Abstract
Aims
To assess the clinical relevance of a history of atrial fibrillation (AF) in hospitalized patients with coronavirus disease 2019 (COVID-19).
Methods and results
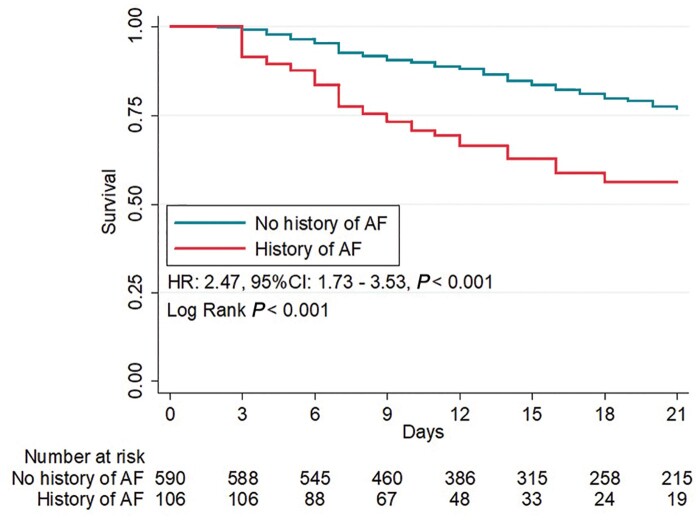
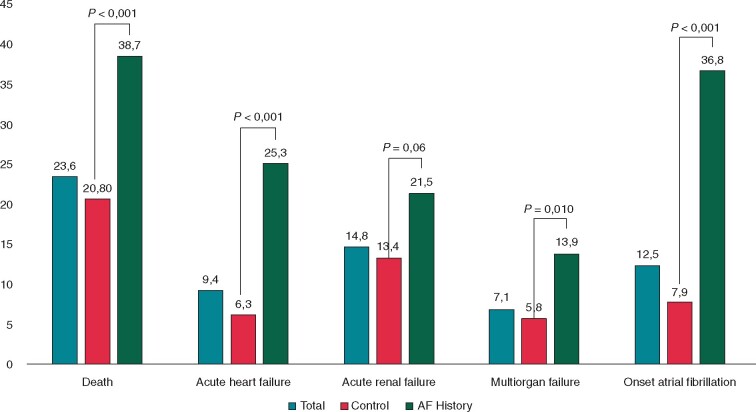
We enrolled 696 consecutive patients (mean age 67.4 ± 13.2 years, 69.7% males) admitted for COVID-19 in 13 Italian cardiology centres between 1 March and 9 April 2020. One hundred and six patients (15%) had a history of AF and the median hospitalization length was 14 days (interquartile range 9–24). Patients with a history of AF were older and with a higher burden of cardiovascular risk factors. Compared to patients without AF, they showed a higher rate of in-hospital death (38.7% vs. 20.8%; P < 0.001). History of AF was associated with an increased risk of death after adjustment for clinical confounders related to COVID-19 severity and cardiovascular comorbidities, including history of heart failure (HF) and increased plasma troponin [adjusted hazard ratio (HR): 1.73; 95% confidence interval (CI) 1.06–2.84; P = 0.029]. Patients with a history of AF also had more in-hospital clinical events including new-onset AF (36.8% vs. 7.9%; P < 0.001), acute HF (25.3% vs. 6.3%; P < 0.001), and multiorgan failure (13.9% vs. 5.8%; P = 0.010). The association between AF and worse outcome was not modified by previous or concomitant use of anticoagulants or steroid therapy (P for interaction >0.05 for both) and was not related to stroke or bleeding events.
Conclusion
Among hospitalized patients with COVID-19, a history of AF contributes to worse clinical course with a higher mortality and in-hospital events including new-onset AF, acute HF, and multiorgan failure. The mortality risk remains significant after adjustment for variables associated with COVID-19 severity and comorbidities.
Keywords: Coronavirus disease 2019, Severe acute respiratory syndrome coronavirus-2 infection, Atrial fibrillation, Outcome
What’s new?
This is the first large study assessing the clinical and prognostic meaning of pre-existing atrial fibrillation (AF) and the incidence of new-onset AF in critically ill coronavirus disease 2019 (COVID-19) patients.
History of AF is associated with a higher rate of death and increased risk of complications during hospital stay.
Along with other known comorbidities and COVID-19 severity parameters, AF may represent a marker of increased mortality risk, not related to stroke or bleeding events.
Introduction
The novel coronavirus disease (COVID-19) outbreak, caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), is deeply influencing worldwide healthcare systems with more than 120 million affected people as of March 2021.1
Interstitial pneumonia and acute respiratory distress syndrome represent the most common clinical manifestations.1 It has been also shown that the cardiovascular (CV) system is often involved and subjects with previous CV disease are at a higher risk of worse events.2 Atrial fibrillation (AF) represents a well-known CV risk factor and cause of mortality in the general population. Nevertheless, its prevalence and clinical meaning have been less described in COVID-19 patients. Few studies showed that atrial arrhythmias may be a sign of cardiac involvement in COVID-19 disease,3 and sinus rhythm at admission in COVID-19 patients has been shown to be associated with better prognosis compared with AF rhythm.4 Also, new-onset AF can occur as a relevant clinical event during the in-hospital course of patients with COVID-19, but its incidence has not been well explored in large cohorts of affected patients.
