sleep time was only collected from music therapy group). |
| Yap (2017)36 Singapore |
RCT | Older adults (65+) | N= 31 (CG 15, IG 16) 74.7±6.4 (CG 74.9±6.1; IG 74.4±6.8) |
Rhythm-centred music making: group Rhythm Wellness Programme by OneHeart Beat, facilitated by 3 instructors. | Rhythmic music using percussion instruments (conga, cowbell, Djembe, Ashiko tan-tans, dunum, shakers, wood blocks). | 1 hour per session, once per week for 10 weeks | Usual care | PSQI | No differences in PSQI scores across groups |
BPM: beats per minute; CG – control group; EEG: electroencephalogram; HM: hand massage; IG-Intervention group; KK: Kirtan Kriya; ML: music listening; MM: Mantra Meditation; MV: music videos; PDSS-Parkinson’s Disease Sleep Scale; PSG: Polysomnography; PSQI: Pittsburgh Sleep Quality Inventory; RCT: randomized clinical trial; REM: rapid eye movement; RTM: Rest to Music; SE: sleep efficiency; SOL: sleep-onset latency; SSS: Sleepiness- Stanford Sleepiness Scale; TST: Total Sleep Time; TT: Tactile Touch; VAS: visual analog scale; WASO: wake after sleep onset.
Participant Characteristics
The studies included 812 older adults with samples ranging from 2033 to 18935 (Mean number of participants = 51, SD = 41). All the adults were over the age of 50. Seven out of 16 studies included older adults with sleep complaints.21,23,30,37–39,41 Four studies considered participants eligible at screening if they scored at least 5,37,39 623 or 721 on the Pittsburgh Sleep Quality Index (PSQI). Two studies relied on participants’ subjective sleep complaints38,41 and one study used DSM-IV insomnia diagnosis for inclusion criteria.30 The remaining ten studies included healthy older adults,32,34–36 those with cognitive impairment or dementia,22,31,33 pain,40 and depressive symptoms.42
Methodological Quality
The studies included were rated as moderate quality overall, with RCTs having an average score of 9 out of 13 and quasi-experimental studies having an average score of 7 out of 9. Among RCTs, the largest threats to the internal validity were whether the outcome assessors and those delivering the treatment were blind to the treatment assignment. Three of 14 studies were unclear regarding the usage of true randomization while the remaining studies reported appropriate randomization, follow up procedures, and adequately kept track of all participant information. The quasi-experimental studies were also high quality; lack of a control group was the most common source of bias (Appendices A and B).
Sleep Outcomes
The Pittsburgh Sleep Quality Index (PSQI),43 used in nine studies21–23,32,35,36,38,40,42 was the most commonly used scale to assess sleep outcomes. Additional sleep outcomes included polysomnography,37 electroencephalogram (EEG);39 actigraphy,30,39 visual analog scales,31,37,44 and sleep logs and questionnaires.30,34,41 Four studies used a combination of methods to assess sleep outcomes.30,37,39,41
Music Listening Interventions and Control Group Conditions
Music interventions included two categories: music listening in 11 studies and multi-component interventions in five studies. Music listening interventions included listening to an MP3 or a CD player before going to bed. Four of the eleven studies also included additional relaxation instructions.21,23,32,38 Most studies (8/11) reported selecting music based on relaxing characteristics (i.e., tempo 60–80 beats per minute without accented beats);21–23,30,32,38–40 five of those eight studies used culturally-appropriate music,21,23,32,38,44 and in the remaining three studies participants were asked to select their own music.31,41,42 The approaches by which participants selected their own music varied. For example, Johnson and colleagues41 encouraged participants to select their own music which could vary nightly but needed to be in the same category. Wahbeh and colleagues42 asked participants to identify their favorite music from the selection of genres, while Weise et. al31 asked participants, family members, and nursing staff to identify personally-relevant music for each nursing home resident using Gerdner’s evidence-based guidelines.45 Duration and frequency of music listening sessions varied greatly in the eleven studies from 12 to 45 minutes daily (30-minute session most common), every other day to once or twice a week. Intervention duration varied between one week30,39 and three months21 with median value being 4 weeks.
