Abstract
BACKGROUND
Intra-articular osteoid osteoma (iaOO) can be found in 5.2% up to 10% of cases. They may cause non-specific symptoms, mimicking degenerative or traumatic pathologies. If iaOO is left untreated, it may lead to severe muscle atrophy, tenderness, swelling, and limited range of motion. Therefore, surgical treatment is recommended. The main goal of surgical treatment is complete removal or destruction of iaOO.
AIM
To evaluate the efficiency of arthroscopic removal of iaOO of the knee in our cases and cases available in the literature.
METHODS
Analysis of available hospital records of four patients with iaOO of the knee treated by arthroscopic removal from August 2005 to December 2015 at our Department was performed. All patients had a diagnosis of iaOO confirmed by histopathologic analysis. Additional literature review of cases of iaOO of the knee available on PubMed and Google Scholar was made. All cases of iaOO of the knee treated by arthroscopic or arthroscopically assisted removal were reviewed in order to further evaluate the efficiency of the method.
RESULTS
The average age of patients included in our study was 23.2 (range 16-37) years. The average duration of the symptoms prior to surgery was 14.2 (range 6-24) months. All of the patients had persistent knee pain. Three patients reported worsening of pain during the night, while two reported worsening of pain during activity. Three patients reported alleviation of pain on non-steroidal anti-inflammatory drugs (NSAIDs), while one patient reported partial alleviation of pain on NSAIDs. No intraoperative complications were noted, and the postoperative period was uneventful in all patients. The patients reported immediate pain relief in the postoperative period. No recurrence of the disease was noted in any of the patients during the follow-up period of at least 24 mo. The literature review revealed 14 cases with an average age of 27.6 (range 16-48) years and onset of symptoms 27.7 (range 6-108) months prior to surgery, with recurrence of the disease noted in a single case.
CONCLUSION
Arthroscopic removal is an efficient treatment method that allows excision of iaOO that is neither insufficient nor excessive, thus avoiding disease recurrence while obtaining adequate material for histopathologic analysis.
Keywords: Osteoid osteoma, Knee, Arthroscopy, Bone diseases, Surgical procedures, Operative, Pathology, Surgical
Core Tip: Advantages of the arthroscopic or arthroscopic assisted removal of the intra-articular osteoid osteoma of the knee are the ability to obtain adequate material for histopathologic analysis and to perform neither excessive nor insufficient excision, thus avoiding disease recurrence, as well as chondral lesions and bone necrosis.
INTRODUCTION
Osteoid osteoma (OO) is a third most common benign lesion of the bone, commonly localized in the diaphysis of long bones of the lower extremity[1]. Studies report that intra-articular OO (iaOO) can be found in 5.2% up to 10% of cases, with the knee being the third most common localization, after the hip and ankle[1,2]. In 1986, Heuijerjans et al[3] reported on a first successful arthroscopic removal of iaOO. Since then, arthroscopic removal of iaOO was frequently used in various joints, with a high success rate and a low recurrence rate[4-7]. However, despite the first-ever reported arthroscopic removal of iaOO was in the knee, only case reports can be found on this topic in the literature.
The aim of this study was to present the first case series of patients treated with arthroscopic removal of iaOO of the knee and to give a literature overview of arthroscopic and arthroscopically assisted removal of such lesions.
MATERIALS AND METHODS
Case series collection
This research has been approved by the Institutional Ethics Committee of the authors’ affiliated institutions. A retrospective analysis of available hospital records revealed four consecutive patients diagnosed with OO of the knee confirmed by histopathologic analysis that were treated by arthroscopic removal from August 2005 to December 2015 at our Department. All of the patients have agreed to participate in the study. Available hospital records were reviewed in December 2020 by an independent examiner who was not involved in the treatment process. Demographic information, including age and gender, as well as clinical characteristics, such as symptoms, effects of non-steroidal anti-inflammatory drugs (NSAIDs) on pain relief, duration of the symptoms until the accurate diagnosis, history of trauma, diagnostic imaging utilized preoperatively, intraoperative findings, results of histopathological analysis, follow-up duration and recurrence of the disease were analyzed.