The aim of our report is to evaluate the clinical and prognostic meaning of pre-existing AF and to assess the incidence of new-onset AF during the clinical course of COVID-19 in patients enrolled in the Cardio-COVID-Italy study, a multicentre retrospective, observational study.5
Methods
Study population
The Cardio-COVID study is a retrospective, multicentre, observational study that included consecutive patients with laboratory-confirmed COVID-19 admitted to 13 Cardiology Units in Italy from 1 March to 9 April 2020. All patients underwent diagnosis of COVID-19 by the amplification of SARS-CoV-2 RNA by real-time reverse transcriptase–polymerase chain reaction of pharyngeal swabs or lower respiratory tract aspirates. The study complied with the Declaration of Helsinki and was approved by the ethical committee of Spedali Civili di Brescia, Brescia, Italy (no. NP 4105) and of each recruiting centre. Informed consent was obtained from all patients who could give it. Patients were deidentified (anonymized) for data analysis.
Data collection
Patients’ data included demographics, medical history, in-hospital clinical course, treatment, and in-hospital outcomes and were extracted from the hospital medical records. History of AF was assessed through the collection of anamnestic data. Atrial fibrillation subtypes (paroxysmal, persistent, and permanent) were defined according to the recent AF guidelines.6 Electrocardiogram (ECG) was recorded at admission during the in-hospital stay and at discharge. Electrocardiogram analysis was performed by experienced cardiologists according to standard definitions and diagnostic criteria. New-onset AF was defined by the occurrence of AF at ECG during the in-hospital stay and not present at admission. Laboratory exams were collected at the time of hospitalization and during the hospital stay upon clinical indications. The Chronic Kidney Disease-Epidemiology Collaboration equation was used to estimate glomerular filtration rate (eGFR). Chest X-ray and echocardiography were performed when clinically indicated.
Statistical analysis
Patients were stratified based on their history of AF. Differences according to the new-onset AF are analysed in Supplementary material online. Normally distributed continuous variables were reported as means and standard deviations, skewed variables as medians and interquartile ranges, and dichotomous variables as counts and percentages.
Comparisons between groups were made using Student’s t-test for means, Wilcoxon test for medians, and χ2 test for proportions. Survival curves were obtained using the Kaplan–Meier analysis and compared among patients with vs. without history of AF using the log-rank test. Cox regression analysis was performed to identify the variables that were significantly associated with an increased risk of death (Supplementary material online, Table S1). The number of variables entered into the Cox regression model was limited according to the number of events, based on the principle of not having more than 1 variable every 10 events. The variables selected for the final model had to be clinically significant and associated with an increased risk of death at univariate analysis (P-value ≤ 0.01). The variables entered into the Cox regression model were demographic and clinical variables, including age, sex, HF, coronary artery disease, AF, hypertension, previous treatment with oral anticoagulant, and variables measured at the time of admission, including creatinine clearance, oxygen saturation, serum troponin, C-reactive protein, red blood count, and haemoglobin.
A two-tailed P-value <0.05 was considered statistically significant. Statistical analysis was performed using STATA statistical software version 9.4 (StataCorp LLC, College Station, TX, USA).
Results
Clinical characteristics
The study included 696 consecutive patients, mean age was 67.4 ± 13.2 years, 69.7% were males. One hundred and six patients (15%) had a history of AF. Demographic and clinical characteristics of the patients stratified by history of AF are shown in Table 1. Of these, 36 (36%) suffered from paroxysmal AF, 14 (14%) from persistent AF, and 49 (49%) from permanent AF. Compared with controls, patients with a history of AF were older, with a higher prevalence of heart failure (HF) and CV risk factors (such as hypertension, dyslipidaemia, diabetes) and ischaemic heart disease. Also, other comorbidities, including chronic kidney disease and chronic obstructive pulmonary disease, were more frequent in those with a history of AF. As expected, patients with a history of AF were more likely to receive oral anticoagulant treatment (both warfarin and direct oral anticoagulants, DOACs) and treatment with ACEi/ARBs, mineralocorticoid receptor antagonists, beta-blockers, and statins. At admission, patients with a history of AF showed higher body temperature and slightly lower systolic and diastolic blood pressure.
Table 1.
