Abstract
Background
Beginning March 2020, the COVID-19 pandemic has disrupted different aspects of life. The impact on children's rate of weight gain has not been analysed.
Methods
In this retrospective cohort study, we used United States (US) Electronic Health Record (EHR) data from Optum® to calculate the age- and sex- adjusted change in BMI (∆BMIadj) in individual 6-to-17-year-old children between two well child checks (WCCs). The mean of individual ∆BMIadj during 2017–2020 was calculated by month. For September-December WCCs, the mean of individual ∆BMIadj (overall and by subgroup) was reported for 2020 and 2017–2019, and the impact of 2020 vs 2017–2019 was tested by multivariable linear regression.
Findings
The mean [95% Confidence Interval - CI] ∆BMIadj in September-December of 2020 was 0·62 [0·59,0·64] kg/m2, compared to 0·31 [0·29, 0·32] kg/m2 in previous years. The increase was most prominent in children with pre-existing obesity (1·16 [1·07,1·24] kg/m2 in 2020 versus 0·56 [0·52,0·61] kg/m2 in previous years), Hispanic children (0·93 [0·84,1·02] kg/m2 in 2020 versus 0·41 [0·36,0·46] kg/m2 in previous years), and children who lack commercial insurance (0·88 [0·81,0·95] kg/m2 in 2020 compared to 0·43 [0·39,0·47] kg/m2 in previous years). ∆BMIadj accelerated most in ages 8–12 and least in ages 15–17.
Interpretation
Children's rate of unhealthy weight gain increased notably during the COVID-19 pandemic across demographic groups, and most prominently in children already vulnerable to unhealthy weight gain. This data can inform policy decisions critical to child development and health as the pandemic continues to unfold.
Funding
Amgen, Inc.
Keywords: Pediatrics, Obesity, Overweight, COVID-19, Public health, Vulnerable populations
Research in context.
Evidence before this study
We searched PubMed for articles published unitil April 12, 2021 regarding pediatric weight gain during the COVID-19 lockdown era. The following search terms were used: “BMI”, “body mass index”, “obesity”, “overweight”, “activity”, “exercise”, or “weight” in combination with “COVID” or “lockdown” and “pediatric”, “children”, “teens”, “teenager”, or “adolescent”. Numerous papers based on parent-reported lifestyle survey data have been published, almost all recounting increased screen time and decreased physical activity time for children relative to the pre-lockdown era. While there are many survey studies of lifestyle changes and a few with questions regarding weight gain, no study has compared objective rate of unhealthy BMI gain across a broad pediatric population between pre- and post-lockdown eras.
Added value of this study
To the best of our knowledge, this is the first study to provide data on the impact of the lockdown on the rate of change of children's BMI. It uses the age- and sex-adjusted BMI change, which offers a consistent description of BMI change across categories of children (healthy weight, overweight, and obese). It compares the post-lockdown rate of age- and sex-adjusted BMI change with pre-lockdown rates, overall and by select sub-groups.
Implications of all the available evidence
Pediatric weight gain has increased during the lockdown. The increase in rate of BMI change was highest among the groups of children who were already most vulnerable to unhealthy weight gain. Results of this study support careful consideration of the physical, social, educational, and mental well-being of children as the pandemic continues into its second year, with special attention to the role decreased physical activity and increased electronic use may play in the future.
Alt-text: Unlabelled box
1. Introduction
Since March 2020, the Coronavirus Disease 2019 (COVID-19) pandemic has disrupted all aspects of life, with children greatly impacted by the sudden shift to lockdown restrictions which focused on school closures or remote learning and the removal of peer-to-peer interactive play. Numerous papers based on parent-reported lifestyle surveys in many countries have described increased use of electronic devices (i.e., screen time) and decreased physical activity since the start of the COVID-19 pandemic [[1], [2], [3], [4], [5]]. These papers predict health effects including an increase in obesity. Unhealthy weight gain in childhood, in turn, carries long-term health implications, including increased risk of obesity, hypertension, and diabetes in adulthood [6]. As the aforementioned literature raises a concern for increased childhood weight gain with consequences both immediate and reaching into adulthood, it is important to determine the extent to which the pandemic has increased the rate of weight gain in children. No papers have yet compared rate of weight gain before and during the pandemic.
