Abstract
Following the outbreak of the COVID-19 pandemic, the delivery of face-to-face (F2F) therapeutic interventions and neuroimaging assessments for children with Autism Spectrum Disorder (ASD) has been disrupted. To resume interventions and assessments, many services are now using telehealth-based online platforms. Using the Zoom conferencing platform, our research group has been providing creative play-based interventions to school-age children with Autism Spectrum Disorder. The feedback on this telehealth intervention experience has been generally positive (Mean satisfaction score: 4.4 out of the 5-point Likert scoring range) and our preliminary data from 6 children with ASD suggest training-related improvements in gross motor, balance, and imitation. Despite the positive results, it remains to be explored if the effects of telehealth interventions are similar to those of F2F interventions. Neuroimaging techniques could provide objective measures of intervention effects. However, this will require researchers to resume neuroimaging research by adopting safe public health protocols to control the risk of COVID-19 transmission. In this short report, we summarize existing safety protocols for F2F neuroimaging research, our own experiences of safely conducting alternative, on-site and off-site neuroimaging data collection, as well as the potential opportunities of using online data sharing and low-cost, remote neuroimaging/electrophysiological techniques to continue brain research during the pandemic.
Keywords: Autism, COVID-19, Telehealth, Neuroimaging, Remote brain research
Lay abstract:
The COVID-19 pandemic has caused disruption in F2F healthcare delivery and neuroimaging research, especially when involving vulnerable populations such as children with Autism Spectrum Disorder. Given the easy access to multiple video conferencing platforms, many healthcare services have moved to an online delivery format (i.e., telehealth). It is important to monitor the behavioral and neural effects of telehealth interventions, and resume neuroimaging research while adopting public health safety protocols to control the risk of COVID-19 transmission. We summarize the existing safety protocols and our own experience from in-person fNIRS neuroimaging data collection (on-site, home, and outdoor settings), as well as the potential opportunities of using online data sharing and low-cost, remote neuroimaging/electrophysiological techniques to continue brain research during the pandemic.
The global COVID-19 pandemic has caused major disruptions in basic science and applied research. The pandemic has imposed significant restrictions on conducting in-person, neuroimaging research as well as research evaluating the efficacy of different therapeutic interventions. However, considering the projected and protracted timeline for the pandemic over the next several months, it is crucial that we resume neuroimaging research as well as applied research that has important implications for clinical practice, while adopting appropriate public health and safety measures to control the risk of COVID-19 transmission. The current opinion paper summarizes existing protocols, guidelines, and potential opportunities available for safe conduct of online and in-person basic science and applied research amidst the pandemic. We also summarize our own experience with remote therapy delivery using telehealth and the use of neuroimaging techniques to assess intervention effects.
Healthcare delivery during the COVID-19 pandemic and the importance of outcome monitoring
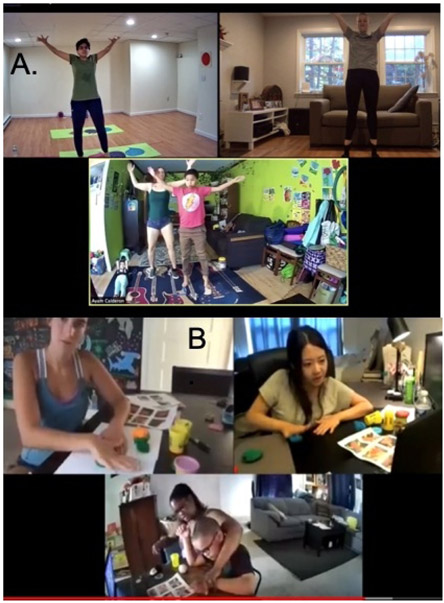
Following the outbreak of COVID-19, the delivery of therapeutic interventions to children with special needs has been significantly disrupted. Children with special needs including those with Autism Spectrum Disorder (ASD) are not receiving adequate amount and types of interventions (Jeste et al., 2020). For example, in a survey circulated to parents of children with intellectual and developmental disabilities, 74% of the parents reported that their children lost access to at least one therapeutic or educational service following the onset of the pandemic (Jeste et al., 2020). The availability and ease of access to multiple virtual communication platforms has enabled many healthcare services, including physical, occupational, and speech therapies to move to an online delivery format. A survey study on tele-rehabilitation reported 93.7-99% patient satisfaction with online delivery of physical therapy, occupational therapy, and speech and language therapy services, suggesting that telehealth seems to be a promising avenue for continuing clinical care of patients remotely (Tenforde et al., 2020). Our own research team is presently conducting an NIH-funded, telehealth-based pilot randomized controlled trial comparing the effects of creative movement interventions to a standard of care, seated play intervention in school-age children with ASD (Figure 1). Based on our experiences, there are advantages and disadvantages to delivering telehealth movement interventions. The advantages include (1) reduced cost/time to commute between lab and intervention site (child’s