Abstract
Observational studies suggest alcohol use promotes the development of some adverse cardiometabolic traits but protects against others including outcomes related to coronary artery disease. We used Mendelian randomization (MR) to explore causal relationships between the degree of alcohol consumption and several cardiometabolic traits in the UK Biobank. Using the well-established ADH1B Arg47His variant (rs1229984) and up to 24 additional SNPs recently found to be associated with alcohol consumption in an independent dataset as instruments, we conducted two-stage least squares and inverse weighted variance MR analyses, both as one-sample analyses in the UK Biobank and as two-sample analyses in external consortia. In the UK Biobank inverse variance weighted analyses, we found that one additional drink of alcohol per day was positively associated with systolic blood pressure (beta = 2.65 mmHg [1.40, 3.89]), hemorrhagic stroke (OR = 2.25 [1.41, 3.60]), and atrial fibrillation (OR = 1.26 [1.07, 1.48]), which were replicated in multivariable analyses. Alcohol was also associated with all cardiovascular disease and all-cause death. A positive association with myocardial infarction did not replicate in multivariable analysis, with suggestive mediation through blood pressure; similarly, a positive association between alcohol use with type 2 diabetes was mitigated by BMI in multivariable analysis. Findings were generally null in replication with two-sample analyses. Alcohol was not protective for any disease outcome with any analysis method, dataset, or strata. Stratifications by sex and smoking in the UK Biobank revealed higher point estimates of risk for several outcomes for men and mixed results for smoking strata, but no statistically significant heterogeneity. Our results are consistent with an overall harmful and/or null effect of alcohol on cardiometabolic health at all levels of use and suggest that even moderate alcohol use should not be promoted as a part of a healthy diet and lifestyle.
Introduction
The relationship between alcohol and cardiovascular disease is important to understand given the high prevalence of alcohol consumption [1, 2]. In decades of epidemiological work, alcohol consumption has shown an inverse or J-shape association with multiple traits related to cardiometabolic health including Type 2 diabetes [3, 4], non-fatal and fatal coronary heart disease [5–7], ischemic stroke [8–10], atrial-fibrillation [11], and congestive heart failure [12].
One interpretation of these relationships has been that moderate drinking is beneficial to cardiometabolic health. A problem with this interpretation is that the relationship is inconsistent with that observed for some known risk factors; for example, alcohol has been directly associated with outcomes such as hypertension irrespective of the degree of intake [13]. A long-standing hypothesis to reconcile these observations stipulates that the negative effects on blood pressure are modest and are surpassed by the positive effects on HDL levels [14, 15] that are either directly affected by alcohol and/or a consequence of an improvement in insulin sensitivity [16]. However, this hypothesis has been challenged in the last decade by multiple randomized control trials of HDL-raising drugs, as well as Mendelian randomization studies that have failed to demonstrate the benefits on risk of cardiovascular disease (CVD) of pharmacologically or genetically raised HDL [17–19].
The extent to which observational studies can shed light on the relationship between alcohol and CVD is questionable due to confounding and reverse causality [20]. Alcohol use is related to cultural, socioeconomic, and lifestyle factors which cannot be fully accounted for in observational analyses. Furthermore, several studies have suggested substantial differences in the effects of alcohol on cardiometabolic traits between men and women [3, 4, 11, 12, 16, 21]. Mendelian randomization (MR) facilitates a comparison of groups of subjects that consume more vs. less alcohol that is free of confounding, allowing us to better understand the causal effect of consumption. In this study, we determine the causal relationship between alcohol and cardiovascular risk factors and disease in the UK Biobank by performing an instrumental variable analysis using a genetic variant in a gene (ADH1B) that is known to be responsible for the metabolism of alcohol and associated with the amount of alcohol consumed. We attempt to validate findings using summary statistics from external consortial studies for related phenotypes. Within the UK Biobank, we also take advantage of the large numbers to explore strength of associations stratified by sex and smoking status.
Methods
Study cohort
The UK Biobank is a prospective study of over 500,000 participants recruited in 2006–2010 [22]. Data collected from the participants included questionnaires, physical measures, sample assays, genotyping, and ongoing longitudinal hospital records. Participants were enrolled at age 40–69. This research has been conducted using the UK Biobank Resource under Application Number 13721. The Research Ethics Committee reference for UK Biobank is 16/NW/0274. The Stanford IRB reviewed the protocol and determined the research did not include human subjects as defined in 45 CFR 46, nor 21 CFR 56.
Outcomes and quantitative traits
We extracted systolic and diastolic blood pressure, BMI, waist circumference, and body fat percentage from survey data which included physical measurement at the baseline clinic visit. We obtained lipids, blood count variables, and HbA1C from the biomarkers data. We extracted primary and secondary diagnosis disease outcomes from hospital data for myocardial infarction, stroke (hemorrhagic, ischemic, and any stroke), heart failure, atrial fibrillation, and a composite outcome of all cardiovascular events combined, as well as death from each of these disease outcomes according to the relevant ICD codes (Table A in S1 Text). We derived type 2 diabetes status from a combination of diabetes-related questions and self-reported medications (S1 Text).
Main exposure and covariates
Our main exposure variable of interest was self-reported alcohol use by number of drinks per week or month and type of drink obtained from the survey data. Use of all types of alcohol was aggregated into total grams of alcohol intake per year [23], which was then transformed into equivalent daily glasses of wine (0, >0–1, >1–2, >2–3, and >3) to facilitate interpretability. Covariates also from survey data included sex, age, region of recruitment, socioeconomic status, ethnicity, smoking status, blood pressure medications, cholesterol-lowering medications, insulin and other diabetes drugs, and fasting status (for biomarkers) (S2 Text).
We used two instrumental variables (IV) for our MR analyses of alcohol use. First, we used the ADH1B Arg47His variant (rs1229984) in isolation. This variant is arguably the strongest and most established genetic predictor of self-reported alcohol use in European populations with a frequency of about 0.5% (Northern Europe) to 4% (Southern Europe) [24, 25]. The variant was directly genotyped using the UK Biobank array and thus no imputation of this variant was necessary. Second, we used a set of up to 25 variants including rs1229984 that had previously been associated with alcohol use and alcohol use disorder in Million Veterans Program; thus, discovery of the instruments used was entirely independent of the UK Biobank (Table A in S3 Text).
Statistical analysis
We characterized the observational relationship between alcohol use and continuous variable risk factors using linear regression for quantitative traits, logistic regression for type 2 diabetes, and Cox proportional hazards regression for cardiovascular events or death. The reference group for all observational analyses was current non-drinkers. For our Cox analyses, we defined the start of follow up as time of enrollment into the UK Biobank study and excluded those with a cardiovascular event prior to the questionnaire to minimize survivor bias. We created two models for each outcome in our observational analysis, one model minimally adjusted for typical epidemiologic covariates (sex, age, region of recruitment as a proxy for locality, socioeconomic status, ethnicity, and smoking status; for biomarker outcomes, fasting status was also included) and one model additionally adjusted for heart disease risk factors as well as medications that affect those risk factors (BMI and waist circumference, in all models other than those for anthropometric measures; SBP and DBP, in all models other than those for blood pressure; HbA1C and diabetic medications, in models other than for type 2 diabetes; LDL, HDL, and triglycerides, in all models other than those for lipids; and lipid-lowering, or anti-hypertensive medications) (Table A in S2 Text).
