Abstract
Enterobius vermicularis is the most common parasitic worm responsible for gastrointestinal infection worldwide. Acute appendicitis due to E. vermicularis is a rare infection, affecting mostly the children. In this report, we present the case of a 5-year-old girl infant infected by E. vermicularis found in the appendix lumen. A couple of histopathological and parasitological analyses followed by imaging allowed us to diagnose accurately the etiologic agent. Clinicians should be aware of this parasitosis as a possible cause of acute appendicitis.
Keywords: Enterobiasis, Enterobius vermicularis, Pinworm, Acute appendicitis
Introduction
Enterobius vermicularis infection, a nematode worm of the class Secernentea known as pinworm, is the most common parasitic infection affecting about 200 million people worldwide [1]. It has a pervasive distribution including developed countries but is mainly prevalent in tropical developing countries [2]. It is the most common helminthiasis among pediatric populations [3]. Humans get infected by the fecal-oral route through ingesting the contaminated food or water containing the parasite’s eggs [4]. Enterobius vermicularis life cycle lasts about one month. Adults are mainly located in ileum and ascending colon but can be seen in the appendix lumen. The females leave the colon at night, pass the anus, and depose their eggs at the host’s perianal skin [5]. The disease manifests commonly as nocturnal anal pruritus but insomnia, irritability, colitis are other symptoms can found in some cases [6]. Besides these manifestations, E. vermicularis is reported as a rare cause of acute appendicitis, as the most common abdominal emergency worldwide. Its incidence in appendicitis varies from 0.2 to 4.8 % and seems to affect mostly the young girls [7].
Case presentation
A 5-year-old girl, accompanied with her parents, was referred by her general practitioner to the emergency department of Robert Ballanger hospital (Aulnay-sous-Bois, France). She was originally from Sri-Lanka with no notion of recent travel. She had no history of hospital admission, surgical history or known drugs allergies. On arrival, the patient had a 48 -h history of predominant abdominal pain in the right iliac fossa (RIF), accompanied by nausea and vomiting, without fever. The primary clinical examination revealed a focal tenderness to deep palpation of the McBurney point, without any palpable masses. These manifestations made us suspicious to an acute appendicitis. Biochemical analysis showed an increased C-reactive protein (68 mg/L, N = 0−5 mg/L) and a normal hepatic function. Blood analysis revealed a normal eosinophil (0.09*109/L, N = 0.02-0.62*109/L) and a mild leukocytosis (12.8*109/L, N = 6.4–10.6*109/L). Ultrasonography showed an enlarged appendix, 5 mm in diameter, with a fat stranding infiltration. Following diagnosis confirmation of appendicitis, a laparoscopic appendectomy was performed. Surgical intervention and histopathological examination revealed a mucous membrane remodeled by follicular lymphoid hyperplasia and the presence of four worms in appendix lumen (Fig. 1). Parasitological direct examination of the worms by microscopy confirmed the diagnosis of acute appendicitis caused by E. vermicularis.
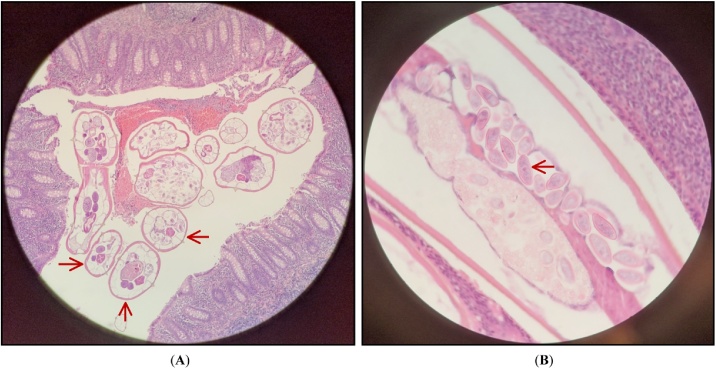
Fig. 1.
Histopathological HES-stained section. A) Cross-sectional view of the appendix containing several pinworms (red arrows) in ×100 magnification, B) Longitudinal-section view demonstrating the presence of a gravid female with uterine tubes filled out by developping eggs (red arrow) in ×400 magnification.
Discussion
Appendicitis, caused by a blockage of the hollow portion of the appendix, is the most common cause of abdominal pain and one of the most common reasons for emergency gastrointestinal surgery [8]. It is commonly caused by fecal stasis, fecaliths and lymphoid hyperplasia [9]. Beside mentioned causative agents, undigested vegetable residues, fruit seeds, tumors and intestinal parasites have been reported as other appendicitis etiologies [10]. Infection of the appendix itself by parasites is rather rare. Nevertheless, some parasitic agents such as Schistosoma spp, Taenia spp and Ascaris lumbricoides have been reported as the causative agent [11,12]. Based on the literature, few cases of appendicitis caused by E. vermicularis have been reported in Asia and Canada [13,14]. Despite the widespread prevalence of this parasite mainly in the tropics [2], our patient was most probably infected in France based on her medical record. On the other side, the role of this parasite in appendicitis is still controversial as usually resected specimens show little or no histological signs of inflammation [6]. When located in the appendix lumen, pinworms might mimic appendicitis clinical features but can rarely be associated with pathologic findings of acute appendicitis [15]. The problem of determining whether pinworms are causative agent of the appendicitis or incidental findings during appendectomy has been discussed for more than a century. Nevertheless, the pinworms infestation is still reported as an etiology causing acute appendicitis [7,13]. In absence of laboratory test specific for appendicitis, a couple of histopathological and parasitological analyses followed by imaging, allowed us to diagnose acute appendicitis in our patient, caused by E. vermicularis.