Surgical technique
The senior author performed arthroscopic removal of iaOO of the knee in all patients (Table 1). Patients were in a supine position, under spinal anesthesia, with the affected knee placed in a leg holder. A tourniquet was applied in all of the procedures. Knee arthroscopy was performed with a 4.0 mm arthroscope angled at 30°. Standard anteromedial and anterolateral portals were used in all of the procedures, while in some, due to OO’s localization, additional portals were utilized (Figures 1 and 2)[8,9]. After a thorough examination of the knee, a cherry-red, elevated lesion was localized, consistent with the typical appearance of the nidus. An arthroscopic curette was used to remove the nidus, and an arthroscopic grasper was used to remove the tissue, obtaining a suitable specimen for histopathologic analysis. An arthroscopic burr and curette were used to remove the remaining part of the lesion and surrounding bone sclerosis until visualizing healthy trabecular bone. Afterward, lavage of the knee was performed. Insertion of a drain through the anterolateral portal and closure of the skin at the arthroscopic portals followed.
Table 1.
Demographic information, clinical presentation, preoperative and postoperative features of the patients treated by arthroscopic removal of intra-articular osteoid osteoma of the knee
|
Age (yr)/gender
|
Side
|
Symptoms
|
Pain alleviating on NSAIDs
|
Duration of symptoms until the accurate diagnosis (mo)
|
Trauma history
|
Location
|
Diagnostic imaging
|
Arthroscopic portals
|
HPA confirmed osteoid osteoma
|
Follow-up (mo)
|
Recurrence
|
| 16/F | L | Persistent knee pain worsening at night | Yes | 15 | Yes | Anterolateral part of the femur above the cartilage border of the trochlea | CT, bone scan | AM, AL, SL | Yes | 171 | No |
| 23/M | L | Persistent knee pain worsening in activity and at night | Partially | 24 | No | Anteromedial part of the femur on the cartilage border of the trochlea | MRI (2)1, bone scan | AM, AL | Yes | 24 | No |
| 17/F | L | Persistent knee pain worsening in activity and at night | Yes | 6 | No | Anterolateral part of the femur above the cartilage border of the trochlea | MRI, CT | AM, AL, SL | Yes | 55 | No |
| 37/F | R | Persistent knee pain and swelling | Yes | 12 | No | Posterior aspect of the lateral femoral condyle | MRI, CT, bone scan | AM, AL, PM, PL | Yes | 24 | No |
Patient had a first magnetic resonance imaging (MRI) performed, after which another physician performed an open biopsy at our department. As the symptoms persisted over the course of 10 mo, the patient was referred to the senior author to re-evaluate the case. After detailed analysis, the senior author suspected of intra-articular osteoid osteoma (iaOO) of the knee and issued a bone scan and a follow-up MRI, which confirmed the diagnosis of iaOO of the knee. NSAIDs: Non-steroidal anti-inflammatory drugs; HPA: Histopathologic analysis; F: Female; M: Male; CT: Computerized tomography; MRI: Magnetic resonance imaging; AM: Anteromedial; AL: Anterolateral; SL: Superolateral; PM: Posteromedial; PL: Posterolateral.
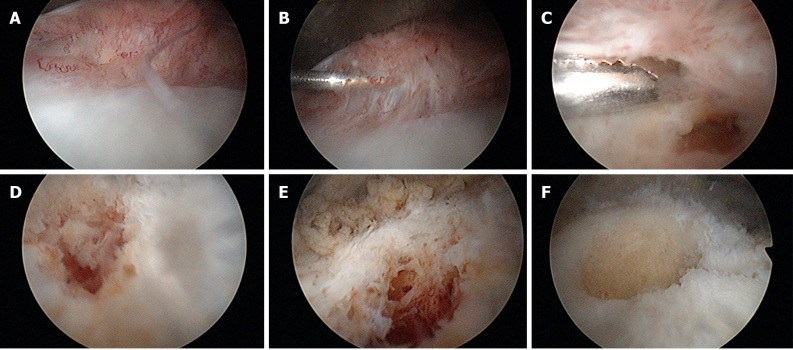
Figure 1.
Sequential arthroscopic views of the anteromedial part of the femur above the cartilage with the arthroscope in the anterolateral portal. A: synovial hyperplasia; B: Palpation of the elevated synovial tissue with a probe; C: Removal of the synovial tissue reveals the altered tissue; D and E: After partial removal, the extensiveness of the altered tissue is revealed; F: The remaining crater after complete removal of the lesion.
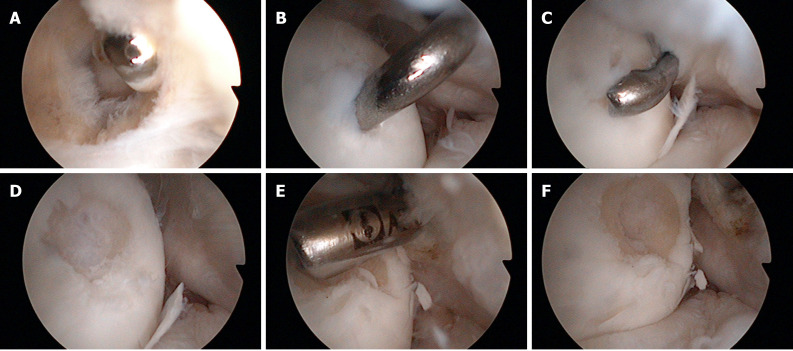
Figure 2.
