Abstract
Objective
Despite a growing literature on potential risk factors for eating disorders, longitudinal research starting before adolescence is scarce, and little is known about risk factors in males. We investigated risk factors in preadolescent boys and girls for the development of eating pathology in adolescence and young adulthood.
Method
This study is part of TRAILS (TRacking Adolescents' Individual Lives Survey), a Dutch population‐based cohort study (N = 2,229) from preadolescence into adulthood. Potential risk factors were measured at age 11, based on self‐report, reports of one of the parents, and records of the Preventive Child Healthcare. Variables included sociodemographic variables, pregnancy and perinatal factors, eating‐ and weight‐related factors, psychological functioning, stressful experiences and family factors. At age 19, two‐stage screening including interviews by eating disorder experts was used to examine the prevalence of eating disorders. At age 22 and 26, eating pathology was assessed by the Eating Disorder Diagnostic Scale.
Results
Preadolescent anxious distress and high weight were associated with eating pathology in adolescence and young adulthood in both boys and girls. Overeating in preadolescence was found to be a prodromal symptom of eating disorders during late adolescence. No evidence was found for sex‐specific risk factors.
Discussion
Anxious preadolescents with high weight are at increased risk for the development of eating pathology later on. Clinicians should be aware of eating disorder symptoms — like overeating — in this high‐risk group of children, and could consider an early intervention to prevent the development of full‐blown eating disorders.
Keywords: adolescence, anxiety, body weight, eating disorders, longitudinal, overeating, risk factors
1. INTRODUCTION
The present study investigates risk factors in preadolescent girls and boys for the development of eating pathology later on. Eating disorders are severe mental disorders which often run a chronic course and which have many negative outcomes, including long‐term functional impairment and an elevated mortality risk (Iwajomo et al., 2020; van Hoeken & Hoek, 2020; Wonderlich, Bulik, Schmidt, Steiger, & Hoek, 2020). Help‐seeking is often delayed, for example, for reasons of denial (particularly in anorexia nervosa [AN]), or shame and stigma (particularly in bulimia nervosa [BN] and binge eating disorder [BED]), with ensuing risk of chronicity. Prevention programs may reduce the onset of eating pathology. Although some eating disorder prevention programs have been developed, their efficacy has to be improved (Stice, Johnson, & Turgon, 2019). Because of the relatively low prevalence of eating disorders, focused targeted prevention would generally be more (cost‐) effective than universal prevention strategies at population level. Thus, it is important to identify target groups at high risk for the development of an eating disorder. Research into risk factors for eating pathology advances our knowledge of the etiology and high‐risk subgroups and is therefore needed.
The risk factor most consistently found in the eating disorder literature is being a female (Jacobi, Hayward, de Zwaan, Kraemer, & Agras, 2004). Subsequently, most studies have exclusively focused on females (Culbert, Racine, & Klump, 2015; Raevuori, Keski‐Rahkonen, & Hoek, 2014). Although the prevalence of eating disorders among males is relatively low — which might be an underestimation due to underdetection and unawareness — the negative consequences of eating disorders in males are equally serious (van Hoeken & Hoek, 2020). Mortality rates in males are comparable to those in females (Iwajomo et al., 2020; Suokas et al., 2013). Results from studies in females are not automatically generalizable to males, because risk factors for eating disorders may be sex‐specific (Micali et al., 2015; Raevuori et al., 2014). For example, contrary to females, higher parental education has not been associated with eating disorders in males (Ahren et al., 2013). Another study showed that dietary restraint in childhood was a significant predictor for eating pathology in adolescent boys, but not in girls (Evans et al., 2017). In contrast, depressive symptoms were only associated with eating pathology in girls in that study. Sex‐related differences could have implications for the development of targeted intervention and prevention programs. Therefore, it is important to investigate risk factors in both boys and girls.
It has been argued that preadolescence may be a key age period for prevention, before the high‐risk period of eating disorder onset (Culbert et al., 2015; Evans et al., 2017; Rohde, Stice, & Marti, 2015). Exploring risk factors in this life phase could elucidate clues for intervention and prevention. Precedence is a crucial criterion in the establishment of a variable's status as a risk factor (Jacobi et al., 2004). Establishing precedence requires longitudinal, preferably prospective, studies. Recently, a systematic literature review of prospective studies in nonclinical cohorts of children and adolescents (McClelland, Robinson, Potterton, Mountford, & Schmidt, 2020) showed that eating and feeding problems in childhood and dieting, body dissatisfaction, weight/shape concerns, and anxiety and depression in preadolescence were identified as possible risk factors for eating pathology in adolescence and young adulthood. Despite a growing literature on potential risk factors for eating disorders, authors asked for more research to establish their findings, especially before adolescence, because longitudinal research in this life period is scarce (Culbert et al., 2015; Jacobi et al., 2004; McClelland et al., 2020).
The etiology of eating pathology is complex and involves an interplay of biological, psychological and behavioral factors, which is not fully understood (Jacobi et al., 2004). Many studies have specifically focused on one area of interest, like pregnancy and perinatal factors (Larsen, Bulik, Thornton, Koch, & Petersen, 2020; Watson et al., 2019), weight and shape concerns (Killen et al., 1996; Stice & Shaw, 2002), affective symptoms (Ranta et al., 2017; Schaumberg et al., 2019), early childhood eating problems (Kotler, Cohen, Davies, Pine, & Walsh, 2001; Marchi & Cohen, 1990), sexual abuse (Johnson, Cohen, Kasen, & Brook, 2002; Smolak & Murnen, 2002) and family factors (Dominy, Johnson, & Koch, 2000; Shoebridge & Gowers, 2000). In general, effect sizes for risk factors tend to be small. This underscores the importance of joint examination of potential risk factors to better understand the relative contribution of each factor in the etiology of eating pathology, and to identify high‐risk subgroups. In recent years, several prospective studies have investigated combinations of potential risk factors (Jacobi et al., 2011; Stice, Gau, Rohde, & Shaw, 2017), but these studies focused on already high‐risk groups of females. A community approach in both males and females could elucidate other risk factors, and help generate hypotheses about the etiology of eating pathology and identify high‐risk subgroups.
The aim of the present study is to explore risk factors for the development of eating pathology in a prospective, community cohort study covering preadolescence through young adulthood. We will examine whether risk factors are sex‐specific. A diverse range of putative risk factors is included in our study based on prior (review) studies on risk factors for the development of eating disorders (Culbert et al., 2015; Jacobi et al., 2004; Jacobi et al., 2011; McClelland et al., 2020; Rohde et al., 2015; Stice et al., 2017; Stice et al., 2019).
2. METHOD
2.1. Study population
This study is based on data from TRAILS (TRacking Adolescents' Individual Lives Survey), a Dutch longitudinal population‐based cohort study that has followed participants from preadolescence into adulthood. A full description of the population under study and design can be found elsewhere (de Winter et al., 2005; Oldehinkel et al., 2015). Briefly, in 2001, TRAILS enrolled 2,229 children through selection by community registers and primary schools, with an initial response rate of 76.0%. The sample includes predominantly Caucasian children from the north of the Netherlands, including both urban and rural areas. Follow‐up assessment waves took place approximately every third year. The present study used data from the first assessment wave (T1): mean age 11.1 years, SD = 0.6, the fourth assessment wave (T4): n = 1,881, response 84.3%, mean age 19.1 years, SD = 0.6; the fifth assessment wave (T5): n = 1,782, response 79.9%, mean age 22.3 years, SD = 0.7; and the sixth assessment wave (T6): n = 1,618, response 72.6%, mean age 25.7 years, SD = 0.6. The proportion of female participants ranged from 50.8% (T1) to 54.5% (T6). Informed consent was obtained from the participants themselves at each assessment wave and from their parent(s) or guardian at T1. The Dutch Central Committee on Research Involving Human Subjects has approved the TRAILS study.
2.2. Measures
2.2.1. Eating pathology — DSM‐5 diagnoses
At T4, a two‐stage screening approach was used to assess the prevalence of eating disorders (AN, BN, BED, other specified feeding or eating disorder (OSFED), and unspecified feeding or eating disorder (UFED)) (Smink, van Hoeken, Oldehinkel, & Hoek, 2014). In the first stage, participants at high risk for an eating disorder were identified through 11 selection criteria based on the core characteristics of an eating disorder: low or high BMI, binge eating, compensatory behaviors and a distorted body image (American Psychiatric Association, 2000). In the second stage, participants in the high‐risk group (n = 312) were invited for an additional interview by telephone, conducted by a resident in psychiatry or a psychologist, both clinically experienced in diagnosing eating disorders. The eating disorder module of the Structured Clinical Interview for DSM Axis I disorders (SCID‐I; First, Spitzer, Gibbon, & Williams, 1995; Groenestijn, Akkerhuis, Kupka, Schneider, & Nolen, 1998) with adjusted skip rules and parts of the Eating Disorder Examination (EDE; Fairburn, Cooper, & O'Connor, 2008) were administered. All possible eating disorder cases were discussed in a consensus meeting with an eating disorder expert and member of the DSM‐5 eating disorders Work Group (co‐author HWH) to yield current and lifetime (including diagnoses at or before T1) diagnoses of eating disorders according to DSM‐5 criteria. More details about the selection criteria and diagnostic procedure have been published elsewhere (Smink et al., 2014).