Multi-component music interventions included music therapy,33 and music listening combined with: hand massage,34 videos,37 percussion music making,36 tai chi exercise, mindfulness awareness practice, and art therapy.35 Music therapy intervention included group singing at a hospital setting once a week for six months. The sessions were carried out by a professional singer and a pianist, who were part of the research team and included a voice training method, which incorporated learning and practice singing familiar songs. Participants in this study were also asked to practice singing at home three times a week for 20 minutes using a karaoke system.33 Given the benefits of therapeutic touch, two of the included studies reported the effects of listening to music with massage on sleep in older adults. Choi and colleagues34 combined hand massage using aroma essential oil with listening to music in which participants were provided three popular Korean songs according to their preference. The music intervention was delivered at the same time as hand massage. In other studies, listening to music was combined with nature science and texts of Buddha’s teaching37 and rhythm music making.36 The largest number of co-occurring group activities took place in a quasi-experimental pre/post study of 189 older adults who engaged in music reminiscence, mindfulness awareness practice, tai chi exercise and art therapy over one year.35
Control group conditions varied. The most common control group condition included the lack of the active intervention component (n=9) in the form of usual care,23,32–34,37,38 wait-list group,31 or subjects serving as their control.30,36,39 Other control group conditions included sleep hygiene21 and meditation.22,40,42
Efficacy of music interventions by sleep outcomes
Sleep quality
There was mixed evidence regarding the efficacy of music interventions to improve sleep quality in older adults. Three RCTs that examined sleep quality as a sleep outcome found no difference between music intervention and comparison conditions,22,32,36 three RCTs found significant improvements in the intervention group21,23,38 and one quasi-experimental study did not find any changes in sleep quality post intervention.35 Two studies that compared music intervention to mediation found that participants in the meditation group showed greater improvements in sleep quality compared to older adults in the music intervention group.40,42 The common characteristics of music intervention in three RCTs that found significant improvements in sleep quality included a variety of sedative and culturally appropriate music (i.e., Chinese orchestra folk and classical genres) as well as relaxation instructions.21,23,38 The frequency and duration of music intervention varied between the three studies: each music session was between 30 and 45 minutes, administered daily or once a week and with each intervention lasting between three weeks and three months.
Three RCTs that found no differences in sleep quality between the intervention and control groups used meditative, Chinese classical music,32 relaxing instrumental Classical music22 and compared group rhythm-centered music making to usual care.36 In one quasi-experimental study the researchers used a combination of tai chi exercise, mindfulness awareness practice, art therapy, and music reminiscence therapy to examine pre- and post-changes in sleep quality.35
Objective sleep
Three studies reported that music intervention improved objective sleep outcomes as measured by actigraphy30,39 and polysomnography.37 Music interventions shortened wake after sleep onset,39 increased sleep efficiency30 and decreased SOL.37
Sleep quality measured by the Visual Analog Scale
For three studies that used visual analog scale to assess sleep quality, two found no difference between the groups.37,39 On the contrary, Weise and colleagues reported nursing home residents who listened to an individualized playlist 30 minutes every day for four weeks reported significantly better sleep quality compared to participants in the control group (p=0.038, d=0.52).31
Sleep Logs and Questionnaires
Four studies that used sleep logs and sleep questionnaires included three RCTs and one pre/post quasi-experimental design study. One RCT, however, which reported an increase in total sleep time for the music therapy group did not collect data on sleep outcomes from the control group.33 There were no significant differences between intervention and control groups in the remaining two RCTs.30,34 Using Stanford Sleepiness Scale and sleep logs, Johnson and colleagues41 found that after listening to music daily for 10 days participants reported greater levels of sleepiness at bedtime (t = 3.72, p < 0.01) and lower sleep onset (t = 3.12, p < 0.01) and less number of awakenings at night (t = 2.30, p<0.05).
