Abstract
Background/ Objectives
Food insecurity has emerged as a critical health issue for older adults. Food insecurity has been shown to disrupt healthy eating patterns, but these associations have not been widely studied among older adults. The objectives of the present study were to: 1) examine national trends in food insecurity across a ten-year period, and 2) evaluate the associations between food insecurity and multiple diet quality indices in a recent and nationally representative sample of adults aged 60 or older.
Design
Cross-sectional analysis of the 2007–2016 National Health and Nutrition Examination Surveys
Setting
Nationally representative sample of the United States
Participants
The analytic sample was comprised of 5,097 adults aged 60 or older, with household incomes at or below 300% of the federal poverty level
Measurements
Household food security was measured using the 18-item US Household Food Security Survey Module. Diet was assessed using two 24-hour dietary recalls. Multivariate linear and logistic regression models examined the associations between household food security and three evidence-based diet quality indices, adjusting for sociodemographic and health characteristics.
Results
Across the ten-year period, food insecurity increased significantly from 5.5% to 12.4% among older adults; this increase was more pronounced among lower-income older adults. From the linear regression models, food insecurity was associated with lower scores on the Healthy Eating Index (β=−1.90, 95% CI −3.70, −0.09), the Alternate Healthy Eating Index-2010 (β=−1.47, 95% CI −2.51, −0.44), and the Mediterranean Diet Score (β=−0.54, 95% CI −1.06, −0.001) after multivariate adjustment. Further adjustment for the presence of chronic medical conditions did not attenuate these results.
Conclusion
Food insecurity is associated with lower overall diet quality among older adults, supporting the need for clinical efforts to identify those at risk of food insecurity and public health efforts to alleviate food insecurity and promote healthy eating behaviors among older adults.
Keywords: food insecurity, diet quality, healthy eating patterns, National Health and Nutrition Examination Surveys
INTRODUCTION
Food insecurity, a condition of limited access to nutritious foods due to a lack of financial resources, has persisted in the United States since national surveys began tracking its prevalence in 1998.1 Food insecurity has emerged as a critical health issue for older adults (ages 60 and older), disproportionately affecting those who live alone, have fixed incomes, and have chronic health concerns.2–5 Since 2001, the number of older adults experiencing food insecurity increased from 2.3 million to 5.3 million, and is expected to grow to 8 million by 2050 due, in part, to population growth.2 In 2018, it was estimated that 7.5% of households with older adults were food-insecure and 8.9% of households with older adults living alone were food-insecure.1
Core components of the experience of food insecurity involve disruptions to normal eating patterns, such as eating inexpensive foods of lower quality, eating less than one should, and skipping meals, all of which are attributed to not having enough money for food. Although the relationship between food insecurity and dietary outcomes has been previously examined, studies have predominantly focused on children and adolescents, pregnant women, and younger adult populations.6–11 Despite the importance of high diet quality for healthy aging and chronic disease outcomes,12–15 few studies have examined the associations between food insecurity and diet quality in older adults. In one study, using data from the Nutrition Survey of the Elderly in New York State and the Third National Health and Nutrition Examination Survey (NHANES), older adults (ages 60 years and older) with food insecurity had lower mean intakes of 12 nutrients than those with food security.16 Another study using data from the Third NHANES found that food insecurity was associated with lower diet quality among adults 65 and older.17 A more recent study was conducted among adults aged 49 and older from the Blue Mountains Eye Study. Their results showed no association between food insecurity and diet quality, though both food insecurity and diet quality were associated with lower quality of life.18 The existing body of research is characterized by a lack of recent data to investigate the association between food insecurity and diet quality in older adults, inconsistencies in findings across studies, varying aspects of nutritional status examined in relation to food insecurity (e.g. nutrients, diet quality indices), and potential residual confounding by household income, a key predictor of household food security and diet quality. Furthermore, few studies have taken into account the role that participation in the Supplemental Nutrition Assistance Program (SNAP) may have on these associations.19, 20 SNAP, formerly the Food Stamp Program, is the largest federal nutrition assistance program that aims to reduce food security and improve nutritional intake through benefits that can be used to purchase food.21 Thus, there may be differential associations between household food security and diet quality depending on whether older adults receive SNAP benefits.
The objectives of the study were to: 1) examine national trends in household food security across a ten-year period among all older adults aged 60 or older, and 2) evaluate the associations between household food security and diet quality indices in older adults with household incomes ≤300% of the federal poverty level (FPL). We further examined effect modification of the associations between household food security and diet quality indices by participation in SNAP.
METHODS
Study population
Data for the present study came from 2007–2016 NHANES, an ongoing, multistage survey representative of the civilian, noninstitutionalized US population that includes an oversample of adults aged 60 years and older. To examine ten-year trends of household food security in the national population, the study sample was comprised of 9,623 adults, ages 60 years and older. For analyses of household food security and diet quality indices, older adults were excluded for the following reasons: household incomes >300% FPL (n=2,912), missing dietary data (n=1,590), or missing education, marital status, smoking, or physical activity data (n=24) resulting in a final analytic sample of 5,097 older adults with household incomes ≤300% FPL.