2.2.2. Eating pathology — EDDS cut‐off score
Eating pathology at T5 and T6 was assessed by means of the Dutch translation of the Eating Disorder Diagnostic Scale (EDDS) by Krabbenborg et al. (Krabbenborg et al., 2012). This 22‐item self‐report questionnaire generates an overall symptom composite score that indicates the level of eating pathology, not the specific type of eating disorder problems (Krabbenborg et al., 2012; Stice, Fisher, & Martinez, 2004; Stice, Telch, & Rizvi, 2000). When at least half of the required items had been answered, the EDDS standardized score (ranging from 0 to 100) was constructed by summing standardized item scores, excluding items regarding height, weight, amenorrhea and use of birth control (van Eeden, Hoek, van Hoeken, Deen, & Oldehinkel, 2020). The internal consistency of the EDDS score has been shown to be satisfactory (Stice et al., 2004), and the EDDS score correlates strongly (r = 0.85, p < .001) with the symptom composite score of the EDE (Fairburn et al., 2008; Krabbenborg et al., 2012), the most frequently used questionnaire for examining eating disorders. The two‐week test–retest stability of the Dutch translation of the EDDS was 0.81 for females diagnosed with an eating disorder (n = 59) and 0.69 for healthy controls (Krabbenborg et al., 2012). We used an EDDS cut‐off score of 16.5 to classify participants with eating pathology. This cut‐off score has previously been shown to be the optimal trade‐off between sensitivity (0.88) and specificity (0.91) (Krabbenborg et al., 2012).
2.2.3. Eating pathology at T1
The prediction of eating pathology in later life by variables at T1 could be confounded by eating problems at T1. At this assessment wave, the EDDS was not administered. To correct for potential eating pathology, we constructed T1 proxies of core characteristics of eating disorders: distorted body image and compensatory behaviors for overeating (American Psychiatric Association, 2000). Distorted body image was indicated as a discrepancy between self‐reported and objective body weight, as displayed by a combination of “very true or often true” on the “overweight” item of the Youth Self‐Report (YSR, item 55) and an objective BMI below average (BMI z‐score < 0). Compensatory behaviors for overeating was defined as a combination of “very true or often true” on the “overeating” item of the YSR (item 53) or Child Behavior Checklist (CBCL, item 53) and on the “vomiting” item of the YSR (item 56 g). Items of the YSR and CBCL have been shown to have moderate to good test–retest stability (Achenbach & Rescorla, 2001).
2.2.4. Putative risk factors
Most of the potential risk factors were measured at T1 and were based on self‐report, reports of one of the parents (96% mothers), and records of the Preventive Child Healthcare. The variables included sociodemographic variables, pregnancy and perinatal factors, eating‐ and weight‐related factors, psychological functioning, stressful experiences and family factors.
Sociodemographic factors included sex, socioeconomic status, and ethnicity. Sex was coded as “female” = 1 and “male” = 0. Socioeconomic status was calculated as the average of the z‐scores of income, educational and occupational level of each parent at T1, using the International Standard Classification for Occupations (Ganzeboom & Treiman, 1996). For ethnicity, participants who had at least one parent born in a non‐developed country were categorized as “belonging to an ethnic minority group” (coded as 1, vs. 0 for “all other participants”).
Pregnancy and perinatal factors were based on records of the Preventive Child Healthcare when available (n = 1,816, 81.5%) and parental reports. The maternal variables alcohol use, smoking, physical and mental problems (among them pelvic instability, back problems, rubella infection, depression and psychosis) and dietary adjustments (like diet low in salt, sugar free, gluten free, iron rich) were coded as “present during pregnancy” = 1 versus “absent” = 0. Maternal and paternal ages in years at child's birth were calculated by subtracting the date of child's birth from the parent's date of birth. Information related to the birth and perinatal period was predominately obtained from the Preventive Child Healthcare records, and included the variables gestational age (in weeks), birth weight (in grams), multiple birth (“yes” = 1, “no” = 0), congenital malformations (“yes” = 1, “no” = 0) and perinatal complications (like caesarean section, incubation, oxygen administration, jaundice, blood transfusion and maternal physical, social, or psychological problems in the first month after birth, coded as “yes” = 1 vs. “no” = 0). Weight was categorized into “small” and “high weight for gestational age” according to prescriptive birth weight standards for the Dutch population (Hoftiezer et al., 2019; Hoftiezer, Hukkelhoven, Hogeveen, Straatman, & van Lingen, 2016).
Eating‐ and weight‐related factors included eating problems as toddler, food allergy, undereating, overeating, reported overweight, vomiting, excessive sport activity, and body mass index (BMI). At T1, parents were retrospectively asked about the presence of eating problems and food allergy during their child's toddler years (coded as “yes” = 1 vs. “no” = 0). Information regarding presence of eating problems in toddler years in records of the PHC was combined with the parental information. Undereating (YSR or CBCL, item 24), overeating (YSR or CBCL, item 53), reported overweight (YSR, item 55) and vomiting (YSR, item 56 g) were based on the corresponding items of the YSR and CBCL, administered at T1. The answers were coded as “very true or often true” = 1 versus “sometimes true” or “not true” = 0. Items of the YSR and CBCL have been shown to have moderate to good test–retest stability (Achenbach & Rescorla, 2001). Sport activity was measured by the question “How often do you sport (for example swimming, playing football, horse‐riding)?”. Excessive sport activity was categorized as “6 to 7 times a week” = 1 versus “less than 6 times a week” = 0. Trained research assistants measured participants' weight and height using calibrated scales at T1. Age‐standardized BMI z‐scores per sex were calculated according to the BMI WHO growth reference data for 5–18 year olds (de Onis et al., 2007; WHO, 2007).
Variables related to psychological functioning were assessed at T1 and included negative affectivity, self‐esteem (global and physical appearance related), alcohol use and symptoms of anxiety and depression. Negative affectivity was measured by the parent‐ and the self‐report versions of the Dutch translation of the Early Adolescent Temperament Questionnaire — Revised (EATQ‐R; Ellis, 2002; Hartman, 2000; Putnam, Ellis, & Rothbart, 2001). The Negative Affectivity scale contains 10 items (α = 0.72) in the parental version and 13 items (α = 0.80) in the children's version (r = 0.16). Each item could be rated on a 5‐point scale ranging from 1 (“hardly ever true”) to 5 (“almost always true”). Mean scores for negative affectivity were calculated when at least half of the items had been answered (van Eeden et al., 2020). The mean score of the parental and children's scores together was used in this study. The Self‐Perception Profile for Children (SPPC; Harter, 1982) was used to assess global self‐esteem and self‐perceptions regarding physical appearance. Both scales contain 6 items (global self‐esteem: α = 0.81; physical appearance: α = 0.77). High scores indicate high self‐esteem. The SPPC has been shown to have good reliability and validity (Muris, Meesters, & Fijen, 2003). Alcohol use was measured with the “alcohol” item of the Antisocial Behavior Questionnaire (ASBQ, item 7; Moffitt & Silva, 1988) and was coded as “any alcohol use” = 1 versus “never used alcohol” = 0. Symptoms of anxiety and depression were assessed by the Revised Child Anxiety and Depression Scale (RCADS; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000). We used the subscales for symptoms of generalized anxiety disorder (GAD, 6 items, α = 0.78), social phobia (SP, 9 items, α = 0.78), separation anxiety disorder (7 items, α = 0.66), panic disorder (9 items, α = 0.75), obsessive–compulsive disorder (6 items, α = 0.68) and major depression disorder (10 items, α = 0.71).
Stressful experiences included being bullied, adverse events and sexual abuse. Being bullied at T1 was based on the corresponding item (38) of the YSR and CBCL and was coded as “very true or often true” = 1 versus “sometimes true” or “not true” = 0. An adverse events score was calculated by summing up the number of adverse events experienced between birth and T1. Identical events that occurred more than once before T1 were counted three times at maximum. Adverse events included moves to other houses, hospital admissions, illness or death of dear one, parental divorce and long stay away from home. Sexual abuse before T1 was retrospectively assessed at T4 with a questionnaire of Traumatic Youth Experiences developed by TRAILS (Bonvanie, van Gils, Janssens, & Rosmalen, 2015). The answers were categorized into “experienced any form of sexual abuse (non‐contact, assault or rape) before the participant's age at T1” = 1 versus “never experienced any form of sexual abuse” = 0.