Clinical characteristics, laboratory and echocardiographic findings, in-hospital management, and outcome of the study population stratified by history of atrial fibrillation
| Variables | Total (N = 696) | No history of atrial fibrillation (N = 590) | History of atrial fibrillation (N = 106) | P-value |
|---|---|---|---|---|
| Clinical characteristics | ||||
| Age (years) | 67.4 ± 13.2 | 65.8 ± 13.0 | 75.8 ± 10.9 | <0.001 |
| Sex (male) | 485 (69.7) | 414 (70.2) | 71 (67.0) | 0.51 |
| Body mass index (kg/m2) | 27.3 ± 5.3 | 27.4 ± 5.2 | 26.6 ± 5.8 | 0.21 |
| Smoker, n (%) | 160 (27.2) | 133 (26.2) | 27 (33.3) | 0.18 |
| Hypertension, n (%) | 398 (57.2) | 315 (53.4) | 83 (78.3) | <0.001 |
| Hyperdyslipidaemia, n (%) | 193 (27.8) | 140 (23.8) | 53 (50.0) | <0.001 |
| Diabetes, n (%) | 162 (23.3) | 125 (21.2) | 37 (34.9) | 0.002 |
| Heart failure | 93 (13.4) | 51 (8.6) | 42 (39.6) | <0.001 |
| AF, n (%) | 106 (15.2) | 0 (0) | 106 (100) | <0.001 |
| Paroxysmal AF | – | – | 36 (36) | |
| Persistent AF | – | – | 14 (14) | |
| Permanent AF | – | – | 49 (49) | |
| Coronary artery disease, n (%) | 148 (21.3) | 104 (17.6) | 44 (41.5) | <0.001 |
| Previous percutaneous valve implantation, n (%) | 23 (3.3) | 15 (2.5) | 8 (7.5) | 0.008 |
| Heart transplant/LVAD, n (%) | 4 (0.6) | 4 (0.7) | 0 0 | 0.40 |
| COPD, n (%) | 68 (9.8) | 45 (7.6) | 23 (21.7) | <0.001 |
| CKD, n (%) | 128 (18.4) | 80 (13.6) | 48 (45.3) | <0.001 |
| Treatment before hospitalization | ||||
| ACE-i/ARBs/ARNI, n (%) | 250 (38.2) | 201 (36.3) | 49 (49.0) | 0.016 |
| Mineralocorticoids, n (%) | 43 (8.0) | 27 (5.9) | 16 (20.8) | <0.001 |
| Beta-blockers, n (%) | 249 (38.0) | 185 (33.3) | 64 (64.6) | <0.001 |
| Direct oral anticoagulants, n (%) | 48 (7.4) | 11 (2.0) | 37 (37.0) | <0.001 |
| Warfarin, n (%) | 49 (7.5) | 24 (4.4) | 25 (24.8) | <0.001 |
| Statins, n (%) | 181 (27.5) | 131 (23.5) | 50 (50.0) | <0.001 |
| Baseline findings | ||||
| Temperature (°C) | 37.3 ± 1.0 | 37.3 ± 1.0 | 36.9 ± 1.0 | <0.001 |
| Fever, n (%) | 447 (64.4) | 396 (67.2) | 51 (48.6) | <0.001 |
| Systolic blood pressure (mmHg) | 129.7 ± 21.7 | 130.5 ± 21.3 | 126.0 ± 21.6 | <0.001 |
| Heart rate (b.p.m.) | 86.7 ± 18.1 | 87 ± 16.7 | 81.6 ± 14.3 | 0.30 |
| Respiratory rate ≥22, n (%) | 279 (52.1) | 246 (53.5) | 33 (43.4) | 0.10 |
| Oxygen saturation (%) | 90.4 ± 7.7 | 90.3 ± 7.7 | 91.4 ± 7.8 | 0.15 |
| SOFA score ≥3, n (%) | 197 (43.3) | 161 (41.4) | 36 (54.5) | 0.046 |
| Laboratory measurements | ||||
| PaO2/FiO2 (mmHg/%) | 235.2 ± 131.7 | 228.9 ± 133.9 | 270.0 ± 113.5 | 0.007 |
| Red blood cell count (×106/µL) | 4.5 (4.0–4.9) | 4.5 (4.1–4.9) | 4.3 (3.7–4.7) | <0.001 |
| Haemoglobin (g/dL) | 13.4 (11.8–14.4) | 13.5 (12.1–14.6) | 12.2 (10.2–13.9) | <0.001 |
| Haematocrit (%) | 39.1 (35.5–42.8) | 39.5 (36.1–42.9) | 36.5 (30.9–41.3) | <0.001 |
| White blood cell count (per μL) | 6815 (5000–9330) | 6730 (5000–9100) | 7460 (5100–10020) | 0.17 |
| Lymphocytes count (per μL) | 930 (621–1300) | 944 (621–1300) | 900 (670–1250) | 0.58 |
| Platelets count (×103/µL) | 204 (156–270) | 207 (155–274) | 194.5 (159–251) | 0.42 |
| Creatinine (mg/dL) | 1.0 (0.8–1.3) | 1.0 (0.8–1.2) | 1.3 (0.9–1.9) | <0.001 |
| eGFR (CKD-EPI) (mL/min) | 74 (50.1 –90.4) | 78.6 (57.2–92.3) | 49.9 (31–64.7) | <0.001 |
| Sodium (mEq/L) | 138 (135–140) | 137 (135–140) | 138 (136–141) | 0.022 |
| Potassium (mEq/L) | 3.9 (3.6–4.3) | 3.9 (3.6–4.3) | 4.0 (3.7–4.6) | 0.10 |
| CRP on admission (mg/dL) | 23.7 (11.0–36.0) | 24.2 (11.2–36.1) | 20.9 (92.0–34.6) | 0.27 |
| Peak CRP (mg/dL) | 98.8 (29.8–179.0) | 100.4 (31.4–186.9) | 79.0 (21.2–150.2) | 0.023 |
| Elevated troponin,a n (%) | 276 (45.3) | 209 (41.1) | 67 (67.0) | <0.001 |
| NT-proBNP (pg/mL) | 304.5 (96.5–1193.0) | 211 (87.5–660) | 3094 (1298.0–6276.5) | <0.001 |
| D-dimer (ng/mL) | 870 (431.5–1803.5) | 870 (430–1800) | 870 (464–1876) | 0.71 |
| Aspartate transaminase (u/L) | 41 (26–63) | 42 (27–64) | 31 (21–63) | 0.007 |
| INR | 1.1 (1.0–1.2) | 1.1 (1.0–1.2) | 1.2 (1.0–1.5) | <0.001 |
Values are reported as means ± standard deviations or medians (interquartile ranges).