To fill that gap, we use routinely collected BMI data from preventive care visits. From birth, children's height, weight, and body mass index (BMI) are consistently documented as part of routine pediatric care, known among pediatricians in the United States (US) as Well Child Checks (WCC). WCCs are attended by a high percentage of US children [7] and are used to promote health and monitor the rate of growth over time. Children, unlike adults, are expected to increase BMI as part of healthy growth. However, children's growth trajectories should not, on average, cross established BMI percentiles [8], available in CDC age- and sex-specific growth charts [9]. BMI in children is typically categorized into underweight BMIs (< 5th percentile), healthy BMIs (between 5th and 85th percentile), overweight BMIs (between 85th and 95th percentile), or with obesity BMIs (≥ 95th percentile). WCC attendance in 2019 was above 90% across races and poverty levels [9]; BMI data from WCCs therefore will not be subject to the selection bias that might result from using BMI data from sick visits, which may be associated with conditions either decreasing or increasing a child's weight. It will also avoid the self-selection and subjectivity of survey-based data.
Because healthy BMI changes through childhood, the methods of longitudinal BMI assessment in children are different from those in adults [[10], [11], [12], [13], [14]]. To measure longitudinal changes in BMI among children is challenging as the range of ‘healthy’ BMIs increases with age; consequently, the absolute change in BMI between health care encounters cannot be used to monitor appropriate weight gain. Fortunately, this difficulty can be surmounted by using the age- and sex-adjusted BMI change (∆BMIadj), which is the change in distance from the median BMI for age and sex [11] between two successive WCCs, to measure and quantify harmful weight gain. This metric has advantages compared to the use of BMI percentile or Z-score, both of which tend to be compressed in the higher BMI ranges and will therefore mask increases in children with pre-existing obesity while relatively inflating increases in children with pre-existing healthy weight [11–15].
Prior research has indicated lower physical activity and higher screen time during the COVID-19 pandemic, raising concern for increased unhealthy weight gain in children, but has not described the actual change in rate of weight gain, if any, associated with the pandemic. This study aims to describe the trend in ∆BMIadj measured at WCCs 2017–2020 among US children, and test for differences between 2020 and 2017–2019, to identify temporal changes in the rate of BMI change associated with the pandemic era.
2. Methods
2.1. Data sources
This is a retrospective cohort study using the Optum® de-identified COVID-19 Electronic Health Record (Optum® COVID-19 EHR) dataset, which is a subset of Optum® de-identified Electronic Health Record dataset (Optum® EHR). The Optum® de-identified Electronic Health Record dataset contains longitudinal data from more than 50 healthcare provider organizations that includes more than 700 hospitals and 7000 clinics. All 50 United States and all types of payors are represented, including Medicare, Medicaid, commercial, self-pay, and others.
The Optum® COVID-19 EHR is a subset of Optum® EHR that provides near-real-time data on the COVID-19 pandemic. Patients from the Optum® EHR, if they have a history of any COVID-19 diagnosis or test, regardless of the test result, are included in the Optum® COVID-19 EHR database. All the patient's data, from before and after the COVID-19 diagnosis or test, is contained in the Optum® COVID-19 database.
While the COVID testing and diagnosis was not pertinent to our study, the near-real-time nature of the data was essential. Both databases start in 2007. The end date for Optum® COVID-19 EHR was March 03, 2021. The end date for Optum® EHR, by contrast, was September 30, 2020, which was too early to capture BMI changes through the end of 2020. Therefore this study uses Optum® COVID-19 EHR data for its primary analysis, and includes sensitivity analysis to ensure that the COVID-testing-related selection of patients from the larger Optum® EHR into the smaller but near-real-time Optum® COVID-19 EHR did not introduce selection bias.
For both databases, the data are certified as de-identified by an independent statistical expert following HIPAA statistical de-identification rules and managed according to Optum® customer data use agreements. As the study used only de-identified patient data, it was exempt of IRB approval.
2.2. Primary outcome measure
The unit of analysis was the ∆BMIadj at a qualifying WCC, calculated as ΔBMIadj (BMIB-BMIA)-(BMIB,median-BMIA,median), where BMIB,median and BMIA,median denote the median BMI for the child's age and sex at WCC dates A and B, respectively.
2.3. Inclusion criteria
WCCs were identified by procedure codes (CPT-4) 99383, 99384, 99393, or 99394, which are the evaluation and management service codes are used in billing for WCCs.
