Abstract
Background
As the population ages, the incidence of ventral hernias in older adults is increasing. Ventral hernia repairs (VHR) should not be considered low risk operations, particularly in older adults who are disproportionately affected by multiple age-related factors that can complicate surgery and adversely affect outcomes. Although age-related risk factors have been well established in other surgical fields, there is currently little data describing their impact on VHR.
Methods
We performed a systematic review of the literature to identify studies that examine the effects of age-related risk factors on VHR outcomes. This was conducted using Cochrane Library, Embase, PubMed (Medline), and Google Scholar databases, all updated through June 2020. We selected relevant studies using the keywords, multimorbidity, comorbidities, polypharmacy, functional dependence, functional status, frailty, cognitive impairment, dementia, sarcopenia, and malnutrition. Primary outcomes include mortality and overall complications following VHR.
Results
We summarize the evidence basis for the significance of age-related risk factors in elective surgery and discuss how these factors increase the risk of adverse outcomes following VHR. In particular, we explore the impact of the following risk factors: multimorbidity, polypharmacy, functional dependence, frailty, cognitive impairment, sarcopenia, and malnutrition. As opposed to chronological age itself, age-related risk factors are more clinically relevant in determining VHR outcomes.
Conclusions
Given the increasing complexity of VHR, addressing age-related risk factors pre-operatively has the potential to improve surgical outcomes in older adults. Preoperative risk assessment and individualized prehabilitation programs aimed at improving patient-centered outcomes may be particularly useful in this population.
Keywords: Geriatric Syndromes, Ventral Hernia, Age, Frailty, Polypharmacy, Functional Status
Introduction
Ventral incisional hernias are extremely common and occur following 11%−50% of all laparotomies.1,2 It is also estimated that 5% of the United States population will develop either a primary epigastric or umbilical hernia.3 Further, ventral hernia incidence is likely to increase in the future.4 Concurrently, VHRs are becoming more intricate and surgeons are utilizing increasingly complex techniques for abdominal wall reconstruction.2 Ventral hernias are associated with significant pain, risk of intestinal obstruction, strangulation, and the small, but real possibility of requiring an urgent repair.1,5 Although VHRs are common operations performed by general surgeons and hernia specialists alike, they should not be considered low risk and are associated with significant morbidity and mortality.1,5
The increasing complexity and prevalence of VHRs is complicated by the fact that a growing number of these patients will be over the age of 65 years. Older adults are at increased risk of developing ventral hernias.1,6–9 Impaired tissue repair mechanisms and weak anterior abdominal walls in older adults contribute to their enhanced susceptibility for ventral hernias.1,6–8 Furthermore, comorbidities frequently experienced by older adults, including chronic pulmonary disease, benign prostatic hypertrophy, constipation, and ascites, result in increased intrabdominal pressure, which can increase the risk of wound dehiscence and incisional hernias by increasing the strain on wound edges and displacing the sutures in the post-operative period.1,6–9
Furthermore, the population is aging, and a large proportion of adults are older than 65 years. The 2010 United States Census estimates that adults at least 65 years old will more than double by 2050, reaching 89 million people.10 Due both to these demographic changes and surgical advances, there is an increasing number of older patients undergoing both elective and emergency surgery.1,11 Despite the benefits of surgery in this population, there is an increased rate of adverse postoperative complications.1,11,12 Older individuals present not only with pathology requiring operative intervention, but also with a number of age-related risk factors and morbidities.11–13 These age-related risk factors, often termed geriatric syndromes, have been utilized and explored in the existing literature and include multimorbidity, polypharamacy, functional status, frailty, cognitive status, sarcopenia, and nutritional status.12,13 As opposed to the term, “geriatric syndromes,” “age-related risk factors” highlights the imperfect relationship between these risk factors and age. Age-related risk factors are not present in every older (“geriatric”) patient and may affect individuals under 65 years old. However, these risk factors are strongly associated with aging and may predict mortality and morbidity following VHR.12–17 Further, age-related risk factors are better predictors of postoperative outcomes than chronological age.3,6,7,14 Given the aging demographic, age-related risk factors will likely become increasingly important in the VHR field.
The susceptibility to develop ventral hernias, combined with an aging demographic, is producing a growing demand for VHRs in older adults.14 Therefore, there is a critical need to define the unique risk factors for older patients presenting with ventral hernias and to target interventions that could improve outcomes. Currently, there is a paucity of literature on this topic and, to our knowledge, this is the first review to address surgical outcomes in older patients undergoing VHR. The goals of this review are two-fold. First, we introduce age-related risk factors and review the present literature for their use in the context of VHRs. Secondly, we proceed by outlining these age-related risk factors’ potential significance in clinical practice. As opposed to chronological age, age-related risk factors are more clinically relevant due to their modifiability and ability to predict VHR outcomes. As such, these risk factors may be used to guide preoperative surgeon-patient consultations and as a stepping-stone to create hernia specific prehabilitation in older adults. By exposing the gaps in the current literature, we suggest future directions to improve the surgical treatment of older patients with ventral hernias.
Methods
Literature Search Strategy
The Preferred Reporting Items for Systemic Reviews and Meta-Analyses (PRISMA) guidelines were followed in conducting this systemic review.18 Figure 1 summarized the literature search strategy using the PRISMA flow diagram template. We performed a systematic literature search in Cochrane Library, PubMed (Medline), Embase, and Google Scholar databases, all updated through June 2020. We searched for relevant studies using the following keywords related to age-related risk factors: multimorbidity, comorbidities, polypharmacy, functional dependence, functional status, frailty, cognitive impairment, dementia, sarcopenia, and malnutrition. Using the Boolean operator “AND,” we combined each of the aforementioned keywords with the phrases, ventral hernia, abdominal wall hernia, incisional hernia, or umbilical hernia. Additionally, we screened the reference list of all the retrieved articles and relevant reviews for any related studies that were not identified during the initial search.
Figure 1.
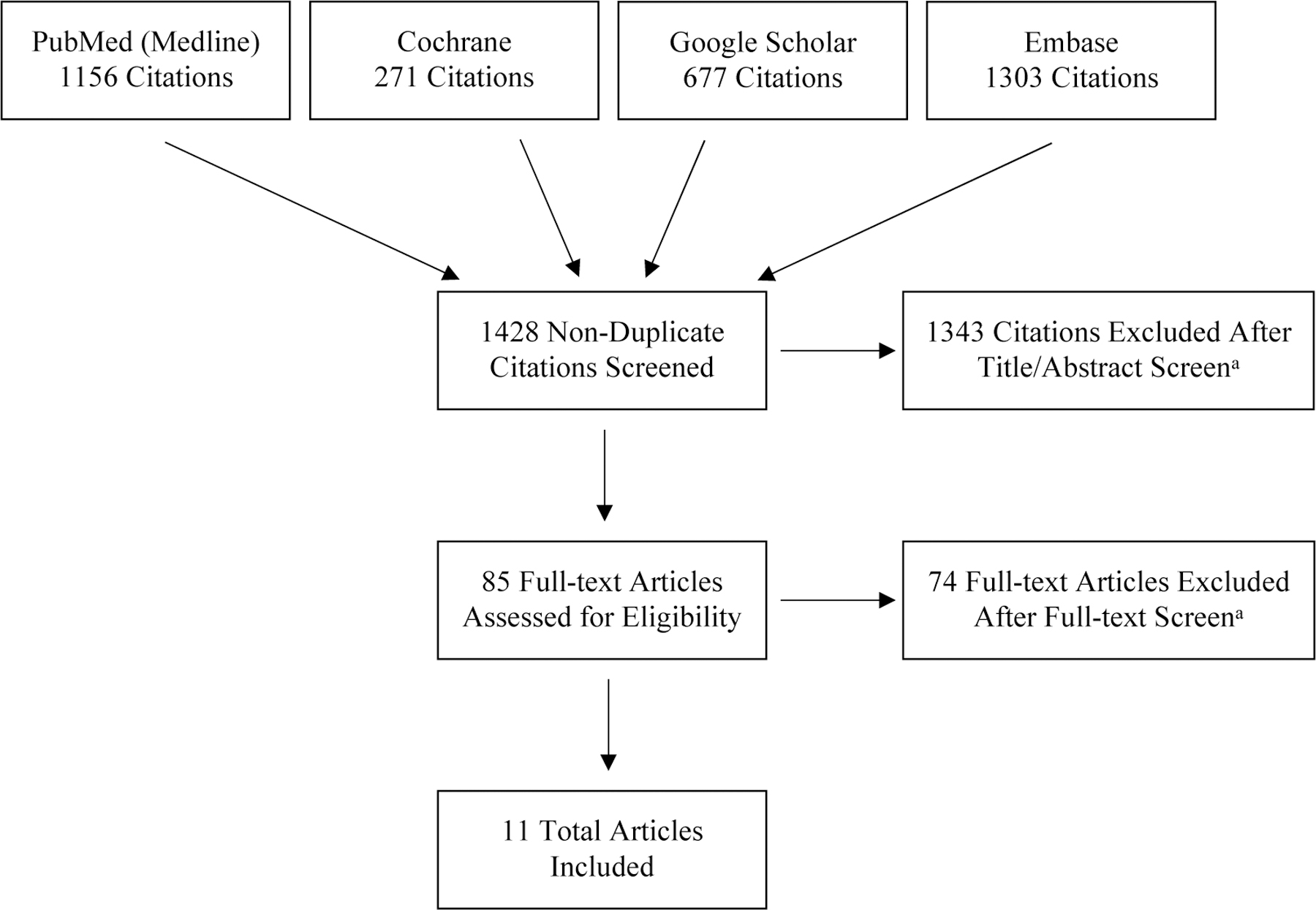
PRISMA Literature Selection Flow Diagram
Notes: a) We included only randomized controlled trials, cohort studies, and case control studies that were published in a peer-review journal, written in English, and involved human subjects. Included articles also contained at least one age-related risk factor as an independent variable.
