Abstract
We follow Medicare cohorts to estimate Hurricane Katrina’s long-run mortality effects on victims initially living in New Orleans. Including the initial shock, the hurricane improved eight-year survival by 2.07 percentage points. Migration to lower-mortality regions explains most of this survival increase. Those migrating to low-versus high-mortality regions look similar at baseline, but their subsequent mortality is 0.83–1.01 percentage points lower per percentage point reduction in local mortality, quantifying causal effects of place on mortality among this population. Migrants’ mortality is also lower in destinations with healthier behaviors and higher incomes but is unrelated to local medical spending and quality.
JEL: I12, Q51, Q54, R23
Hurricane Katrina, the costliest storm in US history, devastated the Gulf Coast in 2005. The immediate impact of the storm killed nearly 2,000 individuals and displaced more than one million residents, resulting in the largest migration of US residents since the Dust Bowl of the 1930s (Nigg, Barnshaw, and Torres 2006). Climate models predict that such extreme weather events will increase in frequency and severity (Field et al. 2012), yet little is known about the effects of environmental catastrophes on long-run health and longevity, which represent considerable economic value (Murphy and Topel 2006).
The disruption induced by extreme weather events can be used to illuminate factors that affect the accumulation or depreciation of health capital (Grossman 1972). For example, when a disaster displaces people from their homes, the regions they move to may play an important role in shaping long-term health outcomes. While life expectancy varies significantly across US locations (Chetty et al. 2016, Dwyer-Lindgren et al. 2017), little is known about the extent to which this variation reflects the causal effect of place on health. Because Hurricane Katrina displaced many survivors, it can serve as a natural experiment of how place affects long-term health. If the geographic variation in life expectancy reflects causal effects of place, then the widespread migration out of New Orleans to regions with better economic and health conditions may have generated health benefits.
This paper has two primary aims. The first is to estimate the short- and long-run mortality impacts of Hurricane Katrina on the elderly and the long-term disabled of New Orleans. Prior studies have evaluated how demographic and economic outcomes evolve after environmental catastrophes (e.g., Hornbeck 2012; Hornbeck and Naidu 2014; Nakamura, Sigurdsson, and Steinsson 2017), but little is known about the long-run health effects of these events, especially among adults. The second aim is to estimate how the mortality of displaced survivors was shaped by their destinations.
Quantifying the long-run health impacts of events like Hurricane Katrina has proven difficult, largely due to lack of data that capture pre-disaster outcomes and track individuals post-disaster with minimal attrition. To overcome this challenge, we use Medicare administrative data from 1992 to 2013 that allow us to follow elderly and long-term disabled individuals over time and space and provide exact dates of death. We identify Medicare cohorts living in New Orleans just prior to Hurricane Katrina and trace out their mortality rates up to eight years after the storm, regardless of whether or where they move.
To identify how outcomes would have evolved in the absence of Hurricane Katrina, we measure mortality for comparable Medicare cohorts initially residing in ten cities that were not directly affected by the hurricane, following Deryugina, Kawano, and Levitt (2018). To validate this control group, we show that mortality trends in the New Orleans and control city cohorts were similar prior to Hurricane Katrina as far back as 1992, the earliest year for which we have data. We then estimate the causal effects of the hurricane by comparing how the New Orleans cohort’s post-hurricane outcomes changed relative to those of the comparison cohort (i.e., a cohort-level difference-in-differences event study analysis).1
We find that in 2005, the year of the storm, Hurricane Katrina increased mortality by 0.56 percentage points (over 10 percent of the mean). Most of these excess deaths occurred within a week of the hurricane’s landfall, and this immediate effect dissipated over several months. In contrast to the short-run mortality increase, we find that Hurricane Katrina led to sustained reductions in mortality from 2006 to 2013. This long-run mortality decline is not explained by short-run mortality displacement, or “harvesting.” Inclusive of the initial increase in mortality, Hurricane Katrina increased the probability of surviving through 2013, eight years past the storm, by 2.07 percentage points, a 3.2 percent increase relative to the overall eight-year survival rate of the 2005 New Orleans cohort.
We also find that the hurricane led to a massive and lasting dislocation of the elderly and long-term disabled, consistent with prior evidence on the demographic effects of the hurricane (Deryugina, Kawano, and Levitt 2018; Eyer et al. 2018). Medicare beneficiaries living in New Orleans as of March 2005 were nearly 50 percentage points more likely to leave their commuting zone of residence than members of the control group. Over one-half of those who left had not returned as of 2013, conditional on being alive. New Orleans was one of the highest mortality areas in the country prior to Hurricane Katrina, and displaced individuals generally moved to lower-mortality regions. To the extent that local mortality outcomes reflect place-specific determinants of health, relocation to lower-mortality regions may have driven the decline in mortality among Hurricane Katrina victims.
To directly examine the role of place on health, we examine the mortality patterns among New Orleans residents who had moved away by March 2006. We find that hurricane survivors who moved to low-mortality regions subsequently experienced lower mortality than survivors who moved to high-mortality regions. Specifically, each percentage point increase in the destination region’s mortality rate corresponds to a 0.83–1.01 percentage point increase in the movers’ mortality rate. This effect emerges quickly after the move, suggesting it does not arise entirely through slow-moving channels such as lifestyle.
The relationship between local and migrant mortality describes the causal effect of place on individual mortality under the assumption that baseline mortality risk among those who move is uncorrelated with mortality rates in the destination region. Supporting this assumption, we find little correlation between destination mortality rates and movers’ ex ante predicted mortality, which we construct from detailed data on demographic characteristics, past health care utilization, and preexisting chronic conditions. In addition, the estimated relationship between movers’ mortality and destination mortality is highly stable, even with rich controls, including variables that are strongly predictive of mortality. Changes in the local mortality rate experienced by hurricane victims can explain over 70 percent of the long-run mortality decline caused by the hurricane.
Next, we examine how other local attributes correlate with movers’ mortality. We find that movers’ mortality increases with local rates of obesity and smoking and decreases with average income, home values, and urban population share. Movers’ mortality is not statistically significantly correlated with local physician or hospital bed supply or a hospital quality index. We also do not find a relationship between movers’ mortality and local health care spending, shedding new light on a long-standing question of whether higher-spending regions generate better health outcomes than lower-spending regions and pointing to low returns to living in a high-spending region.2
Our study adds to a growing body of literature that uses migration to identify how local conditions affect individual outcomes. Song et al. (2010); Finkelstein, Gentzkow, and Williams (2016); and Molitor (2018) study movers in Medicare to identify local determinants of diagnosis rates, medical spending, and physician practice styles, respectively. Movers have also been used to study how local conditions affect education and earnings (Chetty, Hendren, and Katz 2016; Nakamura, Sigurdsson, and Steinsson 2017; Chyn 2018; Chetty and Hendren 2018a), income reporting in tax filings (Chetty, Friedman, and Saez 2013), and brand preferences (Bronnenberg, Dubé, and Gentzkow 2012). Black et al. (2015) and Johnson and Taylor (2019) estimate mortality effects of migration but do not study how migrant outcomes depend on destination characteristics.
We contribute to this literature by studying how the long-run mortality outcomes of those displaced by Hurricane Katrina depend on the destination region. Our finding that migrants’ realized mortality outcomes correspond closely to their destination region’s mortality rate suggests that local conditions are an important determinant of individual health outcomes. Our study complements contemporaneous work by Finkelstein, Gentzkow, and Williams (2019), who estimate the mortality effects of place among Medicare movers using a novel method to account for potentially endogenous sorting on unobservables. They also find that current location matters greatly for life expectancy, although the correlation they find between the effect of place on mortality and local mortality is smaller than what we estimate. Because Hurricane Katrina displaced many people who would not have otherwise moved, this pattern suggests that place may matter less for the typical mover than for the typical stayer, analogous to evidence of negative selection on children’s economic gains among movers to better neighborhoods (Chyn 2018).
Our results also shed light on why life expectancy differs across the United States and how health capital accumulates over the life cycle. Regional differences in life expectancy correlate strongly with numerous demographic factors and health behaviors, like income and smoking (Chetty et al. 2016, Dwyer-Lindgren et al. 2017). Our results suggest that geographic variation in life expectancy is at least partly driven by contemporaneous location characteristics and not just by differences in demographics or health behaviors that affect mortality only over long time horizons. In addition, the sharp and enduring decline in the mortality rate of Hurricane Katrina victims contrasts with the canonical Grossman (1972) model of health capital, which posits that health capital changes slowly, although it is consistent with a version of the model in which health capital depreciates rapidly, as may be the case with the elderly and long-term disabled.
We also provide the longest-run controlled estimates of the mortality effects of a disaster on adult victims. Prior research on disasters and health has been largely limited to considering birth outcomes and infant health (e.g., Torche 2011, Currie and Rossin-Slater 2013, Currie and Schwandt 2016), immediate post-disaster mortality (e.g., Kahn 2005), or survey-based measures of longer-run health for a subset of the victims.3 Survey approaches, however, generally suffer from nonrandom sampling, rarely measure preexisting outcomes, and usually lack a control group. By contrast, our data track the mortality and location of every Medicare-eligible individual. Our finding that Hurricane Katrina reduced long-run mortality among the elderly and long-term disabled populations builds on recent evidence that the hurricane indirectly generated other long-run benefits, including higher earnings among the working-age population (Groen, Kutzbach, and Polivka 2020; Deryugina, Kawano, and Levitt 2018) and improved test scores among displaced students (Sacerdote 2012).
The paper proceeds as follows. Section I provides an overview of Hurricane Katrina. Section II describes the data and estimation sample. Section III outlines our research design, and Section IV presents the results. Section V concludes.
I. Overview of Hurricane Katrina
Hurricane Katrina formed as a tropical depression on August 23, 2005 (National Weather Service 2016). As the storm’s strength and path became apparent, Louisiana officials declared a state of emergency on August 26. The next day, an evacuation order was given for New Orleans, resulting in an evacuation rate of 80–90 percent (Wolshon 2006). On August 29, Hurricane Katrina struck New Orleans as a Category 3 hurricane with sustained winds of 125 miles per hour and a storm surge that breached numerous levees and floodwalls, resulting in widespread flooding (see online Appendix Figure A.1). The heavy winds and flooding severely damaged thousands of homes and other infrastructure in New Orleans (Rowland 2007). Hospital capacity and utilization in New Orleans fell by over 70 percent (see online Appendix Figure A.2) as all nine large hospitals in the city closed; most remained closed for years or never reopened. In total, Hurricane Katrina caused $161 billion (2017 dollars) in direct damages, making it the costliest US natural disaster on record (National Hurricane Center 2018, National Oceanic and Atmospheric Administration 2018).
Hurricane Katrina’s official death toll was 1,833, also making it the deadliest US natural disaster since the 1928 Okeechobee hurricane (Beven-II et al. 2008). The storm further displaced an estimated one million individuals living in its path (Nigg, Barnshaw, and Torres 2006), including up to 200,000 Medicare beneficiaries (Super and Biles 2005). The Federal Emergency Management Agency (FEMA) prohibited most New Orleans residents from returning home for months.4 Because of the widespread damages across Louisiana, many of the displaced were transported to other states. Texas received about 200,000 evacuees, and Arkansas received about 50,000, but refugees were also evacuated to at least 32 other states.5 Storm victims unable to find suitable living arrangements were given housing assistance, but little systematic information is available on how victims chose where to relocate in the longer run.
The aid response to Hurricane Katrina was considerable.6 The federal government provided about $50 billion in disaster aid to Louisiana, excluding flood insurance payments and loans. Most of these funds were earmarked for rebuilding infrastructure rather than given directly to victims. In total, aid spending for New Orleans was as much as $125,000 per capita, of which about $17,000 consisted of direct transfers to individuals (Deryugina, Kawano, and Levitt 2018). Absent the massive aid response, the long-term impacts of Hurricane Katrina could have been much worse than what occurred.
The losses and disruption caused by Hurricane Katrina could have persistently worsened the health of elderly and long-term disabled victims, groups that are thought to be especially vulnerable to environmental catastrophes (Morrow 1999, Fernandez et al. 2002).7 It is also possible that Hurricane Katrina improved long-run health if victims relocated to areas that were more conducive to good health. Our goal in the remainder of the paper is to shed light on these possibilities.
II. Data and Estimation Sample
A. Data
The primary data for our analysis are Medicare administrative records for all Medicare beneficiaries from 1992 to 2013 (Centers for Medicare and Medicaid Services 1992–2013). These data offer three key features for studying health dynamics in our setting. First, Medicare covers nearly all US residents aged 65 and older as well as non-elderly individuals who have received Social Security disability benefits for at least 24 months or have end-stage renal disease (ESRD) or amyotrophic lateral sclerosis. Second, annual beneficiary summary files report the nine-digit beneficiary zip code where Social Security Administration (SSA) benefits and official communication are mailed, which we call the “zip code of residence.” This allows us to identify individuals living in a specific place at a certain time (e.g., New Orleans residents prior to Hurricane Katrina) and to track them over time even if they move.8 Third, Medicare reports exact dates of death based on SSA records.
We use two sets of annually recorded Medicare variables.9 The first set, which comes from Medicare eligibility files and is available for every Medicare beneficiary, contains beneficiary zip code, race, sex, birth and death dates, cause of death, and ESRD information. Beneficiary zip code is based on a snapshot taken at the end of the year (file years 1999, 2007, and 2009–2013) or in March of the following year (all other file years in the sample). For individuals who die prior to the location snapshot, the zip code reflects their last address on record. Cause of death codes are available only for years 1999–2008.