We included all non-related individuals of European descent (for sample independence and to avoid population stratification) in the UK Biobank for our MR analyses. We collapsed heterozygous and homozygous carriers of rs1229984 into one group (dominant model), quantified the strength of the instrumental variable using ANOVA, and tested the relationship between the instrument variable and alcohol consumption using linear regression. We performed a one-sample MR with individual level UK Biobank data to estimate the causal effect on traits of consuming one additional drink per day on average. We used both (1) the two-stage least squares (2SLS) method with the single SNP IV and (2) the inverse variance weighted (IVW) method with the 25 SNP IV. Given possible differences in drinking patterns by sex and smoking status, we also conducted stratified analyses in male, female, current smoker, and never smoker subgroups. We used the Cochran’s Q test for heterogeneity of odds ratios to test whether outcomes varying substantially between strata were significantly different [26]. We also performed a multivariable MR (MVMR) analysis for event outcomes with any positive findings. This analysis tested the third assumption of MR (specifically, whether alcohol’s effect on these outcomes was independent of possible upstream effect or via another path) using a priori related factors. Lastly, we conducted an analysis of hemoglobin, hematocrit, and mean corpuscular volume levels by instrument variable status as an additional check on the potential confounding effects of anemia for our association analyses involving HbA1C.
For replication in other datasets, we collected summary statistics for the largest available study of European or mostly European ancestry for each outcome and IV (S1 Table) [27–44]. We used these summary statistics for a two-sample MR, calculating the ratio of each summary statistic coefficient to the exposure-IV coefficient from the UK Biobank. We also used the multiple SNP IV for a two-sample IVW analysis using GWAS summary statistics.
Association analyses were performed using plink 2.0, and other analyses were conducted in R 3.6.3 including the MendelianRandomization package.
Results
UK Biobank participant characteristics are described in Tables 1 and S2. At recruitment, 92% of participants consumed alcohol. About half of participants reported drinking alcohol 1–4 times per week, and an additional one fifth of participants reported drinking daily. On average, participants reported drinking 7.7 (± 9.4) glasses per week.
Table 1. Summary of characteristics of UK Biobank participants by analysis dataset.
| Variable | Total dataset | Observational analysis | Mendelian randomization |
|---|---|---|---|
| n | 502536 | 481150 | 337484 |
| Age (years) | 67.3 (8.1) | 67 (8.1) | 67.6 (8) |
| Townsend index | -1.3 (3.1) | -1.3 (3.1) | -1.6 (2.9) |
| Sex | |||
| Female | 273402 (54.4) | 267459 (55.6) | 181236 (53.7) |
| Male | 229134 (45.6) | 213691 (44.4) | 156248 (46.3) |
| Region | |||
| England | 445883 (88.7) | 427194 (88.8) | 297645 (88.2) |
| Wales | 20808 (4.1) | 19936 (4.1) | 14824 (4.4) |
| Scotland | 35845 (7.1) | 34020 (7.1) | 25015 (7.4) |
| Ethnic group | |||
| White | 472725 (94.1) | 452534 (94.1) | 337484 (100) |
| Asian or Asian British | 11456 (2.3) | 10847 (2.3) | 0 (0) |
| Black or Black British | 8061 (1.6) | 7863 (1.6) | 0 (0) |
| Mixed or other | 7517 (1.5) | 7279 (1.5) | 0 (0) |
| Don’t know/refused | 2777 (0.6) | 2627 (0.5) | 0 (0) |
| Smoking status | |||
| Never-smoker | 273537 (54.4) | 265259 (55.1) | 183826 (54.5) |
| Current smoker | 52979 (10.5) | 50453 (10.5) | 33977 (10.1) |
| Former smoker | 173070 (34.4) | 162687 (33.8) | 118505 (35.1) |
| No response | 2950 (0.6) | 2751 (0.6) | 1176 (0.3) |
| Drinking status | |||
| Never-drinker | 22388 (4.5) | 21234 (4.4) | 10392 (3.1) |
| Current drinker | 460386 (91.6) | 441728 (91.8) | 315257 (93.4) |
| Former drinker | 18108 (3.6) | 16631 (3.5) | 11543 (3.4) |
| No response | 1654 (0.3) | 1557 (0.3) | 292 (0.1) |
| Drinking frequency | |||
| Daily or almost daily | 101774 (20.3) | 97438 (20.3) | 72270 (21.4) |
| Three or four times a week | 115445 (23) | 111123 (23.1) | 81462 (24.1) |
| Once or twice a week | 129297 (25.7) | 124157 (25.8) | 88747 (26.3) |
| One to three times a month | 55858 (11.1) | 53724 (11.2) | 37367 (11.1) |
| Special occasions only | 58012 (11.5) | 55286 (11.5) | 35411 (10.5) |
| Never | 40648 (8.1) | 38009 (7.9) | 21991 (6.5) |
| No response | 1502 (0.3) | 1413 (0.3) | 236 (0.1) |
| Alcohol (weekly equivalent glasses of wine) | 7.7 (9.4) | 7.7 (9.4) | 8.1 (9.5) |
| Systolic blood pressure (mmHg) | 139.7 (19.7) | 139.7 (19.7) | 140.2 (19.7) |
| Diastolic blood pressure (mmHg) | 82.2 (10.7) | 82.3 (10.7) | 82.2 (10.7) |
| Body mass index (kg/m^2) | 27.4 (4.8) | 27.4 (4.8) | 27.4 (4.7) |
| Waist circumference (cm) | 90.3 (13.5) | 90 (13.4) | 90.3 (13.5) |
| Body fat percentage | 31.5 (8.5) | 31.5 (8.6) | 31.4 (8.5) |
| Cholesterol (mmol/L) | 5.7 (1.1) | 5.7 (1.1) | 5.7 (1.1) |
| LDL (mmol/L) | 3.6 (0.9) | 3.6 (0.9) | 3.6 (0.9) |
| HDL (mmol/L) | 1.4 (0.4) | 1.5 (0.4) | 1.5 (0.4) |
| Triglycerides (mmol/L) | 1.7 (1) | 1.7 (1) | 1.8 (1) |
| HbA1c (mmol/mol) | 36.1 (6.8) | 36 (6.5) | 36 (6.5) |
| Glucose (mmol/L) | 5.1 (1.2) | 5.1 (1.2) | 5.1 (1.2) |
| Type 2 diabetes | 25217 (5) | 22083 (4.6) | 15493 (4.6) |
| Coronary heart disease | 24047 (4.8) | 11297 (2.3) | 16102 (4.8) |
| All stroke | 11785 (2.3) | 6857 (1.4) | 8044 (2.4) |
| Ischemic stroke | 5081 (1) | 3217 (0.7) | 3427 (1) |
| Hemorrhagic stroke | 2814 (0.6) | 1608 (0.3) | 1877 (0.6) |
| Heart failure | 8956 (1.8) | 5128 (1.1) | 5921 (1.8) |
| Atrial fibrillation | 22197 (4.4) | 14292 (3) | 15483 (4.6) |
| Any cardiovascular disease | 52219 (10.4) | 30833 (6.4) | 35499 (10.5) |
| All-cause death | 20284 (4) | 17635 (3.7) | 13700 (4.1) |
| ADH1B status | |||
| Wildtype | 458807 (91.3) | 439084 (91.3) | 322519 (95.6) |
| Carrier | 26534 (5.3) | 25593 (5.3) | 14777 (4.4) |
| Homozygous minor allele | 1979 (0.4) | 1928 (0.4) | 188 (0.1) |
N (%) for categorical variable traits or mean (standard deviation) for quantitative variable traits (in listed units)
Exclusion of those with prior CVD (n = 21,386) yielded a dataset of 481,150 (Table 1). For our observational analysis (S1, S2 Figs, Tables A-F in S4 Text), increased alcohol use was directly related to higher systolic and diastolic blood pressure, total cholesterol, HDL, and atrial fibrillation in the fully adjusted model. We observed a J-shape association (compared with no drinking, equal or lower coefficient/odds ratio/hazard ratio with moderate drinking, but higher with heavy drinking) with BMI, waist circumference, body fat percentage, LDL, stroke (total, ischemic, and hemorrhagic), and all-cause death. Triglycerides, type 2 diabetes, myocardial infarction, heart failure and total cardiovascular disease also had a J-shape association, but with lower betas/odds ratio/hazard ratio at all drinking levels compared with non-drinkers. Alcohol was inversely associated with HbA1C.