Regarding the infection route of enterobiasis, the main preventive actions rely mainly on the hygienic measures especially in recurring cases. Furthermore, surgical removal of the appendix by laparotomy or laparoscopy is a conventional intervention performed for acute appendicitis. In case of our patient, she underwent an appendectomy. The treatment was followed by using Flubendazole (100 mg/d) for 15 day. The health improvement was noticed 24 -h after the first dose.
Conclusion
We highlight the appendix infection caused by E. vermicularis. We emphasize on the importance of early diagnosis and accurate identification of the causative agent responsible of appendicitis, which allows effective anti-microbial therapy. Physicians should also screen family members of affected patient because the family members usually share similar eating habits. It is important for clinicians to pay attention to patient having enterobiasis and consider the possibility on an eventual acute appendicitis. Clinicians should be aware of this parasitosis with appendicular colic leading to potentially severe complications.
Declaration of Competing Interest
The authors report no declarations of interest.
Funding
This research received no external funding.
Ethical approval
A written consent was provided and signed by the parents of the patient including the authorization for publishing the clinical information.
CRediT authorship contribution statement
Jimmy Anders Antilahy: Conceptualization, Methodology, Validation, Writing - original draft. Mohammad Akhoundi: Conceptualization, Methodology, Validation, Writing - original draft, Writing - review & editing. Mohamed Belaloui: Methodology. Anna Borovkov: Methodology. Anthony Marteau: Methodology, Validation. Eric Bonte: Methodology. Arezki Izri: Conceptualization, Methodology, Validation, Writing - review & editing.
References
- 1.Hasan A., Nafie K., El-Sayed S., Nasr M., Abdulmohaymen A., Baheeg M. Enterobius vermicularis in appendectomy specimens; Clinicopathological assessment: cross sectional study. Ann Med Surg. 2020;60:168–172. doi: 10.1016/j.amsu.2020.10.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laoraksawong P., Pansuwan P., Krongchon S., Pongpanitanont P., Janwan P. Prevalence of Enterobius vermicularis infections and associated risk factors among schoolchildren in Nakhon Si Thammarat. Thailand. Trop Med Health. 2020;48:1–15. doi: 10.1186/s41182-020-00270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ariyarathenam A.V., Nachimuthu S., Tang T.Y., Courtney E.D., Harris S.A., Harris A.M. Enterobius vermicularis infestation of the appendix and management at the time of laparoscopic appendicectomy: case series and literature review. Int J Surg. 2010;8:466–469. doi: 10.1016/j.ijsu.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Efared B., Atsame-Ebang G., Soumana B.M., Tahiri L., Hammas N., El Fatemi H. Acute suppurative appendicitis associated with Enterobius vermicularis: an incidental finding or a causative agent? A case report. BMC Res Notes. 2017;10:1–4. doi: 10.1186/s13104-017-2822-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehlhorn H. Enterobius vermicularis. In: Mehlhorn H., editor. Encyclopedia of parasitology. Springer Berlin Heidelberg; Berlin, Heidelberg: 2014. pp. 1–5. [Google Scholar]
- 6.Jardine M., Kokai G.K., Dalzell A.M. Enterobius vermicularis and colitis in children. J Pediatr Gastroenterol Nutr. 2006;43:610–612. doi: 10.1097/01.mpg.0000243425.01593.58. [DOI] [PubMed] [Google Scholar]
- 7.El Bakouri A., Hajri A., Ettaoussi A., Bouali M., Bensardi F., El Hattabi K. Acute appendicitis secondary to Enterobius vermicularis infestation: a case report. Eur J Med Heal Sci. 2020;2:1–3. [Google Scholar]
- 8.Shogilev D.J., Duus N., Odom S.R., Shapiro N.I. Diagnosing appendicitis: evidence-based review of the diagnostic approach in 2014. West J Emerg Med. 2014;(15):859–871. doi: 10.5811/westjem.2014.9.21568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prystowsky J.B., Pugh C.M., Nagle A.P. Appendicitis. Curr Probl Surg. 2005;42:694–742. doi: 10.1067/j.cpsurg.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Yilmaz M., Akbulut S., Kutluturk K., Sahin N., Arabaci E., Ara C. Unusual histopathological findings in appendectomy specimens from patients with suspected acute appendicitis. World J Gastroenterol. 2013;19:4015–4022. doi: 10.3748/wjg.v19.i25.4015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bourée P., Bisaro F., Kanner A., Djibo N. Appendicites parasitaires. Rev Francoph des Lab. 2008;399:79–86. [Google Scholar]
- 12.Engin O., Calik S., Calik B., Yildirim M., Coskun G. Parasitic appendicitis from past to present in Turkey. Iran J Parasitol. 2010;5:57–63. [PMC free article] [PubMed] [Google Scholar]
- 13.Hammood Z.D., Salih A.M., Mohammed S.H., Kakamad F.H., Salih K.M., Omar D.A. Enterobius vermicularis causing acute appendicitis, a case report with literature review. Int J Surg Case Rep. 2019;63:153–156. doi: 10.1016/j.ijscr.2019.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Habashi R., Patrick Lisi M. Acute appendicitis and Enterobius vermicularis infestation. Cmaj. 2019;191:E477. doi: 10.1503/cmaj.181194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gialamas E., Papavramidis T., Michalopoulos N., Karayannopoulou G., Cheva A., Vasilaki O. Enterobius vermicularis: a rare cause of appendicitis. Turkiye Parazitol Derg. 2012;36:37–40. doi: 10.5152/tpd.2012.09. [DOI] [PubMed] [Google Scholar]