The second set of Medicare variables is available only for beneficiaries enrolled in fee-for-service Medicare (over 80 percent of our sample). These variables provide information on medical spending and the presence of chronic conditions from fee-for-service claims. We measure total annual medical spending as the sum of payments due to providers (including hospitals and physicians), excluding payments for Part D drugs. We use Medicare indicators for the presence of 27 common chronic conditions inferred from medical claim histories. In most cases, we group the 27 individual conditions into eight broad categories: heart disease and stroke, respiratory disease, blood and kidney disease, cancer, diabetes, musculoskeletal diseases, Alzheimer’s/dementia, and other. The chronic condition indicators are available only for individuals who are continuously enrolled in fee-for-service Medicare over a condition-specific look-back window (usually two years).
We use counties as the primary unit of geography for the analysis. In some cases, we consider commuting zones (CZs), which aggregate counties into 709 regions based on work commute patterns in 2000. We refer to a county by the primary city located in the county and use the terms “city” and “county” interchangeably. For New Orleans, a consolidated city-county, the county and city boundaries are identical.
We obtain several county-level attributes related to public health, the environment, and economic conditions, including average Medicare spending, the number of physicians per capita, smoking and obesity rates, fine particulate matter (PM2.5) levels, frequency of temperature extremes, the crime rate, local government expenditure, and per-capita income. The construction of these variables is detailed in online Appendix Section A.1.4.
Finally, we match Medicare beneficiaries to more detailed flood and neighborhood income characteristics based on their nine-digit zip code of residence at baseline.10 We use five-meter resolution Hurricane Katrina flood depth data from the National Oceanic and Atmospheric Administration (NOAA 2005). We classify a nine-digit zip code as “flooded” if the average flood depth within a 50-meter radius of the centroid is at least two feet. We define neighborhood income for a nine-digit zip code to be the 2000 Census median income among household heads age 65 or older in the block group in which it falls. A beneficiary is “below median income” if their neighborhood income measure is below the median in New Orleans.
B. Estimation Sample
Identifying the causal effect of Hurricane Katrina on mortality requires estimating counterfactual mortality outcomes for New Orleans victims. We do so by examining how outcomes evolve among Medicare beneficiaries initially residing in other regions. Our primary control regions are the ten US cities with a population of at least 100,000 chosen by Deryugina, Kawano, and Levitt (2018) to most closely match the median earnings, population growth, and racial composition of New Orleans in 2000–2005: Baltimore, MD; Birmingham, AL; Detroit, MI; Gary, IN; Jackson, MS; Memphis, TN; Newark, NJ; Portsmouth, VA; Richmond, VA; and St. Louis, MO (see online Appendix Figure A.3 for a map). Online Appendix Section A.2.1 reports the robustness of our main results to alternative control groups.
Our preferred estimation sample consists of individuals who were eligible for Medicare in 2004 and whose baseline location is reported as of March 2005, just prior to Hurricane Katrina (the “2004 cohort”). Table 1 summarizes the baseline (2004) characteristics of this cohort for the 65,457 beneficiaries initially residing in New Orleans (column 1) and the 941,685 beneficiaries from the ten control cities (column 2). Gender composition, age distribution, and claims-based Medicare spending and chronic condition prevalence were similar for the New Orleans and control city groups. Relative to the control group, New Orleans beneficiaries were more likely to be Black (60.5 percent versus 39.2 percent), more likely to live in a below-median income neighborhood (49.9 percent versus 34.8 percent), and less likely to be enrolled in fee-for-service Medicare (68.6 percent versus 92.5 percent). Over half of the New Orleans beneficiaries lived in a nine-digit zip code with two or more feet of flooding caused by Katrina.
Table 1—
Summary Statistics (2004 Medicare Cohort)
| New Orleans (1) | Ten control cities (2) | New Orleans movers (3) | |
|---|---|---|---|
| Percent male | 43.0 | 41.9 | 41.4 |
| Percent black | 60.5 | 39.2 | 75.6 |
| Age | 70.1 | 71.0 | 67.2 |
| Percent 65+ | 77.7 | 81.2 | 69.5 |
| Percent 75+ | 40.7 | 42.2 | 32.9 |
| Income for 65+ year-olds in 9-digit zip | 28,230 | 30,962 | 25,005 |
| Percent below median income | 49.9 | 34.8 | 55.4 |
| Percent who experienced 2+ feet of flooding during Katrina | 56.5 | 0.0 | 67.1 |
| Percent enrolled in fee-for-service Medicare in 2004 | 68.6 | 92.5 | 69.7 |
| 2004 Medicare spending (fee-for-service only) | 10,460 | 9,640 | 8,857 |
| Percent with end-stage renal disease | 2.1 | 1.7 | 2.0 |
| Percent with blood and kidney disease | 46.2 | 52.7 | 43.6 |
| Percent with heart disease and stroke | 64.8 | 69.4 | 63.2 |
| Percent with diabetes | 27.4 | 28.5 | 28.9 |
| Percent with musculoskeletal condition | 28.6 | 30.4 | 27.0 |
| Percent with respiratory disease | 12.8 | 14.0 | 12.8 |
| Percent with cancer | 6.8 | 8.3 | 4.9 |
| Percent with Alzheimer’s / dementia | 12.4 | 12.6 | 8.5 |
| Percent with other chronic condition | 39.9 | 41.1 | 38.9 |
| Number of individuals | 65,457 | 941,685 | 26,467 |
Notes: The table summarizes baseline (2004) characteristics of the 2004 Medicare cohort. The unit of observation is a beneficiary. Income and flood variables are available only for individuals with valid nine-digit zip codes (57,314 New Orleans individuals, 23,295 New Orleans movers, and 847,509 individuals from the ten control cities). Medicare spending is available only for individuals enrolled in fee-for-service Medicare (44,913 New Orleans individuals, 18,695 New Orleans movers, and 871,007 individuals from the 10 control cities). Chronic condition variables are only available for beneficiaries who have been continuously enrolled in fee-for-service Medicare over a condition-specific look-back window, typically two years. Chronic conditions sample sizes range from 31,027 to 37,944 for New Orleans individuals, from 12,532 to 15,797 for New Orleans movers, and from 656,230 to 769,430 for individuals from the ten control cities.
Between March 2005 and March 2006, 26,467 beneficiaries in the 2004 New Orleans cohort left the New Orleans CZ, a group we call “movers” (see column 3 of Table 1). Relative to the average New Orleans beneficiary, movers were younger, were more likely to be Black, and came from poorer and more heavily flooded neighborhoods. Movers were slightly less likely to have some chronic conditions (e.g., heart disease and cancer) but equally or slightly more likely to have others (e.g., diabetes). New Orleans movers also scattered broadly: the top 20 destination counties accounted for about one-half of all movers, while the other half relocated to counties that each attracted less than 1 percent of the movers (see online Appendix Table A.1).
We use cohorts based on Medicare eligibility in 1992 and 1999 to assess mortality trends prior to Hurricane Katrina. Figure 1 plots raw annual death rates for the 1999 Medicare cohort, by initial region of residence.11 For example, the 2005 mortality rate for New Orleans is the fraction of beneficiaries who died in 2005 out of those who lived in New Orleans in 1999 (regardless of subsequent moves) and survived through 2004. Mortality rates for the New Orleans cohort are plotted in black, and mortality rates for cohorts from each of the ten control cities are plotted in blue. For comparison to the rest of the United States, light gray lines plot mortality rates for the cohorts initially residing in each CZ except the one containing New Orleans.
Figure 1.
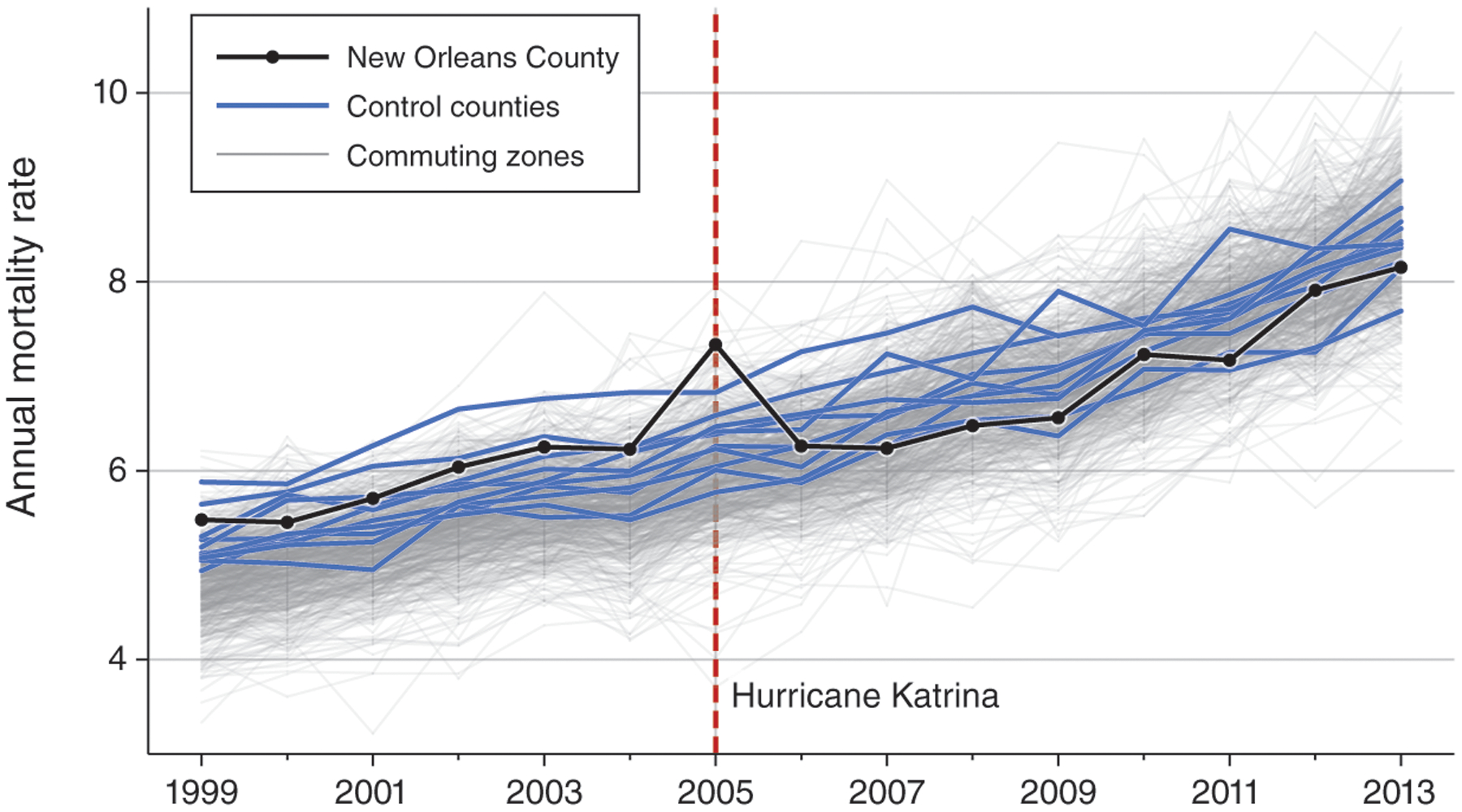
Cohort Annual Mortality Rates for New Orleans versus Other Areas
Notes: The figure shows raw annual death rates for the 1999 Medicare cohort, by initial region of residence. Mortality rates for the New Orleans county cohort are plotted in black, and mortality rates for the ten control county cohorts are plotted in blue. The light gray lines plot mortality rates for each US commuting zone cohort with at least 1,000 beneficiaries, except for the New Orleans commuting zone.
Figure 1 reveals one of the key findings we formally estimate below. Prior to Hurricane Katrina, the New Orleans cohort had one of the highest mortality rates in the United States. Cohorts from the ten control cities also generally had high mortality rates that trended similarly to the New Orleans cohort’s mortality in 1999–2004.In 2005, the year of Hurricane Katrina, the New Orleans cohort’s mortality rate increased substantially. But in 2006, mortality among the New Orleans cohort fell to the middle of the mortality rate distribution and remained there through 2013, suggesting that Hurricane Katrina led to a long-run decline in mortality among the New Orleans cohort. This long-run decline is not explained by regression to the mean: in other regional cohorts with high pre-2005 mortality, post-2005 annual mortality rates approximately paralleled those from lower mortality cohorts (online Appendix Figure A.5). As we estimate formally below, the mortality decline also cannot fully be explained by mortality displacement, or harvesting, as would occur if Hurricane Katrina killed individuals who would have died soon anyway.
III. Research Design
A. Short-Run Effects of Hurricane Katrina
We estimate the short-run mortality effects of Hurricane Katrina on the New Orleans Medicare population using a difference-in-differences event study analysis of the 2004 New Orleans and control city cohorts. We define event week t = 0 as the seven-day period beginning on Monday, August 29, 2005, the day Hurricane Katrina struck New Orleans. We construct a panel dataset with observations for each individual i and week t over the 100-week period beginning 34 weeks prior to and ending 65 weeks after Hurricane Katrina, which corresponds to weeks starting on January 3, 2005, and on November 27, 2006, respectively. We omit any observations for weeks after an individual dies. We then estimate
| (1) |
where the outcome, Diedit, equals 0 if individual i survived through week t and equals 1 if he or she died that week. We define a “treatment” indicator NOLAi as equal to 1 if individual i lived in New Orleans at baseline and equal to 0 otherwise. Fixed effects for the five-digit zip code of an individual’s residence in the base year capture baseline geographic differences in mortality rates, while event week fixed effects capture how mortality evolves over time for the sample as a whole. Standard errors are clustered by baseline zip code.
The focal parameters in equation (1) are βt, the coefficients on the interactions of event week and treatment indicators. The term βt nonparametrically captures how the change in the New Orleans cohort’s mortality between the reference week and week t differs from the change in the control city cohorts’ mortality over the same period. Specifically, βt identifies the causal effect of Hurricane Katrina on the New Orleans cohort’s mortality rate under the assumption that the mortality rate among the New Orleans cohort would have paralleled the control city cohorts’ mortality rates in the absence of the hurricane. The plausibility of this assumption can be assessed by testing for parallel trends in the weeks prior to the storm (i.e., βt = 0 for t < 0), which motivates the inclusion of the 34 pre-event week indicators in equation (1). To minimize sensitivity of the results to the choice of reference week, we calculate and report adjusted estimates , where is the average value of βt for t < 0 (including β−1, which is mechanically zero). Thus, bt reflects Hurricane Katrina’s mortality effect in week t, relative to average mortality rate differences in the 34 weeks prior to the hurricane.
