Abstract
Background
Around 184,000 deaths per year could be attributable to sugar-sweetened beverages (SSBs) consumption worldwide. Epidemiological and decision models are important tools to estimate disease burden. The purpose of this study was to identify models to assess the burden of diseases attributable to SSBs consumption or the potential impact of health interventions.
Methods
We carried out a systematic review and literature search up to August 2018. Pairs of reviewers independently selected, extracted, and assessed the quality of the included studies through an exhaustive description of each model’s features. Discrepancies were solved by consensus. The inclusion criteria were epidemiological or decision models evaluating SSBs health interventions or policies, and descriptive SSBs studies of decision models. Studies published before 2003, cost of illness studies and economic evaluations based on individual patient data were excluded.
Results
We identified a total of 2766 references. Out of the 40 included studies, 45% were models specifically developed to address SSBs, 82.5% were conducted in high-income countries and 57.5% considered a health system perspective. The most common model’s outcomes were obesity/overweight (82.5%), diabetes (72.5%), cardiovascular disease (60%), mortality (52.5%), direct medical costs (57.35%), and healthy years -DALYs/QALYs- (40%) attributable to SSBs. 67.5% of the studies modelled the effect of SSBs on the outcomes either entirely through BMI or through BMI plus diabetes independently. Models were usually populated with inputs from national surveys -such us obesity prevalence, SSBs consumption-; and vital statistics (67.5%).
Only 55% reported results by gender and 40% included children; 30% presented results by income level, and 25% by selected vulnerable groups. Most of the models evaluated at least one policy intervention to reduce SSBs consumption (92.5%), taxes being the most frequent strategy (75%).
Conclusions
There is a wide range of modelling approaches of different complexity and information requirements to evaluate the burden of disease attributable to SSBs. Most of them take into account the impact on obesity, diabetes and cardiovascular disease, mortality, and economic impact. Incorporating these tools to different countries could result in useful information for decision makers and the general population to promote a deeper implementation of policies to reduce SSBs consumption.
PROSPERO protocol number
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-021-11046-7.
Keywords: Sugar sweetened beverages (SSBs), Burden of disease, Economic evaluations, Decision models, Epidemiological models, Health policies
Background
Non-communicable diseases (NCD) were responsible for more than 50% of the global health burden in 2013, accounting for 38.3 million deaths worldwide [1]. About 80% of these premature NCD deaths occur in low- and middle-income countries (LMICs) [2]. Additionally, these non-communicable diseases have a huge attributable cost on health systems as well as to the society as a whole [3–8]. This enormous disease burden represents a major barrier to the achievement of the Millennium Development Goals [2].
Obesity is an important determinant of the burden of disease currently attributable to NCDs. In 2015, nearly 110 million children and more than 600 million adults were obese [9]. Since 1980, the prevalence of obesity has doubled in more than 70 countries and has continuously increased in most other countries [10]. The proportion of overweight or obese adults increased between 1980 and 2013 from 28.8 to 36.9% in men, and from 29.8 to 38.0% in women around the world [11]. Obesity-attributable diseases cause more than 17 million global deaths each year [9, 12]. The rates of childhood overweight and obesity have increased across all age and socioeconomic status (SES) groups. These trends have been remarkable in highly urbanized areas. Obese children are at increased risk of type 2 diabetes, high blood pressure, asthma, sleep disorders, liver disease, low self-esteem, depression and social isolation, and obese adults are more prone to cardiovascular diseases (CVD) and obesity-related cancers [13, 14].
Obesity is a multi-causal phenomenon, that includes unhealthy dietary patterns and sedentarism, among others. Dietary surveys indicate that foods and beverages high in free sugars can constitute a major source of discretionary calories: added sugars supply food energy but no other nutrients (also called “empty calories”).
Sugar sweetened beverages (SSBs) consumption has been linked to an increased risk of type 2 diabetes, obesity [13–15], obesity-related cancers [16], hypertension [17], coronary heart disease [15], and tooth decay [18–23]. Dental burden can also represent 5–10% of health-care budgets in industrialized countries, and even more so in low-income countries [24, 25].
Worldwide, it has been estimated that 184,000 deaths per year could be attributable to SSBs consumption: 133000 from diabetes mellitus, 45,000 from CVD, and 6450 from cancers [26]. .SSB consumption varies considerably by geographic location, gender, age and socio-economic status. The mean daily SSB consumption among adults was estimated at 137 mL (95% CI: 88 to 211 mL) in 2010 and is usually higher younger persons, low-income groups and among males [26], with large disparities between countries. These beverages include soft drinks, sodas, fruit drinks, sweetened coffees and teas, energy drinks, sports drinks, and sweetened waters. SSB constitutes the single largest source of added sugars in the American diet, and over 5% of overall caloric intake [27, 28]. Although full-calorie beverage consumption is declining, beverage consumption as a whole is increasing, especially with the mid-calorie drinks (e.g., sports drinks, teas, and energy drinks) [29].
Although many countries around the world are considering, or have begun to implement, a series of measures aimed at tackling SSB consumption, there is also a lack of awareness of this topic from decision-makers, stakeholders and the general population. Furthermore, many interventions (such as tax increases) meet with resistance. There is a wide range of interventions wherein decision makers and key leaders of various sectors are involved; the spectrum includes fiscal policies taxings SSB, front of package regulations, educational measures, modification of the school environment, publicity bans, promotion and sponsorship, among other interventions [30–34]. .Having information on the burden of disease such as the impact on health and the economics of SSB consumption as well as cost-effectiveness and the expected impact of implementing public health policies could facilitate moving forward [22].
Assessments based on epidemiological and decision models are widely accepted as decision-making tools and can provide valuable information for optimizing the allocation of health resources [35].
This study is part of a larger multi-country study funded by the International Development Research Centre (IDRC) and oriented to empowering healthcare decision makers to achieve regional needs in SSB policies in Latin America and the Caribbean through the evaluation of disease and economic burden, as well as the cost-effectiveness of available interventions.
The purpose of the study was to identify epidemiological or decision models to assess the burden of disease attributable to SSB consumption or the cost-effectiveness of interventions aimed at reducing SSB consumption, to describe the different methodological approaches through a systematic review. In other words, which are the best available published models applicable to assess SSB related problems?
Methods
A systematic review of the published literature was carried out according to the reporting parameters proposed in the guidelines: Preferred reporting items for systematic reviews and meta-analyses (PRISMA) [36].
We undertook a systematic search up to August 2018 in the following biomedical bibliographic databases: MEDLINE (Ovid), Cochrane (Wiley), EMBase (Elsevier), CINAHL (EBSCO), LILACS (iAH). Details about the performed electronic searches are provided in the Additional file 1. Search strategy. For further information we also hand-searched reference-lists of published systematic reviews (SR) of models and performed a prospective citation tracking.
Selection process, eligibility, and risk of bias (quality) assessment
Pairs of reviewers independently selected articles, initially by title and abstract and subsequently by evaluating the full texts of studies meeting the inclusion criteria, using the software Covidence [37, 38]. For article eligibility, the following criteria were established: 1) epidemiological or decision models exploring SSBs-related disease burden which report attributable deaths and at least one of the following outcomes: Disability-Adjusted Life Years (DALYs), Quality-Adjusted Life Years (QALYs), and Years of Life Lost (YLLs), 2) model-based economic evaluations of health interventions or policies, implemented or implementable at the city, state, or national level, and 3) descriptive studies of decision models that explore disease burden or cost-effectiveness. The exclusion criteria were: 1) publishing date before the year 2003 -since the relationship between SSBs and health risk was not previously clear-, 2) cost-only studies (health effects not included), 3) models not specifically about SSBs or which do not distinctively show SSBs effects, 4) economic evaluations based only on randomized controlled trials (piggyback studies). Based on the paper by Brennan et al. paper [39] we defined a model as a formal quantified comparison, which summarize sources of evidence on costs and benefits, in order to identify the best option for decision makers to adopt. These authors additionally proposed a model taxonomy according to different dimensions. We simplified this taxonomy to account for different model characteristics: whether they incorporated interactions between the individuals; whether they were epidemiological (a simple usually excel based model), aggregated (nonindividual) or at individual level; how they handled the time variable (as a continuous variable, as discrete steps/cycles or were untimed); or were based on cohorts (state-transition/Markov models).
Pairs of reviewers independently extracted data using a previously piloted data extraction form and assessed the risk of bias (quality) of the included studies. In case of disagreements, it was resolved by consensus. If reaching a consensus proved to be difficult, a third author made the final decision. Considering the nature of our research question, a specific risk of bias (quality) assessment tool was not deemed to be applicable. Nevertheless, we used the items in the data extraction template to assess the exhaustiveness of the model features and description.
Data synthesis
We performed a descriptive synthesis of the main characteristics of the identified models.
For each model we considered its type, frequency of use in public health, specificity for SSBs- attributable effects, time horizon, perspective, age, sex, SES and countries of application to allow subgroup analyses. We assessed the following features: presence of interaction between individuals, degree of information aggregation (individual, aggregate, econometric or epidemiological), temporal dimension incorporation, and number of cohorts required (single cohort vs multicohort). Regarding model inputs, we specified data requirements such as incidence, data by condition, vital data, longitudinal data, representative surveys, or other data.