ACE-i, angiotensin-converting enzyme inhibitors; AF, atrial fibrillation; ARBs, angiotensin receptor blockers; ARDS, acute respiratory distress syndrome; ARNI, angiotensin receptor-neprilysin inhibitor; COPD, chronic obstructive pulmonary disease; CKD, chronic kidney disease (eGFR < 60 mL/min/m2); CKD-EPI, chronic kidney disease epidemiology collaboration formula; CRP, C reactive protein; fever, temperature >37.5°C; eGFR, estimated glomerular filtration rate; FiO2, fraction of inspired oxygen; INR, international normalized ratio; No., number of patients; NT-proBNP, N-terminal-pro-hormone brain natriuretic peptide.
Elevated troponin value was defined as above the 99% percentile of normal values.
Laboratory findings are summarized in Table 1. Patients with AF had lower haemoglobin levels, worse renal function and higher NT-proBNP plasma levels [3094 (1298–6276) vs. 211 (87.5–660) pg/mL, P < 0.001]. Serum troponin levels were more likely to be elevated among AF patients (67.0% vs. 41.1%, P < 0.001).
Patients with a history of AF also showed lower left ventricle ejection fraction (LVEF) (46.1 ± 12.6% vs. 54.2 ± 10.3%; P < 0.001), although in-hospital echocardiographic measurements were only available for 262 patients, of whom 56 in the AF group.
Data about in-hospital management and outcome are shown in Table 2. Patients without a history of AF were less likely to be treated with hydroxychloroquine, anti-interleukin agents (e.g. tocilizumab), and corticosteroids. Oxygen saturation was similar across the two groups. Patients with a history of AF showed higher PaO2/FiO2 and were less likely to be treated with non-invasive ventilation and intubation compared with the others (26.9% vs. 46.4% and 3.8% vs. 17.5%, P < 0.001 for both). Patients ‘too sick’ for invasive ventilatory support were more frequent in the AF group (34.3% vs. 20.2%, P = 0.002) (Table 2).
Table 2.
In-hospital management and outcome of the study population stratified by history of atrial fibrillation
| Variables | Total (N = 696) | No history of atrial fibrillation (N = 590) | History of atrial fibrillation (N = 106) | P-value |
|---|---|---|---|---|
| In-hospital treatment | ||||
| Hydroxychloroquine, n (%) | 580 (83.9) | 500 (85.5) | 80 (75.5) | 0.010 |
| Lopinavir/ritonavir, n (%) | 185 (26.8) | 153 (26.2) | 32 (30.2) | 0.39 |
| Darunavir/ritonavir, n (%) | 157 (26.8) | 18 (17.0) | 16 (18.0) | 0.032 |
| Tocilizumab, n (%) | 80 (11.6) | 76 (13) | 4 (3.8) | 0.006 |
| Corticosteroids, n (%) | 343 (49.6) | 303 (51.8) | 40 (37.7) | 0.008 |
| Antibiotics, n (%) | 609 (88.1) | 517 (88.4) | 92 (86.8) | 0.64 |
| Heparin, n (%) | 472 (73.1) | 412 (75.3) | 60 (60.6) | 0.002 |
| Ventilatory supporta | ||||
| Oxygen support with FiO2 <50% | 301 (43.7) | 240 (41.1) | 61 (58.1) | 0.001 |
| Oxygen support with FiO2 ≥50% | 380 (55.9) | 332 (57.6) | 48 (46.2) | 0.030 |
| Non-invasive ventilation, n (%) | 300 (43.5) | 272 (46.4) | 28 (26.9) | <0.001 |
| Intubation, n (%) | 103 (17.5) | 102 (17.0) | 4 (3.8) | <0.001 |
| Too sick for intubation, n (%) | 132 (22.7) | 98 (20.2) | 35 (34.3) | 0.002 |
| Outcomes | ||||
| Death, n (%) | 164 (23.6) | 123 (20.8) | 41 (38.7) | <0.001 |
| Cause of death | ||||
| Respiratory insufficiency | 125 (67.6) | 96 (68.1) | 29 (65.9) | 0.79 |
| Acute MI | 5 (2.7) | 3 (2.1) | 2 (4.5) | 0.39 |
| Pulmonary embolism | 13 (7.0) | 13 (9.2) | 0 0 | 0.037 |
| Multiorgan failure | 31 (18.9) | 21 (17.1) | 10 (24.3) | 0.97 |
| Acute heart failure, n (%) | 52 (9.4) | 29 (6.3) | 23 (25.3) | <0.001 |
| Atrial fibrillation onset, n (%) | 68 (12.5) | 36 (7.9) | 32 (36.8) | <0.001 |
| STEMI, n (%) | 11 (1.6) | 10 (1.7) | 1 (1.0) | 0.56 |
| NSTEMI, n (%) | 17 (3.1) | 11 (2.4) | 6 (6.6) | 0.033 |
| Ventricular arrhythmia, n (%) | 8 (1.2) | 5 (0.9) | 3 (2.9) | 0.08 |
| Stroke event | 3 (0.4) | 2 (0.3) | 1 (1.0) | 0.39 |