Food security status
Household food security was measured using the 18-item US Household Food Security Survey Module, a widely used instrument from the U.S. Department of Agriculture (USDA).22 Briefly, questions are asked in stages about experiences or behaviors related to insufficient resources to acquire food over the past 12 months. Eight questions pertained to children’s experiences of food insecurity, which were omitted if no children are present in the household. Food security is defined as 0 affirmative responses, meaning that all individuals in the household had sufficient resources for food at all times. Marginal food security is defined as 1–2 affirmative responses, meaning that individuals within the household may have had concerns about food running out, but did not exhibit any more severe behavioral manifestations of food insecurity. Food insecurity is defined as 3 or more affirmative responses, meaning that individuals within the household reduced the quality, variety, and/or quantity of food consumed as a result of insufficient resources for food.
Dietary quality indices
Dietary intake was assessed using two 24-hour dietary recalls conducted by trained interviewers. The first recall is administered in-person in the Mobile Examination Center. The second recall is scheduled after the first recall is completed and administered by telephone 3–10 days later. Standardized protocols are used to ensure all NHANES participants complete the dietary interviews using the same methods.23, 24 The 24-hour recall collects information on all foods and beverages consumed from midnight to midnight of the previous day, including information on the time of consumption, the name of the eating occasion, where the food was eaten, etc. The USDA Automated Multiple Pass Method is used in the administration of the 24-hour dietary recalls, which consists of the following five steps: 1) a quick list of all remembered foods, 2) a probe of commonly forgotten foods and beverages, 3) the eating occasions and times from the previous day, 4) additional details of each food or beverage consumed, and 5) a final review probe. Dietary recalls are collected on weekdays and weekend days. The validity of the 24-hour recall method has been previously established.25, 26
In the present analysis, we examined three diet quality indices: the Healthy Eating Index (HEI)-2015, the Alternate Healthy Eating Index (AHEI)-2010, and the Mediterranean Diet (MedDiet) score because they each measure distinct aspects of overall diet quality (Supplementary Table S1). Data from the NHANES dietary interview files and the USDA Food Patterns Equivalents Database, which converts food items to standard food groups and food pattern components, were merged to calculate all diet quality indices. The HEI-2015 is a measure of diet quality developed by the USDA Center for Nutrition Policy and Promotion that measures adherence to the 2015–20 Dietary Guidelines for Americans.27 Scored out of 100 points, the HEI-2015 has nine adequacy components: total fruits, whole fruits, dark green/orange vegetables and legumes, greens and beans, whole grains, milk/dairy, total protein foods, seafood and plant proteins, and unsaturated to saturated fatty acid ratio, where higher scores denote higher intakes; and four moderation components: refined grains, sodium, added sugars, saturated fats, where higher scores denote lower intakes. The HEI-2015 score was calculated according to the simple HEI scoring algorithm using the NHANES dietary interview files and the USDA Food Patterns Equivalents Database through publicly-available SAS macros.28 The AHEI-2010 is a measure of diet quality predictive of major chronic disease risk.29 Scored out of 110 points, higher scores are awarded to high intakes of vegetables, fruits, whole grains, nuts and legumes, long-chain fats, and polyunsaturated fats; low intakes of sugar-sweetened beverages and fruit juice, red/processed meats, trans fats, and sodium; and moderate alcohol intake. Because trans fats is not available in the NHANES dietary nutrient files, the AHEI-2010 was modified to exclude this component and the overall score was rescaled to the original total for comparison with previous studies. The MedDiet score is a measure of adherence to the traditional Mediterranean diet, which has been associated with healthy aging outcomes among older adults.30–32 Scored out of 55 points, higher scores are awarded to high intakes of whole grains, fruits, vegetables, potatoes, legumes, fish, and monounsaturated fats; low intakes of red meat, poultry, and full-fat dairy products; and moderate alcohol consumption. For analysis, each of the diet quality indices were examined as both continuous scores and as quintiles comparing the top quintile to the bottom four quintiles. The decision to compare the older adults in the top quintile of diet quality to the bottom four quintiles was guided by prior literature demonstrating that individuals of the highest diet quality have the lowest relative risks for diet-sensitive chronic conditions and all-cause mortality.29, 33, 34
Study covariates
Study covariates were chosen based on prior knowledge and previous research on sociodemographic and health correlates of both food insecurity and diet quality. Sociodemographic covariates included age (60–64, 65–69, 70–74, 75–79, 80 and older), sex, race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, Other), highest educational attainment (<12 years, high school graduate or equivalent, some college, or college graduate), marital status (married or living with partner, never married, separated or divorced or widowed), and household income relative to the federal poverty line (FPL) (0–130% FPL, 131–300% FPL). A missing indicator was used to account for individuals with missing data on household income relative to the FPL (n=637). Health covariates included smoking status (never smoker, former smoker, current smoker), and vigorous or moderate recreational physical activity in a typical week (any, none). We also investigated the prior diagnosis of chronic medical conditions as a potential intermediate: diabetes, congestive heart failure, coronary heart disease, angina, myocardial infarction, stroke, emphysema, thyroid problems, liver condition, and cancer. For analysis, the number of self-reported chronic medical conditions was categorized as: 0, 1, 2, 3, or 4 or more conditions. SNAP participation was defined as any receipt of SNAP or food stamp benefits by the study participant or any member of their family within the past 12 months.