Study Selection
We included randomized controlled trials, cohort studies, and case control studies exploring VHR outcomes of age-related risk factors. We limited our search to studies that were published in a peer-review journal, written in English, and involved human subjects. Selected studies included at least one age-related risk factor as an independent variable (Figure 1). Primary outcomes of interest included mortality and overall complications (both often within 30 days of VHR). Additional reported outcomes include discharge disposition, surgical site occurrence (SSO), surgical site infection (SSI), hernia recurrence, need for additional operation(s), need for emergency surgery, hospital readmission, duration of ileus, and length of hospital stay. We identified potentially relevant articles by first reviewing by their titles and abstracts. Afterwards, we performed a full-text review of selected articles.
Age-Related Risk Factors for Ventral Hernia Repair Adverse Outcomes
Multimorbidity
Aging is typically accompanied by the accumulation of various biological deficits, many of which can ultimately manifest as disease.19 Multimorbidity, or the diagnosis of multiple chronic medical problems, is often operationalized using scoring systems such as APACHE-II, Charlson Comorbidity Index (CCI), or American Society of Anesthesiologists Physical Status Classification System (ASA class).20 For example, one working definition of multimorbidity is CCI greater than or equal to 3.21 Between 55% and 98% of adults over 65 years old present with multimorbidity. In contrast, multimorbidity is present in only 30% of younger adults.19 In light of these statistics and the rapid growth of our aging population, researchers anticipate a worldwide multimorbidity epidemic.11,12,19,22
Multimorbidity is associated with increased length of hospital stay and costs, postoperative complications, postoperative delirium (POD), and functional decline.23,24 Mortality following major elective surgery in older adults is associated with greater CCI.25 Multimorbidity (measured by ASA class) is linked to the development of POD following elective major abdominal surgery.20,26 POD itself is associated with a range of adverse outcomes, including increased mortality, morbidity, length of hospital stay, health care costs, functional dependence, non-home discharge, and reduced quality of life.11,12,24,27,28
Patients with multimorbidity also have poor VHR outcomes, although data is limited (Table 1). Compared to individuals with no comorbidities, patients with multimorbidity (CCI ≥ 3) have greater in-hospital mortality following both elective and emergency VHRs.21 Similarly, multimorbidity (ASA class ≥ 3) also confers a greater risk of mortality within 30 days of open VHR.29 Multimorbid (ASA class ≥ 3) patients also have an increased risk of non-home discharge after complex abdominal wall reconstructions.30 Further, the number of comorbidities that a patient presents with preoperatively tends to increase their risk of non-home discharge. As compared to patients without comorbidity, those with two or more comorbidities are between 4 and 40 times more likely to be discharged to a facility.30 As opposed to those returning home, patients facing discharge to a facility tend to experience a greater number of complications and readmissions.
Table 1.
Primary Sources Investigating the Impact of Age-Related Risk Factors on VHR Outcomes
| Age-Related Risk Factor | Source | Sample Size | Procedure(s)a | Database | Operation-alization of Age-Related Risk Factor | Results | ||
|---|---|---|---|---|---|---|---|---|
| Outcome | OR | 95% CI | ||||||
| Multimorbidity | Wolf et al. 2016 | 92,295 | Inpatient, open & laparoscopic VHRs | 2003–2011 U.S. Nationwide Inpatient Sample | CCI ≥ 3 | Need for emergency VHR | 1.68* | 1.56–1.80 |
| In-hospital mortality | 4.02* | 3.03–5.33 | ||||||
| Basta et al. 2016 | 55,760 | Inpatient, open VHR | 2005–2012 ACS-NSQIP | ASA ≥ 3 | 30-day mortality | 2.63* | 1.94–3.57 | |
| Ayyala et al. 2020 | 4,549 | Complex abdominal wall reconstruction | 2005–2016 ACS-NSQIP | ASA ≥ 3 | Non-home discharge | 1.71* | 1.083–2.708 | |
| 2+ comorbiditiesb | ≥ 3.88* | - | ||||||
| Functional Status | Albright et al. 2012 | 76,397 | All types of VHRs | 2005–2010 ACS-NSQIP | Ability to perform ADLs | PDP: 30-day mortality | 4.48* | 3.20–6.28 |
| TDP: 30-day mortality | 11.55* | 7.58–17.59 | ||||||
| PDP: 30-day operation | 2.11* | 1.70–2.62 | ||||||
| TDP: 30-day operation | 3.01* | 2.13–4.25 | ||||||
| PDP & TDP: Complicationsc | ≥ 1.52* | - | ||||||
| Balla et al. 2019 | 97,905 | Open & laparoscopic VHRs | 2011–2016 ACS-NSQIP | Ability to perform ADLs | Overall complications | 2.97* | 2.88–3.05 | |
| Major complications | 3.51* | 3.43–3.57 | ||||||
| Non-home discharge | 13.43* | 12.42–14.71 | ||||||
| Mortality | NR | NR | ||||||
| Basta et al. 2016 | 55,760 | Inpatient, open VHR | 2005–2012 ACS-NSQIP | Ability to perform ADLs | 30-day mortality | 2.64* | 1.92–3.62 | |
| Ayyala et al. 2020 | 4,549 | Complex abdominal wall reconstruction | 2005–2016 ACS-NSQIP | Ability to perform ADLs | Non-home discharge | 4.448* | 1.742–11.360 | |
| Frailty | Joseph et al. 2020 | 70,339 | Complex abdominal wall reconstruction | 2005–2013 ACS-NSQIP | 11-variable mFI | Overall complications | 7.77* | 5.97–10.13 |
| Major complications | 35.71* | 23.32–54.69 | ||||||
| Surgical site complications | 3.85* | 2.77–5.36 | ||||||
| 30-day mortality | 62.05* | 28.78–133.80 | ||||||
| Readmissions | 1.4 | 0.44–4.49 | ||||||
| Balla et al. 2019 | 97,905 | Open & laparoscopic VHRs | 2011–2016 ACS-NSQIP | 5-variable mFId | Overall complicationsd | ≥ 1.15* | - | |
| Major complicationsd | ≥ 1.21* | - | ||||||
| Non-home discharged | ≥ 1.22* | - | ||||||
| Mortalityd | NR | NR | ||||||
| Sarcopenia | Barnes et al. 2018 | 58 | VHR with component separation | 2009–2013 institutional database | HUAC < 19.6 | Overall complications | 5.31* | 1.121–25.174 |
| Readmissionse | MD: 0.07 | p = .91 | ||||||
| Repeat surgical interventionse | MD: 0.20 | p = .48 | ||||||
| Rinaldi et al. 2016 | 148 | Elective complex VHR | 2011–2013 one surgeon’s database | Males: SMI ≤ 52.4; Females: SMI ≤ 38.5 | Duration of ileuse | MD = 1.25* | p = .0156 | |
| Length of hospital staye | MD = 2.18* | p = .0218 | ||||||
| Recurrencee | MD = 9 | p = 1.0000 | ||||||
| SSOe | MD = 20 | p = .1137 | ||||||
| Siegal et al. 2018 | 135 | All types of VHRs | 2014–2015 two surgeons’ database | Males: SMI ≤ 52.4; Females: SMI ≤ 38.5 | Overall complicationse | MD = 30 | p = .701 | |
| Recurrencee | MD = 17 | p = .895 | ||||||
| SSOe | MD = 31 | p = .113 | ||||||
| SSIe | MD = 22 | p = .140 | ||||||
| Length of hospital staye | MD = 0 | p = .988 | ||||||
| SMI decrease of 10 | Overall complications | 1.44* | 1.00–2.07 | |||||
| Schlosser et al. 2019 | 1,178 | Open VHR | 2007–2018 institutional database | Males: SMI ≤ 54.5; Females: SMI ≤ 38.5 | Major complications | NR | NR | |
| SSO | NR | NR | ||||||
| Recurrence | NR | NR | ||||||
| Readmissions | NR | NR | ||||||
| Reoperation | NR | NR | ||||||
| Nutritional Statusf | Basta et al. 2016 | 55,760 | Inpatient, open VHR | 2005–2012 ACS-NSQIP | 10% weight loss over past 6 months | 30-day mortality | 1.37* | 1.03–1.81 |
| BMI < 19.0 | 30-day mortality | 3.23* | 1.75–5.95 | |||||
| Owei et al. 2017 | 102,191 | Open VHR | 2005–2015 ACS-NSQIP | BMI < 18.5 | Overall complications | 1.26 | 0.93–1.70 | |
| Polypharmacy | No VHR studies to date. | |||||||