B. Long-Run Effects of Hurricane Katrina
Annual Mortality and Relocation.—
We estimate the long-run effects of Hurricane Katrina on mortality and relocation using a cohort approach very similar to our short-run weekly analysis, except that we define the time dimension of the panel data to be annual and extend our period of analysis to cover up to eight years after 2005, the year of Hurricane Katrina. Specifically, we include observations for each individual i and year t starting from the base year used to define the cohort (1992, 1999, or 2004) through 2013, omitting any observations for years after the individual dies. We then estimate
| (2) |
where the outcome Yit measures either mortality or relocation. The mortality outcome, Diedit, equals 0 if individual i survived through year t and equals 1 if he or she died that year. The relocation outcome, LeftCZit, equals 0 if the individual resided in their baseline CZ in year t and equals 1 if he or she was living in another CZ.
For simplicity, we estimate equation (2) with no demographic controls beyond baseline zip code fixed effects. Because the residual demographic balance between treatment and control group cohorts may shift over time and thereby influence mortality trends through a change in cohort composition, the online Appendix also reports event study results that include fixed effects Xit for all combinations of baseline age (in one-year bins), race, and sex. All other variables are defined as in equation (1), except that the time period t reflects years instead of weeks and we thus include year fixed effects instead of week fixed effects. Standard errors are clustered by baseline zip code, although for robustness we also carry out inference using the synthetic control method with permutation tests conducted at the county and CZ levels (see online Appendix Section A.2.1).
We use 2004, the year prior to Hurricane Katrina, as the reference period so that βt captures how the change in the New Orleans cohort’s mortality between 2004 and year t differs from changes in the control city cohorts’ mortality over the same period. As with the weekly analysis, βt identifies the causal effect of Hurricane Katrina on the New Orleans cohort’s mortality rate in a given year under the assumption that the New Orleans cohort’s mortality would have paralleled the control city cohorts’ mortality rates in the absence of the hurricane. The plausibility of this assumption can be assessed by testing for parallel trends in the years prior to the storm (i.e., βt = 0 for t < 2004), which can be done when estimating equation (2) for cohorts formed in base years prior to 2004.
We estimate equation (2) separately for the 1992, 1999, and 2004 Medicare cohorts. The 1992 and 1999 cohorts allow us to examine pretrends over a long time horizon, but these cohorts may only partially capture Hurricane Katrina’s impact on Medicare victims, as about two-thirds (one-third) of individuals in the 1992 (1999) cohort had moved away or died before 2005.12 Thus, we use the 2004 Medicare cohort to calculate our preferred estimates of the magnitude of Hurricane Katrina’s mortality effect.
Cumulative Mortality.—
The annual mortality results obtained from equation (2) can be used to calculate the effect of Hurricane Katrina on changes in cumulative mortality for the New Orleans cohort.13 Specifically, for each post-Katrina year t between 2005 and 2013, the change in cumulative mortality probability ΔMt is given by
| (3) |
where βτ are the annual mortality effects of Hurricane Katrina and mτ is the empirical fraction of the New Orleans cohort who die in year τ.14 We estimate ΔMt and its standard error using the estimates from equation (2).
Concise Difference-in-Differences.—
Event study estimates from equation (2) nonparametrically identify treatment effects over time and also help to assess the plausibility of the parallel trends assumption. If there are no pretends, and if the treatment effect is constant over a period of time, then a more efficient approach is to combine years into longer periods. To that end, we group years into a pretreatment reference period (base year through 2004), the year of treatment (2005) for capturing short-run effects, and a post-treatment period (2006–2013) for estimating long-run effects. Specifically, we estimate
| (4) |
The indicators 1(t = 2005) and 1(t ≥ 2006) denote whether the year of observation is 2005 or falls within the period 2006–2013, respectively. As with equation (2), we include year and baseline zip code fixed effects. For robustness, some specifications include additional controls Xit, such as baseline demographics. The coefficients βSR and βLR thus describe the average short-run (2005) and long-run (2006–2013) causal effects, respectively, of Hurricane Katrina on mortality among the New Orleans cohort under the same identification assumption required for interpreting equation (2) estimates as causal.
C. Migration and Place Effects
To examine the role of relocation in determining mortality risk following Hurricane Katrina, we estimate how mortality outcomes of individuals displaced by the hurricane depend on characteristics of the area they moved to. To do so, we restrict our sample to individuals in the 2004 New Orleans cohort who survived through 2005 and moved to another county at some point between March 2005 and March 2006. Plausibly, most of these migrants left New Orleans in the aftermath of Hurricane Katrina. To avoid conflating local characteristics with Hurricane Katrina’s impact in the vicinity of New Orleans, we further exclude from the movers sample individuals who moved to a county in the same CZ as New Orleans.
We estimate the relationship between a New Orleans mover’s post-Katrina (2006–2013) annual mortality rate and the average annual post-Katrina mortality rate of the county in which mover i resided in 2006, which we denote by MDR2006C(i).15 To avoid a mechanical relationship between migrant mortality outcomes and our measure of destination mortality, we calculate MDR2006C(i) as the annual mortality rate of the county’s 2004 Medicare cohort (i.e., of Medicare beneficiaries who lived in that county as of March 2005) averaged over 2006–2013. We then estimate
| (5) |
Because only New Orleans movers are included in this empirical exercise, it is not necessary to have New Orleans indicators in equation (5). All remaining control variables are defined as before. Note that year fixed effects will control for any mortality effects that are common to all migrants, such as the effect of moving in with relatives. The coefficient γ describes the causal effect of place, as captured by local mortality, on migrant mortality under the assumption that migrants do not sort to high- or low-mortality regions based on unobserved mortality risk. When we present the results, we evaluate the plausibility of this assumption by assessing the degree of sorting along observable risk factors as well as the sensitivity of estimates of γ to the inclusion of rich controls, including baseline demographics, medical spending, and chronic conditions.
We also estimate other local correlates of migrant mortality by replacing MDR2006C(i) in equation (5) with other attributes of each mover’s 2006 destination county, such as health behaviors, income, and medical spending and quality. To avoid capturing the outcomes of Hurricane Katrina movers in the destination characteristics, we measure Medicare-derived characteristics (mortality and medical spending) using the 2004 cohort from each region and, when possible, all other characteristics before 2005 (see online Appendix Section A.1.4).16 As with local mortality, the estimated relationship captures the causal effect of living in a low- or high-attribute place only if unobserved mortality risk is uncorrelated with that attribute. Additionally, for an estimate to reflect the causal effect of that attribute on mortality, there must be no other unobserved local characteristic that is both correlated with the attribute of interest and affects movers’ mortality.
IV. Results
A. Short-Run Effects of Hurricane Katrina
Panel A of Figure 2 reports raw weekly mortality rates for the 2004 New Orleans and control city cohorts. Panel B reports the corresponding weekly difference-in-differences mortality effects of Hurricane Katrina from equation (1), adjusted such that the reference period is the 34 weeks prior to the hurricane (as described in Section IIIA).17 The gray dashed line 14 weeks after the hurricane indicates the week of FEMA’s “look-and-leave”/“look-and-stay” announcement on December 9, 2005; prior to this date, most New Orleans residents were formally prohibited from returning to their homes. The lack of differential trends in mortality prior to Hurricane Katrina supports interpreting the post-Katrina estimates as causal effects of the hurricane on mortality rather than preexisting differences between treatment and control individuals.
Figure 2.
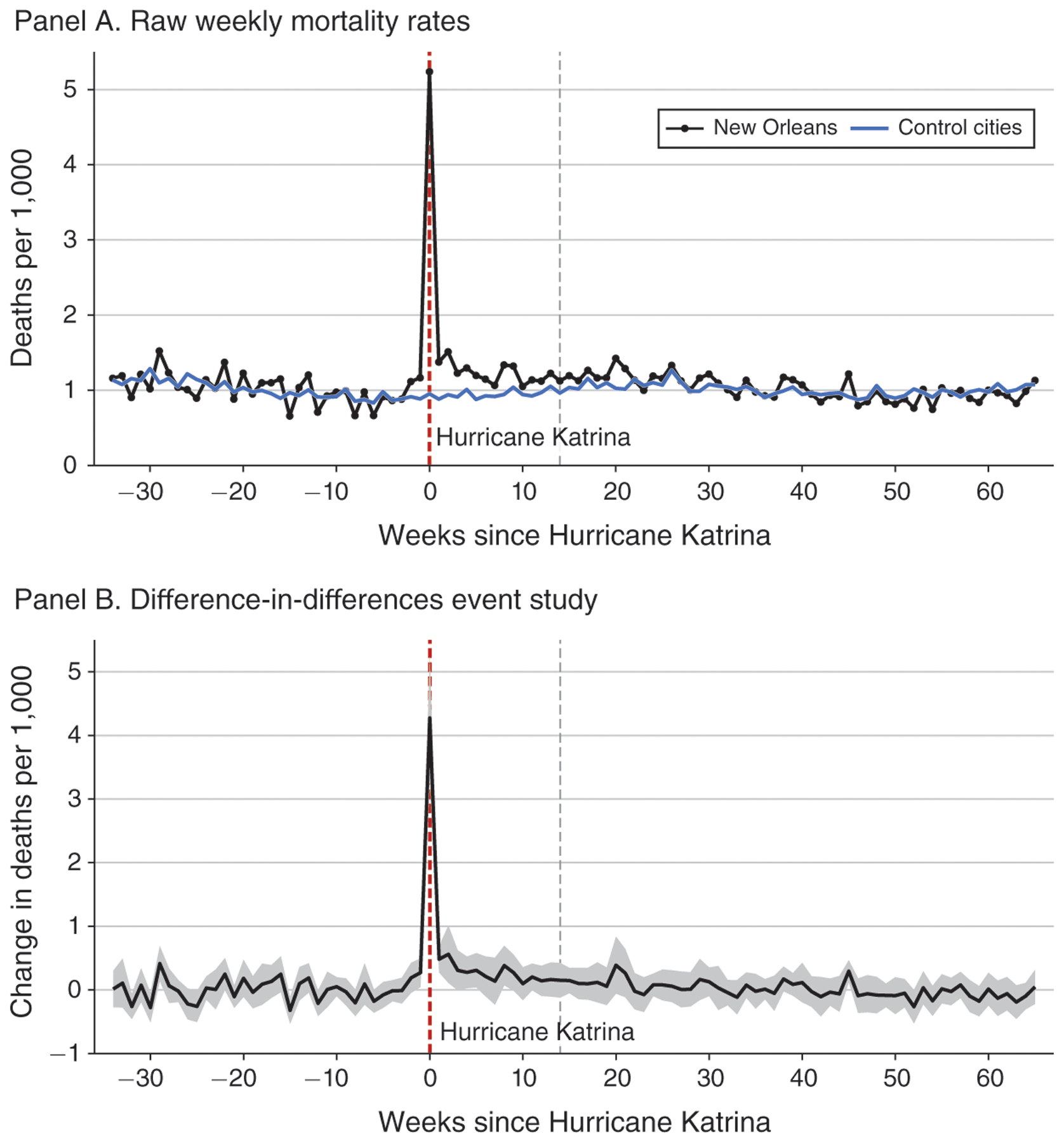
Short-Run Effects of Hurricane Katrina (2004 Medicare Cohort)
Notes: Panel A shows raw weekly mortality rates over the 34 weeks preceding and the 65 weeks following Hurricane Katrina for the New Orleans cohort (black line) and for the control cities cohort (blue line). Panel B shows difference-in-differences estimates and corresponding 95 percent confidence intervals from equation (1), adjusted such that the reference period is the average of the 34 weeks prior to the hurricane. The dependent variable is a mortality indicator equal to 0 if a beneficiary was alive during the entire week and is equal to 1 if the beneficiary died in a given week. The week in which Hurricane Katrina struck New Orleans is labeled 0 on the horizontal axis (this week begins on Monday, August 29, 2005). The gray dashed line indicates the week of FEMA’s “look-and-leave”/“look-and-stay” announcement date (December 9, 2005). Standard errors are clustered by beneficiary baseline zip code. Coefficients and confidence intervals have been scaled by 1,000 to reflect changes in deaths per 1,000 beneficiaries. See online Appendix Table A.3 for numerical values of a subset of the statistics plotted here.
Perhaps unsurprisingly, mortality increases were heavily concentrated in the week of Hurricane Katrina. That week, the New Orleans cohort’s mortality increased by 4.27 deaths per 1,000 (0.427 percentage points), which can account for over three-quarters of the excess 2005 mortality we identify later in our annual analysis. Relative to the sample average of 1.01 deaths per 1,000 beneficiaries, the mortality rate more than quintupled in the week of Katrina. Statistically significant mortality increases persisted as long as eight weeks after landfall. While the effects in these eight weeks are about an order of magnitude smaller (0.014–0.056 percentage points) than in the week of the storm, they nonetheless represent large relative mortality increases (14–55 percent). The remaining 57 weeks show a pattern of declining point estimates that, after 30 weeks, are more frequently negative than positive.
B. Long-Run Effects of Hurricane Katrina
Annual Mortality and Relocation.—
Panel A of Figure 3 shows estimated effects of Hurricane Katrina on annual mortality (equation (2), solid black lines) as well as on cumulative mortality (equation (3), dashed lines) for the 2004 Medicare cohort.18 The hurricane increased mortality in 2005 by 0.56 percentage points (over 10 percent of the mean), which is particularly large given that these additional deaths occurred in the last four months of the year. Remarkably, this initial mortality increase quickly reversed and became a mortality reduction: in 2006, the death rate fell below pre-Katrina levels and remained depressed by at least 0.25 percentage points each year through 2013 (all estimates after 2006 are statistically significant at the 5 percent level). The decrease in the mortality rate was approximately constant over time in absolute terms, corresponding to a declining relative effect as the cohort’s mortality rate grew (see Figure 1).
