Abstract
As the main pathogen threatening human and animal health, viruses can affect the immunity and metabolism of bodies. There are innate microbial barriers in the digestive tract of the body to preserve the homeostasis of the animal body, which directly or indirectly influences the host defence against viral infection. Understanding the interaction between viruses and intestinal microbiota or probiotics is helpful to study the pathogenesis of diseases. Here, we review recent studies on the interaction mechanism between intestinal microbiota and viruses. The interaction can be divided into two aspects: inhibition of viral infection by microbiota and promotion of viral infection by microbiota. The treatment of viral infection by probiotics is summarized.
Introduction
Recently, intestinal microorganisms are attracting more attention. Many studies indicate that these microorganisms are correlated with various functions of human body. Intestinal microorganisms are composed of prokaryotic bacteria, archaea, eukaryotic fungi, viruses, and other microorganisms [1]. The study of intestinal microorganisms mainly focuses on intestinal bacteria.
Intestinal microbiota form bacterial communities that mutually benefit humans and are divided into probiotics, opportunistic pathogens, and neutral bacteria. There are about 35,000 types of bacteria in the human intestine [2]. Most of these bacteria are anaerobes, whilst the number of aerobic and facultative anaerobes are much smaller than that of anaerobes [3]. There is a fine-tuned, elastic balance between the microbiota and the host. This relative stability is preserved by a high-level microbial diversity, the geographical distribution of microorganisms, and complex intermolecular communication between multiple parts of the whole organism [4]. The intestinal microbiota is closely related to various diseases of human body, including digestive diseases, respiratory diseases, immune diseases, and metabolic diseases. Hence, the intestinal microbiota plays an important role in treating many human diseases.
Viruses, as pathogens with no cellular structure, pose a serious threat to human health in the way that they parasitize and self-replicate within cells. We should understand the diversities and ecology of viruses as well as the reasons for their emergence. Therefore, multinational experts launched the Global Virome Project (GVP) in 2018 to identify major viral threats to prevent viral pandemics [5]. Many viruses (including enteroviruses, parvovirus, HIV (human immunodeficiency virus), avian influenza virus) affect the intestinal microbiota after they invade the human body, and they also affect the abundance and diversity of the microbiota. Therefore, research into the relationship between viruses and intestinal microbiota will help us to treat some diseases and lay a foundation for clinical diagnosis and treatment.
Physiological Role of Intestinal Microbiota
The intestinal microbiota plays many physiological roles, which can induce normal intestinal function and produce nutrients such as vitamin K, vitamin B12, short-chain fatty acids, and essential amino acids needed by the human body. It can also resist pathogens (the physiological function of intestinal microbiota is illustrated in Fig. 1). Sun et al. found that the bacterial microbiota produces sodium deoxycholate (DCA, a secondary bile acid) and can reduce campylobacter (C) jejuni-induced colitis [6]. Intestinal microbiota-derived metabolites or direct regulation of host immunity and metabolism were reported to profoundly affect tumourigenesis [7]. NOD2 that is a member of the NLR family can alleviate intestinal inflammation by regulating intestinal microbiota [8] and enhancing neutrophil infiltration and alveolar macrophage response to Escherichia coli pneumonia through the TLR4 pathway killing activity [9]. Clinical experiments indicate that hepatic damage in viral hepatitis can be enhanced by improving the intestinal microbiota [10]. In addition, intestinal microbiota can regulate the storage of host fat [11] and facilitate the digestion of dietary fibre to acquire more energy [12]. Bacterial dysbiosis is also associated with a variety of diseases. Intestinal microbiota interactions affect immune development, abnormal intestinal microbiota in preterm infants, or increase the risk of necrotizing enterocolitis (NEC) [13], and intestinal microbiota also increases the rate of thrombosis and atherosclerosis formation through the trimethylamine N-oxide (TMAO) [14, 15], which affects cardiovascular and cerebrovascular diseases. Bian et al. found that the addition of saccharin to drinking water for a period of 6 months led to the aggravation of liver inflammation in mice, which may be owing to saccharin-induced intestinal microbiome damage inducing changes in host inflammation-related bacterial pathways and metabolites [16]. A further study implies that the intestinal microbiota also affects allergic diseases and asthma [17].
Fig. 1.
Physiological function of intestinal microbiota. The maintenance of normal physiological function of intestinal microbiota needs coordination in many aspects. The variety and heredity of animals, dietary factors, the use of antibiotics, stress, and changes in surrounding environment may affect the intestinal microbiota of the body
The Interaction Between Virus Infection and Intestinal Microbiota
The Effect of Virus Infection on Intestinal Microbiota
Many bacteria are present in the intestinal tracts of animals and they play an essential role in health and disease; bacteria that play a positive role in the health of the body are called beneficial bacteria. When subject to viral infection, the number of beneficial bacteria is reduced and the number of harmful bacteria is increased in the intestine [18]. When the microbiota is out of balance, both exogenous and symbiotic microorganisms may invade the organism. For example, amongst the HIV-related microbiota, the phylum Firmicutes exhibits the highest transcription activity. The expression of anti-inflammatory pathway, including short-chain fatty acid biosynthesis and indole production, is decreased. These microbiota maintain an inflammatory environment [19]. Wang et al. found that, after respiratory influenza viral infection, intestinal microbiota disorders occur. The proportion of enterobacteria will increase significantly, whilst the proportion of segmented filamentous bacteria and lactic acid bacteria will decrease significantly, which is mediated by IFN-γ produced by lung-derived CCR9 + CD4 + T cells collected in the small intestine by ccl25 and ccl9. [20]. Segmented filamentous bacteria are an important probiotic in intestinal microbiota, which cannot be cultured in vitro. Studies have shown that it can drive autoimmune arthritis by regulating T-helper 17 cells [21]. Transmissible gastroenteritis virus (TGEV) is an important pathogen that causes transmissible gastroenteritis in pigs. It belongs to the family of coronaviruses and can cause severe diarrhoea, vomiting, and dehydration in pigs. The mortality rate amongst piglets less than 2 weeks old is 100% [22]. A study on TGEV through real-time quantitative PCR for quantitatively detecting bacteria in pigs with transmissible gastroenteritis found that TGEV caused the number of Lactobacillus to decrease and the increased number of Enterobacteriaceae may cause secondary infection [23]. Akin to TGEV, rotavirus is also a virus that causes enteritis, it has been demonstrated that rotavirus infection causes a decrease in Lactobacillus and an increase in Escherichia and Streptococcus in calves [24]. H9N2 avian influenza virus is one of the subtypes of the avian influenza virus. Although its pathogenicity is not as strong as other subtypes, a recent study indicates that it will affect the intestinal microbiota in the ileum of chickens and cause a significant increase in the content of E. coli in the ileum, which caused high mortality amongst infected chickens [25].
In another study, the faeces of 20 hospitalized children with severe or complex acute viral gastroenteritis (AGE) and 20 healthy children were sequenced with 16S rRNA. It was found that complicated AGE patients contained more Campylobacteriaceae, Neisseria family, Methylobacteriaceae, Sphingomonas family, and Enterobacteriaceae than the normal control group [26]. Campylobacter is one of the main sources of bacterial diarrhoea. Neisseria meningitidis and Neisseria gonorrhoeae in Neisseria family are important pathogens of epidemic meningitis and gonorrhoea, which cannot be ignored.