| Cognitive Status | No VHR studies to date. | |||||||
Abbreviations: Asterisk signifies significant results (p < .05); Dash (−) signifies that data is not applicable; NR: Not reported; MD: Mean difference; OR: Odds Ratio; 95% CI: 95% Confidence Interval; CCI: Charlson Comorbidity Index; ASA: American Society of Anesthesiologists Physical Status Classification; SSI: surgical site infections; SSO: surgical site occurrence; PDP: partially dependent patients; TDP: totally dependent patients; ADLs: activities of daily living; mFI: modified Frailty Index; HUAC: Hounsfield unit average calculation (HU); SMI: skeletal muscle index (cm2/m2); BMI: body mass index (kg/m2);
Notes:
Unless otherwise noted, studies did not mention filtering VHRs by elective/emergent procedures or by inpatient/outpatient settings.
Patients with 0 comorbidity are separately compared to those with 2, 3, 4, 5, 6, and 7+ comorbidities. All comparisons are significant.
Each complication is considered separately. Partial and total dependence are significantly associated with superficial SSI, wound dehiscence, pneumonia, ventilation > 48 h, UTI, DVT, and sepsis. Acute MI and deep SSI/pulmonary embolism are significantly associated with partial and total dependence, respectively. All other comparisons are nonsignificant.
Authors report statistics for each variable, rather than for total mFI.
MD and p-value are reported, rather than OR and 95% CI, respectively. Student’s t-test, rank-sum test, or chi-square test was used to compare patients with and without sarcopenia.
This table does not include findings on overnutrition, due to the large number of relevant studies.
Multimorbid patients (CCI ≥ 3) are also at increased risk of requiring an emergency VHR relative to patients without comorbidites.21 As compared to elective VHRs, emergency procedures are associated with increased in-hospital mortality, greater cost, and longer hospital stays, even after risk-adjustment.21 However, this study did not report the percentage of multimorbid patients who were offered elective repair. From review, it is unclear whether the increased rates of emergency VHRs represent surgeons’ unwillingness to operate electively on this population or whether there is a fundamental difference in the hernias’ characteristics in this population.
While there is a clear relationship between multimorbidity and negative VHR outcomes, this has not been explored specifically in the older adult population. However, multimorbidity’s connection to both aging and adverse VHR outcomes suggests that multimorbidity is a noteworthy factor to consider when treating older patients with ventral hernias. As such, future research on multimorbidity in the geriatric VHR population would be valuable.
Polypharmacy
Polypharmacy, or the use of multiple medications at the same time, is a growing problem affecting surgeons.31 While there is no consensus on definition, polypharmacy is often operationalized by using a strict numerical threshold (e.g. 5 or more drugs).31,32 The number of total medications increases with age and therefore, presents a unique challenge in treating older adults.33 Polypharmacy affects approximately 39% of adults over the age of 65 in the United States.31 In a recent cohort study of older adults undergoing major non-cardiac elective surgery, polypharmacy was found in 64.8% of patients.34
Polypharmacy has been linked to a host of negative outcomes including drug-drug and drug-disease interactions, lack of adherence, falls, renal failure, frailty, cognitive decline, sarcopenia, hospitalization, mortality, POD, and other adverse postoperative outcomes.20,24,31–34 Polypharmacy is also associated with adverse drug events and the prescription of potentially inappropriate medications (drugs whose potential adverse outcomes outweigh their benefits), which are prevalent in surgical populations.34,35 In patients undergoing either elective or emergency general surgery, the number of preoperative medications unrelated to the operation are associated with an almost threefold increased risk of developing postoperative complications.36 In patients older than 65 years undergoing their first elective non-cardiac surgery, polypharmacy (5 or more drugs) conferred an increased risk of in-hospital complications, 90-day mortality, non-home discharge, 30-day readmission, and use of hospital resources.32
While these results are compelling, prospective studies are needed to confirm a causal relationship between polypharmacy and poor surgical outcomes, and to disentangle multimorbidity as a potential confounder.31,32 To date, polypharmacy has not been studied in the context of VHRs and therefore demands future research (Table 1).
Functional Status
Functional status is often defined based on an individual’s ability to independently perform activities of daily living (ADL; e.g. dressing, bathing, feeding). The individual is deemed functionally independent if they require no assistance from another person to perform ADLs. If they require another person’s assistance with either some or all ADLs, they are deemed partially or totally dependent, respectively.12,25,37 Functional dependence is linked to adverse outcomes in a number of surgical settings.12,25,38 As compared to a functionally independent cohort with matched patient and procedure-related variables, functionally dependent patients are more likely to die after major elective surgery.38 Similarly, among individuals at least 65 years old, functional dependence is linked to mortality after elective surgery.25 In adults over 80 years old, functional dependence increased the risk of dying after non-cardiac surgery by three-fold.12
In the VHR population, in particular, functional dependence is linked to negative surgical outcomes (Table 1). This was most directly shown by a retrospective analysis of 76,397 patients undergoing all types of VHRs. As compared to their independent peers, both partially dependent and totally dependent patients showed an increased risk of complications and need for additional operation(s) and death within 30 days of VHR.37 This held true even after adjusting for age, wound class, operative complexity, and ASA class. Within 30 days of surgery, partially and totally dependent patients were about four and twelve times more likely to die than independent patients, respectively.37 Additionally, partially or totally dependent patients are at increased risk of overall morbidity (Clavien-Dindo Grade 1 or higher (CD1+)), major morbidity (CD3+), and non-home discharge following all-types of VHRs.39 Functional status is the strongest indicator of these adverse outcomes, as compared to four other predictors including history of diabetes, hypertension, congestive heart failure, and COPD/pneumonia. In order to accentuate the importance of functional status, the authors highlight the fact that non-home discharge is greater for functionally dependent patients who lack comorbidities, as compared to independent patients with hypertension, diabetes, and COPD.39 In another study, mortality within 30 days of open VHRs was nearly three times more likely for partially or totally dependent patients, as compared to those who were independent.29 Finally, functionally dependent patients are nearly 4.5 times more likely than their independent peers to be discharged to a facility after complex abdominal wall reconstruction.30 This holds true even after controlling for patients’ number of comorbidities.