school/home), (2) increased pragmatic nature of the intervention with more family (i.e., parent and sibling) involvement, and (3) provide individualized intervention that is tailored to the child’s needs and interests to facilitate carryover to real-world interactions and daily activities. These opportunities encourage the parent and child to continue the training activities beyond the context of the remote intervention and in their daily lives. For example, parents inform us that their child is communicating more during mealtimes or spontaneously initiating more instances of social interactions with their caregivers and siblings during the course of the day. The disadvantages of this approach however include (1) increased time to develop the intervention and to build a relationship with the child, (2) need for high energy remote trainers due to the lack of physical presence, and (3) technical difficulties with video conferencing software. During telehealth sessions, given the physical proximity between parents and children, the researchers need to rely on parents to provide prompting, reinforcement, modeling, redirection, and manual assistance to the child, making them equal partners, or cotherapists. Although this makes the intervention externally valid, there is more time and effort devoted to training parents compared to the time taken when interventions are directly provided to the child. The virtual nature of the intervention requires remote partners to be more energetic and animated (i.e., louder voice and exaggerated gestures) to engage children with ASD. Lastly, there are technical glitches such as slowed internet streaming and voice over internet protocol (voip) issues leading to lagging of the video and audio that undermine the moment-to-moment social interactions and synchronous movements between the child and the remote trainer.
Figure 1:
Zoom-based interventions offered to participating children. 1A shows activity in the Creative Movement group and 1B shows activity in the standard of care, seated play group. Written permission for publication of participant and experimenter pictures has been taken.
Our pilot data from 6 children with ASD suggest that children were able to engage in 60 minutes of either gross-motor activities including music making, dance, yoga (Figure 1A), or seated play activities including story reading and fine-motor games such as building and art-craft (Figure 1B). These activities were delivered through Zoom, twice a week, for 8 weeks. When providing remote, telehealth interventions we have used a family/child-centered, collaborative model to ensure that the intervention fits with the parent and child’s level of comfort, ability, and functioning. In our current intervention study, we schedule orientation and training meetings with the parent before the start of both the testing and training sessions to explain the various activities that will be done, the parent’s role during testing/training, and strategies they can use to guide, model, and reinforce their child. Through discussions with the parent during this meeting, we also make sure to understand the child’s needs, strengths, and likes/dislikes to tailor the intervention to the child’s preferences, needs, and functional level. We also incorporate parent-recommended behavioral strategies to motivate the child during training activities. Moreover, we establish reasonable parent and child-determined goals using the Goal Attainment Scaling system (GAS; Kiresuk & Sherman, 1968) for the training sessions. Thereafter, across training weeks, we assess progress on training goals on a weekly basis as well as at the end of the intervention using the GAS.
Feedback from both parents and children with ASD on their experience of the telehealth intervention has been generally positive (Mean satisfaction score: children gave a 4.4 and parents gave a 4.3 out of the 5-point Likert scoring range) and our preliminary data suggest that participants are showing training-related improvements in gross motor, balance, and imitation skills, which we plan to report in future publications after study completion. Although remote interventions may yield positive results, it remains to be explored if the effects of telehealth interventions are similar to those of face-to-face (F2F) interventions. We are addressing this question through our neuroimaging-based pre and post-tests. In these testing sessions, the child and adult engage in (1) solo, (2) F2F, and (3) remote synchronous actions while drumming and swaying to evaluate the differential effects of F2F versus remote action synchrony on the amount of cortical activation in children with ASD. This will give us some insight on how the telehealth/remote nature of our intervention might differentially impact brain activity patterns of the participating children. There is evidence supporting greater cortical activation when observing and imitating live actions compared to video recordings or 2D stimuli (Järveläinen et al., 2001; Reader & Holmes, 2015; Jola & Grosbras, 2013) suggesting that the telehealth intervention might not evoke similar levels of engagement and cortical activation as F2F interventions.
