Highlights
-
•
A moderate level of post-traumatic growth was identified among Syrian refugees in Istanbul.
-
•
Higher post-traumatic growth was associated with younger age and moderate levels of post-traumatic stress disorder.
-
•
Mental health services could explore supporting post-traumatic growth, while addressing potentially negative consequences.
Keywords: Post-traumatic growth, Refugees, Syria, Turkey, Post-traumatic stress disorder
Abstract
Aims
The negative mental health effects of exposure to trauma are well-documented. However, some individuals are theorized to undergo post-traumatic growth (PTG) after exposure to trauma, potentially experiencing positive psychological change across five domains: appreciation for life, relationships with others, new possibilities in life, personal strength, and spiritual change. PTG is less studied in forcibly displaced populations in low- and middle-income countries. This study aimed to explore levels of PTG and associated factors among Syrian refugee adults living in Istanbul, Turkey.
Methods
A cross-sectional survey was conducted with 1678 respondents. This study analyzed PTG data from 768 individuals as measured by the Post-Traumatic Growth Inventory (PTGI). Descriptive analysis and univariate and multivariate least squares linear regression modeling were used. Factor analysis and Cronbach's alpha tests assessed the psychometric properties of the PTGI.
Results
The sample exhibited a moderate level of PTG at 55.94 (SD=22.91, range 0–105). Factor analysis of PTGI revealed only four factors instead of five, and the PTGI yielded high internal reliability (Cronbach's α=0.90). PTG and post-traumatic stress disorder (PTSD) had a curvilinear relationship, with the highest PTG levels experienced by those with moderate PTSD levels. Five other variables were significantly associated with PTG: older age, less education, somatic distress, and history of an overnight stay at a health facility for mental health care were associated with lower PTG, while more years of education were associated with higher PTG.
Conclusions
This study identified the role of the sociodemographic and psychological determinants that influence post-traumatic growth among Syrian refugees in Istanbul. These findings could be used to inform future research and programs seeking to understand PTG in refugees.
1. Background
Syrians who have fled to neighboring countries and beyond since the outbreak of conflict in 2011 comprises the single largest group of displaced people worldwide (UNHCR, 2020). Turkey currently hosts the largest number of Syrian refugees at roughly 3.6 million (UNHCR, 2020). In Turkey, high rates of PTSD, depression and anxiety have been recorded among Syrian refugees due to exposure to traumatic events, forced displacement, and daily stressors after displacement including social isolation, discrimination, poverty, unemployment, and poor living conditions (Alpak et al., 2015; Acarturk et al., 2020). However, the current health system response in Turkey is inadequate, resulting in a high mental health treatment gap (Fuhr et al., 2019; Hendrickx et al., 2020).
Post-traumatic growth (PTG) describes positive psychological change that occurs after the experience of trauma (Calhoun and Tedeschi, 2006). PTG is commonly measured by the Post-Traumatic Growth Inventory (PTGI) that divides the construct of PTG into five domains: appreciation of life, relationships with others, new possibilities in life, personal strength, and spiritual change (Tedeschi and Calhoun, 1996). By processing previous traumas, individuals who undergo PTG have been assumed to experience a decrease in emotional distress and increase in acceptance of new realities. It is theorized that they emerge with those five new domains that help them deal with daily life post-trauma (Calhoun and Tedeschi, 2006). On the other hand, it has also been proposed that PTG may be maladaptive and reflect defensive or avoidant coping, since it has been found to be related to greater psychological distress and PTSD symptoms, both in cross-sectional studies (Hall et al., 2010) and prospective studies (Engelhard et al., 2015). The relationship between PTSD and PTG is complex. Some studies have indicated PTSD scores (based on standardized screening checklists) have a positive linear relationship with PTG scores, whereby higher PTSD scores are related to more PTG (Zalta et al., 2017). Other studies have reported a negative relationship, as higher PTSD corresponds to less PTG (Ssenyonga et al., 2013), while some cross-sectional studies have indicated no association (Zoellner and Maercker, 2006). A number of studies have reported a curvilinear relationship, typically an inverted U-shape: PTSD and PTG increase linearly until a threshold, after which PTG decreases as PTSD score increases (Nuttman-Shwartz et al., 2011; Joseph et al., 2012; Dar and Iqbal, 2020). Research on non-Syrian refugees groups has found evidence of all four types of association (Chan et al., 2016).
Demographic factors reported to be associated with PTG include older individuals tending to experience less PTG, while younger individuals report more PTG (Helgeson et al., 2006). Females tend to report more PTG than males (Vishnevsky et al., 2010), and more educated individuals tend to have higher PTG scores (Weiss, 2004). Other factors commonly associated with PTG are hope and optimism, religiosity, coping strategies, and personality traits (Wilson and Boden, 2008; Prati and Pietrantoni, 2009; Scrignaro et al., 2011).
The associations of factors with PTG in refugee-specific studies have both confirmed and deviated from mainstream literature on PTG. A recent review revealed that certain factors, like age and social support, have replicated trends found in PTG studies on other populations (Chan et al., 2016). However, other factors such as gender have diverged from the wider literature, as female refugees do not display more PTG as compared to male refugees (Teodorescu et al., 2012; Ssenyonga et al., 2013). As the refugee population faces unique challenges not encountered by other groups, the available literature inadequately portrays the distinct PTG profile of refugees. Factors related to the experience of resettlement, such as cultural friction and post-migration stressors, have been particularly understudied (Chan et al., 2016).
Although there has been wide acknowledgment of the mental health needs of conflict-affected populations, there is substantially less research available on psychological constructs that can potentially aid this group in recovery and sustained wellbeing. Studying constructs like PTG could help elucidate the mechanisms that strengthen individual agency (albeit recognizing there is also evidence that PTG can also be maladaptive (Zalta et al., 2017)). In the context of Syrian refugees in Istanbul, mapping PTG against health, sociodemographic, and post-displacement variables can provide insight into patterns and inform future consideration of PTG with other forcibly displaced populations. Studies on PTG have historically focused on populations from high-income countries who face trauma, such as chronic illness survivors (Barskova and Oesterreich, 2009; Shand et al., 2015). There remains more limited research with refugees in low- and middle-income countries, including Syrian refugees (Rizkalla and Segal, 2018; Ersahin, 2020). Moreover, data on the psychometric properties of the PTGI among refugees remain scarce (Chan et al., 2016).
This study sought to answer the research question, ‘What are the drivers of post-traumatic growth among Syrian refugee adults living in Istanbul, Turkey?’ and aimed to examine levels of post-traumatic growth and associated factors in this group. The specific objectives were threefold: (i) analyze the distribution of post-traumatic growth in the sample; (ii) assess psychometric properties of the Post-Traumatic Growth Inventory scale; and (iii) analyze factors associated with post-traumatic growth, particularly post-traumatic stress disorder.
