This study reports the ocular injuries sustained by survivors of the Port of Beirut blast in Beirut, Lebanon, on August 4, 2020.
Key Points
Question
What are the ocular injuries sustained by survivors of the August 4, 2020, Port of Beirut blast, one of the most powerful nonnuclear explosions in history?
Findings
In this study of 48 eyes of 39 patients treated at the American University of Beirut Medical Center, the injuries encountered were predominantly shrapnel based, with a relatively high rate of open globe injuries.
Meaning
A review of the responding physicians’ experience during the Port of Beirut blast may help guide future ophthalmic disaster response plans; reverting to basic approaches was necessary in the context of a malfunctioning electronic medical record system.
Abstract
Importance
A review of the injury patterns, treatment strategies, and responding physicians’ experience during the Port of Beirut blast may help guide future ophthalmic disaster response plans.
Objective
To present the ophthalmic injuries and difficulties encountered as a result of the Port of Beirut blast on August 4, 2020.
Design, Setting, and Participants
A retrospective medical record review of all patients who presented to the emergency department and 13 ophthalmology outpatient clinics at the American University of Beirut Medical Center for treatment of ophthalmic injuries sustained from the explosion in Port of Beirut, Beirut, Lebanon, from August 4 to the end of November 2020. Patients were identified from emergency records, outpatient records, and operative reports.
Main Outcomes and Measures
Types of ocular injuries, final best-corrected visual acuity, and need for surgical intervention were evaluated. Visual acuity was measured with correction based on noncycloplegic refraction using the Snellen medical record.
Exposures
Ocular or ocular adnexal injuries sustained from the Port of Beirut explosion.
Results
A total of 39 blast survivors with ocular injuries were included in this study. Twenty-two patients presented with ocular injuries on the day of the blast, and 17 patients presented within the following 3 months to the ophthalmology clinics for a total of 48 eyes of 39 patients were treated secondary to the blast. Thirty-five patients (89.6%) were adults, and 24 (61.5%) were female. A total of 21 patients (53.8%) required surgical intervention, more than half of which were urgently requested on the same day of presentation (14 [35.9%]). Most eye injuries were caused by debris and shrapnel from shattered glass leading to surface injury (26 [54.2%]), eyelid lacerations (20 [41.6%]), orbital fractures (14 [29.2%]), brow lacerations (10 [20.8%]), hyphema (9 [18.8%]), open globe injuries (10 [20.8%]), and other global injuries. Only 7 injured eyes (14.5%) had a final best-corrected visual acuity of less than 20/200, including all 4 open globe injuries with primary no light perception (8.3%) requiring enucleation or evisceration.
Conclusions and Relevance
In the aftermath of the Port of Beirut explosion, a review of the ophthalmic injuries showed a predominance of shrapnel-based injuries, many of which had a delayed presentation owing to the strain placed on health care services. Reverting to basic approaches was necessary in the context of a malfunctioning electronic medical record system.
Introduction
Shortly after 6 pm on August 4, 2020, white smoke and fire were noticed coming out of the Port of Beirut in Beirut, Lebanon. Minutes later, a devastating massive explosion ensued, creating a mushroomlike cloud and a supersonic blast wave that rippled through the densely populated capital city of Beirut, resulting in widespread destruction with at least 200 deaths, more than 6000 injured, and 300 000 citizens displaced from their homes.1,2 The cause was determined to be a detonation of around 2700 tons of ammonium nitrate, making it one of the largest nonnuclear explosions in history.3,4 The sheer magnitude of the blast was so strong that it generated seismic waves that were felt around 200 km away in the neighboring Mediterranean island of Cyprus.5
The explosion severely damaged multiple nearby hospitals and medical centers and paralyzed first aid services, which resulted in a massive surge and overflow of injuries to the remaining near hospitals’ emergency departments (EDs).4,6,7,8 At our tertiary care institution, the American University of Beirut Medical Center (AUBMC), a disaster code was activated and shortly afterwards, the ED was filled beyond capacity with moderate to severe casualties and mild injuries were immediately turned away at the door.