Sequential arthroscopic views of posterior part of lateral femoral condyle with the arthroscope positioned in the posteromedial portal. A: Trans-septal approach; B: Palpation of the altered tissue with a probe from the posterolateral portal; C: Removal of the altered tissue with a cochlea; D: Visualization of the sclerotic bone after removal of altered tissue; E: Removal of the nidus and surrounding sclerosis with a motorized instrument; F: The remaining crater after complete removal of the lesion.
Postoperative management
All patients followed the same postoperative regimen. On the first postoperative day, the drain was removed, and the patients started active and passive range of motion exercises. Partial weight-bearing as tolerated with crutches was advised for the first two weeks, with full weight-bearing advised afterward. During the first postoperative month, they underwent a course of physiotherapy, consisting of range of motion and strengthening exercises. The patients underwent monthly follow-up examinations for the first three postoperative months. After that, the follow-up visits were scheduled at six, twelve, and 24 mo postoperatively.
Literature review
A literature review of cases with iaOO of the knee available on PubMed and Google Scholar was made. Search strategy for PubMed included two search queries: (1) Osteoma, Osteoid[MeSH] AND Knee[MeSH]; and (2) osteoid osteoma AND knee. Search strategy for Google Scholar included one search query: osteoid osteoma AND knee. The search was performed on December 29, 2020. All results available on PubMed and the first 1000 results on Google Scholar were screened. Only cases of iaOO of the knee treated by arthroscopic or arthroscopically assisted removal were included and further reviewed in order to evaluate the efficiency of the method.
Data interpretation
Statistical analyses were performed using SPSS (version 21). Continuous variables were described as average (range minimum-maximum). The normality of distribution was tested using the Shapiro-Wilks test.
RESULTS
Demographic information, clinical presentation, preoperative and postoperative features of the patients treated by arthroscopic removal of iaOO of the knee are presented in Table 1. The average patient age was 23.2 (range 16-37) years. The average duration of the symptoms prior to surgery was 14.2 (range 6-24) months. Symptoms occurred in one patient after suffering a first-time lateral patellar dislocation, which became recurrent over time. One of the patients underwent an open biopsy performed by another physician ten months before he was referred to the senior author for re-evaluation. The biopsy was performed in an incorrect location of the bone due to an extensive bone marrow edema found on magnetic resonance imaging (MRI) in the medial femoral condyle. The result of the biopsy was negative, and patient’s symptoms persisted. A detailed analysis of symptoms showed the patient had worsening of pain at night and after activity, which partially alleviated on NSAIDs. As the senior author suspected of iaOO of the knee, a bone scan and a follow-up MRI were performed that confirmed the diagnosis of iaOO. Computerized tomography (CT) was performed in other patients to better localize the lesion, thus allowing efficient preoperative planning.
No intraoperative complications were noted, and the postoperative period was uneventful in all patients. The patients reported immediate pain relief in the postoperative period. No recurrence of the disease was noted in any of the patients during the follow-up period of at least 24 mo.
The literature review revealed 14 cases of iaOO of the knee treated by arthroscopic or arthroscopically assisted removal, which are presented in Table 2[1,3,10-20]. The average age of those patients was 27.6 (range 16-48) years, the average onset of symptoms was 27.7 (range 6-108) mo prior to surgery, and recurrence of the disease was noted in a single case.
Table 2.
Literature review of cases with intra-articular osteoid osteoma of the knee treated by arthroscopic or arthroscopically assisted removal
|
Ref.
