Abstract
Childhood maltreatment (CM) is a known risk factor for adolescent pregnancy. Sleep disturbances and psychological distress, both common negative sequelae of CM, often co-occur during pregnancy, although directionality remains unclear. Furthermore, little is known about how CM affects sleep–distress associations during pregnancy. In pregnant adolescents, we examined: (a) whether there are significant predictive associations from CM to sleep quality and distress and (b) bidirectional influences of distress and sleep quality. Healthy pregnant adolescents (n = 204) were recruited before or during the 2nd trimester. CM was assessed at enrollment; sleep quality and distress were assessed in the 2nd and 3rd trimesters. Hypotheses were tested using path analysis. Findings revealed that CM was associated with worse 2nd trimester sleep quality and distress (β = .19, p < .05 for sleep; β = .30, p < .001 for distress). Higher levels of 2nd trimester distress were associated with lower 3rd trimester sleep quality (β = .19, p < .05). Findings provide novel information about (a) associations from CM to prenatal mood and sleep in pregnant adolescents, and (b) sleep–distress directionality over the course of pregnancy. These results have implications for better understanding the ways in which CM potentially exerts influences later in life, and for targeting interventions to address physical and mental health during pregnancy.
Keywords: adolescent pregnancy, childhood maltreatment, distress, sleep
Childhood maltreatment (CM), which is defined as sexual, physical, or emotional abuse and/or physical or emotional neglect before the age of 18, has been established as a major public health risk in the United States. Approximately 678,000 children experienced substantiated incidents of maltreatment in 2018 alone (U.S. Department of Health & Human Services & Administration on Children, 2020). CM is associated with a host of negative health outcomes in adulthood (Wegman & Stetler, 2009; Widom, Czaja, Bentley, & Johnson, 2012), including poor sleep (Abajobir, Kisely, Williams, Strathearn, & Najman, 2017; Chapman et al., 2013), as well as increased incidence of psychopathology and psychosocial distress (Edwards, Holden, Felitti, & Anda, 2003; Kessler et al., 2010). Although there is emerging evidence to suggest that the associations between CM and negative health outcomes are already present by adolescence (Hussey, Chang, & Kotch, 2006; Tanaka, Wekerle, Schmuck, Paglia-Boak, & Team, 2011), the majority of the literature examining health outcomes of CM has used adult samples (typically ages 40 to 60 years). The lack of focus on health outcomes in adolescents with a history of CM is a significant gap in the literature.
A population that is at particular risk for CM and negative health outcomes is pregnant adolescents. CM is a risk factor for pregnancy during adolescence (Garwood, Gerassi, Jonson-Reid, Plax, & Drake, 2015; Noll & Shenk, 2013; Noll, Shenk, & Putnam, 2009), and pregnancy during this developmental period may increase risk for atypical alterations to biological stress regulation and in turn the likelihood of poor sleep and mood regulation (Bublitz, Parade, & Stroud, 2014; Gonzalez, 2013; Shea et al., 2007). Pregnancy is also a time of increased psychosocial stress, particularly for adolescents (Geller, 2004; Hodgkinson, Beers, Southammakosane, & Lewin, 2014). Taken together, pregnant adolescents with CM history may experience a combination of risk factors that increase their likelihood of distress and poor sleep. To date, the extent and direction of these associations – whether distress leads to mood disturbance or vice versa, and whether CM moderates these associations – are unknown.
Childhood maltreatment and poor sleep in adolescence
Given the importance of sleep for overall health, sleep quality has emerged as a health outcome of particular interest in adolescents. When examining adverse effects of CM, sleep is thought to be impacted due to both psychological factors, such as the belief that sleep is not a safe state (Moore, 1989; Noll, Trickett, Susman, & Putnam, 2006), and biological influences, such as alterations to stress hormone regulation (De Bellis et al., 1996) and the sympathetic adrenergic system, which can yield difficulties initiating and maintaining sleep (Ouyang, Hellman, Abel, & Thomas, 2004). Studies examining sleep have consistently demonstrated lower sleep quality and quantity among adolescents with CM history. In a large nationally representative US population-based sample of almost 10,000 adolescents, individuals with exposure to at least one form of childhood adversity were at higher risk of insomnia, with risk of insomnia rising with increased exposure (Wang, Raffeld, Slopen, Hale, & Dunn, 2016). There is also evidence for associations between childhood sexual abuse and increased levels of sleep disturbances in adolescence, above and beyond contributions from psychopathology (e.g., depression, posttraumatic stress disorder; Noll et al., 2006). Further, McPhie and colleagues reported similar findings in 2014, demonstrating that higher levels of CM are associated with greater sleep disturbances in adolescence; they also found that this association is mediated by psychological distress (McPhie, Weiss, & Wekerle, 2014), underscoring the importance of considering mental health factors that may be implicated in the pathways between CM and sleep quality.
Childhood maltreatment and distress in adolescence
CM is associated with increased psychopathology and psychological distress during adolescence. In both prospective and retrospective studies, associations between CM and worse mental health symptoms are consistently found to be moderate to strong (Gilbert et al., 2009). There is longitudinal evidence that children with a history of childhood abuse as compared with nonabused children demonstrate elevated rates of major depressive disorder in early adolescence (Brown, Cohen, Johnson, & Smailes, 1999) A meta-analysis of both prospective and retrospective studies examining long-term outcomes of childhood abuse and neglect documented significantly increased odds of depressive disorders in maltreated versus nonmaltreated individuals (Norman et al., 2012). Looking beyond diagnostic criteria, CM is also a risk factor for general psychological distress (McPhie et al., 2014) and increased internalizing symptoms in adolescents (Heleniak, Jenness, Vander Stoep, McCauley, & McLaughlin, 2016).
Childhood Maltreatment, Sleep, and Distress in Pregnant Adolescents
Given the higher rates of CM they experience, pregnant adolescents are a population for whom CM, poor sleep, and distress are all highly relevant. Adolescence and pregnancy, individually and concomitantly, are both life phases during which poor sleep and psychological distress can increase. Pregnant and parenting adolescents report depressive symptoms at a two- to four-fold rate as compared with nonpregnant/nonparenting adolescents and pregnant/parenting adults (Hodgkinson et al., 2014; Mollborn & Morningstar, 2009). Sleep quality and quantity often decline during adolescence due to a convergence of biological, psychological, and sociocultural influences related to changes in circadian rhythm, autonomy to choose sleeping hours, academic pressure, and the use of screen devices and social networks (Carskadon, 2011; Gradisar, Gardner, & Dohnt, 2011). Adolescents with restricted sleep quantity over only a few nights report increased negative emotions, suggesting that lack of quality sleep has an immediate impact on mood (Baum et al., 2014). Further, a positive history of CM has been associated with increased psychopathology in pregnant adolescents: exposure to multiple types of CM was associated with a significantly increased risk of conduct disorder, while sexual abuse was associated with an increased risk of depression (Romano, Zoccolillo, & Paquette, 2006).
Pregnancy-specific Distress
Much of the work evaluating psychological outcomes of early CM uses clinical diagnoses (such as major depressive disorder or posttraumatic stress disorder) to index outcomes, rather than transdiagnostic symptoms like psychological distress. However, assessing distress symptoms may offer better identification of individuals for whom early CM is associated with psychological difficulties, yet who do not meet criteria for a diagnosis. Importantly, many adolescent girls may demonstrate symptoms of psychological distress, generally defined as a state of emotional suffering characterized by mood, stress, and anxiety symptoms, without meeting full diagnostic criteria for a psychiatric disorder (Treutiger & Lindberg, 2013). For this reason, assessing mood symptoms, rather than diagnosis, may provide more nuanced information about adolescent girls’ mental health and better identify those in need of intervention.