Statistical analysis
Complex interview and dietary sampling weights were used to account for unequal selection probabilities, patterns of non-response, and to make nationally representative estimates across the 10-year period. We first estimated the prevalences of marginal food security and food insecurity among all older adults and lower-income older adults with household incomes ≤300% FPL within each two-year NHANES cycle. Linear time trends were examined for the outcomes of marginal food security and food insecurity using logistic regression models with survey year modeled as an ordinal predictor variable. Next, we examined differences in sociodemographic and health characteristics by household food security status among lower-income older adults with household incomes ≤300% FPL using χ2 tests. To examine the associations between household food security status and diet quality indices among lower-income adults, six multivariate-adjusted regression models were fit: three multivariate linear regression models were fit for each continuous diet quality index outcome (HEI-2015, AHEI-2010, and MedDiet); three additional multivariate logistic regression models were fit for each categorical diet quality index outcome comparing the top quintile to the bottom four quintiles. All models adjusted for study covariates, as well as NHANES cycle and total energy intake. Further adjustment of chronic medical conditions was included in each model to determine the extent to which it mediated the associations between household food security and diet quality. We then examined potential effect modification by SNAP participation on the multivariate-adjusted associations between household food security and continuous diet quality indices among older adults ≤130% FPL, the income threshold for SNAP. As a sensitivity analysis, we also examined the associations between household food security and diet quality in the study sample of older adults at all income levels (n=9,623).
All statistical tests were 2-sided, and statistical significance was considered at P<0.05. Statistical analyses were performed using SAS 9.3 (SAS Institute, Cary, NC).
RESULTS
Ten-year trends in marginal food security and food insecurity are shown in Figure 1. Among all older adults, marginal food security increased from 4.8% to 7.5% and food insecurity increased from 5.5% to 12.4% from 2007–08 to 2015–16. Among older adults ≤300% FPL, marginal food security increased from 7.1% to 12.2% and food insecurity increased from 8.5% to 20.9% from 2007–08 to 2015–16. All linear time trends were statistically significant (Ps<0.01).
Figure 1:
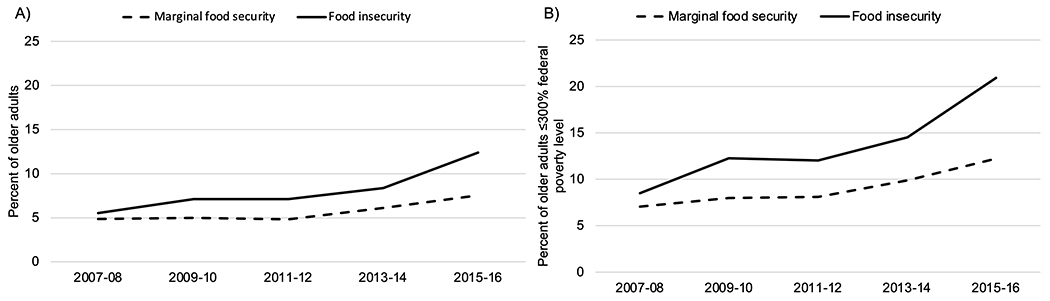
Trends in household food security from 2007–16 among A) all older adults and B) lower-income older adults (household incomes ≤300% of the federal poverty level)
In the analytic sample of 5,097 lower-income older adults, differences in sociodemographic and health covariates by household food security status are shown in Table 1. Compared to their food-secure counterparts, marginally food secure and food-insecure older adults were more likely to be of younger age, of minority race/ethnicity, have lower educational attainment, have household incomes at or below 130% FPL, and be separated, divorced or widowed (Ps<0.0001). Marginally food secure and food-insecure older adults were also more likely to be current smokers and engage in less physical activity (Ps<0.0001). In bivariate analyses, marginally food secure and food-insecure older adults were less likely to be in the top quintile of the HEI-2015 (P<0.0001), AHEI-2010 (P<0.0001), and MedDiet scores (P=0.03). There was a marginal difference between household food security and the presence of chronic medical conditions (P=0.06).