| Bleeding | 5 (2.7) | 4 (2.8) | 1 (2.3) | 0.84 |
| Pulmonary embolism, n (%) | 52 (7.6) | 49 (8.5) | 3 (2.9) | 0.046 |
| Other thromboembolic events, venous or arterial, n (%) | 61 (8.8) | 56 (9.5) | 5 (4.7) | 0.11 |
| ARDS, n (%) | 100 (17.3) | 94 (19.2) | 6 (6.7) | 0.004 |
| Sepsis, n (%) | 68 (10.1) | 59 (10.3) | 9 (8.7) | 0.60 |
| Acute renal failure, n (%) | 72 (14.8) | 55 (13.4) | 17 (21.5) | 0.06 |
| Multiorgan failure, n (%) | 34 (7.1) | 23 (5.8) | 11 (13.9) | 0.010 |
Values are reported as means ± standard deviations or medians (interquartile ranges).
FiO2, fraction of inspired oxygen; MI, myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; PaO2, oxygen partial pressure at arterial gas analysis; STEMI, ST-elevation myocardial infarction.
Patients could receive more than one ventilatory support during hospitalization.
In-hospital mortality
Median hospitalization length of stay was 14 days (interquartile range 9–24). In-hospital death occurred in 164 patients (23.6%). Patients with a history of AF had higher mortality (38.7% vs. 20.8%, P < 0.001) (Table 1). Kaplan–Meier survival curves are shown in Figure 1. History of AF was associated with an increased risk of death at both univariate [hazard ratio (HR) 2.47, 95% confidence interval (CI) 1.73–3.53; P < 0.001] (Table 3) and multivariable analysis including demographic and clinical variables (adjusted HR 1.73, 95% CI 1.06–2.84; P = 0.029) (Table 3). The higher rate of death was not related to stroke or bleeding events (2.3% vs. 2.8%, P = 0.84 and 1.0% vs. 0.3%, P = 0.39, respectively). Similar results were observed when adding potential confounders to the main model (Supplementary material online, Table S1). The role of in-hospital treatment was evaluated in exploratory analyses. The association between history of AF and mortality was not modified by the previous or in-hospital use of anticoagulants (P for interaction = 0.91) and in-hospital steroid treatment (P for interaction = 0.98). The rate of mortality did not differ across AF subtype (36% for paroxysmal AF vs. 35% for persistent AF vs. 40% for permanent AF, P = 0.65).
Figure 1.
Kaplan–Meier survival curves stratified by history of AF. AF, atrial fibrillation; CI, confidence interval; HR, hazard ratio.
Table 3.
Univariate and multivariable Cox regression model for in-hospital death
| Univariable |
Multivariable |
||||
|---|---|---|---|---|---|
| Level/units | HR (95% CI) | P-value | HR (95% CI) | P-value | |
| Clinical characteristics | |||||
| Age | +5 years | 1.06 (1.05–1.08) | <0.001 | 1.28 (1.14–1.43) | <0.001 |
| Gender | Male vs. female | 1.32 (0.92–1.90) | 0.125 | 2.12 (1.26–3.56) | 0.005 |
| Heart failure | Yes vs. no | 2.44 (1.70–3.52) | <0.001 | 1.78 (1.05–3.03) | 0.033 |
| Hypertension | Yes vs. no | 1.91 (1.37–2.67) | <0.001 | 1.01 (0.64–1.60) | 0.96 |
| Atrial fibrillation | Yes vs. no | 2.47 (1.73–3.53) | <0.001 | 1.73 (1.06–2.84) | 0.029 |
| Ischaemic cardiomyopahty | Yes vs. no | 2.28 (1.65–3.16) | <0.001 | 1.02 (0.63–1.66) | 0.922 |
| Treatment before hospitalization | |||||
| Anticoagulation therapy | Yes vs. no | 1.43 (0.94–2.17) | 0.091 | 0.73 (0.43–1.24) | 0.250 |
| Baseline findings | |||||
| Oxygen saturation | +5% | 0.96 (0.95–0.98) | <0.001 | 0.96 (0.94–0.98) | <0.001 |
| Laboratory measurements | |||||
| Red blood cell count | +1 ×106/µL | 0.68 (0.54–0.86) | 0.001 | 0.51 (0.28–0.92) | 0.025 |
| Haemoglobin | +1 g/dL | 0.92 (0.85–0.98) | 0.018 | 1.15 (0.94–1.41) | 0.183 |
| eGFR (CKD-EPI) | +10 mL/min | 1.13 (1.05–1.21) | 0.001 | 0.99 (0.99–1.00) | 0.280 |
| CRP peak | +1 mg/dL | 1.00 (1.00–1.00) | <0.001 | 1.37 (1.09–1.72) | 0.007 |
| Troponin | Elevated vs. normal | 3.19 (2.24–4.55) | <0.001 | 1.58 (1.02–2.45) | 0.040 |
CKD-EPI, chronic kidney disease epidemiology collaboration formula; CRP, C reactive protein; eGFR, estimated glomerular filtration rate.