Much of the existing literature examining associations between distress and sleep or CM in pregnancy has used measures of general distress. While use of general distress measures allows for comparison with findings in nonpregnant samples, there are potentially distressing experiences unique to pregnancy that are not captured with a more general measure. For example, pregnancy-specific concerns can include physical symptoms, bodily changes, the health of the fetus, and thoughts about childbirth and parenting (Alderdice, Lynn, & Lobel, 2012; Lobel, 1998; Lynn, Alderdice, Crealey, & McElnay, 2011). Accordingly, use of a more general distress measure may inaccurately assess distress experienced during pregnancy. In addition, the use of a prenatal distress measure allows for data to be compared to a pregnant normative sample, which offers a more precise comparison group.
The Current Study
Cross-sectional data with pregnant women indicate that sleep quality is negatively associated with pregnancy-specific distress (Blair, Porter, Leblebicioglu, & Christian, 2015). There are longitudinal data that poor sleep in the 2nd trimester is associated with depressive mood symptoms in the 3rd trimester (Kamysheva, Skouteris, Wertheim, Paxton, & Milgrom, 2010; Skouteris, Germano, Wertheim, Paxton, & Milgrom, 2008). In contrast, there is evidence that distress may predict later sleep concerns. Symptoms of depression in the 2nd trimester have been associated with sleep problems in the 3rd trimester (Field et al., 2007). Women identified as depressed by the midpoint in pregnancy (20 weeks’ gestation) had worse quality sleep at 20 and 30 weeks’ gestation as compared with nondepressed women (Okun, Kiewra, Luther, Wisniewski, & Wisner, 2011). In this case, distress earlier in pregnancy could yield biological dysregulation that may interfere with healthy sleep (Ouyang et al., 2004). Sleep and distress may have bidirectional influences over time during pregnancy; however, to date there is a dearth of studies with the necessary methodology and analytic plans to examine this question.
There is a notable lack of research investigating effects of CM on the sleep and mood associations, especially in a population at risk for each health issue – pregnant adolescents. Limited evidence suggests that CM is associated with higher odds of stress-related sleep disturbance and poor sleep quality in pregnant women, indicating that CM continues to exert its long-reaching influence even during pregnancy (Gelaye et al., 2015). There is a critical gap in the literature in assessing the directionality of these associations, especially in pregnant adolescents. It is important to examine the potential mutual influences of sleep and distress on one another simultaneously in one single analysis in the context of CM. Measuring both distress and sleep simultaneously and at multiple time points allows for tests of both concurrent and cross-lagged bidirectional associations between these two constructs, a critical analytic approach that is needed to help clarify the mechanisms of action in this cascade so as to provide effective intervention. Further, in spite of their increased rates of CM, poor sleep, and mood difficulties, research investigating the influence of CM on both sleep and distress in pregnant adolescents is sorely lacking.
The purposes of this study with pregnant adolescents were to (a) establish whether there are predictive associations from CM to sleep quality and psychological distress and (b) test bidirectional influences of psychological distress and sleep quality. We hypothesized that, consistent with prior literature (Gelaye et al., 2015; McPhie et al., 2014; Noll et al., 2006), there would be a significant association between higher levels of CM and both higher distress and worse sleep quality. In addition, we hypothesized that psychological distress earlier in pregnancy would be associated with lower sleep quality later in pregnancy. However, given the lack of clarity about the directionality of sleep–distress associations, we deemed it important to assess the mutual influence between these two constructs. We also tested whether there is bidirectionality in the associations between sleep quality and distress. This study provides the first longitudinal examination of associations between CM, sleep quality, and pregnancy-related distress over the course of pregnancy in a sample of pregnant adolescents.
Method
Participants
As part of a larger study investigating associations between prenatal stress and nutrition with birth outcomes, nulliparous pregnant adolescents (n = 204, ages 14–19 years) were recruited through the Department of Obstetrics and Gynecology at a large academic medical center in the northeast United States, and flyers were posted in the surrounding neighborhoods (please see Figure 1 for enrollment). Participants gave informed consent, and procedures were in accordance with the local institutional review board. Parental consent and participant assent were obtained for participants under the age of 18. All participants were experiencing a healthy, low-risk pregnancy. Participants were excluded if they reported use of tobacco, recreational drug use, or cardiovascular medication use, or if they were not fluent in English. Demographic information such as education and household socioeconomic status was collected upon enrollment. Pregnant adolescents included in the current analyses were on average 17.89 years (SD = 1.18) at enrollment; 85% self-identified as Hispanic, while the remaining 15% self-identified as non-Hispanic Black or African-American. The median household income was $16,000–$25,000 (range = $0–$15,000 to >$101,000). Forty-two percent of the fetuses were female.
Figure 1.
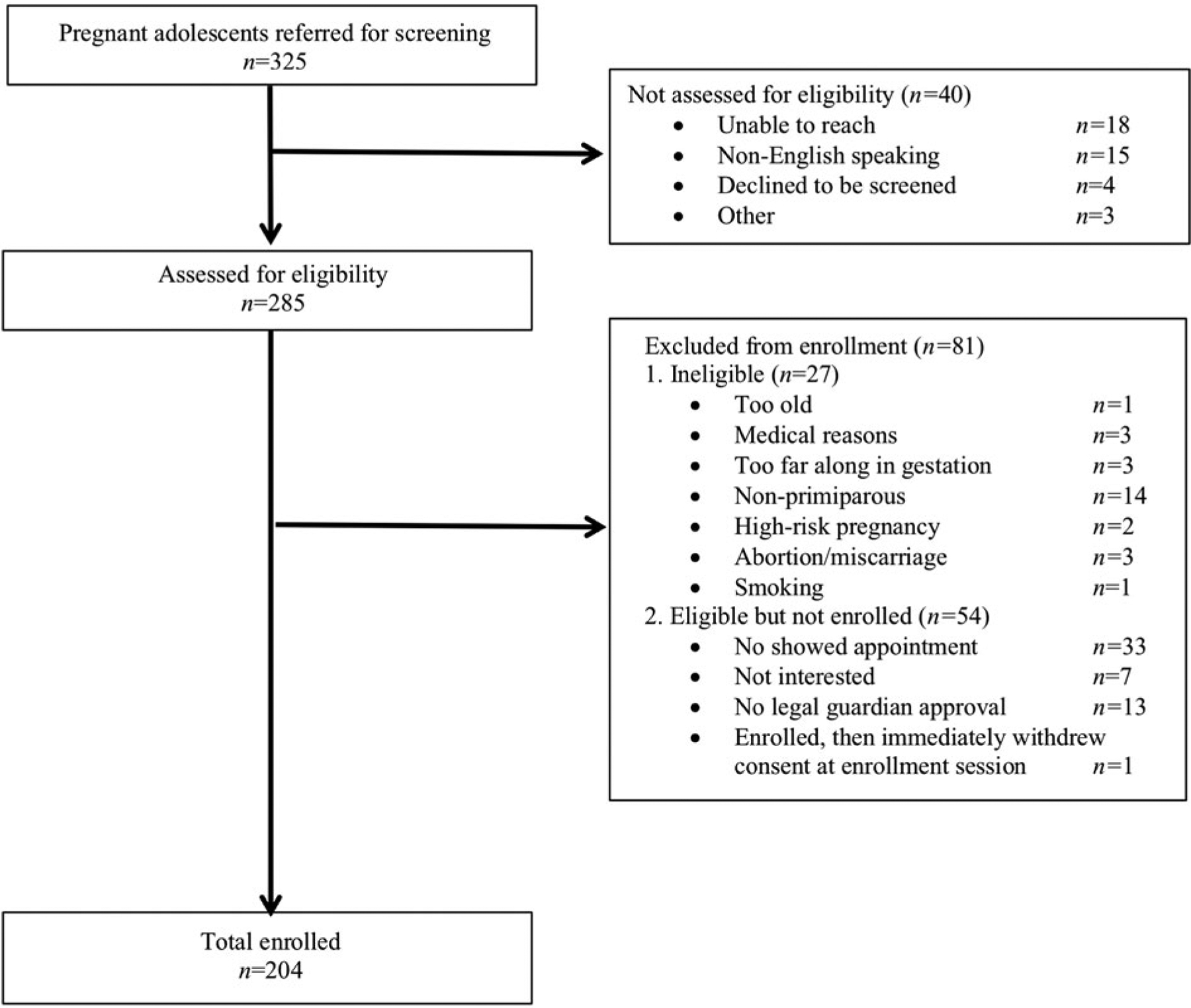
Recruitment and enrollment information for this sample.