Functionally dependent patients have unique risk factors that adversely affect outcomes after elective VHR.22 In one study sample, of those functionally dependent patients who are over the age of 70, 6.1% died within 30 days of surgery.22 Within this functionally dependent sample, increasing age, ascites, renal failure, and pulmonary compromise (COPD, pneumonia, and/or ventilation) were associated with increased 30-day mortality.22 These results imply that functionally dependent patients require unique considerations for VHR. Functionally dependent patients would benefit from a two-way shared decision-making process with their surgeon highlighting the risks and benefits of surgery versus non-operative management. In this particularly challenging patient population, it is paramount to weigh the risks of surgery with the expected postoperative functional level and potential quality of life improvement.
Frailty
Approximately half of all patients presenting for elective cardiac and non-cardiac surgery are frail.15 While there is some disagreement about the exact definition of frailty, it is broadly defined as diminished physiological reserve in multiple organ systems resulting in an increased vulnerability to adverse outcomes.12,15,16 Generally, there are two major approaches to diagnosing frailty.15,40 First, a frailty phenotype may exist, based solely on physiological factors, such as stamina and strength. Alternatively, frailty may be defined more broadly, considering physiological and social factors, comorbidities and measures of disabilities. The latter definition is referred to as an accumulation of deficits and is often operationalized through the use of a frailty index, which accounts for these wide-ranging factors.40 Based off of these two approaches, numerous ways of calculating frailty have been established‒many of which involve studying patients’ comorbidities, functional status, mobility, cognition, nutrition, sarcopenia, and more.12,15,16,39 However, frailty is distinct from both age and disease. Although frailty shares characteristics with the other risk factors discussed in this review, it is a separate entity that warrants its own consideration.
Frailty is associated with increased mortality, morbidity, length of hospital stay, and non-home discharge in a variety of surgical settings.13,15 A recent meta-analysis including 56 studies and over one million patients concluded that frailty is strongly associated with non-home discharge, mortality, complications, and POD following non-cardiac surgery.41 Further, frailty increases the risk of mortality both within 30 days and one year of non-cardiac surgery by three-fold.41
The very limited data exploring frailty in the VHR population is consistent with these findings in the broader surgical population (Table 1).39,42 In a retrospective analysis of 70,339 patients undergoing complex abdominal wall reconstruction, patients with complications are significantly frailer (defined by an 11-variable modified Frailty Index (mFI)) than those without.42 The same study showed that frailty is associated with an enhanced risk of surgical site complications, overall morbidity, major complications (CD4), and 30-day mortality. Most dramatically, high mFI increased the likelihood of life-threatening complications and death by 35 and 62 times, respectively.42 Likewise, in a recent study of 97,905 patients, frailty (defined by a 5-variable mFI) is associated with overall complications (CD1+), major complications (CD3+), and non-home discharge following all types of VHRs.39 Based on the currently available literature, frailty is associated with adverse postoperative VHR outcomes and must be considered when evaluating a patient preoperatively.
Cognitive Status
Dementia is broadly defined as cognitive impairment that adversely affects functional independence. Cognitive decline in the absence of functional impairment is defined as mild cognitive impairment. Patients can be screened for cognitive impairment through validated cognitive screening tools such as the Mini-Cog or Montreal Cognitive Assessment (MoCA), although dementia remains largely a clinical diagnosis.12,27 It is estimated that approximately half of older patients greater than 65 years old undergoing elective surgery have some degree of cognitive impairment.28,42 Patients’ cognitive status can impact various aspects of their care. Most assuredly, a patient’s ability to make an informed decision is of paramount importance throughout the preoperative counseling process, particularly in the case of elective surgeries such as VHRs. Additionally, preoperative cognitive impairment is associated with increased mortality, postoperative complications, and non-home discharge in the general surgical population.12,27,43 Among the complications associated with cognitive impairment is postoperative cognitive dysfunction and POD, which are in and of themselves risk factors for additional adverse outcomes. Moreover, cognitive status is related to adverse postoperative complications beyond neurological complications. Patients with impaired sensorium are more likely to experience pneumonia, ventilator dependence, stroke, venous embolism, urinary tract infection, and progressive renal insufficiency following general non-emergent inpatient surgery.27
Despite the high incidence of cognitive impairment in the elective surgery population, we were unable to locate any studies exploring the effects of cognitive impairment in the VHR population (Table 1). However, the implications of cognitive impairment on the pre-operative shared decision-making and consent process, as well as the associations of cognitive impairment with a range of adverse peri- and postoperative outcomes in other types of surgery, highlights the importance of assessing cognition prior to surgery. Filling in this gap in the literature is imperative in order to best treat cognitively impaired individuals with ventral hernias.
Sarcopenia
Sarcopenia is defined as the reduction of lean body mass. It is associated with functional impairment and is thought of as a radiological marker of frailty.44,45 Although multiple definitions are in use, sarcopenia is generally identified based on muscle measurements obtained via image analysis of cross-sectional lumbar CT scans.46 Sarcopenia is characteristic of aging, with a 10% prevalence in the general population over the age of 65 and up to 50% prevalence in patients over 80 years old.17,44,46–48 The prevalence is increased in patients with certain diseases, such as cancer or liver disease.17 Most notably, sarcopenia is present in about a quarter of patients undergoing abdominal wall reconstruction or VHR.17,46,47
Sarcopenia is associated with negative postoperative outcomes in a number of surgical populations and settings.17,46 In numerous studies focusing on abdominal surgery, sarcopenia is linked to higher mortality, morbidity, length of hospital stay, infections, costs, and readmission rates.46 A meta-analysis including 16 studies and almost 5,000 patients concluded that sarcopenia is associated with mortality within 30 days of elective abdominal surgery.49 In regard to VHRs in particular, a recent systematic review described the current gaps in the literature.46 Only four articles met the requirements of the review (Table 1).45,47,50,51 Unlike the other two studies, Barnes et al. and Rinaldi et al. showed that sarcopenia is associated with increased postoperative complications and length of hospital stay, respectively. Despite no significant effects of sarcopenia, Siegal et al. found an association between decreased muscle index and postoperative complications, after adjusting for BMI, critical care status, and diabetes. These studies’ heterogenous results may be explained by the lack of consistency in the methodology and definitions of sarcopenia employed.46 For example, Barnes et al. defines sarcopenia based on a study-specific cutoff value while the remaining studies employ gender-specific cutoffs. The studies’ measurements also differ in which muscles are included and at what level of the lumbar vertebrae they are taken.50 These findings call for further investigation into the sarcopenia’s impact on VHR patients and a standardization in our approach moving forward.46
Nutritional Status
Nutritional status affects outcomes of surgeries, more generally, and VHRs in particular. Nutritional status is relevant in both overnourished and malnourished (undernourished) individuals.52 Historically, nutrition has been assessed by measuring albumin or prealbumin, skin fold thickness, body weight, body mass index (BMI), or muscle strength.12,17,53 More recently, these methods’ accuracy has been questioned and they have been replaced by various screening tools and questionnaires such as Nutritional Risk Screening 2002 or Nutrition Risk in Critically Ill.17,52,53
In the case of older patients, malnutrition is particularly relevant.12,52,54 A 2010 multi-national study found approximately two-thirds of older adults are either at-risk of becoming or are already malnourished. The prevalence of malnourished older patients in the hospital and rehabilitation centers are estimated to be 38.7% and 50.5%, respectively.54 Malnutrition is associated with increased postoperative mortality, length of hospital stay, readmissions, and delayed recovery of bowel function.12,17,53
In the context of VHRs, little is known regarding the relationship between malnutrition and postoperative outcomes. Further, the few studies that exist do not provide a comprehensive report on the subject and fail to utilize the aforementioned screening tools/questionnaires (Table 1). In patients undergoing open VHR, malnutrition (10% weight loss over the last six months) and low BMI (< 19 kg/m2) are significant predictors of 30-day mortality.29 In contrast, a separate study found no connection between low BMI (< 18.5 kg/m2) and complications following open VHR.55
Most evidence exploring nutrition in the VHR population focuses on obese patients, rather than malnutrition (although the two are not mutually exclusive). Increasing BMI is associated with exponentially increased complication rates and surgical site infections (SSI). A retrospective review of the American Hernia Society Quality Collaborative (AHSQC) found a proportional increase for both SSIs and surgical site occurrences requiring operative intervention with increasing BMI.56 Other large data series have shown similar results: Patients with a BMI > 40 kg/m2 have twice the risk for complications.55 Lastly, a recent literature review concluded that obesity is associated with increased hernia incidence and postoperative complications including incarceration and reoperation.57 In the treatment of geriatric VHR patients, it is important to determine how these results would translate to older obese individuals. Additionally, research on the effects of malnutrition in the VHR population is needed to appropriately address the needs of older patients.