Parental factors included parental psychopathology (internalizing and externalizing disorders) and participant's perceived parental rearing styles. During the parental interview at T1, parental psychiatric disorders were assessed. Mothers were mostly interviewed (96%) and reported on their own and the participant's father's (history) of anxiety and depression (internalizing disorders) and antisocial behavior and substance use (externalizing disorders). The answers were categorized into “(probably) disorder” = 1 versus “no disorder” = 0. Perceived parental emotional warmth, rejection and overprotection were measured with the EMBU‐C (Swedish acronym for: My Memories of Upbringing; Markus, Lindhout, Boer, Hoogendijk, & Arrindell, 2003). The scale of emotional warmth contains 18 items (α = 0.91 for both parents), of rejection 17 items (α = 0.84 for both parents) and of overprotection 12 items (α = 0.70 for father and α = 0.71 for mother). The scores of perceived father's and mother's rearing styles were highly correlated and were combined in a mean score. High scores indicate more parental warmth, more rejection or overprotection.
All continuous variables were converted to a z‐score. All categorical variables were coded such that a value “1” indicated present/risk and “0” absent/no risk. This was applied on a priori grounds and before the analysis proper. For socioeconomic status, maternal and paternal age at child's birth, gestational age, birth weight, BMI, parental warmth, parental rejection, and parental overprotection, we checked for both linear and quadratic effects, in line with the literature (Jacobi et al., 2004; Larsen et al., 2020; West, Goldschmidt, Mason, & Neumark‐Sztainer, 2019) that both relatively low and relatively high scores (U‐shaped relations) could predict eating pathology.
2.3. Statistical analysis
Logistic regression was used to examine whether each potential risk indicator at T1 was univariately associated with the development of eating pathology: an eating disorder DSM‐5 diagnosis between T1 and T4 or an EDDS score above the cut‐off for eating pathology at T5 or T6. Due to the small number of cases in each eating disorder group at T4, the different groups were analyzed together and disorder‐specific analyses were not performed. In order to guarantee precedence of the potential risk factor in the development of eating disorders, participants with an age of onset preceding or being equal to their age at T1 (n = 3) were excluded from the analysis. Since risk factors for eating disorders may be sex‐specific, all univariate analyses were repeated including variables' interactions with sex. The variables and interactions with sex that showed a consistent significant (p < .05) association in univariate analyses for outcomes at T4, T5 and T6, were examined in multivariate analyses using logistic regression with forward and backward stepwise selection. The final multivariate analyses with EDDS scores were repeated in the subgroup of participants without eating pathology at T1. First, analyses were performed with participants without any missing data (complete case analysis) resulting in sample sizes per analysis that ranged from 864 to 1,589. The final multivariate analyses were confirmed in all participants using multiple imputations for missing data. The multiple imputation analysis used all variables as input variables. The analyses were conducted for each of 20 imputed data sets, and the results were recombined. Furthermore, we investigated with logistic regression models which variables at baseline predicted the development of eating pathology between T4 and T5, and between T5 and T6, after excluding participants with eating pathology at previous assessment waves. All analyses were conducted using SPSS version 25, and significance levels were set at .05.
3. RESULTS
3.1. Descriptive statistics
Table 1 provides descriptive data for the present sample. The lifetime (n = 58) and point prevalence (n = 36) rates of DSM‐5 eating disorders were, respectively, 5.7% and 3.7% among females, and 1.2% and 0.5% among males. The mean age at which first symptoms of the eating disorder occurred as reported in the diagnostic interview (age of onset) was 14.7 years (SD = 2.5). Based on this interview, 46 females and 9 males were diagnosed with an eating disorder that had developed between T1 and T4: 15 AN, 8 BN, 23 BED, 7 OSFED and 2 UFED. At T5 and T6, respectively 24.6% and 31.4% of the participants scored above the EDDS cut‐off score for eating pathology. The prevalence was higher among females than males at both T5 (females: 35%; males: 11.2%) and T6 (females: 43.1% and males: 14.2%). At T1, eight participants displayed a distorted body image. Perceived overweight in combination with vomiting was found in two participants.
TABLE 1.
Descriptive statistics
| Variable | N | Mean (SD) or percentage |
|---|---|---|
| Sociodemographic factors | ||
| Sex (female) | 2,229 | 50.7% |
| Age T1 | 2,229 | 11.1 (0.6) |
| Age T4 | 1,880 | 19.1 (0.6) |
| Age T5 | 1,781 | 22.3 (0.7) |
| Age T6 | 1,616 | 25.7 (0.6) |
| Socioeconomic status z‐score T1 | 2,187 | −0.05 (0.8) |
| Ethnicity (minority group) | 2,229 | 10.6% |
| Pregnancy and perinatal factors | ||
| Maternal alcohol use during pregnancy | 2,181 | 13.5% |
| Maternal smoking during pregnancy | 2,185 | 30.8% |
| Maternal problems during pregnancy | 2,189 | 36.1% |
| Maternal dietary adjustments | 1,424 | 23.5% |
| Maternal age at child's birth | 2,115 | 29.3 (4.6) |
| Paternal age at child's birth | 1,673 | 32.0 (4.8) |
| Gestational age (weeks) | 2,200 | 39.6 (1.9) |
| Birth weight (grams) | 2,186 | 3,398.7 (571.3) |
| Small for gestational age | 2,154 | 15.0% |
| Large for gestational age | 2,154 | 9.2% |
| Multiple birth | 1,806 | 2.0% |
| Congenital malformations | 2,213 | 1.7% |
| Perinatal complications | 2,172 | 39.4% |
| Eating‐ and weight‐related factors | ||
| Eating problems as toddler | 2,212 | 23.7% |
| Food allergy as toddler | 2,172 | 6.4% |
| Undereating T1 | 2,224 | 8.9% |
| Overeating T1 | 2,223 | 7.3% |
| Reported overweight T1 | 2,183 | 7.4% |
| Vomiting T1 | 2,156 | 1.6% |
| Excessive sport activity T1 | 2,190 | 13.3% |
| Body mass index WHO z‐score T1 | 2,160 | 0.04 (1.2) |
| Psychological functioning | ||
| Negative affectivity T1 | 2,211 | 2.6 (0.5) |
| Self‐esteem — Global T1 | 2,207 | 3.3 (0.5) |
| Self‐esteem — Physical appearance T1 | 2,207 | 3.1 (0.7) |
| Alcohol use T1 | 2,198 | 30.9% |
| Generalized anxiety disorder T1 | 2,207 | 0.7 (0.5) |
| Social phobia T1 | 2,208 | 0.8 (0.4) |
| Separation anxiety disorder T1 | 2,208 | 0.4 (0.4) |
| Panic disorder T1 | 2,207 | 0.4 (0.4) |
| Obsessive–compulsive disorder T1 | 2,205 | 0.6 (0.4) |
| Major depression disorder T1 | 2,208 | 0.6 (0.3) |
| Stressful experiences | ||
| Being bullied T1 | 2,185 | 5.7% |
| Adverse events | 2,186 | 3.4 (2.1) |
| Sexual abuse | 1,525 | 2.2% |
| Family factors | ||
| Parental psychopathology — Internalizing | 2,134 | 41.5% |
| Parental psychopathology — Externalizing | 2,119 | 13.4% |
| Perceived parental warmth T1 | 2,206 | 3.2 (0.5) |
| Perceived parental rejection T1 | 2,205 | 1.5 (0.3) |
| Perceived parental overprotection T1 | 2,205 | 1.9 (0.4) |
| Eating pathology | ||
| DSM‐5 eating disorder diagnoses T4 | 1,592 | 3.6% |
| EDDS > cut‐off scorea T5 | 1,496 | 24.6% |
| EDDS > cut‐off scorea T6 | 1,297 | 31.4% |
Abbreviation: EDDS, Eating Disorder Diagnostic Scale.
EDDS standardized scores could range between 0 (no eating pathology) and 100 (high level of eating pathology). An EDDS cut‐off score of 16.5 was used to classify participants with eating pathology.
Figure 1 shows the flow chart of participants with available information regarding eating pathology at T4, T5, and T6. At T4, 55 participants were identified with an eating disorder that had developed between T1 and T4. At T5, 20.1% (309/1534) of the participants without an eating disorder up to T4, scored above the cut‐off for eating pathology. At T6, 15.0% (152/1016) of the participants without eating pathology at T4 and T5, scored above the cut‐off for eating pathology.
FIGURE 1.