Study procedures
Data used in the current study came from a series of laboratory visits that occurred when participants were 23–27 (2nd trimester) and 34–37 (3rd trimester) weeks’ pregnant. The average number of weeks between these visits was 9.60 (SD = 1.83), with a range of 3.29–13.29 weeks. At each visit, participants completed self-report questionnaires about their sleep quality, mood, and other experiences, as well as demographics and basic medical information. The full study procedures are described in Spicer et al., 2013.
Sleep quality
Sleep quality was assessed using the self-report Pittsburgh sleep quality index (PSQI; Buysse, Reynolds, Monk, Berman, & Kupfer, 1989), which captures sleep quality over the past month. Participants rated how frequently they experienced seven markers of poor sleep (e.g., sleep latency, awakenings, nightmares, sleep apnea, pain/discomfort associated with sleep) on 4-point Likert-type scales (0 = not during the past month to 3 = three or more times a week). Consistent with standard scoring procedures, the seven items were summed to yield a global score of sleep quality ranging from 0 to 21 (α = 0.73 in the 2nd and α = 0.72 in the 3rd trimester); higher scores indicate worse sleep.
Prenatal distress
Prenatal distress was measured using the Prenatal Distress Questionnaire (PDQ; Yali & Lobel, 1999), a self-report measure assessing pregnancy-related worries, anxiety, and distress in each trimester. Respondents rated how bothered they felt by 12 symptoms (including concerns regarding medical problems, physical symptoms, parenting, relationships, bodily changes, labor and delivery, and the health of the baby) at each point in the pregnancy on 3-point scales (0 = not at all to 2 = very much). Scores were summed to create a total score ranging from 0 to 24 (α = .76 in the 2nd and α = .84 in the 3rd trimester). Higher scores indicate greater distress.
Childhood maltreatment
The history of CM was assessed with the short form of the Childhood Trauma Questionnaire (CTQ; Bernstein et al., 2003), a 28-item self-report measure that uses a 5-point scale (1 = never true to 5 = very often true) to assess exposure to specific traumatic events during childhood (i.e., maltreatment). There are five scales assessing different types of maltreatment (emotional abuse, emotional neglect, physical abuse, physical neglect, and sexual abuse). Sample items include, “I was called names by family,” “I felt loved” (reverse coded), “I was hit hard enough to leave bruises,” “I was made to do sexual things,” and “I got taken care of” (reverse coded). Scores from all five scales were summed to create a total score to index overall level of CM, with total scores ranging from 5 to 125 (α = .78). Higher scores indicate more maltreatment.
Analytic strategy
Our hypotheses were tested via path analysis using Mplus 7.4 (Muthén & Muthén, 1998–2017) and the maximum likelihood estimator. Missing data were handled using full information maximum likelihood (Arbuckle, Marcoulides, & Schumacker, 1996). Model fit was examined using the comparative fit index (CFI), Tucker–Lewis index, and root mean squared error of approximation (RMSEA). CFI and Tucker–Lewis index values above 0.90 and RMSEA values below 0.08 indicate adequate model fit (Hu & Bentler, 1999). Prior to testing our research questions, we examined whether potential relevant covariates (maternal prepregnancy body mass index [BMI], maternal age, household income, newborn birthweight, infant sex, and gestational age at birth) were significantly correlated with our focal variables (p < .05). Variables that showed significant bivariate correlations with at least one focal variable were included in all analyses (see below for details).
Our research questions were tested using a path model in which the following paths were estimated. Initially, we accounted for construct stability by estimating autoregressive paths between the 2nd and 3rd trimester assessments of sleep and distress. Next, cross-lagged paths were estimated, such that 3rd trimester sleep quality was regressed on 2nd trimester distress, and 3rd trimester distress was regressed on 2nd trimester sleep quality. A significant cross-lagged path coefficient in this model would indicate that the 2nd trimester construct (e.g., sleep problems) is associated with significant change in the 3rd trimester construct (e.g., an increase in prenatal distress). In addition, we regressed 2nd trimester distress and 2nd trimester sleep problems on the total maltreatment score. Paths were also estimated from each covariate identified in preliminary analyses (described above) to both the 3rd trimester sleep problems and 3rd trimester distress scores. Indirect effects were tested using the Model Indirect command as well as via examination of 95% confidence intervals.
Results
Descriptive statistics
Table 1 presents descriptive statistics for the study variables. According to the authors of the PSQI (Buysse et al., 1989), a global sleep score of >5 indicates poor sleep quality. In the 2nd trimester, 33% of participants scored >5; in the 3rd trimester, 39% of participants scored >5. Based on criteria outlined by the authors of the CTQ (Bernstein et al., 2003), 56% of participants reported experiences that indicated at least one type of CM, with over one-third of participants reporting multiple types of maltreatment. Table 2 presents correlations between CM, sleep quality, and distress at each time point in pregnancy. Of the potential covariates examined in preliminary analyses, maternal prepregnancy BMI and maternal age at enrollment were correlated with the focal study variables, and thus were included as covariates in analyses. In terms of missing data, 15% of our sample were missing CTQ scores, 27% PSQI scores in the 2nd trimester, 32% PSQI in the 3rd trimester, 30% PDQ in the 2nd trimester, and 37% PDQ in the 3rd trimester. No participants were missing prepregnancy BMI or age data.
Table 1.
Demographic and psychosocial information
| Mean or % | SD | |
|---|---|---|
| CTQ total score | 37.53 | 14.01 |
| CTQ number of types of maltreatment | – | – |
| 0 | 36% | – |
| 1 | 19% | – |
| 2 | 15% | – |
| 3 | 9% | – |
| 4 | 9% | – |
| 5 | 4% | – |
| Missing | 8% | – |
| PSQI global sleep – 2nd trimester | 6.05 | 3.41 |
| PSQI global sleep – 3rd trimester | 7.70 | 3.96 |
| PDQ distress – 2nd trimester | 7.52 | 4.45 |
| PDQ distress – 3rd trimester | 12.28 | 6.13 |
| Maternal age at enrollment (years) | 17.89 | 1.18 |
| Newborn weight at birth (grams) | 3,157.36 | 602.59 |
| Child sexa | 42% | – |
| Gestational age at birth (weeks) | 38.85 | 2.65 |
| Pre-pregnancy body mass index | 27.65 | 6.77 |
| Maternal race/ethnicity | -- | – |
| Hispanic/Latina | 85% | – |
| Non-Hispanic Black/African-American | 15% | – |
| Maternal household income | – | – |
| $0–$15,000 | 38% | – |
| $16,000–$25,000 | 29% | – |
| $26,000–$50,000 | 14% | – |
| $51,000-$–$$100,000 | 3% | – |
| >$101,000 | 1% | – |
| Declined to answer | 15% | – |
| Marital/Relationship status | – | – |
| Married | 5% | – |
| In relationship | 73% | – |
| Single | 16% | – |
| Declined to answer | 6% | – |
| Living status | – | – |
| With parent(s) | 59% | – |
| With father of baby | 21% | – |
| With other family member(s) | 9% | – |
| With friends | 2% | – |
| With parent(s) and father of baby | 6% | – |
| Declined to answer | 3% | – |
Note: CTQ = Childhood Trauma Questionnaire; PDQ = Prenatal Distress Questionnaire; PSQI = Pittsburgh Sleep Qality Index;
percent female.