Significance and Future Directions
Risk Factors’ Superiority Over Chronological Age
Although age is a risk factor for the aforementioned syndromes, chronological age in and of itself neither predicts VHR outcomes nor can be modified in any way. For the most part, age is unrelated to VHR outcomes and should not be considered a contraindication for surgery.3,6,7,14,58,59 Although laparoscopic VHRs are associated with less morbidity and recurrence than open surgeries, both are considered reasonable options for older patients.6,60 As compared to younger adults, those at least 65 years old have comparable complication rates following laparoscopic and robotic VHRs.7,61 Even 50 months after surgery, there is no difference in the complication rates following laparoscopic VHR in adults at least 55 years old and younger adults.62 Similarly, in patients undergoing component separation procedures, morbidity is unaffected by age.14 Finally, adults at least 65 years old and younger adults undergoing complex abdominal wall hernia repairs with biologic mesh have similar complication and recurrence rates, length of hospital stay, mortality, and discharge dispositions.58 In contrast, one study found that patients at least 80 years old undergoing VHRs (open and laparoscopic) showed higher morbidity and 30-day mortality as compared to younger patients.63 These results may diverge from the others based on its higher age cutoff, implying that octogenarians are at high risk of adverse outcomes due to a greater prevalence of age-related risk factors. However, other researchers have documented appropriately low complications following laparoscopic and robotic VHRs in adults 80 years old or greater.3,59 Although octogenarians may require further investigation, the overall literature implies that age alone is an imperfect indicator of VHR outcomes.3,6,7,14,58,59
Age-related risk factors are more clinically relevant and informative than chronological age alone, and importantly, may be modified to improve patient outcomes. All of the risk factors previously outlined in this review have been identified as potentially modifiable.11,17,46 As a result, age-related risk factors may impact the preoperative period by informing preoperative risk assessment, counseling, and prehabilitation.
Preoperative Risk Assessment and Counseling
Establishing the relationship between age-related risk factors and VHR outcomes is imperative because it allows for the accurate determination of preoperative status. The hope is that, after adequate research, clinicians can use the presence or absence of the age-related risk factors (multimorbidity, polypharmacy, functional dependence, frailty, cognitive impairment, sarcopenia, malnutrition, and obesity) to draft an individualized surgical risk to each patient.12,13 Although these risk factors are associated with adverse outcomes, they are largely ignored in traditional preoperative risk scores or calculators, such as NSQIP and CeDAR.
Proper risk assessment of older patients is particularly important for elective surgeries, such as VHRs, that can then directly inform shared decision-making.13 As compared to healthier, younger adults, the decision to operate on older patients with associated age-related risk factors or past procedures is more complex.7,14,61 The risks for adverse surgical outcomes are greater for many older adults and must be weighed against potential benefits.7 This shared decision-making process should be driven by patient values and goals and probable outcomes based on their individualized risk assessment.
Age-related risk factors may also guide preoperative counseling by influencing which type of VHR procedure would best suit each patient. For example, would a frail, functionally dependent patient fair better following an open, laparoscopic, or robotic VHR? Can an older adult with various comorbidities and polypharmacy appropriately recover from a complex VHR or would a simpler procedure yield better outcomes? Although shared-decision making (SDM) aligns naturally with the treatment complexity present in hernia surgery, especially in patients with multiple age related risk-factors, SDM in this field is still in its infancy. Given the paucity of high quality data (Figure 2), the authors are currently enrolling patients in a randomized control trial evaluating the feasibility and effectiveness of a formal SDM aid/tool for older adults deemed operative candidates for a VHR. Our main objective is to improve the surgical decision-making process of patients being offered an elective repair of their ventral hernia using previously validated visual and verbal SDM aids. We are evaluating the tool’s effectiveness for improving patient satisfaction and understanding, postoperative outcomes, and the type of surgical repair decided upon.
Figure 2.
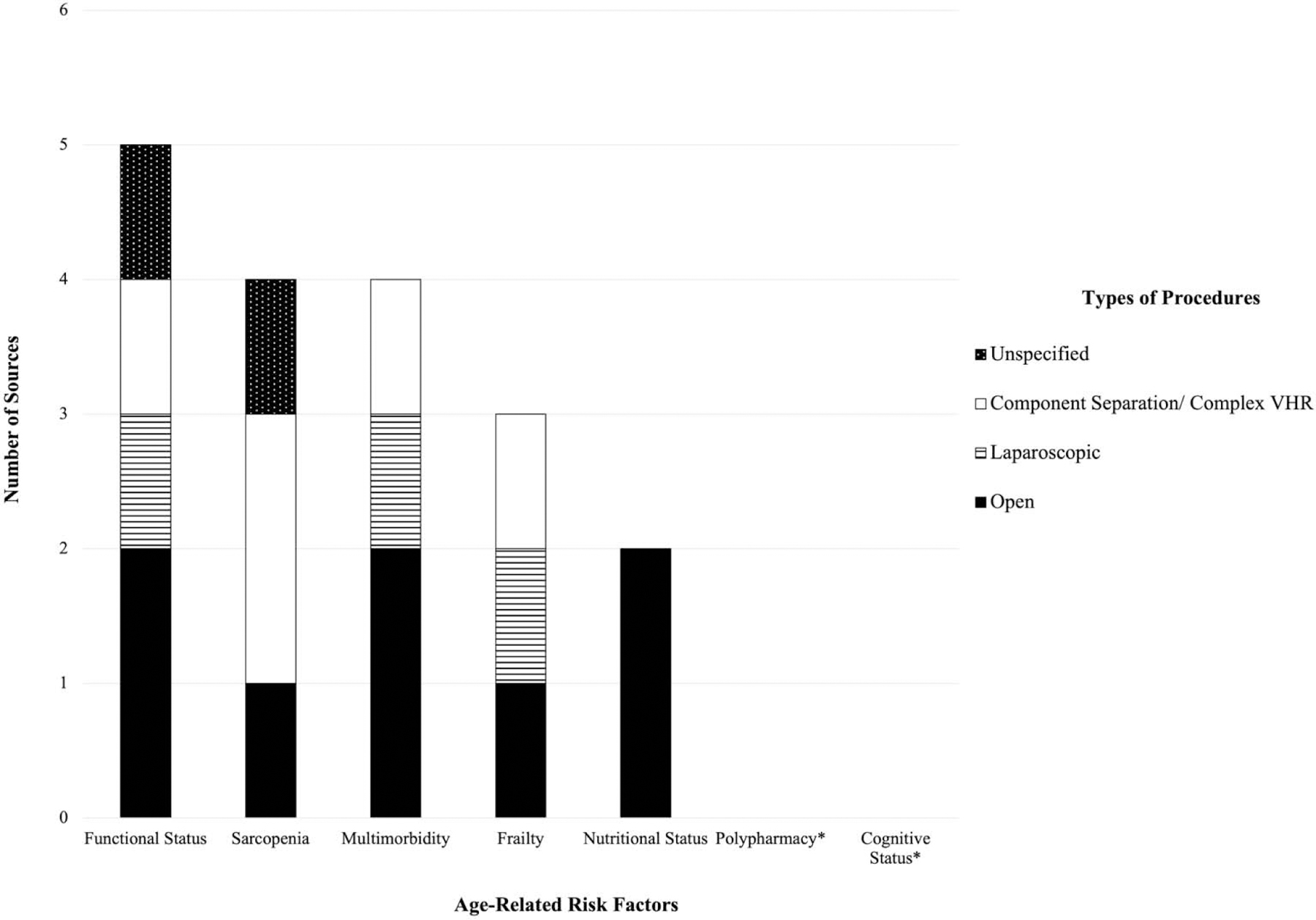
Primary Sources Investigating the Impact of Age-Related Risk Factors on Various Types of VHR Procedures
Notes: Asterisk signifies age-related risk factors with 0 relevant primary sources. Some sources were counted multiple times if the authors specifically mentioned that they investigated multiple types of VHR procedures or age-related risk factors. This figure does not include findings on overnutrition, due to the large number of relevant studies. No studies investigated robotic VHRs.