As for outcomes, we analyzed if they reported: variations in the degree of consumption, obesity/overweight, diabetes, mortality, cardiovascular disease, cancer, tooth cavities, bullying, other health outcomes; DALYs, QALYs or YLL; direct or indirect costs; tax revenue, sales of sugary drinks and health equity aspects. For cost-effectiveness models we also considered which type of intervention was being evaluated: taxation, school environment modifications, advertising, labeling, or others. We estimated the workload needed to complete populating models according to their type, as well as their applicability to the Latin-American and Caribbean context. In all cases they scored as low, medium or high effort /applicability and the final decision was reached by group consensus.
Finally, we identified each model’s underlying disease causal pathway and graphically assigned it to a group according to its pathway and / or the manner in which results were reported.
Results
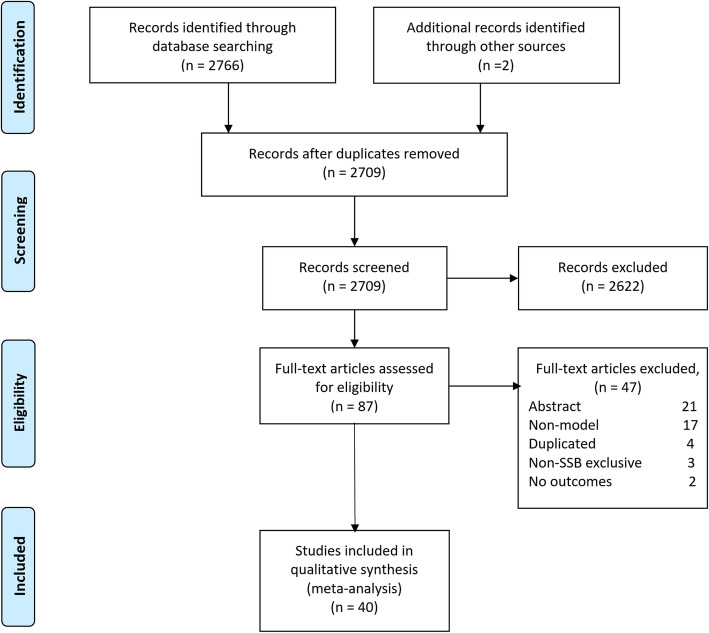
We identified a total of 2766 references from the bibliographic databases (2709 after removal of duplicates). We selected 87 of those for eligibility by full text-screening and we finally included 40 studies [18, 23, 25–27, 32, 40–73] published between 2012 and 2018 (See Fig. 1. Study flow diagram).
Fig. 1.
Flow diagram of studies in the systematic review. Note: Abstract refers to articles classified as not meeting the inclusion criteria through its abstract. Duplicated refers to the fact that it is exactly the same study. Non-SSBs exclusive refers to models that do not allow differentiating the exclusive effects of SSBs. No outcomes: the study don’t report the outcomes of interest.
The descriptive statistics of the characteristics of the included SSBs models are described in Tables 1 and 2. A detailed description of each model’s features, taxonomy, inputs, results, subgroups analyzed, interventions evaluated, and applicability can be found in Additional file 2. Tables 1 to 5. These characteristics were considered as an indirect proxy of the study quality.
Table 1.
Descriptive statistics of the included SSBs models: features, taxonomy, and applicability
| Model | Descriptive variables | Frequency (N = 40 studies) | % |
|---|---|---|---|
| Features | Specific to SSBs | N = 18 | 45.0% |
| Time horizon (maximum) | 1 year = 8 | 22.5% | |
| 2–10 years = 14 | 35.0% | ||
| 11–25 years = 9 | 22.5% | ||
| Lifetime = 8 | 20.0% | ||
| Population | Adults only = 21 | 52.5% | |
| Childs only = 2 | 5.0% | ||
| Total population = 17 | 42.5% | ||
| Country by income | High income = 30 | 75,00% | |
| Low and middle income = 9 | 22,50% | ||
| Worldwide = 1 | 2,50% | ||
| Perspective | Government = 6 | 15.0% | |
| Health system = 23 | 57.5% | ||
| Societal = 11 | 27.5% | ||
| Taxonomy | Interaction allowed | N = 0 | 0% |
| Aggregate/ Individual/ econometric/ epidemiological | Aggregate = 14 | 35.0% | |
| Individual = 1 | 2.5% | ||
| Econometric = 8 | 20.0% | ||
| Epidemiological = 17 | 42.5% | ||
| Time incorporation | Timed = 20 | 50.0% | |
| Untimed = 13 | 32.5% | ||
| Continuous =6 | 15.0% | ||
| Not applicable = 1 | 2.5% | ||
| Cohort | Cohort =25 | 62.5% | |
| Multi-cohort = 8 | 20.0% | ||
| Not reported/applicable = 7 | 17.5% | ||
| Applicability | Effort / requirements | Low = 4 | 10.0% |
| Moderate = 34 | 85.0% | ||
| High = 2 | 5.0% | ||
| Applicability / reproducibility | Moderate = 35 | 87.5% | |
| High = 5 | 12.5% |
Table 2.
Descriptive statistics of the included SSBs models: inputs, results, subgroups, and interventions
| Model | Descriptive variables | Frequency (N = 40 studies) | % |
|---|---|---|---|
| Inputs | Incidence | N = 21 | 52.5% |
| Vital statistics | N = 27 | 67.5% | |
| Longitudinal data | N = 9 | 22.5% | |
| Population survey | N = 37 | 87.5% | |
| Demand elasticity | N = 11 | 27.5% | |
| Results | Obesity/Overweight | N = 36 | 90.0% |
| Diabetes | N = 29 | 72.5% | |
| Cardiovascular disease | N = 31 | 77.5% | |
| Cancer | N = 13 | 32.5% | |
| Cavities | N = 2 | 5.0% | |
| Osteoarthritis | N = 2 | 5.0% | |
| Incidence | N = 3 | 7.5% | |
| Prevalence | N = 6 | 15.0% | |
| Mortality | N = 21 | 52.5% | |
| Life years | N = 11 | 27.5% | |
| DALYs/QALYs | N = 16 | 40.0% | |
| Direct costs | N = 23 | 57.5% | |
| Indirect costs | N = 6 | 15.0% | |
| Cost-effectiveness | N = 7 | 17.5% | |
| Variation in consumption | N = 34 | 85.0% | |
| SSBs sales | N = 7 | 17.5% | |
| Tax collection | N = 7 | 17.5% | |
| Equity | N = 13 | 32.5% | |
| Subgroups | Children/teenage | N = 16 | 40.0% |
| Gender | N = 22 | 55.0% | |
| Income level | N = 12 | 30.0% | |
| Vulnerable groups | N = 10 | 25.0% | |
| Interventions evaluated | Taxes | N = 30 | 75.0% |
| School environment | N = 5 | 12.5% | |
| Advertising | N = 4 | 10.0% | |
| Labelling | N = 2 | 5.0% | |
| Subsidies | N = 2 | 5.0% |
SSBs sugar sweetened beverages. Demand elasticity is an economic measure of the sensitivity of demand of SSBs relative to a change in another variable, usually the price. Vulnerable groups: ethnicity, rural status, literacy, education level or participants of a nutritional assistance program
Out of the 40 included studies only 45% were exclusive for SSBs, while in the rest of the models SSBs was one of the risk factors evaluated among others (e.g., obesity or cardiovascular risk factors). 72.5% analyzed a maximum time horizon of 10 or more years; only 25% considered child population separately. Only 12.5% included a Latin-American country while 82.5% were conducted in high income countries, mainly in USA, Australia and the UK. Most models were based on healthcare system perspective (57.5%).
Regarding the model taxonomy, none incorporated interactions between the individuals; most were classified as epidemiological (42.5%), aggregated -non individual- level (35.5%), timed (50%), and based on cohort (62.5%). A detailed description of each model can be found in Additional file 2. Table 6.
The majority of the models involve moderate applicability efforts or requirements (85%) and show moderate applicability to Latin-America and the Caribbean region (87.5%).
Most models required inputs from national surveys -such as obesity prevalence, SSBs consumption-; vital statistics (67.5%) mainly related to specific disease mortality; and each country’s disease incidence (52.5%). See Table 1.
The most common results provided by the burden of disease models were obesity/overweight (82.5%), diabetes (72.5%), cardiovascular disease (60%), mortality (52.5%), direct medical costs (57.35%), and DALYs/QALYs (40%) attributable to SSBs. Only two models incorporate diseases not related to obesity such as cavities. Equity analysis was considered in one third of the studies. Models that evaluated the impact of interventions also included the variation in SSBs consumption (85%) but only 17.5% reported tax collection or SSBs sales.
Regarding the analysis of different population subgroups, 55% reported results by gender and 40% included children; only 30% of the models presented results by income level, and only 25% by vulnerable groups.
Most of the models evaluated at least one intervention (92.5%), taxes being the most evaluated intervention (75%) followed by school environments (12.5%) and advertising (10%). See Table 2.