The Arg47His ADH1B variant was found in 4.4% of individuals in the UK Biobank, with only 188 subjects found to be homozygous for the variant. Our MR analysis (n = 337,484) showed that carriers of the wildtype consumed 2.1 drinks/week more than carriers of the Arg47His variant in ADH1B (7,127 g/year or 8.2 glasses/week for wildtype vs 5,276 g/year or 6.1 glasses/week for carriers; F = 718) (Tables 2 and S2). All 25 SNPs of the second instrumental variable investigated were found in the UK Biobank, while only 9 to 10 SNPs were present in the external datasets ICBP, both GIANT GWAS, body fat percentage GWAS, MAGIC, and GLGC. The remaining external datasets included nearly all of the IV SNPs (Figs 1A–1C, Tables A-C in S5 Text).
Table 2. Alcohol consumption in equivalent glasses of wine per week by group and ADH1B status.
| Group | Wildtype, mean (SD) glasses/week | Variant, mean (SD) glasses/week | Increase for wildtype, glasses/week |
|---|---|---|---|
| all | 8.2 (9.5) | 6.1 (7.6) | 2.1 |
| male | 11.2 (11.3) | 8.4 (8.8) | 2.8 |
| female | 5.5 (6.7) | 3.9 (5.4) | 1.6 |
| current smoker | 11.1 (13.4) | 7.6 (9.9) | 3.5 |
| never-smoker | 6.5 (7.8) | 4.6 (6.1) | 1.9 |
Mean (standard deviation) per category. p value for difference between wildtype and variant was < 2 x 10−16 for all rows.
Fig 1. Results from Mendelian randomization (MR) of outcome variables in UK Biobank and external datasets.
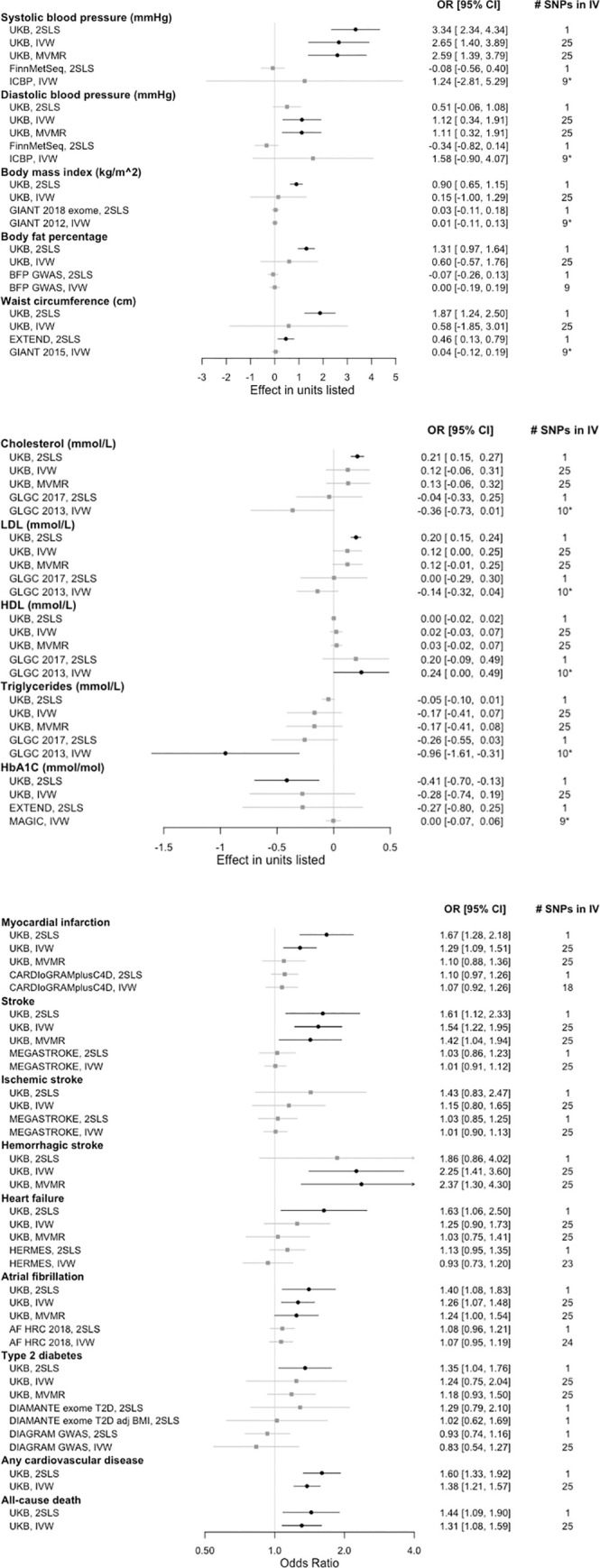
MR results for blood pressure and anthropometric measures (a), lipid and glycemic biomarkers (b), as well as disease outcomes and death (c). Mendelian randomization analysis outcomes for two-stage least squares (2SLS), inverse variance weighted (IVW), and multivariate Mendelian randomization (MVMR) methods in the UK Biobank (UKB) or external datasets. Beta or odds ratio (OR) [95% confidence interval (CI)] for one additional drink/day as instrumented by rs1229984 or by the indicated number of SNPs present from the 25 SNP instrumental variable (IV) set. Significant results shown in black with circles; non-significant results shown in gray with squares. * = the strongest SNP, rs1229984, was not available in the listed dataset. Sample sizes: FinnMetSeq 19,291; GIANT (2018) 449,889; GIANT (2012) 133,154; BFP GWAS 100,716; EXTEND 7,159; GIANT (2015) 232,101; GLGC (2017) 300,000; GLGC (2013) 188,577; MAGIC 123,665. Case numbers: CARDIOGRAMplusC4D 60,801; MEGASTROKE 67,162 (all stroke) and 60,341 (ischemic stroke); HERMES 47,309; AF HRC 65,446; DIAMANTE 48,286; DIAGRAM 26,676.