|
Age (yr) /gender
|
Side
|
Symptoms
|
Pain alleviating on NSAIDs
|
Duration of symptoms until the accurate diagnosis (mo)
|
Trauma history
|
Location
|
Diagnostic imaging
|
Surgery
|
HPA confirmed osteoid osteoma
|
Follow-up (mo)
|
Recurrence
|
| Heuijerjans et al[3], 1986 | 29/F | NR | Knee pain, limited ROM | NR | 108 | NR | Lateral tibial plateau | NR | Arthroscopic removal | Yes | 18 | No |
| Franceschi et al[13], 2005 | 28/M | NR | Light knee pain worsening at night, swelling, limited ROM | Yes | 12 | NR | Lateral tibial plateau | MRI, CT | Arthroscopically assisted removal – percutaneous K wire insertion to the tumor under CT, arthroscopic visualization of the knee, tumor removal by a core reamer and curettage, bone defect filled with autologous bone graft from proximal tibia | Yes | 24 | No |
| Franceschi et al[14], 2008 | 16/F | L | Light knee pain worsening at night, swelling, limited ROM | Yes | NR | NR | Central region of the patella | MRI, CT, bone scan | Arthroscopically assisted removal – percutaneous K wire insertion to the tumor under CT, arthroscopic visualization of the knee, tumor removal by a hollow drill and curettage, bone defect filled with autologous bone graft from proximal tibia | Yes | 36 | No |
| Abnousi et al[15], 2008 | 35/M | L | Diffuse dull knee pain worsening on activity, limited ROM, swelling | Partially | 24 | No | Medial femoral condyle | MRI, CT | Arthroscopically assisted removal – arthroscopic visualization of the tumor and en-bloc resection via miniature arthrotomy | Yes | 22 | No |
| Gunes et al[16], 2008 | 18/M | R | Knee pain worsening at night | Yes | 6 | NR | Medial femoral condyle | MRI, CT | Arthroscopic removal | Yes | 15 | No |
| Furukawa et al[17], 2011 | 23/F | L | Persistent knee painworsening at night, swelling | Partially | 24 | NR | Lateral femoral condyle | MRI, CT, bone scan | Arthroscopic removal | Yes | 24 | No |
| Saeed et al[18], 2011 | 38/M | L | Mild knee pain worsening at night | Yes | 26 | NR | Lateral tibial plateau | MRI, CT, bone scan | Arthroscopic removal | Yes | 72 | Yes1 |
| Adachi et al[19], 2014 | 32/M | L | Severe knee pain, worsening at night, limited ROM | Partially | NR | No | Lateral tibial plateau | MRI | Arthroscopically assisted removal – arthroscopic visualization of the tumor, insertion of a K wire in the tumor under fluoroscopy and removal with core reamer, bone defect filled with artificial bone | Yes | 18 | No |
| Kang et al[20], 2016 | 20/F | R | Mild knee pain worsening at night | No | 12 | No | Lateral femoral condyle | MRI, CT, bone scan | Arthroscopic removal | Yes | 24 | No |
| Rolvien et al[1], 2016 | 26/M | NR | Knee pain worsening at night | Yes | 24 | No | Lateral tibial plateau | MRI, CT | Arthroscopic removal | Yes | 3 | No |
| Krause et al[10], 2016 | 26/M | NR | Knee pain worsening at night | Partially | 19 | NR | Lateral tibial plateau | MRI, CT | Arthroscopic removal | Yes | 3 | No |
| Rolvien et al[11], 2019 | 48/M | R | Persistent knee pain | Yes | 24 | NR | Lateral femoral condyle | MRI, CT | Arthroscopic removal | Yes | NR | NR |
| Monroe et al[12], 2019 | 20/M | R | Knee pain worsening in activity | No | 18 | No | Medial femoral trochlea | MRI, CT | Arthroscopic removal – bone defect filled with allograft | Yes | 84 | No |
| 28/M | R | Persistent knee pain | Partially | 36 | NR | Medial femoral condyle | MRI, CT | Arthroscopically assisted removal – arthroscopic visualization of the tumor and removal via small arthrotomy, bone defect filled with allograft | Yes | 6 | No |
Six years following the arthroscopic removal, the patient had similar symptoms, and the follow-up imaging revealed recurrence of the osteoid osteoma at the same location. Another arthroscopic removal could cause extensive damage of the lateral tibial plateau, and to avoid such complication, the authors decided to perform an unicondylar knee arthroplasty. HPA: histopathologic analysis, NSAIDs: Non-steroidal anti-inflammatory drugs; NR: Not reported; F: Female; M: Male; MRI: Magnetic resonance imaging; CT: Computerized tomography; K: Kirschner; ROM: Range of motion.
DISCUSSION
This article reports on a successful treatment of iaOO of the knee using arthroscopy. Patients suffering from iaOO usually have non-specific and variable symptoms, different from the classic night pain relieved by NSAIDs found in extra-articular OOs[21]. Such clinical presentation may mislead the clinician to suspect other more common knee pathologies such as meniscal or chondral lesions[15]. A study of patients with OO that presented with knee pain showed that in 60% of them, OO was located adjacent to the hip or in the middle femoral shaft instead of the knee[22]. Moreover, some authors suggest that the worsening of pain during the night in iaOO is not typical as for extra-articular OOs[21,23,24]. However, in more than 80% of reviewed cases and three of our cases, patients complained of worsening pain during the night. Furthermore, Spiker et al[7] reviewed cases of iaOO of the hip and showed that in cases that recorded the presence of pain during the night, 83.3% reported positive. Also, Allen et al[23] report that iaOOs are less responsive to NSAIDs than extra-articular OO. Spiker et al[7] report that in iaOO of the hip in cases which recorded the effect of NSAIDs on pain, 69.7% reported alleviation of pain on NSAIDs. From cases of iaOO of the knee that recorded the effect of NSAIDs, 84.6% reported on either partial or complete alleviation of pain on NSAIDs[1,3,10-20].