2. Methods
2.1. Study design
A cross-sectional survey was conducted in February-May 2018 among Syrian refugees aged 18 years old and older living in Sultanbeyli, Istanbul, Turkey. Sultanbeyli is a district in Istanbul that hosts one of the largest communities of Syrian refugees in Istanbul (Erdoğan, 2017). Participants were randomly sampled using Sultanbeyli Municipality's registration system, which maintains a record of all Syrian refugees living in Sultanbeyli granted the official ‘Temporary Protection’ status from the Turkish government (Republic of Turkey: Ministry of Interior, 2020). Individuals who were under the influence of alcohol or drugs, who faced severe mental impairments, or who were non-native Arabic speakers were excluded. Potential participants were first recruited via telephone, then invited to be interviewed face-to-face at a refugee community center in central Sultanbeyli. The interviews were conducted in Arabic by trained researchers supervised by an experienced researcher with a degree in clinical psychology. Interviews lasted <45 min, and participants received 30 Turkish Lira (approximately €6) as compensation. Informed consent was obtained, and participants and researchers were matched by gender. Further details on the survey methods have been reported elsewhere (Fuhr et al., 2019; McGrath et al., 2020). The survey was part of the broader Scaling Up Psychological Interventions with Syrian Refugees (STRENGTHS) research project (Sijbrandij et al., 2017). Ethics approval was received from the Institutional Review Boards at Istanbul Sehir University and the London School of Hygiene and Tropical Medicine.
2.2. Measures
The primary outcome of PTG was measured with the 21-item PTGI (Tedeschi and Calhoun, 1996). This inventory uses 6-point Likert scales (0 to 5) to measure positive outcomes and yields a summed score as well as scores in five subscales: ‘New Possibilities‘ (five items), ‘Personal Strength‘ (four items), ‘Appreciation of Life‘ (three items), ‘Relating to Others‘ (seven items), and ‘Spiritual Change‘ (two items). The PTGI has been previously validated in conflict-affected populations (Powell et al., 2003; Salo et al., 2005), and the Arabic translation has been validated in multiple Palestinian samples (Kira et al., 2012; Shamia et al., 2015; Veronese and Pepe, 2019).
The following mental health-related measures were also screened: depression and anxiety symptoms using the Hopkins Symptoms Checklist (HSCL-25) (Mollica et al., 2004), where scores were summed and compared to a cut-off score of ≥2.1 (depression) and ≥2.0 (anxiety) (Fares et al., 2019); PTSD symptoms measured using the PTSD Checklist for DSM-5 (PCL-5), where scores were summed and compared to a cut-off of ≥33 (Bovin et al., 2016); and somatic distress symptoms using the Patient Health Questionnaire-15 (PHQ-15), where a range of scores from 0 to 30 measured four severity distress levels of ‘minimal‘ (0–4), ‘mild‘ (5–9), ‘moderate‘ (10–14), or ‘severe‘ (≥15) (Kroenke et al., 2002). These scales have been validated in several settings, including in conflict-affected populations (Mollica et al., 1987; Kroenke et al., 2002; Semrau et al., 2012; Blevins et al., 2015). In this study, they demonstrated high internal validity: the PHQ-15, PCL-5, and HSCL-25 had Cronbach's alpha values of 0.83, 0.84, and 0.91, respectively.
The researchers collected a variety of demographic and mental health information, including age, sex, mental ill health treatment history, years of displacement, and attitudes toward people with mental health issues adapted from the Program for Improving Mental Health Care (PRIME) (De Silva et al., 2016).
2.3. Data analysis
Three types of statistical analyses were conducted, reflecting the three study objectives. First, descriptive analysis was conducted on levels of PTG, mental health outcomes, and sociodemographic variables. Second, we tested the psychometric properties of PTGI: internal reliability was assessed using Cronbach's alpha for the entire PTGI scale and its five subscales, and construct validity was tested through exploratory factor analysis using principal components analysis with varimax rotation (as used in the original study by Tedeschi and Calhoun (1996) and subsequent studies (Ho et al., 2004; Weiss and Berger, 2006)).
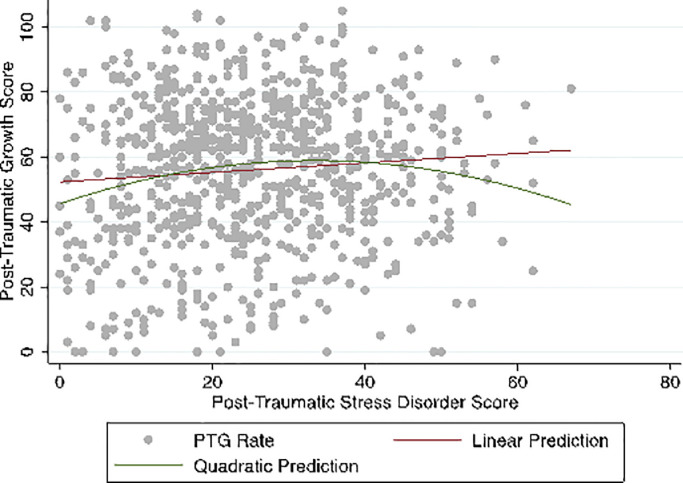
The third analysis explored factors associated with PTG. Initial T-tests and ANOVA tests were run to detect any differences in mean PTG scores between demographic and socioeconomic groups. The associations between the PTG score and independent variables were then tested using univariate ordinary least squares regression. Scatterplots with overlaid linear prediction plots were used to determine linearity between PTG and each continuous exposure variable. Because PTSD may have a positive, negative, or curvilinear relationship with PTG (Dar and Iqbal, 2020), a scatterplot of PTG and PTSD, overlaid with linear and quadratic prediction plots, was built to assess curvilinearity between these two variables. Forward stepwise regression was then used to build the exploratory multiple linear regression model. Possible confounding variables were added to the null model. Sociodemographic and psychological outcome variables were then added individually in a stepwise fashion. Variables with p-values <0.05 were kept, while those >0.05 were removed until the final model based on a complete case analysis was achieved (Rothman et al., 2008). The data were tested for multicollinearity by analysing the variance inflation factor (Williams et al., 2013). All data were analysed using Stata/IC 16.0.
3. Results
A total of 1678 individuals were surveyed, representing a 59% response rate. Of these participants, 768 people were administered the PTGI because they selected “yes” to the screening question, “Have you ever experienced yourself or witnessed others experience very stressful life events?” Table 1 displays key sociodemographic and psychological characteristics of these 768 respondents. Approximately two-thirds of the sample were male (59.2%). The mean age in the sample was 35.5 years (range 18–67 years). The mean number of years of education was 7.4 years, and the majority of participants had either a primary school education (43.9) or pre-secondary education (32.6%). Nearly all women in the sample (94.9%) were “not in employment.” Nearly half of the men (44.8%) were regularly employed, while approximately one-quarter of men (24.6%) were irregularly employed. In this sample, the estimated prevalence of PTSD, anxiety, and depression was 28.8%, 43.2%, and 47.0%, respectively. On average, the number of years displaced was 3.4 years.
Table 1.