Apart from directly causing intestinal microbiota disorder, viruses can also produce intestinal microbiota disorder through other organs, of which brain-gut axis is the most well-known. Evidence has proved that microbiota plays a key role in brain function regulation [27]. Regulating intestinal microbiota by taking probiotic Lactobacillus rhamnosus IMC 501 can affect zebra fish behaviour and brain-derived neurotrophic factor and 5-hydroxytryptamine metabolism levels [28]. A study showed that, when Theiler’s murine encephalomyelitis virus was inoculated intracranially in mice, the numbers of Alloprevotella (Bacteroidetes), Akkermansia (Verrucomicrobia), and Anaerotruncus (Firmicutes) decreased at 14 dpi, whilst Clostridium XIVa (Firmicutes) increased at 28 dpi [29]. This result not only indicates that the brain affected by viruses will lead to bacterial imbalance but also reflects the fact that the intestinal microbiota varies constantly in each phase of the disease.
Effect of Intestinal Microbiota on Viruses
Intestinal Microbiota Resists Viral Infection
In a study by Andrew Gewirtz’s team at Georgia State University, segmented filamentous bacteria (SFB) in microbiota can resist the rotavirus (RV). Its resistance does not rely on immune factors, such as natural lymphocytes, interferons, IL-17, and IL-22. Instead, it resists RV infection by promoting the proliferation, migration, and shedding of intestinal epithelial cells [30]. Respiratory syncytial virus (RSV) is an RNA virus that can cause viral pneumonia in children. A study has shown that a high-fibre diet can create acetic acid in intestinal microbiota of mice. Acetic acid can directly inhibit the virus, induce IFN-β production in lungs, and activate the type 1 IFN signalling pathway. IFN-1 receptor (IFNAR) mediates the resistance of acetic acid to RSV infection [31]. Norovirus can cause diarrhoea. Studies by Lee et al. found that the administration of Vitamin A to mice inoculated with norovirus caused an increase of intestinal lactobacilli. Additionally, in the RAW264.7 cell line, lactobacilli played an antiviral role by up-regulating IFN–β [32].
Although intestinal microbiota can resist viral invasion in many ways, if the intestinal microbiota is destroyed by external forces during treatment, it will result in severe consequences. Some studies have shown that if antibiotics are only used to treat viral diseases and the intestinal microbiota is out of control, the symptoms of viral diseases may be aggravated [33]. Even maternal antibiotic treatment during pregnancy has an impact on intestinal microbiota colonization in infants and young children, with reduced resistance to certain viruses. The establishment of intestinal microbiota is relevant to the transmission of maternal and infant microbiota. Studies have shown that maternal and infant microbiota transmission can promote the establishment and development of infant intestinal microbiota. Maternal strains are more adaptable in the infant intestine than other strains [34], and the intestinal microbiota is also associated with the immune response in the body. Mouse models are used to assess the effect of gastrointestinal microbiota disorder on CD8 + T cell-mediated antiviral immunity. Maternal antibiotic treatment (MAT) administered to pregnant and lactating mice induced changes to the intestinal microbiota in females and pups. Mortality of MAT pups increased after injecting vaccinia virus. In addition, CD8 + T cells of uninfected MAT pups decreased the ability to produce IFN-γ after in vitro activation [35], that is, CD8 + T cell-mediated immunity was associated with intestinal microbiota. The intestinal epithelium in neonatal mice expresses Fc receptor (FcRn), which transports IgG in breast milk from intestinal lumen to blood via FcRn [36], thus producing immune effects: the results show that intestinal microbiota disorder can weaken the antiviral capacity. Another similar study showed that if antivirals, probiotics, and antibiotics were combined to treat H7N9 virus, the microbial diversity and abundance of beneficial bacteria in the intestine of H7N9 patients could be improved [37].
Intestinal Microbiota Promotes Viral Infection
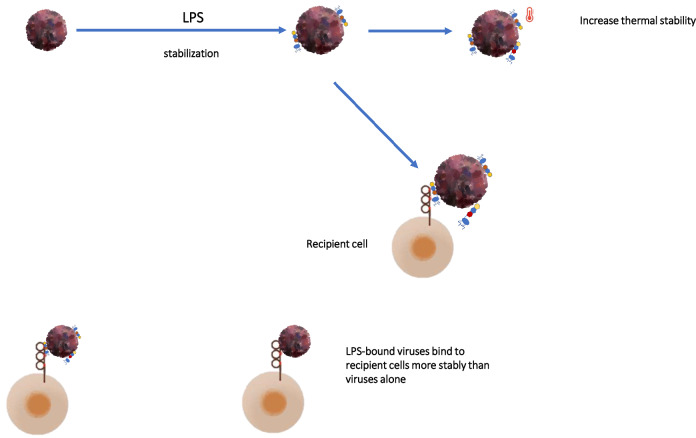
In fact, the relationship between the intestinal microbiota and viral infections has always been a focus amongst researchers. In various discoveries, the presence of intestinal microbiota is a boost to a virus trying to invade the body. Uchiyama et al. found that intestinal microbiota can promote rotavirus infection, which can be alleviated by antibiotic treatment [38]. Jones et al. firstly found that commensal bacteria were responsible for enhancing acute norovirus infection [39]. Wilen et al. further elaborated the principle that both the immune and the intestinal microbiota can promote norovirus infection, and it spreads through cluster cells. Type 2 immune response cytokines represented by the immune factor IL-4 can lead to the proliferation of cluster cells and increase the probability of norovirus infection [40]. Previous research has established that bile acids (BAs) are essential for GII.3 human norovirus replication and are associated with BA hydrophobicity [41]. Studies found that the rate of curing of patients was improved when the mice were given antibiotics to reduce the number of intestinal microbiota before being vaccinated with polio virus. This result indicated that pre-use of antibiotics to reduce intestinal bacteria reduced the rate of infection in mice receiving oral reovirus [42]. In another related study, bacteria isolated from the caecal contents of mice were cultured and combined with poliovirus: a variety of bacteria can be combined, amongst them, Lactobacillus johnsonii has the highest degree of binding. Bacteria can also mediate the recombination of two or more viruses and improve their defects to promote the infection of the body [43] (the interaction between intestinal microbiota and virus is shown in Fig. 2 and Table 1); however, studies have also shown that LPS on the surface of bacteria, when combined with poliovirus, will increase the stability of the virus [44]. Coincidentally, LPS can also enhance the heat stability of a reovirus and increase its ability to infect cells [45] (LPS enhancement of virus infectivity is shown in Fig. 3).
Fig. 2.
The interaction between virus and intestinal microbiota. The promoting mechanisms include: 1. enhance the infectivity of virus (stabilize the structure of virus and increase the differentiation of target cells); 2. destroy the immune system of the body and weaken the defence against virus. The antagonistic mechanisms include: 1. bacteria and their metabolites directly fight viruses; 2. bacteria and their metabolites eliminate viruses by mobilizing the body’s immune system
Table1.