In-hospital events
Patients with a history of AF were at higher risk of clinical events during hospitalization, such as new-onset AF (36.8% vs. 7.9%; P < 0.001), acute HF (25.3% vs. 6.3%; P < 0.001), multiorgan failure (13.9% vs. 5.8%; P = 0.010), and acute renal failure (21.5% vs. 13.4%; P = 0.06) (Table 2 and Figure 2). New-onset AF occurred during hospitalization in 68 (12.5%) of the 542 patients in whom these data were available. Of these, 30 patients (44%) had a history of paroxysmal AF. Thirty-six (52.9%) of these events were new-onset AF in patients with no history of AF. Eighteen (26.4%) patients underwent cardioversion for haemodynamic instability. Of these, 14 were pharmacological and 4 electrical. There was no difference in terms of in-hospital systemic embolic events among patients with and without history of AF. Nevertheless, pulmonary embolism was slightly more common in patients without a history of AF (2.9% vs. 8.5%, P = 0.046) as well as for acute respiratory distress syndrome (6.7% vs. 19.2%, P = 0.004). Clinical characteristics, laboratory findings, in-hospital management, and outcome of patients who developed in-hospital AF are shown in Supplementary material online, Table S3.
Figure 2.
In-hospital clinical outcome stratified by history AF. AF, atrial fibrillation.
Discussion
Our results show that 15% of the patients hospitalized for COVID-19 had a history of AF and this was associated with an increased risk of death and more in-hospital clinical events including new-onset AF, acute HF, and multiorgan failure. In-hospital death occurred in 38.7% of the patients with AF history vs. 20.8% of those without AF history. The association between AF and mortality remained significant after adjustment for variables associated with COVID-19 severity, such as comorbidities, previous use of anticoagulant, oxygen saturation, red blood cells count, haemoglobin, CRP, plasma troponin, and HF history. Our results highlight the prognostic relevance of a history of AF as a marker of increased risk, along with other common concomitant factors associated with an unfavourable prognostic impact.5,7 We also found that new-onset AF occurred in 12.5% of the patients and in 36 (52.9%) of them, it was the first episode of AF.
The proportion of patients hospitalized for COVID-19 with a history of AF ranged from 5% to 20% in previous reports.8–10 In our experience, the high prevalence of AF history (15%) may be linked to the older age of our population (mean age was 67.4 ± 13.2 years) and the characteristics of our cohort with a high prevalence of cardiovascular comorbidities. From this perspective, the prognostic role of a history of AF should be interpreted in the context of other conditions contributing to the higher risk of death. Several studies suggest that the presence of pre-existing cardiovascular diseases identifies patients at higher risk of adverse COVID-19 outcomes.11,12 It has been also shown a higher risk of development of cardiac arrhythmias following COVID-19 as well as the risk of worse clinical course in those patients who developed AF. Nevertheless, the prognostic role of AF history during COVID-19, on top of other established risk factors, has not yet been clearly described in previous reports. Only one multicentre cohort study showed higher odds of mortality among COVID-19 patients with AF history, but the study did not take into account significant confounders associated with COVID-19 severity, such as respiratory and laboratory parameters, including troponin plasma levels.13
Regardless of COVID-19, AF is a well-known CV risk factor in the general population associated with a high risk of mortality and CV complications.14,15 Among patients admitted to intensive care unit, AF is an independent risk factor for weaning failure and is significantly associated with poor hospital outcome in mechanically ventilated patients, and with a higher percentage of respiratory failure due to ARDS, even in the absence of HF.16 Our data confirm the prognostic role of AF, along with age and other well-known comorbidities, also in patients affected by COVID-19. The relationship between COVID-19 and AF seems to be bidirectional. AF may increase the incidence and severity of COVID-19 and COVID-19 may favour episodes of AF. The correlation between viral infection and onset AF is established, as well as risk factors and possible predictors. Nevertheless, our understanding of arrhythmic complications in COVID-19 is still evolving.17
SARS-CoV-2 uses direct binding with ACE2 to enter the host cells including type 2 pneumocytes, macrophages, cardiomyocytes, pericytes, and endothelial cells.2 Plasma ACE2 activity is elevated in multiple conditions, including HF, hypertension, vascular disease, and AF, and is directly associated with more advanced atrial structural remodelling.2 In this perspective, AF could increase susceptibility to SARS-CoV-2 infection, especially in case of advanced atrial disease, such as in older patients with multiple CV comorbidities. In addition, resulting systemic inflammation may overlap with the basal inflammatory state present in case of AF and may be a potential mechanism for worse outcomes.18
On the other hand, acute respiratory infections may represent a precipitant factor for new-onset or recurrent AF. Viral infection is associated with direct myocardial injury and inflammation, metabolic dysfunction, electrolyte abnormalities, dehydration, hypoxia, and activation of the sympathetic nervous system, all of which predispose to cardiac arrhythmia.2
During COVID-19 disease, especially in case of critical illness, new-onset AF can be promoted by arrhythmogenic triggers, such as prolonged hypotension, inadequate oxygen delivery, positive fluid balance, and previous vasopressor use. From this perspective, new-onset AF may represent both a marker of disease severity as well as a likely contributor to poor outcomes.