PTG scores and key sociodemographic and mental health characteristics of Syrian refugee adult sample (N = 768).
| PTG Score | |||||
|---|---|---|---|---|---|
| Variable | n/N | % | M | SD | 95% CI |
| Sex | |||||
| Male | 455/768 | 59.24 | 55.53 | 23.14 | 53.39–57.66 |
| Female | 313/768 | 40.76 | 56.55 | 22.58 | 54.04–59.06 |
| Age (in years) | |||||
| 18–24 | 165/766 | 21.54 | 56.76 | 21.65 | 53.44–60.09 |
| 25–34 | 249/766 | 32.50 | 59.47 | 22.54 | 56.66–62.28 |
| 35–44 | 177/766 | 23.11 | 57.74 | 22.44 | 54.41–61.07 |
| 45–54 | 106/766 | 13.84 | 48.92 | 22.02 | 44.68–53.17 |
| 55+ | 69/766 | 9.01 | 46.74 | 25.29 | 40.66–52.82 |
| Education | |||||
| No formal education | 43/764 | 5.63 | 48.40 | 25.60 | 40.52–56.27 |
| Primary school (1–6 years) | 335/764 | 43.85 | 53.85 | 23.55 | 51.32–56.38 |
| Pre-secondary (7–9 years) | 249/764 | 32.59 | 58.06 | 22.44 | 55.26–60.87 |
| Upper secondary (10–12 years) | 83/764 | 10.86 | 56.47 | 20.18 | 52.06–60.88 |
| Higher education (>12 years) | 54/764 | 7.07 | 64.98 | 18.09 | 60.04–69.92 |
| Employment | |||||
| Regular employment | 213/768 | 27.73 | 58.72 | 21.02 | 55.87–61.57 |
| Irregular employment | 118/768 | 15.36 | 58.14 | 23.92 | 53.77–62.50 |
| Unemployed | 64/768 | 8.33 | 52.61 | 22.05 | 47.10–58.11 |
| Not in employment a | 373/768 | 48.57 | 54.33 | 23.46 | 51.94–56.73 |
| Post-traumatic stress disorder | |||||
| Yes | 220/765 | 28.76 | 57.37 | 20.62 | 54.62–60.11 |
| No | 545/765 | 71.24 | 55.56 | 23.46 | 53.58–57.54 |
| Anxiety | |||||
| Yes | 331/767 | 43.16 | 57.86 | 20.77 | 55.60–60.11 |
| No | 436/767 | 56.84 | 54.70 | 24.10 | 52.43–56.97 |
| Somatic distress | |||||
| No distress | 181/766 | 23.63 | 57.80 | 24.02 | 54.26–61.34 |
| Mild distress | 204/766 | 26.63 | 58.19 | 22.85 | 55.03–61.35 |
| Moderate distress | 182/766 | 23.76 | 55.35 | 21.06 | 52.27–58.43 |
| Severe distress | 199/766 | 25.98 | 52.91 | 22.83 | 49.71–56.11 |
| Ever admitted for overnight stay in healthcare facility | |||||
| Yes | 73/765 | 9.54 | 49.19 | 24.53 | 43.47–54.92 |
| No | 692/765 | 90.46 | 56.92 | 22.34 | 55.25–58.60 |
| Total Sample | 768 | 100 | 55.94 | 22.91 | 54.32–57.57 |
“Not in employment” refers to individuals who selected “housewife,” “maternity,” “retired,” “student,” “volunteer,” or “other.”
There was a moderate level of PTG in the sample, with a mean score of 55.94 (SD=22.91, range 0–105). The distribution of PTG scores was roughly normal.
The internal reliability of total PTGI score was high, with a Cronbach's α=0.90. The subscales of ‘Personal Strength’, ‘New Possibilities’, ‘Relating to Others, and ‘Spiritual Change’ reported acceptable Cronbach's α of 0.79, 0.77, 0.75, and 0.65 respectively. However, ‘Appreciation for Life’ had a low α of 0.59.
The PTGI's construct validity was tested with principal components analysis with varimax rotation. The analysis failed to replicate all five factors but did produce four factors with eigenvalues >1 that accounted for 53.76% of the variance. The items retained were items with loadings >0.5, with no loading on another factor >0.4, and with a difference >0.3 between an item's loading on two factors. Table 2 outlines twelve items out of the 21-item scale that met these criteria and maps them onto the four factors identified. Factor I (5 items, 19.02% of variance) broadly described changes to the self, combining two items from the original ‘Spiritual Change’ subscale and three from the ‘Personal Strength’ subscale. The remaining three factors were very similar to original subscales: Factor II (3 items, 15.86% of variance) contained items from the ‘New Possibilities’ subscale; Factor III (3 items, 11.15% of variance) possessed items from ‘Relating to Others’; and Factor IV (1 item, 7.54% of variance) had one item from ‘Relating to Others.’
Table 2.
Factor loadings of the PTGI in a Syrian refugee sample (N = 768).
| Item, Text, and New Factor | Original Factor | New Factor Loadings |
|||
|---|---|---|---|---|---|
| I | II | III | IV | ||
|
Factor I: Self (19.02% of variance) 5. I have a better understanding of spiritual matters. 10. I know better that I can handle difficulties. 12. I am better able to accept the way things work out. 18. I have a stronger religious faith. 19. I discovered that I'm stronger than I thought I was. |
SC PS PS SC PS |
0.60 0.65 0.68 0.73 0.68 |
0.33 |
||
|
Factor II: New Possibilities (15.86% of variance) 3. I developed new interests. 7. I established a new path for my life. 14. New opportunities are available which wouldn't have been otherwise. |
NP NP NP |
0.65 0.73 0.69 |
0.32 |
||
|
Factor III: Relating to Others (11.15% of variance) 6. I more clearly see that I can count on people in times of trouble. 20. I learned a great deal about how wonderful people are. 21. I accept needing others. |
RO RO RO |
0.69 0.66 0.76 |
0.36 |
||
|
Factor IV: Appreciation of Life (7.54% of variance) 1. I changed my priorities about what is important in life. |
AL |
0.76 |
|||
|
Items failing to load differentially: 2. I have a greater appreciation for the value of my own life. 4. I have a greater feeling of self-reliance. 8. I have a greater sense of closeness with others. 9. I am more willing to express my emotions. 11. I am able to do better things with my life. 13. I can better appreciate each day. 15. I have more compassion for others. 16. I put more effort into my relationships. 17. I am more likely to try to change things which need changing. |
AL PS RO RO NP AL RO RO NP |
0.53 0.30 0.43 0.52 0.51 0.33 0.50 |
0.42 0.42 0.42 0.60 0.52 0.25 0.43 0.45 |
0.55 0.3 |
0.47 0.33 0.40 |
Note: PS: Personal strength; NP: New possibilities; RO: Relating to others; AL: Appreciation of life; SC: Spiritual change. Only loadings >0.3 are shown. Bolded loadings correspond to items that were retained based on the criteria that one factor loaded >0.5, that no other factor loaded >0.4, and that the difference between two loadings was >0.3.
