Abstract
Ceramic bearing surfaces have gained popularity in total hip arthroplasty as a result of the favorable mechanical properties and low wear rates. Despite the recognition as an attractive articulation, problems such as ceramic head fracture persist. Smaller heads and higher body mass indices are touted as risk factors for ceramic head fracture and are often associated with antecedent trauma. We present a case report of an 83-year-old male with a body mass index of 26.7 kg/m2 who suffered a fracture of a 40-mm ceramic femoral head. This occurred atraumatically 5 years from his index surgery. This patient underwent revision total hip arthroplasty which included debridement of ceramic debris and alteration of the bearing surface with femoral head and polyethylene liner exchange.
Introduction
Contemporary bearing surfaces in total hip arthroplasty (THA) have a sound and proven performance [1]. Historically, THA component failure has been a result of wear and bearing issues leading to component loosening and compromise [2]. Longevity and survivorship of implants have ultimately been limited by bearing surface quality [3]. While there are certainly disadvantages and unique failure mechanisms across all bearing types, the use of newer generation ceramic alloy femoral heads articulating with modern highly cross-linked polyethylene liners has provided a favorable wear pattern, excellent survivorship, and low complication rates [3].
Ceramics, introduced in arthroplasty in the 1970s [4], boasted strong mechanical properties and very low wear characteristics when compared to hard-on-soft bearing options and were emphasized for younger and more active patients. Despite improved hardness, high biocompatibility, and low wear rates, earlier generations of ceramic bearings were not devoid of complications, particularly squeaking and fracture occurring at unacceptably high rates [[5], [6], [7], [8]]. Early generation ceramics had fracture rates in vivo of up to 26 per 100,00 bearings [9]. Ceramic head failures by fracture can be catastrophic making it near impossible to retrieve all minute comminutia of the fragmented head [10,11]. Newer generation ceramics (BIOLOX delta; CeramTec AG, Plochingen, Germany) have attempted to mitigate this risk with higher bending strength and increased toughness [12,13]. Specifically, fortification and optimization with zirconia, strontium oxide, and chromium oxide serve to resist crack propagation and improve hardness [12,14]. Despite these improvements, ceramic femoral head fractures can, and do, continue to occur.
This case report describes an atraumatic fracture of a ceramic femoral head articulating with a polyethylene liner 5 years from the index surgery. The intent to publish was discussed with the patient who willingly consented to this case report being documented and published.
Case history
Case 1
An 83-year-old man with a body mass index of 26.7 kg/m2 presented to our hospital for evaluation. His past medical history was significant for a primary renal cancer s/p nephrectomy in 2004. He underwent staged bilateral THAs for primary hip osteoarthritis at an outside hospital through a standard posterior approach. His left side, the side of focus in this case, was performed in 2015 with the following implants: Accolade II (Stryker Orthopedics, Inc, Allendale, NJ) varus neck with a stem size 6, 40-mm (-2.5 mm) BIOLOX delta (CeramTec, Plochingen, Germany) ceramic femoral head with a titanium sleeve seated inside a 56-mm Trident PSL acetabular cup (Stryker Orthopedics, Inc, Allendale, NJ), and a polyethylene acetabular liner (Fig. 1). The patient was noted postoperatively to have a partial palsy of the peroneal branch of his sciatic nerve with diminished sensation and weak but intact dorsiflexion strength compared with the contralateral limb. This deficit was mild but persisted and was managed conservatively without bracing. Otherwise, he recovered from his index arthroplasty uneventfully. There were no wound issues nor additional postoperative complications, other than the nerve palsy, noted by the patient and was generally considered to have had a good outcome.