It is important to note that in our AF population, the rate of death was higher than for stroke or systemic embolic events. Our findings highlight that, as observed for the general population, among COVID-19 patients, AF increases the risk of worse outcome pointing out the need to adopt integrated multilevel prevention strategies to improve outcomes, beyond stroke prevention, as it is recommended in the AF Better Care (ABC) holistic pathway for integrated AF care, reported in the most recent ESC AF guidelines.6
In our report, the association between AF and worse outcome was not modified by previous or concomitant use of anticoagulant. This finding supports recent studies showing that neither antiplatelet therapy nor anticoagulant therapy before admission influenced the risk of hospital admission for COVID-19, as well as the risk of severe clinical presentation or death during hospitalization.19 As previously shown by our group,7 patients with AF, as well as patients with a history of HF, were less likely to be treated with corticosteroids. One possible explanation may be the prominent role of the cardiac involvement as a main cause of reduced survival and symptoms in these patients. This concept is corroborated by the slightly lower degree of COVID-19 severity at admission (higher values of PaO2/FiO2 ratio, lower SOFA score, and body temperature) in these patients with concomitant AF. Consistently, patients with AF were also less likely to receive antiviral therapy in this study.
Proper pharmacological management of patients with COVID-19 infection and AF is required. Recommendations have recently been provided for the pharmacological management of patients with COVID-19 and concomitant AF, which include the effects and potential pro-arrhythmic interactions between antiarrhythmic drug, anticoagulants, and emerging COVID-19 pharmacotherapies. General recommendations for AF management in patients with COVID-19 are summarized in Table 4.20,21
Table 4.
General recommendations for AF management in patients with COVID-19
| General recommendations |
|---|
| ECG is recommended in all patients with suspected COVID-19 infection at admission. |
| Is recommended to perform an ECG before the initiation of antiarrhythmic drug and ECG monitoring after initiation. |
| QT interval should be monitored in patients treated with class IA, IC, and III AADs, hydroxychloroquine/chloroquine, macrolide, fingolimod, and/or lopinavir/ritonavir. |
| Drug management |
| Classes IA and IC are contraindicated in COVID-19 patients on fingolimod. |
| Beta-blockers are recommended as a first-line therapy to rate control. |
| Calcium channel blockers are not recommended in acute myocarditis patients with decompensated HF. |
| Digoxin can be used in CHF or combination with β-blockers or calcium channel blockers for rate control. |
| Heparin is the anticoagulant of choice in hospitalized COVID-19 patients with AF, especially if patients are being treated with lopinavir/ritonavir. |
| Direct oral anticoagulants can be used in AF patients with COVID-19 after discharge without lopinavir/ritonavir. |
| Amiodarone can be used for rhythm and rate control in critically ill COVID-19 patients with CHF. Close monitoring with caution is recommended with concurrent lopinavir/ritonavir use. It is not recommended in patients undergoing treatment with fingolimod. |
| Flecainide or propafenone is a good option for pharmacological cardioversion in patients with no structural heart disease or coronary artery disease who are on fingolimod. |
| Ibutilide, flecainide, propafenone can be used for cardioversion in patients not treated with fingolimod and without structural heart disease or coronary artery disease. |
AADs, anti arrhythmic drugs; AF, atrial fibrillation; CHF, chronic heart failure; COVID-19, coronavirus disease 2019; ECG, electrocardiogram; HF, heart failure.
Modified from Ref.20
Limitations
This study had some limitations. Our population was characterized by a relatively old age with a significant burden of CV comorbidities. Since residual confounding could not be excluded, the prognostic role of history AF should be interpreted accordingly. Nevertheless, the multivariable model used accounted for relevant clinical and demographic confounders. Not all patients were subjected to continuous electrocardiographic monitoring and the diagnosis of AF was carried out through ECG. Therefore, the occurrence of paroxysmal AF may have been underdiagnosed. Echocardiographic data were available for a small proportion of subjects, limiting the possibility to assess the association between AF, death, and cardiac structure and function. Finally, our analysis lacks post-discharge follow-up data, thus we could not assess the occurrence of AF after hospitalization.
Conclusions
History of AF is a frequent comorbidity in patients hospitalized for COVID-19. It significantly contributes to worse clinical course with a higher mortality and in-hospital events, on top of other variables related with AF and COVID-19 severity. Atrial fibrillation history and careful electrocardiogram monitoring may be useful to stratify high-risk COVID-19 patients. Atrial fibrillation is an important risk factor to improve risk modelling of adults with COVID‐19 and an optimal management of AF is necessary to potentially improve the outcomes.