We aim to describe the experience of the ophthalmology team at AUBMC by presenting the different types of injuries treated as well as to detail the management of several unique and challenging cases. A review of their treatment provides insight into the unique injury patterns and highlights the importance of developing comprehensive disaster response strategies.
Methods
This is a single-center retrospective medical record review of patients who presented to the ED or the ophthalmology outpatient clinics at AUBMC from August until November 2020 with ocular or orbital injuries from the Port of Beirut explosion on August 4. This study was approved by the biomedical institutional review board at AUBMC and abides by the tenets of the Declaration of Helsinki.9 A waiver of patient consent was obtained from the institutional review board at AUBMC because this study poses no more than minimal risk to individuals. Patient permission for publication was obtained for all patients described in cases 1 to 5.
All patients were identified from outpatient records, emergency records, and operative reports. Outpatient records were retrieved from the clinic of all 12 ophthalmology faculty and the resident-run clinic at AUBMC within 3 months of the explosion. Data review was conducted from September 9 to January 15, 2020. The review was done through the electronic medical record system (Epic) by screening all patients seen by the ophthalmology team from the night of the explosion onwards. The review also included handwritten documentation and medical records of patients seen on the first day of the explosion when electronic documentation was limited. The data collected from the medical record review included patient demographics, eye examination (vision, intraocular pressure, anterior segment examination, fundus ophthalmoscopy), imaging results, treatment strategies, and patient outcomes. Ocular injuries involving the globe were classified according to the Birmingham Eye Trauma Terminology System at the time of medical record review, and 2 authors (W.J.K. and R.M.A.) independently reviewed the distribution with agreement. The Birmingham Eye Trauma Terminology System is a standardized classification system used to describe mechanical injuries to the eye globe and is particularly useful in the management of trauma cases requiring multidisciplinary care.10
Regarding the triage system initiated on the day of the blast, all patients were screened for ophthalmic complaints (decreased visual acuity, eye redness, eye pain, clear eye injuries), except for critically ill patients rushed to urgent life-saving surgeries, who were assessed later. Once an ophthalmic complaint was identified, the patient was assessed by an attending physician with the support of the ophthalmology residents or fellows. Visual acuity (pocket visual acuity chart), intraocular pressure (Tono-Pen; Reichert Technologies), pupils, and extraocular movements were assessed, then dilating drops were instilled and indirect ophthalmoscopy was performed. Some patients were not cleared for dilation and had to be examined in the days following the blast. Patients were then referred for surgery (performed by attending physicians) or further imaging. Repair of some eyelid lacerations had to be postponed until later in the night or to the next morning to prioritize more urgent cases. On follow-up, best-corrected visual acuity for all patients was measured based on a noncycloplegic refraction using the Snellen chart.
Results
At least 500 patients who presented to the ED on the night of the explosion were screened and evaluated for ocular or periocular injuries. The overall frequency and distribution of injuries has not yet been officially tallied. The number of injuries given is the most accurate estimate provided by the hospital at the time of manuscript submission. The ophthalmology team consisted of 4 attending physicians and 7 ophthalmology residents/fellows. All but 1 were on site or arrived within 15 minutes of the blast. The last to arrive had extensive damage to his home and car and therefore arrived on foot 1 hour after the blast.
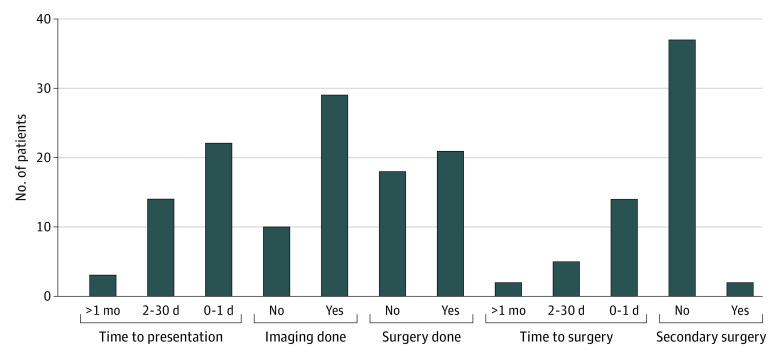
Twenty-two patients were treated by the ophthalmology team immediately after the blast for ocular or orbital injuries, and 14 patients required surgical intervention. In the coming 3 months, a total of 48 eyes of 39 patients with ocular injuries related to the Beirut blast were treated by the ophthalmology team at AUBMC, as patients continued to present to the ophthalmology clinics many weeks afterwards. All ocular injuries in were evaluated using Birmingham Eye Trauma Terminology System (eFigure 1 in the Supplement). A total of 21 patients (53.8%) required surgical intervention (Figure 1).