Szendroi et al[2] state that plain radiographs were sufficient for diagnosis of iaOO prior to surgery in 36.8%, compared to 73.3% for diagnosis of extra-articular OOs. Furthermore, Papagrigorakis et al[25] state that when the first symptoms occur in iaOO patients, over 80% of patients have no visible nidus or sclerosis on plain radiographs. Therefore, further diagnostic imaging is often needed. As clinicians commonly suspect other more common knee pathologies, MRI is usually issued as a diagnostic procedure after obtaining plain radiographs. MRI may be useful in obtaining a correct diagnosis. However, joint effusion, bone edema, and soft tissue edema are frequently present and may mask the nidus[17,26]. Furthermore, Allen et al[23] note that the nidus is either not visible or poorly visible in 50% of iaOOs on MRI. Moreover, Bhure et al[27] reported that MRI may lead to misdiagnosis in up to 35% of cases if used as a solitary diagnostic procedure. Therefore, MRI findings combined with non-specific symptoms may mimic conditions such as osteomyelitis or malignant bone tumors[28]. Such a case occurred in one of our patients, who underwent an open biopsy performed in the incorrect location on the bone, resulting in persistence of symptoms and delay in diagnosis.
If MRI does not confirm iaOO, further diagnostic imaging is issued. A bone scan proved to be useful in diagnosing iaOO. It lacks the usual “double-density” sign seen in extra-articular OOs, but it presents with increased focal uptake matching with the localization of the nidus[23]. When the localization is found, a CT scan may be performed. Assoun et al[26] report that CT scan proved to be more accurate than MRI in detection of the nidus in 63% of cases. Also, CT scans proved to be a valuable tool in preoperative planning of the surgery[29]. Therefore, we have performed a CT scan in three of our patients.
Peculiarities of the clinical presentation and diagnostic imaging of iaOOs lead to a significant delay in diagnosis in comparison to extra-articular OOs. Rolvien et al[1] report that the mean time for a correct diagnosis of iaOO was 20.7 mo, while Szendroi et al[2] state that the mean time for diagnosing extra-articular OO was 8.5 mo in comparison to 26.6 mo for iaOO. When considering the duration of symptoms of iaOO of the knee, the average duration until obtaining a diagnosis in our patients was 14.2 mo (range 6-24), while of those we have analyzed from the literature was 27.7 mo (range 6-108)[1,3,10-20]. The symptoms duration in our patients is somewhat shorter than reported in the literature. However, due to the small number of cases we report, we consider that the actual delay in diagnosis is usually closer to the average expressed from the analyzed literature.
Nowadays, the treatment of choice for extra-articular OOs is the CT-guided radiofrequency ablation (RFA), with a success rate of up to 97%[10]. However, the treatment of iaOO with RFA requires certain precautions, as this method may cause a cortical and bone marrow necrosis of up to 1.3 cm in diameter[30]. As iaOO may be located close to the cartilage and other joint tissues, this may be the limiting factor for the use of RFA. Another minimally invasive method that proved to be efficient is the CT-guided percutaneous resection[14]. However, percutaneous resection may result in cutaneous necrosis, neurapraxia, osteomyelitis, and fractures[14]. Furthermore, these methods are often unable to provide a sufficient sample for the histopathologic analysis[17].
The most significant concerns of arthroscopic removal of iaOO are the difficulty of localization of the lesion intraoperatively and the possibility of recurrence due to incomplete excision. However, with adequate preoperative planning, the advantage of great visualization allowed by 30° and 70° arthroscopes, and possible intraoperative fluoroscopic assessment, we believe no difficulties in localizing iaOO should occur. So far, for only one arthroscopically treated case of iaOO of the knee recurrence of the disease was reported, meaning the success rate of this method is 94.4%[1,3,10-20]. The success rate of arthroscopic removal of iaOO in the ankle is 96%, in the upper extremity is 93.8%, while in the hip is 100%[4-7]. Advantages of the arthroscopic removal are the ability to obtain adequate material for histopathologic analysis and to perform an excision of iaOO that would neither be insufficient nor excessive, thus avoiding both recurrence of the disease, as well as chondral lesions and bone necrosis. As Furukawa et al[17] note, arthroscopic removal is at least as effective as CT-guided methods for both localizing and removal of the lesion.