Efficacy of Music Interventions by Type of Intervention
We examined the efficacy of music interventions on sleep outcomes according to the intervention type: music listening (n=11; 9 RCT) and multi-component interventions (n=5). Three RCTs of the nine studies that examined the effects of music listening intervention on sleep quality showed no difference between intervention and control groups.32 In two of these RCTs music listening was compared to an alternative activity (brisk walking39 and meditation22), while Chan and colleagues compared the effects of music listening to a rest period.32 Four out of nine RCTs that examined the effect of music listening on sleep quality reported significant improvement in the intervention group compared to sleep hygiene21 and usual care.23,31,38 Two studies reported improved sleep quality in the meditation group compared to the music listening group.40,42 Two studies that used actigraphy outcomes reported decrease in wake after sleep onset in the music intervention group39 and increase in sleep efficiency.30 In one quasi-experimental one group pre/post design study, Johnson and colleagues reported increased sleepiness, shorter sleep onset and decreased number of night awakenings in 52 older women with chronic insomnia who were exposed to music listening intervention.41
The results from five multi-component music intervention studies on sleep outcomes were mixed. Sleep quality did not improve in older adults after participating in the intervention across all of the studies.34–37 Older adults who participated in multi-component interventions experienced shorter sleep onset,37 less sleep disturbances,35 and increased sleep time.33
Discussion
In this systematic review we examined intervention characteristics and the effect of music listening interventions on sleep outcomes in persons living with dementia and their caregivers. We included 16 studies; 11 were RCTs, two were cross-over RCTs and three studies used quasi-experimental design. We found mixed evidence in the efficacy of music interventions to improve sleep outcomes in older adults, which included sleep quality, objective and subjective sleep characteristics. Most of the music listening interventions contained relaxing music with several research teams personalizing music choice based on participants’ preference. Multi-component interventions included listening to music in addition to one or more other non-pharmacological approaches, such as massage, tai chi, and nature scenes. In contrast to our review which focused solely on older adults with and without sleep problems, previous reviews focused on the efficacy of music interventions on sleep problems in all adults (18+) including older adults who reported insomnia24 or sleep-related complaints.13 Our review suggests that while music interventions can be efficacious in improving sleep among older adults, future studies should aim to personalize music selections for research participants, examine the dose of the intervention and its ability to have an impact on specific sleep characteristics.
We identified several common characteristics of music listening interventions across the studies. Eight out of 11 research teams that examined the effect of music listening interventions on sleep used relaxing music, identified as meditative, instrumental, and having a tempo between 60–80 beats per minute. These findings are in line with published reviews of sleep-inducing music in other populations, such as adults in the ICU setting,46 and pregnant women.47 The authors in the reviewed studies cited previous literature to support the selection of music. Four studies also reported the addition of relaxation instructions which included wearing sleepwear, playing music at a comfortable volume, and minimizing environmental distractions. Since all these studies took place in the community, providing participants with the additional relaxation instructions may promote adherence to the intervention, standardize its delivery and enhance the effect of relaxing music. The duration and frequency of music listening sessions varied in the included studies with 30-minute sessions being the most common duration. Future studies should consider the length of exposure to music listening that would more likely have an effect on sleep outcomes and consider the addition of relaxation instructions as part of their intervention.
Tailoring of music has been shown to be an important aspect of delivering person-centered behavioral interventions; however, only eight studies reported tailoring selected music for research participants. Tailoring varied; most research teams (n=5) selected relaxing music that was culturally appropriate for their research participants. For example, Wang and colleagues21 created a music database with 169 pieces of music which included Chinese instrumental classic and Western classic music for older adults recruited from Xi’an, the capital of Shaanxi Province in China. While all the included studies provided the genre of selected music, only two studies provided the exact song titles.23,39 Music can differ significantly between different artists, therefore providing the exact song titles and performers’ information in the journal appendices can assist in the interpretation of results across studies in future research.25 It is noteworthy that three students made an effort to further personalize music selections.31,41,42 Previous research suggests the importance of selecting preferred music as it may enhance the efficacy of the intervention and improve its adherence in older adults.18,48,49 It is unclear from the review if one music selection method is associated with increased efficacy of the intervention. Future studies may consider using Gerdner’s recommendations for selecting personally-relevant music for older adults.45 Personally-relevant music, however, may not have the relaxing characteristics commonly used in sleep studies. An alternative for the researcher team is to identify personally relevant genres of music and artists, then select music from the suggested list that still fits the relaxing characteristics. For instance, older adults who share their favorite artist’s popular hits may also enjoy lesser known to them songs by the same artist. Our review suggests that future studies should aim to tailor music selections for participants based on relaxing music characteristics and personal preference.