Figure 1. Patient Distribution According to Time of Presentation, Time of Surgical Intervention, and Need for Imaging or Surgery After the Port of Beirut Explosion.
Of the 39 patients treated, 35 (89.7%) were Lebanese, 24 (61.5%) were female, and 27 (69.2%) held Beirut as a primary residence. While most patients were adults (35 [89.6%]), we also treated 4 pediatric patients, one of whom had a scleral laceration with uveal prolapse requiring scleral suturing. Another child required evisceration that was performed by an ophthalmologist at another hospital before presenting to our institution for continuity of care.
Of 48 ophthalmic injuries treated, the most common ocular and orbital injuries were surface disease (26 [54.2%]), including chemical injury or abrasion; eyelid laceration (20 [41.6%]); orbital fracture (14 [29.2%]); brow laceration (10 [20.8%]); hyphema (9 [18.8%]); and open globe injuries (10 [20.8%]). Other injuries included vitreous hemorrhage, various retinal pathologies (hemorrhage, tears, detachment, and commotio retinae), optic nerve compression, retrobulbar hemorrhage, and intraocular foreign bodies (Table 1). Twenty patients (51.2%) had globe injury combined with oculoplastic or neuro-ophthalmologic injury. Only 5 patients (12.8%) had isolated oculoplastic injuries including eyelid laceration, brow laceration, and orbital fracture.
Table 1. Types of Ocular Injuries.
| Ophthalmic injury | No. (%) |
|---|---|
| Oculoplastic injury | |
| Orbital fracture | 14 (29.2) |
| Eyelid laceration | 20 (41.6) |
| Brow laceration | 10 (20.8) |
| Corneal injury | |
| Ocular surface injury | 26 (54.2) |
| Chemical | 6 (12.5) |
| Physical | 20 (41.7) |
| Retinal injury | |
| Commotio retinae | 4 (8.3) |
| Choroid rupture | 1 (2.1) |
| Retinal tear(s) | 1 (2.1) |
| Retinal detachment | 1 (2.1) |
| Bleeding/hemorrhage | |
| Hyphema | 9 (18.8) |
| Vitreous hemorrhage | 3 (6.3) |
| Retinal hemorrhage | 3 (6.3) |
| Retrobulbar hemorrhage | 2 (4.2) |
| Neurologic injury | |
| Optic nerve compression | 2 (4.3) |
| Central vision loss | 2 (4.3) |
| Nerve palsy | 2 (4.3) |
| Open globe injury | |
| Corneal laceration | 1 (2.1) |
| Scleral laceration | 1 (2.1) |
| Corneoscleral laceration | 6 (12.5) |
| Intraocular foreign body | 2 (4.3) |
Of 39 patients, 9 (23%) had bilateral eye involvement, and 10 (25.6%) needed eye-saving surgeries, including repair of open globes, foreign body removal, and repair of complicated orbital fractures with optic nerve compression; only 4 patients required minor surgery for isolated eyelid/brow laceration (Table 2). Two patients also required secondary surgeries (Figure 1). One patient underwent repair of left lower eyelid retraction secondary to left zygomaticomaxillary complex fracture repair at an outside hospital. Another patient had incomplete enucleation of the right eye done at another hospital and required revision surgery. The blast also left a few patients with nonsalvageable eyes, which required evisceration or enucleation. Of note, 6 patients (15.4%) first presented to outside hospitals where first aid treatment and urgent surgeries were done, then sought help at AUBMC for continuity of care or for specialized treatment. On initial encounter, 13 of 48 injured eyes (27.1%) had best-corrected visual acuity of less than 20/200, including 4 that had no light perception. In addition, 2 patients with ocular injuries were in a coma, and visual acuity could not be assessed. All resources were devoted to recovering the visual potential of every injured eye and priority was given to the patients with the most severe injuries. Only 7 injured eyes (14.5%) had a final best-corrected visual acuity of less than 20/200, including all 4 open globe injuries with primary no light perception (8.3%) that required enucleation or evisceration. The 2 patients who were in a coma did not have significant global injury and were later lost to follow-up.