Table 1:
Sociodemographic and health characteristics by household food security status among older adults with household incomes ≤300% federal poverty level: NHANES 2007-2016
| Total (n=5,097) | Food secure (n=3,604) | Marginal food secure (n=559) | Food insecure (n=934) | P-value1 | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Age | <0.0001 | ||||||||
| 60-64 | 1350 | 24.9 | 798 | 22.8 | 186 | 29.7 | 366 | 33.8 | |
| 65-69 | 1047 | 20.8 | 689 | 19.2 | 126 | 26.7 | 232 | 25.8 | |
| 70-74 | 955 | 18.4 | 695 | 18.2 | 106 | 19.6 | 154 | 18.6 | |
| 75-79 | 726 | 14.8 | 548 | 15.8 | 69 | 9.1 | 109 | 13.0 | |
| ≥80 | 1019 | 21.2 | 874 | 24.0 | 72 | 14.9 | 73 | 8.8 | |
| Sex | 0.67 | ||||||||
| Male | 2363 | 41.1 | 1686 | 41.4 | 253 | 41.0 | 424 | 39.0 | |
| Female | 2734 | 58.9 | 1918 | 58.6 | 306 | 59.0 | 510 | 61.0 | |
| Race/ethnicity | <0.0001 | ||||||||
| Non-Hispanic White | 2399 | 72.7 | 1947 | 78.0 | 194 | 60.0 | 258 | 49.9 | |
| Non-Hispanic Black | 1116 | 11.2 | 726 | 9.4 | 158 | 17.4 | 232 | 17.7 | |
| Hispanic | 1307 | 10.7 | 740 | 7.6 | 176 | 16.2 | 391 | 25.5 | |
| Other | 275 | 5.4 | 191 | 5.0 | 31 | 6.3 | 53 | 7.0 | |
| Educational attainment | <0.0001 | ||||||||
| <12 years | 1957 | 28.0 | 1214 | 24.5 | 244 | 32.8 | 499 | 45.6 | |
| High school graduate or equivalent | 1336 | 30.0 | 1011 | 31.4 | 130 | 31.6 | 195 | 20.2 | |
| Some college | 1204 | 27.6 | 880 | 28.0 | 137 | 24.4 | 187 | 27.7 | |
| College graduate | 600 | 14.4 | 499 | 16.1 | 48 | 11.3 | 53 | 6.5 | |
| Poverty income ratio | <0.0001 | ||||||||
| ≤130% FPL | 2015 | 30.0 | 1125 | 23.4 | 300 | 45.9 | 590 | 58.9 | |
| 131-<300% FPL | 2445 | 56.9 | 1968 | 62.1 | 212 | 45.1 | 265 | 34.1 | |
| Missing | 637 | 13.0 | 511 | 14.5 | 47 | 8.9 | 79 | 7.1 | |
| Marital status | <0.0001 | ||||||||
| Married or living with partner | 2615 | 54.2 | 1937 | 57.1 | 264 | 48.6 | 414 | 40.5 | |
| Never married | 306 | 5.4 | 202 | 5.5 | 34 | 4.5 | 70 | 5.5 | |
| Separated, divorced, widowed | 2176 | 40.4 | 1465 | 37.4 | 261 | 46.9 | 450 | 54.0 | |
| Smoking status | <0.0001 | ||||||||
| Never smoker | 2446 | 47.7 | 1773 | 48.6 | 257 | 44.9 | 416 | 43.9 | |
| Former smoker | 1941 | 40.0 | 1423 | 41.0 | 212 | 41.6 | 306 | 32.9 | |
| Current smoker | 710 | 12.3 | 408 | 10.4 | 90 | 13.4 | 212 | 23.2 | |
| Moderate or vigorous physical activity | 1625 | 34.8 | 1237 | 37.5 | 142 | 26.9 | 246 | 24.4 | <0.0001 |
| Healthy Eating Index-2015 quintiles | 0.001 | ||||||||
| Top quintile (67.3-99.5) | 1058 | 19.6 | 813 | 20.9 | 102 | 18.5 | 143 | 12.6 | |
| Bottom four quintiles (15.1-67.3) | 4038 | 80.4 | 2791 | 79.1 | 456 | 81.5 | 791 | 87.4 | |
| Alternate Healthy Eating Index-2010 quintiles | <0.0001 | ||||||||
| Top quintile (54.0-93.3) | 1007 | 20.2 | 799 | 22.5 | 82 | 12.9 | 126 | 11.3 | |
| Bottom four quintiles (8.1-53.9) | 4089 | 79.8 | 2805 | 77.5 | 476 | 87.1 | 808 | 88.7 | |
| MedDiet Score quintiles | 0.03 | ||||||||
| Top quintile (26.5-42.0) | 1019 | 18.6 | 770 | 19.5 | 91 | 13.2 | 158 | 16.6 | |
| Bottom four quintiles (8.0-26.0) | 4077 | 81.4 | 2834 | 80.5 | 467 | 86.8 | 776 | 83.4 | |
| Chronic medical conditions | 0.06 | ||||||||
| 0 conditions | 1865 | 35.4 | 1322 | 36.0 | 205 | 34.8 | 338 | 32.3 | |
| 1 condition | 1637 | 32.4 | 1182 | 33.1 | 173 | 33.1 | 282 | 27.7 | |
| 2 conditions | 862 | 17.7 | 611 | 17.3 | 100 | 16.5 | 151 | 20.5 | |
| 3 conditions | 397 | 7.7 | 268 | 7.4 | 40 | 6.2 | 89 | 10.2 | |
| 4 or more conditions | 336 | 6.8 | 221 | 6.1 | 41 | 9.5 | 74 | 9.2 | |
From chi-squared tests
The correlations between the HEI-2015, AHEI-2010, and MedDiet Score ranged from 0.66 to 0.67. Multivariate-adjusted associations between household food security and diet quality indices are shown in Table 2. For the HEI-2015, food insecurity was significantly associated with lower continuous scores (β=−1.90, 95% CI −3.70, −0.09, P-trend=0.03) and lower odds of being in the top quintile (vs. bottom four quintiles) of the HEI-2015 (OR 0.67, 95% CI 0.47, 0.96, P-trend=0.06). For the AHEI-2010, marginal food security and food insecurity were associated with lower continuous scores (marginal food security: β=−2.42, 95% CI −3.76, −1.07; food insecurity: β=−1.47, 95% CI −2.51, −0.44, P-trend=0.0008), and lower odds of being in the top quintile of the AHEI-2010 (marginal food security: OR 0.58, 95% CI 0.41, 0.83; food insecurity OR 0.58, 95% CI 0.43, 0.77, P-trend<0.0001). For the MedDiet score, marginal food security and food insecurity were associated with lower continuous scores (marginal food security: β= −0.62, 95% CI −1.11, −0.12; food insecurity: β=−0.54, 95% CI −1.06, −0.01, P-trend=0.02), and lower odds of being in the top quintile of the MedDiet score (marginal food security, OR 0.69, 95% CI 0.48, 0.99, P-trend=0.56). All associations persisted after further adjustment for chronic medical conditions. The complete multivariate-adjusted regression results are provided in Supplementary Tables S2-S3.