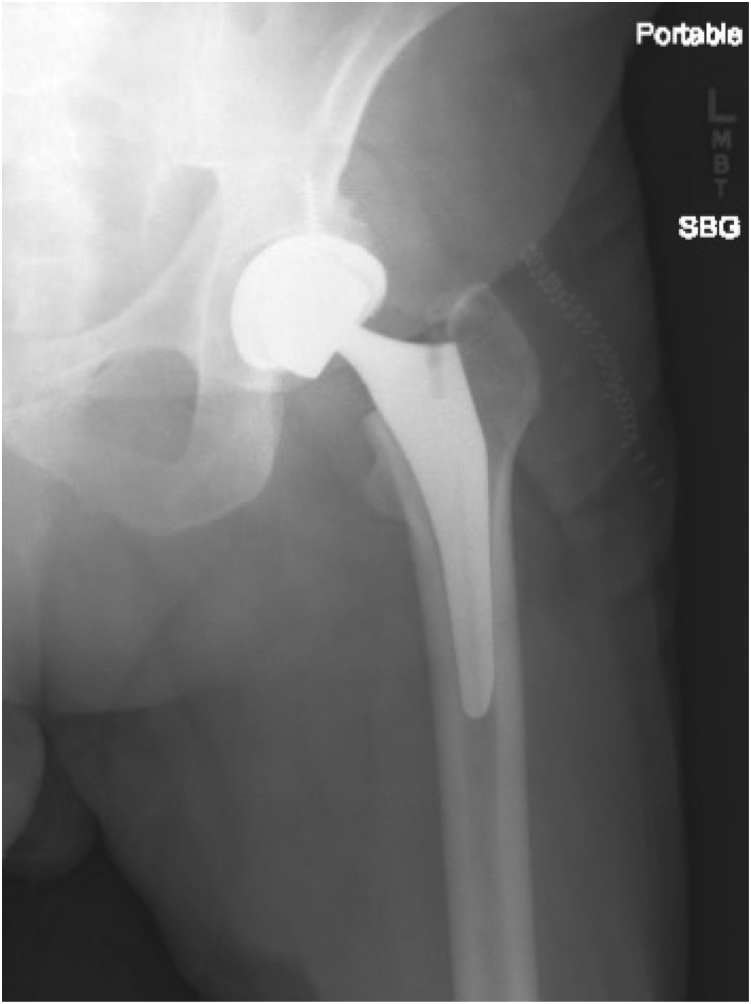
Figure 1.
Preinjury left hip radiograph showing intact femoral head and components positioned within acceptable limits.
Five years after the index surgery, the patient presented to the emergency department for orthopedic evaluation after acute-onset of atraumatic hip pain encountered during community ambulation. Radiographs of the pelvis and left hip at the time of presentation revealed fracture of the ceramic head (Fig. 2). Presenting examination of the left lower extremity revealed well-healed posterior surgical incision with active and passive motion of the hip limited by pain and notable for palpable crepitus. Sensory and motor examination revealed no deficits with the exception of the previously mentioned dorsiflexion and great toe extension weakness.
Figure 2.
Left hip radiographs taken in emergency room at the time of presentation showing comminuted ceramic femoral head fracture.
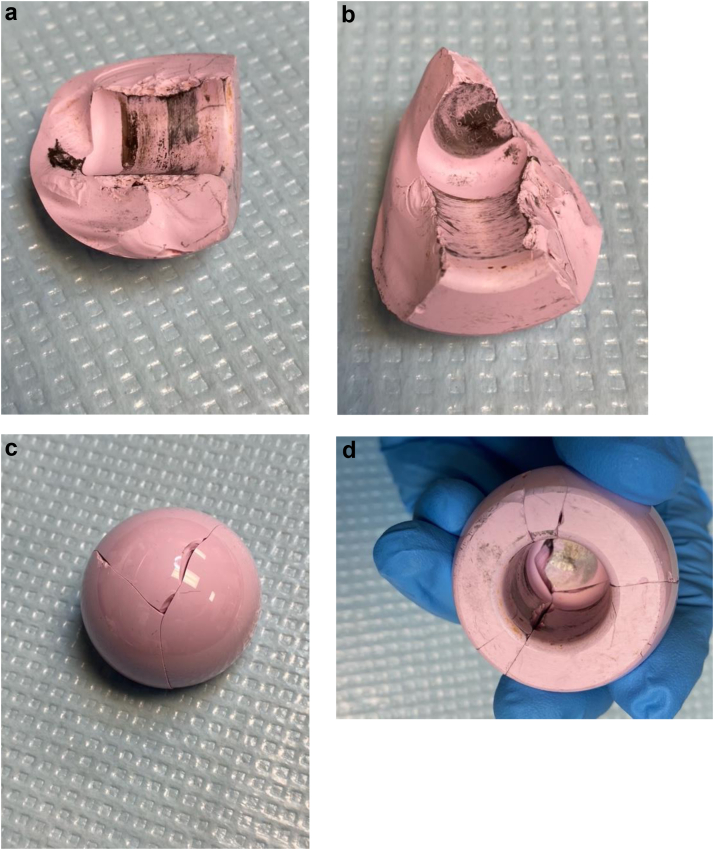
Preoperative evaluation included radiographs and computed tomography scan which showed, in addition to the previously seen ceramic comminution, the acetabular cup position appeared to have anteversion within acceptable parameters and inclination of 32 degrees. While this patient did not have ideal cup position, it was felt that component position was acceptable, and the decision was made to leave the acetabular component. He was diagnosed with a failed left THA with fracture of the ceramic femoral head. He was indicated for revision surgery and was taken to the operating room the following day. The hip was accessed through a standard posterior approach through the prior incision, and the fractured ceramic head was encountered. There were several large fragments still contained within the acetabular shell and, as expected, a number of smaller, comminuted pieces (Fig. 3a-d) all of which were removed to include a complete synovectomy. Great care was taken to remove all ceramic debris so as not to leave potential sources for third body wear. The neck was then gently dislocated from the acetabular component to visualize the femoral neck and the trunnion sleeve. It became obvious, after multiple failed attempts at disassociation, that in addition to sleeve and trunnion damage (Fig. 4), the titanium sleeve had become cold-welded to the trunnion. Removing this sleeve was crucial to replacing the head component; therefore, it was decided to remove the stem in its entirety and continue with a revision stem prosthesis. Unfortunately, initial efforts to remove the stem with standard extraction devices were unsuccessful, and the decision to proceed with an extended trochanteric osteotomy was made. During the extended trochanteric osteotomy, a portion of the greater trochanter was fractured separate from the main osteotomy fragment. While not standard practice, a