The relationship between virus infection and gut microbiome
| Virus | Intestinal microbiota changes caused by infection | Interaction mechanism |
|---|---|---|
| PV | Not reported | ➀ LPS or peptidoglycan can enhance virus activity [43] |
| ➁ LPS can enhance the binding ability of viruses and cell surface receptors [44] | ||
| ➂ LPS or other polysaccharide components can enhance virus stability [42] | ||
| NV | Lactobacillaceae populations were significantly decreased [32] | ➀ Type 2 cytokines can induce tuft cell proliferation and promote MNoV infection in vivo [40] |
| α-diversity was increased [47] | ➁ HBGA can bind to viral capsid protein and enhance its ability to infect cells [39] | |
| ➂ Bile acid can change the structure of intestinal flora and regulate viral regionalization [48] | ||
| RV | Lactobacillus species reduced from the ileum; Bacteroides and Akkermansia were increased [49] | Segmented filamentous bacteria (SFB) can directly reduce the rotavirus infectivity and accelerate the renewal of infected epithelial cells to help mice resist viral infections [30] |
| TEGV | Lactobacillus was reduced. Enterobacteriaceae was enriched | Epithelial–mesenchymal transition enhances the adhesion of the secondary pathogen ETEC K88 [50] |
| HIV | Lactobacillus were significantly lower. E. coli, E. faecalis, and E. faecium were much higher [51] | ➀ Primarily mediated indirectly through increased expression of CCR5 on LP CD4 T cells without concomitant large scale T cell activation [52] |
| α-Diversity was decreased [53] | ➁ Loss of immune cells and gut microbiota dysbiosis contribute to structural damage to the GI tract and systemic translocation of GI tract microbial products [54] | |
| RSV | S24_7, Clostridiales, Odoribacteraceae, Lactobacillaceae, and Actinomyces were increased. Severe α-diversity was decreased [55] | ➀ Intestinal microbiota significantly stimulated IL-17 production from intestinal epithelial cells, which subsequently promoted Th17 cell polarization reduced intestinal injury [20] |
| ➁ Acetic acid can activate IFN-β by regulating GPR43 and interferon receptor to exert antiviral activity [31] |
Fig. 3.
LPS enhances virus infectivity. LPS, as a component of bacteria, can enhance the thermal stability of the virus, enhance the adhesion between the virus and the receptor cells, and enhance the infectivity of the virus. It is an important part in the process of viral invasion of the body
Dengue virus is a virus transmitted by Aedes aegypti. The symbiotic microorganism in the mosquito gut is closely related to the replication of dengue virus. Some experiments have shown that Serratia marcescens, one of the symbiotic bacteria in mosquitoes, promotes the infection of arbovirus through a secretory protein called SmEnhancin, which can digest the membrane-binding mucin on mosquito intestinal epithelial cells, thus enhancing the transmission ability of the virus and making mosquitoes more susceptible to dengue virus infection [46].
Antiviral Effects of Probiotics
At present, the research on the antiviral effect of probiotics is still in the developmental stage, and most of the antiviral effects of probiotics are lactobacilli and bifidobacterial related [56]. Wang et al. found that B. subtilis OKB105 and its surfactin can inhibit one animal coronavirus, TGEV, entering the intestinal porcine epithelial cell line (IPEC-J2) [57]. Similarly, the exopolysaccharide of Lactobacillus delbrueckii OLL1073R-1 (LDR-1) can regulate the innate antiviral immune response of pig intestinal epithelial cells [58]. Other studies have shown that, in addition to the antiviral activities of probiotics, some foods that enhance the energy sources of probiotics can be used in combination with probiotics, and the combined antiviral effect will be better. For example, by feeding rice bran + probiotics to germ-free swine, a variety of metabolites of the two can improve intestinal barrier function, regulate the immune response, and prevent diarrhoea caused by rotavirus [59]. The combination of drugs exerts a synergistic effect, and the combination of the two probiotics will have a similar effect. In a clinical trial, 57 children with rotavirus diarrhoea were selected and given oral probiotic Bifidobacterium longum BORI and Lactobacillus acidophilus AD031 or placebo + standard diarrhoea treatment. The results showed that the duration of illness in children in the probiotic group was significantly shorter than that in the control group. It indicates that the two probiotics exert a certain inhibitory effect on rotavirus [60].
In addition, probiotics were cultured in cell-free spent medium (CFSM), and different species of lactobacilli had different inhibitory effects on viruses. If exposed to CFSM of Bifidobacterium bifidum JCM 1254, Lactobacillus plantarum 6 ATCC 14917, and Lactobacillus rhamnosus DSM 20021, the percentages of viral titre reduction were 98.3, 98.5, and 97.6%, respectively, and B. longum 20219 resulted in a 96.3% reduction in Newcastle disease virus (NDV) titre. Compared with chicken infectious bursal disease virus (IBDV), probiotic strains have much higher inhibitory effect on NDV [56].
Other research showed that the previously mentioned Enterococcus faecium also plays a protective role against transmissible gastroenteritis virus (TGEV) in pigs. When probiotics are added to cells along with the virus during infection, at the highest concentration of E. faecium, protective effect can reach 100% (competition assay) [61]. In other words, although bacteria are harmful to the organism under conditions of intestinal disorder, they will compete with exotic pathogens if pathogens are emerging; therefore, it is critical to maintain the stability of intestinal microbiota in organisms for the control of certain diseases.
Current Treatment of Viral Infection from the Perspective of Bacteria (Probiotics)
Many studies have shown that probiotics and their metabolites can reduce the risk of viral infection and bacteria also antagonize viruses to interfere with homeostasis in the host. At present, there are several ways in which bacteria fight viral infections:
1. Bacteria (probiotics) directly antagonize viruses through evolutionary mechanisms [62–67]; after long evolution, bacteria also produce the immune mechanism CRISPR/Cas system for viruses [68], and CRISPR is essentially a protective mechanism for bacteria. The CRISPR/Cas system is an acquired immune system found in most bacteria and most archaea.
2. Bacteria (probiotics) and their metabolites antagonize viruses by immune means. Other studies have claimed that the new peptide P18 produced by Bacillus subtilis has anti-influenza virus effect both in vitro and in vivo. The protective effect of P18 on mice was observed at concentrations ranging from 12.5 to 100 ug/ml, which is comparable to that of Oseltamivir phosphate (Tamiflu) [69].
The methods of treating viral diseases from the perspective of bacteria (probiotics) are summarized as follows:
1. Faecal bacteria transplantation, as a newly emerging treatment method, also has a certain effect on viral diseases. Studies have shown that antiviral protection can be transmitted to immunodeficient mice by faecal bacterial transplantation [70]. Besides, clinical trials show that faecal bacterial transplantation for dogs infected with Canine parvovirus (CPV) can shorten the course of disease with no adverse effects detected [71].
2. Taking probiotics such as L. gasseri SBT2055 is efficacious in protecting mice infected with influenza A/PR8 virus [72]. In a study by Inatomi on epidemic diarrhoea in pigs, researchers divided sows from farms where PEDV was present in the environment into two groups, one group taking probiotic preparations and the other group taking control. Both groups were accompanied by vaccine injection. The results showed that the contents of IgA, IgG, and PED-specific antibodies in the colostrum of sows taking probiotics were significantly increased, that is to say, new-born piglets could acquire more maternal antibodies from the colostrum, which had stronger effect on the disease [73].
3. The intestinal microbiota, as the symbiotic microbiota of the body, is also closely related to the body’s daily diet, and different diets will also have different effects on the intestinal microbiota. Fermentable carbohydrates in a high-fibre diet have a positive effect on the intestinal barrier, whereas Western-style diets have a negative impact on the intestinal barrier [74]. The intestinal barrier is also an important line of defence for the body to resist pathogens and an important part of the intestinal barrier. Hence, it is believed that a normal and active diet will help to avoid viral infection by way of the intestinal microbiota.
Gene Engineering Technology
Some studies have shown that transforming plasmids that contain specific genes into the intestinal symbiont Snodgrassella alvi of bees can regulate the expression of certain genes in the host. As a result, intestinal symbionts with specific targeting plasmids can reduce the infection of residual wing virus [75].
Probiotics have been included in several controlled clinical trials in patients with infectious diseases for prevention of viral diarrhoea (Table 2).
Table 2.