Table 2:
Multivariate-adjusted associations between household food security and diet quality indices among older adults with household incomes ≤300% of the federal poverty level
| Continuous diet quality indices | Quintiles of diet quality indices (comparing top quintile to bottom four quintiles | |||||||
|---|---|---|---|---|---|---|---|---|
| Multivariate-adjusted1 | Multivariate-adjusted plus chronic medical conditions1 | Multivariate-adjusted2 | Multivariate-adjusted plus chronic medical conditions2 | |||||
| β | 95% CI | β | 95% CI | OR | 95% CI | OR | 95% CI | |
| Healthy Eating Index-2015 | ||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | ||||
| Marginally food secure | −1.43 | −3.18, 0.33 | −1.42 | −3.19, 0.35 | 0.96 | 0.67, 1.38 | 0.96 | 0.67, 1.38 |
| Food insecure | −1.90 | −3.70, −0.09 | −1.91 | −3.72, −0.10 | 0.67 | 0.47, 0.96 | 0.68 | 0.47, 0.98 |
| P-trend | 0.03 | 0.03 | 0.06 | 0.06 | ||||
| Alternate Healthy Eating Index-2010 | ||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | ||||
| Marginally food secure | −2.42 | −3.76, −1.07 | −2.41 | −3.77, −1.04 | 0.58 | 0.41, 0.83 | 0.58 | 0.41, 0.83 |
| Food insecure | −1.47 | −2.51, −0.44 | −1.49 | −2.53, −0.45 | 0.58 | 0.43, 0.77 | 0.57 | 0.43, 0.76 |
| P-trend | 0.0008 | 0.0008 | <0.0001 | <0.0001 | ||||
| Mediterranean Diet (MedDiet) Score | ||||||||
| Food secure | Ref. | Ref. | Ref. | Ref. | ||||
| Marginally food secure | −0.62 | −1.11, −0.12 | −0.63 | −1.12, −0.14 | 0.69 | 0.48, 0.99 | 0.69 | 0.48, 0.99 |
| Food insecure | −0.54 | −1.06, −0.01 | −0.55 | −1.09, −0.02 | 0.96 | 0.65, 1.42 | 0.94 | 0.64, 1.40 |
| P-trend | 0.02 | 0.02 | 0.56 | 0.51 | ||||
Coefficients obtained from linear regression models adjusted for age, sex, race/ethnicity, educational attainment, poverty income ratio, marital status, smoking status, moderate or vigorous physical activity, and survey year
Coefficients obtained from logistic regression models adjusted for age, sex, race/ethnicity, educational attainment, poverty income ratio, marital status, smoking status, moderate or vigorous physical activity, and survey year
There was no evidence that SNAP participation modified the associations between food insecurity and diet quality indices (P-interactions>0.10) (data not shown). In sensitivity analyses, results were similar when examining the associations in older adults across all income levels (data not shown).
DISCUSSION
In this national sample, the prevalence of both marginal food security and food insecurity increased significantly among adults aged 60 and older from 2007–2016. Independent of sociodemographic and health characteristics, food insecurity was associated with lower diet quality, as evident by lower scores across all three indices. These results corroborate prior studies among older adults that have examined food insecurity in relation to the older Healthy Eating Index17 and the Total Diet Score.18 Together, there is evidence to suggest that food insecurity is negatively associated with older adults’ dietary behaviors. Dietary intake is an integral contributor to healthy aging for older adults.35 The results of the present study help to shed light on how diet quality may explain, in part, the observed associations between food insecurity and aging-related outcomes, such as functional limitations,36, 37 chronic disease risk and management,3, 38 cognitive impairment,39–41 and lower self-rated health.16 In particular, the results that food-insecure older adults were significantly less likely to be in the top quintile of HEI-2015 and AHEI-2010 scores may hold clinical significance, as a recent meta-analysis showed that adults in the top categories of HEI and AHEI had significantly lower risks of cardiovascular disease, cancer, type 2 diabetes, neurodegenerative diseases, and all-cause mortality.33 Further research using longitudinal studies is needed to understand whether the relatively small differences in continuous diet quality indices scores found in the present study are clinically meaningful.