Table 2. Number and Classification of Surgeries.
| Surgeries | No. of patients |
|---|---|
| Oculoplastic surgery | |
| Enucleation/evisceration | 4 |
| Zygomaticomaxillary complex fracture repair | 5 |
| Complicated medial orbital wall fracture repair | 1 |
| Isolated eyelid/brow laceration repair | 4 |
| Corneal/scleral laceration repair | 6 |
| Craniotomy for compressive lesion causing mass effect on prechiasmatic portion of the optic nerve | 1 |
| Total | 21 |
Patients were followed up regularly depending on their condition; however, 5 patients were lost to follow-up. The mean number of follow-up visits was 2, and the mean follow-up period was 2 months. Patients with severe injuries required more frequent visits, whereas those with less severe injuries or previously seen in outside hospitals did not require further follow-up. We also report a few cases that highlight the complexity of problems our ophthalmology team dealt with.
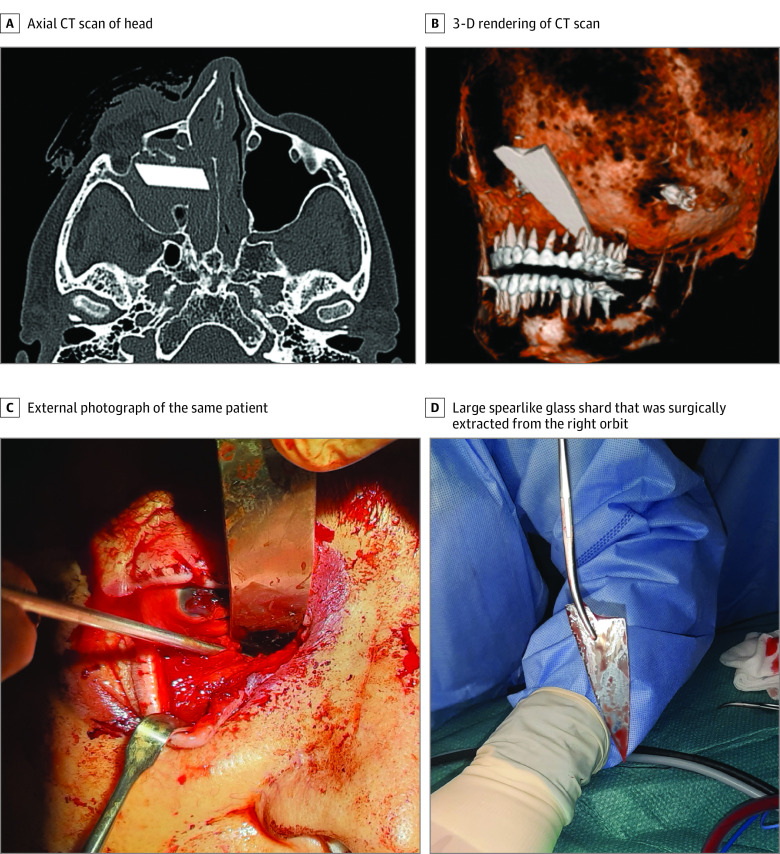
Case 1: Life-threatening Injury
An 80-year-old male individual presented with right eye injury and significant nasal epistaxis, in addition to multiple facial lacerations. Computed tomography scan revealed a large sharp-tipped foreign body lodged in the ethmoid and maxillary sinuses reaching the pharynx (Figure 2A and B). The patient was immediately taken to the operating room for exploration. The point of entry of the spearlike glass shrapnel appeared to be the right orbit, resulting in an open right globe (Figure 2C). Transcaruncular and inferior transconjunctival incisions were made, along with nasal endoscopic assistance. The glass piece was removed through the orbit, followed by control of bleeding (Figure 2D). The patient also underwent right eye evisceration and repair of full thickness eyelid and facial lacerations and had an uneventful postoperative course.