Clinical efficacy of probiotics on infectious diseases
| Strain | Target Disease (Virus) | Individuality | Result | Refs |
|---|---|---|---|---|
| Enterococcus faecalis strain FK-23 | HCV | Anti-HCV-positive adults | AST and ALT were detected | [76] |
| Lactobacillus plantarum 299v | HIV | HIV-infected child | Enhance immune response | [77] |
| Lactobacillus casei Shirota | Cytomegalovirus Epstein–Barr | Healthy athletes | Reduced plasma CMV and EBV antibody titres | [78] |
| HIV | HIV-infected child | CD4 + T cells increase; induced decreases in plasma HIV load and CD8 + T- ell activation | [79] | |
| Norovirus | Elderly people | No significant difference in infection rate | [80] | |
| Lactobacillus rhamnosus GG | Rhinovirus | Preterm infant | Reduce the risk of rhinovirus infections | [81] |
| Rotavirus and Cryptosporidium | 6 M-5Y children with rotavirus and cryptosporidial gastroenteritis | Decrease repeated episodes of rotavirus diarrhoea; improvement in intestinal function in children with rotavirus and cryptosporidial gastroenteritis | [82] | |
| Enterococcus faecium SF68 | Cats latent feline herpesvirus 1 | FHV1-infected cats | Reduce incidence rate | [83] |
| Lactobacillus paracasei Strain ST11 | Non-rotavirus | Infant with diarrhoea | Ineffective in those with rotavirus diarrhoea | [84] |
| Lactobacillus pentosus strain b240 | Common cold | Elderly adults | Reduced the incidence rate of the common cold | [85] |
| Clostridium butyricum and B. infantis | Minimal hepatic encephalopathy (MHE) in patients with hepatitis B virus (HBV)-induced liver cirrhosis | HBV-induced liver cirrhosis patients | Reduction in venous ammonia; the parameters of the intestinal mucosal barrier were obviously improved | [86] |
| Bifidobacterium Lactis Bb12 | Rotavirus and poliovirus | Six-week-old healthy, full-term infants | Anti-rotavirus- and anti-poliovirus-specific IgA increased | [87] |
| Bifidobacterium | Acute viral diarrhoea (rotavirus) | Children(3 months and 3 years) | Reduce diarrhoea and promote viral shedding | [88] |
| Saccharomyces boulardii | Acute rotavirus diarrhoea | Children (3 months–5 years) | The duration of diarrhoea was significantly shorter | [89] |
HCV hepatitis C virus, AST aspartate aminotransferase, ALT alanine aminotransferase, HIV human immunodeficiency virus, CMV cytomegalovirus, EBV epstein–barr virus, FHV1 feline herpesvirus 1, MHE minimal hepatic encephalopathy, HBV hepatitis B virus
Effect of Intestinal Microbiota Composition on Immunogenicity of Rotavirus Vaccine
The relationship between the intestinal microbiota and the immunogenicity of rotavirus vaccines has also been analysed [90, 91]. Michael et al. found that after inoculating attenuated human rotavirus vaccine, the number of total IgM immunoglobulin-secreting cells in intestinal tissues and the total IgG immunoglobulin-secreting cells in blood was significantly higher in germ-free pigs transplanted with human infant faecal microbiota [92]. Twitchell et al. found that the levels of rotavirus-specific immunoglobulins such as IgG and IgA in small intestinal contents and IgA in large intestinal contents were higher in the intestine of Gn pigs colonized with healthy human intestinal microbiota [93]. A study in Pakistan showed that the immunogenic strength of rotavirus vaccine was positively correlated with the ratio of Gram-negative to Gram-positive bacteria in the intestinal microbiota of the subjects, particularly the abundance of Serratia and E. coli [94]. However, the relationship amongst intestinal flora, rotavirus, and host genetic background is not clear and needs further study.
Summary
As an important member of the intestinal barrier of the organism, the complexity and diversity of the intestinal microbiota are different from other organs. Its essential particularity as an important component of the organs also causes it to become a hub associated with other systemic organ diseases. Similar situations may occur in the environment that is similar to the intestine in the body, such as the oral cavity and respiratory tract. The study thereof may help us to deepen our understanding of symbiotic microorganisms and understand the relationship between the intestinal microbiota and viruses in the body. It may provide a powerful tool for the treatment of viral infections in the future. The intestinal microbiome also contains Archaea and Virome: we are far from reaching a perfect understanding of the intestinal microbiota. At present, the research into intestinal microbiota in faecal bacteria transplantation and the brain-gut axis is flourishing, and the relationship between tumours and feed toxins has gradually attracted attention amongst researchers. In clinical aspects, scholars around the world have also linked the intestinal microbiota to a variety of diseases, but some studies exaggerate the role of probiotics. In response to the related hyperbole, we need to pay attention to the fact that the relationship between viruses and intestinal microbiota remains in its exploratory stage. In particular, in 2020–2021, the Covid-19 epidemic has received worldwide attention, and we need to continue studying the relationship between the good microbiota, probiotics, and viruses. In recent years, there has been more research into the antiviral effect of probiotics and the interaction of probiotics; however, the specific immune mechanism remains to be clarified, and the study thereof could offer a theoretical basis for clinical trials, which is of potential medical value.
Author Contributions
Z.L wrote the paper; D.X. and J. S. revised the paper; M.L. and Z.C reviewed and edited the paper.
Funding
This work was financially supported by the National Natural Science Foundation of China (Grant Nos. 31772809; 31872538); This work was also supported by National Key Research and Development Program Projects of China (2017YFD0500305, 2017YFD0500901), the National Key Program for Infectious Disease of China (2018ZX10101002-002), the State Key Program of National Natural Science of China (U1808202), NSFC International (Regional) Cooperation and Exchange program (31961143024), and Major science and technology projects of Inner Mongolia of China.
Declarations
Conflict of interest
The authors declare no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zhiming Lv, Email: 2019240364@stu.syau.edu.cn.
Dongwei Xiong, Email: 2019220557@stu.syau.edu.cn.
Jichao Shi, Email: sjc6319@126.com.
Miao Long, Email: longmiao@syau.edu.cn.
Zeliang Chen, Email: chzl@syau.edu.cn.