Localization of iaOO in our case series was on the femur exclusively, with 3 cases proximal to the superior cartilage border of the trochlea and one case in the posterior part of the lateral femoral condyle (Table 1). On the contrary, seven cases from the literature report that iaOO was localized on the femoral side, six were on the tibial side, and one was in the patella (Table 2)[1,3,10-20]. However, due to the relatively small number of cases, it is difficult to pinpoint the typical localization of the iaOO in the knee.
This study has shown the efficiency of arthroscopic removal of iaOO of the knee. However, its retrospective nature presents a limitation. Furthermore, we have not compared our results with open surgical treatment or removal of OO in other locations, as these also represent the limitations of this study. Due to a small number of cases in our study, as well as limited availability of more valued study designs in the literature, we did not find it justified to compare our results with arthroscopic treatment of iaOO in other locations, which have much larger case series. This suggests that only uncommon and novel cases of iaOO of the knee have been published, and further research will additionally clarify peculiarities of this pathology. Moreover, a possible limitation to the study is that no follow-up diagnostic imaging was performed. However, it is suggested that follow-up diagnostic imaging should be performed only in patients with a thorough suspicion of a recurrence of OO. Therefore, as our patients were all symptom-free during follow-up, we believed no diagnostic imaging is needed.
CONCLUSION
Our case series, as well as the literature review, suggest that arthroscopic removal is an efficient and safe method of treatment in patients with intra-articular osteoid osteoma of the knee. It enables excision of the tumor that is neither insufficient nor excessive, thus avoiding both recurrence of the disease, as well as chondral lesions and bone necrosis, while obtaining adequate material for histopathologic analysis. Therefore, arthroscopic removal should be considered as a treatment option when dealing with this rare entity.
ARTICLE HIGHLIGHTS
Research background
Intra-articular osteoid osteoma of the knee is a rare entity that may present with non-specific symptoms and may lead to severe disability if left untreated. There are several treatment options, one of which is arthroscopic removal.
Research motivation
As there is a low number of reported cases of intra-articular osteoid osteoma of the knee, our goal was to report our results and further elaborate on the results available in the literature.
Research objectives
To analyze whether arthroscopic removal is an effective treatment option for intra-articular osteoid osteoma of the knee.
Research methods
A first case series ever of such patients was reported, as well as the review of all available cases in the literature that report on the same pathology and treatment options.
Research results
Both the case series and cases from the literature report that arthroscopic removal of intra-articular osteoid osteoma is an effective treatment option with a low chance for recurrence of the disease.
Research conclusions
Arthroscopic removal of intra-articular osteoid osteoma enables excision that is neither insufficient nor excessive, thus avoiding both recurrence of the disease, as well as chondral lesions and bone necrosis, while obtaining adequate material for histopathologic analysis. Therefore, it should be considered as a treatment option if physicians come across such a case.
Research perspectives
Future research will additionally clarify the efficiency of arthroscopic removal of intra-articular osteoid osteoma, possibly on a larger case series than reported in this article and in the literature so far.
Footnotes
Institutional review board statement: The study was approved by the Institutional Ethics Committee (8.1-20/187-2 No. 02/21 AG).
Informed consent statement: All participants agreed to be enrolled in the study.
Conflict-of-interest statement: The authors declare that there is no conflict of interest.
STROBE statement: The authors have read the STROBE Statement-checklist of items, and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
Manuscript source: Invited manuscript
Peer-review started: February 27, 2021
First decision: March 31, 2021
Article in press: July 12, 2021
Specialty type: Orthopedics
Country/Territory of origin: Croatia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Labusca L S-Editor: Wang JL L-Editor: A P-Editor: Xing YX
Contributor Information
Mihovil Plečko, Department of Orthopedic Surgery, University Hospital Centre Zagreb, Zagreb 10000, Croatia. mplecko@kbc-zagreb.hr.
Alan Mahnik, Department of Orthopedic Surgery, University Hospital Centre Zagreb, Zagreb 10000, Croatia.
Damjan Dimnjaković, Department of Orthopedic Surgery, University Hospital Centre Zagreb, Zagreb 10000, Croatia.
Ivan Bojanić, Department of Orthopedic Surgery, University Hospital Centre Zagreb, Zagreb 10000, Croatia; Department of Orthopedic Surgery, School of Medicine, University of Zagreb, Zagreb 10000, Croatia.