Figure 2. Life-threatening Injury to the Face .
A, Axial computed tomography (CT) scan of the head showing a large foreign body lodged in the right ethmoid and maxillary sinuses. B, Three-dimensional (3-D) rendering of the CT scan showing the sharp-tip foreign body penetrating facial structures reaching the pharynx. C, External photograph of the same patient during surgical exploration demonstrating the foreign body’s point of entry through the medial caruncle and orbit. D, Large spearlike glass shard that was surgically extracted from the right orbit.
Case 2: Typical Glass Injury to Periocular Area
A 56-year old woman presented with complex lacerations to the right forehead, brow, and eyelid (Figure 3A). The lacerations were deep, reaching the underlying bone, with disruption and prolapse of the retro-orbicularis oculi and preaponeurotic fat pads. Lacerations were primarily sutured, and the postoperative course was complicated with right supraorbital neuralgia and upper eyelid cicatricial retraction necessitating oral steroids and 5-fluorouracil injections.
Figure 3. Typical Facial and Ocular Injuries Secondary to Glass Shrapnel .
A, External photograph of a patient with a complex deep right brow and upper eyelid laceration. Note the orbital and retro-orbicularis oculi fat herniation. B, External photograph of a patient 7 weeks after the explosion, with resulting extensive facial and periocular scars and left eye phthisis bulbi secondary to multiple globe lacerations.
Case 3: Extensive Facial Injuries
A 49-year-old man presented with extensive facial injuries including left eyelid lacerations and extensive globe lacerations. He also had multiple widespread bodily injuries including injuries to the right forearm, hand, and leg, necessitating below-knee amputation and extensive forearm reconstruction. He developed left eye phthisis following suturing of globe lacerations and later underwent left eye evisceration, implant placement, and left upper eyelid secondary reconstruction with a Tenzel flap. His postoperative course was uncomplicated, and he underwent CO2 laser therapy for scar management (Figure 3B).
Case 4: Combined Glass Shrapnel and Overpressure Wave Injuries to Ocular Surface
A 27-year-old woman with a history of laser-assisted in situ keratomileusis 5 years earlier presented with a right eye corneoscleral laceration, which had to be sutured in the operating room. The left eye had significant corneal edema with no lacerations and vitreous hemorrhage on B scan and visual acuity of hand motion. While receiving topical steroids, the patient’s visual acuity improved a week later to 20/100 and 2 months later to 20/20, with an epithelial ingrowth under the laser-assisted in situ keratomileusis flap noted superotemporally (eFigure 2A and 2B in the Supplement).
Case 5: Glass Shrapnel Injury to Cornea
A 26-year-old woman presented with complex facial lacerations and a left eye partial thickness corneal laceration across the visual axis with 50% hyphema in the anterior chamber. Visual acuity was counting fingers near face. Two weeks after careful observation while receiving topical antibiotics and corticosteroids, the patient’s hyphema resolved and visual acuity improved to 20/80. However, the laceration was still uptaking fluorescein, so one 10-0 nylon suture was placed at the deepest area of corneal wound to approximate wound edges to hasten the healing process. There is currently residual corneal scarring with a best-corrected visual acuity of 20/40 (eFigure 2C and 2D in the Supplement).
Discussion
The Port of Beirut explosion is one of the largest nonnuclear explosions in history and is only historically outmatched by a few blasts, the greatest of which was the 1917 Halifax explosion in Canada.11 In the past decade, 2 similar but substantially less powerful ammonium nitrate blasts occurred in West Texas, Texas, in 2013, and Tianjin, China, in 2015.12,13 Similar to these aforementioned incidents, a fire preceded the Port of Beirut explosion and contributed to the large number of ocular injuries, as people watched the fire through their glass windows before the detonation.