References
- 1.Sekirov I, Russell SL, Antunes LC, Finlay BB. Gut microbiota in health and disease. Physiol Rev. 2010;90(3):859–904. doi: 10.1152/physrev.00045.2009. [DOI] [PubMed] [Google Scholar]
- 2.Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci U S A. 2007;104(34):13780–13785. doi: 10.1073/pnas.0706625104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clemente JC, Ursell LK, Parfrey LW, Knight R. The impact of the gut microbiota on human health: an integrative view. Cell. 2012;148(6):1258–1270. doi: 10.1016/j.cell.2012.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pitlik SD, Koren O. How holobionts get sick-toward a unifying scheme of disease. Microbiome. 2017;5(1):64. doi: 10.1186/s40168-017-0281-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carroll D, Daszak P, Wolfe ND, Gao GF, Morel CM, Morzaria S, Pablos-Mendez A, Tomori O, Mazet JAK. The global virome project. Science. 2018;359(6378):872–874. doi: 10.1126/science.aap7463. [DOI] [PubMed] [Google Scholar]
- 6.Sun X, Winglee K, Gharaibeh RZ, Gauthier J, He Z, Tripathi P, Avram D, Bruner S, Fodor A, Jobin C. Microbiota-derived metabolic factors reduce campylobacteriosis in mice. Gastroenterology. 2018;154(6):1751–1763 e1752. doi: 10.1053/j.gastro.2018.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang Z, Tang H, Chen P, Xie H, Tao Y. Demystifying the manipulation of host immunity, metabolism, and extraintestinal tumors by the gut microbiome. Signal Transduct Target Ther. 2019;4:41. doi: 10.1038/s41392-019-0074-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Biswas A, Petnicki-Ocwieja T, Kobayashi KS. Nod2: a key regulator linking microbiota to intestinal mucosal immunity. J Mol Med (Berl) 2012;90(1):15–24. doi: 10.1007/s00109-011-0802-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsay TB, Yang MC, Chen PH, Hsu CM, Chen LW. Gut flora enhance bacterial clearance in lung through toll-like receptors 4. J Biomed Sci. 2011;18:68. doi: 10.1186/1423-0127-18-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu D, Huang Y, Wang J. Gut microbiota modulate the immune effect against hepatitis B virus infection. Eur J Clin Microbiol Infect Dis. 2015;34(11):2139–2147. doi: 10.1007/s10096-015-2464-0. [DOI] [PubMed] [Google Scholar]
- 11.Tsai F, Coyle WJ. The microbiome and obesity: is obesity linked to our gut flora? Curr Gastroenterol Rep. 2009;11(4):307–313. doi: 10.1007/s11894-009-0045-z. [DOI] [PubMed] [Google Scholar]
- 12.Gerritsen J, Smidt H, Rijkers GT, de Vos WM. Intestinal microbiota in human health and disease: the impact of probiotics. Genes Nutr. 2011;6(3):209–240. doi: 10.1007/s12263-011-0229-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dessi A, Pintus R, Marras S, Cesare Marincola F, De Magistris A, Fanos V. Metabolomics in necrotizing enterocolitis: the state of the art. Expert Rev Mol Diagn. 2016;16(10):1053–1058. doi: 10.1080/14737159.2016.1211933. [DOI] [PubMed] [Google Scholar]
- 14.Zhu W, Gregory JC, Org E, Buffa JA, Gupta N, Wang Z, Li L, Fu X, Wu Y, Mehrabian M, Sartor RB, McIntyre TM, Silverstein RL, Tang WHW, DiDonato JA, Brown JM, Lusis AJ, Hazen SL. Gut microbial metabolite TMAO enhances platelet hyperreactivity and thrombosis risk. Cell. 2016;165(1):111–124. doi: 10.1016/j.cell.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Z, Roberts AB, Buffa JA, Levison BS, Zhu W, Org E, Gu X, Huang Y, Zamanian-Daryoush M, Culley MK, DiDonato AJ, Fu X, Hazen JE, Krajcik D, DiDonato JA, Lusis AJ, Hazen SL. Non-lethal inhibition of gut microbial trimethylamine production for the treatment of atherosclerosis. Cell. 2015;163(7):1585–1595. doi: 10.1016/j.cell.2015.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bian X, Tu P, Chi L, Gao B, Ru H, Lu K. Saccharin induced liver inflammation in mice by altering the gut microbiota and its metabolic functions. Food Chem Toxicol. 2017;107(Pt B):530–539. doi: 10.1016/j.fct.2017.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bjorksten B. Effects of intestinal microflora and the environment on the development of asthma and allergy. Springer Semin Immunopathol. 2004;25(3–4):257–270. doi: 10.1007/s00281-003-0142-2. [DOI] [PubMed] [Google Scholar]
- 18.Wen W, Qi Z, Wang J. The function and mechanism of enterovirus 71 (EV71) 3C protease. Curr Microbiol. 2020;77(9):1968–1975. doi: 10.1007/s00284-020-02082-4. [DOI] [PubMed] [Google Scholar]
- 19.Vazquez-Castellanos JF, Serrano-Villar S, Jimenez-Hernandez N, Soto Del Rio MD, Gayo S, Rojo D, Ferrer M, Barbas C, Moreno S, Estrada V, Rattei T, Latorre A, Moya A, Gosalbes MJ. Interplay between gut microbiota metabolism and inflammation in HIV infection. ISME J. 2018;12(8):1964–1976. doi: 10.1038/s41396-018-0151-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang J, Li F, Wei H, Lian ZX, Sun R, Tian Z. Respiratory influenza virus infection induces intestinal immune injury via microbiota-mediated Th17 cell-dependent inflammation. J Exp Med. 2014;211(12):2397–2410. doi: 10.1084/jem.20140625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu HJ, Ivanov II, Darce J, Hattori K, Shima T, Umesaki Y, Littman DR, Benoist C, Mathis D. Gut-residing segmented filamentous bacteria drive autoimmune arthritis via T helper 17 cells. Immunity. 2010;32(6):815–827. doi: 10.1016/j.immuni.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Laude H, Rasschaert D, Delmas B, Godet M, Gelfi J, Charley B. Molecular biology of transmissible gastroenteritis virus. Vet Microbiol. 1990;23(1–4):147–154. doi: 10.1016/0378-1135(90)90144-k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xia L, Yang Y, Wang J, Jing Y, Yang Q. Impact of TGEV infection on the pig small intestine. Virol J. 2018;15(1):102. doi: 10.1186/s12985-018-1012-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jang JY, Kim S, Kwon MS, Lee J, Yu DH, Song RH, Choi HJ, Park J. Rotavirus-mediated alteration of gut microbiota and its correlation with physiological characteristics in neonatal calves. J Microbiol. 2019;57(2):113–121. doi: 10.1007/s12275-019-8549-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li H, Liu X, Chen F, Zuo K, Wu C, Yan Y, Chen W, Lin W, Xie Q. Avian influenza virus subtype H9N2 affects intestinal microbiota, barrier structure injury, and inflammatory intestinal disease in the chicken ileum. Viruses. 2018 doi: 10.3390/v10050270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen SY, Tsai CN, Lee YS, Lin CY, Huang KY, Chao HC, Lai MW, Chiu CH. Intestinal microbiome in children with severe and complicated acute viral gastroenteritis. Sci Rep. 2017;7:46130. doi: 10.1038/srep46130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sandhu KV, Sherwin E, Schellekens H, Stanton C, Dinan TG, Cryan JF. Feeding the microbiota-gut-brain axis: diet, microbiome, and neuropsychiatry. Transl Res. 2017;179:223–244. doi: 10.1016/j.trsl.