Data sharing statement
No additional data are available.
References
- 1.Rolvien T, Zustin J, Mussawy H, Schmidt T, Pogoda P, Ueblacker P. Intra-articular osteoid osteoma as a differential diagnosis of diffuse mono-articular joint pain. BMC Musculoskelet Disord . 2016;17:455. doi: 10.1186/s12891-016-1313-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Szendroi M, Köllo K, Antal I, Lakatos J, Szoke G. Intraarticular osteoid osteoma: clinical features, imaging results, and comparison with extraarticular localization. J Rheumatol . 2004;31:957–964. [PubMed] [Google Scholar]
- 3.Heuijerjans W, Dandy DJ, Harris D. Arthroscopic excision of an intra-articular osteoid osteoma at the knee. Arthroscopy . 1986;2:215–216. doi: 10.1016/s0749-8063(86)80074-3. [DOI] [PubMed] [Google Scholar]
- 4.Ge SM, Marwan Y, Abduljabbar FH, Morelli M, Turcotte RE. Arthroscopic management of intra- and juxta-articular osteoid osteoma of the upper extremity: a systematic review of the literature. Eur J Orthop Surg Traumatol . 2020;30:1333–1344. doi: 10.1007/s00590-020-02710-6. [DOI] [PubMed] [Google Scholar]
- 5.Ge SM, Marwan Y, Addar A, Algarni N, Chaytor R, Turcotte RE. Arthroscopic Management of Osteoid Osteoma of the Ankle Joint: A Systematic Review of the Literature. J Foot Ankle Surg . 2019;58:550–554. doi: 10.1053/j.jfas.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 6.Marwan YA, Abatzoglou S, Esmaeel AA, Alqahtani SM, Alsulaimani SA, Tanzer M, Turcotte RE. Hip arthroscopy for the management of osteoid osteoma of the acetabulum: a systematic review of the literature and case report. BMC Musculoskelet Disord . 2015;16:318. doi: 10.1186/s12891-015-0779-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spiker AM, Rotter BZ, Chang B, Mintz DN, Kelly BT. Clinical presentation of intra-articular osteoid osteoma of the hip and preliminary outcomes after arthroscopic resection: a case series. J Hip Preserv Surg . 2018;5:88–99. doi: 10.1093/jhps/hnx042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schreiber SN. Arthroscopy update #9. Posterior compartment observation and instrumentation in the knee using anteromedial and anterolateral portals and an interchangeable cannula system. Orthop Rev . 1991;20:67–68, 73, 76. [PubMed] [Google Scholar]
- 9.Ahn JH, Ha CW. Posterior trans-septal portal for arthroscopic surgery of the knee joint. Arthroscopy . 2000;16:774–779. doi: 10.1053/jars.2000.7681. [DOI] [PubMed] [Google Scholar]
- 10.Krause M, Oheim R, Meenen NM, Frosch KH, Amling M. Intra-articular osteoid osteoma in the proximal tibia and its imaging characteristics. Knee . 2016;23:915–919. doi: 10.1016/j.knee.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Rolvien T, Krause M, Zustin J, Yastrebov O, Oheim R, Barvencik F, Frosch KH, Amling M. Intra-articular osteoid osteoma accompanied by extensive bone marrow edema. A clinical and micro-morphological analysis. J Bone Oncol . 2019;18:100256. doi: 10.1016/j.jbo.2019.100256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Monroe EJ, Chambers CC, Davoodian A, Cho SJ, Motamedi D, Allen CR. Intra-articular Osteoid Osteoma of the Distal Femur Treated with Osteochondral Grafting: A Report of 2 Cases. JBJS Case Connect . 2019;9:e0211. doi: 10.2106/JBJS.CC.18.00211. [DOI] [PubMed] [Google Scholar]
- 13.Franceschi F, Marinozzi A, Rizzello G, Papalia R, Rojas M, Denaro V. Computed tomography-guided and arthroscopically controlled en bloc retrograde resection of a juxta-articular osteoid osteoma of the tibial plateau. Arthroscopy . 2005;21:351–359. doi: 10.1016/j.arthro.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Franceschi F, Longo UG, Ruzzini L, Marinozzi A, Rizzello G, Papalia R, Denaro V. En-bloc retrograde resection of an osteoid osteoma of the patella using computed tomography under arthroscopic control. J Knee Surg . 2008;21:136–140. doi: 10.1055/s-0030-1247808. [DOI] [PubMed] [Google Scholar]