Prehabilitation
The identification of older patients at risk for adverse outcomes also presents the opportunity to intervene through prehabilitation.11,13,17 Given that postoperative complications are directly related to higher rates of perioperative and long-term mortality, as well as higher hospital costs, there has been a push towards prehabilitation of at-risk patients.11,12,15,64–66 Prehabilitation is a team-based approach including geriatricians, surgeons, clinical nurse specialists, occupational therapists, physical therapists, and administrators.24,64 In the United Kingdom, the POPS (Proactive Care of Older People Undergoing Surgery) Service has pioneered this model. After screening all patients, those deemed eligible are referred to the optimization clinic where they partake in education and training specifically designed to target their organ-specific comorbidities.64 Retrospective analysis has shown that these targeted programs decrease the incidence of postoperative medical conditions (delirium, pneumonia, pressure sores), decrease length of hospital stay, and increase the rate of postoperative mobilization.64 Similar groups exist at other academic medical centers around the United States, including Duke’s POSH (Peri-operative Optimization of Senior Health) program, which is a multidisciplinary clinic focused on optimizing nutrition, exercise, mindfulness, medication review, function, and cognition for at-risk patients.65 A recent meta-analysis of eight randomized controlled trials showed that prehabilitation prior to major abdominal surgery correlates with reduced pulmonary complications and overall morbidity.66
Within the field of ventral hernias, Joslyn et al. outline a number of prehabilitative strategies to improve outcomes of abdominal wall reconstruction.17 The authors emphasize the optimization of modifiable preoperative variables, such as the aforementioned age-related risk factors.11,17,46 As an example, a combination of resistance exercises and protein intake of 1.5–2.5 gm/kg/d can reduce sarcopenia and improve postoperative outcomes.17 Similar regimes target the remaining modifiable risk factors. One group has evaluated prehabilitation programs for VHR.67 Prior to VHR, obese patients (BMI 30–40 kg/m2) were randomized to either a structured prehabilitation program or to standard counseling. Patients enrolled in prehabilitation programs are more likely to be hernia and complication free at one month follow up. However, the prehabilitation group had a higher dropout rate and four patients required an emergent repair for an incarcerated hernia and strangulated bowel.67 The link between prehabilitation programs and the need for emergency repair is unclear: the time of enrollment to emergent repair varied amongst the four patients with one patient requiring surgery only six days after study enrollment and the others within one month. Multiple prehabilitation protocols currently exist, but in order for prehabilitation programs to become standard of care for VHRs further work is needed to tailor specific programs to the needs of the ventral hernia patient population.
The imperative need for prehabilitation in the ventral hernia population is highlighted by its potential impact on healthcare costs. In 2009, a small minority (15%) of patients were responsible for half of the total hospital costs of inpatient VHRs across over 1,000 United States hospitals.17,68 Although the average VHR-associated hospital cost for most patients was $32,000, that of the higher-cost minority was $173,000. This minority also experienced increased length of hospital stay and mortality, as compared to their lower-cost peers.68 The preoperative identification and prehabilitation of these high-cost patients have the potential to drastically diminish complications and concomitant costs. This effect will only be magnified with the increasing complexity and prevalence of VHRs in an aging demographic.17 Given its potentially high impact, prehabilitation is essential in improving the treatment of VHR patients. However, these programs must adequately target the age-related risk factors that, as of yet, are still poorly defined in the ventral hernia population.
Conclusion
As the population continues to age, older adults are increasingly in need of complex and potentially high-risk VHRs. These older adults are particularly complicated to treat, given the unique risk factors associated with aging. Despite the increasing complexity of both the procedures and the patient population, there is a paucity of literature exploring the factors affecting older adults’ VHR outcomes. The little data that exists suggests that multimorbidity, polypharamacy, functional status, frailty, cognitive status, sarcopenia, and nutritional status are associated with adverse VHR outcomes in older adults. The fifteen primary sources (displayed in Table 1) that do investigate these topics do show a consistent pattern of worse VHR, such as mortality, complications, non-home discharge, and length of hospital stay, with increased age-related risk factors. These age-related risk factors are perhaps more indicative of adverse outcomes than the risk factors traditionally considered preoperatively, such as chronological age, and yet they have largely been ignored by surgeons. For example, while Joseph et al. showed that frailty increases the risk of life-threatening complications and mortality by 35 and 62 times, respectively, frailty is rarely considered in preoperative evaluation.41
Despite the emerging connection between VHR outcomes and age-related risk factors, future work is required. The existing literature is limited in a number of ways. First, there is a shortage of articles investigating the impact of age-related risk factors in patient outcomes following both component separations and robotic VHRs (Figure 2). Secondly, the effects of polypharmacy and cognitive status has not been evaluated in those undergoing VHRs (Table 1, Figure 2). Based on the established negative impact of polypharmacy and cognitive status in other surgical populations,12,27,32,34–36,43 studies in the VHR setting would be worthwhile. Finally, although studies exist investigating the relationship between undernutrition, operationalized as low BMI, and VHR outcomes (Table 1), there is a need to confirm these results using more valid measurements, such as via questionnaires. In addition, many of the existing studies rely on large national databases, such as ACS-NSQIP (Table 1). While these databases are readily available and nationally representative, they are susceptible to significant inter-site variability in surgical technique, data collection, and coding of procedures. Also, the inflated sample size has the potential to lead to statistically significant, though clinically irrelevant findings.
Future research will allow for the identification of older adults at increased risk of adverse outcomes, which will directly inform pre-operative assessment and counseling, shared decision-making, and prehabilitation programs specifically geared towards VHR patients. Doing so has the potential to improve patient satisfaction and patient-centered outcomes, lower healthcare costs, and appropriately address the needs of our rapidly aging population.
Acknowledgements
This study was supported by National Institute of Health [T35 NHLBI, 2020]. The authors have no additional acknowledgements.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Caglià P, Tracia A, Borzì L, et al. Incisional hernia in the elderly: Risk factors and clinical considerations. Int J Surg 2014;12:S164–S169. doi: 10.1016/j.ijsu.2014.08.357 [DOI] [PubMed] [Google Scholar]
- 2.Pauli EM, Rosen MJ. Open Ventral Hernia Repair with Component Separation. Surg Clin North Am 2013;93(5):1111–1133. doi: 10.1016/j.suc.2013.06.010 [DOI] [PubMed] [Google Scholar]