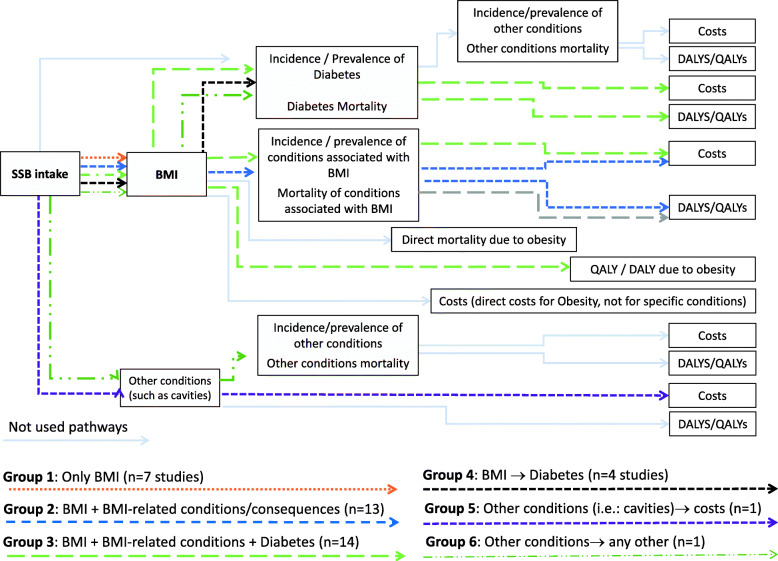
After analyzing each model causal (structural) pathway, we grouped them in six main pathway patterns, which are graphically presented in Fig. 2 Models’ pathways groups; complemented by the data in Table 3. The most frequent pathway (35%) included the effects of SSBs intake on BMI with the mortality and quality of life of the obesity plus the effects of diabetes and other related diseases/conditions including mortality, DALYS/QALYs and the cost associated with their treatment. A similar pathway that was almost as frequent (32.5%) did not consider diabetes independently, but it was included with all the other conditions (mainly cardiovascular disease and cancer) (see Fig. 2, groups 2 and 3). Models that used the simplest pathway, which only include SSBs intake to BMI represent 17.55% of the cases. Other pathways were less frequent or not used at all. Each model pathway is graphically represented in figures in Additional file 3. Pathways by study.
Fig. 2.
Model pathways groups
Table 3.
Disease pathway pattern groups of the included SSBs models
| Pathway pattern | N (%) | Studies ID | References | |
|---|---|---|---|---|
| Group 1 | Only BMI | 7 (17.5%) | Briggs 2013a, Briggs 2013b, Kristensen 2014, Lee 2018, Manyema 2014, Vecino-Ortiz 2018, Wilson 2015. | [25, 46, 47, 55, 57, 62, 72] |
| Group 2 | BMI + BMI-related conditions / consequences | 13 (32.5%) | Collins 2015, Gortmaker 2015b, Gortmaker 2015a, Lin 2011, Long 2015, Manyema 2015, Manyema 2016, Nomaguchi 2017, Pearson-Stuttard 2017, Rezende 2016, Sacks 2011, Singh 2015, Wright 2015 | [23, 26, 27, 32, 51, 53, 54, 59, 61, 64, 65, 67, 73] |
| Group 3 | BMI + BMI-related conditions + Diabetes | 14 (35.0%) | Afshin 2015, Basu 2013, Brown 2018, Breeze 2017, Briggs 2017, Cobiac 2017, Crino 2017, Lal 2017, Magnus 2016, Mekonnen 2013, Penalvo 2017, Sanchez Romero 2016, Veerman 2016, Wang 2012 | [18, 40, 43, 45, 48–50, 52, 56, 61, 66, 68, 70, 71] |
| Group 4 | BMI + Diabetes | 4 (10.0%) | Barrientos-G. 2017, Basu 2014 a, Basu 2014b, Ma 2016 | [41, 42, 44, 60] |
| Group 5 | Other, such as cavities, → costs | 1 (2.5%) | Schwendicke 2016 | [69] |
| Group 6 | Other → any other | 1 (2.5%) | Lieffers 2018 | [58] |
Discussion
Our systematic review offers a unique and up to date snapshot of current SSBs models, and provides a detailed description of the 40 included studies involving model features, inputs, results, pathways, interventions and applicability issues. This can significantly facilitate the use, adaptation, or development of future models that will improve the current tools aiming to implement a successful SSBs policy.
Remarkably, less than half of the models were specifically designed for SSBs, though all of them provided useful information in order to facilitate the use and adapt or develop a model in future endeavors. The information identified can be used in different contexts; we incorporated information from five continents, including some global approaches [25] and from all perspectives, such as healthcare systems, governments and society as a whole.
As to the complexity of the required input parameters, most models require available or feasible inputs, like representative population surveys -mainly for obesity prevalence-, or vital statistics for mortality by conditions; while some other inputs -such as incidence or longitudinal data- could be more difficult to obtain in many settings, though required by fewer models. This can also be true for the level of disaggregation of some parameters; for example, finding data by age by single year or by gender could be difficult to achieve in some countries or regions. Information regarding SSBs consumption could be difficult to find in Latin-American and the Caribbean countries and specific information on children is usually unavailable. Additionally, the models that evaluating the impact of a required intervention required demand elasticity for SSBs, ideally by age and gender groups, which data is not easily available in many countries.
Models offer relevant results to assess the burden of disease and / or the cost-effectiveness of interventions including the expected variation on SBBs consumption of different policies, obesity/overweight, diabetes, cardiovascular disease, and mortality. Many of the models do not report results in a sufficiently disaggregated manner, thus limiting their applicability and usefulness to end users such as decision makers. The evidence identifies presents some limitations. SSBs consumption is really dissimilar among subgroups, for example adolescents usually consumes more than adults and there are big differences between genders by ages groups or income quintiles [74]. Moreover, the prevalence of obesity and disease has different effects according to gender, age, and income [10, 75, 76]; so it is really usefully to have the opportunity to analyze the effects of SSBs in a disaggregated manner.
Direct and indirect costs and quality of life -DALYs and QALYs- are measures which usually serve as a guide for resource allocation and are valuable for decision makers; but only 57.5 and 40% of the models incorporated them, respectively. Children were usually omitted in most of the studies, even though they are a widely affected population and a high-priority target for the prevention policies advocated by international organizations such as UNICEF and by numerous health systems.
It is encouraging that most of the interventions studied are those most grounded on evidence such as taxes, school food policies and advertising [77, 78].
Our results show that a variety of specific modelling approaches to SSBs consumption has been used to understand its associated burden. Most of the published studies model the effects of SSBs consumption through increased BMI and the consequences for health -and sometimes for quality of life and the cost- implied. While sometimes the models separate the effects of diabetes, the effect through BMI is invariably considered without including the direct effect of SSBs on diabetes as well [79]. A direct effect of SSBs on cardiovascular disease has been recently recognized (independently of BMI), which no model had previously included [80]. The Australian Assessing Cost-Effectiveness (ACE) model [81] was the most frequently used model, including adaptations to the USA [50, 52–54, 56, 59, 64, 67, 70, 73]. This model is both time- and data- consuming and requires researchers and users to have a high level of understanding of modelling issues, so it is probably difficult to apply in many countries. Our review finds many other model and model causal pathways that could be used. The selection of the appropriate model for each country could depend on the availability of local data, the time horizon selected, the health policy to be evaluated, among others.
A systematic review evaluating the impact of taxes on SSBs according to socio-economic status uncovered that models are focused on SSBs consumption rather than on the burden of disease; few models evaluate the impact on BMI but most of them only evaluated the impact on SSBs consumption [82]. We similarly found out that few studies specifically disaggregated results according to income groups.
Worldwide -and more so in low- and middle-income countries- the general population and decision-makers are not yet fully aware of the dimension of the problem that an excessive SBBs consumption can cause; therefore, studies estimating the attributable disease burden are really important. Also, the interventions that need to be implemented -taxes, labeling, publicity limitation, school environment modifications- are both politically and socially sensitive, and the beverage industry frequently obstructs their implementation [83]. While SSBs taxes have been instituted in over 40 countries and cities [84], the epidemiological shift towards NCDs diseases in low- and middle-income countries (LMICs) warrants the implementation of an even stricter SSBs control policy encompassing all the effective interventions available [77, 78].
The value of non-communicable disease modelling to inform health policy is well established [85–87]. These models guide decision-makers in the implementation of policies to improve risk factors for chronic diseases. The tobacco experience has shown that the burden of disease and economic evaluations have promoted an effective WHO framework implementation all around the world [88]. Four our SSBs-related focus, we found 40 published models that attempt to assess this information on burden of disease that could guide and promote the implementation of evidence-based policies aiming to decrease SSBs consumption and its associated burden. Implementing effective SSBs policies is particularly important for LMICs with double nutritional burden of malnutrition and obesity.
Based on this information each country could select a simple or a more advanced model to apply within its boundaries and also identify what the main inputs and results that could be useful for making decisions in the local context are.
Conclusions
There is a wide range of modelling approaches with different complexities and information requirements to evaluate the burden of disease attributable to SSBs. The majority of these approaches consider the impact on obesity, diabetes and cardiovascular disease, mortality, and economic impact. The incorporation of these tools in different countries could generate useful information for decision makers and the general population and promote a deeper implementation of policies to diminish SSBs consumption.