PTG scores did not differ significantly between women and men (t=−0.61, p = 0.54), between those with PTSD and those without (t=−0.85, p = 0.40), between those with anxiety and those without (t=−1.81, p = 0.07), nor among somatic distress levels (F(3762)=2.49, p = 0.06). PTG scores did differ significantly among age groups (F(4761)=7.32, p<0.001). Beyond the 18–24 age group, PTG decreases with increasing age: individuals aged 25–34 years recorded the highest level of PTG (M = 59.47, 95% CI 56.66–62.28), while the oldest group of 55+ years recorded the lowest level (M = 46.74, 95% CI 40.66–52.82). Similarly, PTG varied among education levels (F(4759)=4.63, p = 0.001). The highest PTG levels existed among individuals with the highest level of >12 years of education (M = 64.98, 95% CI 60.04–69.92), while the lowest PTG was found in those with no formal education (M = 48.40, 95% CI 40.52–56.27). There were smaller differences in PTG scores among employment types overall (F(3764)=2.80, p = 0.04), with similar levels recorded between those in employment and irregular employment, while those unemployed had the lowest PTG scores.
An augmented component-plus-residual plot demonstrated a curvilinear relationship between PTG and PTSD: PTG scores appear to increase until a PTSD score of approximately 30, then decreases as PTSD increases past 30 (see Fig. 1). To account for this negative quadratic relationship, the continuous PTSD variable was squared (Shakespeare-Finch and Lurie-Beck, 2014).
Fig. 1.
Two-way scatterplot of PTG and PTSD, overlaid with linear and quadratic prediction plots.
Univariate analysis revealed that the variables with strong evidence of a linear relationship with PTG were age group (p < 0.001), years of education (p < 0.001), PTSD score (p = 0.01)/squared PTSD score (p < 0.001), somatic distress score (p = 0.02), overnight hospital stay (p = 0.006), and two PRIME variables (p = 0.03 and p = 0.04, respectively (see Online Annex A). Variances of these seven exposure variables remained low, explaining only 0.1–8% of the variation in PTG rate. These seven variables, along with potential confounders, were tested in the multivariate model.
Table 3 describes the results of the forward stepwise procedures. In Step 1, a priori confounders of age and sex were added to the null model. When age and sex were included, only the 45–54 group (β=−0.12, p = 0.007) and 55+ group (β = −0.13, p = 0.007) were meaningful additions to the model. ‘Age group’ was thus kept in Step 2, while sex (β = 0.01, p = 0.08) was omitted. In Step 2, the sociodemographic variables of education and employment were added stepwise into the model. The same two age groups remained statistically significant, and there was strong evidence that ‘Education’ had a non-zero coefficient and thus real effect on PTG (β = 0.13, p < 0.001). None of the employment categories resulted in strong evidence of a linear association with PTG (p = 0.96, 0.49, 0.43, respectively), so the ‘Employment’ variable was excluded in the next step. In Step 3, psychological outcome variables were added to the model: PTSD score (p < 0.001), somatic distress score (p = 0.001), and lifetime history (p = 0.007) of an overnight stay at a facility for mental healthcare. Given the negative quadratic relationship between PTSD and PTG, the squared PTSD score variable was added. Once added, the variance of the model improved from 0.08 (F(8747)=8.42, p < 0.001) to 0.10 (F(9746)=8.71, p < 0.001). All four of the new variables added in Step 3 showed strong evidence of an association with PTG, and education and age remained statistically significant. The Step 3 model, which demonstrates strong evidence of an association between PTG and five variables (F(9746)=8.71, p < 0.001), explained 3% more of the variation in PTG than the Step 2 model (adjusted R2 = 0.08). Finally, the two PRIME variables that describe attitudes toward mental health were added in Step 4. Neither PRIME variable demonstrated evidence of an association with PTG, so the Step 3 model was the final model. Age, education, PTSD score (and squared PTSD score), somatic distress score, and lifetime history of an overnight stay for mental health care were the final five variables that predict PTG. This model demonstrated a lack of multicollinearity (vif=3.98).
Table 3.
Factors associated with PTG in multivariate regression analysis.
| Step 1 |
Step 2 |
Step 3* |
Step 4 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | B (SE) | β | p | B (SE) | β | p | B (SE) | β | p | B (SE) | β | p |
| Sex Female Age group 25–34 years 35–44 years 45–54 years 55+ years Education (in years) Employment Irregular employment Unemployed Not in employment PTSD score Squared PTSD score⁎⁎ Somatic distress score Overnight stay Yes Medication⁎⁎⁎ Agree slightly Neither Disagree slightly Disagree strongly Willing to live⁎⁎⁎⁎ Agree slightly Neither Disagree slightly Disagree strongly |
0.42 (1.67) 2.55 (2.26) 0.64 (2.45) −7.71 (2.83) −10.13 (3.24) - - - - - - - - - - - - - - - - |
0.01 0.05 0.01 −0.12 −0.13 - - - - - - - - - - - - - - - - - |
0.08 0.26 0.79 0.007 0.002 - - - - - - - - - - - - - - - - - |
- 2.29 (2.25) 0.84 (2.43) −6.93 (2.85) −8.58 (3.28) 0.82 (0.22) −0.1 (2.6) −2.3 (3.3) −1.6 (2.0) - - - - - - - - - - - - - |
- 0.05 0.02 −0.10 −0.11 0.13 0.002 −0.03 −0.03 - - - - - - - - - - - - - |
- 0.31 0.73 0.02 <0.001 <0.001 0.96 0.49 0.43 - - - - - - - - - - - - - |
- 1.45 (2.20) 1.42 (2.39) −7.17 (3.74) −7.85 (3.16) 0.69 (0.22) - - - 0.91 (0.22) −0.01 (0.004) −0.52 (0.15) −7.38 (2.71) - - - - - - - - - |
- 0.03 0.03 −0.11 −0.10 0.11 - - - 0.53 −0.40 −0.14 −0.10 - - - - - - - - - |
- 0.51 0.55 0.01 0.01 0.002 - - - <0.001 0.001 0.001 0.007 - - - - - - - - - |
- 0.68 (2.29) 0.28 (2.49) −8.43 (2.85) −8.38 (3.37) 0.63 (0.22) - - - 0.75 (0.23) −0.01 (0.004) −0.44 (0.16) −8.63 (2.80) −4.39 (2.07) 2.82 (3.57) −8.15 (2.79) −4.62 (2.33) 1.53 (2.40) −0.05 (3.41) 4.48 (3.34) −4.17 (2.06) |
- 0.01 0.01 −0.13 −0.10 0.11 - - - 0.45 −0.32 −0.13 −0.11 −0.09 0.03 −0.11 −0.08 0.03 −0.001 0.05 −0.09 |
- 0.77 0.91 0.003 0.01 0.004 - - - 0.001 0.02 0.007 0.002 0.03 0.43 0.004 0.05 0.52 0.99 0.18 0.04 |
| Observations (n) R2 Adjusted R2 F Prob>F Δ Adjusted R2 |
762 0.04 0.03 5.69 <0.001 - |
762 0.06 0.05 5.56 <0.001 0.02 |
756 0.10 0.08 8.71 <0.001 0.03 |
668 0.13 0.10 5.51 <0.001 0.03 |
||||||||
Note: B=unstandardized regression coefficient; SE=standard error; β=standardized regression coefficient; p = p-value; R²=variance; adjusted R²=adjusted variance; F = F statistic; Prob>F=probability that the null hypothesis (all regression coefficients in model are zero) is true; Δ Adjusted R²=difference in the variance between steps.
This is the final adjusted model.