Supplementary material
Supplementary material is available at Europace online.
Conflict of interest: R.M.I received speaker and advisor honoraria from Daiichi-Sankyo, Boehringer Ingelheim. P.A. received speaker and advisor honoraria from Novartis, AstraZeneca, Vifor, Daiichi-Sankyo, Boehringer Ingelheim, Pfizer, GSK and MSD. V.C. received consulting honoraria from CVie Therapeutics Limited, Servier, and Windtree Therapeutics. A.M. reports personal consulting honoraria from Novartis, Servier, AstraZeneca for participation in advisory board meetings and receives grants from Novartis and Niccomo for research trials. M.P. received research grant and speaking fees from Novartis, Servier, Vifor. M.M. reports personal consulting honoraria from Abbott, Actelion, Amgen, Bayer, Servier, Vifor Pharma and Windtree Therapeutics for participation in advisory board meetings and executive committees of clinical trials. All other authors have nothing to disclose.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Supplementary Material
References
- 1. Guan W, Ni Z, Hu Y, Liang W, Ou C, He J et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tomasoni D, Italia L, Adamo M, Inciardi RM, Lombardi CM, Solomon SD et al. COVID-19 and heart failure: from infection to inflammation and angiotensin II stimulation. Searching for evidence from a new disease. Eur J Heart Fail 2020;22:957–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gopinathannair R, Merchant FM, Lakkireddy DR, Etheridge SP, Feigofsky S, Han JK et al. COVID-19 and cardiac arrhythmias: a global perspective on arrhythmia characteristics and management strategies. J Interv Card Electrophysiol 2020;59:329–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Denegri A, Pezzuto G, Arienzo MD, Morelli M, Savorani F, Cappello CG et al. Clinical and electrocardiographic characteristics at admission of COVID-19/SARS-CoV2 pneumonia infection. Intern Emerg Med 2021;4:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lombardi CM, Carubelli V, Iorio A, Inciardi RM, Bellasi A, Canale C et al. Association of troponin levels with mortality in Italian patients hospitalized with coronavirus disease 2019: results of a multicenter study. JAMA Cardiol 2020;5:1274–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2020;42:373–498. [DOI] [PubMed] [Google Scholar]
- 7. Tomasoni D, Inciardi RM, Lombardi CM, Tedino C, Agostoni P, Ameri P et al. Impact of heart failure on the clinical course and outcomes of patients hospitalized for COVID-19. Results of the Cardio-COVID-Italy multicentre study. Eur J Heart Fail 2020;22:2238–47. [DOI] [PubMed] [Google Scholar]
- 8. Peltzer B, Manocha KK, Ying X, Kirzner J, Ip JE, Thomas G et al. Arrhythmic complications of patients hospitalized with COVID-19: incidence, risk factors, and outcomes. Circ Arrhythm Electrophysiol 2020;13:e009121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Colon CM, Barrios JG, Chiles JW, McElwee SK, Russell DW, Maddox WR et al. Atrial arrhythmias in COVID-19 patients. JACC Clin Electrophysiol 2020;6:1189–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bertini M, Ferrari R, Guardigli G, Malagù M, Vitali F, Zucchetti O et al. Electrocardiographic features of 431 consecutive, critically ill COVID-19 patients: an insight into the mechanisms of cardiac involvement. Europace 2020;22:1848–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Guo T, Fan Y, Chen M, Wu X, Zhang L, He T et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:811–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Inciardi RM, Adamo M, Lupi L, Cani DS, Di Pasquale M, Tomasoni D et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J 2020;41:1821–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Peltzer B, Manocha KK, Ying X, Kirzner J, Ip JE, Thomas G et al. Outcomes and mortality associated with atrial arrhythmias among patients hospitalized with COVID-19. J Cardiovasc Electrophysiol 2020;31:3077–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet 2015;386:154–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Inciardi RM, Giugliano RP, Claggett B, Gupta DK, Chandra A, Ruff CT et al. Left atrial structure and function and the risk of death or heart failure in atrial fibrillation. Eur J Heart Fail 2019;21:1571–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shaver CM, Chen W, Janz DR, May AK, Darbar D, Bernard GR et al. Atrial fibrillation is an independent predictor of mortality in critically ill patients. Crit Care Med 2015;43:2104–011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Inciardi RM, Adamo M, Lupi L, Metra M. Atrial fibrillation in the COVID-19 era: simple bystander or marker of increased risk? Eur Heart J 2020;41:3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Inciardi RM, Solomon SD, Ridker PM, Metra MC. Disease (COVID-19), systemic inflammation, and cardiovascular disease. J Am Heart Assoc 2020;9:e017756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Flam B, Wintzell V, Ludvigsson JF, Mårtensson J, Pasternak B. Direct oral anticoagulant use and risk of severe COVID‐19. J Intern Med 2020;10:1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rattanawong P, Shen W, El Masry H, Sorajja D, Srivathsan K, Valverde A et al. Guidance on short-term management of atrial fibrillation in coronavirus disease 2019. J Am Heart Assoc 2020;9:e017529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. European Society of Cardiology. ESC guidance for the diagnosis and management of CV disease during the COVID-19 pandemic. https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.