Figure 3.
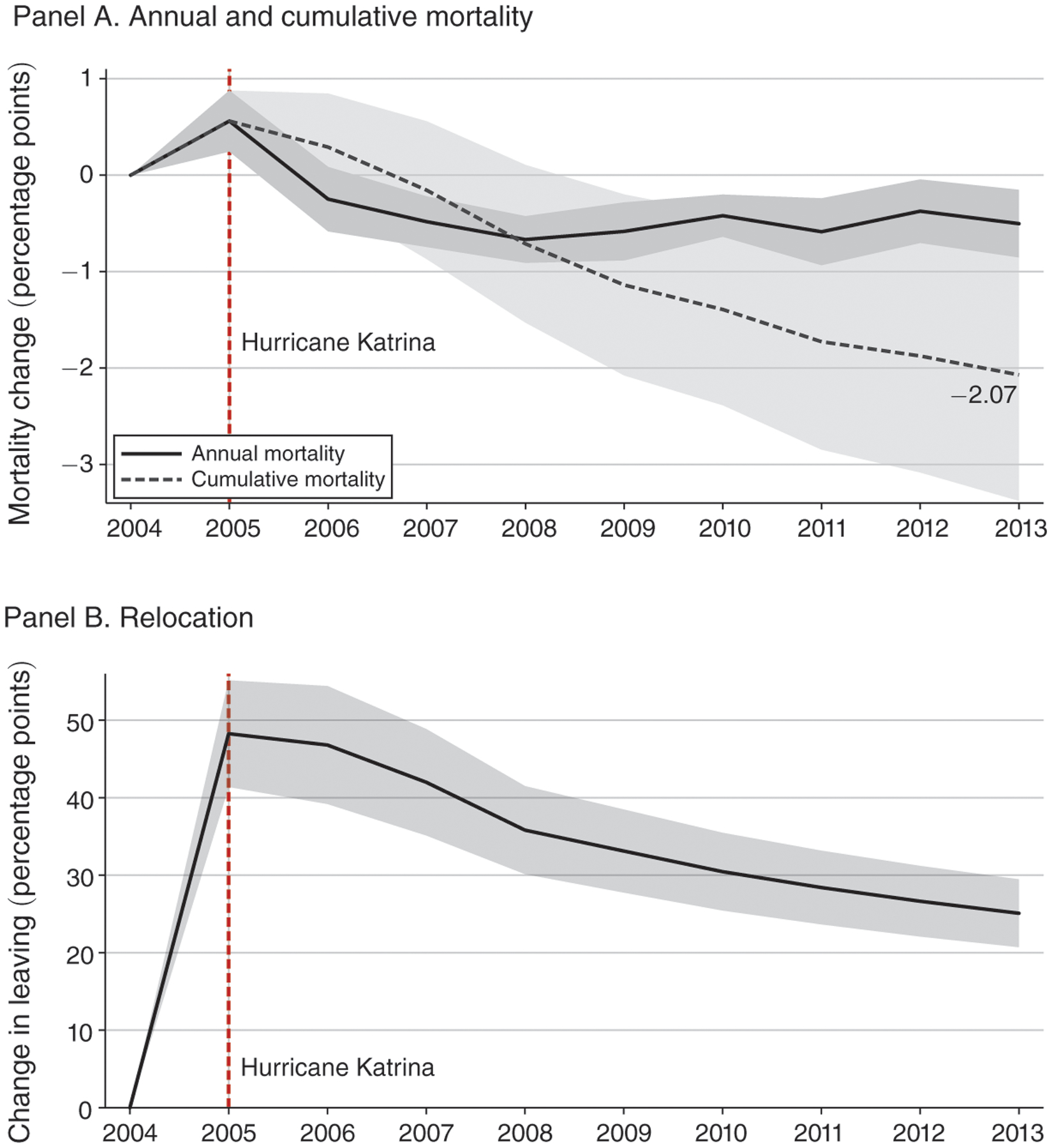
Long-Run Effects of Hurricane Katrina (2004 Medicare Cohort)
Notes: The figure shows estimates of changes in the probability that an individual dies (panel A) or is living outside of their 2004 CZ of residence (panel B). The black solid lines reflect estimates from equation (2). The dashed line in panel A tracks the implied changes in cumulative mortality probability (equation (3)). The gray shaded areas represent 95 percent confidence intervals based on standard errors that are clustered by beneficiary baseline zip code. Section IIIB defines the dependent variables. Coefficients and confidence intervals have been scaled by 100 to reflect changes in percentage points. Online Appendix Table A.4 reports numerical values of these point estimates and their standard errors along with the empirical survival rate of the 2004 New Orleans cohort.
After an initial increase in 2005, changes in cumulative mortality (dashed lines) fell and became negative by 2007, indicating that mortality displacement can explain, at most, two years of post-Katrina mortality reductions. The change in cumulative mortality became increasingly negative throughout the post-Katrina period: the cumulative share of the 2004 New Orleans cohort dying by 2013, the end of the sample period, was 2.07 percentage points lower than if their mortality rates had trended in parallel with the control group. Relative to the 64 percent survival rate of the 2004 cohort over this time period, a decrease in cumulative mortality of 2.07 percentage points represents a survival improvement of 3.2 percent.
Using a value of $150,000 (2017 dollars) per life-year (Cutler and Richardson 1999) and a discount rate of 3 percent (Siegel 1992), we calculate that the net present value of the changes in cumulative mortality brought about by Hurricane Katrina over the period 2005–2013 is $10,114 per capita ($12,345 per capita without discounting). Because the cumulative mortality reduction likely persisted beyond 2013, this figure plausibly provides a lower bound on the value of the mortality reduction. For our sample of 62,094 elderly and long-term disabled victims from the 2004 New Orleans cohort who were alive as of January 1, 2005, the implied aggregate value of the mortality changes over the period 2005–2013 is about $628 million ($767 million without discounting). Because Hurricane Katrina had other negative consequences, improved mortality outcomes do not imply that the storm increased victims’ aggregate welfare.
Finally, panel B of Figure 3 shows the effect of Hurricane Katrina on Medicare beneficiaries’ long-run relocation. In 2005, Hurricane Katrina displaced about 48 percentage points more New Orleans victims than would have otherwise left, and most of the displaced stayed away in 2006. They began returning slowly in 2007; however, by 2013, those from the New Orleans cohort who were alive remained about 25 percentage points less likely to be living in their baseline CZ than were individuals from the control city cohorts. Thus, a large share of New Orleans elderly and long-term disabled left the city after Hurricane Katrina and never returned. These estimates of cohort-level migration responses to Hurricane Katrina over time complement recent evidence on the effect of natural disasters on county-level net migration (Strobl 2011, Deryugina 2017, Boustan et al. 2017).
Robustness.—
By construction, individuals in the 2004 Medicare cohort were alive on January 1, 2004, so we use earlier cohorts to compare pre-Katrina mortality trends of New Orleans and the control city cohorts. In Figure 4, we re-estimate equation (2) using the 1992 and 1999 Medicare cohorts.19 For both cohorts, mortality trends are similar between the New Orleans and control city cohorts, with no statistically significant differences. The post-Katrina differences in mortality rates are also broadly similar across the cohorts.20
Figure 4.
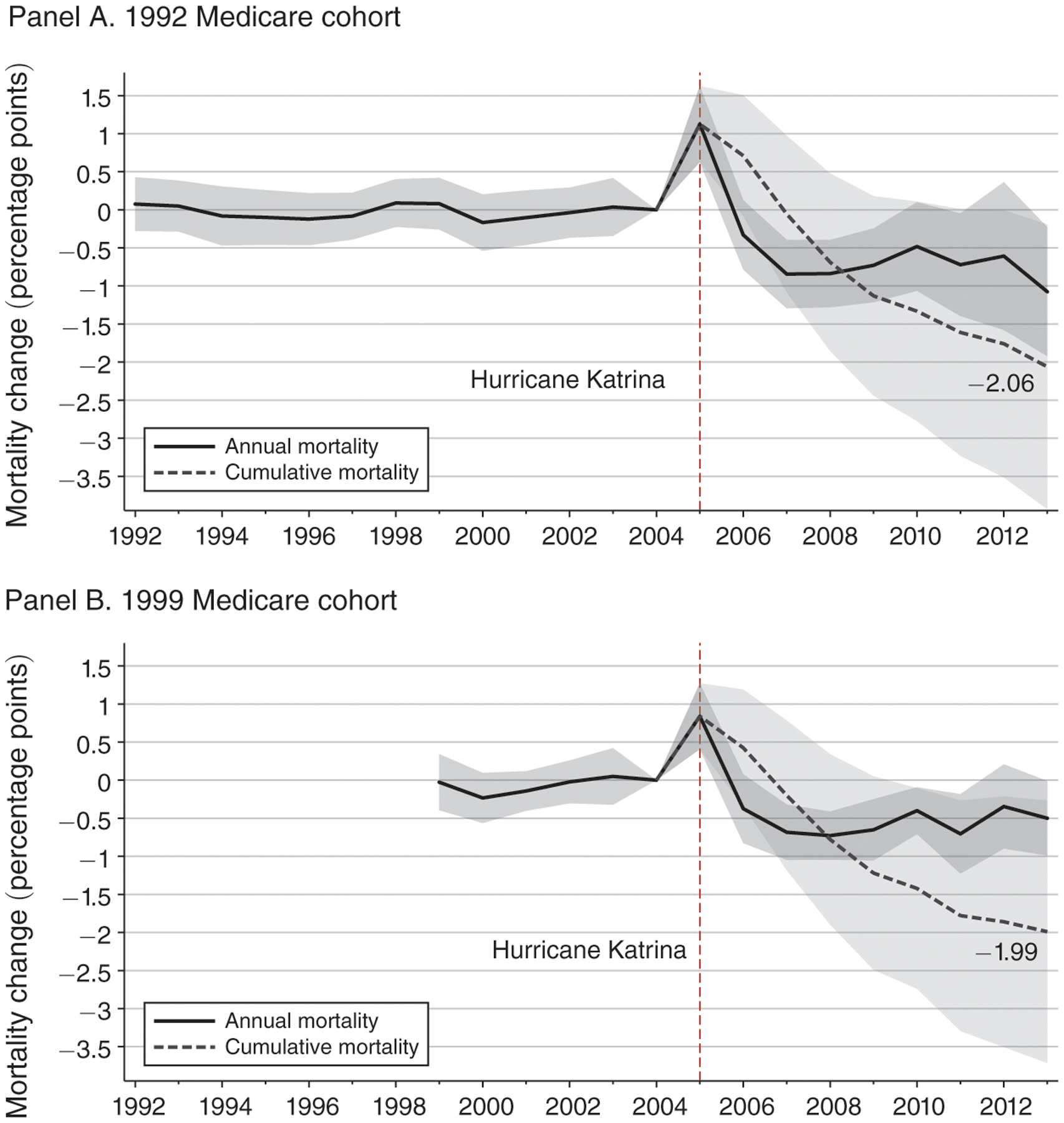
Long-Run Mortality Effects of Hurricane Katrina (Earlier Medicare Cohorts)
Notes: The figure shows estimates and 95 percent confidence intervals from equation (2) for the Medicare cohort indicated below each panel. The dependent variable is a mortality indicator equal to 0 if a beneficiary was alive during the entire year and is equal to 1 if the beneficiary died in a given year. Standard errors are clustered by beneficiary baseline zip code. Coefficients and confidence intervals have been scaled by 100 to reflect changes in percentage points. Online Appendix Table A.5 reports numerical values of these point estimates and their standard errors.
Our results are also robust to including detailed demographic controls (online Appendix Figure A.7); estimating a proportional hazard model version of equation (2) (online Appendix Figure A.8); using the rest of the United States as the control group (online Appendix Figure A.9); and re-estimating the mortality effects of Hurricane Katrina for the 1999 cohort using the synthetic control method of Abadie, Diamond, and Hainmueller (2010, 2015) (online Appendix Figures A.10 and A.11). These robustness checks are described in more detail in online Appendix Section A.2.1.
Concise Difference-in-Differences.—
Table 2 shows mortality estimates from equation (4) for the 2004 cohort (columns 1–3) and the 1999 cohort (columns 4–6). In addition to our preferred specification (columns 1 and 4, labeled A), we also show results that additionally control for every possible combination of one-year age bins, sex, and race (labeled B) and where we further allow the year fixed effects to vary by each one-year age bin, sex, and race combination (labeled C).
Table 2—
Concise Mortality Difference-in-Differences Estimates
| 2004 cohort | 1999 cohort | |||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| 2005 × New Orleans | 0.56 (0.16) | 0.55 (0.16) | 0.56 (0.16) | 0.91 (0.18) | 0.91 (0.19) | 1.00 (0.15) |
| (2006–2013) × New Orleans | −0.48 (0.12) | −0.49 (0.14) | −0.36 (0.11) | −0.49 (0.14) | −0.48 (0.17) | −0.23 (0.09) |
| Included controls | A | B | C | A | B | C |
| Dependent variable mean Observations | 5.55 7,987,100 |
5.55 7,987,100 |
5.55 7,986,926 |
6.31 10,470,949 |
6.31 10,470,949 |
6.31 10,470,692 |
Notes: The table reports difference-in-differences estimates of equation (4) based on the 2004 cohort (columns 1–3) and the 1999 cohort (columns 4–6). The dependent variable is a mortality indicator equal to 0 if a beneficiary was alive during the entire calendar year and is equal to 1 if the beneficiary died in a given year. Coefficients, standard errors (in parentheses), and the dependent variable mean have been scaled by 100. Controls are as follows: A includes baseline zip code and year fixed effects; B also includes fixed effects for each age (one-year bins), race, and sex combination. C additionally controls for age-race-sex effects by year. Standard errors are clustered by beneficiary baseline zip code.