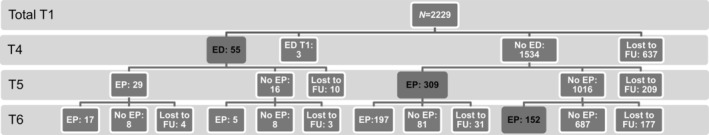
Flow chart eating pathology. Number of participants with eating pathology at each assessment wave. Mean ages: T1 11.1 years, T4 19.1 years, T5 22.3 years, T6 25.7 years. ED = lifetime eating disorder diagnosis; ED T1 = eating disorder diagnosis with an age of onset preceding or being equal to age at T1; EP = eating pathology according to the Eating Disorder Diagnostic Scale (EDDS), an EDDS cut‐off score of 16.5 was used to classify participants with eating pathology. FU = follow‐up. Black: incident eating pathology developed between T1 and T4, between T4 and T5 or between T5 and T6
3.2. Univariate analyses
Table 2 shows the results of the logistic regression analyses examining whether each potential risk indicator was associated with the development of eating pathology. The following variables were consistently significantly associated with an increased risk of eating pathology at T4, T5, and T6: sex, BMI, overeating, reported overweight, negative affectivity, low self‐esteem (both global and physical appearance related), symptoms of anxiety and depressive disorders, and parental overprotection. Next, we investigated which risk factors for eating disorders were sex‐specific in logistic regression analyses including variables' interactions with sex. The results are shown in Table S1. No consistent significant interactions were found.
TABLE 2.
Associations between putative risk factors and lifetime eating disorder diagnoses till T4 or EDDS at T5–T6
| Variable | Lifetime eating disorder diagnoses | EDDS T5 | EDDS T6 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | OR | 95%CI | N | OR | 95%CI | N | OR | 95%CI | |
| Sociodemographic factors | |||||||||
| Sex (female) T1 | 1,589 | 4.6 | 2.2–9.4 | 1,496 | 4.3 | 3.2–5.7 | 1,297 | 4.6 | 3.4–6.1 |
| Socioeconomic status T1 | 1,568 | 0.8 | 0.6–1.1 | 1,476 | 1.1 | 0.9–1.2 | 1,278 | 1.0 | 0.9–1.2 |
| Socioeconomic status T1 — quadratic | 1,568 | 0.8 | 0.6–1.1 | 1,476 | 1.1 | 1.0–1.2 | 1,278 | 1.0 | 0.9–1.1 |
| Ethnicity (minority group) T1 | 1,589 | 2.4 | 1.1–5.1 | 1,496 | 1.2 | 0.7–1.8 | 1,297 | 0.8 | 0.5–1.3 |
| Pregnancy and perinatal factors | |||||||||
| Maternal alcohol use during pregnancy | 1,563 | 0.6 | 0.2–1.4 | 1,475 | 1.1 | 0.8–1.5 | 1,278 | 0.8 | 0.6–1.2 |
| Maternal smoking during pregnancy | 1,564 | 1.0 | 0.5–1.8 | 1,477 | 1.2 | 0.9–1.5 | 1,279 | 1.2 | 0.9–1.6 |
| Maternal problems during pregnancy | 1,565 | 0.9 | 0.5–1.7 | 1,476 | 1.2 | 1.0–1.6 | 1,278 | 1.1 | 0.9–1.4 |
| Maternal dietary adjustments | 1,056 | 0.9 | 0.4–2.3 | 1,009 | 1.4 | 1.0–1.9 | 864 | 1.1 | 0.8–1.6 |
| Maternal age at child's birth | 1,522 | 0.8 | 0.6–1.0 | 1,436 | 1.1 | 1.0–1.2 | 1,248 | 1.0 | 0.9–1.1 |
| Maternal age at child's birth — quadratic | 1,522 | 0.9 | 0.7–1.1 | 1,436 | 1.0 | 0.9–1.1 | 1,248 | 1.0 | 1.0–1.1 |
| Paternal age at child's birth | 1,248 | 0.9 | 0.6–1.2 | 1,179 | 1.1 | 0.9–1.2 | 1,014 | 1.0 | 0.9–1.1 |
| Paternal age at child's birth — quadratic | 1,248 | 0.9 | 0.7–1.2 | 1,179 | 1.0 | 0.9–1.1 | 1,014 | 1.0 | 1.0–1.1 |
| Gestational age | 1,570 | 1.2 | 0.9–1.7 | 1,481 | 1.1 | 1.0–1.2 | 1,283 | 1.0 | 0.9–1.2 |
| Gestational age — quadratic | 1,570 | 0.9 | 0.8–1.1 | 1,481 | 1.0 | 0.9–1.0 | 1,283 | 1.0 | 0.9–1.0 |
| Birth weight | 1,570 | 0.9 | 0.7–1.2 | 1,475 | 1.0 | 0.9–1.1 | 1,279 | 0.9 | 0.8–1.1 |
| Birth weight — quadratic | 1,570 | 0.8 | 0.6–1.1 | 1,475 | 1.0 | 0.9–1.1 | 1,279 | 1.0 | 0.9–1.1 |
| Small for gestational age | 1,547 | 1.0 | 0.4–2.2 | 1,455 | 1.1 | 0.8–1.5 | 1,260 | 1.0 | 0.7–1.4 |
| Large for gestational age | 1,547 | 0.4 | 0.1–1.6 | 1,455 | 1.3 | 0.8–1.9 | 1,260 | 1.1 | 0.7–1.7 |
| Multiple birth | 1,335 | 0 | 0 | 1,255 | 1.6 | 0.8–3.5 | 1,083 | 2.1 | 1.0–4.8 |
| Congenital malformations | 1,582 | 0 | 0 | 1,490 | 1.5 | 0.7–3.3 | 1,291 | 0.6 | 0.2–1.6 |
| Perinatal complications | 1,556 | 0.9 | 0.5–1.6 | 1,467 | 1.1 | 0.8–1.3 | 1,270 | 0.7 | 0.6–0.9 |
| Eating‐ and weight‐related factors | |||||||||
| Eating problems as toddler | 1,581 | 0.8 | 0.4–1.7 | 1,489 | 0.9 | 0.7–1.2 | 1,290 | 0.8 | 0.6–1.0 |
| Food allergy as toddler | 1,556 | 1.3 | 0.5–3.6 | 1,466 | 1.7 | 1.1–2.6 | 1,268 | 1.4 | 0.8–2.2 |
| Undereating T1 | 1,588 | 1.6 | 0.7–3.7 | 1,495 | 0.7 | 0.4–1.1 | 1,296 | 1.0 | 0.7–1.6 |
| Overeating T1 | 1,587 | 5.6 | 2.9–10.7 | 1,494 | 2.8 | 1.8–4.3 | 1,295 | 2.4 | 1.5–3.8 |
| Reported overweight T1 | 1,561 | 5.0 | 2.6–9.8 | 1,473 | 5.7 | 3.7–8.8 | 1,275 | 5.1 | 3.1–8.4 |
| Vomiting T1 | 1,544 | 0 | 0 | 1,453 | 1.1 | 0.4–3.1 | 1,264 | 1.4 | 0.5–3.7 |
| Excessive sport activity T1 | 1,565 | 0.9 | 0.4–2.2 | 1,475 | 0.9 | 0.6–1.4 | 1,277 | 1.0 | 0.7–1.5 |
| Body mass index T1 | 1,549 | 1.9 | 1.4–2.5 | 1,460 | 2.1 | 1.8–2.4 | 1,264 | 1.9 | 1.7–2.2 |
| Body mass index T1 — quadratic | 1,549 | 1.3 | 1.1–1.5 | 1,460 | 1.1 | 1.0–1.2 | 1,264 | 1.1 | 1.0–1.2 |
| Psychological functioning | |||||||||
| Negative affectivity T1 | 1,579 | 1.5 | 1.2–2.0 | 1,490 | 1.4 | 1.2–1.6 | 1,292 | 1.3 | 1.1–1.4 |
| Self‐esteem — global T1 | 1,577 | 0.7 | 0.5–0.9 | 1,486 | 0.7 | 0.6–0.8 | 1,288 | 0.8 | 0.7–0.9 |
| Self‐esteem — physical appearance T1 | 1,577 | 0.5 | 0.4–0.7 | 1,486 | 0.6 | 0.5–0.7 | 1,288 | 0.7 | 0.6–0.8 |
| Alcohol use T1 | 1,572 | 0.7 | 0.4–1.4 | 1,482 | 0.9 | 0.7–1.1 | 1,283 | 0.9 | 0.7–1.1 |
| Generalized anxiety disorder T1 | 1,577 | 1.7 | 1.3–2.1 | 1,486 | 1.4 | 1.3–1.6 | 1,287 | 1.3 | 1.2–1.5 |
| Social phobia T1 | 1,577 | 1.8 | 1.5–2.3 | 1,486 | 1.5 | 1.4–1.7 | 1,287 | 1.6 | 1.4–1.8 |
| Separation anxiety disorder T1 | 1,577 | 1.4 | 1.2–1.8 | 1,486 | 1.3 | 1.2–1.5 | 1,287 | 1.3 | 1.1–1.4 |
| Panic disorder T1 | 1,577 | 1.3 | 1.1–1.7 | 1,486 | 1.3 | 1.1–1.4 | 1,287 | 1.2 | 1.1–1.4 |
| Obsessive–compulsive disorder T1 | 1,576 | 1.5 | 1.2–1.9 | 1,486 | 1.3 | 1.1–1.4 | 1,287 | 1.2 | 1.0–1.3 |
| Major depression disorder T1 | 1,577 | 1.6 | 1.2–2.0 | 1,486 | 1.3 | 1.2–1.5 | 1,287 | 1.2 | 1.1–1.4 |
| Stressful experiences | |||||||||
| Being bullied T1 | 1,565 | 1.9 | 0.7–4.8 | 1,479 | 1.5 | 1.0–2.5 | 1,280 | 1.4 | 0.9–2.4 |
| Adverse events | 1,568 | 1.2 | 0.9–1.5 | 1,475 | 1.0 | 0.9–1.2 | 1,277 | 1.1 | 1.0–1.2 |
| Sexual abuse | 1,403 | 2.1 | 0.5–9.1 | 1,302 | 2.4 | 1.1–5.2 | 1,141 | 1.5 | 0.7–3.3 |
| Family factors | |||||||||
| Parental psychopathology — internalizing | 1,533 | 1.0 | 0.6–1.7 | 1,444 | 1.3 | 1.1–1.7 | 1,253 | 1.2 | 1.0–1.6 |
| Parental psychopathology — externalizing | 1,530 | 1.7 | 0.9–3.5 | 1,442 | 1.2 | 0.8–1.8 | 1,250 | 0.8 | 0.5–1.2 |
| Perceived parental warmth T1 | 1,576 | 0.9 | 0.7–1.1 | 1,486 | 1.1 | 1.0–1.2 | 1,286 | 1.2 | 1.1–1.4 |
| Perceived parental warmth T1 — quadratic | 1,576 | 1.1 | 1.0–1.3 | 1,486 | 0.9 | 0.9–1.0 | 1,286 | 1.0 | 0.9–1.1 |
| Perceived parental rejection T1 | 1,575 | 1.2 | 1.0–1.5 | 1,486 | 1.1 | 1.0–1.3 | 1,286 | 1.1 | 1.0–1.2 |
| Perceived parental rejection T1 — quadratic | 1,575 | 1.0 | 0.9–1.1 | 1,486 | 1.0 | 1.0–1.0 | 1,286 | 1.0 | 1.0–1.1 |
| Perceived parental overprotection T1 | 1,575 | 1.4 | 1.1–1.8 | 1,485 | 1.3 | 1.1–1.4 | 1,285 | 1.2 | 1.1–1.4 |
| Perceived parental overprotection T1 — quadratic | 1,575 | 1.0 | 0.8–1.2 | 1,485 | 1.1 | 1.0–1.1 | 1,285 | 1.0 | 0.9–1.1 |
Note: If the 95% confidence interval for an OR includes 1, the results are not statistically significant. Bold: p < .05. Mean ages: T1 11.1 years, T4 19.1 years, T5 22.3 years, T6 25.7 years.