Table 2.
Bivariate correlations among study variables
| Variable | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. CTQ total score | – | – | – | – |
| 2. PSQI global sleep – 2nd trimester | .20* | – | – | – |
| 3. PSQI global sleep – 3rd trimester | .26** | .58** | – | |
| 4. PDQ distress – 2nd trimester | .29** | .26** | .33** | – |
| 5. PDQ distress – 3rd trimester | .30** | .29** | .37** | .65** |
Note:
p < .05,
p < .01.
CTQ = Childhood Trauma Questionnaire; PDQ = Prenatal Distress Questionnaire; PSQI = Pittsburgh Sleep Quality Index.
Results of Path Model
As shown in Figure 2, maternal sleep problems and prenatal distress showed moderate stability between the 2nd and 3rd trimesters of pregnancy (β = .53, p < .001 for sleep problems and β = .62, p < .001 for prenatal distress). In addition, higher levels of distress in the 2nd trimester were associated with increases in sleep problems by the 3rd trimester (β = .19, p = .02). The path predicting 3rd trimester distress from 2nd trimester sleep problems was not statistically significant (p = .08). Greater CM predicted both increased 2nd trimester sleep problems (β = .19, p = .03) and increased 2nd trimester distress (β = .30, p < .001), and was indirectly associated with 3rd trimester sleep via increased 2nd trimester distress (β = .06, p = .048, 95% CI = .0001, .115). These effects were above and beyond the influence of maternal prepregnancy BMI, which was not significantly associated with maternal sleep or distress when considered in the complete model. This model fit the data adequately, χ2 (9, N = 204) = 18.81, p = .03, CFI = .95, RMSEA = 0.07.
Figure 2.
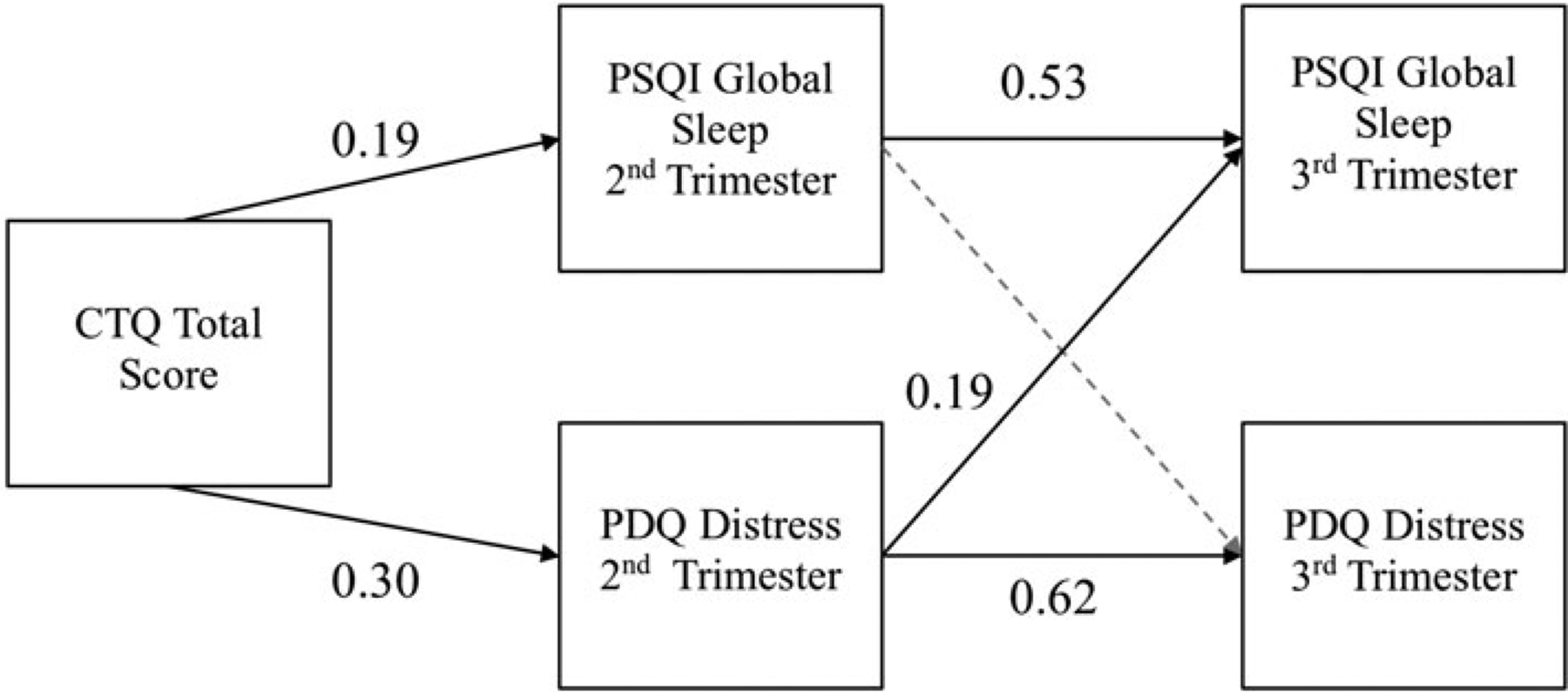
Final model relating childhood maltreatment (CM), sleep quality, and distress over the course of pregnancy. Note: χ2 (9, N = 204) = 18.81, p = .03, CFI = .95, RMSEA = 0.07. Indirect effect of childhood trauma on 3rd trimester sleep via 2nd trimester distress: β = .06, p = .048, 95% CI = .0001, .115. Gray dashed lines indicate nonsignificant paths; solid black lines indicate significant paths. All parameter estimates presented are standardized. CFI = comparative fit index; CTQ = Childhood Trauma Questionnaire; PDQ = Prenatal Distress Questionnaire; PSQI = Pittsburgh Sleep Quality Index; RMSEA = root mean squared error of approximation.
Discussion
The goals of this study were twofold: the first was to establish whether there are significant associations between reported CM, sleep quality, and distress in a sample of pregnant adolescents. Our second goal was to test whether there were bidirectional influences of psychological distress and sleep quality during pregnancy in adolescents. Consistent with our first hypothesis, our findings indicate that greater CM was associated with both worse sleep quality and higher levels of psychological distress for adolescents in the 2nd trimester of pregnancy. Further, child maltreatment was indirectly associated with increased poor quality sleep in the 3rd trimester, via its effect on 2nd trimester distress. This effect was observed after controlling for relevant confounds and for the stability in each construct over time. There was no significant association between 2nd trimester sleep and 3rd trimester distress, suggesting that, in this sample, distress appears to be driving changes in sleep and not vice versa. These results provide novel evidence to help answer both of our research questions. First, these findings are consistent with prior work demonstrating that CM is associated with psychological distress in pregnant adolescents (Hodgkinson et al., 2014; Mollborn & Morningstar, 2009; Romano et al., 2006), and with both poor sleep and psychological distress in nonpregnant adolescents (Cohen, Brown, & Smaile, 2001; Gilbert et al., 2009; McPhie et al., 2014; Noll et al., 2006; Norman et al., 2012; Wang et al., 2016) and pregnant adults (Gelaye et al., 2015). This study provides the first known evidence that CM is associated with both worse sleep and distress in pregnant adolescents, a population at increased risk for CM, poor sleep, and distress.