A WCC qualified for inclusion in the study using the following criteria:
-
(1)
The patient was 6 to 17 years old at the time of the qualifying WCC and the WCC occurred between 2017 and 2020.
-
(2)
The patient had a prior WCC 9–15 months before to the qualifying WCC.
-
(3)
Both WCCs (the qualifying WCC and the prior WCC, known together as a WCC pair) had a BMI documented.
-
(4)
Both BMIs were “plausible” according to the CDC definition [16] (i.e., between -4 and +8 standard deviations from the median) to avoid distortion of the results by data error.
Children were excluded from the study for missing or unknown age or sex information, which precludes the calculation of median BMI for age and sex. Additionally, patients were excluded if any of the following conditions were recorded in 2015 or later, as these might indicate a need for weight gain or a medical cause of changed tendency to gain or lose weight: cancer, Cystic Fibrosis, eating disorder, Sickle Cell, Crohn's disease, Ulcerative Colitis, HIV, growth hormone deficiency, Cushing syndrome, panhypopituitarism, BMI less than 5th percentile for age and sex, pregnancy, or bariatric surgery. In case this exclusion should lead to bias, a sensitivity analysis was performed that did not exclude on the basis of BMI less than 5th percentile.
2.4. Age determination
As part of the de-identification process, only the birth year is reported in the Optum® data. For this analysis, every child was assigned a July 2nd birthdate in the documented birth year; this date was then used to calculate age at the time of the WCC. This allows for a uniform distribution in differences between assigned ages and actual ages, which are unavailable in the data. Because the difference between assigned and actual age will be identical for each WCC in a given child's WCC pair, and the second derivative of the BMI percentiles is small, the bias for any one child will be small. Because the bias for children born in one half of the year will be positive and in the other half negative, straightforward calculations from CDC growth charts will show that the largest possible resulting bias of mean ΔBMIadj in a cohort of children 6–17 years old with balanced birthdates is less than 0.002 kg/m2.
2.5. Statistical analysis
As part of an exploratory analysis in preparation for this investigation, WCC attendance during the months of the pandemic in 2020 were tallied and compared to WCC attendance in the pre-pandemic era (2017–2019). WCC attendance returned to near-normal levels in September 2020 (as detailed in results section). Hence, the comparative regression analysis was pre-specified to include only the months of near-normal WCC attendance from September to December. This reduced bias that would be introduced in earlier months if patients already being monitored for weight concerns were preferentially encouraged to attend WCCs during times of high community spread.
Descriptive statistics were calculated for baseline characteristics of the study population (counting distinct WCC pairs contributed to the study) and categorized by age group, BMI at prior WCC, insurance payor, race, sex, and census division. To investigate trends over time, the mean ΔBMIadj stratified by month from 2017 to 2020 for qualifying WCCs among age groups 6–9, 10–13, 14–17 was calculated. The mean was calculated for September-December 2017–2019, and separately for September-December 2020, overall and for subgroups of age, sex, race, prior WCC BMI, and prior WCC insurance status. Finally, a multivariable linear regression was performed to estimate the difference in the mean of individual ΔBMIadj in September – December 2020 compared to ΔBMIadj in September – December 2017–2019. Individual ΔBMIadj was regressed on year=2020 and coviariates age, sex, race, prior WCC BMI, and prior WCC insurance status.
A sensitivity analysis was conducted to assess the potential distortion of results by selection into the cohort. Cohort selection happens at three stages: (1) the patient is selected into the Optum® COVID-19 data because of a COVID-19 diagnosis or test; (2) the patient attended the WCC; and (3) the patient's BMI was not missing. The challenges of processing near-real-time data led to increased missingness in BMI data during the last few months of 2020. To evaluate the first point of selection, the sensitivity analysis compared September (of 2019 or 2020) ΔBMIadj between patients who were and were not selected into the Optum® COVID-19 data. To assess the second and third points of selection, the sensitivity analysis compared ΔBMIadj in September – December 2019 and September – December 2020 among four groups: patients who attended a WCC and had non-missing BMI during both years, patients who attended a WCC during 2019 but not 2020, patients who attended a WCC during 2020 but not 2019, and patients who attended WCC both years but had missing BMI in 2020. All data processing and statistical analyses were performed using SAS version 9·4 (Cary, NC) and R version 4·0·3 (R Core Team, 2020).