It is important to note that marginal food security was also significantly associated with lower AHEI-2010 and MedDiet scores in the present study at magnitudes equal to or greater than the effect estimates observed between food insecurity and AHEI-2010 or MedDiet scores. The USDA considers marginal food security to be less severe than food insecurity. Thus, we expected to observe a gradient in the associations between more severe food insecurity and lower diet quality. The finding that older adults with marginal food security had similar dietary outcomes when compared to older adults with food insecurity suggests that even the earliest indicators of food insecurity, including mild anxiety about food running out or not being able to afford a balanced meal, can be associated with more unhealthful eating patterns. These associations may be driven, in part, by the chronic stress of experiencing food insecurity, which has been known to alter eating behaviors resulting in lower diet quality.42, 43 Similarly, other studies of household food security status and diet-related health outcomes have not been consistent in observing a graded association with more adverse outcomes. One study found that mild food insecurity, but not severe food insecurity, was associated with obesity in women,44 while another study found that adults with marginal food security had the highest odds of metabolic syndrome.45 Further research of the experiences of older adults with both marginal food security and food insecurity is needed to better understand the psychosocial consequences, the behavioral adaptations, and the coping strategies employed to manage their household food situation at different levels of uncertainty and severity.
With rising rates of food insecurity among older adults, continued investment in nutrition programs is needed to simultaneously improve food security and provide healthy food assistance. This could include efforts to screen for food insecurity in clinical settings, provide referrals to congregate meal programs and local food pantries, and provide SNAP application assistance.46 In the present study, few older adults reported consuming congregate meals (8.2%), or receiving home-delivered meals (3.9%). A previous study among older adults in Florida showed that a home-delivered meal program substantially improved food insecurity, total caloric intake, and protein intake, and also resulted in improvements in social isolation and emotional functioning.47 Similarly, a 2019 report showed that the SNAP participation rate among eligible older adults was only 48%, compared to 84% among all individuals.48 In the present study, approximately 27% of income-eligible adults (i.e. households with incomes ≤130% federal poverty level) reported receiving SNAP in the past year. Because SNAP targets those who experience more severe food hardships, a prior study found that seniors participating in SNAP had higher levels of food insecurity, greater need for free food, and more physical disabilities than those who were not participating in SNAP.49 Leveraging existing programs, such as Meals on Wheels or SNAP, is critical to meet the nutritional needs of older adults, particularly in areas where access to food is challenging or during times of national economic hardship.
The primary limitation of this study is the cross-sectional nature of the data, which precludes the ability to make causal inferences. Although research in younger populations supports food insecurity as adversely affecting diet quality, we cannot rule out reverse causation, whereby poor diet quality leads to chronic health conditions, financial instability, and subsequently, food insecurity. We also cannot rule out the possibility of unmeasured confounding by factors such as neighborhood food availability or additional proxies of socioeconomic status. The decision to use a dichotomous physical activity variable was guided by the few questions on physical activity administered to NHANES participants and 65% of adults in the analytic sample who reported no activity in a typical week. However, potential residual confounding by physical activity is another limitation of the analysis. Finally, dietary intake was captured through two 24-hour recalls using the USDA Automated Multiple-Pass Method. Although this approach has been validated, other limitations may include the food database not capturing all possible foods consumed by NHANES participants and the fact that NHANES participants were aware that they would be completing interviews about their dietary intake ahead of time.25 Related to this particular analysis, older adults with cognitive impairment may also have reduced validity in their ability to accurately recall their dietary intake in the short-term.50 Another limitation is the prevalence of chronic medical conditions could also be subject to error if the individual had an underlying health condition but was not formally diagnosed in a clinical setting. However, this study also has multiple strengths, including the large sample size, the use of recently collected data on food insecurity and dietary intake, a focus on overall diet quality as measured by three evidence-based indices, and adjustment for multiple known confounders related to food insecurity and diet quality among older adults.
In the present study, food insecurity, and at times, even marginal food security, were associated with lower overall diet quality among older adults, supporting the need for additional food assistance programs to reach this population. Further research is needed to explore the underlying mechanisms to explain the observed associations, and to better understand social factors and policy strategies that can improve both food insecurity and dietary intake among older adults.
Supplementary Material
Supplemental Table 1: Criteria for scoring the Healthy Eating Index-2015, Alternate Healthy Eating Index-2010, and Mediterranean Diet Score
Supplemental Table 2: Full statistical results from multivariate-adjusted linear regression models for the Healthy Eating Index-2015, Alternate Healthy Eating Index-2010, and the Mediterranean Diet Score
Supplemental Table 3: Full statistical results from multivariate-adjusted logistic regression models comparing individuals in the top quintile to the bottom four quintiles of Healthy Eating Index-2015, Alternate Healthy Eating Index-2010, and the Mediterranean Diet Score
Funding support:
This work was supported by the National Institutes of Health (R00 HD084758 to C.W.L. and K01 DK119166 to J.A.W)
Sponsor’s Role:
The National Institutes of Health had no role in the design, methods, subject recruitment, data collection, analysis or preparation of this study.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to declare.