When we examined the efficacy of music interventions by sleep outcomes and by intervention type (music listening vs multi-component) we found mixed evidence due to low methodological rigor of the included studies. The outcome assessors were often not blinded to treatment assignment. Studies that examined the effects of music intervention on sleep quality were split between reporting no improvement in sleep quality22,32,35,36 and reporting better sleep quality in the intervention group compared to control condition.21,23,38 When examining only the effects of music listening interventions on sleep quality, we found that four out of nine RCTs reported significant improvement.21,23,31,38 Since sleep quality is a broad concept, which may encompass objective measures such as sleep duration, sleep latency, sleep efficiency and subjective perception of one’s sleep quality, it may lend itself to being appropriate to measure the effects of music listening interventions on sleep. Mixed sleep outcome efficacy could be attributed to the fact that only seven out of the 16 studies included older adults who reported sleep problems at baseline.21,23,30,37–39,41 While music listening interventions in this review were delivered at nighttime, there was limited evidence that listening to music prior to bedtime improved sleep onset,37 sleep efficiency30 and shortened wake after sleep onset using objective sleep measures.37,39 Feelings of sleepiness may be an alternative measure of the effects of listening to music at bedtime, as suggested by Johnson and colleagues.41 Future studies may consider including a measure of sleepiness before older adults fall asleep, if music intervention is delivered 30 minutes before bedtime, assessing for changes in sleep quality and daytime function. In addition, future studies should include older adults with sleep problems at baseline.
Strengths and Limitations
In this systematic review we examined music intervention characteristics and determined whether music interventions improve sleep outcomes in older adults. While previous reviews on the topic of music interventions and sleep in adults have been published, our review identifies gaps in knowledge and provides future directions on ways music interventions can be used to improve sleep specifically in older adults. We also examined study quality of the included studies and provided direction for future research. We included studies with different types of music interventions as well as varying sleep outcomes. Instead of limiting our review by a particular disease process in older adults, we included a broad spectrum of disease conditions. We provided a detailed description of music interventions and grouped them by music listening or multi-component type. We provided a narrative synthesis of the efficacy results grouped by the intervention type and sleep outcome.
There are several limitations to our study. First, we limited our search to articles published in English, therefore we have missed relevant articles published in another language. Second, while the topic of sleep disturbances in older adults has gained attention in recent years, we were only able to locate a limited number of studies. The heterogeneity of sample, types of interventions and sleep outcomes prevented us from completing a meta-analysis. Third, we did not include unpublished research studies thus increasing the risk for publication bias. Fourth, the limited description of the intervention limits us in concluding which type of the music intervention is most efficacious in improving sleep among older adults.
Recommendations for Future Research
Future studies should use music with characteristics that have been shown as effective in improving sleep among older adults (such as meditative, instrumental, and having a tempo between 60–80 beats per minute). In addition, future protocols need to tailor music based on older adults’ preferences. These preferences can be identified using a music preference questionnaire.45 Sleep outcomes should include both subjective and objective measures in line with the proposed mechanism of action of the intervention. Reporting of music intervention research should include music intervention details (i.e., number of songs, composer, performer, and versions used). We recommend a recent publication,25 which outlines guidelines to improve the quality of reporting music interventions in healthcare research.
Conclusion
In this systematic review we found that music interventions demonstrated mixed efficacy in improving sleep among older adults. Music interventions range from passive music listening and multi-component music approaches. We recommend future studies to provide a detailed description of music interventions and tailor music selections to older adults’ preferences. In addition, future studies should incorporate both subjective and objective measures of sleep outcomes to account that certain music interventions may have a larger effect on the type of sleep measurement.
Highlights.
Most research teams used meditative, instrumental with tempo between 60–80 bpm.
Four studies also reported the addition of relaxation instructions.