This is the squared continuous PTSD score.
The full statement is, “Medication can be an effective treatment for people with mental health problems.”
The full statement is, “I would be willing to live with someone with a mental health problem.”
4. Discussion
The study provides new evidence on levels of PTG and associated influence of sociodemographic and psychological factors among refugees in a low- and middle-income country context. The mean PTG score reported in our study of 55.94 can be considered a moderate level of PTG (Holtmaat et al., 2017; Rizkalla and Segal, 2018). A similar mean score of 51.36 (SD=19.90) was reported with Syrian refugees living in Jordan (Rizkalla and Segal, 2018) and in Turkey (M = 49.11, SD=29.11) (Ersahin, 2020). The prevalence of PTSD in this sample (28.76%) was within the range (11.4%−83.4%) found in other studies of Syrian refugees living in Turkey and European host countries (Alpak et al., 2015; Tinghög et al., 2017; Chung et al., 2018; Georgiadou et al., 2018).
Older age and PTG appear to have a strong negative linear relationship, with age groups of 45–54 and 55+ years being the strongest contributing factors associated with PTG (negatively) in the model. In these two older groups, PTG is expected to decrease by nearly 8 points as compared to the youngest 25–34 group. Although age had an inconsistent relationship with PTG in previous refugee studies, this negative relationship aligns with the mainstream literature and some refugee studies (Powell et al., 2003). It is hypothesized that younger individuals exhibit more PTG because they may be more adept at making significant changes in their lives, while older individuals are less likely to interpret their larger accumulated number of traumas experiences as beneficial (Powell et al., 2003; Helgeson et al., 2006).
Additionally, an increase in years of education was associated with some increase in PTG (B = 0.69, p = 0.002). Though research on this relationship is less established, previous studies on refugee populations have verified the positive relationship between education and PTG found in this study. For instance, Salo et al. found internally displaced Palestinian men who were more highly educated experienced more PTG, and Ersahin found the same positive PTG-education correlation in Syrian refugees (Salo et al., 2005; Ersahin, 2020). Although the exact pathways are unclear, education may equip individuals with skills that facilitate opportunities in life.
However, there was no evidence of an association between employment and PTG, nor was economic situation an associated factor in the multivariate model. This was unexpected because such factors have had a significant association with PTG in previous studies, including with Syrian refugees in Jordan (Rizkalla and Segal, 2018). The divergence in our data could potentially be due to a ‘floor effect’ for our variable on household economic situation, with less than 5% of the sample describing their household economic situation as ‘Very good’ or ‘Good’ and a clustering of responses in the bottom two categories of ‘Average’ or ‘Bad.’ Consequently, this meant our scale lacked adequate range/variability to distinguish meaningful differences in economic situation.
The lack of association between gender and PTG in this study diverges from previous studies, which have commonly observed higher PTG scores in women (Ssenyonga et al., 2013). However, some other studies with refugees have also found no relationship between gender and PTG. This may be related to the severity and quantity of traumatic experiences, where the accumulation of trauma in women hinders PTG. The type of traumatic event is also likely to play a role, since the likelihood of experiencing certain traumatic events differs by gender (Tolin and Foa, 2008; Kilic et al., 2016); for instance, female refugees are more likely to experience sexual violence than male refugees (Vu et al., 2014). Women affected by conflict do tend to report higher rates of common mental disorders than men, and these disorders may obstruct PTG. Indeed, there was strong evidence of differences in levels of anxiety (t(765)=−7,52, p < 0.001), depression (t(765)=−6.93, p < 0.001), and PTSD (t(763)=−3.61, p < 0.001) between women and men. These higher rates of common mental disorders in women in the sample may have contributed to their lower-than-expected PTG.
The curvilinear PTG-PTSD relationship found in the data indicates that the highest level of PTG was experienced by those with moderate levels of PTSD. Less straightforward than a linear relationship, the U-shaped trend accounts for not only the psychologically significant events that trigger PTG (as suggested by the original study (Tedeschi and Calhoun, 1996)) but also the severe trauma that inhibits PTG. This curvilinearity has been confirmed by a number of studies (Nuttman-Shwartz et al., 2011; Shakespeare-Finch and Lurie-Beck, 2014, Dar and Iqbal 2020). A theorized mediator of the relationship is time: studies that measured PTG and PTSD directly after a traumatic event see a positive relationship between the two (Hall et al., 2010; Pietrzak et al., 2010; Teodorescu et al., 2012), but this correlation attenuates or inverts over time. Individuals in this study had been displaced 0–8 years, implying a certain amount of temporal distance from trauma, so this range may have influenced the PTG-PTSD curvilinear association. However, temporality of traumatic experiences was not directly measured in this study, so explanatory scope is limited.
Of the other mental health outcomes, neither depression nor anxiety was significantly associated with PTG in the model. However, somatic distress did show strong evidence of an association with PTG, demonstrating an inverse relationship with PTG (B=−0.52, p = 0.001). The research on somatic distress and PTG is scarce, especially in refugees, though the results from this study are consistent with those found in studies with non-forcibly displaced populations in high-income countries. For example, Ruini et al. found in breast cancer survivors that those with more PTG had decreased somatization (Ruini et al., 2013).
Having stayed overnight for mental healthcare had a strongly negative association with PTG (B = −7.38, p = 0.007). This variable indicates one or several experiences of mental illness so severe that an overnight stay was necessary, with the implication that the need must have been quite severe given the low healthcare utilization and high treatment gap in Syrian refugees (Fuhr et al., 2019). Potentially, these experiences of mental ill health had the additional effect of inhibiting PTG. However, the interpretation of this variable is challenging as few, if any, previous PTG studies have included such a variable.
To the best of our knowledge, ours is one of the few studies that analyses the psychometric properties of the PTGI with refugees in a low- and middle-income setting. There was high (Tavakol and Dennick, 2011) internal reliability of the PTGI overall, with a Cronbach's α of 0.90, and these findings are consistent with the original PTGI study (Tedeschi and Calhoun, 1996) that yielded Cronbach's α=0.90 in the full scale and between 0.67–0.85 in the subscales. The PTGI subscales had acceptable (Tavakol and Dennick, 2011) levels of alpha (0.65–0.79), with the exception of ‘Appreciation for Life’ which produced a low (Tavakol and Dennick, 2011) alpha at 0.59. Other refugee samples have similarly reported low values from this subscale, such as α = 0.52 (Kroo and Nagy, 2011)) and α=0.48 (Rizkalla and Segal, 2018). It is possible that this subscale yields low alpha values because the relatively recent resettlement of Syrian refugees in Turkey has not allowed greater appreciation for adjusted circumstances to develop (Rizkalla and Segal, 2018).
The factor analysis failed to replicate all five factors of the PTGI, but it produced four factors with eigenvalues >1 that accounted for 53.76% of the variance. This was comparable to the variance of 60% accounted for by the original study (Tedeschi and Calhoun, 1996). The four factors were also aligned with PTGI concepts, reflecting findings from other studies (Ho et al., 2004). Items from ‘Spiritual Change’ and ‘Personal Strength’ overlapped, loading onto the same factor. Speculatively, this may be related to the major role that religion plays in finding strength to overcome difficulties in resettled Syrians; qualitative studies have indicated that Islamic faith has been a source of empowerment and coping (Hasan et al., 2018; Şafak-AyvazoĞlu et al., 2020). Previous studies have also found that the PTGI is best represented by fewer than five factors, though methodologically this may be explained by high correlations among factors or the small number of items within certain subscales (Cobb et al., 2006; Taku et al., 2008; Kira et al., 2012).