Systolic blood pressure was elevated for UK Biobank analyses with both IVs, including in MVMR analyses adjusted for BMI, but this finding was not replicated in FinnMetSeq and was not statistically significant in ICBP (Fig 1A, Tables A and D in S5 Text). BMI showed an increase due to drinking per the UK Biobank 2SLS analysis but null results otherwise. Body fat percentage showed a positive association with the UK Biobank 2SLS analysis only. Waist circumference was increased with alcohol use per both UK Biobank and external 2SLS tests, but not with either IVW analysis.
Total cholesterol and LDL showed a positive association with alcohol via the UK Biobank 2SLS analysis, but these were null for further tests, including in multivariable analysis (Fig 1B, Tables B and D in S5 Text). There was a positive association between HDL and alcohol in the GLGC IVW analyses, but all HDL associations in the UK Biobank were not significant, including the MVMR analysis. Triglycerides showed a negative point estimate with alcohol for all analyses, a result that was significant only for the GLGC IVW analysis. HbA1C also had negative point estimates for the relationship with alcohol for all analyses, though all except the UK Biobank 2SLS were null.
Myocardial infarction was positively related to alcohol in the UK Biobank 2SLS and IVW analyses, but this association did not hold in the MVMR analysis in which blood pressure approached significance, nor was it replicated in CARDIOGRAMplusC4D (Fig 1C, Tables C and E in S5 Text). All stroke was positively associated with alcohol in all UK Biobank analyses including the MVMR, but null in MEGASTROKE. While ischemic stroke analyses were all null, hemorrhagic stroke was positively associated with alcohol use in UK Biobank IVW and MVMR analyses. Heart failure was positively associated with alcohol use in the initial UK Biobank analysis, but associations were null thereafter. Atrial fibrillation showed a positive association with alcohol in all UK Biobank analyses including the MVMR, but two-sample MR associations were null. Type 2 diabetes showed a positive association with alcohol in the UK Biobank 2SLS analysis, but this association disappeared in the MVMR where BMI was the significant factor. The DIAMANTE exome 2SLS result was also attenuated when adjusted for BMI. Type 2 diabetes associations in DIAGRAM were null. Alcohol use was positively associated with any cardiovascular disease and all-cause death.
Drinking varied by sex (men: 11.1 glasses/week vs. women: 5.4 glasses/week) and by smoking status (current smokers: 9.8 glasses/week vs. never-smokers: 6.5 glasses/week) in stratified analyses (Table 2, p<2e-16 for all). All strata showed an increase in systolic blood pressure with alcohol use for both MR methods. Anthropometric measurements, total cholesterol, and LDL were also elevated in all strata in the 2SLS analysis, but these results were not universally found in the IVW analysis. For the disease outcomes, women had no increased risk with alcohol use, while men had an increased risk of myocardial infarction, stroke, atrial fibrillation, any cardiovascular disease, and death in both MR analyses. However, the p-values for heterogeneity showed no difference by sex. Never smokers had higher odds ratios and more statistically significant results than current smokers for nearly all disease outcomes, but P-values for heterogeneity showed no consistent difference by smoking strata except for a borderline case for HDL. None of the disease outcomes had a protective effect from alcohol for any strata (Tables F-I in S5 Text).
Analysis of blood count data by rs1229984 carrier status showed that those with the wildtype, who drink more, had a lower hemoglobin (-0.02 g/dL, p = 0.0018) and hematocrit (-0.09%, p = 0.0024), and a higher mean corpuscular volume (+0.27 fL, p = 2.4 x 10−13) (Table J in S5 Text).
Discussion
Our principal analyses within the UK Biobank suggest that alcohol use is positively associated with blood pressure, hemorrhagic stroke, atrial fibrillation, any cardiovascular disease, and all-cause death. The association between alcohol and myocardial infarction appears to be driven by other factors such as blood pressure, and the association between alcohol and type 2 diabetes appears to be driven by BMI. In summary statistics from external datasets, alcohol was predictive only of increased waist circumference (EXTEND), increased HDL (GLGC), and decreased triglycerides (GLGC), with other associations null. Associations between alcohol and anthropometric measures, total cholesterol, LDL, ischemic stroke, and heart failure were null or inconsistent between UK Biobank and external datasets. Our MR findings that alcohol is associated directly with blood pressure and atrial fibrillation were also supported by observational analyses. Our MR analyses gave discrepant results when compared to the analogous observational analysis for other phenotypes, which suggests the presence of residual confounding from unmeasured factors in observational analysis and counters the hypothesis of a protective effect of alcohol.
Two findings in our analyses are inconsistent with the hypothesis of a causal negative effect on cardiometabolic outcomes mediated through risk factors. First, we found alcohol to be causally associated with a lower level of triglycerides in GLGC, as well as a negatively trending association in the UK Biobank, which would be expected to reduce the risk of atherosclerosis related outcomes. We note this finding is contrary to what has been observed experimentally [45] but consistent with other MR studies [46–48]. Although multiple MR studies suggest triglycerides are causally associated with CVD, clinical trials of triglyceride-lowering agents have not consistently supported this relationship, leading to the conclusion that how triglycerides are lowered plays an important role in whether that lowering translates to cardiovascular benefit. Second, we found alcohol to be inversely associated with HbA1C in our observational and 2SLS MR analyses in the UK Biobank and trending towards an inverse association in the IVW analysis as well, which would be expected to reduce the risk of Type 2 diabetes. We suspect this counterintuitive set of associations related to glycemia may be a technical artifact driven by the presence of a mild (possibly nutritional) macrocytosis we observed among participants not carrying the minor allele at rs1229984 that biases HgA1C levels downwards without truly altering the risk of diabetes [49, 50].