Mixed efficacy of music interventions to improve sleep outcomes in older adults.
Tailored music accounted for older adults’ personal preferences.
Funding:
This work was supported by the National Institutes of Health [grants number F32 AG060630 and R01 NR015226]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix A: Joanna Briggs Institute Checklist for Randomized Control Trials
| Author, Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Total score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chan 2010 | Y | U | U | U | N | N | Y | Y | Y | Y | Y | Y | Y | 8 |
| Choi 2015 | U | U | Y | U | N | U | Y | Y | Y | Y | Y | Y | Y | 8 |
| Huang 2016 | Y | U | Y | N | U | U | Y | Y | Y | Y | Y | Y | Y | 9 |
| Innes 2016 | Y | Y | Y | U | NA | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Innes 2018 | Y | Y | Y | N | NA | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Lai 2005 | Y | U | Y | N | NA | U | Y | Y | u | Y | Y | Y | Y | 8 |
| Lai 2015 | Y | U | Y | N | U | U | Y | Y | U | Y | Y | Y | Y | 8 |
| Satoh 2015 | U | U | Y | U | U | U | Y | Y | Y | Y | Y | Y | Y | 8 |
| Shum 2014 | Y | Y | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | 10 |
| Wahbeh 2019 | U | U | Y | N | NA | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Wang 2016 | Y | U | Y | U | NA | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Weise 2020 | Y | Y | Y | U | N | N | Y | Y | U | Y | Y | Y | Y | 9 |
| Yap 2017 | Y | Y | Y | N | N | N | Y | Y | N | Y | Y | Y | Y | 9 |
Was true randomization used for assignment of participants to treatment groups?
Was allocation to treatment groups concealed?
Were treatment groups similar at the baseline?
Were participants blind to treatment assignment?
Were those delivering treatment blind to treatment assignment?
Were outcomes assessors blind to treatment assignment?
Were treatment groups treated identically other than the intervention of interest?
Was follow up complete and if not, were differences between groups in terms of their follow up adequately described and analyzed?
Were participants analyzed in the groups to which they were randomized?
Were outcomes measured in the same way for treatment groups?
Were outcomes measured in a reliable way?
Was appropriate statistical analysis used?
Was the trial design appropriate, and any deviations from the standard RCT design (individual randomization, parallel groups) accounted for in the conduct and analysis of the trial?
Appendix B: Joanna Briggs Institute Checklist for Quasi-Experimental Trials
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Total score | |
|---|---|---|---|---|---|---|---|---|---|---|
| Johnson 2003 | Y | Y | N | N | Y | Y | Y | Y | Y | 7 |
| Rawtaer 2018 | Y | Y | Y | N | Y | U | Y | Y | Y | 7 |
| Ziv 2008 | Y | Y | Y | N | Y | Y | Y | Y | Y | 8 |
Is it clear in the study what is the ‘cause’ and what is the ‘effect’ (i.e. there is no confusion about which variable comes first)?
Were the participants included in any comparisons similar?
Were the participants included in any comparisons receiving similar treatment/care, other than the exposure or intervention of interest?
Was there a control group?
Were there multiple measurements of the outcome both pre and post the intervention/exposure?
Was follow up complete and if not, were differences between groups in terms of their follow up adequately described and analyzed?
Were the outcomes of participants included in any comparisons measured in the same way?
Were outcomes measured in a reliable way?
Was appropriate statistical analysis used?
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest:
None
Contributor Information
Darina V. Petrovsky, University of Pennsylvania School of Nursing, Claire M. Fagin Hall, 418 Curie Blvd., Philadelphia, Pennsylvania, USA 19104-4217.
Pranav Ramesh, Irvington High School, 41800 Blacow Rd, Fremont, CA 94538.
Miranda Varrasse McPhillips, University of Pennsylvania, 3615 Chestnut Street, Philadelphia, PA 19104.
Nancy A. Hodgson, University of Pennsylvania School of Nursing, Claire M. Fagin Hall, 418 Curie Blvd., Philadelphia, Pennsylvania, USA 19104-4217.