The key policy consideration arising from our study is the need to explore activities to support PTG within mental health and psychosocial support programmes for Syrian refugees in Istanbul. These activities may be more appropriate for individuals who are more likely to exhibit PTG, such as those with moderate levels of PTSD and from younger adult age groups. However, the potentially maladaptive nature of PTG (Hall et al., 2010) should be recognised and addressed through careful service development and further research, ideally using longitudinal studies (Engelhard et al., 2015).
4.1. Limitations
This study had two main limitations. First, the final model had poor predictive power (adjusted R2 = 0.08, p < 0.001). This likely resulted from limited data collected through individual items on trauma exposure (which was not collected due to ethical concerns of risking re-traumatizing respondents). However, this restricted the ability to draw conclusions on the exposure of different types of trauma exposure, timing of trauma exposure, and cumulative trauma impact. However, a straightforward dose-response model, where level of PTG is linearly dependent on level of exposure, is often insufficient because traumatic experiences can have a cumulative impact. That cumulative trauma may decrease tolerance to distress, and thus ability to adapt to it (Kira et al., 2019). While there was no evidence of confounding based on the statistical tests used, it is still possible that an unmeasured variable confounded the association between PTG and a measured exposure variable, contributing to the final model's low variance.
Second, there may have been risks of response bias. Non-Arabic-speaking Syrian refugees were excluded, but these are very low in number in the study area. The non-response rate of 41% to the survey, as well as restrictions on sampling from a registry of temporary protection recipients (rather than one that also included undocumented refugees), may have increased response bias. Another possible source of response bias was the low proportion of individuals who responded to the PTGI after self-reporting experience of trauma (45.77%, n = 768).
The cross-sectional nature of the data does not show evidence of causation, nor can it reveal temporal relations among variables. Future research with refugees could utilize longitudinal designs to better understand the temporal effects of factors on PTG as done with other populations (Engelhard et al., 2015).
5. Conclusions
The study adds to emerging evidence on PTG and its determinants among refugees in low- and middle-income countries. It provides new evidence for the role that sociodemographic and psychological factors play in shaping PTG among Syrian refugees, highlighting PTSD, age, and education as particularly important determinants influencing PTG. This study also provides new insight into the phenomena of PTG that could inform future research and programs on PTG and PTSD with refugees in Istanbul and more globally.
Statement of ethical approval
Ethics approval was received from the Institutional Review Boards at Istanbul Sehir University and the London School of Hygiene and Tropical Medicine.
Statement of funding
The STRENGTHS Project is funded under Horizon 2020 the Framework Programme for Research and Innovation (20142020)(Grant agreement number is 733337). The content of this article reflects only the authors’ views and the European Community is not liable for any use that may be made of the information contained therein.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgment
We would like to thank the survey respondents and data collection team.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jmh.2020.100010.
Appendix. Supplementary materials
References
- Acarturk C., McGrath M., Roberts B., Ilkkursun Z., Cuijpers P., Sijbrandij M., Sondorp E., Ventevogel P., McKee M., Fuhr D.C. Prevalence and predictors of common mental disorders among Syrian refugees in Istanbul, Turkey: a cross-sectional study. Soc. Psychiatry Psychiatr. Epidemiol. 2020 doi: 10.1007/s00127-020-01941-6. [DOI] [PubMed] [Google Scholar]
- Alpak G., Unal A., Bulbul F., Sagaltici E., Bez Y., Altindag A., Dalkilic A., Savas H.A. Post-traumatic stress disorder among Syrian refugees in Turkey: a cross-sectional study. Int. J. Psychiatry Clin. Pract. 2015;19(1):45–50. doi: 10.3109/13651501.2014.961930. [DOI] [PubMed] [Google Scholar]
- Barskova T., Oesterreich R. Post-traumatic growth in people living with a serious medical condition and its relations to physical and mental health: a systematic review. Disabil. Rehabil. 2009;31(21):1709–1733. doi: 10.1080/09638280902738441. [DOI] [PubMed] [Google Scholar]
- Blevins C.A., Weathers F.W., Davis M.T., Witte T.K., Domino J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and Initial psychometric evaluation. J. Trauma Stress. 2015;28(6):489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Bovin M.J., Marx B.P., Weathers F.W., Gallagher M.W., Rodriguez P., Schnurr P.P., Keane T.M. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL-5) in veterans. Psychol. Assess. 2016;28(11):1379–1391. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Calhoun L.G., Tedeschi R.G. Lawrence Erlbaum Associates Publishers; Mahwah, NJ, US: 2006. Handbook of Posttraumatic Growth: Research & Practice. [Google Scholar]
- Chan K.J., Young M.Y., Sharif N. Well-being after trauma: a review of posttraumatic growth among refugees. Can. Psychol. 2016;57(4):291–299. [Google Scholar]
- Chung M.C., AlQarni N., AlMazrouei M., Al Muhairi S., Shakra M., Mitchell B., Al Mazrouei S., Al Hashimi S. Posttraumatic stress disorder and psychiatric co-morbidity among syrian refugees of different ages: the role of trauma centrality. Psychiatr. Q. 2018;89(4):909–921. doi: 10.1007/s11126-018-9586-3. [DOI] [PubMed] [Google Scholar]
- Cobb A.R., Tedeschi R.G., Calhoun L.G., Cann A. Correlates of posttraumatic growth in survivors of intimate partner violence. J. Trauma. Stress Off. Publ. Int. Soc. Trauma. Stress Stud. 2006;19(6):895–903. doi: 10.1002/jts.20171. [DOI] [PubMed] [Google Scholar]
- Dar I., Iqbal N. Beyond linear evidence: the curvilinear relationship between secondary traumatic stress and vicarious posttraumatic growth among healthcare professionals. Stress Health. 2020:1–10. doi: 10.1002/smi.2932. [DOI] [PubMed] [Google Scholar]