trochanteric plate was placed as it was felt to better capture and secure the greater trochanter and the main osteotomy fragment. A modular splined-tapered revision stem was placed (RECLAIM Modular Revision stem; Depuy, Warsaw, IN). The osteotomy was reduced and fixed with a combination of cerclage wires and a trochanteric plate, and the final 40-mm (+1.5 mm) femoral head with a titanium sleeve was impacted into place (Fig. 5). Excellent stability was demonstrated, and the patient was awoken and taken to recovery. The patient remained in the hospital for several days and was discharged home in good condition after demonstrating safety with therapy. He was discharged to a rehab facility for several weeks before returning home. At his 5-month orthopedic follow-up, his symptoms were greatly improved as was his function. He was ambulating with a cane for long distances with good pain control. Further 8-month follow-up correspondence with his physical therapist shows continued improvement with strength and conditioning.
Figure 3.
(a-d) Clinical photographs of ceramic head fracture after explant.
Figure 4.
Clinical photograph of trunnion and sleeve after explant.
Figure 5.
Postrevision left hip radiograph showing revision components and well-reduced extended trochanteric osteotomy.
Discussion
Ceramic head fracture after THA is a feared complication which obligates revision surgery and has worse outcomes with significantly higher failure rates [10,15]. The rarity of ceramic fractures leaves us with outcomes data obtained primarily from small series and case reports. The largest survivorship study after ceramic head fracture published in 2003 was based on multicenter data collected following up 105 patients at an average of 3.5 years and showed 5-year survivorship to be only 63% [15]. Thankfully, rates of fourth-generation ceramic fracture are low. BIOLOX delta was initially promoted with a fracture risk of 0.001% to 0.021% [16]; however, these rates may have been underestimated with recent registry data published in 2017 showing an incidence of 0.1% [17]. Notably, however, these rates are based on ceramic-on-ceramic articulations, and the true rates of fracture of ceramic-on-polyethylene are likely even less [18].
This case report is the first in the literature describing a fourth-generation ceramic femoral head fracture of the 40-mm size. Prior case reports and small series have described ceramic head fracture of various sizes, ranging from 28 to 36 mm, and they are summarized in a review of the literature provided by Rankin et al. in October 2019 [14]. Larger heads are seemingly protective based on prior literature with accepted risk factors for fracture including ceramic-on-ceramic bearing surfaces (risk ratio of 6.02 compared to ceramic-on-polyethylene [19]), obesity [16], smaller head size, and short neck lengths [1].