3. Funding
The study was funded by Amgen, Inc. All authors are employees, contractors, or consultants of Amgen, Inc. This work was done under the COVID-19 efforts of Amgen's Center for Observational Research. The authors worked as an independent team to design and conduct the study. All authors had access to the data and concurred with the decision to submit the manuscript for publication.
4. Results
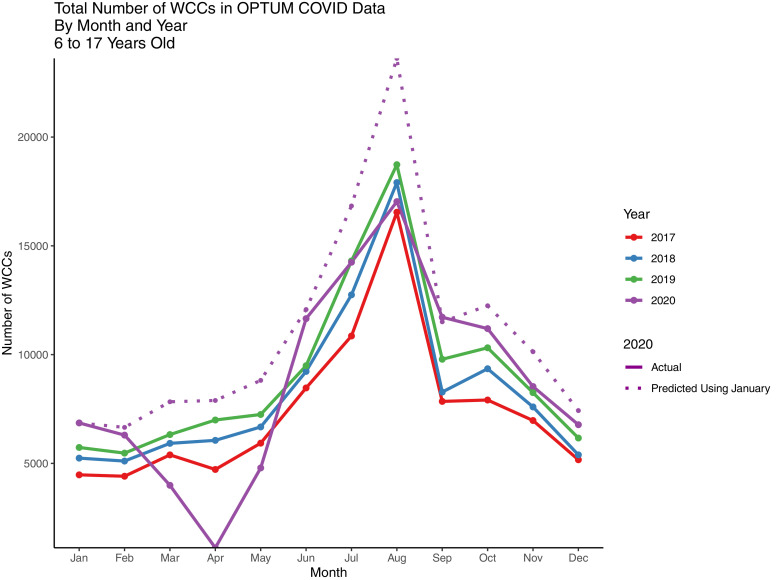
WCC attendance in the US was nearly absent in April 2020, likely as a direct effect of the pandemic lockdown restrictions or fear of infection. However, WCC attendance returned to predicted levels by September 2020 and remained near predicted levels for the remainder of 2020 (Fig. 1). Therefore, this study omitted data from April 2020 from the descriptive analysis figure and chose the time period September – December 2020 for the comparative analysis.
Fig. 1.
Count of all well check checks documented in Optum® COVID-19 EHR by month and year. Dotted line represents the expected number in February-December 2020 extrapolated from the observed number in January 2020 (before pandemic shutdowns) using the ratios observed in February-December of 2017–2019 to January 2017–2019.
There were 183 725 children with at least one WCC in Optum® COVID-19 data during 2017–2020. Of these, 104 852 had at least one qualifying WCC pair, of whom 96 501 did not meet any exclusion criteria and were included in the analyses (Supplementary Fig. 1). The 96 501 individual patients contributed 191 846 WCC pairs to the study. The age groups were roughly balanced, with slightly more 14-to-17-year-olds (38%) than 6-to-9-year-olds (30%) and 10-to-13-year-olds (32%). Two-thirds of the BMIs at the prior WCC where healthy, with the remainder evenly split between overweight BMIs and obese BMIs. Of the pairs, 81% had commercial insurance or an alternative payor at the prior WCC, 14% had Medicaid or were uninsured, and 5% were unknown. The population was largely based in the Northeast (i.e., New England with 21% and Middle Atlantic with 13%) and Midwest (East North Central with 20% and West North Central with 32%) areas of the US (Table 1). For 32,211 (68%) of the WCC pairs in 2020, the patient also contributed at least one ΔBMIadj to the study in 2017–2019 (data not shown).
Table 1.
Baseline characteristics, counted by the WCC pairs that each contributed one ΔBMIadj measurement to the analysis rather than by distinct patient. One patient may have contributed WCC pairs in multiple years.