Second, when assessing the bidirectionality of sleep and distress during pregnancy, these results suggest that distress earlier in pregnancy is associated with poor sleep later in pregnancy. These findings are consistent with prior research demonstrating predictive associations from distress to poor sleep quality in adolescents (Johnson, Roth, & Breslau, 2006) and pregnant adults (Field et al., 2007; Obeysekare et al., 2020; Okun et al., 2011), and again provide novel evidence that this cascade is also present in pregnant adolescents. However, in these findings, poor sleep earlier in pregnancy was not associated with increased distress later in pregnancy, as has been found in some previous studies with pregnant adults (Kamysheva et al., 2010; Skouteris et al., 2008). It is possible that the addition of CM to this model or studying these associations in pregnant adolescents, rather than adults, could have resulted in a lack of significant associations between 2nd trimester sleep quality and 3rd trimester distress.
The findings about directionality in the context of CM are also consistent with previous research conducted with nonpregnant adolescents (e.g., McPhie et al., 2014), suggesting that psychological distress may be a potential mechanism through which early maltreatment is associated with poor sleep in the teenage years. Studying these indicators of CM in pregnant adolescents is long overdue given the increased levels of maltreatment that are typically seen in this population (Garwood et al., 2015; Noll & Shenk, 2013; Noll et al., 2009). Rates of self-reported CM in our sample were consistent with prior literature, with over half of our participants endorsing at least one type of maltreatment. Researchers estimate that from 50% to 70% of adolescent mothers report an early history of abuse or neglect using standardized questionnaires and interviews (Blinn-Pike, Berger, Dixon, Kuschel, & Kaplan, 2002; Klein & American Academy of Pediatrics Committee on, A, 2005; Noll et al., 2009). Over one-third of our participants reported multiple types of maltreatment, which is also consistent with prior findings suggesting the commonality of co-occurrence of multiple forms of abuse and neglect (Edwards et al., 2003).
In addition, the findings from this study provide insight into the bidirectional nature (or lack thereof) of the associations between sleep and distress over time during pregnancy. While sleep quality and distress have been examined in pregnant adults and nonpregnant adolescents, these questions to date have not been explicitly tested using a study design and analytic approach that simultaneously tested the effect of sleep on distress and distress on sleep while allowing for bidirectional associations. As mentioned above, the unidirectional predictive association we found between earlier distress and later sleep quality is consistent with previous studies examining these constructs in individuals with a history of CM. However, it will be important to conduct similar studies in pregnant adult and adolescent women without a history of CM to better understand sleep–distress bidirectionality during pregnancy in nonmaltreated individuals.
Ultimately, the findings of this study suggest that assessing the quality of both physical health (i.e., sleep) and psychological functioning (i.e., distress) is important to gain a thorough understanding of how these two factors are reciprocally associated with individual wellbeing during adolescence. This is especially so for pregnant adolescents, who are at elevated risk for psychological distress, as well as sleep problems due to their age and pregnant status. Furthermore, CM appears to exert long-lasting effects that can be seen in how sleep quality, a measure of physical health, interacts with pregnancy-related distress, a measure of psychological health. This is consistent with a host of evidence supporting associations of early maltreatment with subsequent psychological distress and psychiatric disorders (Chapman et al., 2004; Cohen et al., 2001; Edwards et al., 2003; Gilbert et al., 2009; Grassi-Oliveira & Stein, 2008; Norman et al., 2012; Romano et al., 2006; Spertus, Yehuda, Wong, Halligan, & Seremetis, 2003), and of childhood adversity with later health outcomes into adolescence and adulthood (Abajobir et al., 2017; Anda et al., 2006; Gelaye et al., 2015; Greenfield, Lee, Friedman, & Springer, 2011; Noll et al., 2006). Our results suggest that clinical intervention for young women experiencing sleep problems and/or psychological distress during pregnancy should involve an assessment of relevant psychosocial factors, including CM history. Based on what is known about the psychological (Anda et al., 2006; Chapman et al., 2004; Cohen et al., 2001; Gilbert et al., 2009; Grassi-Oliveira & Stein, 2008; Moore, 1989) and physiological changes (Bublitz et al., 2014; Cicchetti, Rogosch, Gunnar, & Toth, 2010; Gonzalez, 2013) that can occur following CM, further research is needed to understand better the potential mediating mechanisms between CM and both mood and sleep.
The potential role of distress in the trajectory between CM and sleep quality during pregnancy is also important for intervention planning. Although sleep quality is reported to be consistently low across pregnancy (Mindell, Cook, & Nikolovski, 2015), some research suggests that there are further changes to sleep architecture (decreases in slow-wave and rapid eye movement sleep) and increased night wakings in the 3rd trimester as compared with the 1st and 2nd trimesters (Pien & Schwab, 2004). While pregnancy-related endocrinological and physiological changes and physical discomfort may have at least some impact on these changes in sleep architecture, our findings raise the possibility that distress earlier in pregnancy could also be contributing to alterations in sleep physiology in pregnant adolescents who have experienced CM. Use of trauma-sensitive interventions for maternal distress (Seng, Low, Sperlich, Ronis, & Liberzon, 2009) earlier in pregnancy may improve subsequent sleep quality, potentially alleviating some of the effects of poor maternal sleep on peri- and postnatal outcomes (Sharma et al., 2016).
This study has several strengths. A notable strength of this study is that it was conducted with a sample comprising Hispanic/Latina and Black adolescents, both groups that are historically underrepresented in research despite their high-risk status for adolescent pregnancy and negative health outcomes (Matthews & Hamilton, 2019). Studies such as this one are important to ensure that research provides information that is relevant to the demographic groups who are experiencing the health concerns under evaluation. In addition, this study is one of only a few to assess sleep quality and prenatal distress multiple times during pregnancy, and the only known study to do so in a sample of pregnant adolescents, allowing us to examine questions of temporal directionality. The inclusion of a measure of CM also provides important data about a factor that may influence both sleep and mood, but is typically omitted from studies assessing sleep and distress in pregnancy. Further, the use of a pregnancy-specific distress measure is fairly unique in the literature examining associations between distress, sleep, and CM. When assessing these associations in a pregnant sample, using a pregnancy-specific measure allows for measurement of distress that may arise in direct relation to the pregnancy itself, and also increases the clinical relevance of the findings.
This study also has some limitations. Because of the sample make-up, it is unclear if results would generalize to adolescents of different ethnic/racial backgrounds or to pregnant adults. Further, although the measures used have been established as reliable and valid for use in adolescent and/or pregnant populations (CTQ: Bernstein, Ahluvalia, Pogge, & Handelsman, 1997; Spinhoven et al., 2014); (PSQI: Qiu et al., 2016; Raniti, Waloszek, Schwartz, Allen, & Trinder, 2018); (PDQ: Alderdice & Lynn, 2011; Lobel et al., 2008), they are all self-report measures. There are consistent associations found between self-reported sleep quality and retrospective self-reported CM (see Kajeepeta, Gelaye, Jackson, & Williams, 2015 for a review). We do expect that these same associations would be seen in studies using nonself-report measures, such as records of substantiated reports of CM, clinical psychodiagnostic evaluation, and objective measures of sleep quality. There is existing evidence that associations between CM and poor sleep quality remain present when CM is assessed with substantiated reports (e.g., Abajobir et al., 2017; McPhie et al., 2014; Noll et al., 2006) and when sleep quality is assessed using objective measures (Bader, Schafer, Schenkel, Nissen, & Schwander, 2007). CM has also been associated with both objective (actigraphy-based) and subjective (self-report standardized sleep diaries) measures of sleep quality in the same sample (Brindle et al., 2018; Sheehan, Li, & Friedman, 2020), indicating concordance between these different forms of sleep measurement. In general, however, there is a dearth of literature that uses objective measures of both CM and sleep in the same study.