The resulting storm of debris and shrapnel from shattered glass windows and building facades was the main source of injury to most patients.6 These secondary blast injuries are the most common form of ocular injuries associated with high explosives and the most severe threat to eyes, accounting for around 80% of ocular injuries seen in military warfare.14,15 This was also reflected in the present series, where surface injuries (eyelid laceration, brow laceration, corneal injury) were the most commonly encountered injuries (Table 1). Moreover, the high-velocity shrapnel explains the extensive damage to ocular and adnexal structures and the relatively high rate of open globe injuries (20.8%). This rate is comparable with the Oklahoma City bombing (22%) and Texas ammonium nitrate blast (42.9%) that similarly occurred in close proximity to residential buildings. In contrast, a substantially lower rate of open globe injuries (4.5%) was seen in the Boston marathon terrorist bombing, likely owing to the bomb’s ground level location in an outdoor setting.16 Our findings were consistent with the ocular injuries seen in the aforementioned incidents, however, at a much larger scale. The chemical injuries were also caused by the plumes of nitrous dioxide, in addition to contaminants from by-products of pesticides, pharmaceuticals, industrial chemicals, lead, and other potentially toxic material that were stored in the port.17,18
At our institution, despite having robust disaster contingency plans and an advanced electronic patient record system, the magnitude of casualties overwhelmed all hospital systems.8,19 More than 500 patients were received at the emergency services at our institution within the first few hours of the explosion, which greatly surpassed the hospital’s maximum emergency plan capacity of 300 patients.19 Disaster code was activated, and most residents and faculty reached the hospital (some by foot) despite personal shock, loss of property, and harm to relatives. Their focus, dedication, and quick instincts resulted in an efficient division of labor for the screening of all patients in the ED and prompt identification, triage, and treatment of severe vision-threatening injuries. Medical treatment was delayed for most patients with low acuity, and emergent care was mainly restricted to treating patients with severe injuries. For most patients, immediate clinical documentation reverted back to pen and paper because of power outages, insufficient electronic stations, a spotty institutional Wi-Fi connection, and incomplete patient registrations at triage. Initial ophthalmologic examination was limited and, in some cases, delayed depending on the patients’ condition, associated systemic injuries, and need for life-saving care.
Ocular injuries are frequently encountered in patients who were affected by the blast and occur in up to 28% of those who survived the blast.20 In our series, 22 patients (4.4%) admitted to the ED had ocular or ocular adnexal injuries, a rate comparable with the Texas ammonium nitrate explosion (6.4%) and other explosions in urban cities such as the Oklahoma City terrorist bombing (8%), along with similar mechanisms of injury.12,21 We estimate the true rate to be higher than reported as many patients with relatively minor ocular injuries were denied entry to the ED and treated elsewhere.
The statistics from the Lebanese Ophthalmological Society in the aftermath of the blast account for more than 400 ophthalmic injuries received in Beirut hospitals, excluding extraocular injuries such as orbital fractures. A total of 60 ocular surgeries were performed, 48 of these surgeries were performed on open globe injuries. A total of 17 eyes required additional ocular surgeries. Ten patients developed functional blindness.