- 3.Blount AL, Craft RO, Harold KL. Safety of Laparoscopic Ventral Hernia Repair in Octogenarians. JSLS 2009;13(3):323–326. [PMC free article] [PubMed] [Google Scholar]
- 4.Poulose BK, Shelton J, Phillips S, et al. Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia 2012;16(2):179–183. doi: 10.1007/s10029-011-0879-9 [DOI] [PubMed] [Google Scholar]
- 5.Al Chalabi H, Larkin J, Mehigan B, McCormick P. A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg 2015;20:65–74. doi: 10.1016/j.ijsu.2015.05.050 [DOI] [PubMed] [Google Scholar]
- 6.Neupane R, Fayezizadeh M, Majumder A, Novitsky YW. Is old age a contraindication to elective ventral hernia repair? Surg Endosc 2017;31(11):4425–4430. doi: 10.1007/s00464-017-5492-2 [DOI] [PubMed] [Google Scholar]
- 7.Saber AA, Elgamal MH, Mancl TB, Norman E, Boros MJ. Advanced Age: Is It an Indication or Contraindication for Laparoscopic Ventral Hernia Repair? JSLS 2008;12(1):46–50. [PMC free article] [PubMed] [Google Scholar]
- 8.Le Huu Nho R, Mege D, Ouaïssi M, Sielezneff I, Sastre B. Incidence and prevention of ventral incisional hernia. J Visc Surg 2012;149(5, Supplement):e3–e14. doi: 10.1016/j.jviscsurg.2012.05.004 [DOI] [PubMed] [Google Scholar]
- 9.van Ramshorst GH, Nieuwenhuizen J, Hop WCJ, et al. Abdominal Wound Dehiscence in Adults: Development and Validation of a Risk Model. World J Surg 2009;34(1):20. doi: 10.1007/s00268-009-0277-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.US Census Bureau CHS. 2010 Overview - History - U.S. Census Bureau Accessed June 25, 2020. https://www.census.gov/history/www/through_the_decades/overview/2010_overview_1.html
- 11.Knittel JG, Wildes TS. Preoperative Assessment of Geriatric Patients. Anesthesiol Clin 2016;34(1):171–183. doi: 10.1016/j.anclin.2015.10.013 [DOI] [PubMed] [Google Scholar]
- 12.Oresanya LB, Lyons WL, Finlayson E. Preoperative Assessment of the Older Patient: A Narrative Review. JAMA 2014;311(20):2110–2120. doi: 10.1001/jama.2014.4573 [DOI] [PubMed] [Google Scholar]
- 13.Watt J, Tricco AC, Talbot-Hamon C, et al. Identifying older adults at risk of harm following elective surgery: a systematic review and meta-analysis. BMC Med 2018;16(1):2. doi: 10.1186/s12916-017-0986-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Docimo S, Bates A, Alteri M, Talamini M, Pryor A, Spaniolas K. Evaluation of the use of component separation in elderly patients: results of a large cohort study with 30-day follow-up. Hernia 2020;24(3):503–507. doi: 10.1007/s10029-019-02069-6 [DOI] [PubMed] [Google Scholar]
- 15.Partridge JSL, Harari D, Dhesi JK. Frailty in the older surgical patient: a review. Age Ageing 2012;41(2):142–147. doi: 10.1093/ageing/afr182 [DOI] [PubMed] [Google Scholar]
- 16.Ahmed N, Mandel R, Fain MJ. Frailty: An Emerging Geriatric Syndrome. Am J Med 2007;120(9):748–753. doi: 10.1016/j.amjmed.2006.10.018 [DOI] [PubMed] [Google Scholar]
- 17.Joslyn NA, Esmonde NO, Martindale RG, Hansen J, Khansa I, Janis JE. Evidence-Based Strategies for the Prehabilitation of the Abdominal Wall Reconstruction Patient. Plast Reconstr Surg 2018;142(3S):21S. doi: 10.1097/PRS.0000000000004835 [DOI] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Med 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vetrano DL, Palmer K, Marengoni A, et al. Frailty and Multimorbidity: A Systematic Review and Meta-analysis. J Gerontol A Biol Sci Med Sci 2019;74(5):659–666. doi: 10.1093/gerona/gly110 [DOI] [PubMed] [Google Scholar]
- 20.Janssen T, Alberts A, Hooft L, Mattace-Raso F, Mosk C, van der Laan L. Prevention of postoperative delirium in elderly patients planned for elective surgery: systematic review and meta-analysis. Clin Interv Aging 2019;14:1095–1117. doi: 10.2147/CIA.S201323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolf LL, Scott JW, Zogg CK, et al. Predictors of emergency ventral hernia repair: Targets to improve patient access and guide patient selection for elective repair. Surgery 2016;160(5):1379–1391. doi: 10.1016/j.surg.2016.06.027 [DOI] [PubMed] [Google Scholar]
- 22.Reynolds D, Davenport D, Roth JS. Predictors of poor outcomes in functionally dependent patients undergoing ventral hernia repair. Surg Endosc 2013;27(4):1099–1104. doi: 10.1007/s00464-012-2587-7 [DOI] [PubMed] [Google Scholar]
- 23.Prados-Torres A, Calderón-Larrañaga A, Hancco-Saavedra J, Poblador-Plou B, van den Akker M. Multimorbidity patterns: a systematic review. J Clin Epidemiol 2014;67(3):254–266. doi: 10.1016/j.jclinepi.2013.09.021 [DOI] [PubMed] [Google Scholar]
- 24.Olotu C, Weimann A, Bahrs C, Schwenk W, Scherer M, Kiefmann R. The Perioperative Care of Older Patients. Dtsch Ärztebl Int 2019;116(5):63–69. doi: 10.3238/arztebl.2019.0063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim S, Han H-S, Jung H, et al. Multidimensional frailty score for the prediction of postoperative mortality risk. JAMA Surg 2014;149(7):633–640. doi: 10.1001/jamasurg.2014.241 [DOI] [PubMed] [Google Scholar]
- 26.Janssen TL, Steyerberg EW, Faes MC, et al. Risk factors for postoperative delirium after elective major abdominal surgery in elderly patients: A cohort study. Int J Surg Lond Engl 2019;71:29–35. doi: 10.1016/j.ijsu.2019.09.011 [DOI] [PubMed] [Google Scholar]
- 27.Axley MS, Schenning KJ. Preoperative Cognitive and Frailty Screening in the Geriatric Surgical Patient: A Narrative Review. Clin Ther 2015;37(12):2666–2675. doi: 10.1016/j.clinthera.2015.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith NA, Yeow YY. Use of the Montreal Cognitive Assessment Test to Investigate the Prevalence of Mild Cognitive Impairment in the Elderly Elective Surgical Population. Anaesth Intensive Care 2016;44(5):581–586. doi: 10.1177/0310057X1604400507 [DOI] [PubMed] [Google Scholar]
- 29.Basta MN, Fischer JP, Wink JD, Kovach SJ. Mortality after inpatient open ventral hernia repair: developing a risk stratification tool based on 55,760 operations. Am J Surg 2016;211(6):1047–1057. doi: 10.1016/j.amjsurg.2015.03.009 [DOI] [PubMed] [Google Scholar]
- 30.Ayyala HS, Weisberger J, Le T-M, Chow A, Lee ES. Predictors of discharge destination after complex abdominal wall reconstruction. Hernia 2020;24(2):251–256. doi: 10.1007/s10029-019-02054-z [DOI] [PubMed] [Google Scholar]
- 31.Wastesson JW, Morin L, Tan ECK, Johnell K. An update on the clinical consequences of polypharmacy in older adults: a narrative review. Expert Opin Drug Saf 2018;17(12):1185–1196. doi: 10.1080/14740338.2018.1546841 [DOI] [PubMed] [Google Scholar]
- 32.McIsaac DI, Wong CA, Bryson GL, Walraven C van. Association of Polypharmacy with Survival, Complications, and Healthcare Resource Use after Elective Noncardiac SurgeryA Population-based Cohort Study. Anesthesiol J Am Soc Anesthesiol 2018;128(6):1140–1150. doi: 10.1097/ALN.0000000000002124 [DOI] [PubMed] [Google Scholar]
- 33.Lai S-W, Liao K-F, Liao C-C, Muo C-H, Liu C-S, Sung F-C. Polypharmacy Correlates With Increased Risk for Hip Fracture in the Elderly: A Population-Based Study. Medicine (Baltimore) 2010;89(5):295–299. doi: 10.1097/MD.0b013e3181f15efc [DOI] [PubMed] [Google Scholar]
- 34.Forget M-F, McDonald EG, Shema AB, Lee TC, Wang HT. Potentially Inappropriate Medication Use in Older Adults in the Preoperative Period: A Retrospective Study of a Noncardiac Surgery Cohort. Drugs - Real World Outcomes 2020;7(2):171–178. doi: 10.1007/s40801-020-00190-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boeker EB, de Boer M, Kiewiet JJ, Lie-A-Huen L, Dijkgraaf MG, Boermeester MA. Occurrence and preventability of adverse drug events in surgical patients: a systematic review of literature. BMC Health Serv Res 2013;13(1):364. doi: 10.1186/1472-6963-13-364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kennedy JM, van Rij AM, Spears GF, Pettigrew RA, Tucker IG. Polypharmacy in a general surgical unit and consequences of drug withdrawal. Br J Clin Pharmacol 2000;49(4):353–362. doi: 10.1046/1365-2125.2000.00145.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Albright EL, Davenport DL, Roth JS. Preoperative Functional Health Status Impacts Outcomes after Ventral Hernia Repair. Am Surg 2012;78(2):230–234. [PubMed] [Google Scholar]