REFERENCES
- [1].Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2018, ERR-270. U.S. Department of Agriculture, Economic Research Service, 2019. [Google Scholar]
- [2].Ziliak JP, Gundersen C. The State of Senior Hunger in American in 2017: An Annual Report. Feedinng America, 2019. [Google Scholar]
- [3].Jih J, Stijacic-Cenzer I, Seligman HK, Boscardin WJ, Nguyen TT, Ritchie CS. Chronic disease burden predicts food insecurity among older adults. Public Health Nutr. 2018;21: 1737–1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Tarasuk V, Mitchell A, McLaren L, McIntyre L. Chronic physical and mental health conditions among adults may increase vulnerability to household food insecurity. The Journal of nutrition. 2013;143: 1785–1793. [DOI] [PubMed] [Google Scholar]
- [5].Lee JS, Frongillo EA Jr. Factors associated with food insecurity among U.S. elderly persons: importance of functional impairments. J Gerontol B Psychol Sci Soc Sci. 2001;56: S94–99. [DOI] [PubMed] [Google Scholar]
- [6].Hanson KL, Connor LM. Food insecurity and dietary quality in US adults and children: a systematic review. The American journal of clinical nutrition. 2014;100: 684–692. [DOI] [PubMed] [Google Scholar]
- [7].Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet. 2014;114: 1943–1953 e1942. [DOI] [PubMed] [Google Scholar]
- [8].Gamba R, Leung CW, Guendelman S, Lahiff M, Laraia B. Household Food Insecurity is Not Associated with Overall Diet Quality Among Pregnant Women in NHANES 1999–2008. Maternal and child health journal. 2016;20: 2348–2356. [DOI] [PubMed] [Google Scholar]
- [9].Eicher-Miller HA, Mason AC, Weaver CM, McCabe GP, Boushey CJ. Food insecurity is associated with diet and bone mass disparities in early adolescent males but not females in the United States. The Journal of nutrition. 2011;141: 1738–1745. [DOI] [PubMed] [Google Scholar]
- [10].Fram MS, Ritchie LD, Rosen N, Frongillo EA. Child experience of food insecurity is associated with child diet and physical activity. The Journal of nutrition. 2015;145: 499–504. [DOI] [PubMed] [Google Scholar]
- [11].Gregorio MJ, Rodrigues AM, Graca P, et al. Food Insecurity Is Associated with Low Adherence to the Mediterranean Diet and Adverse Health Conditions in Portuguese Adults. Front Public Health. 2018;6: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Lorenzo-Lopez L, Maseda A, de Labra C, Regueiro-Folgueira L, Rodriguez-Villamil JL, Millan-Calenti JC. Nutritional determinants of frailty in older adults: A systematic review. BMC Geriatr. 2017;17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Wengreen HJ, Neilson C, Munger R, Corcoran C. Diet quality is associated with better cognitive test performance among aging men and women. The Journal of nutrition. 2009;139: 1944–1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Reedy J, Krebs-Smith SM, Miller PE, et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. The Journal of nutrition. 2014;144: 881–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].George SM, Ballard-Barbash R, Manson JE, et al. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: evidence to inform national dietary guidance. American journal of epidemiology. 2014;180: 616–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Lee JS, Frongillo EA Jr. Nutritional and health consequences are associated with food insecurity among U.S. elderly persons. The Journal of nutrition. 2001;131: 1503–1509. [DOI] [PubMed] [Google Scholar]
- [17].Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. Journal of health economics. 2004;23: 839–862. [DOI] [PubMed] [Google Scholar]
- [18].Russell JC, Flood VM, Yeatman H, Wang JJ, Mitchell P. Food insecurity and poor diet quality are associated with reduced quality of life in older adults. Nutr Diet. 2016;73: 50–58. [Google Scholar]
- [19].Nord M How much does the Supplemental Nutrition Assistance Program alleviate food insecurity? Evidence from recent programme leavers. Public Health Nutr. 2012;15: 811–817. [DOI] [PubMed] [Google Scholar]
- [20].Nord M, Golla AM. Does SNAP Decrease Food Insecurity? Untangling the Self-Selection Effect. Economic Research Service, U.S. Department of Agriculture, 2009. [Google Scholar]
- [21].SNAP Participation and Costs, 1969–2019. Volume 2020: Food and Nutrition Service, U.S. Department of Agriculture, 2020. [Google Scholar]
- [22].U.S. Household Food Security Survey Module: Three-Stage Design, With Screeners. Economic Research Service, U.S. Department of Agriculture, 2012. [Google Scholar]
- [23].National Health and Nutrition Examination Survey (NHANES) - MEC In-Person Dietary Interviewers Procedures Manual. National Center for Health Statistics, 2010. [Google Scholar]
- [24].National Health and Nutrition Examination Survey (NHANES) - Phone Follow-Up Dietary Interviewer Procedures Manual. National Center for Health Statistics, 2010. [Google Scholar]
- [25].Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C. Update on NHANES Dietary Data: Focus on Collection, Release, Analytical Considerations, and Uses to Inform Public Policy. Adv Nutr. 2016;7: 121–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Baranowski T 24-Hour Recall and Diet Record Methods. In: Willett WC, ed. Nutritional Epidemiology, Volume 40. New York, NY: Oxford University Press, 2012, pp. 49–69. [Google Scholar]
- [27].Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118: 1591–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Code SAS. The Healthy Eating Index, Volume 2018: Division of Cancer Control and Population Sciences, National Cancer Institute, 2018. [Google Scholar]