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 28.Borrelli L, Aceto S, Agnisola C, De Paolo S, Dipineto L, Stilling RM, Dinan TG, Cryan JF, Menna LF, Fioretti A. Probiotic modulation of the microbiota-gut-brain axis and behaviour in zebrafish. Sci Rep. 2016;6:30046. doi: 10.1038/srep30046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carrillo-Salinas FJ, Mestre L, Mecha M, Feliu A, Del Campo R, Villarrubia N, Espejo C, Montalban X, Alvarez-Cermeno JC, Villar LM, Guaza C. Gut dysbiosis and neuroimmune responses to brain infection with Theiler's murine encephalomyelitis virus. Sci Rep. 2017;7:44377. doi: 10.1038/srep44377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shi Z, Zou J, Zhang Z, Zhao X, Noriega J, Zhang B, Zhao C, Ingle H, Bittinger K, Mattei LM, Pruijssers AJ, Plemper RK, Nice TJ, Baldridge MT, Dermody TS, Chassaing B, Gewirtz AT. Segmented filamentous bacteria prevent and cure rotavirus infection. Cell. 2019;179(3):644–658 e613. doi: 10.1016/j.cell.2019.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Antunes KH, Fachi JL, de Paula R, da Silva EF, Pral LP, Dos Santos AA, Dias GBM, Vargas JE, Puga R, Mayer FQ, Maito F, Zarate-Blades CR, Ajami NJ, Sant'Ana MR, Candreva T, Rodrigues HG, Schmiele M, Silva Clerici MTP, Proenca-Modena JL, Vieira AT, Mackay CR, Mansur D, Caballero MT, Marzec J, Li J, Wang X, Bell D, Polack FP, Kleeberger SR, Stein RT, Vinolo MAR, de Souza APD. Microbiota-derived acetate protects against respiratory syncytial virus infection through a GPR43-type 1 interferon response. Nat Commun. 2019;10(1):3273. doi: 10.1038/s41467-019-11152-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee H, Ko G. Antiviral effect of vitamin A on norovirus infection via modulation of the gut microbiome. Sci Rep. 2016;6:25835. doi: 10.1038/srep25835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thackray LB, Handley SA, Gorman MJ, Poddar S, Bagadia P, Briseno CG, Theisen DJ, Tan Q, Hykes BL, Jr, Lin H, Lucas TM, Desai C, Gordon JI, Murphy KM, Virgin HW, Diamond MS. Oral antibiotic treatment of mice exacerbates the disease severity of multiple flavivirus infections. Cell Rep. 2018;22(13):3440–3453 e3446. doi: 10.1016/j.celrep.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.York A. Delivery of the gut microbiome. Nat Rev Microbiol. 2018;16(9):520–521. doi: 10.1038/s41579-018-0059-3. [DOI] [PubMed] [Google Scholar]
- 35.Gonzalez-Perez G, Hicks AL, Tekieli TM, Radens CM, Williams BL, Lamouse-Smith ES. Maternal antibiotic treatment impacts development of the neonatal intestinal microbiome and antiviral immunity. J Immunol. 2016;196(9):3768–3779. doi: 10.4049/jimmunol.1502322. [DOI] [PubMed] [Google Scholar]
- 36.Zheng W, Zhao W, Wu M, Song X, Caro F, Sun X, Gazzaniga F, Stefanetti G, Oh S, Mekalanos JJ, Kasper DL. Microbiota-targeted maternal antibodies protect neonates from enteric infection. Nature. 2020;577(7791):543–548. doi: 10.1038/s41586-019-1898-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qin N, Zheng B, Yao J, Guo L, Zuo J, Wu L, Zhou J, Liu L, Guo J, Ni S, Li A, Zhu Y, Liang W, Xiao Y, Ehrlich SD, Li L. Influence of H7N9 virus infection and associated treatment on human gut microbiota. Sci Rep. 2015;5:14771. doi: 10.1038/srep14771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Uchiyama R, Chassaing B, Zhang B, Gewirtz AT. Antibiotic treatment suppresses rotavirus infection and enhances specific humoral immunity. J Infect Dis. 2014;210(2):171–182. doi: 10.1093/infdis/jiu037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jones MK, Watanabe M, Zhu S, Graves CL, Keyes LR, Grau KR, Gonzalez-Hernandez MB, Iovine NM, Wobus CE, Vinje J, Tibbetts SA, Wallet SM, Karst SM. Enteric bacteria promote human and mouse norovirus infection of B cells. Science. 2014;346(6210):755–759. doi: 10.1126/science.1257147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilen CB, Lee S, Hsieh LL, Orchard RC, Desai C, Hykes BL, Jr, McAllaster MR, Balce DR, Feehley T, Brestoff JR, Hickey CA, Yokoyama CC, Wang YT, MacDuff DA, Kreamalmayer D, Howitt MR, Neil JA, Cadwell K, Allen PM, Handley SA, van Lookeren CM, Baldridge MT, Virgin HW. Tropism for tuft cells determines immune promotion of norovirus pathogenesis. Science. 2018;360(6385):204–208. doi: 10.1126/science.aar3799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Murakami K, Tenge VR, Karandikar UC, Lin SC, Ramani S, Ettayebi K, Crawford SE, Zeng XL, Neill FH, Ayyar BV, Katayama K, Graham DY, Bieberich E, Atmar RL, Estes MK. Bile acids and ceramide overcome the entry restriction for GII.3 human norovirus replication in human intestinal enteroids. Proc Natl Acad Sci U S A. 2020;117(3):1700–1710. doi: 10.1073/pnas.1910138117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kuss SK, Best GT, Etheredge CA, Pruijssers AJ, Frierson JM, Hooper LV, Dermody TS, Pfeiffer JK. Intestinal microbiota promote enteric virus replication and systemic pathogenesis. Science. 2011;334(6053):249–252. doi: 10.1126/science.1211057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Erickson AK, Jesudhasan PR, Mayer MJ, Narbad A, Winter SE, Pfeiffer JK. Bacteria facilitate enteric virus co-infection of mammalian cells and promote genetic recombination. Cell Host & Microbe. 2018;23(1):77–8875. doi: 10.1016/j.chom.2017.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robinson CM, Jesudhasan PR, Pfeiffer JK. Bacterial lipopolysaccharide binding enhances virion stability and promotes environmental fitness of an enteric virus. Cell Host & Microbe. 2014;15(1):36–46. doi: 10.1016/j.chom.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Berger AK, Yi H, Kearns DB, Mainou BA. Bacteria and bacterial envelope components enhance mammalian reovirus thermostability. PLoS Pathog. 2017;13(12):e1006768. doi: 10.1371/journal.ppat.1006768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu P, Sun P, Nie K, Zhu Y, Shi M, Xiao C, Liu H, Liu Q, Zhao T, Chen X, Zhou H, Wang P, Cheng G. A gut commensal bacterium promotes mosquito permissiveness to arboviruses. Cell Host & Microbe. 2019;25(1):101–11105. doi: 10.1016/j.chom.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 47.Pearson JA, Tai N, Ekanayake-Alper DK, Peng J, Hu Y, Hager K, Compton S, Wong FS, Smith PC, Wen L. Norovirus changes susceptibility to type 1 diabetes by altering intestinal microbiota and immune cell functions. Front Immunol. 2019;10:2654. doi: 10.3389/fimmu.2019.02654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grau KR, Zhu S, Peterson ST, Helm EW, Philip D, Phillips M, Hernandez A, Turula H, Frasse P, Graziano VR, Wilen CB, Wobus CE, Baldridge MT, Karst SM. The intestinal regionalization of acute norovirus infection is regulated by the microbiota via bile acid-mediated priming of type III interferon. Nat Microbiol. 2020;5(1):84–92. doi: 10.1038/s41564-019-0602-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Engevik MA, Banks LD, Engevik KA, Chang-Graham AL, Perry JL, Hutchinson DS, Ajami NJ, Petrosino JF, Hyser JM. Rotavirus infection induces glycan availability to promote ileum-specific changes in the microbiome aiding rotavirus virulence. Gut Microbes. 2020;11(5):1324–1347. doi: 10.1080/19490976.2020.1754714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xia L, Dai L, Yu Q, Yang Q. Persistent transmissible gastroenteritis virus infection enhances enterotoxigenic Escherichia coli K88 adhesion by promoting epithelial-mesenchymal transition in intestinal epithelial cells. J Virol. 