Overall, the point estimates remain stable across control specifications and are similar in magnitude to those obtained in the event study but are more precisely estimated. The estimated initial (2005) mortality increase for the 2004 cohort is 0.55–0.56 percentage points. In 2006–2013, the 2004 New Orleans cohort experienced a statistically significant mortality rate decline of 0.36–0.49 percentage points. The 1999 New Orleans cohort likewise experienced a short-run mortality rate increase, with an estimated magnitude ranging from 0.91 to 1.00 percentage points across control specifications. In the longer run, annual mortality declined by 0.23–0.49 percentage points.
Heterogeneous Treatment Effects.—
The cohort-level mortality effects presented above could mask heterogeneity in Hurricane Katrina’s effects across subpopulations of victims. We estimate the annual event study specification in equation (2) separately by gender, race, and age group for the 1992 and 2004 cohorts (see online Appendix Figure A.12). We find no evidence of differential pre-Katrina mortality trends for any group, further reinforcing the validity of our counterfactual. The initial effect of Hurricane Katrina on mortality was larger for those aged 65 and older, non-Black individuals, and men, but the mortality declines in 2006–2013 were similar for each group, supporting our decision to combine them in our main analyses.
To more concisely estimate heterogeneous treatment effects along these and other dimensions, including the extent of flooding in one’s neighborhood and preexisting chronic conditions, we also augment equation (4) to include interactions between the treatment indicators and an indicator for the characteristic of interest. We describe this specification in more detail in online Appendix Section A.2.1 and present the results in online Appendix Table A.6. We find that long-term mortality reductions following Hurricane Katrina do not appear to be limited to narrow subsets of New Orleans victims. Even individuals that seemed more vulnerable ex ante, such as those with chronic conditions, did not experience increases in long-run mortality, and the long-run survival gains for low-income individuals were statistically larger than those for higher-income individuals.
C. Migration and Place Effects
Thus far, we have shown that Hurricane Katrina led to significant declines in long-run mortality among the elderly and long-term disabled. This result, in isolation, is counterintuitive, as natural disasters are unlikely to have positive direct effects on health. A natural hypothesis, then, is that the mortality improvements following Hurricane Katrina came about indirectly, through other effects of the hurricane. Such indirect benefits of Hurricane Katrina have been demonstrated in other contexts including higher earnings among the working-age population (Deryugina, Kawano, and Levitt 2018) and improved test scores among displaced students (Sacerdote 2012). In this section, we explore the hypothesis that Hurricane Katrina may have increased long-run survival rates by causing elderly and long-term disabled individuals to move to areas more conducive to good health.21
The elderly and long-term disabled mortality rate in New Orleans was among the highest in the country prior to Hurricane Katrina, and individuals displaced by the storm generally relocated to places with better health outcomes. To the extent that regional mortality differences reflect causal effects of place, migrant health may have improved as a result of the move. To examine the effect of place on mortality outcomes, we focus on individuals who were displaced by the hurricane and relate their mortality outcomes to the local mortality rate of the region they moved to, as outlined in Section IIIC and captured by equation (5).
Determinants of Migration.—
The relationship in equation (5) reflects the causal effect of place, as captured by mortality rates, on individual mortality under the assumption that baseline mortality risk among those who move is uncorrelated with mortality rates in the destination region. This identification assumption would be violated if migrants with lower latent mortality risk systematically sort to destinations with different mortality rates.
As a direct test of differential sorting, we estimate how migrants’ predicted mortality risk varies with the local mortality of the county to which they move. To predict mortality risk, we model the relationship between mortality and baseline (2004) characteristics Xi,2004 as
We estimate this model using the 2004 control county cohorts over the period 2006–2013. The fitted model is then used to generate out-of-sample mortality predictions, PredictedMortalityi, for individuals in the 2004 New Orleans cohort, providing a time-invariant index of an individual’s ex ante mortality risk over the period 2006–2013. Our preferred set of predictors Xi,2004, described below, yields mortality predictions that are strongly correlated with realized mortality among the New Orleans movers (see online Appendix Figure A.14).
To test whether migrants’ predicted mortality risk is correlated with the local mortality of the county they move to, we estimate the following regression:
| (6) |
where MDR2006C(i) is the mortality rate in migrant i’s destination county, as in equation (5). We estimate equation (6) using one observation per mover from the 2004 New Orleans cohort.
Table 3 reports the results of estimating equation (6) using increasingly rich sets of baseline characteristics Xi,2004 to generate migrants’ predicted mortality risk. When mortality risk is predicted using demographics alone (all possible one-year age, race, and sex combinations), the relationship between predicted mortality and destination mortality is a small and statistically insignificant (column 1). However, when augmenting the mortality predictors to also include indicators for ESRD, eight chronic condition groups, and ventiles of health care spending at baseline (our preferred set of predictors), the coefficient on predicted mortality remains small but becomes statistically significant at the 5 percent level.
Table 3—
Correlation between ex ante Predicted Mortality and Destination Mortality (New Orleans Movers)
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Predicted mortality | 0.0007 (0.0009) | 0.0016 (0.0008) | 0.0004 (0.0009) | 0.0004 (0.0008) | 0.0006 (0.0008) |
| Alzheimer’s / dementia dropped | No | No | Yes | Yes | Yes |
| Two-way | |||||
| Chronic conditions predictors | None | Grouped | Grouped | interactions | Individual |
| Baseline spending predictors | None | Ventiles | Ventiles | Ventiles | Centiles |
| Dependent variable mean | 5.40 | 5.40 | 5.39 | 5.39 | 5.39 |
| Observations | 26,467 | 12,319 | 11,268 | 11,268 | 11,268 |
Notes: The table reports the results of estimating equation (6) using increasingly rich sets of baseline characteristics to generate migrants’ predicted mortality risk. The dependent variable is the average 2006–2013 mortality rate of the destination county’s 2004 cohort. All regressions control for baseline zip code fixed effects. Both predicted mortality and destination mortality are expressed in percentage points. Standard errors (in parentheses) are clustered by each beneficiary’s 2006 county.
Online Appendix Table A.7, which reports the relationship between destination mortality and Xi,2004 directly (i.e., without combining the characteristics into a mortality risk measure), suggests that this relationship is driven by a small number of individuals with Alzheimer’s/dementia who have high predicted mortality risk and who move to higher-mortality areas. When we exclude these individuals from the sample (column 3), the estimated relationship between predicted mortality and destination mortality ceases to be statistically significant and the magnitude of the coefficient falls nearly to 0. For this sample, the coefficient remains small and statistically insignificant even when enriching mortality predictors to include all two-way interactions between chronic condition groups (column 4) or when replacing grouped chronic conditions and spending ventiles with all available 27 chronic condition indicators and centiles of baseline spending (column 5).22
The limited degree of sorting on observable mortality risk supports the assumption that the underlying mortality risk of New Orleans migrants was unrelated to destination mortality, especially among those without Alzheimer’s/dementia. As a second test of this assumption, we report in the next section how estimates of the relationship between mover mortality and destination region mortality rates change when using increasingly comprehensive controls and when restricting the movers sample to those without Alzheimer’s/dementia.
Movers’ Mortality and Local Mortality.—
Table 4 reports how movers’ 2006–2013 mortality varies with the mortality rate in their destination county (equation (5)). Column 1 reports effects for the full movers sample when controlling only for baseline zip code and year fixed effects. The results show that each percentage point reduction in the destination mortality rate corresponds to a 0.85 percentage point reduction in the mortality rate of New Orleans migrants who had relocated to that region by 2006. Because many beneficiaries who left New Orleans after Hurricane Katrina eventually returned (Figure 3, panel B), the relationship between local mortality and movers’ subsequent mortality should be interpreted as an intent-to-treat estimate.23
Table 4—
Migrant Mortality by Destination Mortality (New Orleans Movers)
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Mean death rate in 2006 county | 0.85 (0.29) | 0.83 (0.23) | 0.86 (0.23) | 1.01 (0.30) | 0.94 (0.29) | 0.98 (0.29) |
| Set of fixed effects | A | B | C | C | C | C |
| Alzheimer’s / dementia dropped | No | No | No | No | Yes | Yes |
| Chronic conditions controls | No | No | No | Gr. | Gr. | All int. |
| Dependent variable mean | 5.55 | 5.55 | 5.54 | 6.11 | 5.48 | 5.47 |
| Observations | 175,936 | 175,936 | 175,821 | 80,084 | 75,142 | 75,137 |
| R2 | 0.00 | 0.04 | 0.05 | 0.09 | 0.08 | 0.08 |
Notes: The table reports estimates of equation (5). The dependent variable is a mortality indicator equal to 0 if a beneficiary was alive during the entire calendar year and is equal to 1 if the beneficiary died in a given year. Coefficients, standard errors (in parentheses), and dependent variable mean have been scaled by 100. Controls are as follows: A includes baseline zip code and year fixed effects; B also includes fixed effects for each age (one-year bins), race, and sex combination. C additionally controls for age-race-sex effects by year. Gr. means that indicators for eight groups of chronic conditions are included; All int. means that indicators for each possible interaction of the eight groups of chronic conditions are included. All specifications that include chronic condition controls also include fixed effects for centiles of baseline Medicare spending. Standard errors are clustered by each beneficiary’s 2006 county.
Columns 2–6 of Table 4 show the results of estimating equation (5) using increasingly comprehensive controls for baseline demographics and chronic conditions. Whenever we control for chronic conditions, which restricts us to a subset of fee-for-service beneficiaries, we also include fixed effects for centiles of beneficiaries’ 2004 Medicare spending. The estimated coefficient on destination mortality changes little across these specifications, ranging from 0.83 to 1.01. Importantly, excluding beneficiaries with Alzheimer’s/dementia (columns 5 and 6) yields similar results to estimates that include those individuals (column 4). The stability of this estimate across the various sets of controls further suggests that significant migrant sorting on latent mortality risk is unlikely in our context.
The results reported in Table 4 are robust to controlling for the 27 individual chronic condition indicators, controlling for move distance, and excluding individuals who moved to Houston or Baton Rouge, the two most common destinations for New Orleans movers (online Appendix Table A.10); using an indicator for death by the end of 2013 as the outcome, thus capturing cumulative mortality (online Appendix Table A.11); and constructing the movers sample based on where individuals lived as of March 2007 to exclude short-term moves and include moves that had not been reported by the beneficiary until later in 2006 (online Appendix Table A.12). We discuss these robustness checks in more detail in online Appendix Section A.2.3.
Figure 5 shows a graphical representation of the results in column 5 of Table 4. Specifically, we residualize destination county mortality by the fixed effects included in each regression and bin observations by centile of the resulting residuals, yielding 100 groups. For each centile, we plot movers’ mean residualized mortality (black circles) and mean residualized predicted mortality (green squares), with the sample means added for interpretability. The resulting relationship between local mortality and movers’ subsequent mortality reflects a general upward trend, demonstrating that the findings in Table 4 are not driven by a few outliers. The relationship between destination mortality and movers’ ex ante predicted mortality appears to be flat, supporting the absence of mover sorting on this dimension.
Figure 5.
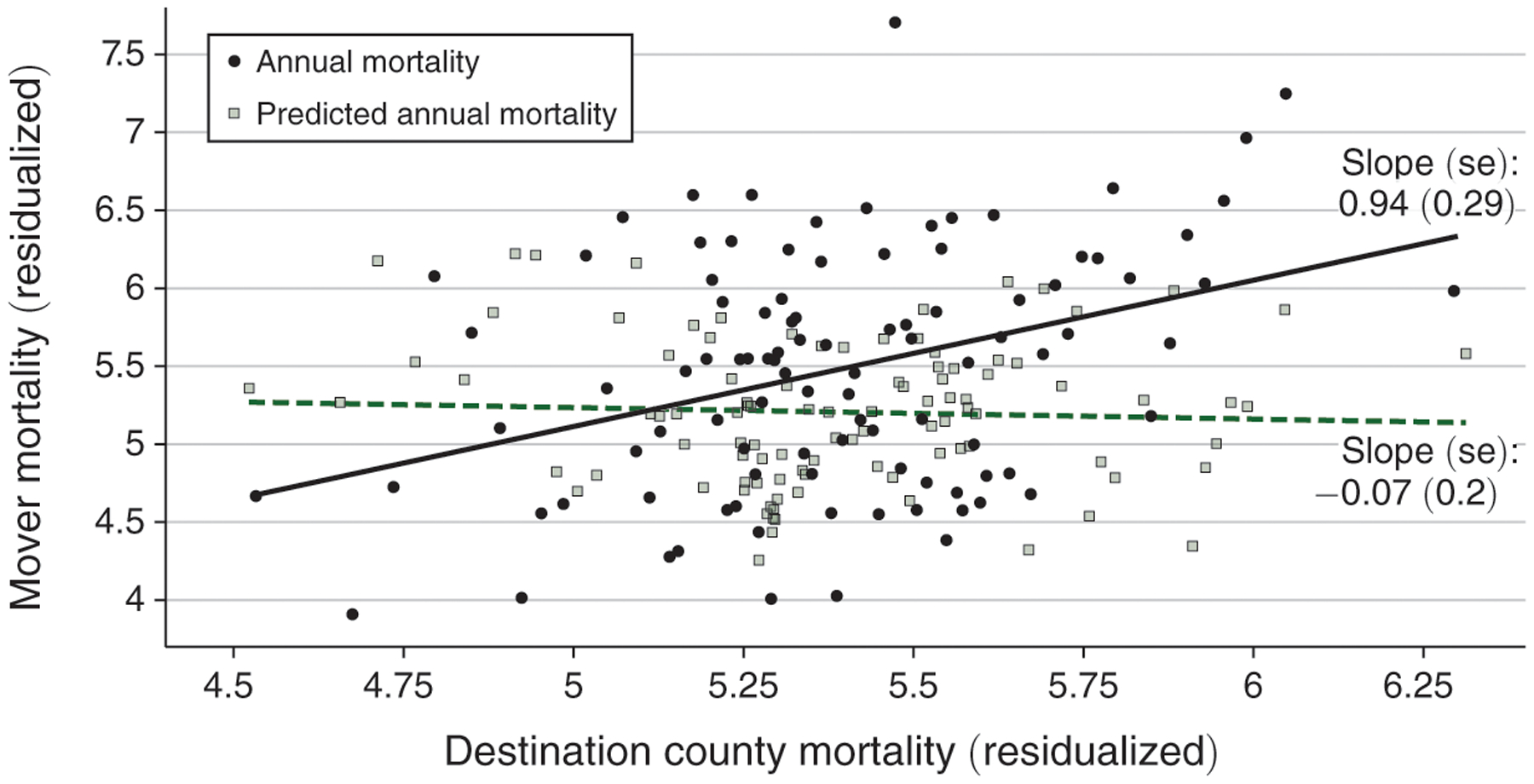
Mover Mortality by Destination Mortality
Notes: The figure shows a graphical representation of the results in column 5 of Table 4, which describes how movers’ realized mortality rates relate to the local mortality of their destination county (solid black line). The figure also shows how movers’ ex ante predicted mortality rates relate to the local mortality of their destination county (dashed green line). For each outcome, the outcome and destination county mortality are residualized by partialing out the fixed effects included in their respective regression and then adding sample means for interpretability. For each centile of residualized destination county mortality, the plot shows movers’ mean residualized mortality (black circles) and mean residualized predicted mortality (green squares).