| 2017-2019 | 2020 | Overall | |
|---|---|---|---|
| Overall | 144,714 | 47,132 | 191,846 |
| Age Group | |||
| 6 to 9 | 42,327 (29·2%) | 15,019 (31·9%) | 57,346 (29·9%) |
| 10 to 13 | 47,052 (32·5%) | 15,056 (31·9%) | 62,108 (32·4%) |
| 14 to 17 | 55,335 (38·2%) | 17,057 (36·2%) | 72,392 (37·7%) |
| BMI at Prior WCC | |||
| Healthy Weight | 94,857 (65·5%) | 30,233 (64·1%) | 125,090 (65·2%) |
| Overweight | 24,818 (17·1%) | 8,074 (17·1%) | 32,892 (17·1%) |
| Obese | 25,039 (17·3%) | 8,825 (18·7%) | 33,864 (17·7%) |
| Insurance at Prior WCC | |||
| Commercial / Other Payor | 117,216 (81·0%) | 38,682 (82·1%) | 155,898 (81·3%) |
| Medicaid / Uninsured | 19,110 (13·2%) | 7,421 (15·7%) | 26,531 (13·8%) |
| Unknown | 8,388 (5·8%) | 1,029 (2·2%) | 9,417 (4·9%) |
| Race | |||
| Asian | 2,607 (1·8%) | 907 (1·9%) | 3,514 (1·8%) |
| White | 111,765 (77·2%) | 35,276 (74·8%) | 147,041 (76·6%) |
| Other / Unknown | 11,507 (8·0%) | 4,448 (9·4%) | 15,955 (8·3%) |
| Black | 7,691 (5·3%) | 2,508 (5·3%) | 10,199 (5·3%) |
| Hispanic | 11,144 (7·7%) | 3,993 (8·5%) | 15,137 (7·9%) |
| Sex | |||
| Female | 73,167 (50·6%) | 23,772 (50·4%) | 96,939 (50·5%) |
| Male | 71,547 (49·4%) | 23,360 (49·6%) | 94,907 (49·5%) |
| Census Division | |||
| East North Central | 28,700 (19·8%) | 9,898 (21·0%) | 38,598 (20·1%) |
| East South Central | 625 (0·4%) | 201 (0·4%) | 826 (0·4%) |
| Middle Atlantic | 17,135 (11·8%) | 8,229 (17·5%) | 25,364 (13·2%) |
| Mountain | 1,736 (1·2%) | 584 (1·2%) | 2,320 (1·2%) |
| New England | 31,702 (21·9%) | 8,756 (18·6%) | 40,458 (21·1%) |
| Other/Unknown | 3,287 (2·3%) | 1,218 (2·6%) | 4,505 (2·3%) |
| Pacific | 1,953 (1·3%) | 635 (1·3%) | 2,588 (1·3%) |
| South Atl/West South Crl | 11,682 (8·1%) | 4,045 (8·6%) | 15,727 (8·2%) |
| West North Central | 47,894 (33·1%) | 13,566 (28·8%) | 61,460 (32·0%) |
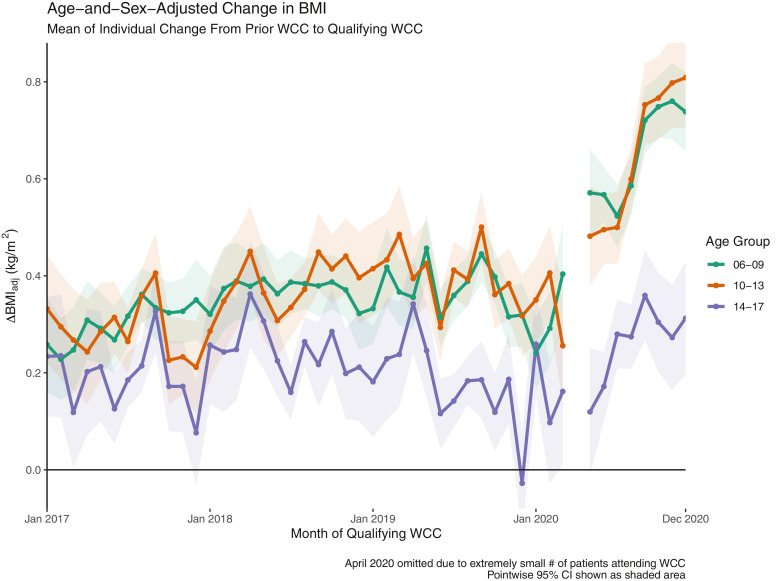
The mean ΔBMIadj by age group and month of qualifying BMI is shown in Fig. 2. From 2017 through March 2020, the mean [95% CI] ΔBMIadj for 6-to-9-year-olds was 0·35 [0·33,0·38] kg/m2 with an upward trend of 0·002 [0·000, 0·004] kg/m2/month; the mean [95% CI] for 10-to-13-year-olds was 0·37 [0·35, 0·39] kg/m2 with an upward trend of 0·003 [0·001, 0·005] kg/m2/month; the mean [95% CI] for 14-to-17-year-olds was 0·20 [0·18, 0·22] kg/m2 with no statistically significant trend. WCC attendance nearly ceased in April, which is not shown for that reason, and continued low through the summer. By the time WCC attendance returned to its predicted level in September, ΔBMIadj for the younger two groups had doubled to 0·72 [0·65, 0·79] for 6-to-9-year-olds and 0·75 [0·67, 0·84] for 10-to-13-year-olds, an increase sustained until the end of the year.