- 15.Abnousi F, Saliman JD, Fanton GS. Arthroscopic visualization and assisted excision of osteoid osteoma at the knee: a case report and review. Am J Sports Med . 2008;36:375–378. doi: 10.1177/0363546507307865. [DOI] [PubMed] [Google Scholar]
- 16.Gunes T, Erdem M, Bostan B, Sen C, Sahin SA. Arthroscopic excision of the osteoid osteoma at the distal femur. Knee Surg Sports Traumatol Arthrosc . 2008;16:90–93. doi: 10.1007/s00167-007-0380-2. [DOI] [PubMed] [Google Scholar]
- 17.Furukawa M, Anazawa U, Horiuchi K, Yabe H, Morioka H, Mukai M, Toyoda T, Chiba K, Morii T, Shiraishi T, Toyama Y. Arthroscopic removal of intra-articular osteoid osteoma in the knee: case report and review of the literature. J Orthop Sci . 2011;16:321–325. doi: 10.1007/s00776-011-0060-4. [DOI] [PubMed] [Google Scholar]
- 18.Saeed MZ, Saragaglia D. Unicondylar knee replacement for intra-articular osteoid osteoma of the tibial plateau. Eur Orthop Traumatol . 2011;2:157–160. [Google Scholar]
- 19.Adachi N, Shimose S, Nakamae A, Okuhara A, Kamei G, Ochi M. Intra-articular osteoid osteoma of the lateral tibial plateau treated with arthroscopically assisted removal and retrograde osteochondral grafting. Knee . 2014;21:343–348. doi: 10.1016/j.knee.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 20.Kang S, Kim YS, Lee HM, Lee MY, Kim JP. Arthroscopic Excision of an Intraarticular Osteoid Osteoma in the Distal Femur. Clin Orthop Surg . 2016;8:475–480. doi: 10.4055/cios.2016.8.4.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.García-Germán D, Sánchez-Gutiérrez S, Bueno A, Carballo F, López-González D, Canillas F, Martel J. Intra-articular osteoid osteoma simulating a painful fabella syndrome. Knee . 2010;17:310–312. doi: 10.1016/j.knee.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 22.Georgoulis AD, Papageorgiou CD, Moebius UG, Rossis J, Papadonikolakis A, Soucacos PN. The diagnostic dilemma created by osteoid osteoma that presents as knee pain. Arthroscopy . 2002;18:32–37. doi: 10.1053/jars.2002.30010. [DOI] [PubMed] [Google Scholar]
- 23.Allen SD, Saifuddin A. Imaging of intra-articular osteoid osteoma. Clin Radiol . 2003;58:845–852. doi: 10.1016/s0009-9260(03)00213-7. [DOI] [PubMed] [Google Scholar]
- 24.Eggel Y, Theumann N, Lüthi F. Intra-articular osteoid osteoma of the knee: clinical and therapeutical particularities. Joint Bone Spine . 2007;74:379–381. doi: 10.1016/j.jbspin.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 25.Papagrigorakis E, Benetos IS, Bakalakos M, Rozis M, Pneumaticos S. A Rare Cause of Anterior Knee Pain in a Young Athlete and a Delayed Diagnosis: Osteoid Osteoma of the Patella. Cureus . 2019;11:e6420. doi: 10.7759/cureus.6420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Assoun J, Richardi G, Railhac JJ, Baunin C, Fajadet P, Giron J, Maquin P, Haddad J, Bonnevialle P. Osteoid osteoma: MR imaging versus CT. Radiology . 1994;191:217–223. doi: 10.1148/radiology.191.1.8134575. [DOI] [PubMed] [Google Scholar]
- 27.Bhure U, Roos JE, Strobel K. Osteoid osteoma: multimodality imaging with focus on hybrid imaging. Eur J Nucl Med Mol Imaging . 2019;46:1019–1036. doi: 10.1007/s00259-018-4181-2. [DOI] [PubMed] [Google Scholar]
- 28.Chai JW, Hong SH, Choi JY, Koh YH, Lee JW, Choi JA, Kang HS. Radiologic diagnosis of osteoid osteoma: from simple to challenging findings. Radiographics . 2010;30:737–749. doi: 10.1148/rg.303095120. [DOI] [PubMed] [Google Scholar]
- 29.Sagtas E, Gokkus K, Aydin AT. Intra-Articular Osteoid Osteoma as a Cause of Anteromedial Knee Pain. Case Rep Orthop . 2017;2017:5846368. doi: 10.1155/2017/5846368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tillotson CL, Rosenberg AE, Rosenthal DI. Controlled thermal injury of bone. Report of a percutaneous technique using radiofrequency electrode and generator. Invest Radiol . 1989;24:888–892. doi: 10.1097/00004424-198911000-00009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No additional data are available.