Furthermore, there is growing research on the use of functional Magnetic Resonance Imaging (fMRI) and electroencephalogram (EEG) as an objective measure to track training-related changes in cortical activation and connectivity in children with ASD (Corbett et al., 2016; Sharda et al., 2018). Corbett et al. (2016) found training-related changes in evoked response potentials over the parietal cortices in children with ASD after they received peer-mediated, theater-based intervention. Using fMRI, Sharda et al. (2018) found greater resting-state connectivity between temporal/frontal cortices and striatal regions as well as reduced connectivity between temporal and visual cortices in children with ASD after they received a bout of musical intervention. These findings support our approach of studying changes in cortical activation/connectivity as an objective measure to monitor treatment response to creative movement interventions.
Neuroimaging assessments and brain research during the COVID-19 pandemic
Neuroscientists are also facing difficulties when conducting neural assessments during the COVID-19 pandemic. The restricted access to on-site facilities limits the feasibility of conducting neuroimaging research. Neuroimaging equipment are traditionally expensive, not portable due to size, and require trained experts to perform the assessments. As a result, after the outbreak of COVID-19, most of the non-emergency neuroimaging assessments and on-site brain research had suddenly come to a halt. For instance, in Italy, the number of EEG assessments reduced by 76 ± 20% (Assenza et al., 2020). It is important to resume neuroimaging assessments for the purposes of disease diagnosis, progression monitoring, and assessment of the efficacy of therapeutic interventions while taking proper precautions to prevent COVID-19 transmission. Here, we summarize the existing methods and protocols, and share our own experiences conducting neural assessments during the COVID-19 pandemic.
Neuroimaging data sharing across sites: During the COVID-19 pandemic, it is important to decentralize the healthcare system/neuroimaging facilities and limit the number of staff/patients on-site at a time. Teleradiology, a practice that allows neuroimaging data to be transferred between sites and for radiologists to read/interpret the images off-site, has been increasingly applied in several US clinics during the COVID-19 pandemic (Quraishi, Rizvi, & Heidel, 2020). Along similar lines, sharing of neuroimaging data has been encouraged during the pandemic, as it facilitates the reproducibility of studies, increases the quantity and diversity of neuroimaging data (i.e., data collected in different locations can be pooled), and reduces the requirement of participants to visit neuroimaging facilities in-person (Poline et al., 2012). Here we list some of the neuroimaging databases for data sharing, including the International Neuroimaging Data Sharing Initiative (http://fcon_1000.projects.nitrc.org/), Open fMRI (http://openfmri.org/), and the NIH Pediatric MRI Data Repository (https://www.nitrc.org/projects/pediatric_mri/).
-
On-site neuroimaging with minimized transmission risk: Following initial strict lockdown mandates, presently, several research institutions have resumed onsite research provided researchers adhere to strict COVID-19 safety protocols while conducting neuroimaging with participants. For example, Simmons & Luck (2020) published their protocol to conduct safe EEG research during COVID-19 which includes the following methods: a) prior screening of participants and experimenters for recent contact with individuals presenting COVID-19-related symptoms; b) body temperature checks prior to site entry; c) minimizing on-site exposure time by completing participant orientation and consent procedures in advance online and minimizing the time to apply electrodes; d) use of appropriate personal protective equipment (PPE), including gloves, masks, lab coats, and face shields by participants and research staffs; e) disinfection of equipment and other common touch points; and f) limiting the number of people in the same room while maintaining appropriate social distancing as much as possible (e.g., use of separate areas for EEG application and recording). Similar guidelines have been published for other neuroimaging techniques, e.g., Transcranial Magnetic Stimulation (Bikson et al., 2020). In accordance with our University’s human subjects research guidance, we have been conducting F2F tests by giving participating families two clear options: (1) to engage in remote testing for behavioral tests only or (2) F2F functional neuroimaging tests conducted while following appropriate social distancing and other safety precautions. To alleviate any ethical concerns, we ensure that families know that they can make their independent and voluntary decisions regarding participation in neuroimaging tests which will not affect their overall study participation.
So far, 4 families have enrolled in our study in the current round of testing/training. We generally see 4-8 families in each round of testing/training because we have 4 training teams for this study. Of the 4 families we recruited in the latest round, 2 agreed to complete the F2F neuroimaging testing protocol. The other 2 families chose to engage in remote testing because of geographic distance (>1-hour driving distance) or concerns regarding COVID-19 transmission. In short, it appears that we will have neuroimaging data from a subset of our sample because some families will not participate in the F2F protocol due to aforementioned reasons.