Fig. 2.
Mean of individual ΔBMIadj values during WCCs divided by age group. Mean is represented at a given month relative to the individual's previous WCC (9-to-15 months previous) stratified by age group, with shaded 95% CIs.
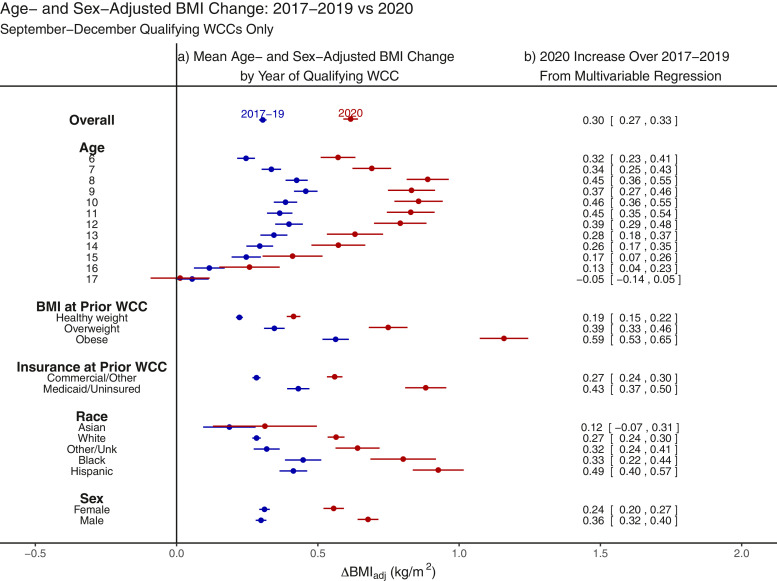
The results of the multivariable regression comparing ΔBMIadj in qualifying WCCs from September – December 2020 to those in September – December 2017 – 2019 is displayed in Fig. 3. Subgroups of children with the highest ΔBMIadj at baseline also had the largest pandemic increases in ΔBMIadj above baseline. These subgroups included children aged 8 to 12, children with pre-existing obesity, children with Medicaid or who were uninsured, and Black and Hispanic children. The change in BMI was most profound in children with pre-existing obesity; the mean ΔBMIadj of this group at September – December WCCs was 1·15 [1·07,1·24] kg/m2, more than double the previous ΔBMIadj of this group.
Fig. 3.
Age- and Sex-adjusted BMI change, years 2017-2019 vs 2020 (September-December WCCs). (a) mean of individual ΔBMIadj values during WCC of September-December 2017–2019 (blue) or September-December 2020 (red), overall and by subgroups, with bars representing 95% CIs; (b) regression coefficients and CIs of binary independent variable year=2020, from multivariable linear regression of ΔBMIadj on independent variables year=2020 and covariates age, prior WCC BMI category, prior WCC insurance status, race, and sex (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.).
The bias analysis showed similar statistics (mean, standard deviation, 50th and 90th percentiles) in September 2019 between children who were in Optum® COVID-19 data and children who were only in Optum® EHR (non-COVID) data. Both groups showed similar increases in September 2020 over September 2019 (Supplementary Table 1). Additional bias analysis showed similar September – December 2019 statistics in children who did not attend or whose BMI was missing at a WCC in September – December 2020, compared to those who did (Supplementary Table 2).
Sensitivity analysis with < 5th percentile BMI removed from the list of exclusion criteria yielded a 5% bigger cohort with nearly identical regression coefficients (data not shown).
5. Discussion
The results of this study showed an increase in the rate of unhealthy weight gain during the pandemic compared to the rate before the pandemic.