Multiple risk factors have been shown to affect the visual prognosis after blast injuries, including vitreous hemorrhage, retinal detachment, and globe rupture or penetration.22 However, initial best-corrected visual acuity appears to be the single most important factor in predicting final visual acuity in patients who were affected by the blast.20 In review of previous blast events, individuals with primary visual acuity of no light perception had the worst visual outcomes. In our case, all 4 injured eyes with primary visual acuity of no light perception required enucleation or evisceration. The overall rate of enucleation (8.3%) is comparable with the 2015 Tianjin explosion (9.6%) but was much lower than the estimated 42% enucleation rate seen in the 1917 Halifax explosion. This can be attributed to advanced modern treatment options and decreased fear of sympathetic ophthalmia from penetrating eye injuries.13,23
Limitations
Our study, although comprehensive, is not without its limitations. As the major tertiary hospital in Beirut and the largest unscathed center at close proximity to the blast, we received the largest number of patients who were affected by the blast. Low-acuity ophthalmic injuries were likely missed because those patients were referred to other nearby hospitals or clinics. Therefore, the study may have failed to capture mild ocular injuries. Furthermore, on the night of the blast, there was little time for ophthalmologists to wait for consults and make detailed records for patients. More accurate examination information came from follow-ups in the days after the blast. Some patients did not return for follow-up; therefore, a more comprehensive assessment was not possible for all patients. A more rigorous quantitative statistical analysis could not be performed because of the small sample size and the paucity of accurate official documentation on the number and distribution of injuries.
Conclusions
We present a review of the ocular injuries that were encountered at the AUBMC following the 2020 Port of Beirut explosion. We also highlighted a few representative cases and shared the ophthalmologists’ perspectives in the management of this difficult event. The injuries encountered were predominantly shrapnel based, with close to half presenting in the days following the blast owing to the strain placed on health care services. A power outage, spotty internet connection, and a malfunctioning electronic medical record system made it necessary for medical staff to go back to basics by temporarily reverting to paper medical records. In our opinion, this disaster showed how physicians can be resilient and have strong intuitions to manage tragic situations sometimes by resorting to basic approaches. The Port of Beirut explosion overwhelmed all hospital systems despite all existing disaster response strategies and an advanced electronic health care system, with an almost complete breakdown of the latter. The authors believe that such scenarios should be included in disaster emergency preparation plans despite the low rate of such severe and unfortunate events.
eFigure 1. Ocular injuries that were encountered classified according to the Birmingham Eye Trauma Terminology System
eFigure 2. A, Anterior segment OCT 8 weeks after presentation demonstrating the epithelial ingrowth under the LASIK flap B, External slit lamp photograph of the same eye showing supero-temporal epithelial ingrowth C, Anterior segment OCT of the left eye of her sister, demonstrating a partial thickness corneal laceration that was secondarily sutured 2 weeks after presentation D, External slit lamp photograph of the left eye 8 weeks after presentation, demonstrating a central corneal scar
References
- 1.Agapiou A. Damage proxy map of the Beirut explosion on 4th of august 2020 as observed from the Copernicus sensors. Sensors (Basel). 2020;20(21):1-21. doi: 10.3390/s20216382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Devi S. Lebanon faces humanitarian emergency after blast. Lancet. 2020;396(10249):456. doi: 10.1016/S0140-6736(20)31750-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rigby SE, Lodge TJ, Alotaibi S, et al. . Preliminary yield estimation of the 2020 Beirut explosion using video footage from social media. Shock Waves. 2020;30(6):671-675. doi: 10.1007/s00193-020-00970-z [DOI] [Google Scholar]