Supplementary Information
Acknowledgments
Daniel Comandé, Mónica Soria, Natalie Soto, María Belén Rodriguez, Sebastian García Marti.
Authors’ contributions
AA coordinated the overall activities, designed the strategies, extracted data, plan the analysis, discussed the results and write the final draft. AC designed the strategies, extracted, plan and analyze data, discussed the results and write the final draft. APR, AP, AB y FA designed the strategies, extracted data, plan the analysis and discussed the results. DB and LP extracted data and discussed the results. All authors contributed to the interpretation of the results and contributed to edit the final draft. The author(s) read and approved the final manuscript.
Funding
International Development Research Centre (IDRC) Project Number-Activity Number-Component Number: 108646–001. The sponsor supported all the activities and material needed to achieve the project objective, but it was not involved in any stage of the study.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 2.Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, Baugh V, Bekedam H, Billo N, Casswell S, Cecchini M, Colagiuri R, Colagiuri S, Collins T, Ebrahim S, Engelgau M, Galea G, Gaziano T, Geneau R, Haines A, Hospedales J, Jha P, Keeling A, Leeder S, Lincoln P, McKee M, Mackay J, Magnusson R, Moodie R, Mwatsama M, Nishtar S, Norrving B, Patterson D, Piot P, Ralston J, Rani M, Reddy KS, Sassi F, Sheron N, Stuckler D, Suh I, Torode J, Varghese C, Watt J. Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 3.Sultan-Taieb H, Chastang JF, Mansouri M, Niedhammer I. The annual costs of cardiovascular diseases and mental disorders attributable to job strain in France. BMC Public Health. 2013;13(1):748. doi: 10.1186/1471-2458-13-748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seuring T, Archangelidi O, Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. PharmacoEconomics. 2015;33(8):811–831. doi: 10.1007/s40273-015-0268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmid T, Xu W, Gandra SR, Michailov G. Costs of treating cardiovascular events in Germany: a systematic literature review. Value Health. 2014;17(7):A485. doi: 10.1016/j.jval.2014.08.1418. [DOI] [PubMed] [Google Scholar]
- 6.Joo H, Zhang P, Wang G. Cost of informal care for patients with cardiovascular disease or diabetes: current evidence and research challenges. Qual Life Res. 2017;26(6):1379–1386. doi: 10.1007/s11136-016-1478-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaziano TA. Economic burden and the cost-effectiveness of treatment of cardiovascular diseases in Africa. Heart. 2008;94(2):140–144. doi: 10.1136/hrt.2007.128785. [DOI] [PubMed] [Google Scholar]
- 8.Evans N. Managing the cost of cardiovascular prevention in primary care. Heart. 2004;90(Suppl 4):iv26–iv28. doi: 10.1136/hrt.2004.037598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9(1):88. doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Collaborators GBDO, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27. doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, Abraham JP, Abu-Rmeileh NME, Achoki T, AlBuhairan FS, Alemu ZA, Alfonso R, Ali MK, Ali R, Guzman NA, Ammar W, Anwari P, Banerjee A, Barquera S, Basu S, Bennett DA, Bhutta Z, Blore J, Cabral N, Nonato IC, Chang JC, Chowdhury R, Courville KJ, Criqui MH, Cundiff DK, Dabhadkar KC, Dandona L, Davis A, Dayama A, Dharmaratne SD, Ding EL, Durrani AM, Esteghamati A, Farzadfar F, Fay DFJ, Feigin VL, Flaxman A, Forouzanfar MH, Goto A, Green MA, Gupta R, Hafezi-Nejad N, Hankey GJ, Harewood HC, Havmoeller R, Hay S, Hernandez L, Husseini A, Idrisov BT, Ikeda N, Islami F, Jahangir E, Jassal SK, Jee SH, Jeffreys M, Jonas JB, Kabagambe EK, Khalifa SEAH, Kengne AP, Khader YS, Khang YH, Kim D, Kimokoti RW, Kinge JM, Kokubo Y, Kosen S, Kwan G, Lai T, Leinsalu M, Li Y, Liang X, Liu S, Logroscino G, Lotufo PA, Lu Y, Ma J, Mainoo NK, Mensah GA, Merriman TR, Mokdad AH, Moschandreas J, Naghavi M, Naheed A, Nand D, Narayan KMV, Nelson EL, Neuhouser ML, Nisar MI, Ohkubo T, Oti SO, Pedroza A, Prabhakaran D, Roy N, Sampson U, Seo H, Sepanlou SG, Shibuya K, Shiri R, Shiue I, Singh GM, Singh JA, Skirbekk V, Stapelberg NJC, Sturua L, Sykes BL, Tobias M, Tran BX, Trasande L, Toyoshima H, van de Vijver S, Vasankari TJ, Veerman JL, Velasquez-Melendez G, Vlassov VV, Vollset SE, Vos T, Wang C, Wang XR, Weiderpass E, Werdecker A, Wright JL, Yang YC, Yatsuya H, Yoon J, Yoon SJ, Zhao Y, Zhou M, Zhu S, Lopez AD, Murray CJL, Gakidou E. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9945):766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, AlMazroa MA, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Abdulhak AB, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, de Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FGR, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Memish ZA, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KMV, Nasseri K, Norman P, O'Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA, III, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, de León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJL. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98(4):1084–1102. doi: 10.3945/ajcn.113.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malik VS, Willett WC, Hu FB. Sugar-sweetened beverages and BMI in children and adolescents: reanalyses of a meta-analysis. Am J Clin Nutr. 2009;89(1):438–439. doi: 10.3945/ajcn.2008.26980. [DOI] [PubMed] [Google Scholar]
- 15.Vos MB, Kaar JL, Welsh JA, Van Horn LV, Feig DI, Anderson CAM, Patel MJ, Cruz Munos J, Krebs NF, Xanthakos SA, et al. Added sugars and cardiovascular disease risk in children: a scientific statement from the American Heart Association. Circulation. 2017;135(19):e1017–e1034. doi: 10.1161/CIR.0000000000000439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. International Agency for Research on Cancer handbook working G: body fatness and Cancer--viewpoint of the IARC working group. N Engl J Med. 2016;375(8):794–798. doi: 10.1056/NEJMsr1606602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jayalath VH, de Souza RJ, Ha V, Mirrahimi A, Blanco-Mejia S, Di Buono M, Jenkins AL, Leiter LA, Wolever TM, Beyene J, et al. Sugar-sweetened beverage consumption and incident hypertension: a systematic review and meta-analysis of prospective cohorts. Am J Clin Nutr. 2015;102(4):914–921. doi: 10.3945/ajcn.115.107243. [DOI] [PubMed] [Google Scholar]
- 18.Mekonnen TA, Odden MC, Coxson PG, Guzman D, Lightwood J, Wang YC, Bibbins-Domingo K. Health benefits of reducing sugar-sweetened beverage intake in high risk populations of California: results from the cardiovascular disease (CVD) policy model. PLoS One. 2013;8(12):e81723. doi: 10.1371/journal.pone.0081723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang H, Steffen LM, Zhou X, Harnack L, Luepker RV. Consistency between increasing trends in added-sugar intake and body mass index among adults: the Minnesota heart survey, 1980-1982 to 2007-2009. Am J Public Health. 2013;103(3):501–507. doi: 10.2105/AJPH.2011.300562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Koning L, Malik VS, Kellogg MD, Rimm EB, Willett WC, Hu FB. Sweetened beverage consumption, incident coronary heart disease, and biomarkers of risk in men. Circulation. 2012;125(14):1735–1741. doi: 10.1161/CIRCULATIONAHA.111.067017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. Bmj. 2012;346(jan15 3):e7492. doi: 10.1136/bmj.e7492. [DOI] [PubMed] [Google Scholar]
- 22.Moynihan PJ, Kelly SA. Effect on caries of restricting sugars intake: systematic review to inform WHO guidelines. J Dent Res. 2014;93(1):8–18. doi: 10.1177/0022034513508954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rezende LF, Azeredo CM, Canella DS, Luiz Odo C, Levy RB, Eluf-Neto J. Coronary heart disease mortality, cardiovascular disease mortality and all-cause mortality attributable to dietary intake over 20years in Brazil. Int J Cardiol. 2016;217:64–68. doi: 10.1016/j.ijcard.2016.04.176. [DOI] [PubMed] [Google Scholar]
- 24.Meier T, Deumelandt P, Christen O, Stangl GI, Riedel K, Langer M. Global burden of sugar-related dental diseases in 168 countries and corresponding health care costs. J Dent Res. 2017;96(8):845–54. [DOI] [PubMed]
- 25.Vecino-Ortiz AI, Arroyo-Ariza D. A tax on sugar sweetened beverages in Colombia: estimating the impact on overweight and obesity prevalence across socio economic levels. Soc Sci Med. 2018;209:111–116. doi: 10.1016/j.socscimed.2018.05.043. [DOI] [PubMed] [Google Scholar]
- 26.Singh GM, Micha R, Khatibzadeh S, Lim S, Ezzati M, Mozaffarian D. Estimated global, regional, and National Disease Burdens Related to sugar-sweetened beverage consumption in 2010. Circulation. 2015;132(8):639–666. doi: 10.1161/CIRCULATIONAHA.114.010636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin BH, Smith TA, Lee JY, Hall KD. Measuring weight outcomes for obesity intervention strategies. The case of a sugar-sweetened beverage tax. Econ Hum Biol. 2011;9(4):329–341. doi: 10.1016/j.ehb.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 28.Huth PJ, Fulgoni VL, Keast DR, Park K, Auestad N. Major food sources of calories, added sugars, and saturated fat and their contribution to essential nutrient intakes in the U.S. diet: data from the National Health and Nutrition Examination Survey (2003-2006) Nutr J. 2013;12:116. doi: 10.1186/1475-2891-12-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pomeranz JL, Munsell CR, Harris JL. Energy drinks: an emerging public health hazard for youth. J Public Health Policy. 2013;34(2):254–271. doi: 10.1057/jphp.2013.6. [DOI] [PubMed] [Google Scholar]
- 30.Roberto CA, Swinburn B, Hawkes C, Huang TT, Costa SA, Ashe M, Zwicker L, Cawley JH, Brownell KD. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet. 2015;385(9985):2400–2409. doi: 10.1016/S0140-6736(14)61744-X. [DOI] [PubMed] [Google Scholar]
- 31.von Philipsborn PSJ, Burns J, Busert LK, Pfadenhauer LM, Polus S, Holzapfel C, Hauner H, Rehfuess E. Environmental interventions to reduce the consumption of sugar-sweetened beverages and their effects on health. Cochrane Database Syst Rev. 2016;7:CD012292. doi: 10.1002/14651858.CD012292.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manyema M, Veerman JL, Chola L, Tugendhaft A, Labadarios D, Hofman K. Decreasing the burden of type 2 diabetes in South Africa: the impact of taxing sugar-sweetened beverages. PLoS One. 2015;10(11):e0143050. doi: 10.1371/journal.pone.0143050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cobiac LJ, Tam K. Taxes and Subsidies for Improving Diet and Population Health in Australia: A Cost-Effectiveness Modelling Study. 2017;14(2):e1002232. [DOI] [PMC free article] [PubMed]
- 34.Barrientos-Gutierrez T. Expected population weight and diabetes impact of the 1-peso-per-litre tax to sugar sweetened beverages in Mexico. PLoS Med. 2017;12(5):e0176336. doi: 10.1371/journal.pone.0176336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thomas R CKCeaICJ, Papanicolas I, Smith PC, editors. Health system efficiency: How to make measurement matter for policy and management [Internet]. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2016. (Health Policy Series, No. 46.) 6. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436886/. [PubMed]
- 36.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Babineau J. Product Review: Covidence (Systematic Review Software). J Can Health Libraries Assoc Journal de l'Association des bibliothèques de la santé du Canada 2014, 35(2). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2707599/pdf/pmed.1000097.pdf.