This is likely, in part or in whole, a result of the pandemic-related lifestyle changes reported in previous literature [17] (including decreased physical activity [18,19], changes in diet composition [20], and increased indoor sedentary behaviors [19]). The findings are consistent in direction to predictions made by a simulation study [21].
The gap widened between subgroups who were, and subgroups who were not, already vulnerable to excess weight gain. Children who lack commercial insurance, who had pre-existing obesity, and who were Black or Hispanic had the highest rate of ΔBMIadj before the pandemic and, on top of that, suffered the biggest increase over pre-pandemic rates. This finding highlights important public health implications for disparities as part of the pandemic.
It was to some degree unexpected that 8-to-12-year-olds had more marked increases in weight gain than adolescents. One possible explanation is that screen time habits may be well-established by the time a child reaches adolescence, whereas younger children may have been pressed to accommodate enhanced screen time in response to the COVID-19 pandemic.
Interestingly, boys’ ΔBMIadj increased more than girls’ relative to pre-pandemic levels, although pre-pandemic levels were roughly equal. This may also be reflective of greater prevalence of electronic gaming device use among boys, another means of screen time during the pandemic [22].
Strengths of this research include the size of the pediatric population accessible and the longitudinal quality of the study. These data, drawing from all payor types, represent a diverse range of socioeconomic status. Moreover, the recency of data availability was a unique strength of this study. The ΔBMIadj metric allows longitudinal evaluation of BMI more consistent than change in BMI percentile or z-score and more sensitive than change in percent-obesity. Evaluating ΔBMIadj at WCCs in the setting of high WCC attendance prevents the selection bias encountered by relying on BMIs measured at sick visits or on self-reporting in surveys.
The study has some limitations. The method of age assignment will not bias the results noticeably, as already discussed, but will widen CIs slightly, particularly in younger age groups. Additionally, this database does not reflect the geographic and racial diversity of the US, being drawn mainly from the northeast and midwest. While sub-group analyses provided data on minority subgroups, the Asian subgroup in particular was small enough that its confidence intervals were quite large. Finally, the cohort passed through three selection steps discussed above to be included in the study. While it is possible that these children had a different outcome from those not selected, the sensitivity analysis identifying similar and comparable results between 2019 and 2020 strongly reassures against selection playing a determinant role in the results.
Opportunities for further research include evaluating the weight gain trends in pre-school children. Only school-aged children were included in this analysis, as these children were likely most impacted by school closures and lockdown restrictions in the US since the start of the pandemic. Additionally, opportunities exist to explore the influence of geographic factors and local school closure patterns. As part of the de-identification process, patient location in this data was only reported as the census division, which is a geographical area much bigger than standard policy-forming regions. Further, there is limited knowledge regarding the equivalence and generalizability of the health care systems sending data from different census divisions to Optum®. Therefore, we did not attempt geographic analysis with this data. Finally, examining the association between ΔBMIadj and individual food choices, activity patterns, and mental health would be informative but it was not possible to explore with this data.
Although this study focused on the early effect of pandemic restrictions on children and resulting unhealthy weight gain observed during the first year of COVID-19, it will be important to continue monitoring health indicators in this population. During the next phase of the pandemic, as restrictions are eased, state-based re-openings are planned and implemented, and vaccines are distributed, information on the health outcomes of children will be critical to policy-makers, educators, and health care professionals as health promotion and mitigation efforts are enacted which provide more robust immediate and long-term support to one of the US's most vulnerable populations.
Data sharing
The data that support the findings of this study are available, where permitted, from the corresponding author (CGB) upon reasonable request.
Funding
Amgen, Inc.
Declaration of Competing Interest
AC is an employee of Amgen, Inc; AL, JM, CAB, JHP, KAR, FH and CGB are employees at Amgen, Inc and declare stock option in Amgen, Inc; AL declares stock in Johnson and Johnson as well; JMS is a consultant of Amgen, Inc, reports consulting fees at Amgen, Inc and is a formal employee of Amgen, Inc; JRS is a contract employee at Amgen, Inc through SimulStat and declares stock option at Amgen, Inc.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.eclinm.2021.101026.