- 4.Landry MD, Alameddine M, Jesus TS, Sassine S, Koueik E, Raman SR. BMC health services research title: the 2020 blast in the port of Beirut: can the Lebanese health system “build back better”? BMC Health Serv Res. 2020;20(1):1040. doi: 10.1186/s12913-020-05906-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guglielmi G. Why Beirut’s ammonium nitrate blast was so devastating. Published online August 10, 2020. Nature. doi: 10.1038/d41586-020-02361-x [DOI] [PubMed] [Google Scholar]
- 6.Dyer O. Beirut’s battered hospitals struggle in aftermath of explosion. BMJ. 2020;370:m3171. doi: 10.1136/bmj.m3171 [DOI] [PubMed] [Google Scholar]
- 7.Farha L, Abi Jaoude J. Lebanese healthcare system: how will the aftermath look? Cureus. 2020;12(9):e10270. doi: 10.7759/cureus.10270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El Sayed MJ. Beirut ammonium nitrate explosion: a man-made disaster in times of the COVID-19 pandemic. Disaster Med Public Health Prep. 2020;1-5. doi: 10.1017/dmp.2020.451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 10.Kuhn F, Morris R, Witherspoon CD. Birmingham Eye Trauma Terminology (BETT): terminology and classification of mechanical eye injuries. Ophthalmol Clin North Am. 2002;15(2):139-143, v. doi: 10.1016/S0896-1549(02)00004-4 [DOI] [PubMed] [Google Scholar]
- 11.Hernandez M, Scarr S. How powerful was the Beirut blast? Reuters. Published August 14, 2020. Accessed March 1, 2021. https://graphics.reuters.com/LEBANON-SECURITY/BLAST/yzdpxnmqbpx/
- 12.Zuzek C. The night West blew up. Tex Med. 2013;109(7):41-45. [PubMed] [Google Scholar]
- 13.Liu Y, Feng K, Jiang H, et al. Characteristics and treatments of ocular blast injury in Tianjin explosion in China. BMC Ophthalmol. 2020;20(1):185. doi: 10.1186/s12886-020-01448-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scott R. The injured eye. Philos Trans R Soc Lond B Biol Sci. 2011;366(1562):251-260. doi: 10.1098/rstb.2010.0234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abbotts R, Harrison SE, Cooper GL. Primary blast injuries to the eye: a review of the evidence. J R Army Med Corps. 2007;153(2):119-123. doi: 10.1136/jramc-153-02-10 [DOI] [PubMed] [Google Scholar]
- 16.Yonekawa Y, Hacker HD, Lehman RE, et al. Ocular blast injuries in mass-casualty incidents: the marathon bombing in Boston, Massachusetts, and the fertilizer plant explosion in West, Texas. Ophthalmology. 2014;121(9):1670-6.e1. doi: 10.1016/j.ophtha.2014.04.004 [DOI] [PubMed] [Google Scholar]
- 17.Schlein L. UN warns of hazardous waste threat after Beirut blast. Voice of America. Published September 2, 2020. Accessed May 1, 2021. https://www.voanews.com/middle-east/un-warns-hazardous-waste-threat-after-beirut-blast
- 18.Neill P. Major air pollution concern following Beirut explosion. Air Quality News. Published August 5, 2020. Accessed May 1, 2021. https://airqualitynews.com/2020/08/05/major-air-pollution-concern-following-beruit-explosion
- 19.Plaster L. The Beirut blast: reflections of an emergency physician. Emergency Physicians International. Published September 1, 2020. Accessed March 1, 2021. https://www.epijournal.com/home/2020/9/1/the-beirut-blast-reflections-of-an-emergency-physician
- 20.Morley MG, Nguyen JK, Heier JS, Shingleton BJ, Pasternak JF, Bower KS. Blast eye injuries: a review for first responders. Disaster Med Public Health Prep. 2010;4(2):154-160. doi: 10.1001/dmp.v4n2.hra10003 [DOI] [PubMed] [Google Scholar]
- 21.Mines M, Thach A, Mallonee S, Hildebrand L, Shariat S. Ocular injuries sustained by survivors of the Oklahoma City bombing. Ophthalmology. 2000;107(5):837-843. doi: 10.1016/S0161-6420(00)00030-0 [DOI] [PubMed] [Google Scholar]
- 22.Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008;115(1):202-209. doi: 10.1016/j.ophtha.2007.04.008 [DOI] [PubMed] [Google Scholar]
- 23.McAlister CN, Murray TJ, Lakosha H, Maxner CE. The Halifax disaster (1917): eye injuries and their care. Br J Ophthalmol. 2007;91(6):832-835. doi: 10.1136/bjo.2006.113878 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Ocular injuries that were encountered classified according to the Birmingham Eye Trauma Terminology System
eFigure 2. A, Anterior segment OCT 8 weeks after presentation demonstrating the epithelial ingrowth under the LASIK flap B, External slit lamp photograph of the same eye showing supero-temporal epithelial ingrowth C, Anterior segment OCT of the left eye of her sister, demonstrating a partial thickness corneal laceration that was secondarily sutured 2 weeks after presentation D, External slit lamp photograph of the left eye 8 weeks after presentation, demonstrating a central corneal scar