Next, we describe the typical protocol we follow for families who have agreed to do F2F neuroimaging testing during the pandemic. After we determine eligibility, parents and children complete the online consent and assent forms and are debriefed about the testing procedures as well as the precautions we take to reduce the risk of transmission. Procedures to minimize the risk of COVID-19 transmission include online and in-person symptom checks, onsite temperature checks, social distancing, mask wearing, hand sanitization, and limiting the number of individuals in the testing room. On the testing day, before the family travels to the lab, we screen the family regarding any COVID-related symptoms and lack of exposure to individuals with COVID-19 infection. Upon arrival, we reconfirm lack of symptoms or exposure, check their body temperature, and reiterate the important precautions. If families were to report symptoms or positive contact at any point, we will reschedule the visit to a future date after they quarantine according to the mandated state guidelines.
During the testing session, the testers maintain 6 feet distance from the parent and the child except when putting on/taking off the fNIRS cap, and when the tester conducts the spatial registration steps (< 10 minutes). After the visit, we sanitize the cap, the contact surfaces, and touch points. The testers have noted that the children with ASD have been compliant about mask wearing due to similar experiences at their school or extracurricular activities. However, they also express the need to complete the testing swiftly to avoid prolonged F2F interactions. The two participating families responded well to the testing and precautionary procedures and are willing to revisit the lab for post-test and follow-up sessions.
Home visits with limited contact: Researchers could consider home visits with portable neuroimaging equipment, such as LightNIRS (Shimadzu, Inc.), Brite (Artinis, Inc.), LUMO (GowerLabs, Inc.) or NIRSPORT (NIRx, Inc.); which could serve as an alternative to in-lab neuroimaging to avoid disruptions in F2F neuroimaging. However, the portable systems will need to be validated for their accuracy against the gold-standard, in-lab EEG/fNIRS systems. In spite of the presence of novel spatial registration methods to determine brain regions underneath fNIRS channels; its current spatial resolution is much lower than fMRI (Tsuzuki & Dan, 2014). Portable fNIRS and EEG systems come with their own advantages. They are better able to tolerate motion artifacts, allow for F2F, naturalistic social interactions with limited constraints of a cap with channels, and promote compliance from children with greater cognitive and behavioral impairments. Majority of the fMRI studies involving individuals with ASD include individuals with typical cognitive abilities (Philip et al., 2012). However, fNIRS has been used to collect cortical activation data from children with ASD with low cognitive abilities as well (Su et al., 2020). Furthermore, with the rapid development of portable EEG/fNIRS, more spatially resolved fNIRS (i.e., high-density fNIRS), and user-friendly software, we are hopeful that the accessibility of alternate neuroimaging/electrophysiological techniques will increase the possibility for participants and their families to engage in citizen science by conducting home-based, remote neuroimaging. Our research group has used the LightNIRS system to collect cortical activation data from infants and children in their homes. However, the time to set up the equipment is relatively long (~45 minutes). In the future, we hope to pilot a system wherein we set up the equipment ahead of time using a power bank, safely transfer the system to the participants’ homes, and begin testing within a short period of time.
Outdoor data collection: Outdoor data collection might be another way to reduce the transmission risk of COVID-19 as indoor settings are usually linked to greater risk of transmission clusters (Leclerc et al., 2020). Several portable equipment and techniques have been used in outdoor settings, including fNIRS (McKendrick et al., 2017; Piper et al., 2014). However, the natural sunlight could interfere with the data leading to oversaturation. Researchers have used aluminum foil or black cloth to cover the fNIRS probe sets and block ambient light (McKendrick et al., 2017; Piper et al., 2014).
New opportunities from low-cost, cloud-enabled neuroimaging: The rapid development of low-cost and highly portable neuroimaging tools (ex: Smartphone EEG, Stopczynski et al., 2014; in-ear EEG, Athavipach, Pan-Ngum, & Israsena, 2019; Muse headband EEG, Krigolson et al., 2017) opens up avenues for remote brain activation monitoring by giving the device to the user and meeting them remotely to administer tasks. Instead of traveling to the neural test site, the neural test could be delivered to the home and used by the participants with minimal setup/online tutorials. Despite some ethical issues that remain to be addressed (Shen et al., 2020), the participant-driven data collection is desirable during the COVID-19 pandemic.