- 38.Scarborough JE, Bennett KM, Englum BR, Pappas TN, Lagoo-Deenadayalan SA. The Impact of Functional Dependency on Outcomes After Complex General and Vascular Surgery. Ann Surg 2015;261(3):432–437. doi: 10.1097/SLA.0000000000000767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Balla FM, Yheulon CG, Stetler JL, Patel AD, Lin E, Davis SS. Ventral hernia repair outcomes predicted by a 5-item modified frailty index using NSQIP variables. Hernia 2019;23(5):891–898. doi: 10.1007/s10029-019-01923-x [DOI] [PubMed] [Google Scholar]
- 40.Fisher AL. Just What Defines Frailty? J Am Geriatr Soc 2005;53(12):2229–2230. doi: 10.1111/j.1532-5415.2005.00510.x [DOI] [PubMed] [Google Scholar]
- 41.Elke KM Tjeertes JMK van F. http://www.aginganddisease.org/CN/abstract/abstract147912.shtml. Aging Dis.:0 doi: 10.14336/AD.2019.1024 [DOI]
- 42.Joseph WJ, Cuccolo NG, Baron ME, Chow I, Beers EH. Frailty predicts morbidity, complications, and mortality in patients undergoing complex abdominal wall reconstruction. Hernia J Hernias Abdom Wall Surg 2020;24(2):235–243. doi: 10.1007/s10029-019-02047-y [DOI] [PubMed] [Google Scholar]
- 43.Robinson TN, Wu DS, Pointer LF, Dunn CL, Moss M. Preoperative Cognitive Dysfunction Is Related to Adverse Postoperative Outcomes in the Elderly. J Am Coll Surg 2012;215(1):12–17. doi: 10.1016/j.jamcollsurg.2012.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010;39(4):412–423. doi: 10.1093/ageing/afq034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schlosser KA, Maloney SR, Thielan ON, et al. Sarcopenia in Patients Undergoing Open Ventral Hernia Repair. Am Surg 2019;85(9):985–991. [PubMed] [Google Scholar]
- 46.Clark ST, Malietzis G, Grove TN, et al. The emerging role of sarcopenia as a prognostic indicator in patients undergoing abdominal wall hernia repairs: a systematic review of the literature. Hernia J Hernias Abdom Wall Surg Published online April 16, 2020. doi: 10.1007/s10029-020-02179-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rinaldi JM, Geletzke AK, Phillips BE, Miller J, Dykes TM, Soybel DI. Sarcopenia and sarcopenic obesity in patients with complex abdominal wall hernias. Am J Surg 2016;212(5):903–911. doi: 10.1016/j.amjsurg.2016.03.003 [DOI] [PubMed] [Google Scholar]
- 48.Shafiee G, Keshtkar A, Soltani A, Ahadi Z, Larijani B, Heshmat R. Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J Diabetes Metab Disord 2017;16:21. doi: 10.1186/s40200-017-0302-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hajibandeh S, Hajibandeh S, Jarvis R, Bhogal T, Dalmia S. Meta-analysis of the effect of sarcopenia in predicting postoperative mortality in emergency and elective abdominal surgery. The Surgeon 2019;17(6):370–380. doi: 10.1016/j.surge.2018.09.003 [DOI] [PubMed] [Google Scholar]
- 50.Barnes LA, Li AY, Wan DC, Momeni A. Determining the impact of sarcopenia on postoperative complications after ventral hernia repair. J Plast Reconstr Aesthet Surg 2018;71(9):1260–1268. doi: 10.1016/j.bjps.2018.05.013 [DOI] [PubMed] [Google Scholar]
- 51.Siegal SR, Guimaraes AR, Lasarev MR, Martindale RG, Orenstein SB. Sarcopenia and outcomes in ventral hernia repair: a preliminary review. Hernia J Hernias Abdom Wall Surg 2018;22(4):645–652. doi: 10.1007/s10029-018-1770-8 [DOI] [PubMed] [Google Scholar]
- 52.Saunders J, Smith T. Malnutrition: causes and consequences. Clin Med 2010;10(6):624–627. doi: 10.7861/clinmedicine.10-6-624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gupta R, Gan TJ. Preoperative Nutrition and Prehabilitation. Anesthesiol Clin 2016;34(1):143–153. doi: 10.1016/j.anclin.2015.10.012 [DOI] [PubMed] [Google Scholar]
- 54.Kaiser MJ, Bauer JM, Rämsch C, et al. Frequency of Malnutrition in Older Adults: A Multinational Perspective Using the Mini Nutritional Assessment. J Am Geriatr Soc 2010;58(9):1734–1738. doi: 10.1111/j.1532-5415.2010.03016.x [DOI] [PubMed] [Google Scholar]
- 55.Owei L, Swendiman RA, Kelz RR, Dempsey DT, Dumon KR. Impact of body mass index on open ventral hernia repair: A retrospective review. Surgery 2017;162(6):1320–1329. doi: 10.1016/j.surg.2017.07.025 [DOI] [PubMed] [Google Scholar]
- 56.Tastaldi L, Krpata DM, Prabhu AS, et al. The effect of increasing body mass index on wound complications in open ventral hernia repair with mesh. Am J Surg 2019;218(3):560–566. doi: 10.1016/j.amjsurg.2019.01.022 [DOI] [PubMed] [Google Scholar]
- 57.Nieto EP, Ponz CB, Ananin SF, Vazquez EB. Obesity as a risk factor for complications and recurrences after ventral hernia repair. Int J Abdom Wall Hernia Surg 2020;3(1):1. doi: 10.4103/ijawhs.ijawhs_35_19 [DOI] [Google Scholar]
- 58.Gogna S, Latifi R, Policastro A, et al. Complex abdominal wall hernia repair with biologic mesh in elderly: a propensity matched analysis. Hernia 2020;24(3):495–502. doi: 10.1007/s10029-019-02068-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gokcal F, Morrison S, Kudsi OY. Robotic ventral hernia repair in octogenarians: perioperative and long-term outcomes. J Robot Surg 2020;14(2):275–281. doi: 10.1007/s11701-019-00979-2 [DOI] [PubMed] [Google Scholar]
- 60.Aly S, de Geus SWL, Carter CO, Hess DT, Tseng JF, Pernar LIM. Laparoscopic versus open ventral hernia repair in the elderly: a propensity score-matched analysis. Hernia Published online June 3, 2020. doi: 10.1007/s10029-020-02243-1 [DOI] [PubMed] [Google Scholar]
- 61.Kudsi OY, Gokcal F, Grange SL, Bou-Ayash N, Chang K. Are elderly patients at high risk for postoperative complications after robotic ventral hernia repair? A propensity score matching analysis. Int J Med Robot 2020;16(3):e2095. doi: 10.1002/rcs.2095 [DOI] [PubMed] [Google Scholar]
- 62.Lee YK, Iqbal A, Vitamvas M, McBride C, Thompson J, Oleynikov D. Is it safe to perform laparoscopic ventral hernia repair with mesh in elderly patients? Hernia 2008;12(3):239–242. doi: 10.1007/s10029-007-0312-6 [DOI] [PubMed] [Google Scholar]
- 63.Spaniolas K, Trus TL, Adrales GL. Ventral hernia repairs in the oldest-old: high-risk regardless of approach. Surg Endosc 2014;28(4):1230–1237. doi: 10.1007/s00464-013-3313-9 [DOI] [PubMed] [Google Scholar]
- 64.Partridge J, Sbai M, Dhesi J. Proactive care of older people undergoing surgery. Aging Clin Exp Res 2018;30(3):253–257. doi: 10.1007/s40520-017-0879-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zietlow K, McDonald SR, Sloane R, Browndyke J, Lagoo-Deenadayalan S, Heflin MT. Preoperative Cognitive Impairment as a Predictor of Postoperative Outcomes in a Collaborative Care Model. J Am Geriatr Soc 2018;66(3):584–589. doi: 10.1111/jgs.15261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Heger P, Probst P, Wiskemann J, Steindorf K, Diener MK, Mihaljevic AL. A Systematic Review and Meta-analysis of Physical Exercise Prehabilitation in Major Abdominal Surgery (PROSPERO 2017 CRD42017080366). J Gastrointest Surg Off J Soc Surg Aliment Tract 2020;24(6):1375–1385. doi: 10.1007/s11605-019-04287-w [DOI] [PubMed] [Google Scholar]
- 67.Liang M, Bernardi K, Holihan J, et al. Modifying Risks in Ventral Hernia Patients With Prehabilitation: A Randomized Controlled Trial. Ann Surg 2018;268(4):674–680. doi: 10.1097/SLA.0000000000002961 [DOI] [PubMed] [Google Scholar]
- 68.Poulose BK, Beck WC, Phillips SE, Sharp KW, Nealon WH, Holzman MD. The chosen few: disproportionate resource use in ventral hernia repair. Am Surg 2013;79(8):815–818. [PubMed] [Google Scholar]