In addition, recent evidence examining retrospective self-report measures of CM in association with prospective tracking of CM has raised concerns about a lack of concordance between the two (e.g., Baldwin, Reuben, Newbury, and Danese, 2019). At this time, it is not clear whether these discrepancies arise from inaccurate reporting or reflect the possibility that prospective versus retrospective reports may each assess unique information (Reuben et al., 2016). Future studies could increase the strength of our findings by using measurements beyond self-report, including substantiated or prospective reports of maltreatment history, clinical interviews for distress symptoms, consideration of biological correlates of these experiences, and sleep actigraphy or polysomnography that would capture objective measurements of sleep quality.
Another methodological limitation to our study is the potential for current distress to bias reporting of CM (Brewin, Andrews, & Gotlib, 1993). Encouragingly, there is evidence that there is stability in retrospective reporting of abuse and neglect over time on the CTQ, even following treatments like trauma-focused psychotherapy and subsequent reduction of mood symptoms. Comparison of pre- and posttreatment symptoms indicates reductions in psychopathology, self-blame, negatively biased memories, avoidance, and minimization of the abuse, while reporting of maltreatment events remained stable (Paivio, 2001). Although we cannot rule out the possibility that distress may have consciously or unconsciously impacted maltreatment reporting in our sample, the available evidence indicates that these reports tend to remain stable even when psychopathology and negative affect are reduced.
In addition, the CTQ does not provide detailed information about timing or chronicity of the maltreatment. Since the participants in this study were still adolescents, it is theoretically possible that the reported neglect or abuse occurred fairly recently. Unfortunately, given that our measure did not assess for chronicity or timing, this study was not able to examine whether these variables impact the associations reported in the current manuscript. By including measures that collect more detailed information about maltreatment history (duration, frequency, timing), future work could better determine whether these nuanced aspects of CM are related to future physical and psychosocial health during pregnancy. There is also evidence that social support can serve as a possible buffer or resilience factor against negative outcomes for adolescent mothers. Higher levels of social support are associated with better mental health outcomes (Bunting & McAuley, 2004), while positive relationships between pregnant adolescents and a parental figure of their own and their child’s father are associated with lower rates of depression (Edwards et al., 2012). Accordingly, future studies examining distress in this population would benefit from including assessments of social support in their models as a possible buffering factor that might positively shape mood and health outcomes.
These findings emphasize the potential for negative physical and psychological health outcomes in pregnant adolescents who have experienced CM, providing key insight into environmental factors that may relate to these markers of health. Sleep is a critical developmental process, especially during adolescence and even more so during pregnancy in adolescence. Distress and low mood during adolescence are also predictive of later physical and mental health challenges, indicating the importance of early intervention. In addition, our results highlight a potential pathway through which psychological distress impacts physical health (i.e., sleep) during pregnancy, which may in turn have implications for prenatal and fetal health (Warland, Dorrian, Morrison, & O’Brien, 2018). The potential multigenerational consequences of poor sleep and distress resulting from CM underline the importance of targeting interventions towards mechanisms of action as early as possible. Additional research is needed to better elucidate potential mediating mechanisms in this trajectory, with a focus on potential physiological or biological markers that may be implicated. In conjunction with future research, the novel results we present in this study should be used to develop trauma-sensitive interventions to target distress in pregnancy, which may in turn promote improved sleep and overall maternal and fetal health.
Acknowledgment.
The authors wish to thank the study staff and participants.
Financial Support. This research was supported by the National Institute of Mental Health (grant numbers R01MH077144, R01MH093677, K01MH120507).
Footnotes
Conflicts of Interest. None.
References
- Abajobir AA, Kisely S, Williams G, Strathearn L, & Najman JM (2017). Childhood maltreatment and adulthood poor sleep quality: A longitudinal study. Journal of Internal Medicine, 47, 879–888. doi: 10.1111/imj.13459 [DOI] [PubMed] [Google Scholar]
- Alderdice F, & Lynn F (2011). Factor structure of the prenatal distress questionnaire. Midwifery, 27, 553–559. [DOI] [PubMed] [Google Scholar]
- Alderdice F, Lynn F, & Lobel M (2012). A review and psychometric evaluation of pregnancy-specific stress measures. Journal of Psychosomatic Obstetrics & Gynecology, 33, 62–77. [DOI] [PubMed] [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, … Giles WH (2006). The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neuro-biology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience, 256, 174–186. doi: 10.1007/s00406-005-0624-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbuckle JL, Marcoulides GA, & Schumacker RE (1996). Full information estimation in the presence of incomplete data. Advanced Structural Equation Modeling: Issues and Techniques, 243, 277. [Google Scholar]
- Bader K, Schafer V, Schenkel M, Nissen L, & Schwander J (2007). Adverse childhood experiences associated with sleep in primary insomnia. Journal of Sleep Research, 16, 285–296. doi: 10.1111/j.1365-2869.2007.00608.x [DOI] [PubMed] [Google Scholar]
- Baldwin JR, Reuben A, Newbury JB, & Danese A (2019). Agreement between prospective and retrospective measures of childhood maltreatment: a systematic review and meta-analysis. JAMA Psychiatry, 76(6), 584–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum KT, Desai A, Field J, Miller LE, Rausch J, & Beebe DW (2014). Sleep restriction worsens mood and emotion regulation in adolescents. Journal of Child Psychology and Psychiatry, 55, 180–190. doi: 10.1111/jcpp.12125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, & Handelsman L (1997). Validity of the childhood trauma questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 340–348. doi: 10.1097/00004583-199703000-00012 [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, … Desmond D (2003). Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse & Neglect, 27, 169–190. [DOI] [PubMed] [Google Scholar]
- Blair LM, Porter K, Leblebicioglu B, & Christian LM (2015). Poor sleep quality and associated inflammation predict preterm birth: Heightened risk among African Americans. Sleep, 38, 1259–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blinn-Pike L, Berger T, Dixon D, Kuschel D, & Kaplan M (2002). Is there a causal link between maltreatment and adolescent pregnancy? A literature review. Perspectives on Sexual and Reproductive Health, 34, 68–75. [PubMed] [Google Scholar]
- Brewin CR, Andrews B, & Gotlib IH (1993). Psychopathology and early experience: A reappraisal of retrospective reports. Psychological Bulletin, 113, 82–98. doi: 10.1037/0033-2909.113.1.82 [DOI] [PubMed] [Google Scholar]