- 38.Covidence systematic review software. In. Melbourne, Australia: Veritas Health Innovation.
- 39.Brennan A, Chick SE, Davies R. A taxonomy of model structures for economic evaluation of health technologies. Health Econ. 2006;15(12):1295–1310. doi: 10.1002/hec.1148. [DOI] [PubMed] [Google Scholar]
- 40.Afshin A, Micha R, Khatibzadeh S, Fahimi S, Shi P, Powles J, Singh G, Yakoob MY, Abdollahi M, Al-Hooti S et al. The impact of dietary habits and metabolic risk factors on cardiovascular and diabetes mortality in countries of the Middle East and North Africa in 2010: A comparative risk assessment analysis. BMJ Open. 2015;5(5):e006385. [DOI] [PMC free article] [PubMed]
- 41.Barrientos-Gutierrez T, Zepeda-Tello R, Rodrigues ER, Colchero-Aragones A, Rojas-Martõnez R, Lazcano-Ponce E, et al. Expected population weight and diabetes impact of the 1-peso-per-litre tax to sugar sweetened beverages in Mexico. PLoS One. 2017;12(5). [DOI] [PMC free article] [PubMed]
- 42.Basu S, Lewis K. Reducing added sugars in the food supply through a cap-and-trade approach. Am J Public Health. 2014;104(12):2432–2438. doi: 10.2105/AJPH.2014.302170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Basu S, Seligman H, Bhattacharya J. Nutritional policy changes in the supplemental nutrition assistance program: a microsimulation and cost-effectiveness analysis. Med Decis Mak. 2013;33(7):937–948. doi: 10.1177/0272989X13493971. [DOI] [PubMed] [Google Scholar]
- 44.Basu S, Vellakkal S, Agrawal S, Stuckler D, Popkin B, Ebrahim S. Averting obesity and type 2 diabetes in India through sugar-sweetened beverage taxation: an economic-epidemiologic modeling study. PLoS Med. 2014;11(1):e1001582. doi: 10.1371/journal.pmed.1001582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Breeze PR, Thomas C, Squires H, Brennan A, Greaves C, Diggle P, Brunner E, Tabak A, Preston L, Chilcott J. Cost-effectiveness of population-based, community, workplace and individual policies for diabetes prevention in the UK. Diabet Med. 2017;34(8):1136–1144. doi: 10.1111/dme.13349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Briggs AD, Mytton OT, Kehlbacher A, Tiffin R, Rayner M, Scarborough P. Overall and income specific effect on prevalence of overweight and obesity of 20% sugar sweetened drink tax in UK: econometric and comparative risk assessment modelling study. BMJ. 2013;347(oct31 4):f6189. doi: 10.1136/bmj.f6189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Briggs AD, Mytton OT, Madden D, O'Shea D, Rayner M, Scarborough P. The potential impact on obesity of a 10% tax on sugar-sweetened beverages in Ireland, an effect assessment modelling study. BMC Public Health. 2013;13(1):860. doi: 10.1186/1471-2458-13-860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Briggs ADM, Mytton OT, Kehlbacher A, Tiffin R, Elhussein A, Rayner M, Jebb SA, Blakely T, Scarborough P. Health impact assessment of the UK soft drinks industry levy: a comparative risk assessment modelling study. Lancet Public Health. 2017;2(1):e15–e22. doi: 10.1016/S2468-2667(16)30037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brown V, Ananthapavan J, Veerman L, Sacks G, Lal A, Peeters A, Backholer K, Moodie M. The Potential Cost-Effectiveness and Equity Impacts of Restricting Television Advertising of Unhealthy Food and Beverages to Australian Children. Nutrients. 2018;10(5):622. [DOI] [PMC free article] [PubMed]
- 50.Cobiac LJ, Tam K, Veerman L, Blakely T. Taxes and Subsidies for Improving Diet and Population Health in Australia: A Cost-Effectiveness Modelling Study. PLoS Med. 2017;14(2). [DOI] [PMC free article] [PubMed]
- 51.Collins B, Capewell S, O'Flaherty M, Timpson H, Razzaq A, Cheater S, Ireland R, Bromley H. Modelling the Health Impact of an English Sugary Drinks Duty at National and Local Levels. PLoS ONE [Electronic Resource] 2015;10(6):e0130770. doi: 10.1371/journal.pone.0130770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Crino M, Mantilla Herrera AM, Ananthapavan J, Wu JHY, Neal B, Yong Yi L, Miaobing Z, Lal A, Sacks G. Modelled cost-effectiveness of a package size cap and a kilojoule reduction intervention to reduce energy intake from sugar-sweetened beverages in Australia. Nutrients. 2017;9(9):1–17. doi: 10.3390/nu9090983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gortmaker SL, Long MW, Resch SC, Ward ZJ, Cradock AL, Barrett JL, Wright DR, Sonneville KR, Giles CM, Carter RC, Moodie ML, Sacks G, Swinburn BA, Hsiao A, Vine S, Barendregt J, Vos T, Wang YC. Cost effectiveness of childhood obesity interventions: evidence and methods for CHOICES. Am J Prev Med. 2015;49(1):102–111. doi: 10.1016/j.amepre.2015.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gortmaker SL, Wang YC, Long MW, Giles CM, Ward ZJ, Barrett JL, Kenney EL, Sonneville KR, Sadaf Afzal A, Resch SC, et al. Three interventions that reduce childhood obesity are projected to save more than they cost to implement. Health Aff. 2015;34(11):1932–1939. doi: 10.1377/hlthaff.2015.0631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kristensen AH, Flottemesch TJ, Maciosek MV, Jenson J, Barclay G, Ashe M, Sanchez EJ, Story M, Teutsch SM, Brownson RC. Reducing childhood obesity through U.S. federal policy: a microsimulation analysis. Am J Prev Med. 2014;47(5):604–612. doi: 10.1016/j.amepre.2014.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lal A, Mantilla-Herrera AM, Veerman L, Backholer K, Sacks G, Moodie M, Siahpush M, Carter R, Peeters A. Modelled health benefits of a sugar-sweetened beverage tax across different socioeconomic groups in Australia: a cost-effectiveness and equity analysis. PLoS Med. 2017;14(6):1–17. doi: 10.1371/journal.pmed.1002326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee BY, Ferguson MC, Hertenstein DL, Adam A, Zenkov E, Wang PI, Wong MS, Gittelsohn J, Mui Y, Brown ST. Simulating the impact of sugar-sweetened beverage warning labels in three cities. Am J Prev Med. 2018;54(2):197–204. doi: 10.1016/j.amepre.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lieffers JRL, Ekwaru JP, Ohinmaa A, Veugelers PJ. The economic burden of not meeting food recommendations in Canada: The cost of doing nothing. PLoS One. 2018;13(4). [DOI] [PMC free article] [PubMed]
- 59.Long MW, Gortmaker SL, Ward ZJ, Resch SC, Moodie ML, Sacks G, Swinburn BA, Carter RC, Claire WY. Cost effectiveness of a sugar-sweetened beverage excise tax in the U.S. Am J Prev Med. 2015;49(1):112–123. doi: 10.1016/j.amepre.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ma Y, He FJ, Yin Y, Hashem KM, MacGregor GA. Gradual reduction of sugar in soft drinks without substitution as a strategy to reduce overweight, obesity, and type 2 diabetes. A modelling study. Lancet Diabetes Endocrinol. 2016;4(2):105–114. doi: 10.1016/S2213-8587(15)00477-5. [DOI] [PubMed] [Google Scholar]
- 61.Magnus A, Moodie ML, Ferguson M, Cobiac LJ, Liberato SC, Brimblecombe J. The economic feasibility of price discounts to improve diet in Australian Aboriginal remote communities. Aust N Z J Public Health. 2016;40(S1):S36–S41. doi: 10.1111/1753-6405.12391. [DOI] [PubMed] [Google Scholar]
- 62.Manyema M, Veerman LJ, Chola L, Tugendhaft A, Sartorius B, Labadarios D, et al. The potential impact of a 20% tax on sugar-sweetened beverages on obesity in South African adults: A mathematical model. PLoS One. 2014;9(8). [DOI] [PMC free article] [PubMed]
- 63.Manyema M, Veerman LJ, Tugendhaft A, Labadarios D, Hofman KJ. Modelling the potential impact of a sugar-sweetened beverage tax on stroke mortality, costs and health-adjusted life years in South Africa. BMC Public Health. 2016;16(1):1–10. doi: 10.1186/s12889-016-3085-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nomaguchi T, Cunich M, Zapata-Diomedi B, Veerman JL. The impact on productivity of a hypothetical tax on sugar-sweetened beverages. Health Policy. 2017;121(6):715–725. doi: 10.1016/j.healthpol.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 65.Pearson-Stuttard J, Bandosz P, Rehm CD, Penalvo J, Whitsel L, Gaziano T, et al. Reducing us cardiovascular disease disparities through dietary policy. BMC Public Health. 2016;16:405.