Our stratified analyses found statistically significant MR associations among men for nearly all disease outcomes. Associations were less strong and often not significant for women but directionally consistent. Tests for heterogeneity showed no statistically significant difference between sex stratified results. Wider confidence intervals for women could simply be due to a smaller proportion of cases in women for cardiovascular diseases. Larger samples sizes are needed to more reliably document a statistically significant modification of effect of alcohol between men and women. If confirmed, these findings would suggest that causal negative effects of alcohol may only begin to express themselves at a higher consumption level despite differences in body surface area and rate of metabolism between females and males. We also observed significant results for a positive association between several disease outcomes and alcohol in never smokers, but not in current smokers. Tests for heterogeneity between smoking strata showed no statistically significant difference, and our results may simply be due to wider confidence intervals from a smaller group of current smokers.
Our findings are largely consistent with the existing literature of MR studies of alcohol and cardiovascular risk factors and outcomes which have found alcohol to be generally harmful and/or neutral for CVD related outcomes and most cardiometabolic risk factors [46–48, 51, 52]. For example, the first large MR study of risk factors and outcomes using data gathered from over 56 cohort studies of individuals of European ancestry and the same genetic instrument in ADH1B found moderate alcohol use to be associated with higher systolic blood pressure, waist circumference, BMI, LDL, and risk of coronary heart disease [47]. Another smaller MR study in Danes also found a direct association with a higher BMI [46]. A study of the China Kadoorie biobank (>500,000) used a combination of instruments in both ALDH2 and ADH1B found alcohol to be positively associated with increasing systolic blood pressure, HDL, ischemic stroke, and intracerebral hemorrhage, but no effect was found for myocardial infarction [51]. Another recent study of alcohol and CVD outcomes in the UK Biobank using a multi-SNP instrument variable found an increase in blood pressure, stroke, and peripheral artery disease [48]. The inverse association of alcohol with triglycerides that we observed has also been shown in several other MR studies [46–48] and could be related to the HDL raising effects. Diabetes has previously been found to have no association with alcohol in an MR meta-analysis (>14,000 cases) as instrumented by the same variant we used [47]. However, another study in a Chinese population using the ALDH2 rs671 variant, which has a more profound effect on alcohol intake, found a higher risk of diabetes with increasing alcohol [52]. Our study adds to the existing literature by showing sex-stratified differences which merit further investigation.
Major strengths of our study include the use of a single SNP as a genetic instrument to predict causality of alcohol consumption combined with a large sample size. Using a single instrument within an alcohol metabolizing gene that is strongly associated with the exposure maximizes the probability that the all assumptions of an MR study have been met and the results are accurately reflecting a relationship that is free from any residual confounding [53]. Further, we have replicated this analysis with a 25 SNP instrumental variable for alcohol use discovered in a dataset independent of the UK Biobank. A potential weakness may be the generalizability of our study given the well-established healthy cohort effect observed for the UK Biobank [54], although the healthy cohort may have helped by minimizing the inclusion of subjects with alcohol use disorder and/or moderate but still high-risk use of alcohol (e.g., binge drinkers). Our results are also limited to UK residents and therefore may vary somewhat in other populations although MR studies to date in other populations including Chinese are largely consistent with our findings [46, 47, 51, 52]. More research is needed on the determination of the causal effects of alcohol consumption in race/ethnic groups other than Europeans and East Asians to determine if effects observed to date generalize to all major race/ethnic groups. Some of our findings were not replicated in external datasets, which could reflect differences in drinking patterns between the cohorts. Two-sample analyses would be biased toward the null in the case that an external dataset has a smaller proportion of drinkers or could show a greater effect with a dataset with more drinkers.
Proposed mechanisms for the negative effect of alcohol on cardiometabolic disease include a pathway via raised blood pressure [55] and atherogenic lipids [56] as well as increased adiposity and subsequent risk of type 2 diabetes, consistent with our MR findings and those of others. Raised HDL has been proposed as a protective factor, but our MR results do not conclusively support that such elevations are directly related to alcohol among a population of predominantly moderate alcohol users. The same relationship with HDL has been observed in other MR studies [47, 48, 52]. Additionally, multiple lines of evidence now suggest that HDL levels are not causally associated with heart disease [17, 18] but instead serve as a marker of a variety of factors that may or may not affect the risk of CVD. In this context, one can speculate that physical activity raises HDL in a health-promoting way [57], while alcohol consumption does not. Further harm of alcohol for stroke could come from alcohol induced thrombocytopenia (hemorrhagic stroke) and reduced fibrinolysis (ischemic stroke) with alcohol use [58].
In conclusion, our analysis adds to the mounting evidence using MR that alcohol use does not improve cardiovascular health even in moderate amounts and likely worsens it when all other factors are considered. Given this evidence and the fact that alcohol is implicated in a number of public health concerns not directly related to cardiometabolic health, including addictive disorders, accidents, suicides, liver disease, and various types of cancers (e.g. esophageal, gastrointestinal, head and neck) [59], we believe it is time to reconsider current public health recommendations in the US and other countries which suggest that up to two drinks/day for men and one drink/day for women is not harmful and possibly beneficial to cardiovascular health [60]. This reconsideration is also supported by a more recent observational study that considered the full spectrum of alcohol related health consequences across the entire age spectrum and concluded that the level of consumption that minimizes health loss is zero [59]. Properly conducted randomized control trials [61] may one day more reliably inform us on this matter but, until that time comes, Mendelian randomization analyses provides an acceptable alternative to help inform health policy in this respect.
Supporting information
ICD codes used for disease definitions. ICD codes found in primary and secondary diagnoses were included. * Including all subcategories.
(PDF)
(PDF)
Variants used for instrumental variable in inverse variance weighted, multivariable, and two-sample MR analyses; data sources for two sample Mendelian randomization.
(PDF)
Glasses/day indicates average number of equivalent glasses of wine per day calculated from annualized intake of all alcohol types. Multiple comparisons corrections with ANOVA: * = significant for alcohol consumption via Holm method, ** = also significant with Bonferroni correction. All results are compared to a reference of no alcohol consumption. Betas and (95% confidence intervals). SBP: Systolic blood pressure (mmHg). DBP: Diastolic blood pressure (mmHg). BMI: Body mass index (kg/m^2). WAIST: Waist circumference (cm). BFP: Body fat percentage. CHOL: Cholesterol (mmol/L). LDL: Low-density lipoprotein (mmol/L). HDL: High-density lipoprotein (mmol/L). TG: Triglycerides (mmol/L). HBA1C: Glycated hemoglobin (mmol/mol). T2D: type 2 diabetes. MI: myocardial infarction. ALLSTROKE: all types of stroke. ISTROKE: ischemic stroke. HSTROKE: hemorrhagic stroke. HF: heart failure. AFIB: atrial fibrillation. CVD: any cardiovascular disease (MI, ALLSTROKE, ISTROKE, HSTROKE, HF, AFIB). Death: all-cause death.