- Brindle RC, Cribbet MR, Samuelsson LB, Gao C, Frank E, Krafty RT, … Hall MH (2018). The relationship between childhood trauma and poor sleep health in adulthood. Psychosomatic Medicine, 80, 200–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown J, Cohen P, Johnson JG, & Smailes EM (1999). Childhood abuse and neglect: Specificity of effects on adolescent and young adult depression and suicidality. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1490–1496. [DOI] [PubMed] [Google Scholar]
- Bublitz MH, Parade S, & Stroud LR (2014). The effects of childhood sexual abuse on cortisol trajectories in pregnancy are moderated by current family functioning. Biological Psychology, 103, 152–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunting L, & McAuley C (2004). Research review: Teenage pregnancy and parenthood: The role of fathers. Child & Family Social Work, 9, 295–303. [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28, 193–213. [DOI] [PubMed] [Google Scholar]
- Carskadon MA (2011). Sleep in adolescents: The perfect storm. PediatricClinics of North America, 58, 637–647. doi: 10.1016/j.pcl.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman DP, Liu Y, Presley-Cantrell LR, Edwards VJ, Wheaton AG, Perry GS, & Croft JB (2013). Adverse childhood experiences and frequent insufficient sleep in 5 US states, 2009: A retrospective cohort study. BMC Public Health, 13, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, & Anda RF (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82, 217–225. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Gunnar MR, & Toth SL (2010). The differential impacts of early physical and sexual abuse and internalizing problems on daytime cortisol rhythm in school-aged children. Child Development, 81, 252–269. doi: 10.1111/j.1467-8624.2009.01393.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen P, Brown J, & Smaile E (2001). Child abuse and neglect and the development of mental disorders in the general population. Development and Psychopathology, 13, 981–999. [PubMed] [Google Scholar]
- De Bellis MD, Dahl RE, Perel JM, Birmaher B, al-Shabbout M, Williamson DE, … Ryan ND (1996). Nocturnal ACTH, cortisol, growth hormone, and prolactin secretion in prepubertal depression. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 1130–1138. doi: 10.1097/00004583-199609000-00010 [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, & Anda RF (2003). Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. The American Journal of Psychiatry, 160, 1453–1460. doi: 10.1176/appi.ajp.160.8.1453 [DOI] [PubMed] [Google Scholar]
- Edwards RC, Thullen MJ, Isarowong N, Shiu CS, Henson L, & Hans SL (2012). Supportive relationships and the trajectory of depressive symptoms among young, African American mothers. Journal of Family Psychology, 26, 585–594. doi: 10.1037/a0029053 [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Hernandez-Reif M, Figueiredo B, Schanberg S, & Kuhn C (2007). Sleep disturbances in depressed pregnant women and their newborns. Infant Behavior and Development, 30, 127–133. [DOI] [PubMed] [Google Scholar]
- Garwood SK, Gerassi L, Jonson-Reid M, Plax K, & Drake B (2015). More than poverty: The effect of child abuse and neglect on teen pregnancy risk. Journal of Adolescent Health, 57, 164–168. doi: 10.1016/j.jadohealth.2015.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaye B, Kajeepeta S, Zhong QY, Borba CP, Rondon MB, Sanchez SE, … Williams MA (2015). Childhood abuse is associated with stress-related sleep disturbance and poor sleep quality in pregnancy. Sleep Medicine, 16, 1274–1280. doi: 10.1016/j.sleep.2015.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller PA (2004). Pregnancy as a stressful life event. CNS Spectrums, 9, 188–197. doi: 10.1017/S1092852900008981 [DOI] [PubMed] [Google Scholar]
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, & Janson S (2009). Burden and consequences of child maltreatment in high-income countries. Lancet, 373, 68–81. doi: 10.1016/S0140-6736(08)61706-7 [DOI] [PubMed] [Google Scholar]
- Gonzalez A (2013). The impact of childhood maltreatment on biological systems: Implications for clinical interventions. Paediatrics & Child Health, 18, 415–418. [PMC free article] [PubMed] [Google Scholar]
- Gradisar M, Gardner G, & Dohnt H (2011). Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Medicine, 12, 110–118. doi: 10.1016/j.sleep.2010.11.008 [DOI] [PubMed] [Google Scholar]
- Grassi-Oliveira R, & Stein LM (2008). Childhood maltreatment associated with PTSD and emotional distress in low-income adults: The burden of neglect. Child Abuse & Neglect, 32, 1089–1094. doi: 10.1016/j.chiabu.2008.05.008 [DOI] [PubMed] [Google Scholar]
- Greenfield EA, Lee C, Friedman EL, & Springer KW (2011). Childhood abuse as a risk factor for sleep problems in adulthood: Evidence from a US national study. Annals of Behavioral Medicine, 42, 245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heleniak C, Jenness JL, Vander Stoep A, McCauley E, & McLaughlin KA (2016). Childhood maltreatment exposure and disruptions in emotion regulation: A transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cognitive Therapy and Research, 40, 394–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgkinson S, Beers L, Southammakosane C, & Lewin A (2014). Addressing the mental health needs of pregnant and parenting adolescents. Pediatrics, 133, 114–122. doi: 10.1542/peds.2013-0927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L. t., & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. [Google Scholar]
- Hussey JM, Chang JJ, & Kotch JB (2006). Child maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatrics, 118, 933–942. doi: 10.1542/peds.2005-2452 [DOI] [PubMed] [Google Scholar]
- Johnson EO, Roth T, & Breslau N (2006). The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. Journal of Psychiatric Research, 40, 700–708. doi: 10.1016/j.jpsychires.2006.07.008 [DOI] [PubMed] [Google Scholar]
- Kajeepeta S, Gelaye B, Jackson CL, & Williams MA (2015). Adverse childhood experiences are associated with adult sleep disorders: A systematic review. Sleep Medicine, 16, 320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamysheva E, Skouteris H, Wertheim EH, Paxton SJ, & Milgrom J (2010). A prospective investigation of the relationships among sleep quality, physical symptoms, and depressive symptoms during pregnancy. Journal of Affective Disorders, 123, 317–320. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, … Williams DR (2010). Childhood adversities and adult psychopathology in the WHO world mental health surveys. British Journal of Psychiatry, 197, 378–385. doi: 10.1192/bjp.bp.110.080499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein JD, & American Academy of Pediatrics Committee on Adolescence (2005). Adolescent pregnancy: Current trends and issues. Pediatrics, 116, 281–286. doi: 10.1542/peds.2005-0999 [DOI] [PubMed] [Google Scholar]
- Lobel M (1998) Pregnancy and mental health. In Friedman HS (Ed.), Encyclopedia of mental health (pp. 229–238). San Diego, CA: Academic Press. [Google Scholar]
- Lobel M, Cannella DL, Graham JE, DeVincent C, Schneider J, & Meyer BA (2008). Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychology, 27, 604–615. doi: 10.1037/a0013242 [DOI] [PubMed] [Google Scholar]
- Lynn FA, Alderdice FA, Crealey GE, & McElnay JC (2011). Associations between maternal characteristics and pregnancy-related stress among low-risk mothers: An observational cross-sectional study. International Journal of Nursing Studies, 48, 620–627. [DOI] [PubMed] [Google Scholar]
- Matthews TJ, & Hamilton BE (2019). Total fertility rates by state and race and Hispanic origin: United States, 2017. National Vital Statistics Reports, 68, 1–11. [PubMed] [Google Scholar]
- McPhie ML, Weiss JA, & Wekerle C (2014). Psychological distress as a mediator of the relationship between childhood maltreatment and sleep quality in adolescence: Results from the maltreatment and adolescent pathways (MAP) longitudinal study. Child Abuse & Neglect, 38, 2044–2052. doi: 10.1016/j.chiabu.2014.07.009 [DOI] [PubMed] [Google Scholar]