- [29].Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. The Journal of nutrition. 2012;142: 1009–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].McEvoy CT, Guyer H, Langa KM, Yaffe K. Neuroprotective Diets Are Associated with Better Cognitive Function: The Health and Retirement Study. Journal of the American Geriatrics Society. 2017;65: 1857–1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Tangney CC, Kwasny MJ, Li H, Wilson RS, Evans DA, Morris MC. Adherence to a Mediterranean-type dietary pattern and cognitive decline in a community population. The American journal of clinical nutrition. 2011;93: 601–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Koyama A, Houston DK, Simonsick EM, et al. Association between the Mediterranean diet and cognitive decline in a biracial population. J Gerontol A Biol Sci Med Sci. 2015;70: 354–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Schwingshackl L, Bogensberger B, Hoffmann G. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: An Updated Systematic Review and Meta-Analysis of Cohort Studies. J Acad Nutr Diet. 2018;118: 74–100 e111. [DOI] [PubMed] [Google Scholar]
- [34].Mitrou PN, Kipnis V, Thiebaut AC, et al. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH-AARP Diet and Health Study. Archives of internal medicine. 2007;167: 2461–2468. [DOI] [PubMed] [Google Scholar]
- [35].Samieri C, Sun Q, Townsend MK, et al. The association between dietary patterns at midlife and health in aging: an observational study. Ann Intern Med. 2013;159: 584–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Chang Y, Hickman H. Food Insecurity and Perceived Diet Quality Among Low-Income Older Americans with Functional Limitations. Journal of nutrition education and behavior. 2018;50: 476–484. [DOI] [PubMed] [Google Scholar]
- [37].Petersen CL, Brooks JM, Titus AJ, Vasquez E, Batsis JA. Relationship Between Food Insecurity and Functional Limitations in Older Adults from 2005–2014 NHANES. J Nutr Gerontol Geriatr. 2019;38: 231–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Fernandes SG, Rodrigues AM, Nunes C, et al. Food Insecurity in Older Adults: Results From the Epidemiology of Chronic Diseases Cohort Study 3. Front Med (Lausanne). 2018;5: 203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Portela-Parra ET, Leung CW. Food Insecurity Is Associated with Lower Cognitive Functioning in a National Sample of Older Adults. The Journal of nutrition. 2019;149: 1812–1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Wong JC, Scott T, Wilde P, Li YG, Tucker KL, Gao X. Food Insecurity Is Associated with Subsequent Cognitive Decline in the Boston Puerto Rican Health Study. The Journal of nutrition. 2016;146: 1740–1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Na M, Dou N, Ji N, et al. Food Insecurity and Cognitive Function in Middle to Older Adulthood: A Systematic Review. Adv Nutr. 2020;11: 667–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Hamelin AM, Beaudry M, Habicht JP. Characterization of household food insecurity in Quebec: food and feelings. Soc Sci Med. 2002;54: 119–132. [DOI] [PubMed] [Google Scholar]
- [43].Laraia B Food Insecurity and Chronic Disease. Adv Nutr. 2013;4: 203–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. Journal of general internal medicine. 2007;22: 1018–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Parker ED, Widome R, Nettleton JA, Pereira MA. Food security and metabolic syndrome in U.S. adults and adolescents: findings from the National Health and Nutrition Examination Survey, 1999–2006. Annals of epidemiology. 2010;20: 364–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Pooler J, Levin M, Hoffman V, Karva F, Lewin-Zwerdling A. Implementing Food Security Screening and Referral for Older Patients in Primary Care: A Resource Guide and Toolkit. American Association of Retired Persons (AARP), 2016. [Google Scholar]
- [47].Wright L, Vance L, Sudduth C, Epps JB. The Impact of a Home-Delivered Meal Program on Nutritional Risk, Dietary Intake, Food Security, Loneliness, and Social Well-Being. J Nutr Gerontol Geriatr. 2015;34: 218–227. [DOI] [PubMed] [Google Scholar]
- [48].Vigil A Trends in Supplemental Nutrition Assistance Program Participation Rates: Fiscal Year 2010 to Fiscal Year 2017. Washington D.C.: Food and Nutrition Service, US Department of Agriculture, 2019. [Google Scholar]
- [49].Fey-Yensan NL, English C, Belyea M, Pacheco H. Food Stamp Program Participation and Perceived Food Insecurity in Older Adults. Top Clin Nutr. 2003;18: 262–267. [Google Scholar]
- [50].Zuniga K, McAuley E. Considerations in selection of diet assessment methods for examining the effect of nutrition on cognition. J Nutr Health Aging. 2015;19: 333–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1: Criteria for scoring the Healthy Eating Index-2015, Alternate Healthy Eating Index-2010, and Mediterranean Diet Score
Supplemental Table 2: Full statistical results from multivariate-adjusted linear regression models for the Healthy Eating Index-2015, Alternate Healthy Eating Index-2010, and the Mediterranean Diet Score
Supplemental Table 3: Full statistical results from multivariate-adjusted logistic regression models comparing individuals in the top quintile to the bottom four quintiles of Healthy Eating Index-2015, Alternate Healthy Eating Index-2010, and the Mediterranean Diet Score