- Dar I.A., Iqbal N. Beyond linear evidence: the curvilinear relationship between secondary traumatic stress and vicarious posttraumatic growth among healthcare professionals. Stress Health. 2020;36(2):203–212. doi: 10.1002/smi.2932. [DOI] [PubMed] [Google Scholar]
- De Silva M.J., Rathod S.D., Hanlon C., Breuer E., Chisholm D., Fekadu A., Jordans M., Kigozi F., Petersen I., Shidhaye R., Medhin G., Ssebunnya J., Prince M., Thornicroft G., Tomlinson M., Lund C., Patel V. Evaluation of district mental healthcare plans: the PRIME consortium methodology. Br. J. Psychiatry J. Ment. Sci. 2016;208(Suppl 56):s63–s70. doi: 10.1192/bjp.bp.114.153858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelhard I.M., Lommen M.J.J., Sijbrandij M. Changing for better or worse? Posttraumatic growth reported by soldiers deployed to Iraq. Clin. Psychol. Sci. 2015;3(5):789–796. [Google Scholar]
- Erdoğan M.M. Gafa Media; 2017. Urban Refugees From" Detachment" to" Harmonization": Syrian Refugees and Process Management of Municipalities: The Case of Istanbul. [Google Scholar]
- Ersahin Z. Post-traumatic growth among Syrian refugees in Turkey: the role of coping strategies and religiosity. Curr. Psychol. 2020 [Google Scholar]
- Fares S., Dirani J., Darwish H. Arabic validation of the hopkins symptom checklist-25 (HSCL) in a Lebanese sample of adults and older adults. Curr. Psychol. 2019 [Google Scholar]
- Fuhr D.C., Acarturk C., McGrath M., Ilkkursun Z., Sondorp E., Sijbrandij M., Ventevogel P., Cuijpers P., McKee M., Roberts B. Treatment gap and mental health service use among Syrian refugees in Sultanbeyli, Istanbul: a cross-sectional survey. Epidemiol. Psychiatr. Sci. 2019;29:e70. doi: 10.1017/S2045796019000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgiadou E., Zbidat A., Schmitt G.M., Erim Y. Prevalence of mental distress among Syrian refugees with residence permission in Germany: a registry-based study. Front. Psychiatry. 2018;9:393. doi: 10.3389/fpsyt.2018.00393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall B.J., Hobfoll S.E., Canetti D., Johnson R.J., Palmieri P.A., Galea S. Exploring the association between posttraumatic growth and PTSD: a national study of Jews and Arabs following the 2006 Israeli-Hezbollah war. J. Nerv. Ment. Dis. 2010;198(3):180. doi: 10.1097/NMD.0b013e3181d1411b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan N., Mitschke D.B., Ravi K.E. Exploring the role of faith in resettlement among Muslim Syrian refugees. J. Relig. Spirit. Soc. Work Soc. Thought. 2018;37(3):223–238. [Google Scholar]
- Helgeson V.S., Reynolds K.A., Tomich P.L. A meta-analytic review of benefit finding and growth. J. Consult. Clin. Psychol. 2006;74(5):797–816. doi: 10.1037/0022-006X.74.5.797. [DOI] [PubMed] [Google Scholar]
- Hendrickx M., Woodward A., Fuhr D.C., Sondorp E., Roberts B. The burden of mental disorders and access to mental health and psychosocial support services in Syria and among Syrian refugees in neighboring countries: a systematic review. J. Public Health Oxf. 2020;42(3):e299–e310. doi: 10.1093/pubmed/fdz097. [DOI] [PubMed] [Google Scholar]
- Ho S., Chan C., Ho R. Post-traumatic growth in Chinese cancer survivors. Psychooncology. 2004;13:377–389. doi: 10.1002/pon.758. [DOI] [PubMed] [Google Scholar]
- Holtmaat K., van der Spek N., Cuijpers P., Leemans C.R., Verdonck-de Leeuw I.M. Posttraumatic growth among head and neck cancer survivors with psychological distress. Psychooncology. 2017;26(1):96–101. doi: 10.1002/pon.4106. [DOI] [PubMed] [Google Scholar]
- Joseph S., Murphy D., Regel S. An affective-cognitive processing model of post-traumatic growth. Clin. Psychol. Psychother. 2012;19:316–325. doi: 10.1002/cpp.1798. [DOI] [PubMed] [Google Scholar]
- Kilic C., Magruder K.M., Koryurek M.M. Does trauma type relate to posttraumatic growth after war? A pilot study of young Iraqi war survivors living in Turkey. Transcult. Psychiatry. 2016;53(1):110–123. doi: 10.1177/1363461515612963. [DOI] [PubMed] [Google Scholar]
- Kira I., Abou-Median S., Ashby J., Lewandowski L., Mohanesh J., Odenat L. Post-traumatic growth inventory: psychometric properties of the Arabic version in Palestinian adults. Int. J. Educ. Psychol. Assess. 2012;11(2):120–137. [Google Scholar]
- Kira I.A., Shuwiekh H., Al Ibraheem B., Aljakoub J. Appraisals and emotion regulation mediate the effects of identity salience and cumulative stressors and traumas, on PTG and mental health: the case of Syrian's IDPs and refugees. Self Identity. 2019;18(3):284–305. [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom. Med. 2002;64(2) doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- Kroo A., Nagy H. Posttraumatic growth among traumatized Somali refugees in Hungary. J. Loss Trauma. 2011;16(5):440–458. [Google Scholar]
- McGrath M., Acarturk C., Roberts B., Ilkkursun Z., Sondorp E., Sijbrandij M., Cuijpers P., Ventevogel P., McKee M., Fuhr D.C. Somatic distress among Syrian refugees in Istanbul, Turkey: a cross-sectional study. J. Psychosom. Res. 2020;132 doi: 10.1016/j.jpsychores.2020.109993. [DOI] [PubMed] [Google Scholar]
- Mollica R.F., Wyshak G., de Marneffe D., Khuon F., Lavelle J. Indochinese versions of the Hopkins symptom checklist-25: a screening instrument for the psychiatric care of refugees. Am. J. Psychiatry. 1987;144(4):497–500. doi: 10.1176/ajp.144.4.497. [DOI] [PubMed] [Google Scholar]
- Mollica R.W., Massagli L., Silove M.D. Massachusetts, Harvard University; Cambridge: 2004. Measuring Trauma, Measuring Torture. [Google Scholar]
- Nuttman-Shwartz O., Dekel R., Tuval-Mashiach R. Post-traumatic stress and growth following forced relocation. Br. J. Soc. Work. 2011;41(3):486–501. [Google Scholar]
- Pietrzak R.H., Goldstein M.B., Malley J.C., Rivers A.J., Johnson D.C., Morgan C.A., III, Southwick S.M. Posttraumatic growth in veterans of operations enduring freedom and Iraqi freedom. J. Affect. Disord. 2010;126(1–2):230–235. doi: 10.1016/j.jad.2010.03.021. [DOI] [PubMed] [Google Scholar]
- Powell S., Rosner R., Butollo W., Tedeschi R., Calhoun L. Posttraumatic growth after war: a study with former refugees and displaced people in Sarajevo. J. Clin. Psychol. 2003;59:71–83. doi: 10.1002/jclp.10117. [DOI] [PubMed] [Google Scholar]
- Prati G., Pietrantoni L. Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: a meta-analysis. J. Loss Trauma. 2009;14(5):364–388. [Google Scholar]
- Republic of Turkey: Ministry of Interior, and Directorate General of Migration Management. 2020. ‘General Principles of Temporary Protection’, Accessed September 7, 2020. https://en.goc.gov.tr/general-principles-of-temporary-protection.