- 66.Penalvo JL, Cudhea F, Micha R, Rehm CD, Afshin A, Whitsel L, Wilde P, Gaziano T, Pearson-Stuttard J, O'Flaherty M, et al. The potential impact of food taxes and subsidies on cardiovascular disease and diabetes burden and disparities in the United States. BMC Med. 2017;15(1):208. doi: 10.1186/s12916-017-0971-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sacks G, Veerman JL, Moodie M, Swinburn B. Traffic-light nutrition labelling and junk-food tax: a modelled comparison of cost-effectiveness for obesity prevention. Int J Obes. 2011;35(7):1001–1009. doi: 10.1038/ijo.2010.228. [DOI] [PubMed] [Google Scholar]
- 68.Sanchez-Romero LM, Penko J, Coxson PG, Fernandez A, Mason A, Moran AE, Avila-Burgos L, Odden M, Barquera S, Bibbins-Domingo K. Projected impact of Mexico's sugar-sweetened beverage tax policy on diabetes and cardiovascular disease: a modeling study. PLoS Med Public Library of Science. 2016;13(11):e1002158. doi: 10.1371/journal.pmed.1002158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schwendicke F, Thomson WM, Broadbent JM, Stolpe M. Effects of taxing sugar-sweetened beverages on caries and treatment costs. J Dent Res. 2016;95(12):1327–1332. doi: 10.1177/0022034516660278. [DOI] [PubMed] [Google Scholar]
- 70.Veerman JL, Sacks G, Antonopoulos N, Martin J. The impact of a tax on sugar-sweetened beverages on health and health care costs: A modelling study. PLoS One. 2016;11(4). [DOI] [PMC free article] [PubMed]
- 71.Wang YC, Coxson P, Shen Y-M, Goldman L, Bibbins-Domingo K. A penny-per-ounce tax on sugar-sweetened beverages would cut health and cost burdens of diabetes. Health Aff. 2012;31(1):199–207. doi: 10.1377/hlthaff.2011.0410. [DOI] [PubMed] [Google Scholar]
- 72.Wilson KJ, Brown HS, Bastida E. Cost-effectiveness of a community-based weight control intervention targeting a low-socioeconomic-status Mexican-origin population. Health Promot Pract. 2015;16(1):101–108. doi: 10.1177/1524839914537274. [DOI] [PubMed] [Google Scholar]
- 73.Wright DR, Kenney EL, Giles CM, Long MW, Ward ZJ, Resch SC, Moodie ML, Carter RC, Wang YC, Sacks G, Swinburn BA, Gortmaker SL, Cradock AL. Modeling the cost effectiveness of child care policy changes in the U.S. Am J Prev Med. 2015;49(1):135–147. doi: 10.1016/j.amepre.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 74.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr. 2006;84(2):274–288. doi: 10.1093/ajcn/84.2.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Muennig P, Lubetkin E, Jia H, Franks P. Gender and the burden of disease attributable to obesity. Am J Public Health. 2006;96(9):1662–1668. doi: 10.2105/AJPH.2005.068874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jiwani SS, Carrillo-Larco RM, Hernandez-Vasquez A, Barrientos-Gutierrez T, Basto-Abreu A, Gutierrez L, Irazola V, Nieto-Martinez R, Nunes BP, Parra DC, et al. The shift of obesity burden by socioeconomic status between 1998 and 2017 in Latin America and the Caribbean: a cross-sectional series study. Lancet Glob Health. 2019;7(12):e1644–e1654. doi: 10.1016/S2214-109X(19)30421-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Heise TL, Katikireddi SV, Pega F, Gartlehner G, Fenton C, Griebler U, et al. Taxation of sugar-sweetened beverages for reducing their consumption and preventing obesity or other adverse health outcomes. Cochrane Database Syst Rev. 2016;8. [DOI] [PMC free article] [PubMed]
- 78.von Philipsborn P, Stratil JM, Burns J, Busert LK, Pfadenhauer LM, Polus S, Holzapfel C, Hauner H, Rehfuess E. Environmental interventions to reduce the consumption of sugar-sweetened beverages and their effects on health. Cochrane Database Syst Rev. 2019;6:CD012292. doi: 10.1002/14651858.CD012292.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. 2010;33(11):2477–2483. doi: 10.2337/dc10-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yin J, Zhu Y, Malik V, Li X, Peng X, Zhang FF, et al. Intake of Sugar-Sweetened and Low-Calorie Sweetened Beverages and Risk of Cardiovascular Disease: A Meta-Analysis and Systematic Review. Adv Nutr. 2021;12(1):89–101. [DOI] [PMC free article] [PubMed]
- 81.Carter R, Moodie M, Markwick A, Magnus A, Vos T, Swinburn B, Haby MM. Assessing cost-effectiveness in obesity (ACE-obesity): an overview of the ACE approach, economic methods and cost results. BMC Public Health. 2009;9(1):419. doi: 10.1186/1471-2458-9-419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Backholer K, Sarink D, Beauchamp A, Keating C, Loh V, Ball K, Martin J, Peeters A. The impact of a tax on sugar-sweetened beverages according to socio-economic position: a systematic review of the evidence. Public Health Nutr. 2016;19(17):3070–3084. doi: 10.1017/S136898001600104X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Du M, Tugendhaft A, Erzse A, Hofman KJ. Sugar-sweetened beverage taxes: industry response and tactics. Yale J Biol Med. 2018;91(2):185–190. [PMC free article] [PubMed] [Google Scholar]
- 84.Bridge G, Lomazzi M, Bedi R. Implementation of a sugar-sweetened beverage tax in low- and middle-income countries: recommendations for policymakers. J Public Health Policy. 2020;41(1):84–97. doi: 10.1057/s41271-019-00196-z. [DOI] [PubMed] [Google Scholar]