The patient in the current case had an atraumatic history leading to presentation, and although most ceramic fractures are the result of direct trauma, there are certainly instances of delayed and atraumatic fracture postoperatively. Pomeroy et al. [20] in 2015 describes the case of a 41-year-old fit and healthy man who underwent THA with a 32-mm BIOLOX delta alumina ceramic femoral head placed on a type 1 taper on a Taperloc femoral component (Zimmer Biomet, Warsaw, IN) articulating with a polyethylene liner. A “clicking” sound was noted postoperatively but was otherwise well until an atraumatic acute onset of pain prompted a clinic visit at approximately 6 weeks postoperatively and was diagnosed with a ceramic femoral head fracture. He was revised to a ceramic-on-polyethylene articulation with stem retention. There was no suggestion of causative etiology of the ceramic head fracture. The implant was a 28-mm (-3 mm) ceramic femoral head, and he was revised to ceramic-on-polyethylene articulation. Rankin et al. [14] in 2019 described a case report and review of the literature of a 52-year-old man with a ceramic on highly cross-linked polyethylene liner who suffered an atraumatic ceramic femoral head fracture 9 months from the primary surgery. This case was unique in that a month before his presentation, he had suffered a heavy fall directly onto the greater trochanter of his operative extremity leaving him with minimal pain, no disability, and the ability to ambulate immediately.
This brings to attention the brittle materials property concept of “subcritical crack growth.” Brittle material, such as alumina ceramics, by definition have low ductility, low tensile strength, and little tendency to deform before fracture but display high compressive strength and hardness. As a result, the yield strength before fracture is very difficult to determine. The macroscopic surface integrity is only as strong as the microscopic structural links, and it is possible that subthreshold trauma may initiate these intermolecular nanocracks. Based on the “weakest link theory,” these cracks may influence the variability in strength of ceramics [21] as these fractures and defects undergo chemical reactions within the crack, cleaving oxide bonds [14] and accumulating inelastic strain within the crack until a threshold is met. This results in fracture propagation away from the largest flaw that is favorably oriented to the tensile strength to which the material is subjected [22] until the burst strength of BIOLOX delta ceramic femoral heads of 52kN is surpassed [23]. Catastrophic failure and fracture are nearly always preceded by subcritical crack growth. This delay to failure is commonly seen in ceramics subjected to a static or repetitive load [24], possibly such as ambulation on a flawed ceramic femoral head. This may explain the delayed presentation of the aforementioned studies and the case of the patient in the current report.
In addition to the atraumatic, delayed presentation of this case, ceramic head fractures are more commonly seen with hard-on-hard bearing surfaces, and while this is not the only case reported, the occurrence of hard-on-soft ceramic femoral head fractures is certainly unusual with only a few instances of ceramic-on-polyethylene fracture in the literature [14,20,25,26]. Slow crack progression and delayed presentation may be more pronounced in individuals with polyethylene bearing surfaces than in those with a hard bearing surface because polyethylene exhibits a protective shock absorption for the femoral head and increase surface area contact [25]. Despite the mild protective capacity, fractures still occur. One of the proposed mechanisms is related to malseating of the ceramic head on the trunnion. The trunnion condition at the time of head impaction may be of underappreciated importance. Debris introduced between the head and trunnion may alter hoop stresses during impaction and activity with overall poor congruence [27]. Interposed fluid, fat, or debris at this junction negatively affects pull-off strength, introduces micromotion of the head on the trunnion, and potentiates fretting [28]. This may have been relevant to this patient’s clinical course. Although speculative, the relatively flat acetabular component and large head in the primary setting may suggest poor visualization or instability. This may have affected the ability to evaluate the trunnion which could have led to the introduction of debris.
Several factors may have impacted the current patient’s clinical course. There was no reported antecedent trauma; however, the amount of force and degree of external trauma required to damage a ceramic femoral head is unknown, and the patient may have experienced a seemingly insignificant trauma not reported, enough to cause irreparable damage through subcritical crack propagation. In addition, the stem from the index surgery uses a titanium alloy (Ti-6Al-4V) with a higher Young’s Modulus of elasticity than prior, softer iterations of titanium alloys, and although a standard alloy is used in contemporary stems, this increased stiffness coupled with other factors may have impacted the force-transfer to the ceramic head. The most likely causative etiology, however, is a combination of issues centered around component malpositioning leading to this unfortunate and rare complication. The intraoperative assessment of the components suggested severe damage to the titanium sleeve allowing for cold-welding of the sleeve to the trunnion as well as a significant amount of damage to the neck distal to the trunnion suggestive of impingement on a relatively flat cup. The decision to use a 40-mm head in a 56-mm cup, while not unheard of, is an unusual combination which may suggest intraoperative instability or impingement. True occurrences of cold-welded components happen infrequently and suggest malalignment during impaction of the head, which may indicate inadequate visualization and exposure which also predispose to debris interposition between the trunnion and the head. While impossible to determine the exact mechanism of failure, this case brings to light potentially modifiable variables to prevent further occurrences of these unfortunate events.