To shed additional light on how place shapes health outcomes, we explore heterogeneity in our baseline results. Online Appendix Table A.13 shows that movers’ mortality rates reflect the local mortality rate as early as 2006–2007, suggesting that faster-moving channels like the quality of local health care delivery or other environmental factors drive the place effects we estimate, rather than slower-moving channels like the development of chronic conditions. Related to this hypothesis, we find that cardiovascular and other internal causes of death are statistically significantly associated with the destination mortality rate, but not cancer and external causes of death (see online Appendix Table A.14). Online Appendix Table A.15 shows that a mover’s mortality is more correlated with the local mortality of beneficiaries of his/her race (Black or not Black) and with the local mortality of his/her age group (65 or older versus 64 or younger), while gender-specific estimates are inconclusive. Finally, online Appendix Table A.16 relates movers’ mortality to destination zip code, county, and CZ mortality and shows that movers’ mortality is more strongly associated county mortality when considered jointly with zip or CZ mortality. These heterogeneity results are described in more detail in online Appendix Section A.2.3.
Movers’ Mortality and Other Local Characteristics.—
Next, we examine how movers’ mortality rates vary with other attributes of the destination county, including health behaviors, health care supply and quality, the environment, income and income mobility, crime, urbanicity, and social capital. The full set of 21 attributes is summarized in online Appendix Table A.17, where we display the median, tenth percentile, and ninetieth percentile of each destination characteristic, as measured in the 2006 cross-section of New Orleans movers.
To estimate the correlation between movers’ mortality and each of these characteristics, we simply replace the local mortality rate in equation (5) with the local characteristic of interest. The correlation reflects the causal mortality effect of place, as captured by the local characteristic, under the assumption that migrants’ baseline mortality risk is uncorrelated with the destination characteristic. Even if this assumption holds, we emphasize that the estimate reflects the causal effect of the given characteristic itself only if the characteristic is uncorrelated with any other local attribute that also affects movers’ mortality. Because each region is a bundle of many, often correlated, characteristics, these results should be viewed as suggestive of what actually determines place effects.
Figure 6 reports the results for the no-Alzheimer’s/dementia sample, controlling for zip code and year-by-age-by-race-by-sex fixed effects as well as for eight chronic condition indicators and centiles of baseline spending. Black markers indicate effects when the outcome is Diedit, an indicator for realized mortality. Green markers indicate effects when the outcome is PredictedMortalityi, which evaluates the extent of differential sorting to regions with high or low values of the characteristic by ex ante predicted mortality risk. In the figure, we report standardized mortality effects and 95 percent confidence intervals, constructed by multiplying coefficients and confidence intervals by the interdecile range of each characteristic.24 Thus, each estimate can be interpreted as the change in actual or predicted mortality when moving from a place in the tenth to a place in the ninetieth percentile of a characteristic’s distribution in the movers sample.
Figure 6.
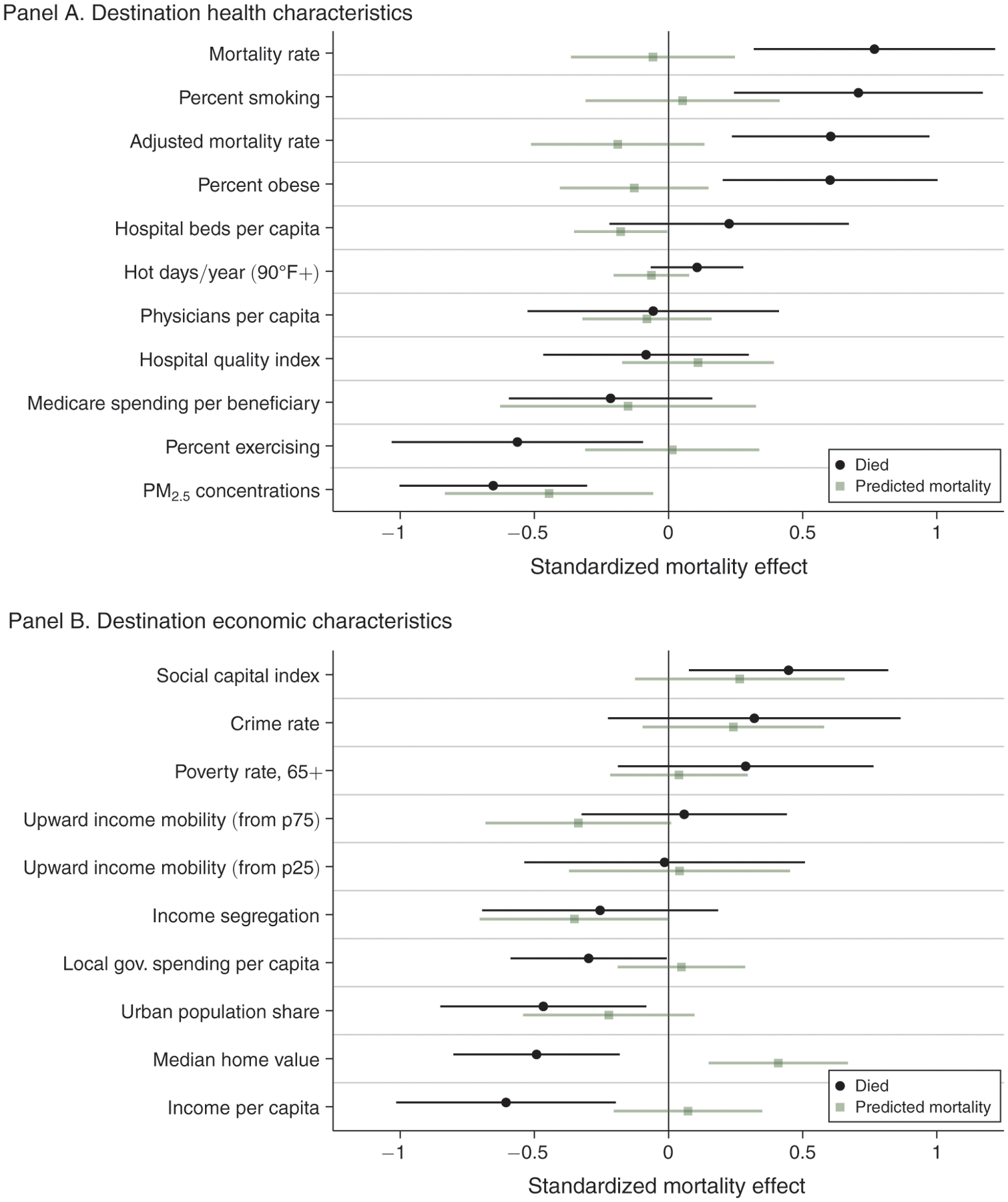
Mover Mortality by Destination Characteristic
Notes: The figure shows estimates and 95 percent confidence intervals of how realized and ex ante predicted mortality rates of movers relate to the local characteristics of the counties to which they moved. The standardized mortality effect reflects the effect of an interdecile range change in the local characteristic reported in the row, based on the tenth and ninetieth percentiles of the local characteristic exposure among movers. Numerical values of the point estimates and standard errors for the Died and Predicted mortality outcomes are reported in columns 1 and 4, respectively, of online Appendix Tables A.18 and A.19. Online Appendix Table A.17 reports summary statistics for each of the destination characteristics. See notes to online Appendix Table A.18 for additional details about the sample and controls.
Across all local health characteristics we consider (Figure 6, panel A), the estimated standardized mortality effect is largest for the local mortality rate: moving to a region in the tenth versus the ninetieth percentile of local mortality corresponds to a 0.76 percentage point decrease in realized mortality. The estimate is similar when we adjust the local mortality rate to account for the demographics of local residents, which we construct by demeaning raw mortality by interactions of one-year age, race, and sex. Migrants’ mortality is also higher in places with higher rates of smoking, higher rates of obesity, or lower rates of exercise. We find small and statistically insignificant relationships between movers’ mortality and the number of hospital beds per capita, the frequency of extremely hot days, the number of MDs per capita, an index of hospital quality, or average medical spending. Surprisingly, moving to areas with more air pollution, as measured by PM2.5, is associated with a lower subsequent mortality rate. However, in contrast with the other local health characteristics, this correlation can largely be explained by sorting of ex ante healthier individuals into more polluted areas.
Our analysis of movers’ mortality and local health care spending sheds new light on a long-standing question of whether higher-spending regions generate better health outcomes than lower-spending regions. Higher-spending regions often have no better or even worse health outcomes than lower-spending regions, suggesting that the returns to additional medical spending may be low (e.g., Fisher, Bynum, and Skinner 2009; Cutler 2010; Skinner and Fisher 2010). However, higher spending could be partly due to worse population health, which could result in a net zero or even positive correlation between local spending and local mortality even if the returns to living in a higher-spending region are positive. Our focus on movers allows us to sidestep this concern, and our results indicate that the return to living in a high-spending region is low.
Low returns to living in a high-spending area need not imply low returns to additional medical spending: it depends on the extent to which differences in local health care spending reflect differences in spending among the migrants themselves. We therefore estimate the relationship between the average spending in destination counties and movers’ own subsequent spending. For this analysis, we restrict the sample to New Orleans residents who were enrolled in fee-for-service Medicare for all 12 months of 2004 and only consider post-2006 spending in years in which they were enrolled in fee-for-service for all 12 months. As reported in online Appendix Table A.20, we find that a mover’s spending increases by $0.61–$0.93 for each $1 increase in average local spending, estimates that are broadly consistent with those of Finkelstein, Gentzkow, and Williams (2016).
Our estimates of the spending and mortality effects of moving to a higher-spending region can be combined in a back-of-the-envelope fashion to derive an implied cost of saving one life-year. Because we do not find a statistically significant relationship between destination spending and movers’ mortality, we focus on deriving the lowest cost that is not ruled out by our estimates. We start with our smallest estimate of the effect of an interdecile range increase in destination medical spending (about a $4,000 increase) on a mover’s own spending (0.61 × $4,000). We divide the result by the lower bound of the 95 percent confidence interval of the estimated annual mortality effect (− 0.21 − 1.96 × 0.19 percentage points). This calculation implies that we can rule out costs of less than $420,000 to save one life-year.
Figure 6, panel B reports how migrant mortality varies with local economic conditions. Migrants to higher-income areas, areas with higher housing prices, more urban areas, or areas with higher local government spending per capita subsequently experience lower mortality. Perhaps counterintuitively, movers to areas with higher social capital experience significantly higher mortality, although this could partly reflect ex ante sorting on mortality risk. We do not find statistically significant differences in mortality with respect to local crime, poverty, upward income mobility, or income segregation. While some of these economic characteristics correlate with migrants’ mortality, all of the estimated standardized mortality effects are smaller than that of the local mortality rate.
Discussion.—
We perform a back-of-the-envelope evaluation of the extent to which migration can account for the average mortality decline among the New Orleans cohort in 2006–2013 (Table 2). The 2005–2006 local mortality change experienced by surviving Hurricane Katrina victims averages −0.31 percentage points (−0.39 of the interquartile range), including individuals who remained in New Orleans, for whom the difference is zero.25 Combining our most carefully controlled estimates of the 2006–2013 mortality reduction (−0.36, column 3 of Table 2) with the normalized relationship between local mortality rates and Katrina movers’ own subsequent mortality (0.67, column 2 of Table A.18), we conclude that changes in victims’ local mortality explain 73 percent ((0.67 × 0.39)/0.36) of the average long-run mortality decline caused by the hurricane.
There are a number of factors that may explain the remaining 27 percent of the 2006–2013 mortality decline. First, some of the long-run mortality decline following Hurricane Katrina may be driven by variation in other destination characteristics that is orthogonal to the local mortality rate. However, we find that additionally considering non-mortality destination characteristics that are individually large and significant predictors of movers’ mortality (e.g., the local smoking rate) do not systematically increase the share of the mortality decrease that we can explain (see online Appendix Table A.21 and additional discussion in online Appendix Section A.2.3).
Second, some of the mortality decline may reflect mortality displacement, although our cumulative mortality results show that harvesting cannot explain the persistent mortality reduction. Third, the mortality decline may be due in part to effects that were uncorrelated with whether or where victims moved. For example, the disaster may have increased resilience among the elderly and long-term disabled (Adams et al. 2011). Fourth, it is possible that earnings gains experienced by Hurricane Katrina victims (Groen, Kutzbach, and Polivka 2020; Deryugina, Kawano, and Levitt 2018) contributed to mortality improvements, although it should be noted that our sample consists mainly of retired and disabled individuals, making this channel less likely.