Appendix. Supplementary materials
References
- 1.Dunton G.F., Do B., Wang S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20(1):1351. doi: 10.1186/s12889-020-09429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Francisco R., Pedro M., Delvecchio E. Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Front Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.570164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McGuine T.A., Biese K.M., Petrovska L. Mental health, physical activity, and quality of life of US adolescent athletes during COVID-19-related school closures and sport cancellations: a study of 13,000 athletes. J Athl Train. 2020 doi: 10.4085/478-20. [DOI] [PubMed] [Google Scholar]
- 4.Moore S.A., Faulkner G., Rhodes R.E. Impact of the COVID-19 virus outbreak on movement and play behaviors of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. 2020;17(1):85. doi: 10.1186/s12966-020-00987-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruiz-Roso M.B., de Carvalho Padilha P., Mantilla-Escalante D.C. COVID-19 Confinement and changes of adolescent's dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients. 2020;12(6) doi: 10.3390/nu12061807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheung Y.B., Machin D., Karlberg J., Khoo K.S. A longitudinal study of pediatric body mass index values predicted health in middle age. J Clin Epidemiol. 2004;57(12):1316–1322. doi: 10.1016/j.jclinepi.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 7.Ray K.N., Shi Z., Ganguli I., Rao A., Orav E.J., Mehrotra A. Trends in pediatric primary care visits among commercially insured US children, 2008-2016. JAMA Pediatr. 2020;174(4):350–357. doi: 10.1001/jamapediatrics.2019.5509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Himes J.H. Challenges of accurately measuring and using BMI and other indicators of obesity in children. Pediatrics. 2009;124(Suppl 1):S3–22. doi: 10.1542/peds.2008-3586D. [DOI] [PubMed] [Google Scholar]
- 9.Center for Disease Control. Interactive Summary Health Statistics for Children –2019. https://wwwn.cdc.gov/NHISDataQueryTool/SHS_child/index.html (accessed 5/1/2021).
- 10.Center for Disease Control. Clinical growth charts. https://www.cdc.gov/growthcharts/clinical_charts.htm (accessed 1/15/2021).
- 11.Freedman D.S., Woo J.G., Ogden C.L., Xu J.H., Cole T.J. Distance and percentage distance from median BMI as alternatives to BMI z score. Br J Nutr. 2020;124(5):493–500. doi: 10.1017/S0007114519002046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berkey C.S., Colditz G.A. Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Ann Epidemiol. 2007;17(1):44–50. doi: 10.1016/j.annepidem.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Chambers M., Tanamas S.K., Clark E.J. Growth tracking in severely obese or underweight children. Pediatrics. 2017;140(6) doi: 10.1542/peds.2017-2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cole T.J., Faith M.S., Pietrobelli A., Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr. 2005;59(3):419–425. doi: 10.1038/sj.ejcn.1602090. [DOI] [PubMed] [Google Scholar]
- 15.Vanderwall C., Eickhoff J., Randall Clark R., Carrel A.L. BMI z-score in obese children is a poor predictor of adiposity changes over time. BMC Pediatr. 2018;18(1):187. doi: 10.1186/s12887-018-1160-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Center for Disease Control. Modified z-scores in the CDC growth charts. https://www.cdc.gov/nccdphp/dnpa/growthcharts/resources/biv-cutoffs.pdf (accessed 1/8/2021).
- 17.Stavridou A., Kapsali E., Panagouli E., Thirios A., Polychronis K., Bacopoulou F., Psaltopoulou T., Tsolia M., Sergentanis T.N., Tsitsika A. Obesity in children and adolescents during COVID-19 pandemic. Children. 2021;8(2):135. doi: 10.3390/children8020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dunton G.F., Do B., Wang S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20(1):1351. doi: 10.1186/s12889-020-09429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jia P., Zhang L., Yu W., Yu B., Liu M., Zhang D., Yang S. Impact of COVID-19 lockdown on activity patterns and weight status among youths in China: the COVID-19 impact on lifestyle change survey (COINLICS) Int J Obes. 2021;45(3):695–699. doi: 10.1038/s41366-020-00710-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adams E.L., Caccavale L.J., Smith D., Bean M.K. Food insecurity, the home food environment, and parent feeding practices in the Era of COVID-19. Obesity. 2020;28(11):2056–2063. doi: 10.1002/oby.22996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.An R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: a microsimulation model. J Sport Health Sci. 2020;9(4):302–312. doi: 10.1016/j.jshs.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sweeting H.N. Gendered dimensions of obesity in childhood and adolescence. Nutr J. 2008;7(1) doi: 10.1186/1475-2891-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.