- Mindell JA, Cook RA, & Nikolovski J (2015). Sleep patterns and sleep disturbances across pregnancy. Sleep Medicine, 16, 483–488. doi: 10.1016/j.sleep.2014.12.006 [DOI] [PubMed] [Google Scholar]
- Mollborn S, & Morningstar E (2009). Investigating the relationship between teenage childbearing and psychological distress using longitudinal evidence. Journal of Health and Social Behavior, 50, 310–326. doi: 10.1177/002214650905000305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore MS (1989). Disturbed attachment in children: A factor in sleep disturbance, altered dream production and immune dysfunction: I. Not safe to sleep: chronic sleep disturbance in anxious attachment. Journal of Child Psychotherapy, 15, 99–111. doi: 10.1080/00754178808254836 [DOI] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2017). Mplus user’s guide (7th ed.). Los Angeles: Muthén & Muthén. [Google Scholar]
- Noll JG, & Shenk CE (2013). Teen birth rates in sexually abused and neglected females. Pediatrics, 131, e1181–e1187. doi: 10.1542/peds.2012-3072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noll JG, Shenk CE, & Putnam KT (2009). Childhood sexual abuse and adolescent pregnancy: A meta-analytic update. Journal of Pediatric Psychology, 34, 366–378. doi: 10.1093/jpepsy/jsn098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noll JG, Trickett PK, Susman EJ, & Putnam FW (2006). Sleep disturbances and childhood sexual abuse. Journal of Pediatric Psychology, 31, 469–480. doi: 10.1093/jpepsy/jsj040 [DOI] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, & Vos T (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PLoS Medicine, 9, e1001349. doi: 10.1371/journal.pmed.1001349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obeysekare JL, Cohen ZL, Coles ME, Pearlstein TB, Monzon C, Flynn EE, & Sharkey KM (2020). Delayed sleep timing and circadian rhythms in pregnancy and transdiagnostic symptoms associated with post-partum depression. Translational Psychiatry, 10, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okun ML, Kiewra K, Luther JF, Wisniewski SR, & Wisner KL (2011). Sleep disturbances in depressed and nondepressed pregnant women. Depression and Anxiety, 28, 676–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouyang M, Hellman K, Abel T, & Thomas SA (2004). Adrenergic signaling plays a critical role in the maintenance of waking and in the regulation of REM sleep. Journal of Neurophysiology, 92, 2071–2082. doi: 10.1152/jn.00226.2004 [DOI] [PubMed] [Google Scholar]
- Paivio SC (2001). Stability of retrospective self-reports of child abuse and neglect before and after therapy for child abuse issues. Child Abuse & Neglect, 25, 1053–1068. doi: 10.1016/s0145-2134(01)00256-3 [DOI] [PubMed] [Google Scholar]
- Pien GW, & Schwab RJ (2004). Sleep disorders during pregnancy. Sleep, 27, 1405–1417. doi: 10.1093/sleep/27.7.1405 [DOI] [PubMed] [Google Scholar]
- Qiu C, Gelaye B, Zhong Q-Y, Enquobahrie DA, Frederick IO, & Williams MA (2016). Construct validity and factor structure of the Pittsburgh sleep quality index among pregnant women in a Pacific-northwest cohort. Sleep and Breathing, 20, 293–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raniti MB, Waloszek JM, Schwartz O, Allen NB, & Trinder J (2018). Factor structure and psychometric properties of the Pittsburgh sleep quality index in community-based adolescents. Sleep, 41, zsy066. [DOI] [PubMed] [Google Scholar]
- Reuben A, Moffitt TE, Caspi A, Belsky DW, Harrington H, Schroeder F, … Danese A (2016). Lest we forget: Comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. Journal of Child Psychology and Psychiatry, 57, 1103–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano E, Zoccolillo M, & Paquette D (2006). Histories of child maltreatment and psychiatric disorder in pregnant adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 329–336. doi: 10.1097/01.chi.0000194563.40418.81 [DOI] [PubMed] [Google Scholar]
- Seng JS, Low LK, Sperlich M, Ronis DL, & Liberzon I (2009). Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstetrics & Gynecology, 114, 839–847. doi: 10.1097/AOG.0b013e3181b8f8a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma SK, Nehra A, Sinha S, Soneja M, Sunesh K, Sreenivas V, & Vedita D (2016). Sleep disorders in pregnancy and their association with pregnancy outcomes: A prospective observational study. Sleep and Breathing, 20, 87–93. doi: 10.1007/s11325-015-1188-9 [DOI] [PubMed] [Google Scholar]
- Shea AK, Streiner DL, Fleming A, Kamath MV, Broad K, & Steiner M (2007). The effect of depression, anxiety and early life trauma on the cortisol awakening response during pregnancy: Preliminary results. Psychoneuroendocrinology, 32, 1013–1020. doi: 10.1016/j.psyneuen.2007.07.006 [DOI] [PubMed] [Google Scholar]
- Sheehan CM, Li L, & Friedman EM (2020). Quantity, timing, and type of childhood adversity and sleep quality in adulthood. Sleep Health, 6, 246–252. [DOI] [PubMed] [Google Scholar]
- Skouteris H, Germano C, Wertheim EH, Paxton SJ, & Milgrom J (2008). Sleep quality and depression during pregnancy: A prospective study. Journal of Sleep Research, 17, 217–220. [DOI] [PubMed] [Google Scholar]
- Spertus IL, Yehuda R, Wong CM, Halligan S, & Seremetis SV (2003). Childhood emotional abuse and neglect as predictors of psychological and physical symptoms in women presenting to a primary care practice. Child Abuse & Neglect, 27, 1247–1258. [DOI] [PubMed] [Google Scholar]
- Spicer J, Werner E, Zhao Y, Choi CW, Lopez-Pintado S, Feng T, … Monk C (2013). Ambulatory assessments of psychological and peripheral stress-markers predict birth outcomes in teen pregnancy. Journal of Psychosomatic Research, 75(4), 305–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinhoven P, Penninx BW, Hickendorff M, van Hemert AM, Bernstein DP, & Elzinga BM (2014). Childhood trauma questionnaire: Factor structure, measurement invariance, and validity across emotional disorders. Psychological Assessment, 26, 717–729. doi: 10.1037/pas0000002 [DOI] [PubMed] [Google Scholar]
- Tanaka M, Wekerle C, Schmuck ML, Paglia-Boak A, & Team MAPR (2011). The linkages among childhood maltreatment, adolescent mental health, and self-compassion in child welfare adolescents. Child Abuse & Neglect, 35, 887–898. doi: 10.1016/j.chiabu.2011.07.003 [DOI] [PubMed] [Google Scholar]
- Treutiger B-M, & Lindberg L (2013). Prevention of depressive symptoms among adolescent girls. In Andershed A-K (Ed.), Girls at risk: Swedish longitudinal research on adjustment (pp. 57–78). New York, NY: Springer New York. [Google Scholar]
- U.S. Department of Health & Human Services & Administration on Children. (2020). Child maltreatment 2018. Retrieved from https://www.acf.hhs.gov/cb/research-data-technology/statistics-research/child-maltreatment
- Wang Y, Raffeld MR, Slopen N, Hale L, & Dunn EC (2016). Childhood adversity and insomnia in adolescence. Sleep Medicine, 21, 12–18. doi: 10.1016/j.sleep.2016.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warland J, Dorrian J, Morrison JL, & O’Brien LM (2018). Maternal sleep during pregnancy and poor fetal outcomes: A scoping review of the literature with meta-analysis. Sleep Medicine Reviews, 41, 197–219. [DOI] [PubMed] [Google Scholar]
- Wegman HL, & Stetler C (2009). A meta-analytic review of the effects of childhood abuse on medical outcomes in adulthood. Psychosomatic Medicine, 71, 805–812. doi: 10.1097/PSY.0b013e3181bb2b46 [DOI] [PubMed] [Google Scholar]
- Widom CS, Czaja SJ, Bentley T, & Johnson MS (2012). A prospective investigation of physical health outcomes in abused and neglected children: New findings from a 30-year follow-up. American Journal of Public Health, 102, 1135–1144. doi: 10.2105/AJPH.2011.300636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yali AM, & Lobel M (1999). Coping and distress in pregnancy: An investigation of medically high risk women. Journal of Psychosomatic Obstetrics & Gynecology, 20, 39–52. [DOI] [PubMed] [Google Scholar]