Future directions
In order to obtain neuroimaging data safely and reliably, customized standard operating procedure (SOP) manuals need to be developed for each clinic/neuroimaging facility. Moreover, the quality and reliability of brain activation data obtained from home visits, outdoor data collection, and remote neuroimaging equipment will need to be carefully assessed and compared. Lastly, further research on the differential behavioral and neural effects of telehealth interventions versus F2F interactions is warranted.
Long-term value of telehealth and remote brain research after COVID-19 pandemic
Despite the challenges in adapting to new methods of healthcare delivery and brain research, the rapid transition to telehealth and online research also brings benefits and new opportunities for researchers. Telehealth reduces commuting costs and increases geographic accessibility in terms of patient populations. Moreover, it affords opportunities for individuals to receive interventions/participate in research studies within their natural environment, including their caregivers and siblings, and makes it a more meaningful intervention for children with developmental disabilities including those with ASD. Lastly, the pandemic has highlighted the value of alternative tools such as portable fNIRS or smartphone EEG to conduct neuroimaging. Compared to fMRI, the aforementioned tools are robust against motion artifacts and permit F2F interactions and naturalistic movements, making them ideal neuroimaging tools for pediatric populations with cognitive and behavioral issues or greater risks to physical health, whose families may prefer to participate through remote or home-based testing.
Statement on Community Involvement.
The intervention described in this paper is a parent-mediated intervention, hence, closely involves parents of children with ASD. However, this short report writing did not involve the parents and only provides results from a parent satisfaction survey completed post-intervention.
Acknowledgments
We would like to thank all the children and families who participated in this study, and the undergraduate students, Marissa Heino, Sarah Williams, Emily Longenecker, Emma Fallon, and Hannah Laue from the University of Delaware for their help with data collections and data analysis.
Funding
This work was supported by the National Institutes of Health through a shared instrumentation grant awarded to the University of Delaware (Grant #: 1S10OD021534-01, PI: Bhat), pilot award funding through an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health (P20 GM103446, PI: Stanhope; U54-GM104941, PI: Binder-Macleod) and funding from the Dana Foundation through a Clinical Neuroscience Award (PI: Bhat).
Footnotes
Declaration of conflicting interests
The author(s) declare no conflicts of interest. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- Assenza G, Lanzone J, Ricci L, Boscarino M, Tombini M, Galimberti CA, … Mecarelli O (2020). Electroencephalography at the time of Covid-19 pandemic in Italy. Neurological sciences, 41(8), 1999–2004. 10.1007/s10072-020-04546-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athavipach C, Pan-Ngum S, & Israsena P (2019). A wearable in-ear EEG device for emotion monitoring. Sensors, 19(18), 4014. 10.3390/s19184014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bikson M, Hanlon CA, Woods AJ, Gillick BT, Charvet L, Lamm C, … Ekhtiari H (2020). Guidelines for TMS/tES clinical services and research through the COVID-19 pandemic. Brain stimulation, 13(4), 1124–1149. 10.1016/j.brs.2020.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett BA, Key AP, Qualls L, Fecteau S, Newsom C, Coke C, & Yoder P (2016). Improvement in social competence using a randomized trial of a theatre intervention for children with autism spectrum disorder. Journal of autism and developmental disorders, 46(2), 658–672. 10.1007/s10803-015-2600-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Järveläinen J, Schürmann M, Avikainen S, & Hari R (2001). Stronger reactivity of the human primary motor cortex during observation of live rather than video motor acts. Neuroreport, 12(16), 3493–3495. 10.1097/00001756-200111160-00024 [DOI] [PubMed] [Google Scholar]
- Jeste S, Hyde C, Distefano C, Halladay A, Ray S, Porath M, … Thurm A (2020). Changes in access to educational and healthcare services for individuals with intellectual and developmental disabilities during COVID-19 restrictions. Journal of intellectual disability research, 10.1111/jir.12776. Advance online publication. 10.1111/jir.12776 [DOI] [PubMed] [Google Scholar]