Fifth, elderly and long-term disabled victims may have become more likely to move in with, or closer to, relatives. This mechanism is difficult to evaluate with existing data, but to the extent that the propensity to move in with relatives is uncorrelated with local mortality, its presence should not affect our conclusion.26 Finally, some of the long-run mortality decline following Hurricane Katrina may be driven by where people move but may be based on local factors that are uncorrelated with the attributes we considered in our analysis.
The finding that destination mortality explains much of the estimated mortality effect among Medicare victims of Hurricane Katrina suggests that the mortality declines in panel A of Figures 1 and 3 would have been even larger had more victims left New Orleans or had fewer returned. Because the hurricane disproportionately displaced vulnerable individuals, including those with higher medical spending or living in low-income neighborhoods (online Appendix Table A.7), one possible explanation for this large effect is that place effects may be larger for this subpopulation than for healthier individuals. A related possibility is that place may have a larger impact for Black individuals, who made up a large share of the New Orleans victims and were also disproportionately likely to move after the hurricane, than for other races. Finally, it may be that place effects are particularly large in our sample of destinations, which, for example, tend to be more urban than the average US location.
V. Conclusion
Hurricane Katrina devastated New Orleans and other parts of the Gulf Coast, causing billions of dollars’ worth of direct damage and displacing over one million individuals from their homes. However, the hurricane appears to have come with a silver lining: the elderly and long-term disabled living in New Orleans at the time of the hurricane experienced reductions in long-run mortality. Our analysis suggests that relocation to areas with better mortality outcomes can explain about 70 percent of the post-Katrina mortality decline among the elderly and long-term disabled. Migrants’ mortality is also lower in destinations with healthier behaviors and higher incomes but is unrelated to local medical spending and quality.
While we find that Hurricane Katrina reduced long-run mortality rates, these effects do not necessarily imply that individuals’ welfare increased, as the destruction of physical assets and lost utility due to displacement may have more than offset any indirect benefits of the hurricane. We estimate that changes in mortality due to the hurricane, inclusive of the initial mortality shock, are worth about $10,000 per capita. Given that moving costs have been estimated to be as high as $300,000 for some populations (Kennan and Walker 2010), New Orleans residents may not have voluntarily relocated for these mortality benefits alone.
Our paper provides novel evidence that one’s location of residence has a causal effect on mortality, adding to a growing body of work on the importance of place for shaping individual choices and well-being. The speed with which movers’ mortality rates respond to the local mortality rate also suggests that health capital may accumulate or depreciate more rapidly than the canonical model of Grossman (1972) implies, at least for the population in our study. Finally, we estimate the effect of a natural disaster on long-run mortality, something that data challenges have hindered in the past. Our conclusion that Hurricane Katrina reduced mortality by inducing relocation demonstrates the importance of accounting for migration and local conditions when projecting the long-run impacts of disasters.
Supplementary Material
Footnotes
Go to https://doi.org/10.1257/aer.20181026 to visit the article page for additional materials and author disclosure statements.
As we show, our central findings are robust to using the entire United States (except New Orleans) or the top 20 mortality regions to define the comparison cohort and to using the synthetic control method to conduct inference that accounts for the aggregate nature of the shock created by Hurricane Katrina.
Higher-spending regions often have no better or even worse health outcomes than lower-spending regions (Fisher et al. 2003a, b; Baicker and Chandra 2004; Sirovich et al. 2006; Skinner 2011), but the direction of causality is not clear from these correlations alone. Doyle (2011) and Doyle et al. (2015) address this limitation by analyzing quasi-random assignment of patients to hospitals and find that patients have better outcomes when treated at higher-spending hospitals. Yet, the returns to being hospitalized in a high-spending region may differ from the returns to living in a high-spending region (e.g., higher-quality health systems could reduce the need for hospitalization).
See, for example, Armenian, Melkonian, and Hovanesian (1998); Sastry and VanLandingham (2009); Rhodes et al. (2010); Adams et al. (2011); Adeola and Picou (2012); Pietrzak et al. (2012).
Residents in 17 out of 19 New Orleans zip codes were not allowed to return to their homes before December 9, 2005 (FEMA 2005). On that date, residents of 10 of the 17 zip codes could return to their homes and stay (“look-and-stay” zip codes); residents in the other 7 zip codes could visit their homes but only during the day (“look-and-leave” zip codes).
Peter Grier, “The Great Katrina Migration,” Christian Science Monitor, September 12, 2005, https://www.csmonitor.com/2005/0912/p01s01-ussc.html.
Deryugina, Kawano, and Levitt (2018) describe Hurricane Katrina aid components in greater detail.
Several studies have found deteriorated mental and physical health among Hurricane Katrina victims, but these studies generally lack a control group to account for secular trends, most lack outcomes measured pre-Katrina, and almost all have focused on short-run effects (see, e.g., Brodie et al. 2006, Kessler et al. 2008, Sastry and VanLandingham 2009, Sastry and Gregory 2013). In the only longer-run study we are aware of, Paxson et al. (2012) follow 532 low-income mothers who lived in New Orleans during Hurricane Katrina and find long-lasting increases in post-traumatic stress symptoms and psychological distress.
We drop individuals who disappear from the annual beneficiary summary file prior to a recorded death or who have gaps in enrollment. For the 2004 cohort, these restrictions drop 0.8 percent of the full sample.
Online Appendix Section A.1 provides additional details on these data and the definitions of key variables used in our analysis, including beneficiary location, chronic conditions, and cause of death.
We use GeoLytics to geocode nine-digit zip codes. We do not assign flood and income characteristics to the 4.4 percent of sample beneficiaries for whom Medicare only reports a five-digit zip code or to the additional 8.2 percent of sample beneficiaries whose nine-digit zip codes are not geocoded by GeoLytics.
Online Appendix Table A.2 lists raw annual mortality rates for the 1992, 1999, and 2004 New Orleans cohorts and the corresponding control city cohorts. Online Appendix Figure A.4 shows annual death rates for the 1999 Medicare cohort, adjusted for all combinations of beneficiaries’ current age (in one-year bins), race, and sex.
By 2004, 6,600 of the 71,433 individuals (9.2 percent) from the 1992 New Orleans cohort were living outside of New Orleans and 39,500 (55.3 percent) had died. Among the 1999 New Orleans cohort, 5,310 of the 67,649 individuals (7.8 percent) were living outside of New Orleans and 17,434 (25.8 percent) had died by 2004.
Because cumulative mortality converges to 1 for each cohort, any differences in baseline annual mortality rates between the treatment and control cohorts imply that the cumulative mortality rates would not have moved in parallel had treatment not occurred. By contrast, annual mortality risk need not converge or diverge over time. For this reason, we estimate annual mortality effects and use the results to infer changes in cumulative mortality.
To derive equation (3), note that , where is the cohort’s observed survival rate and is the counterfactual survival rate.
In principle, we could let the local mortality rate MDR2006C change each year for individuals who continue moving. However, in our setting, this is problematic because a nontrivial share of our movers return to New Orleans in the longer run. As a result, we would either have to drop these individuals from our sample in those years, which would likely bias the estimates, or use the New Orleans mortality rate, which was clearly affected by Hurricane Katrina.
We measure environmental characteristics over the time period 2006–2013 because these are unlikely to be affected by Hurricane Katrina movers.
Numerical values for a subset of the estimates plotted in Figure 2 are reported in online Appendix Table A.3.
Numerical values of the point estimates and standard errors shown in Figure 3 can be found in online Appendix Table A.4.
Online Appendix Table A.5 reports numerical values of the mortality event study point estimates and standard errors shown in Figure 4. Online Appendix Figure A.6 reports relocation event study estimates for the 1999 cohort.
The 2005 increases in the mortality rate for the 1992 and 1999 New Orleans cohorts are even larger than that of the 2004 cohort. This is likely due to elderly individuals in the former cohorts being at least 77 and 70 years old, respectively, at the time of Hurricane Katrina, which may have made them more susceptible to the disaster’s short-run negative effects than younger Medicare beneficiaries.
Hurricane Katrina may have also generated health benefits through other channels, including quality improvements in New Orleans itself: see, e.g., Linda Marsa, “Top-Notch Community Health Care Emerges in New Orleans from Hurricane Katrina’s Rubble,” USA Today, August 28, 2015. As discussed in online Appendix Section A.2.2, we find no evidence of improvements over time in the health of those who stayed in New Orleans (see online Appendix Figure A.13).
By contrast, online Appendix Table A.8 shows that there is a consistent and strong negative relationship between predicted mortality and the probability of leaving New Orleans in 2005–2006.
A potential difficulty with interpreting the intent-to-treat effect is that the probability of returning to New Orleans could differ across high- and low-mortality destinations. However, online Appendix Table A.9 indicates that this was not the case.
Online Appendix Table A.17 reports the interdecile range of each local characteristic among the movers sample. Online Appendix Tables A.18 and A.19 report the numerical values of coefficients and standard errors graphed in Figure 6, along with the correlation between each local characteristic and the local mortality rate.
To measure the changes in local mortality following Hurricane Katrina, we calculate the difference in mortality between each individual’s 2006 county and the New Orleans county using the 2004 mortality rate of each area’s 2004 cohort. Calculating mortality rate differences over the period 2006–2013 instead of 2004 would adhere most closely to our movers’ regression framework, but the 2006–2013 mortality rate for New Orleans would be confounded by the effects of the hurricane. If counterfactual cohort mortality rates trend in parallel across regions, then differences in 2004 mortality rates provide an unbiased, although perhaps less precise, estimate of longer-run differences.
Between October 2005 and October 2006, the Current Population Survey collected information on Hurricane Katrina evacuees and on whom they were living with. However, the sample size of elderly evacuees (58 individuals in the March 2006 survey) is too small for meaningful statistical inference.
REFERENCES
- Abadie Alberto, Diamond Alexis, and Hainmueller Jens. 2010. “Synthetic Control Methods for Comparative Case Studies: Estimating the Effect of California’s Tobacco Control Program.” Journal of the American Statistical Association 105 (490): 493–505. [Google Scholar]
- Abadie Alberto, Diamond Alexis, and Hainmueller Jens. 2015. “Comparative Politics and the Synthetic Control Method.” American Journal of Political Science 59 (2): 495–510. [Google Scholar]
- Adams Vincanne, Kaufman Sharon R., Van Hattum Taslim, and Moody Sandra. 2011. “Aging Disaster: Mortality, Vulnerability, and Long-Term Recovery among Katrina Survivors.” Medical Anthropology 30 (3): 247–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adeola Francis O., and Picou J. Steven. 2012. “Race, Social Capital, and the Health Impacts of Katrina: Evidence from the Louisiana and Mississippi Gulf Coast.” Human Ecology Review 19 (1): 10–24. [Google Scholar]
- Armenian Haroutune K., Melkonian Arthur K., and Hovanesian Ashot P.. 1998. “Long-Term Mortality and Morbidity Related to Degree of Damage Following the 1988 Earthquake in Armenia.” American Journal of Epidemiology 148 (11): 1077–84. [DOI] [PubMed] [Google Scholar]
- Baicker Katherine, and Chandra Amitabh. 2004. “Medicare Spending, the Physician Workforce, and Beneficiaries’ Quality of Care.” Health Affairs 23 (S1). [DOI] [PubMed] [Google Scholar]
- Beven-II John L., Avila Lixion A., Blake Eric S., Brown Daniel P., Franklin James L., Knabb Richard D., Pasch Richard J., et al. 2008. “Annual Summary–Atlantic Hurricane Season of 2005.” Tropical Prediction Center, NOAAN/NWS/National Hurricane Center. [Google Scholar]
- Black Dan A., Sanders Seth G., Taylor Evan J., and Taylor Lowell J.. 2015. “The Impact of the Great Migration on Mortality of African Americans: Evidence from the Deep South.” American Economic Review 105 (2): 477–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boustan Leah Platt, Kahn Matthew E., Rhode Paul W., and Yanguas Maria Lucia. 2017. “The Effect of Natural Disasters on Economic Activity in US Counties: A Century of Data.” NBER Working Paper 23410. [Google Scholar]
- Brodie Mollyann, Weltzien Erin, Altman Drew, Blendon Robert J., and Benson John M.. 2006. “Experiences of Hurricane Katrina Evacuees in Houston Shelters: Implications for Future Planning.” American Journal of Public Health 96 (8): 1402–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronnenberg Bart J., Dubé Jean-Pierre H., and Gentzkow Matthew. 2012. “The Evolution of Brand Preferences: Evidence from Consumer Migration.” American Economic Review 102 (6): 2472–508. [Google Scholar]
- Centers for Disease Control and Prevention. 1995–2004a. “Behavioral Risk Factor Surveillance System.” https://www.cdc.gov/brfss/annual_data/annual_data.htm (accessed October 1, 2019).
- Centers for Medicare and Medicaid Services. 1992–2013. “CMS Medicare Eligibility and Enrollment Files.” National Bureau of Economic Research; [data host]. http://data.nber.org/medicare (accessed July 13, 2020). [Google Scholar]
- Chetty Raj, Friedman John N., and Saez Emmanuel. 2013. “Using Differences in Knowledge across Neighborhoods to Uncover the Impacts of the EITC on Earnings.” American Economic Review 103 (7): 2683–721. [Google Scholar]
- Chetty Raj, and Hendren Nathaniel. 2018a. “The Impacts of Neighborhoods on Intergenerational Mobility I: Childhood Exposure Effects.” Quarterly Journal of Economics 133 (3): 1107–62. [Google Scholar]
- Chetty Raj, and Hendren Nathaniel. 2018b. “Dataset for: The Impacts of Neighborhoods on Intergenerational Mobility II: County-Level Estimates.” https://opportunityinsights.org/paper/neighbor-hoodsii (accessed July 13, 2020).