Summary
Although increasingly rare, fractures of newer generation ceramic femoral heads continue to occur. Surgeons should be cognizant of risk factors for fracture and the possibility of delayed presentation of fracture and appropriate workup and revision options. Mitigation of risk at the time of index surgery may include a complete understanding of acceptable stem-head compatibility, thorough cleaning ensuring a pristine trunnion on which the ceramic may be placed, avoiding malseating of components, and importantly, appropriate component positioning.
Conflicts of interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: M. Bolognsi declares receiving royalties from Zimmer Biomet and TJO; being in the speakers' bureau of Johnson and Johnson; having stock or stock options in Joint Development; receiving research support from Zimmer Biomet, DePuy Synthes, Stryker, and Exactech; being in the editorial or governing board of JOA and Arthroplasty Today; being a board member of AAHKS and EOA.
Informed patient consent
The authors declare that informed patient consent was taken from all the patients.
Appendix A. Supplementary data
References
- 1.Lachiewicz P.F., Kleeman L.T., Seyler T. Bearing surfaces for total hip arthroplasty. J Am Acad Orthop Surg. 2018;26(2):45. doi: 10.5435/JAAOS-D-15-00754. [DOI] [PubMed] [Google Scholar]
- 2.Lee J.H. Midterm results of primary total hip arthroplasty using highly cross-linked polyethylene: minimum 7-year follow-up study. J Arthroplasty. 2011;26(7):1014. doi: 10.1016/j.arth.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 3.Davis E.T., Pagkalos J., Kopjar B. Effect of bearing surface on survival of cementless and hybrid total hip arthroplasty: study of data in the national joint registry for England, Wales, Northern Ireland and the Isle of Man. JB JS Open Access. 2020;5(2):e0075. doi: 10.2106/JBJS.OA.19.00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boutin P. Total arthroplasty of the hip by fritted alumina prosthesis. Experimental study and 1st clinical applications. Orthop Traumatol Surg Res. 2014;100(1):15. doi: 10.1016/j.otsr.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Baek S.H., Kim S.Y. Cementless total hip arthroplasty with alumina bearings in patients younger than fifty with femoral head osteonecrosis. J Bone Joint Surg Am. 2008;90(6):1314. doi: 10.2106/JBJS.G.00755. [DOI] [PubMed] [Google Scholar]
- 6.Ha Y.C. Ceramic liner fracture after cementless alumina-on-alumina total hip arthroplasty. Clin Orthop Relat Res. 2007;458:106. doi: 10.1097/BLO.0b013e3180303e87. [DOI] [PubMed] [Google Scholar]
- 7.Jarrett C.A. The squeaking hip: a phenomenon of ceramic-on-ceramic total hip arthroplasty. J Bone Joint Surg Am. 2009;91(6):1344. doi: 10.2106/JBJS.F.00970. [DOI] [PubMed] [Google Scholar]
- 8.Koo K.H. Isolated fracture of the ceramic head after third-generation alumina-on-alumina total hip arthroplasty. J Bone Joint Surg Am. 2008;90(2):329. doi: 10.2106/JBJS.F.01489. [DOI] [PubMed] [Google Scholar]
- 9.Campbell P., Shen F.W., McKellop H. Biologic and tribologic considerations of alternative bearing surfaces. Clin Orthop Relat Res. 2004;(418):98. doi: 10.1097/00003086-200401000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Traina F. Revision of ceramic hip replacements for fracture of a ceramic component: AAOS exhibit selection. J Bone Joint Surg Am. 2011;93(24):e147. doi: 10.2106/JBJS.K.00589. [DOI] [PubMed] [Google Scholar]
- 11.Whittingham-Jones P. Fracture of a ceramic component in total hip replacement. J Bone Joint Surg Br. 2012;94(4):570. doi: 10.1302/0301-620X.94B4.28013. [DOI] [PubMed] [Google Scholar]