Abbreviation: EDDS, Eating Disorder Diagnostic Scale.
3.3. Multivariate analyses
Risk factors with consistent significant univariate effects for eating pathology at T4, T5, and T6 were included in the multivariate logistic regression models. Results of the models with forward stepwise selection are shown in Table 3. The variables sex, BMI, overeating and anxiety symptoms were consistently identified as unique predictors of eating pathology at T4, T5, and T6. Depending on the model, symptoms of either generalized anxiety disorder (GAD) or social phobia (SP) (r = 0.57) or both disorders showed unique predictive effects. Negative affectivity and self‐perceptions regarding physical appearance were only found to be unique predictors for eating pathology at T5. These variables were moderately correlated with GAD (negative affectivity: r = 0.38; physical appearance: r = −0.26) and SP (negative affectivity: r = 0.38; physical appearance: r = −0.36). Reported overweight (correlated with overeating: r = 0.34) was identified as unique predictor for eating pathology at T6. The results of the models with backward stepwise selection were comparable to those shown in Table 3, with one exception: instead of SP, symptoms of GAD (OR 1.2; 95% CI 1.1–1.4) were found to be a significant predictor of eating pathology at T5 in the case of backward stepwise selection. The results of multivariate analyses with participants without eating pathology at T1 (results available in Table S2) were also comparable to those presented in Table 3, and so were the findings of the multivariate analyses with imputed data (n = 2,229), except for eating pathology at T4: symptoms of either GAD or SP (instead of both; as shown in Table 3) were found to be a significant predictor using the imputed data (Table S3).
TABLE 3.
Multivariate associations between putative risk factors and lifetime eating disorder diagnoses till T4 or EDDS at T5–T6
| Variable | Lifetime eating disorder diagnoses | EDDS T5 | EDDS T6 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | OR | 95%CI | N | OR | 95%CI | N | OR | 95%CI | |
| Sex (female) T1 | 1,513 | 4.3 | 2.0–9.1 | 1,433 | 4.3 | 3.1–5.8 | 1,240 | 4.4 | 3.2–6.0 |
| Overeating T1 | 4.0 | 1.9–8.3 | 1.8 | 1.1–3.1 | |||||
| Reported overweight T1 | 2.0 | 1.1–3.5 | |||||||
| Body mass index T1 | 1.7 | 1.3–2.4 | 2.0 | 1.7–2.3 | 2.0 | 1.7–2.4 | |||
| Negative affectivity T1 | 1.2 | 1.0–1.4 | |||||||
| Self‐esteem — physical appearance T1 | 0.8 | 0.7–0.9 | |||||||
| Generalized anxiety disorder T1 | 1.4 | 1.0–1.9 | |||||||
| Social phobia T1 | 1.4 | 1.0–1.9 | 1.2 | 1.0–1.4 | 1.4 | 1.2–1.6 | |||
Note: Results of the models with forward stepwise selection. All effects significant. Mean ages: T1 11.1 years, T4 19.1 years, T5 22.3 years, T6 25.7 years.
Abbreviation: EDDS, Eating Disorder Diagnostic Scale.
Table 4 presents the results of analyses after excluding participants with eating pathology at previous assessment waves. Compared to the results shown in Table 3 regarding all participants with eating pathology, overeating was not a unique predictor of eating pathology at T5 and T6 in these analyses including only participants with new developed eating pathology. Also, the results for incident eating pathology between T4 and T5 differed somewhat from what is presented in Table 3: parental overprotection (not negative affectivity, r = 0.29) and symptoms of GAD (not SP, r = 0.57) were identified as unique predictors.
TABLE 4.
Multivariate associations between putative risk factors and incident eating pathology at T4–T6
| Variable | Lifetime eating disorder diagnoses | EDDS T5 | EDDS T6 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | OR | 95%CI | N | OR | 95%CI | N | OR | 95%CI | |
| Sex (female) T1 | 1,513 | 4.3 | 2.0–9.1 | 1,268 | 4.7 | 3.3–6.6 | 803 | 3.3 | 2.2–5.0 |
| Overeating T1 | 4.0 | 1.9–8.3 | |||||||
| Body mass index T1 | 1.7 | 1.3–2.4 | 2.0 | 1.7–2.4 | 1.8 | 1.5–2.3 | |||
| Self‐esteem — physical appearance T1 | 0.7 | 0.6–0.9 | |||||||
| Generalized anxiety disorder T1 | 1.4 | 1.0–1.9 | 1.3 | 1.1–1.5 | |||||
| Social phobia T1 | 1.4 | 1.0–1.9 | 1.4 | 1.1–1.7 | |||||
| Perceived parental overprotection T1 | 1.3 | 1.1–1.5 | |||||||
Note: Results of the models with forward stepwise selection. All effects significant. Mean ages: T1 11.1 years, T4 19.1 years, T5 22.3 years, T6 25.7 years.
Abbreviation: EDDS, Eating Disorder Diagnostic Scale.
4. DISCUSSION
This study investigated risk factors in preadolescent boys and girls for the development of eating pathology in adolescence and young adulthood. Data were drawn from TRAILS (Oldehinkel et al., 2015), which follows a large community sample from preadolescence into young adulthood. We found that female sex, high weight, and high anxious distress in preadolescence were consistently associated with the development of eating pathology in adolescence and young adulthood. Contrary to our expectations, we found no evidence for sex‐specific risk factors. Our findings indicate that being a female is — as known — a risk factor for eating pathology, but that both boys and girls with high weight and anxious distress are at increased risk for the development of eating pathology during adolescence. Overeating during preadolescence also predicted the development of clinical eating disorders in adolescence and could be interpreted as a prodromal eating disorder symptom. It is of note that the observed effects were small in magnitude, but very consistent, both over a long time and with use of different eating pathology measurements.