References
- 1.Crowley K. Sleep and sleep disorders in older adults. Neuropsychol Rev. 2011;21(1):41–53. 10.1007/s11065-010-9154-6 [DOI] [PubMed] [Google Scholar]
- 2.Wennberg AMV, Wu MN, Rosenberg PB, Spira AP. Sleep disturbance, cognitive decline, and dementia: A review. Semin Neurol. 2017;37(4):395–406. 10.1055/s-0037-1604351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27(7):1255–1273. 10.1093/sleep/27.7.1255 [DOI] [PubMed] [Google Scholar]
- 4.Gooneratne NS, Vitiello MV. Sleep in older adults: normative changes, sleep disorders, and treatment options. Clin Geriatr Med. 2014;30(3):591–627. 10.1016/j.cger.2014.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schweitzer PK, Feren SD. Pharmacological treatment of insomnia. In: Attarian HP, ed. Clinical Handbook of Insomnia. Third ed. Chicago, IL: Springer; 2017. [Google Scholar]
- 6.Vitiello MV, Borson S. Sleep disturbances in patients with Alzheimer’s disease: epidemiology, pathophysiology and treatment. CNS Drugs. 2001;15(10):777–796. 10.2165/00023210-200115100-00004 [DOI] [PubMed] [Google Scholar]
- 7.Deschenes CL, McCurry SM. Current treatments for sleep disturbances in individuals with dementia. Curr Psychiatry Rep. 2009;11(1):20–26. 10.1007/s11920-009-0004-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peter-Derex L, Yammine P, Bastuji H, Croisile B. Sleep and Alzheimer’s disease. Sleep Med Rev. 2015;19:29–38. 10.1016/j.smrv.2014.03.007 [DOI] [PubMed] [Google Scholar]
- 9.McPhillips MV, Dickson VV, Cacchione PZ, Li J, Gooneratne N, Riegel B. Nursing home eligible, community-dwelling older adults’ perceptions and beliefs about sleep: a mixed-methods study. Clin Nurs Res. 2020;29(3):177–188. 10.1177/1054773819849348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Figueiro MG, Plitnick B, Roohan C, Sahin L, Kalsher M, Rea MS. Effects of a tailored lighting intervention on sleep quality, rest-activity, mood, and behavior in older adults with alzheimer disease and related dementias: a randomized clinical trial. J Clin Sleep Med. 2019;15(12):1757–1767. 10.5664/jcsm.8078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alessi CA, Yoon EJ, Schnelle JF, Al-Samarrai NR, Cruise PA. A randomized trial of a combined physical activity and environmental intervention in nursing home residents: do sleep and agitation improve? J Am Geriatr Soc. 1999;47:784–791. 10.1111/j.1532-5415.1999.tb03833.x [DOI] [PubMed] [Google Scholar]
- 12.Salami O, Lyketsos C, Rao V. Treatment of sleep disturbance in Alzheimer’s dementia. Int J Geriatr Psychiatry. 2011;26(8):771–782. 10.1002/gps.2609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Niet G, Tiemens B, Lendemeijer B, Hutschemaekers G. Music-assisted relaxation to improve sleep quality: meta-analysis. J Adv Nurs. 2009;65(7):1356–1364. 10.1111/j.1365-2648.2009.04982.x [DOI] [PubMed] [Google Scholar]
- 14.Kaufmann CN, Montross-Thomas LP, Griser S. Increased engagement with life: differences in the cognitive, physical, social, and spiritual activities of older adult music listeners. Gerontologist. 2018;58(2):270–277. 10.1093/geront/gnw192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Livesey L, Morrison I, Clift S, Camic P. Benefits of choral singing for social and mental wellbeing: qualitative findings from a cross‐national survey of choir members. J Public Ment Health. 2012;11(1):10–26. https://psycnet.apa.org/doi/10.1108/17465721211207275 [Google Scholar]
- 16.Chen C-K, Pei Y-C, Chen N-H, et al. Sedative music facilitates deep sleep in young adults. J Altern Complement Med. 2014;20(4):312–317. 10.1089/acm.2012.0050 [DOI] [PubMed] [Google Scholar]