- 12.Hamilton W.G. THA with Delta ceramic on ceramic: results of a multicenter investigational device exemption trial. Clin Orthop Relat Res. 2010;468(2):358. doi: 10.1007/s11999-009-1091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeffers J.R., Walter W.L. Ceramic-on-ceramic bearings in hip arthroplasty: state of the art and the future. J Bone Joint Surg Br. 2012;94(6):735. doi: 10.1302/0301-620X.94B6.28801. [DOI] [PubMed] [Google Scholar]
- 14.Rankin C.S. Fracture of a BIOLOX delta ceramic femoral head: a case report and update of the literature. JBJS Case Connect. 2019;9(4):e0336. doi: 10.2106/JBJS.CC.18.00336. [DOI] [PubMed] [Google Scholar]
- 15.Allain J. Revision total hip arthroplasty performed after fracture of a ceramic femoral head. A multicenter survivorship study. J Bone Joint Surg Am. 2003;85(5):825. doi: 10.2106/00004623-200305000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Sentuerk U., von Roth P., Perka C. Ceramic on ceramic arthroplasty of the hip: new materials confirm appropriate use in young patients. Bone Joint J. 2016;98-B(1 Suppl A):14. doi: 10.1302/0301-620X.98B1.36347. [DOI] [PubMed] [Google Scholar]
- 17.Howard D.P. Ceramic-on-ceramic bearing fractures in total hip arthroplasty: an analysis of data from the National Joint Registry. Bone Joint J. 2017;99-B(8):1012. doi: 10.1302/0301-620X.99B8.BJJ-2017-0019.R1. [DOI] [PubMed] [Google Scholar]
- 18.Nho J.H. Ceramic head fracture in ceramic-on-polyethylene total hip arthroplasty. Yonsei Med J. 2013;54(6):1550. doi: 10.3349/ymj.2013.54.6.1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Si H.B. Is a ceramic-on-ceramic bearing really superior to ceramic-on-polyethylene for primary total hip arthroplasty? A systematic review and meta-analysis of randomised controlled trials. Hip Int. 2015;25(3):191. doi: 10.5301/hipint.5000223. [DOI] [PubMed] [Google Scholar]
- 20.Pomeroy E., Rowan F., Masterson E. Atraumatic fracture of a BIOLOX delta ceramic femoral head articulating with a polyethylene liner: a case report. JBJS Case Connect. 2015;5(4):e112. doi: 10.2106/JBJS.CC.O.00146. [DOI] [PubMed] [Google Scholar]
- 21.Le J.L., Bažant Z.P., Bazant M.Z. Subcritical crack growth law and its consequences for lifetime statistics and size effect of quasibrittle structures. J Phys D Appl Phys. 2009;42 [Google Scholar]
- 22.Gonzaga C.C. Slow crack growth and reliability of dental ceramics. Dent Mater. 2011;27(4):394. doi: 10.1016/j.dental.2010.10.025. [DOI] [PubMed] [Google Scholar]
- 23.Tateiwa T. Burst strength of BIOLOX((R))delta femoral heads and its dependence on low-temperature environmental degradation. Materials (Basel) 2020;13(2) doi: 10.3390/ma13020350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wiederhorn S.M. National Institute of Standards and Technology; 2017. Subcritical crack growth in brittle materials: mechanics.https://www.nist.gov/publications/subcritical-crack-growth-brittle-materials-mechanics [Google Scholar]
- 25.Heiner A.D., Mahoney C.R. Fracture of a BIOLOX delta ceramic femoral head articulating against a polyethylene liner: a case report. JBJS Case Connect. 2014;4(4):e97. doi: 10.2106/JBJS.CC.N.00040. [DOI] [PubMed] [Google Scholar]
- 26.Tucker D., Acharya M. Unusual prosthetic femoral head fracture in total hip arthroplasty: ceramic on polyethylene articulation. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2013-202685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Waddell J., Resnick L. Ceramic-on-Poly femoral head fractures: what's going on? JBJS Case Connect. 2015;5(4):e111. doi: 10.2106/JBJS.CC.15.00248. [DOI] [PubMed] [Google Scholar]
- 28.Weiser M.C., Lavernia C.J. Trunnionosis in total hip arthroplasty. J Bone Joint Surg Am. 2017;99(17):1489. doi: 10.2106/JBJS.17.00345. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.