(PDF)
(PDF)
* indicates the source also includes UK Biobank data. CVDKP = Cardiovascular disease knowledge portal [43], http://www.broadcvdi.org/home/portalHome. T2DKP = Type 2 diabetes knowledge portal [44], http://www.type2diabetesgenetics.org/.
(PDF)
n (%) for categorical variable traits or mean (standard deviation) for quantitative variable traits (in listed units). Total column is repeated from main Table 1.
(PDF)
All results are compared to a reference of no alcohol consumption. Bars indicate 95% confidence interval. SBP: Systolic blood pressure (mmHg). DBP: Diastolic blood pressure (mmHg). BMI: Body mass index (kg/m^2). WAIST: Waist circumference (cm). BFP: Body fat percentage. CHOL: Cholesterol (mmol/L). LDL: Low-density lipoprotein (mmol/L). HDL: High-density lipoprotein (mmol/L). TG: Triglycerides (mmol/L). HBA1C: Glycated hemoglobin (mmol/mol).
(TIFF)
All results are compared to a reference of no alcohol consumption. Bars indicate 95% confidence interval. T2D: type 2 diabetes. MI: myocardial infarction. ALLSTROKE: all types of stroke. ISTROKE: ischemic stroke. HSTROKE: hemorrhagic stroke. HF: heart failure. AFIB: atrial fibrillation. CVD: any cardiovascular disease (MI, ALLSTROKE, ISTROKE, HSTROKE, HF, AFIB). Death: all-cause death.
(TIFF)
Data Availability
This study used data are from the UK Biobank (www.ukbiobank.ac.uk) and legal constraints do not permit public sharing of the data. The UK Biobank, however, is open to all qualified researchers anywhere in the world. Thus, the data used in this communication can be easily and directly accessed by applying through the UK Biobank Access Management System (https://www.ukbiobank.ac.uk/register-apply). The data for this study was accessed through application 13271.
Funding Statement
JL was funded by 1F32HL149254 by the National Heart, Lung, and Blood Institute (https://www.nhlbi.nih.gov/) and 2T32DK007217 by the National Institute of Diabetes and Digestive and Kidney Diseases (https://www.niddk.nih.gov/). JL, DZ, EI, and TLA were funded by 1R01HL135313 by the National Heart, Lung, and Blood Institute (https://www.nhlbi.nih.gov/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Erik Ingelsson is now an employee of GlaxoSmithKline, but his contribution to this work was completed before his departure from Stanford University. The funder provided support in the form of salaries for an author [EI], but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section.
References
- 1.Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, et al. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001–2002 to 2012–2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911–23. doi: 10.1001/jamapsychiatry.2017.2161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NHS. Part 4: Drinking behaviours among adults 2020 [Available from: https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-alcohol/2020/part-4.
- 3.Koppes LL, Dekker JM, Hendriks HF, Bouter LM, Heine RJ. Moderate alcohol consumption lowers the risk of type 2 diabetes: a meta-analysis of prospective observational studies. Diabetes Care. 2005;28(3):719–25. doi: 10.2337/diacare.28.3.719 [DOI] [PubMed] [Google Scholar]
- 4.Li XH, Yu FF, Zhou YH, He J. Association between alcohol consumption and the risk of incident type 2 diabetes: a systematic review and dose-response meta-analysis. Am J Clin Nutr. 2016;103(3):818–29. doi: 10.3945/ajcn.115.114389 [DOI] [PubMed] [Google Scholar]
- 5.Friedman LA, Kimball AW. Coronary heart disease mortality and alcohol consumption in Framingham. Am J Epidemiol. 1986;124(3):481–9. doi: 10.1093/oxfordjournals.aje.a114418 [DOI] [PubMed] [Google Scholar]
- 6.Gordon T, Kannel WB. Drinking habits and cardiovascular disease: the Framingham Study. Am Heart J. 1983;105(4):667–73. doi: 10.1016/0002-8703(83)90492-1 [DOI] [PubMed] [Google Scholar]
- 7.Wood AM, Kaptoge S, Butterworth AS, Willeit P, Warnakula S, Bolton T, et al. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. 2018;391(10129):1513–23. doi: 10.1016/S0140-6736(18)30134-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sacco RL, Elkind M, Boden-Albala B, Lin IF, Kargman DE, Hauser WA, et al. The protective effect of moderate alcohol consumption on ischemic stroke. Jama. 1999;281(1):53–60. doi: 10.1001/jama.281.1.53 [DOI] [PubMed] [Google Scholar]
- 9.Reynolds K, Lewis B, Nolen JD, Kinney GL, Sathya B, He J. Alcohol consumption and risk of stroke: a meta-analysis. Jama. 2003;289(5):579–88. doi: 10.1001/jama.289.5.579 [DOI] [PubMed] [Google Scholar]
- 10.Stampfer MJ, Colditz GA, Willett WC, Speizer FE, Hennekens CH. A prospective study of moderate alcohol consumption and the risk of coronary disease and stroke in women. N Engl J Med. 1988;319(5):267–73. doi: 10.1056/NEJM198808043190503 [DOI] [PubMed] [Google Scholar]
- 11.Gallagher C, Hendriks JML, Elliott AD, Wong CX, Rangnekar G, Middeldorp ME, et al. Alcohol and incident atrial fibrillation—A systematic review and meta-analysis. Int J Cardiol. 2017;246:46–52. doi: 10.1016/j.ijcard.2017.05.133 [DOI] [PubMed] [Google Scholar]
- 12.Walsh CR, Larson MG, Evans JC, Djousse L, Ellison RC, Vasan RS, et al. Alcohol consumption and risk for congestive heart failure in the Framingham Heart Study. Ann Intern Med. 2002;136(3):181–91. doi: 10.7326/0003-4819-136-3-200202050-00005 [DOI] [PubMed] [Google Scholar]
- 13.Marmot MG, Elliott P, Shipley MJ, Dyer AR, Ueshima H, Beevers DG, et al. Alcohol and blood pressure: the INTERSALT study. Bmj. 1994;308(6939):1263–7. doi: 10.1136/bmj.308.6939.1263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Castelli WP, Doyle JT, Gordon T, Hames CG, Hjortland MC, Hulley SB, et al. Alcohol and blood lipids. The cooperative lipoprotein phenotyping study. Lancet. 1977;2(8030):153–5. doi: 10.1016/s0140-6736(77)90176-3 [DOI] [PubMed] [Google Scholar]
- 15.Hartung GH, Foreyt JP, Mitchell RE, Mitchell JG, Reeves RS, Gotto AM Jr., Effect of alcohol intake on high-density lipoprotein cholesterol levels in runners and inactive men. Jama. 1983;249(6):747–50. [PubMed] [Google Scholar]
- 16.Schrieks IC, Heil AL, Hendriks HF, Mukamal KJ, Beulens JW. The effect of alcohol consumption on insulin sensitivity and glycemic status: a systematic review and meta-analysis of intervention studies. Diabetes Care. 2015;38(4):723–32. doi: 10.2337/dc14-1556 [DOI] [PubMed] [Google Scholar]
- 17.Voight BF, Peloso GM, Orho-Melander M, Frikke-Schmidt R, Barbalic M, Jensen MK, et al. Plasma HDL cholesterol and risk of myocardial infarction: a mendelian randomisation study. Lancet. 2012;380(9841):572–80. doi: 10.1016/S0140-6736(12)60312-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenson RS. The High-Density Lipoprotein Puzzle: Why Classic Epidemiology, Genetic Epidemiology, and Clinical Trials Conflict? Arterioscler Thromb Vasc Biol. 2016;36(5):777–82. doi: 10.1161/ATVBAHA.116.307024 [DOI] [PubMed] [Google Scholar]
- 19.Armitage J, Holmes MV, Preiss D. Cholesteryl Ester Transfer Protein Inhibition for Preventing Cardiovascular Events: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;73(4):477–87. doi: 10.1016/j.jacc.2018.10.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Emberson JR, Bennett DA. Effect of alcohol on risk of coronary heart disease and stroke: causality, bias, or a bit of both? Vasc Health Risk Manag. 2006;2(3):239–49. doi: 10.2147/vhrm.2006.2.3.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sesso HD, Cook NR, Buring JE, Manson JE, Gaziano JM. Alcohol consumption and the risk of hypertension in women and men. Hypertension. 2008;51(4):1080–7. doi: 10.1161/HYPERTENSIONAHA.107.104968 [DOI] [PubMed] [Google Scholar]
- 22.Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3):e1001779. doi: 10.1371/journal.pmed.1001779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.NHS. Alcohol Units [Available from: https://www.nhs.uk/live-well/alcohol-support/calculating-alcohol-units/.