The observed relation between anxious distress and eating pathology was also found in previous studies (Fulton et al., 2012; Schaumberg et al., 2019). Our study adds to the small body of prospective research, that anxious distress in preadolescence has a long‐lasting effect on the development of eating pathology, still manifest after 15 years of follow‐up. Although anxious distress in preadolescence has previously mainly been described as a risk factor for affective disorders in later life (Hirshfeld‐Becker, Micco, Simoes, & Henin, 2008), our study shows that it acts as a warning signal for eating pathology too. Symptoms of generalized anxiety and social phobia were most strongly associated with the development of eating pathology in our study, although other factors related to these symptoms (like negative affectivity, parental overprotection, low‐self‐esteem and symptoms of obsessive–compulsive disorder) seemed to be important as well, but lost significance in multivariate models. It has been argued that individuals with high generalized anxiety (i.e., proneness to internalize fears) and individuals with high anxiety related to social evaluation are more likely to develop weight and shape concerns than individuals with low anxiety levels, especially in combination with sociocultural pressure to be thin (Schaumberg et al., 2019). Disordered eating could develop in order to cope with fears and worries. Dietary restriction and overeating are coping mechanisms with an anxiolytic effect, providing negative reinforcement and ultimately leading to high risk for development of eating pathology (Kaye, 2008). Eating pathology prevention programs have mainly focused on body dissatisfaction (Stice et al., 2019) and have neglected anxious distress. Given the long‐lasting effect of anxious distress on the development of eating pathology it seems relevant to target these symptoms in eating pathology prevention programs for preadolescents.
Although we found that high weight in preadolescence is prospectively associated with eating pathology, the literature on this is ambiguous (Evans et al., 2017; Jacobi et al., 2004; Rohde et al., 2015; Stice, Presnell, & Spangler, 2002). It has been argued that objective body weight is one of the causes of subjective body dissatisfaction and that the latter is a main risk factor for eating pathology (Stice, 2002). Low appearance‐related self esteem was also a significant predictor of eating pathology in our study, but in multivariate models this factor lost significance in benefit of high weight and anxiety. It is conceivable that high weight could induce unhealthy compensating strategies to manage weight — probably mediated by body dissatisfaction —, especially in individuals with high anxious distress. This could lead to the development of eating pathology. Other studies showed underweight to be a specific risk factor for the development of anorexia nervosa (Stice et al., 2017), but underweight (BMI z‐score < 0) was not found to be a risk factor for eating pathology in our study. Future studies should focus on the pathways and mediating roles of body weight, anxious distress and body dissatisfaction in order to unravel targets for prevention.
In line with Stice et al. (2017), overeating was found to predict eating pathology. It is difficult to distinguish between overeating as a risk factor and overeating as an early symptom of an eating disorder. Prodromal symptoms could serve as predictors for the development of full eating disorder syndromes (Jacobi et al., 2004). Moreover, the selection criteria for the diagnostic eating disorder interview administered at late adolescence included overeating (Smink et al., 2014). Our study suggests that overeating in preadolescence is predominantly a prodromal symptom of eating pathology during late adolescence, since it was not associated with incident eating pathology later in life. Nevertheless, our findings imply that overeating could be targeted (e.g., by interventions that increase self‐control; Duckworth, Tsukayama, & Geier, 2010) in selective prevention programs to prevent the development of full‐blown eating disorders.
In accordance with the eating disorder literature (Jacobi et al., 2004), we found being a female was the most potent risk factor for eating pathology, supported by the greater prevalence rates of eating pathology in comparison to males. In contrast to our expectations, we did not identify sex‐specific risk factors. This may be due to the relatively small number of participants with a formal eating disorder diagnosis. While previous studies found depressive symptoms (Ferreiro, Seoane, & Senra, 2012) and high socioeconomic status (Raevuori et al., 2014) to be female‐specific risk factors, we were not able to replicate these results. This could be explained by the use of measures that covered partly different elements of socioeconomic status (income, educational and occupational level) in comparison to other studies. For the prospective effect of depressive symptoms on eating pathology, sex differences have been reported to emerge around age 13 (Evans et al., 2017; Ferreiro et al., 2012). This may explain the absence of sex‐specific effects of depressive symptoms identified at age 11 in our study. Moreover, the EDDS has not been validated in males, so our results should be interpreted with caution. However, our finding of similar risk factors for eating disorder diagnoses in males and females underscores the need for the development of sex‐neutral prevention programs.
Previous studies that specifically focused on one risk factor domain, like pregnancy factors, usually had larger samples sizes (Larsen et al., 2020; Watson et al., 2019) than our study. Therefore, it is not surprising that we did not replicate all significant associations. However, this does not mean that such associations are absent. Especially for sexual abuse and being bullied, the positive effects at the different measurement waves were comparable to previously reported effect sizes (Molendijk, Hoek, Brewerton, & Elzinga, 2017). In our study the numbers of cases with a history of sexual abuse or being bullied were low and this hampered the power to detect significant differences. Nevertheless, our findings support the need for further research into these stressful experiences and eating pathology among both males and females.
4.1. Strengths and limitations
Our study has a number of strengths, including its large community‐based sample with both males and females, and its longitudinal design covering 15 years of follow‐up from preadolescence into young adulthood. Response rates remained relatively high over the subsequent assessment waves. We used objective measures (BMI), self‐reported data as well as data from other informants (parents and Preventive Child Healthcare). Formal eating disorder diagnoses were assessed by experts using diagnostic interviews. Because a wide range of variables was measured in preadolescence, that is, before the high‐risk period for eating disorder onset, we could prospectively assess their status as a risk factor for eating pathology.
There are also several limitations to consider. The first lies in the use of the cut‐off score of the EDDS of Krabbenborg et al. (2012). This cut‐off score has the advantage over continuous scores of classifying participants with (high risk of) eating pathology. However, it is unclear whether this cut‐off score is generalizable to our general population cohort. We found a mean EDDS score of 12.1 (T5: n 1,496; SD 15.3), whereas Krabbenborg reported a mean EDDS score of 7.2 (n 45; SD 6.6) in their female sample selected for absence of eating pathology. The use of this cut‐off score could have led to overestimation of eating pathology in our community sample, but for the purposes of our study — to identify subgroups at high risk for the development of eating pathology — this is not a major concern. High eating pathology scores have been found to predict even higher scores later in life (Evans et al., 2017). Furthermore, our EDDS findings were comparable to those of the eating disorder diagnoses.
A second limitation is that the EDDS has not been validated in males, which unfortunately applies to many eating disorder instruments (Raevuori et al., 2014). As eating disorder symptoms vary by sex (e.g., muscle dysmorphia in males), the use of a questionnaire that has only been developed and validated in females could have led to underestimation of eating pathology in males. We would advise to use a reliable and valid eating pathology measure for males in future studies. It is conceivable that the use of such an instrument in risk factor research will elucidate male‐specific risk factors.
Another limitation is that the number of participants with a formal eating disorder diagnosis was low in our sample, which (a) restricted the statistical power to detect small differences, and (b) did not allow analyses per eating disorder diagnostic group. Moreover, the EDDS measures the overall level of eating pathology, not specific types of problems. We were therefore not able to examine whether specific eating disorders have specific risk factors. However, we consider our combined analyses of symptoms and eating disorder groups valid in the light of the transdiagnostic approach, which states that eating disorders share the same psychopathology (Fairburn & Cooper, 2011). Furthermore, we used different eating pathology instruments at different measurement waves (interview or questionnaire), because data collection budgets varied over time. Besides, since no validated measure of eating pathology at T1 was available, proxies of core characteristics of eating disorders were used to correct for initial eating problems. This could have led to both under‐ or overcorrection for eating pathology at T1, and thus overestimation and underestimation of the actual relations between putative risk factors and later eating pathology. It will be necessary in future longitudinal studies to use a single, reliable and valid eating pathology measure for all measurement waves.
There are also some limitations in the assessment of putative risk factors to mention. Sexual abuse was only assessed retrospectively at T4. Although we asked for age at time of the experience, recall bias could have influenced the results. Furthermore, our sport activity measure is not a validated construct, but gives an indication of excessive physical activity. This should be kept in mind when interpreting our results.
Finally, our sample includes predominantly Caucasian children, but we suspect that our findings are generalizable to children in areas with different sociodemographic constitutions. We think it is unlikely that cultural influences would strongly bias the associations between risk factors and eating pathology measured in our study.
5. CONCLUSION
Our study suggests that anxious distress and high weight in preadolescent boys and girls predict eating pathology in adolescence and young adulthood. Our findings imply that clinicians should be aware of, and screen for eating disorder symptoms (e.g., with the SCOFF; Morgan, Reid, & Lacey, 1999) among anxious children with high weight, especially among girls. The presence of overeating in this high‐risk group of children could function as an alert for early intervention to prevent the development of full‐blown eating disorders. Future research into selective targeted prevention programs for eating disorders is best directed at preadolescents characterized by anxious distress and high weight.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
Supporting information
AppendixS1. Supporting Information.