- 17.Linnemann A, Ditzen B, Strahler J, Doerr JM, Nater UM. Music listening as a means of stress reduction in daily life. Psychoneuroendocrinology. 2015;60:82–90. 10.1016/j.psyneuen.2015.06.008 [DOI] [PubMed] [Google Scholar]
- 18.Lai HL. Music preference and relaxation in Taiwanese elderly people. Geriatr Nurs. 2004;25(5):286–291. 10.1016/j.gerinurse.2004.08.009 [DOI] [PubMed] [Google Scholar]
- 19.Dickson GT, Schubert E. How does music aid sleep? literature review. Sleep Med. 2019;63:142–150. 10.1016/j.sleep.2019.05.016 [DOI] [PubMed] [Google Scholar]
- 20.Trahan T, Durrant SJ, Mullensiefen D, Williamson VJ. The music that helps people sleep and the reasons they believe it works: A mixed methods analysis of online survey reports. PloS one. 2018;13(11):e0206531. 10.1371/journal.pone.0206531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang Q, Chair SY, Wong EM, Li X. The effects of music intervention on sleep quality in community-dwelling elderly. J Altern Complement Med. 2016;22(7):576–584. 10.1089/acm.2015.0304 [DOI] [PubMed] [Google Scholar]
- 22.Innes KE, Selfe TK, Khalsa DS, Kandati S. Effects of meditation versus music listening on perceived stress, mood, sleep, and quality of life in adults with early memory loss: a pilot randomized controlled trial. J Alzheimers Dis. 2016;52(4):1277–1298. 10.3233/JAD-151106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shum A, Taylor BJ, Thayala J, Chan MF. The effects of sedative music on sleep quality of older community-dwelling adults in Singapore. Complement Ther Med. 2014;22(1):49–56. 10.1016/j.ctim.2013.11.003 [DOI] [PubMed] [Google Scholar]
- 24.Jespersen KV, Koenig J, Jennum P, Vuust P. Music for insomnia in adults. Cochrane Database Syst Rev. 2015(8):CD010459. 10.1002/14651858.CD010459.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robb SL, Hanson-Abromeit D, May L, et al. Reporting quality of music intervention research in healthcare: A systematic review. Complement Ther Med. 2018;38:24–41. 10.1016/j.ctim.2018.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.He W, Muenchrath MN, Kowal P. Shades of Gray: A Cross-Country Study of Health and Well-Being of the Older Populations in SAGE Countries, 2007–2010. Washington, DC, 2012. Available at : https://www.census.gov/content/dam/Census/library/publications/2012/demo/p95-12-01.pdf [Google Scholar]
- 27.Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020) 2020. www.training.cochrane.org/handbook. Accessed June 1, 2020.
- 28.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Br Med J 2015;349:g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 29.Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Chapter 3: Systematic reviews of effectiveness. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. JBI; 2020. [Google Scholar]
- 30.Ziv N, Rotem T, Arnon Z, Haimov I. The effect of music relaxation versus progressive muscular relaxation on insomnia in older people and their relationship to personality traits. J Music Ther. 2008;45(3):360–380. 10.1093/jmt/45.3.360 [DOI] [PubMed] [Google Scholar]
- 31.Weise L, Töpfer NF, Deux J, Wilz G. Feasibility and effects of individualized recorded music for people with dementia: A pilot RCT study. Nord J Music Ther. 2020;29(1):39–56. 10.1080/08098131.2019.1661507 [DOI] [Google Scholar]
- 32.Chan MF, Chan EA, Mok E. Effects of music on depression and sleep quality in elderly people: A randomised controlled trial. Complement Ther Med. 2010;18(3–4):150–159. 10.1016/j.ctim.2010.02.004 [DOI] [PubMed] [Google Scholar]
- 33.Satoh M, Yuba T, Tabei K, et al. Music therapy using singing training improves psychomotor speed in patients with alzheimer’s disease: a neuropsychological and fMRI study. Dement Geriatr Cogn Dis Extra. 2015;5(3):296–308. 10.1159/000436960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Choi N. The effects of hand massage using aroma essential oil and music therapy on anxiety and sleeping for elderly women in the sanatorium. Int J Bio-Sci Bio-Technol. 2015;7(5):151–158. 10.14257/ijbsbt.2015.7.5.14 [DOI] [Google Scholar]