- Chetty Raj, Hendren Nathaniel, and Katz Lawrence F.. 2016. “The Effects of Exposure to Better Neighborhoods on Children: New Evidence from the Moving to Opportunity Experiment.” American Economic Review 106 (4): 855–902. [DOI] [PubMed] [Google Scholar]
- Chetty Raj, Stepner Michael, Abraham Sarah, Lin Shelby, Scuderi Benjamin, Turner Nicholas, Bergeron Augustin, et al. 2016. “The Association Between Income and Life Expectancy in the United States, 2001–2014.” JAMA 315 (16): 1750–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chyn Eric. 2018. “Moved to Opportunity: The Long-Run Effects of Public Housing Demolition on Children.” American Economic Review 108 (10): 3028–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie Janet, and Rossin-Slater Maya. 2013. “Weathering the Storm: Hurricanes and Birth Outcomes.” Journal of Health Economics 32 (3): 487–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie Janet, and Schwandt Hannes. 2016. “The 9/11 Dust Cloud and Pregnancy Outcomes: A Reconsideration.” Journal of Human Resources 51 (4): 805–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler David. 2010. “How Health Care Reform Must Bend the Cost Curve.” Health Affairs 29 (6): 1131–35. [DOI] [PubMed] [Google Scholar]
- Cutler David M., and Richardson Elizabeth. 1999. “Your Money and Your Life: The Value of Health and What Affects It.” In Frontiers in Health Policy Research. Volume 2, edited by Garber Alan, 99–132. Cambridge, MA: MIT Press. [Google Scholar]
- Deryugina Tatyana. 2017. “The Fiscal Cost of Hurricanes: Disaster Aid versus Social Insurance.” American Economic Journal: Economic Policy 9 (3): 168–98. [Google Scholar]
- Deryugina Tatyana, Kawano Laura, and Levitt Steven. 2018. “The Economic Impact of Hurricane Katrina on Its Victims: Evidence from Individual Tax Returns.” American Economic Journal: Applied Economics 10 (2): 202–33. [Google Scholar]
- Deryugina Tatyana, and Molitor David. 2020. “Replication Data for: Does When You Die Depend on Where You Live? Evidence from Hurricane Katrina.” American Economic Association; [publisher], Inter-university Consortium for Political and Social Research [distributor]. 10.3886/E119969V1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle Joseph J. Jr. 2011. “Returns to Local-Area Health Care Spending: Evidence from Health Shocks to Patients Far from Home.” American Economic Journal: Applied Economics 3 (3): 221–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle Joseph J. Jr., Graves John A., Gruber Jonathan, and Kleiner Samuel A.. 2015. “Measuring Returns to Hospital Care: Evidence from Ambulance Referral Patterns.” Journal of Political Economy 123 (1): 170–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwyer-Lindgren Laura, Amelia Bertozzi-Villa Rebecca W. Stubbs, Morozoff Chloe, Mack-enbach Johan P., van Lenthe Frank J., et al. 2017. “Inequalities in Life Expectancy among US Counties, 1980 to 2014: Temporal Trends and Key Drivers.” JAMA Internal Medicine 177 (7): 1003–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyer Jonathan, Dinterman Robert, Miller Noah, and Rose Adam. 2018. “The Effect of Disasters on Migration Destinations: Evidence from Hurricane Katrina.” Economics of Disasters and Climate Change 2 (1): 91–106. [Google Scholar]
- Federal Emergency Management Agency. 2005. “Residents in 17 Orleans Parish Zip Codes May Return Home to Inspect Damage.” https://www.fema.gov/news-release/2005/12/09/residents-17-orleans-parish-zip-codes-may-return-home-inspect-damage (accessed March 23, 2018).
- Fernandez Lauren S., Byard Deana, Lin Chien-Chih, Benson Samuel, and Barbera Joseph A.. 2002. “Frail Elderly as Disaster Victims: Emergency Management Strategies.” Prehospital and Disaster Medicine 17 (2): 67–74. [DOI] [PubMed] [Google Scholar]
- Field Christopher B., Barros Vicente, Stocker Thomas F., Dahe Qin, Dokken David J., Ebi Kristie L., Mastrandrea Michael D., et al. , eds. 2012. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. New York: Cambridge University Press. [Google Scholar]
- Finkelstein Amy, Gentzkow Matthew, and Williams Heidi. 2016. “Sources of Geographic Variation in Health Care: Evidence from Patient Migration.” Quarterly Journal of Economics 131 (4): 1681–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein Amy, Gentzkow Matthew, and Williams Heidi. 2019. “Place-Based Drivers of Mortality: Evidence from Migration.” NBER Working Paper 25975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher Elliott S., Bynum Julie P., and Skinner Jonathan S.. 2009. “Slowing the Growth of Health Care Costs: Lessons from Regional Variation.” New England Journal of Medicine 360 (9): 849–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher Elliott S., Wennberg David E., Stukel Thérèse A., Gottlieb Daniel J., Lucas F. Lee, and Pinder Etoile L.. 2003a. “The Implications of Regional Variations in Medicare Spending. Part 1: The Content, Quality, and Accessibility of Care.” Annals of Internal Medicine 138 (4): 273–87. [DOI] [PubMed] [Google Scholar]
- Fisher Elliott S., Wennberg David E., Stukel Thérèse A., Gottlieb Daniel J., Lucas F. Lee, and Pinder Etoile L.. 2003b. “The Implications of Regional Variations in Medicare Spending. Part 2: Health Outcomes and Satisfaction with Care.” Annals of Internal Medicine 138 (4): 288–98. [DOI] [PubMed] [Google Scholar]
- Groen Jeffrey A., Kutzbach Mark, and Polivka Anne E.. 2020. “Storms and Jobs: The Effect of Hurricanes on Individuals’ Employment and Earnings over the Long Term.” Journal of Labor Economics 38 (3): 653–85 [Google Scholar]
- Grossman Michael. 1972. “On the Concept of Health Capital and the Demand for Health.” Journal of Political Economy 80 (2): 223–55. [Google Scholar]
- Hornbeck Richard. 2012. “The Enduring Impact of the American Dust Bowl: Short- and Long-Run Adjustments to Environmental Catastrophe.” American Economic Review 102 (4): 1477–507. [Google Scholar]
- Hornbeck Richard, and Naidu Suresh. 2014. “When the Levee Breaks: Black Migration and Economic Development in the American South.” American Economic Review 104 (3): 963–90. [Google Scholar]
- Johnson Janna E., and Taylor Evan J.. 2019. “The Long Run Health Consequences of Rural-Urban Migration.” Quantitative Economics 10 (2): 565–606. [Google Scholar]
- Kahn Matthew E. 2005. “The Death Toll from Natural Disasters: The Role of Income, Geography, and Institutions.” Review of Economics and Statistics 87 (2): 271–84. [Google Scholar]
- Kennan John, and Walker James R.. 2010. “Wages, Welfare Benefits and Migration.” Journal of Econometrics 156 (1): 229–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler Ronald C., Galea Sandro, Gruber Michael J., Sampson Nancy A., Ursano Robert J., and Wessely Simon. 2008. “Trends in Mental Illness and Suicidality after Hurricane Katrina.” Molecular Psychiatry 13 (4): 374–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manson Steven, Schroeder Jonathan, Van Riper David, and Ruggles Steven, et al. 2017. IPUMS National Historical Geographic Information System: Version 12.0 [Database]. Minneapolis: University of Minnesota. [Google Scholar]
- Molitor David. 2018. “The Evolution of Physician Practice Styles: Evidence from Cardiologist Migration.” American Economic Journal: Economic Policy 10 (1): 326–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow Betty Hearn. 1999. “Identifying and Mapping Community Vulnerability.” Disasters 23 (1): 1–18. [DOI] [PubMed] [Google Scholar]
- Murphy Kevin M., and Topel Robert H.. 2006. “The Value of Health and Longevity.” Journal of Political Economy 114 (5): 871–904. [Google Scholar]
- Nakamura Emi, Sigurdsson Jósef, and Steinsson Jón. 2017. “The Gift of Moving: Intergenerational Consequences of a Mobility Shock.” NBER Working Paper 22392. [Google Scholar]
- National Hurricane Center. 2018. “Costliest U.S. Tropical Cyclones Tables Update” https://www.nhc.noaa.gov/news/UpdatedCostliest.pdf (accessed March 23, 2018).
- National Oceanic and Atmospheric Administration. 2005. “Extent and Depth of Flooding in Orleans Parish, LA, on August 31, 2005.”
- National Oceanic and Atmospheric Administration. 2006–2013. “Global Historical Climatology Network.” ftp://ftp.ncdc.noaa.gov/pub/data/ghcn/daily/ (accessed October 1, 2019).
- National Oceanic and Atmospheric Administration. 2018. “Billion-Dollar Weather and Climate Disasters: Table of Events.” https://www.ncdc.noaa.gov/billions/ (accessed March 23, 2018).
- National Weather Service. 2016. “Extremely Powerful Hurricane Katrina Leaves a Historic Mark on the Northern Gulf Coast.” https://www.weather.gov/mob/katrina (accessed May 24, 2018).
- Nigg Joanne M., Barnshaw John, and Torres Manuel R.. 2006. “Hurricane Katrina and the Flooding of New Orleans: Emergent Issues in Sheltering and Temporary Housing.” Annals of the American Academy of Political and Social Science 604 (1): 113–28. [Google Scholar]
- Paxson Christina, Fussell Elizabeth, Rhodes Jean, and Waters Mary. 2012. “Five Years Later: Recovery from Post-Traumatic Stress and Psychological Distress among Low-Income Mothers Affected by Hurricane Katrina.” Social Science & Medicine 74 (2): 150–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak Robert H., Tracy Melissa, Galea Sandro, Kilpatrick Dean G., Ruggiero Kenneth J., Hamblen Jessica L., Southwick Steven M., et al. 2012. “Resilience in the Face of Disaster: Prevalence and Longitudinal Course of Mental Disorders Following Hurricane Ike.” PLOS One 7 (6): e38964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes Jean, Chan Christian, Paxson Christina, Cecilia Elena Rouse Mary Waters, and Fussell Elizabeth. 2010. “The Impact of Hurricane Katrina on the Mental and Physical Health of Low-Income Parents in New Orleans.” American Journal of Orthopsychiatry 80 (2): 237–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowland Diane. 2007. “Health Care in New Orleans: Before and After Katrina.” Congressional Testimony, Hearing on Post Katrina Health Care: Continuing Concerns and Immediate Needs in the New Orleans Region. [Google Scholar]
- Sacarny Adam. 2018. “CMS Hospital Compare Data 2004–2016.” https://github.com/asacarny/hospital-compare (accessed October 1, 2019).
- Sacerdote Bruce. 2012. “When the Saints Go Marching Out: Long-Term Outcomes for Student Evacuees from Hurricanes Katrina and Rita.” American Economic Journal: Applied Economics 4 (1): 109–35. [Google Scholar]
- Sastry Narayan, and Gregory Jesse. 2013. “The Effect of Hurricane Katrina on the Prevalence of Health Impairments and Disability among Adults in New Orleans: Differences by Age, Race, and Sex.” Social Science & Medicine 80: 121–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sastry Narayan, and VanLandingham Mark. 2009. “One Year Later: Mental Illness Prevalence and Disparities among New Orleans Residents Displaced by Hurricane Katrina.” American Journal of Public Health 99 (3): S725–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel Jeremy J. 1992. “The Real Rate of Interest from 1800–1990: A Study of the U.S. and the U.K.” Journal of Monetary Economics 29 (2): 227–52. [Google Scholar]
- Sirovich Brenda E., Gottlieb Daniel J., Welch H. Gilbert, and Fisher Elliott S.. 2006. “Regional Variations in Health Care Intensity and Physician Perceptions of Quality of Care.” Annals of Internal Medicine 144 (9): 641–49. [DOI] [PubMed] [Google Scholar]
- Skinner Jonathan. 2011. “Causes and Consequences of Regional Variations in Health Care.” In Handbook of Health Economics, Vol. 2, edited by Pauly Mark, McGuire Thomas, and Barros Pedro, 45–93. Amsterdam: Elsevier. [Google Scholar]
- Skinner Jonathan, and Fisher Elliott. 2010. “Reflections on Geographic Variations in U.S. Health Care” Unpublished.
- Song Yunjie, Skinner Jonathan, Bynum Julie, Sutherland Jason, Wennberg John E., and Fisher Elliott S.. 2010. “Regional Variations in Diagnostic Practices.” New England Journal of Medicine 363 (1): 45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strobl Eric. 2011. “The Economic Growth Impact of Hurricanes: Evidence from U.S. Coastal Counties.” Review of Economics and Statistics 93 (2): 575–89. [Google Scholar]
- Super N, and Biles B. 2005. “Displaced by Hurricane Katrina: Issues and Options for Medicare Beneficiaries.” Henry J. Kaiser Family Foundation Medicare Policy Brief. [Google Scholar]
- Torche Florencia. 2011. “The Effect of Maternal Stress on Birth Outcomes: Exploiting a Natural Experiment.” Demography 48 (4): 1473–91. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services, Health Resources and Services Administration. 2005. “Area Resource File, 2005.” National Bureau of Economic Research; [data host]. http://data.nber.org/homedata (accessed July 13, 2020). [Google Scholar]
- US Department of Health and Human Services, Health Resources and Services Administration. 2009. “Area Resource File, 2009.” National Bureau of Economic Research; [data host]. http://data.nber.org/homedata (accessed July 13, 2020). [Google Scholar]
- US Environmental Protection Agency. 2006–2013. “Air Quality System.” https://aqs.epa.gov/aqsweb/airdata/download_files.html (accessed October 1, 2019).
- Wolshon Brian. 2006. “Evacuation Planning and Engineering for Hurricane Katrina.” Bridge 36 (1): 27–34. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