- 24.Karczewski KJ, Francioli LC, Tiao G, Cummings BB, Alföldi J, Wang Q, et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 2020;581(7809):434–43. doi: 10.1038/s41586-020-2308-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Genome Aggregation Database [Available from: https://gnomad.broadinstitute.org/variant/4-100239319-T-C?dataset=gnomad_r2_1.
- 26.Kaufman JS, MacLehose RF. Which of these things is not like the others? Cancer. 2013;119(24):4216–22. doi: 10.1002/cncr.28359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nikpay M, Goel A, Won HH, Hall LM, Willenborg C, Kanoni S, et al. A comprehensive 1,000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat Genet. 2015;47(10):1121–30. doi: 10.1038/ng.3396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malik R, Chauhan G, Traylor M, Sargurupremraj M, Okada Y, Mishra A, et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat Genet. 2018;50(4):524–37. doi: 10.1038/s41588-018-0058-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shah S, Henry A, Roselli C, Lin H, Sveinbjörnsson G, Fatemifar G, et al. Genome-wide association and Mendelian randomisation analysis provide insights into the pathogenesis of heart failure. Nat Commun. 2020;11(1):163. doi: 10.1038/s41467-019-13690-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roselli C, Chaffin MD, Weng LC, Aeschbacher S, Ahlberg G, Albert CM, et al. Multi-ethnic genome-wide association study for atrial fibrillation. Nat Genet. 2018;50(9):1225–33. doi: 10.1038/s41588-018-0133-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahajan A, Taliun D, Thurner M, Robertson NR, Torres JM, Rayner NW, et al. Fine-mapping type 2 diabetes loci to single-variant resolution using high-density imputation and islet-specific epigenome maps. Nat Genet. 2018;50(11):1505–13. doi: 10.1038/s41588-018-0241-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scott RA, Scott LJ, Mägi R, Marullo L, Gaulton KJ, Kaakinen M, et al. An Expanded Genome-Wide Association Study of Type 2 Diabetes in Europeans. Diabetes. 2017;66(11):2888–902. doi: 10.2337/db16-1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Locke AE, Steinberg KM, Chiang CWK, Service SK, Havulinna AS, Stell L, et al. Exome sequencing of Finnish isolates enhances rare-variant association power. Nature. 2019;572(7769):323–8. doi: 10.1038/s41586-019-1457-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wheeler E, Leong A, Liu CT, Hivert MF, Strawbridge RJ, Podmore C, et al. Impact of common genetic determinants of Hemoglobin A1c on type 2 diabetes risk and diagnosis in ancestrally diverse populations: A transethnic genome-wide meta-analysis. PLoS Med. 2017;14(9):e1002383. doi: 10.1371/journal.pmed.1002383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Turcot V, Lu Y, Highland HM, Schurmann C, Justice AE, Fine RS, et al. Protein-altering variants associated with body mass index implicate pathways that control energy intake and expenditure in obesity. Nat Genet. 2018;50(1):26–41. doi: 10.1038/s41588-017-0011-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang J, Loos RJ, Powell JE, Medland SE, Speliotes EK, Chasman DI, et al. FTO genotype is associated with phenotypic variability of body mass index. Nature. 2012;490(7419):267–72. doi: 10.1038/nature11401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shungin D, Winkler TW, Croteau-Chonka DC, Ferreira T, Locke AE, Mägi R, et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature. 2015;518(7538):187–96. doi: 10.1038/nature14132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ehret GB, Ferreira T, Chasman DI, Jackson AU, Schmidt EM, Johnson T, et al. The genetics of blood pressure regulation and its target organs from association studies in 342,415 individuals. Nat Genet. 2016;48(10):1171–84. doi: 10.1038/ng.3667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Accelerating Medicines Partnership. 2018 [Available from: http://t2d-genetics-portal.blogspot.com/2018/02/federation-brings-three-new-datasets-to.html.
- 40.Lu Y, Day FR, Gustafsson S, Buchkovich ML, Na J, Bataille V, et al. New loci for body fat percentage reveal link between adiposity and cardiometabolic disease risk. Nat Commun. 2016;7:10495. doi: 10.1038/ncomms10495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu DJ, Peloso GM, Yu H, Butterworth AS, Wang X, Mahajan A, et al. Exome-wide association study of plasma lipids in >300,000 individuals. Nat Genet. 2017;49(12):1758–66. doi: 10.1038/ng.3977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Willer CJ, Schmidt EM, Sengupta S, Peloso GM, Gustafsson S, Kanoni S, et al. Discovery and refinement of loci associated with lipid levels. Nat Genet. 2013;45(11):1274–83. doi: 10.1038/ng.2797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cerebrovascular Disease Knowledge Portal, NINDS grant # 1R24NS092983 [Available from: http://www.cerebrovascularportal.org/home/portalHome.
- 44.Type 2 Diabetes Knowledge Portal [Available from: http://www.type2diabetesgenetics.org/.