2017 doi: 10.1128/JVI.01256-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lu J, Ma SS, Zhang WY, Duan JP. Changes in peripheral blood inflammatory factors (TNF-alpha and IL-6) and intestinal flora in AIDS and HIV-positive individuals. J Zhejiang Univ Sci B. 2019;20(10):793–802. doi: 10.1631/jzus.B1900075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dillon SM, Lee EJ, Donovan AM, Guo K, Harper MS, Frank DN, McCarter MD, Santiago ML, Wilson CC. Enhancement of HIV-1 infection and intestinal CD4+ T cell depletion ex vivo by gut microbes altered during chronic HIV-1 infection. Retrovirology. 2016;13:5. doi: 10.1186/s12977-016-0237-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tuddenham SA, Koay WLA, Zhao N, White JR, Ghanem KG, Sears CL, Consortium HIVMR-a The impact of human immunodeficiency virus infection on gut microbiota alpha-diversity: an individual-level meta-analysis. Clin Infect Dis. 2020;70(4):615–627. doi: 10.1093/cid/ciz258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mudd JC, Brenchley JM. Gut mucosal barrier dysfunction, microbial dysbiosis, and their role in HIV-1 disease progression. J Infect Dis. 2016;214(Suppl 2):S58–66. doi: 10.1093/infdis/jiw258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Harding JN, Siefker D, Vu L, You D, DeVincenzo J, Pierre JF, Cormier SA. Altered gut microbiota in infants is associated with respiratory syncytial virus disease severity. BMC Microbiol. 2020;20(1):140. doi: 10.1186/s12866-020-01816-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Abdelhamid AG, El-Masry SS, El-Dougdoug NK. Probiotic lactobacillus and bifidobacterium strains possess safety characteristics, antiviral activities and host adherence factors revealed by genome mining. EPMA J. 2019;10(4):337–350. doi: 10.1007/s13167-019-00184-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang X, Hu W, Zhu L, Yang Q. 2017. Bacillus subtilis and surfactin inhibit the transmissible gastroenteritis virus from entering the intestinal epithelial cells. Biosci Rep. [DOI] [PMC free article] [PubMed]
- 58.Kanmani P, Albarracin L, Kobayashi H, Iida H, Komatsu R, Humayun Kober AKM, Ikeda-Ohtsubo W, Suda Y, Aso H, Makino S, Kano H, Saito T, Villena J, Kitazawa H. Exopolysaccharides from lactobacillus delbrueckii OLL1073R-1 modulate innate antiviral immune response in porcine intestinal epithelial cells. Mol Immunol. 2018;93:253–265. doi: 10.1016/j.molimm.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 59.Nealon NJ, Yuan L, Yang X, Ryan EP. Rice bran and probiotics alter the porcine large intestine and serum metabolomes for protection against human rotavirus diarrhea. Front Microbiol. 2017;8:653. doi: 10.3389/fmicb.2017.00653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Park MS, Kwon B, Ku S, Ji GE. The efficacy of Bifidobacterium longum BORI and Lactobacillus acidophilus AD031 probiotic treatment in infants with rotavirus infection. Nutrients. 2017 doi: 10.3390/nu9080887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chai W, Burwinkel M, Wang Z, Palissa C, Esch B, Twardziok S, Rieger J, Wrede P, Schmidt MF. Antiviral effects of a probiotic Enterococcus faecium strain against transmissible gastroenteritis coronavirus. Arch Virol. 2013;158(4):799–807. doi: 10.1007/s00705-012-1543-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kumar R, Seo BJ, Mun MR, Kim CJ, Lee I, Kim H, Park YH. Putative probiotic Lactobacillus spp. from porcine gastrointestinal tract inhibit transmissible gastroenteritis coronavirus and enteric bacterial pathogens. Trop Anim Health Prod. 2010;42(8):1855–1860. doi: 10.1007/s11250-010-9648-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Alqazlan N, Alizadeh M, Boodhoo N, Taha-Abdelaziz K, Nagy E, Bridle B, Sharif S. Probiotic lactobacilli limit avian influenza virus subtype H9N2 replication in chicken cecal tonsil mononuclear cells. Vaccines (Basel) 2020 doi: 10.3390/vaccines8040605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ermolenko EI, Desheva YA, Kolobov AA, Kotyleva MP, Sychev IA, Suvorov AN. Anti-influenza activity of enterocin B in vitro and protective effect of bacteriocinogenic enterococcal probiotic strain on influenza infection in mouse model. Probiotics Antimicrob Proteins. 2019;11(2):705–712. doi: 10.1007/s12602-018-9457-0. [DOI] [PubMed] [Google Scholar]
- 65.Eguchi K, Fujitani N, Nakagawa H, Miyazaki T. Prevention of respiratory syncytial virus infection with probiotic lactic acid bacterium Lactobacillus gasseri SBT2055. Sci Rep. 2019;9(1):4812. doi: 10.1038/s41598-019-39602-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Waiyamitra P, Zoral MA, Saengtienchai A, Luengnaruemitchai A, Decamp O, Gorgoglione B, Surachetpong W. Probiotics modulate tilapia resistance and immune response against tilapia lake virus infection. Pathogens. 2020 doi: 10.3390/pathogens9110919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cantu-Bernal S, Dominguez-Gamez M, Medina-Peraza I, Aros-Uzarraga E, Ontiveros N, Flores-Mendoza L, Gomez-Flores R, Tamez-Guerra P, Gonzalez-Ochoa G. Enhanced viability and anti-rotavirus effect of Bifidobacterium longum and Lactobacillus plantarum in combination with Chlorella sorokiniana in a dairy product. Front Microbiol. 2020;11:875. doi: 10.3389/fmicb.2020.00875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Barrangou R, Horvath P. A decade of discovery: CRISPR functions and applications. Nat Microbiol. 2017;2:17092. doi: 10.1038/nmicrobiol.2017.92. [DOI] [PubMed] [Google Scholar]
- 69.Starosila D, Rybalko S, Varbanetz L, Ivanskaya N, Sorokulova I. Anti-influenza activity of a Bacillus subtilis probiotic strain. Antimicrob Agents Chemother. 2017 doi: 10.1128/AAC.00539-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ingle H, Lee S, Ai T, Orvedahl A, Rodgers R, Zhao G, Sullender M, Peterson ST, Locke M, Liu TC, Yokoyama CC, Sharp B, Schultz-Cherry S, Miner JJ, Baldridge MT. Viral complementation of immunodeficiency confers protection against enteric pathogens via interferon-lambda. Nat Microbiol. 2019;4(7):1120–1128. doi: 10.1038/s41564-019-0416-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pereira GQ, Gomes LA, Santos IS, Alfieri AF, Weese JS, Costa MC. Fecal microbiota transplantation in puppies with canine parvovirus infection. J Vet Intern Med. 2018;32(2):707–711. doi: 10.1111/jvim.15072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nakayama Y, Moriya T, Sakai F, Ikeda N, Shiozaki T, Hosoya T, Nakagawa H, Miyazaki T. Oral administration of Lactobacillus gasseri SBT2055 is effective for preventing influenza in mice. Sci Rep. 2014;4:4638. doi: 10.1038/srep04638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Inatomi T, Amatatsu M, Romero-Perez GA, Inoue R, Tsukahara T. Dietary probiotic compound improves reproductive performance of porcine epidemic diarrhea virus-infected sows reared in a Japanese commercial swine farm under vaccine control condition. Front Immunol. 2017;8:1877. doi: 10.3389/fimmu.2017.01877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Reimer RA. Establishing the role of diet in the microbiota-disease axis. Nat Rev Gastroenterol Hepatol. 2019;16(2):86–87. doi: 10.1038/s41575-018-0093-7. [DOI] [PubMed] [Google Scholar]