- Jola C, & Grosbras MH (2013). In the here and now: enhanced motor corticospinal excitability in novices when watching live compared to video recorded dance. Cognitive neuroscience, 4(2), 90–98. 10.1080/17588928.2013.776035 [DOI] [PubMed] [Google Scholar]
- Kiresuk TJ, Sherman RE (1968). Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Mental Health Journal,4, 443–453. 10.1007/BF01530764 [DOI] [PubMed] [Google Scholar]
- Krigolson OE, Williams CC, Norton A, Hassall CD, & Colino FL (2017). Choosing MUSE: validation of a low-cost, portable EEG system for ERP research. Frontiers in Neuroscience,11,109. 10.3389/fnins.2017.00109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leclerc QJ, Fuller NM, Knight LE, CMMID COVID-19 Working Group, Funk S, & Knight GM (2020). What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome open research, 5, 83. 10.12688/wellcomeopenres.15889.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKendrick R, Mehta R, Ayaz H, Scheldrup M, & Parasuraman R (2017). Prefrontal hemodynamics of physical activity and environmental complexity during cognitive work. Human factors, 59(1), 147–162. 10.1177/0018720816675053 [DOI] [PubMed] [Google Scholar]
- Philip RC, Dauvermann MR, Whalley HC, Baynham K, Lawrie SM, & Stanfield AC (2012). A systematic review and meta-analysis of the fMRI investigation of autism spectrum disorders. Neuroscience and biobehavioral reviews, 36(2), 901–942. 10.1016/j.neubiorev.2011.10.008 [DOI] [PubMed] [Google Scholar]
- Piper SK, Krueger A, Koch SP, Mehnert J, Habermehl C, Steinbrink J, … Schmitz CH (2014). A wearable multi-channel fNIRS system for brain imaging in freely moving subjects. NeuroImage, 85 Pt 1(0 1), 64–71. 10.1016/j.neuroimage.2013.06.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poline JB, Breeze JL, Ghosh S, Gorgolewski K, Halchenko YO, Hanke M, … Kennedy DN (2012). Data sharing in neuroimaging research. Frontiers in neuroinformatics, 6, 9. 10.3389/fninf.2012.00009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quraishi MI, Rizvi AA, & Heidel RE (2020). Off-site radiology workflow changes due to the coronavirus disease 2019 (COVID-19) Pandemic. Journal of the American College of Radiology, 17(7), 878–881. 10.1016/j.jacr.2020.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reader AT, & Holmes NP (2015). Video stimuli reduce object-directed imitation accuracy: a novel two-person motion-tracking approach. Frontiers in psychology, 6, 644. 10.3389/fpsyg.2015.00644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharda M, Tuerk C, Chowdhury R, Jamey K, Foster N, Custo-Blanch M, … Hyde K (2018). Music improves social communication and auditory-motor connectivity in children with autism. Translational psychiatry, 8(1), 231. 10.1038/s41398-018-0287-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen FX, Wolf SM, Gonzalez RG, & Garwood M (2020). Ethical issues posed by field research using highly portable and cloud-enabled neuroimaging. Neuron, 105(5), 771–775. 10.1016/j.neuron.2020.01.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons AM, & Luck SJ (2020). Protocol for reducing COVID-19 transmission risk in EEG research. Research square, rs.3.pex-974. 10.21203/rs.3.pex-974/v2 [DOI] [Google Scholar]
- Stopczynski A, Stahlhut C, Larsen JE, Petersen MK, & Hansen LK (2014). The smartphone brain scanner: a portable real-time neuroimaging system. PloS one, 9(2), e86733. 10.1371/journal.pone.0086733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su WC, Culotta M, Mueller J, Tsuzuki D, Pelphrey K, & Bhat A (2020). Differences in cortical activation patterns during action observation, action execution, and interpersonal synchrony between children with or without autism spectrum disorder (ASD): An fNIRS pilot study. PloS one, 15(10), e0240301. 10.1371/journal.pone.0240301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenforde AS, Borgstrom H, Polich G, Steere H, Davis IS, Cotton K, … Silver JK (2020). Outpatient physical, occupational, and speech therapy synchronous telemedicine: a survey study of patient satisfaction with virtual visits during the COVID-19 pandemic. American journal of physical medicine & rehabilitation, 10.1097/PHM.0000000000001571. 10.1097/PHM.0000000000001571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuzuki D, & Dan I (2014). Spatial registration for functional near-infrared spectroscopy: from channel position on the scalp to cortical location in individual and group analyses. NeuroImage, 85, 92–103. 10.1016/j.neuroimage.2013.07.025 [DOI] [PubMed] [Google Scholar]