- 45.Rimm EB, Williams P, Fosher K, Criqui M, Stampfer MJ. Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors. Bmj. 1999;319(7224):1523–8. doi: 10.1136/bmj.319.7224.1523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lawlor DA, Nordestgaard BG, Benn M, Zuccolo L, Tybjaerg-Hansen A, Davey Smith G. Exploring causal associations between alcohol and coronary heart disease risk factors: findings from a Mendelian randomization study in the Copenhagen General Population Study. Eur Heart J. 2013;34(32):2519–28. doi: 10.1093/eurheartj/eht081 [DOI] [PubMed] [Google Scholar]
- 47.Holmes MV, Dale CE, Zuccolo L, Silverwood RJ, Guo Y, Ye Z, et al. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. Bmj. 2014;349:g4164. doi: 10.1136/bmj.g4164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Larsson SC, Burgess S, Mason AM, Michaëlsson K. Alcohol Consumption and Cardiovascular Disease: A Mendelian Randomization Study. Circ Genom Precis Med. 2020;13(3):e002814. doi: 10.1161/CIRCGEN.119.002814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lindenbaum J, Roman MJ. Nutritional anemia in alcoholism. Am J Clin Nutr. 1980;33(12):2727–35. doi: 10.1093/ajcn/33.12.2727 [DOI] [PubMed] [Google Scholar]
- 50.Sakamoto N, Hu H, Nanri A, Mizoue T, Eguchi M, Kochi T, et al. Associations of anemia and hemoglobin with hemoglobin A1c among non-diabetic workers in Japan. J Diabetes Investig. 2020;11(3):719–25. doi: 10.1111/jdi.13159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Millwood IY, Walters RG, Mei XW, Guo Y, Yang L, Bian Z, et al. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in China. Lancet. 2019;393(10183):1831–42. doi: 10.1016/S0140-6736(18)31772-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Peng M, Zhang J, Zeng T, Hu X, Min J, Tian S, et al. Alcohol consumption and diabetes risk in a Chinese population: a Mendelian randomization analysis. Addiction. 2019;114(3):436–49. doi: 10.1111/add.14475 [DOI] [PubMed] [Google Scholar]
- 53.Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23(R1):R89–98. doi: 10.1093/hmg/ddu328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, et al. Comparison of Sociodemographic and Health-Related Characteristics of UK Biobank Participants With Those of the General Population. Am J Epidemiol. 2017;186(9):1026–34. doi: 10.1093/aje/kwx246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grogan JR, Kochar MS. Alcohol and hypertension. Arch Fam Med. 1994;3(2):150–4. doi: 10.1001/archfami.3.2.150 [DOI] [PubMed] [Google Scholar]
- 56.Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. Bmj. 2011;342:d636. doi: 10.1136/bmj.d636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wood PD, Stefanick ML, Dreon DM, Frey-Hewitt B, Garay SC, Williams PT, et al. Changes in plasma lipids and lipoproteins in overweight men during weight loss through dieting as compared with exercise. N Engl J Med. 1988;319(18):1173–9. doi: 10.1056/NEJM198811033191801 [DOI] [PubMed] [Google Scholar]
- 58.Ballard HS. The hematological complications of alcoholism. Alcohol Health Res World. 1997;21(1):42–52. [PMC free article] [PubMed] [Google Scholar]
- 59.Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10152):1015–35. doi: 10.1016/S0140-6736(18)31310-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Office of Disease Prevention and Health Promotion. Alcohol [Available from: https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines/appendix-9/.
- 61.Spiegelman D, Lovato LC, Khudyakov P, Wilkens TL, Adebamowo CA, Adebamowo SN, et al. The Moderate Alcohol and Cardiovascular Health Trial (MACH15): Design and methods for a randomized trial of moderate alcohol consumption and cardiometabolic risk. Eur J Prev Cardiol. 2020:2047487320912376. doi: 10.1177/2047487320912376 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ICD codes used for disease definitions. ICD codes found in primary and secondary diagnoses were included. * Including all subcategories.
(PDF)
(PDF)
Variants used for instrumental variable in inverse variance weighted, multivariable, and two-sample MR analyses; data sources for two sample Mendelian randomization.
(PDF)
Glasses/day indicates average number of equivalent glasses of wine per day calculated from annualized intake of all alcohol types. Multiple comparisons corrections with ANOVA: * = significant for alcohol consumption via Holm method, ** = also significant with Bonferroni correction. All results are compared to a reference of no alcohol consumption. Betas and (95% confidence intervals). SBP: Systolic blood pressure (mmHg). DBP: Diastolic blood pressure (mmHg). BMI: Body mass index (kg/m^2). WAIST: Waist circumference (cm). BFP: Body fat percentage. CHOL: Cholesterol (mmol/L). LDL: Low-density lipoprotein (mmol/L). HDL: High-density lipoprotein (mmol/L). TG: Triglycerides (mmol/L). HBA1C: Glycated hemoglobin (mmol/mol). T2D: type 2 diabetes. MI: myocardial infarction. ALLSTROKE: all types of stroke. ISTROKE: ischemic stroke. HSTROKE: hemorrhagic stroke. HF: heart failure. AFIB: atrial fibrillation. CVD: any cardiovascular disease (MI, ALLSTROKE, ISTROKE, HSTROKE, HF, AFIB). Death: all-cause death.
(PDF)
(PDF)
* indicates the source also includes UK Biobank data. CVDKP = Cardiovascular disease knowledge portal [43], http://www.broadcvdi.org/home/portalHome. T2DKP = Type 2 diabetes knowledge portal [44], http://www.type2diabetesgenetics.org/.
(PDF)
n (%) for categorical variable traits or mean (standard deviation) for quantitative variable traits (in listed units). Total column is repeated from main Table 1.
(PDF)
All results are compared to a reference of no alcohol consumption. Bars indicate 95% confidence interval. SBP: Systolic blood pressure (mmHg). DBP: Diastolic blood pressure (mmHg). BMI: Body mass index (kg/m^2). WAIST: Waist circumference (cm). BFP: Body fat percentage. CHOL: Cholesterol (mmol/L). LDL: Low-density lipoprotein (mmol/L). HDL: High-density lipoprotein (mmol/L). TG: Triglycerides (mmol/L). HBA1C: Glycated hemoglobin (mmol/mol).
(TIFF)
All results are compared to a reference of no alcohol consumption. Bars indicate 95% confidence interval. T2D: type 2 diabetes. MI: myocardial infarction. ALLSTROKE: all types of stroke. ISTROKE: ischemic stroke. HSTROKE: hemorrhagic stroke. HF: heart failure. AFIB: atrial fibrillation. CVD: any cardiovascular disease (MI, ALLSTROKE, ISTROKE, HSTROKE, HF, AFIB). Death: all-cause death.
(TIFF)
Data Availability Statement
This study used data are from the UK Biobank (www.ukbiobank.ac.uk) and legal constraints do not permit public sharing of the data. The UK Biobank, however, is open to all qualified researchers anywhere in the world. Thus, the data used in this communication can be easily and directly accessed by applying through the UK Biobank Access Management System (https://www.ukbiobank.ac.uk/register-apply). The data for this study was accessed through application 13271.