- Rizkalla N., Segal S.P. Well-being and posttraumatic growth among Syrian refugees in Jordan. J. Trauma Stress. 2018;31(2):213–222. doi: 10.1002/jts.22281. [DOI] [PubMed] [Google Scholar]
- Rothman K.J., Greenland S., Lash T.L. Lippincott Williams & Wilkins; 2008. Modern Epidemiology. [Google Scholar]
- Ruini C., Vescovelli F., Albieri E. Post-traumatic growth in breast cancer survivors: new insights into its relationships with well-being and distress. J. Clin. Psychol. Med. Settings. 2013;20(3):383–391. doi: 10.1007/s10880-012-9340-1. [DOI] [PubMed] [Google Scholar]
- Şafak-AyvazoĞlu A., KünüroĞlu F., Van de Vijver F., YaĞmur K. Acculturation of Syrian refugees in the Netherlands: religion as social identity andboundary marker. J. Refug. Stud. 2020 [Google Scholar]
- Salo J.A., Qouta S., Punamäki R.-.L. Adult attachment, posttraumatic growth and negative emotions among former political prisoners. Anxiety Stress Coping. 2005;18(4):361–378. [Google Scholar]
- Scrignaro M., Barni S., Magrin M.E. The combined contribution of social support and coping strategies in predicting post-traumatic growth: a longitudinal study on cancer patients. Psychooncology. 2011;20(8):823–831. doi: 10.1002/pon.1782. [DOI] [PubMed] [Google Scholar]
- Semrau M., Ommeren M., Blagescu M., Griekspoor A., Howard L., Jordans M., Lempp H., Marini A., Pedersen J., Pilotte I., Slade M., Thornicroft G. The development and psychometric properties of the humanitarian emergency settings perceived needs (HESPER) scale. Am. J. Public Health. 2012;102:e55–e63. doi: 10.2105/AJPH.2012.300720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakespeare-Finch J., Lurie-Beck J. A meta-analytic clarification of the relationship between posttraumatic growth and symptoms of posttraumatic distress disorder. J. Anxiety Disord. 2014;28(2):223–229. doi: 10.1016/j.janxdis.2013.10.005. [DOI] [PubMed] [Google Scholar]
- Shamia N.A., Thabet A.A., Vostanis P. Exposure to war traumatic experiences, post-traumatic stress disorder and post-traumatic growth among nurses in Gaza. J. Psychiatr. Ment. Health Nurs. 2015;22(10):749–755. doi: 10.1111/jpm.12264. [DOI] [PubMed] [Google Scholar]
- Shand L.K., Cowlishaw S., Brooker J.E., Burney S., Ricciardelli L.A. Correlates of post-traumatic stress symptoms and growth in cancer patients: a systematic review and meta-analysis. Psychooncology. 2015;24(6):624–634. doi: 10.1002/pon.3719. [DOI] [PubMed] [Google Scholar]
- Sijbrandij M., Acarturk C., Bird M., Bryant R.A., Burchert S., Carswell K., de Jong J., Dinesen C., Dawson K.S., El Chammay R., van Ittersum L., Jordans M., Knaevelsrud C., McDaid D., Miller K., Morina N., Park A.L., Roberts B., van Son Y., Sondorp E., Pfaltz M.C., Ruttenberg L., Schick M., Schnyder U., van Ommeren M., Ventevogel P., Weissbecker I., Weitz E., Wiedemann N., Whitney C., Cuijpers P. Strengthening mental health care systems for Syrian refugees in Europe and the Middle East: integrating scalable psychological interventions in eight countries. Eur. J. Psychotraumatol. 2017;8(sup2) doi: 10.1080/20008198.2017.1388102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ssenyonga J., Owens V., Olema D. Posttraumatic growth, resilience, and posttraumatic stress disorder (PTSD) among refugees. Procedia Soc. Behav. Sci. 2013;82 [Google Scholar]
- Taku K., Cann A., Calhoun L., Tedeschi R. The factor structure of the posttraumatic growth inventory: a comparison of five models using confirmatory factor analysis. J. Trauma Stress. 2008;21:158–164. doi: 10.1002/jts.20305. [DOI] [PubMed] [Google Scholar]
- Tavakol M., Dennick R. Making sense of Cronbach's alpha. Int. J. Med. Educ. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedeschi R.G., Calhoun L.G. The posttraumatic growth inventory: measuring the positive legacy of trauma. J. Trauma Stress. 1996;9(3):455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- Teodorescu D.-.S., Siqveland J., Heir T., Hauff E., Wentzel-Larsen T., Lien L. Posttraumatic growth, depressive symptoms, posttraumatic stress symptoms, post-migration stressors and quality of life in multi-traumatized psychiatric outpatients with a refugee background in Norway. Health Qual. Life Outcomes. 2012;10:84. doi: 10.1186/1477-7525-10-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinghög P., Malm A., Arwidson C., Sigvardsdotter E., Lundin A., Saboonchi F. Prevalence of mental ill health, traumas and postmigration stress among refugees from Syria resettled in Sweden after 2011: a population-based survey. BMJ Open. 2017;7(12) doi: 10.1136/bmjopen-2017-018899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin D.F., Foa E.B. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol. Trauma Theory Res. Pract. Policy. 2008;S(1):37–85. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- UNHCR (2020). "Global trends: forced displacement in 2019."
- Veronese G., Pepe A. Using the posttraumatic growth inventory–short form with Palestinian helpers living in conflict areas. Meas. Eval. Counsel. Dev. 2019;52(3):207–221. [Google Scholar]
- Vishnevsky T., Cann A., Calhoun L.G., Tedeschi R.G., Demakis G.J. Gender differences in self-reported posttraumatic growth: a meta-analysis. Psychol. Women Q. 2010;34(1):110–120. [Google Scholar]
- Vu A., Adam A., Wirtz A., Pham K., Rubenstein L., Glass N., Beyrer C., Singh S. The prevalence of sexual violence among female refugees in complex humanitarian emergencies: a systematic review and meta-analysis. PLoS Curr. 2014;6 doi: 10.1371/currents.dis.835f10778fd80ae031aac12d3b533ca7. ecurrents.dis.835f10778fd10780ae10031aac10712d10773b10533ca10777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss T. Guilford Publications.; 2004. Correlates of Posttraumatic Growth in Married Breast Cancer Survivors. [DOI] [PubMed] [Google Scholar]
- Weiss T., Berger R. Reliability and validity of a Spanish version of the posttraumatic growth inventory. Res. Soc. Work Pract. 2006;16(2):191–199. [Google Scholar]
- Williams M., Gomez Grajales C., Kurkiewicz D. Assumptions of multiple regression: correcting two misconceptions. Pract. Assess. Res. Eval. 2013;18 [Google Scholar]
- Wilson J.T., Boden J.M. Massey University; 2008. The Effects of Personality, Social Support and Religiosity on Posttraumatic Growth. [Google Scholar]
- Zalta A.K., Gerhart J., Hall B.J., Rajan K.B., Vechiu C., Canetti D., Hobfoll S.E. Self-reported posttraumatic growth predicts greater subsequent posttraumatic stress amidst war and terrorism. Anxiety Stress Coping. 2017;30(2):176–187. doi: 10.1080/10615806.2016.1229467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoellner T., Maercker A. Posttraumatic growth in clinical psychology - a critical review and introduction of a two component model. Clin. Psychol. Rev. 2006;26(5):626–653. doi: 10.1016/j.cpr.2006.01.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.