ACKNOWLEDGMENTS
We thank Dennis Raven for help with data management, Mathijs Deen for help with statistical analyses and Judith Offringa‐Rodenburg for editing the manuscript. This research is part of the TRacking Adolescents' Individual Lives Survey (TRAILS). Participating centers of TRAILS include the University Medical Center and University of Groningen, the University of Utrecht, the Radboud Medical Center Nijmegen, and Parnassia Psychiatric Institute, all in the Netherlands. TRAILS has been financially supported by various grants from the Netherlands Organization for Scientific Research NWO (Medical Research Council program grant GB‐MW 940‐38‐011; ZonMW Brainpower grant 100‐001‐004; ZonMw Risk Behavior and Dependence grants 60‐60600‐97‐118; ZonMw Culture and Health grant 261‐98‐710; Social Sciences Council medium‐sized investment grants GB‐MaGW 480‐01‐006 and GB‐MaGW 480‐07‐001; Social Sciences Council project grants GB‐MaGW 452‐04‐314 and GB‐MaGW 452‐06‐004; NWO large‐sized investment grant 175.010.2003.005; NWO Longitudinal Survey and Panel Funding 481‐08‐013 and 481‐11‐001; NWO Vici 016.130.002 and 453‐16‐007/2735; NWO Gravitation 024.001.003), the Dutch Ministry of Justice (WODC), the European Science Foundation (EuroSTRESS project FP‐006), the European Research Council (ERC‐2017‐STG‐757364 and ERC‐CoG‐2015‐681466), Biobanking and Biomolecular Resources Research Infrastructure BBMRI‐NL (CP 32), the Gratama foundation, the Jan Dekker foundation, the participating universities, and Accare Centre for Child and Adolescent Psychiatry. We are grateful to everyone who participated in this research or worked on this project to make it possible.
van Eeden AE, Oldehinkel AJ, van Hoeken D, Hoek HW. Risk factors in preadolescent boys and girls for the development of eating pathology in young adulthood. Int J Eat Disord. 2021;54:1147–1159. 10.1002/eat.23496
Action Editor: Ruth Weissman
Funding information Nederlandse Organisatie voor Wetenschappelijk Onderzoek, Grant/Award Numbers: 100‐001‐004, 175.010.2003.005, 481‐08‐013, 481‐11‐001, 60‐60600‐97‐118, 261‐98‐710, GB‐MW 940‐38‐011, GB‐MaGW 480‐01‐006, GB‐MaGW 480‐07‐001, GB‐MaGW 452‐04‐314, GB‐MaGW 452‐06‐004, 016.130.002, 453‐16‐007/2735, 024.001.003; Accare Centre for Child and Adolescent Psychiatry; Jan Dekker foundation; Gratama foundation; Biobanking and Biomolecular Resources Research Infrastructure BBMRI‐NL, Grant/Award Number: CP 32; European Research Council, Grant/Award Numbers: ERC‐CoG‐2015‐681466, ERC‐2017‐STG‐757364; European Science Foundation, Grant/Award Number: EuroSTRESS project FP‐006; Dutch Ministry of Justice (WODC); University Medical Center Groningen University of Utrecht Radboud Medical Center Nijmegen Parnassia Psychiatric Institute
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on reasonable request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school‐age forms and profiles. Burlington, VT: University of Vermont Research Center for Children, Youth, & Families. www.aseba.org. [Google Scholar]
- Ahren, J. C., Chiesa, F., Koupil, I., Magnusson, C., Dalman, C., & Goodman, A. (2013). We are family—parents, siblings, and eating disorders in a prospective total‐population study of 250,000 Swedish males and females. International Journal of Eating Disorders, 46(7), 693–700. 10.1002/eat.22146 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Bonvanie, I. J., van Gils, A., Janssens, K. A., & Rosmalen, J. G. (2015). Sexual abuse predicts functional somatic symptoms: An adolescent population study. Child Abuse & Neglect, 46, 1–7. 10.1016/j.chiabu.2015.06.001 [DOI] [PubMed] [Google Scholar]
- Chorpita, B. F., Yim, L., Moffitt, C., Umemoto, L. A., & Francis, S. E. (2000). Assessment of symptoms of DSM‐IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy, 38(8), 835–855. 10.1016/s0005-7967(99)00130-8 [DOI] [PubMed] [Google Scholar]
- Culbert, K. M., Racine, S. E., & Klump, K. L. (2015). Research review: What we have learned about the causes of eating disorders—A synthesis of sociocultural, psychological, and biological research. Journal of Child Psychology and Psychiatry, 56(11), 1141–1164. 10.1111/jcpp.12441 [DOI] [PubMed] [Google Scholar]
- de Onis, M., Onyango, A. W., Borghi, E., Siyam, A., Nishida, C., & Siekmann, J. (2007). Development of a WHO growth reference for school‐aged children and adolescents. Bulletin of the World Health Organization, 85(9), 660–667. https://www.ncbi.nlm.nih.gov/pubmed/18026621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Winter, A. F., Oldehinkel, A. J., Veenstra, R., Brunnekreef, J. A., Verhulst, F. C., & Ormel, J. (2005). Evaluation of non‐response bias in mental health determinants and outcomes in a large sample of pre‐adolescents. European Journal of Epidemiology, 20(2), 173–181. https://www.ncbi.nlm.nih.gov/pubmed/15792285 [DOI] [PubMed] [Google Scholar]
- Dominy, N. L., Johnson, W. B., & Koch, C. (2000). Perception of parental acceptance in women with binge eating disorder. Journal of Psychology, 134(1), 23–36. 10.1080/00223980009600846 [DOI] [PubMed] [Google Scholar]
- Duckworth, A. L., Tsukayama, E., & Geier, A. B. (2010). Self‐controlled children stay leaner in the transition to adolescence. Appetite, 54(2), 304–308. 10.1016/j.appet.2009.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis, L. K. (2002). Individual differences and adolescent psychosocial development. Eugene, OR: University of Oregon. [Google Scholar]
- Evans, E. H., Adamson, A. J., Basterfield, L., Le Couteur, A., Reilly, J. K., Reilly, J. J., & Parkinson, K. N. (2017). Risk factors for eating disorder symptoms at 12 years of age: A 6‐year longitudinal cohort study. Appetite, 108, 12–20. 10.1016/j.appet.2016.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn, C. G., & Cooper, Z. (2011). Eating disorders, DSM‐5 and clinical reality. British Journal of Psychiatry, 198(1), 8–10. 10.1192/bjp.bp.110.083881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn, C. G., Cooper, Z., & O'Connor, M. E. (2008). Eating Disorder Examination (Edition 16.0 D). In Fairburn C. G. (Ed.), Cognitive behavior therapy and eating disorders (pp. 265–308). New York: Guilford Press. [Google Scholar]
- Ferreiro, F., Seoane, G., & Senra, C. (2012). Gender‐related risk and protective factors for depressive symptoms and disordered eating in adolescence: A 4‐year longitudinal study. Journal of Youth and Adolescence, 41(5), 607–622. 10.1007/s10964-011-9718-7 [DOI] [PubMed] [Google Scholar]
- First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (1995). Structured clinical interview for DSM‐IV axis I disorders‐patient edition (SCID‐I/P, version 2.0). New York: Biometrics Research Department, New York State Psychiatric Institute. [Google Scholar]
- Fulton, J. J., Lavender, J. M., Tull, M. T., Klein, A. S., Muehlenkamp, J. J., & Gratz, K. L. (2012). The relationship between anxiety sensitivity and disordered eating: The mediating role of experiential avoidance. Eating Behaviors, 13(2), 166–169. 10.1016/j.eatbeh.2011.12.003 [DOI] [PubMed] [Google Scholar]
- Ganzeboom, H. B. G., & Treiman, D. J. (1996). Internationally comparable measures of occupational status for the 1988 international standard classification of occupations. Social Science Research, 25(3), 201–239. [Google Scholar]
- Groenestijn, M. A. C. V., Akkerhuis, G. W., Kupka, R. W., Schneider, N., & Nolen, W. A. (1998). SCID‐I Gestructureerd Klinisch Interview voor de vaststelling van DSM‐IV stoornissen (in Dutch). Lisse: Swets and Zeitlinger. [Google Scholar]
- Harter, S. (1982). The perceived competence scale for children. Child Development, 53, 87–97. [PubMed] [Google Scholar]
- Hartman, C. A. (2000). Dutch translation of the early adolescent temperament questionnaire. Groningen: University Medical Center Groningen, Department of Psychiatry (Internal Report). [Google Scholar]
- Hirshfeld‐Becker, D. R., Micco, J. A., Simoes, N. A., & Henin, A. (2008). High risk studies and developmental antecedents of anxiety disorders. American Journal of Medical Genetics. Part C, Seminars in Medical Genetics, 148C(2), 99–117. 10.1002/ajmg.c.30170 [DOI] [PubMed] [Google Scholar]
- Hoftiezer, L., Hof, M. H. P., Dijs‐Elsinga, J., Hogeveen, M., Hukkelhoven, C. W. P. M., & van Lingen, R. A. (2019). From population reference to national standard: New and improved birthweight charts. American Journal of Obstetrics and Gynecology, 220(4), 383 e381‐383 e317. 10.1016/j.ajog.2018.12.023 [DOI] [PubMed] [Google Scholar]