- 75.Leonard SP, Powell JE, Perutka J, Geng P, Heckmann LC, Horak RD, Davies BW, Ellington AD, Barrick JE, Moran NA. Engineered symbionts activate honey bee immunity and limit pathogens. Science. 2020;367(6477):573–576. doi: 10.1126/science.aax9039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Oo KM, Lwin AA, Kyaw YY, Tun WM, Fukada K, Goshima A, Shimada T, Okada S. Safety and long-term effect of the probiotic FK-23 in patients with hepatitis C virus infection. Biosci Microbiota Food Health. 2016;35(3):123–128. doi: 10.12938/bmfh.2015-024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cunningham-Rundles S, Ahrne S, Bengmark S, Johann-Liang R, Marshall F, Metakis L, Califano C, Dunn AM, Grassey C, Hinds G, Cervia J. Probiotics and immune response. Am J Gastroenterol. 2000;95(1 Suppl):S22–25. doi: 10.1016/s0002-9270(99)00813-8. [DOI] [PubMed] [Google Scholar]
- 78.Gleeson M, Bishop NC, Struszczak L. Effects of Lactobacillus casei Shirota ingestion on common cold infection and herpes virus antibodies in endurance athletes: a placebo-controlled, randomized trial. Eur J Appl Physiol. 2016;116(8):1555–1563. doi: 10.1007/s00421-016-3415-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ishizaki A, Bi X, Nguyen LV, Matsuda K, Pham HV, Phan CTT, Khu DTK, Ichimura H. Effects of short-term probiotic ingestion on immune profiles and microbial translocation among HIV-1-infected Vietnamese children. Int J Mol Sci. 2017 doi: 10.3390/ijms18102185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nagata S, Asahara T, Ohta T, Yamada T, Kondo S, Bian L, Wang C, Yamashiro Y, Nomoto K. Effect of the continuous intake of probiotic-fermented milk containing Lactobacillus casei strain Shirota on fever in a mass outbreak of norovirus gastroenteritis and the faecal microflora in a health service facility for the aged. Br J Nutr. 2011;106(4):549–556. doi: 10.1017/S000711451100064X. [DOI] [PubMed] [Google Scholar]
- 81.Luoto R, Ruuskanen O, Waris M, Kalliomaki M, Salminen S, Isolauri E. Prebiotic and probiotic supplementation prevents rhinovirus infections in preterm infants: a randomized, placebo-controlled trial. J Allergy Clin Immunol. 2014;133(2):405–413. doi: 10.1016/j.jaci.2013.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sindhu KN, Sowmyanarayanan TV, Paul A, Babji S, Ajjampur SS, Priyadarshini S, Sarkar R, Balasubramanian KA, Wanke CA, Ward HD, Kang G. Immune response and intestinal permeability in children with acute gastroenteritis treated with Lactobacillus rhamnosus GG: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis. 2014;58(8):1107–1115. doi: 10.1093/cid/ciu065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lappin MR, Veir JK, Satyaraj E, Czarnecki-Maulden G. Pilot study to evaluate the effect of oral supplementation of Enterococcus faecium SF68 on cats with latent feline herpesvirus 1. J Feline Med Surg. 2009;11(8):650–654. doi: 10.1016/j.jfms.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sarker SA, Sultana S, Fuchs GJ, Alam NH, Azim T, Brussow H, Hammarstrom L. Lactobacillus paracasei strain ST11 has no effect on rotavirus but ameliorates the outcome of nonrotavirus diarrhea in children from Bangladesh. Pediatrics. 2005;116(2):e221–228. doi: 10.1542/peds.2004-2334. [DOI] [PubMed] [Google Scholar]
- 85.Shinkai S, Toba M, Saito T, Sato I, Tsubouchi M, Taira K, Kakumoto K, Inamatsu T, Yoshida H, Fujiwara Y, Fukaya T, Matsumoto T, Tateda K, Yamaguchi K, Kohda N, Kohno S. Immunoprotective effects of oral intake of heat-killed Lactobacillus pentosus strain b240 in elderly adults: a randomised, double-blind, placebo-controlled trial. Br J Nutr. 2013;109(10):1856–1865. doi: 10.1017/S0007114512003753. [DOI] [PubMed] [Google Scholar]
- 86.Xia X, Chen J, Xia J, Wang B, Liu H, Yang L, Wang Y, Ling Z. Role of probiotics in the treatment of minimal hepatic encephalopathy in patients with HBV-induced liver cirrhosis. J Int Med Res. 2018;46(9):3596–3604. doi: 10.1177/0300060518776064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Holscher HD, Czerkies LA, Cekola P, Litov R, Benbow M, Santema S, Alexander DD, Perez V, Sun S, Saavedra JM, Tappenden KA. Bifidobacterium lactis Bb12 enhances intestinal antibody response in formula-fed infants: a randomized, double-blind, controlled trial. J Parenter Enteral Nutr. 2012;36(1 Suppl):106S–117S. doi: 10.1177/0148607111430817. [DOI] [PubMed] [Google Scholar]
- 88.Narayanappa D. Randomized double blinded controlled trial to evaluate the efficacy and safety of bifilac in patients with acute viral diarrhea. Indian J Pediatr. 2008;75(7):709–713. doi: 10.1007/s12098-008-0134-2. [DOI] [PubMed] [Google Scholar]
- 89.Das S, Gupta PK, Das RR. Efficacy and safety of Saccharomyces boulardii in acute rotavirus diarrhea: double blind randomized controlled trial from a developing country. J Trop Pediatr. 2016;62(6):464–470. doi: 10.1093/tropej/fmw032. [DOI] [PubMed] [Google Scholar]
- 90.Magwira CA, Taylor MB. Composition of gut microbiota and its influence on the immunogenicity of oral rotavirus vaccines. Vaccine. 2018;36(24):3427–3433. doi: 10.1016/j.vaccine.2018.04.091. [DOI] [PubMed] [Google Scholar]
- 91.Harris VC, Armah G, Fuentes S, Korpela KE, Parashar U, Victor JC, Tate J, de Weerth C, Giaquinto C, Wiersinga WJ, Lewis KD, de Vos WM. Significant correlation between the infant gut microbiome and rotavirus vaccine response in Rural Ghana. J Infect Dis. 2017;215(1):34–41. doi: 10.1093/infdis/jiw518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Michael H, Langel SN, Miyazaki A, Paim FC, Chepngeno J, Alhamo MA, Fischer DD, Srivastava V, Kathayat D, Deblais L, Rajashekara G, Saif LJ, Vlasova AN. Malnutrition decreases antibody secreting cell numbers induced by an oral attenuated human rotavirus vaccine in a human infant fecal microbiota transplanted gnotobiotic pig model. Front Immunol. 2020;11:196. doi: 10.3389/fimmu.2020.00196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Twitchell EL, Tin C, Wen K, Zhang H, Becker-Dreps S, Azcarate-Peril MA, Vilchez S, Li G, Ramesh A, Weiss M, Lei S, Bui T, Yang X, Schultz-Cherry S, Yuan L. Modeling human enteric dysbiosis and rotavirus immunity in gnotobiotic pigs. Gut Pathog. 2016;8:51. doi: 10.1186/s13099-016-0136-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Harris V, Ali A, Fuentes S, Korpela K, Kazi M, Tate J, Parashar U, Wiersinga WJ, Giaquinto C, de Weerth C, de Vos WM. Rotavirus vaccine response correlates with the infant gut microbiota composition in Pakistan. Gut Microbes. 2018;9(2):93–101. doi: 10.1080/19490976.2017.1376162. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Wang X, Hu W, Zhu L, Yang Q. 2017. Bacillus subtilis and surfactin inhibit the transmissible gastroenteritis virus from entering the intestinal epithelial cells. Biosci Rep. [DOI] [PMC free article] [PubMed]