- 85.Stanaway JD, Afshin A, Gakidou E, Lim SS, Abate D, Abate KH, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A, Abdollahpour I, Abdulkader RS, Abebe M, Abebe Z, Abera SF, Abil OZ, Abraha HN, Abrham AR, Abu-Raddad LJ, Abu-Rmeileh NME, Accrombessi MMK, Acharya D, Acharya P, Adamu AA, Adane AA, Adebayo OM, Adedoyin RA, Adekanmbi V, Ademi Z, Adetokunboh OO, Adib MG, Admasie A, Adsuar JC, Afanvi KA, Afarideh M, Agarwal G, Aggarwal A, Aghayan SA, Agrawal A, Agrawal S, Ahmadi A, Ahmadi M, Ahmadieh H, Ahmed MB, Aichour AN, Aichour I, Aichour MTE, Akbari ME, Akinyemiju T, Akseer N, al-Aly Z, al-Eyadhy A, al-Mekhlafi HM, Alahdab F, Alam K, Alam S, Alam T, Alashi A, Alavian SM, Alene KA, Ali K, Ali SM, Alijanzadeh M, Alizadeh-Navaei R, Aljunid SM, Alkerwi A', Alla F, Alsharif U, Altirkawi K, Alvis-Guzman N, Amare AT, Ammar W, Anber NH, Anderson JA, Andrei CL, Androudi S, Animut MD, Anjomshoa M, Ansha MG, Antó JM, Antonio CAT, Anwari P, Appiah LT, Appiah SCY, Arabloo J, Aremu O, Ärnlöv J, Artaman A, Aryal KK, Asayesh H, Ataro Z, Ausloos M, Avokpaho EFGA, Awasthi A, Ayala Quintanilla BP, Ayer R, Ayuk TB, Azzopardi PS, Babazadeh A, Badali H, Badawi A, Balakrishnan K, Bali AG, Ball K, Ballew SH, Banach M, Banoub JAM, Barac A, Barker-Collo SL, Bärnighausen TW, Barrero LH, Basu S, Baune BT, Bazargan-Hejazi S, Bedi N, Beghi E, Behzadifar M, Behzadifar M, Béjot Y, Bekele BB, Bekru ET, Belay E, Belay YA, Bell ML, Bello AK, Bennett DA, Bensenor IM, Bergeron G, Berhane A, Bernabe E, Bernstein RS, Beuran M, Beyranvand T, Bhala N, Bhalla A, Bhattarai S, Bhutta ZA, Biadgo B, Bijani A, Bikbov B, Bilano V, Bililign N, Bin Sayeed MS, Bisanzio D, Biswas T, Bjørge T, Blacker BF, Bleyer A, Borschmann R, Bou-Orm IR, Boufous S, Bourne R, Brady OJ, Brauer M, Brazinova A, Breitborde NJK, Brenner H, Briko AN, Britton G, Brugha T, Buchbinder R, Burnett RT, Busse R, Butt ZA, Cahill LE, Cahuana-Hurtado L, Campos-Nonato IR, Cárdenas R, Carreras G, Carrero JJ, Carvalho F, Castañeda-Orjuela CA, Castillo Rivas J, Castro F, Catalá-López F, Causey K, Cercy KM, Cerin E, Chaiah Y, Chang HY, Chang JC, Chang KL, Charlson FJ, Chattopadhyay A, Chattu VK, Chee ML, Cheng CY, Chew A, Chiang PPC, Chimed-Ochir O, Chin KL, Chitheer A, Choi JYJ, Chowdhury R, Christensen H, Christopher DJ, Chung SC, Cicuttini FM, Cirillo M, Cohen AJ, Collado-Mateo D, Cooper C, Cooper OR, Coresh J, Cornaby L, Cortesi PA, Cortinovis M, Costa M, Cousin E, Criqui MH, Cromwell EA, Cundiff DK, Daba AK, Dachew BA, Dadi AF, Damasceno AAM, Dandona L, Dandona R, Darby SC, Dargan PI, Daryani A, Das Gupta R, Das Neves J, Dasa TT, Dash AP, Davitoiu DV, Davletov K, de la Cruz-Góngora V, de la Hoz FP, de Leo D, de Neve JW, Degenhardt L, Deiparine S, Dellavalle RP, Demoz GT, Denova-Gutiérrez E, Deribe K, Dervenis N, Deshpande A, Des Jarlais DC, Dessie GA, Deveber GA, Dey S, Dharmaratne SD, Dhimal M, Dinberu MT, Ding EL, Diro HD, Djalalinia S, Do HP, Dokova K, Doku DT, Doyle KE, Driscoll TR, Dubey M, Dubljanin E, Duken EE, Duncan BB, Duraes AR, Ebert N, Ebrahimi H, Ebrahimpour S, Edvardsson D, Effiong A, Eggen AE, el Bcheraoui C, el-Khatib Z, Elyazar IR, Enayati A, Endries AY, Er B, Erskine HE, Eskandarieh S, Esteghamati A, Estep K, Fakhim H, Faramarzi M, Fareed M, Farid TA, CSE F, Farioli A, Faro A, Farvid MS, Farzaei MH, Fatima B, Fay KA, Fazaeli AA, Feigin VL, Feigl AB, Fereshtehnejad SM, Fernandes E, Fernandes JC, Ferrara G, Ferrari AJ, Ferreira ML, Filip I, Finger JD, Fischer F, Foigt NA, Foreman KJ, Fukumoto T, Fullman N, Fürst T, Furtado JM, Futran ND, Gall S, Gallus S, Gamkrelidze A, Ganji M, Garcia-Basteiro AL, Gardner WM, Gebre AK, Gebremedhin AT, Gebremichael TG, Gelano TF, Geleijnse JM, Geramo YCD, Gething PW, Gezae KE, Ghadimi R, Ghadiri K, Ghasemi Falavarjani K, Ghasemi-Kasman M, Ghimire M, Ghosh R, Ghoshal AG, Giampaoli S, Gill PS, Gill TK, Gillum RF, Ginawi IA, Giussani G, Gnedovskaya EV, Godwin WW, Goli S, Gómez-Dantés H, Gona PN, Gopalani SV, Goulart AC, Grada A, Grams ME, Grosso G, Gugnani HC, Guo Y, Gupta R, Gupta R, Gupta T, Gutiérrez RA, Gutiérrez-Torres DS, Haagsma JA, Habtewold TD, Hachinski V, Hafezi-Nejad N, Hagos TB, Hailegiyorgis TT, Hailu GB, Haj-Mirzaian A, Haj-Mirzaian A, Hamadeh RR, Hamidi S, Handal AJ, Hankey GJ, Hao Y, Harb HL, Harikrishnan S, Haro JM, Hassankhani H, Hassen HY, Havmoeller R, Hawley CN, Hay SI, Hedayatizadeh-Omran A, Heibati B, Heidari B, Heidari M, Hendrie D, Henok A, Heredia-Pi I, Herteliu C, Heydarpour F, Heydarpour S, Hibstu DT, Higazi TB, Hilawe EH, Hoek HW, Hoffman HJ, Hole MK, Homaie Rad E, Hoogar P, Hosgood HD, Hosseini SM, Hosseinzadeh M, Hostiuc M, Hostiuc S, Hoy DG, Hsairi M, Hsiao T, Hu G, Hu H, Huang JJ, Hussen MA, Huynh CK, Iburg KM, Ikeda N, Ilesanmi OS, Iqbal U, Irvani SSN, Irvine CMS, Islam SMS, Islami F, Jackson MD, Jacobsen KH, Jahangiry L, Jahanmehr N, Jain SK, Jakovljevic M, James SL, Jassal SK, Jayatilleke AU, Jeemon P, Jha RP, Jha V, Ji JS, Jonas JB, Jonnagaddala J, Jorjoran Shushtari Z, Joshi A, Jozwiak JJ, Jürisson M, Kabir Z, Kahsay A, Kalani R, Kanchan T, Kant S, Kar C, Karami M, Karami Matin B, Karch A, Karema C, Karimi N, Karimi SM, Kasaeian A, Kassa DH, Kassa GM, Kassa TD, Kassebaum NJ, Katikireddi SV, Kaul A, Kawakami N, Kazemi Z, Karyani AK, Kefale AT, Keiyoro PN, Kemp GR, Kengne AP, Keren A, Kesavachandran CN, Khader YS, Khafaei B, Khafaie MA, Khajavi A, Khalid N, Khalil IA, Khan G, Khan MS, Khan MA, Khang YH, Khater MM, Khazaei M, Khazaie H, Khoja AT, Khosravi A, Khosravi MH, Kiadaliri AA, Kiirithio DN, Kim CI, Kim D, Kim YE, Kim YJ, Kimokoti RW, Kinfu Y, Kisa A, Kissimova-Skarbek K, Kivimäki M, Knibbs LD, Knudsen AKS, Kochhar S, Kokubo Y, Kolola T, Kopec JA, Kosen S, Koul PA, Koyanagi A, Kravchenko MA, Krishan K, Krohn KJ, Kromhout H, Kuate Defo B, Kucuk Bicer B, Kumar GA, Kumar M, Kuzin I, Kyu HH, Lachat C, Lad DP, Lad SD, Lafranconi A, Lalloo R, Lallukka T, Lami FH, Lang JJ, Lansingh VC, Larson SL, Latifi A, Lazarus JV, Lee PH, Leigh J, Leili M, Leshargie CT, Leung J, Levi M, Lewycka S, Li S, Li Y, Liang J, Liang X, Liao Y, Liben ML, Lim LL, Linn S, Liu S, Lodha R, Logroscino G, Lopez AD, Lorkowski S, Lotufo PA, Lozano R, Lucas TCD, Lunevicius R, Ma S, Macarayan ERK, Machado ÍE, Madotto F, Mai HT, Majdan M, Majdzadeh R, Majeed A, Malekzadeh R, Malta DC, Mamun AA, Manda AL, Manguerra H, Mansournia MA, Mantovani LG, Maravilla JC, Marcenes W, Marks A, Martin RV, Martins SCO, Martins-Melo FR, März W, Marzan MB, Massenburg BB, Mathur MR, Mathur P, Matsushita K, Maulik PK, Mazidi M, McAlinden C, McGrath JJ, McKee M, Mehrotra R, Mehta KM, Mehta V, Meier T, Mekonnen FA, Melaku YA, Melese A, Melku M, Memiah PTN, Memish ZA, Mendoza W, Mengistu DT, Mensah GA, Mensink GBM, Mereta ST, Meretoja A, Meretoja TJ, Mestrovic T, Mezgebe HB, Miazgowski B, Miazgowski T, Millear