- 35.Rawtaer I, Mahendran R, Chan HY, Lei F, Kua EH. A nonpharmacological approach to improve sleep quality in older adults. Asia Pac Psychiatry. 2018;10(2). 10.1111/appy.12301 [DOI] [PubMed] [Google Scholar]
- 36.Yap AF, Kwan YH, Tan CS, Ibrahim S, Ang SB. Rhythm-centred music making in community living elderly: a randomized pilot study. BMC Complement Altern Med. 2017;17(1). 10.1186/s12906-017-1825-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lai HL, Chang ET, Li YM, Huang CY, Lee LH, Wang HM. Effects of music videos on sleep quality in middle-aged and older adults with chronic insomnia: a randomized controlled trial. Biol Res Nurs. 2015;17(3):340–347. 10.1177/1099800414549237 [DOI] [PubMed] [Google Scholar]
- 38.Lai HL, Good M. Music improves sleep quality in older adults. J Adv Nurs. 2005;49(3):234–244. 10.1111/j.1365-2648.2004.03281.x [DOI] [PubMed] [Google Scholar]
- 39.Huang CY, Chang ET, Lai HL. Comparing the effects of music and exercise with music for older adults with insomnia. Appl Nurs Res. 2016;32:104–110. 10.1016/j.apnr.2016.06.009 [DOI] [PubMed] [Google Scholar]
- 40.Innes KE, Selfe TK, Kandati S, Wen S, Huysmans Z. Effects of mantra meditation versus music listening on knee pain, function, and related outcomes in older adults with knee osteoarthritis: an exploratory randomized clinical trial (RCT). Evid Based Complement Alternat Med. 2018;2018 10.1155/2018/7683897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Johnson JE. The use of music to promote sleep in older women. J Community Health Nurs. 2003;20(1):27–35. 10.1207/S15327655JCHN2001_03 [DOI] [PubMed] [Google Scholar]
- 42.Wahbeh H, Nelson M. iRest meditation for older adults with depression symptoms: a pilot study. Int J Yoga Therap. 2019;29(1):9–17. 10.17761/2019-00036 [DOI] [PubMed] [Google Scholar]
- 43.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 44.Huang CY, Chang ET, Lai HL. Comparing the effects of music and exercise with music for older adults with insomnia. Appl Nurs Res. 2016;32:104–110. 10.1016/j.apnr.2016.06.009 [DOI] [PubMed] [Google Scholar]
- 45.Gerdner LA. Evidence-Based Guideline: Individualized Music for Persons with Dementia (6th Edition). Ann Arbor, Michigan: National Nursing Practice Network; University of Michigan, School of Nursing; 2018. [Google Scholar]
- 46.Hu RF, Jiang XY, Hegadoren KM, Zhang YH. Effects of earplugs and eye masks combined with relaxing music on sleep, melatonin and cortisol levels in ICU patients: a randomized controlled trial. Crit Care. 2015;19:115. 10.1186/s13054-015-0855-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu YH, Lee CS, Yu CH, Chen CH. Effects of music listening on stress, anxiety, and sleep quality for sleep-disturbed pregnant women. Women Health. 2015;56(3):296–311. 10.1080/03630242.2015.1088116 [DOI] [PubMed] [Google Scholar]
- 48.Sanchez A, Maseda A, Marante-Moar MP, de Labra C, Lorenzo-Lopez L, Millan-Calenti JC. Comparing the effects of multisensory stimulation and individualized music sessions on elderly people with severe dementia: a randomized controlled trial. J Alzheimers Dis. 2016;52(1):303–315. 10.3233/JAD-151150 [DOI] [PubMed] [Google Scholar]
- 49.Maseda A, Cibeira N, Lorenzo-Lopez L, et al. Multisensory stimulation and individualized music sessions on older adults with severe dementia: effects on mood, behavior, and biomedical parameters. J Alzheimers Dis. 2018;63(4):1415–1425. 10.3233/jad-180109 [DOI] [PubMed] [Google Scholar]