AI, Miller TR, Miller-Petrie MK, Mini GK, Mirarefin M, Mirica A, Mirrakhimov EM, Misganaw AT, Mitiku H, Moazen B, Mohajer B, Mohammad KA, Mohammadi M, Mohammadifard N, Mohammadnia-Afrouzi M, Mohammed S, Mohebi F, Mokdad AH, Molokhia M, Momeniha F, Monasta L, Moodley Y, Moradi G, Moradi-Lakeh M, Moradinazar M, Moraga P, Morawska L, Morgado-da-Costa J, Morrison SD, Moschos MM, Mouodi S, Mousavi SM, Mozaffarian D, Mruts KB, Muche AA, Muchie KF, Mueller UO, Muhammed OS, Mukhopadhyay S, Muller K, Musa KI, Mustafa G, Nabhan AF, Naghavi M, Naheed A, Nahvijou A, Naik G, Naik N, Najafi F, Nangia V, Nansseu JR, Nascimento BR, Neal B, Neamati N, Negoi I, Negoi RI, Neupane S, Newton CRJ, Ngunjiri JW, Nguyen AQ, Nguyen G, Nguyen HT, Nguyen HLT, Nguyen HT, Nguyen M, Nguyen NB, Nichols E, Nie J, Ningrum DNA, Nirayo YL, Nishi N, Nixon MR, Nojomi M, Nomura S, Norheim OF, Noroozi M, Norrving B, Noubiap JJ, Nouri HR, Nourollahpour Shiadeh M, Nowroozi MR, Nsoesie EO, Nyasulu PS, Obermeyer CM, Odell CM, Ofori-Asenso R, Ogbo FA, Oh IH, Oladimeji O, Olagunju AT, Olagunju TO, Olivares PR, Olsen HE, Olusanya BO, Olusanya JO, Ong KL, Ong SK, Oren E, Orpana HM, Ortiz A, Ota E, Otstavnov SS, Øverland S, Owolabi MO, P A M, Pacella R, Pakhare AP, Pakpour AH, Pana A, Panda-Jonas S, Park EK, Parry CDH, Parsian H, Patel S, Pati S, Patil ST, Patle A, Patton GC, Paudel D, Paulson KR, Paz Ballesteros WC, Pearce N, Pereira A, Pereira DM, Perico N, Pesudovs K, Petzold M, Pham HQ, Phillips MR, Pillay JD, Piradov MA, Pirsaheb M, Pischon T, Pishgar F, Plana-Ripoll O, Plass D, Polinder S, Polkinghorne KR, Postma MJ, Poulton R, Pourshams A, Poustchi H, Prabhakaran D, Prakash S, Prasad N, Purcell CA, Purwar MB, Qorbani M, Radfar A, Rafay A, Rafiei A, Rahim F, Rahimi Z, Rahimi-Movaghar A, Rahimi-Movaghar V, Rahman M, Rahman MH, Rahman MA, Rai RK, Rajati F, Rajsic S, Raju SB, Ram U, Ranabhat CL, Ranjan P, Rath GK, Rawaf DL, Rawaf S, Reddy KS, Rehm CD, Rehm J, Reiner RC, Jr, Reitsma MB, Remuzzi G, Renzaho AMN, Resnikoff S, Reynales-Shigematsu LM, Rezaei S, Ribeiro ALP, Rivera JA, Roba KT, Rodríguez-Ramírez S, Roever L, Román Y, Ronfani L, Roshandel G, Rostami A, Roth GA, Rothenbacher D, Roy A, Rubagotti E, Rushton L, Sabanayagam C, Sachdev PS, Saddik B, Sadeghi E, Saeedi Moghaddam S, Safari H, Safari Y, Safari-Faramani R, Safdarian M, Safi S, Safiri S, Sagar R, Sahebkar A, Sahraian MA, Sajadi HS, Salam N, Salamati P, Saleem Z, Salimi Y, Salimzadeh H, Salomon JA, Salvi DD, Salz I, Samy AM, Sanabria J, Sanchez-Niño MD, Sánchez-Pimienta TG, Sanders T, Sang Y, Santomauro DF, Santos IS, Santos JV, Santric Milicevic MM, Sao Jose BP, Sardana M, Sarker AR, Sarmiento-Suárez R, Sarrafzadegan N, Sartorius B, Sarvi S, Sathian B, Satpathy M, Sawant AR, Sawhney M, Saylan M, Sayyah M, Schaeffner E, Schmidt MI, Schneider IJC, Schöttker B, Schutte AE, Schwebel DC, Schwendicke F, Scott JG, Seedat S, Sekerija M, Sepanlou SG, Serre ML, Serván-Mori E, Seyedmousavi S, Shabaninejad H, Shaddick G, Shafieesabet A, Shahbazi M, Shaheen AA, Shaikh MA, Shamah Levy T, Shams-Beyranvand M, Shamsi M, Sharafi H, Sharafi K, Sharif M, Sharif-Alhoseini M, Sharifi H, Sharma J, Sharma M, Sharma R, She J, Sheikh A, Shi P, Shibuya K, Shiferaw MS, Shigematsu M, Shin MJ, Shiri R, Shirkoohi R, Shiue I, Shokraneh F, Shoman H, Shrime MG, Shupler MS, Si S, Siabani S, Sibai AM, Siddiqi TJ, Sigfusdottir ID, Sigurvinsdottir R, Silva DAS, Silva JP, Silveira DGA, Singh JA, Singh NP, Singh V, Sinha DN, Skiadaresi E, Skirbekk V, Smith DL, Smith M, Sobaih BH, Sobhani S, Somayaji R, Soofi M, Sorensen RJD, Soriano JB, Soyiri IN, Spinelli A, Sposato LA, Sreeramareddy CT, Srinivasan V, Starodubov VI, Steckling N, Stein DJ, Stein MB, Stevanovic G, Stockfelt L, Stokes MA, Sturua L, Subart ML, Sudaryanto A, Sufiyan M'B, Sulo G, Sunguya BF, Sur PJ, Sykes BL, Szoeke CEI, Tabarés-Seisdedos R, Tabuchi T, Tadakamadla SK, Takahashi K, Tandon N, Tassew SG, Tavakkoli M, Taveira N, Tehrani-Banihashemi A, Tekalign TG, Tekelemedhin SW, Tekle MG, Temesgen H, Temsah MH, Temsah O, Terkawi AS, Tessema B, Teweldemedhin M, Thankappan KR, Theis A, Thirunavukkarasu S, Thomas HJ, Thomas ML, Thomas N, Thurston GD, Tilahun B, Tillmann T, To QG, Tobollik M, Tonelli M, Topor-Madry R, Torre AE, Tortajada-Girbés M, Touvier M, Tovani-Palone MR, Towbin JA, Tran BX, Tran KB, Truelsen TC, Truong NT, Tsadik AG, Tudor Car L, Tuzcu EM, Tymeson HD, Tyrovolas S, Ukwaja KN, Ullah I, Updike RL, Usman MS, Uthman OA, Vaduganathan M, Vaezi A, Valdez PR, van Donkelaar A, Varavikova E, Varughese S, Vasankari TJ, Venkateswaran V, Venketasubramanian N, Villafaina S, Violante FS, Vladimirov SK, Vlassov V, Vollset SE, Vos T, Vosoughi K, Vu GT, Vujcic IS, Wagnew FS, Waheed Y, Waller SG, Walson JL, Wang Y, Wang Y, Wang YP, Weiderpass E, Weintraub RG, Weldegebreal F, Werdecker A, Werkneh AA, West JJ, Westerman R, Whiteford HA, Widecka J, Wijeratne T, Winkler AS, Wiyeh AB, Wiysonge CS, Wolfe CDA, Wong TY, Wu S, Xavier D, Xu G, Yadgir S, Yadollahpour A, Yahyazadeh Jabbari SH, Yamada T, Yan LL, Yano Y, Yaseri M, Yasin YJ, Yeshaneh A, Yimer EM, Yip P, Yisma E, Yonemoto N, Yoon SJ, Yotebieng M, Younis MZ, Yousefifard M, Yu C, Zaidi Z, Zaman SB, Zamani M, Zavala-Arciniega L, Zhang AL, Zhang H, Zhang K, Zhou M, Zimsen SRM, Zodpey S, Murray CJL. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Webber L, Mytton OT, Briggs ADM, Woodcock J, Scarborough P, McPherson K, Capewell S. The Brighton declaration: the value of non-communicable disease modelling in population health sciences. Eur J Epidemiol. 2014;29(12):867–870. doi: 10.1007/s10654-014-9978-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lopez ADMC, Ezzati M, et al. Editors. Washington (DC). The International Bank for Reconstruction and Development / the World Bank. New York: Oxford University Press; 2006. [Google Scholar]
- 88.Tobacco Free Initiative (TFI). Implementing tobacco control [https://www.who.int/tobacco/control/en/].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.