- Hoftiezer, L., Hukkelhoven, C. W., Hogeveen, M., Straatman, H. M., & van Lingen, R. A. (2016). Defining small‐for‐gestational‐age: Prescriptive versus descriptive birthweight standards. European Journal of Pediatrics, 175(8), 1047–1057. 10.1007/s00431-016-2740-8 [DOI] [PubMed] [Google Scholar]
- Iwajomo, T., Bondy, S. J., de Oliveira, C., Colton, P., Trottier, K., & Kurdyak, P. (2020). Excess mortality associated with eating disorders: Population‐based cohort study. British Journal of Psychiatry, 1–7. 10.1192/bjp.2020.197 [DOI] [PubMed] [Google Scholar]
- Jacobi, C., Fittig, E., Bryson, S. W., Wilfley, D., Kraemer, H. C., & Taylor, C. B. (2011). Who is really at risk? Identifying risk factors for subthreshold and full syndrome eating disorders in a high‐risk sample. Psychological Medicine, 41(9), 1939–1949. 10.1017/S0033291710002631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi, C., Hayward, C., de Zwaan, M., Kraemer, H. C., & Agras, W. S. (2004). Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin, 130(1), 19–65. 10.1037/0033-2909.130.1.19 [DOI] [PubMed] [Google Scholar]
- Johnson, J. G., Cohen, P., Kasen, S., & Brook, J. S. (2002). Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood. American Journal of Psychiatry, 159(3), 394–400. 10.1176/appi.ajp.159.3.394 [DOI] [PubMed] [Google Scholar]
- Kaye, W. (2008). Neurobiology of anorexia and bulimia nervosa. Physiology & Behavior, 94(1), 121–135. 10.1016/j.physbeh.2007.11.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killen, J. D., Taylor, C. B., Hayward, C., Haydel, K. F., Wilson, D. M., Hammer, L., … Strachowski, D. (1996). Weight concerns influence the development of eating disorders: A 4‐year prospective study. Journal of Consulting and Clinical Psychology, 64(5), 936–940. 10.1037//0022-006x.64.5.936 [DOI] [PubMed] [Google Scholar]
- Kotler, L. A., Cohen, P., Davies, M., Pine, D. S., & Walsh, B. T. (2001). Longitudinal relationships between childhood, adolescent, and adult eating disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 40(12), 1434–1440. 10.1097/00004583-200112000-00014 [DOI] [PubMed] [Google Scholar]
- Krabbenborg, M. A., Danner, U. N., Larsen, J. K., van der Veer, N., van Elburg, A. A., de Ridder, D. T., … Engels, R. C. (2012). The eating disorder diagnostic scale: Psychometric features within a clinical population and a cut‐off point to differentiate clinical patients from healthy controls. European Eating Disorders Review, 20(4), 315–320. 10.1002/erv.1144 [DOI] [PubMed] [Google Scholar]
- Larsen, J. T., Bulik, C. M., Thornton, L. M., Koch, S. V., & Petersen, L. (2020). Prenatal and perinatal factors and risk of eating disorders. Psychological Medicine, 1–11. 10.1017/S0033291719003945 [DOI] [PubMed] [Google Scholar]
- Marchi, M., & Cohen, P. (1990). Early childhood eating behaviors and adolescent eating disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 29(1), 112–117. 10.1097/00004583-199001000-00017 [DOI] [PubMed] [Google Scholar]
- Markus, M. T., Lindhout, I. E., Boer, F., Hoogendijk, T. H. G., & Arrindell, W. A. (2003). Factors of perceived parental rearing styles: The EMBU‐C examined in a sample of Dutch primary school children. Personality and Individual Differences, 34(3), 503–519. [Google Scholar]
- McClelland, J., Robinson, L., Potterton, R., Mountford, V., & Schmidt, U. (2020). Symptom trajectories into eating disorders: A systematic review of longitudinal, nonclinical studies in children/adolescents. European Psychiatry: The Journal of the Association of European Psychiatrists, 63(1), e60. 10.1192/j.eurpsy.2020.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micali, N., De Stavola, B., Ploubidis, G., Simonoff, E., Treasure, J., & Field, A. E. (2015). Adolescent eating disorder behaviours and cognitions: Gender‐specific effects of child, maternal and family risk factors. British Journal of Psychiatry, 207(4), 320–327. 10.1192/bjp.bp.114.152371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt, T. E., & Silva, P. A. (1988). Self‐reported delinquency: Results from an instrument for New Zealand. Australian & New Zealand Journal of Criminology, 21(4), 227–240. [Google Scholar]
- Molendijk, M. L., Hoek, H. W., Brewerton, T. D., & Elzinga, B. M. (2017). Childhood maltreatment and eating disorder pathology: A systematic review and dose‐response meta‐analysis. Psychological Medicine, 47, 1–15. 10.1017/S0033291716003561 [DOI] [PubMed] [Google Scholar]
- Morgan, J. F., Reid, F., & Lacey, J. H. (1999). The SCOFF questionnaire: Assessment of a new screening tool for eating disorders. British Medical Journal, 319(7223), 1467–1468. 10.1136/bmj.319.7223.1467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris, P., Meesters, C., & Fijen, P. (2003). The self‐perception profile for children: Further evidence for its factor structure, reliability, and validity. Personality and Individual Differences, 35(8), 1791–1802. [Google Scholar]
- Oldehinkel, A. J., Rosmalen, J. G., Buitelaar, J. K., Hoek, H. W., Ormel, J., Raven, D., … Hartman, C. A. (2015). Cohort profile update: The TRacking Adolescents' individual lives survey (TRAILS). International Journal of Epidemiology, 44(1), 76‐76n. 10.1093/ije/dyu225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam, S. P., Ellis, L. K., & Rothbart, M. K. (2001). The structure of temperament from infancy through adolescence. Advances in Research on Temperament, 165, 182. [Google Scholar]
- Raevuori, A., Keski‐Rahkonen, A., & Hoek, H. W. (2014). A review of eating disorders in males. Current Opinion in Psychiatry, 27(6), 426–430. 10.1097/YCO.0000000000000113 [DOI] [PubMed] [Google Scholar]
- Ranta, K., Vaananen, J., Frojd, S., Isomaa, R., Kaltiala‐Heino, R., & Marttunen, M. (2017). Social phobia, depression and eating disorders during middle adolescence: Longitudinal associations and treatment seeking. Nordic Journal of Psychiatry, 71(8), 605–613. 10.1080/08039488.2017.1366548 [DOI] [PubMed] [Google Scholar]
- Rohde, P., Stice, E., & Marti, C. N. (2015). Development and predictive effects of eating disorder risk factors during adolescence: Implications for prevention efforts. International Journal of Eating Disorders, 48(2), 187–198. 10.1002/eat.22270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaumberg, K., Zerwas, S., Goodman, E., Yilmaz, Z., Bulik, C. M., & Micali, N. (2019). Anxiety disorder symptoms at age 10 predict eating disorder symptoms and diagnoses in adolescence. Journal of Child Psychology and Psychiatry, 60(6), 686–696. 10.1111/jcpp.12984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoebridge, P., & Gowers, S. G. (2000). Parental high concern and adolescent‐onset anorexia nervosa. A case‐control study to investigate direction of causality. British Journal of Psychiatry, 176, 132–137. 10.1192/bjp.176.2.132 [DOI] [PubMed] [Google Scholar]
- Smink, F. R., van Hoeken, D., Oldehinkel, A. J., & Hoek, H. W. (2014). Prevalence and severity of DSM‐5 eating disorders in a community cohort of adolescents. International Journal of Eating Disorders, 47(6), 610–619. 10.1002/eat.22316 [DOI] [PubMed] [Google Scholar]
- Smolak, L., & Murnen, S. K. (2002). A meta‐analytic examination of the relationship between child sexual abuse and eating disorders. International Journal of Eating Disorders, 31(2), 136–150. 10.1002/eat.10008 [DOI] [PubMed] [Google Scholar]
- Stice, E. (2002). Risk and maintenance factors for eating pathology: A meta‐analytic review. Psychological Bulletin, 128(5), 825–848. 10.1037/0033-2909.128.5.825 [DOI] [PubMed] [Google Scholar]
- Stice, E., Fisher, M., & Martinez, E. (2004). Eating disorder diagnostic scale: Additional evidence of reliability and validity. Psychological Assessment, 16(1), 60–71. 10.1037/1040-3590.16.1.60 [DOI] [PubMed] [Google Scholar]
- Stice, E., Gau, J. M., Rohde, P., & Shaw, H. (2017). Risk factors that predict future onset of each DSM‐5 eating disorder: Predictive specificity in high‐risk adolescent females. Journal of Abnormal Psychology, 126(1), 38–51. 10.1037/abn0000219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice, E., Johnson, S., & Turgon, R. (2019). Eating disorder prevention. Psychiatric Clinics of North America, 42(2), 309–318. 10.1016/j.psc.2019.01.012 [DOI] [PubMed] [Google Scholar]
- Stice, E., Presnell, K., & Spangler, D. (2002). Risk factors for binge eating onset in adolescent girls: A 2‐year prospective investigation. Health Psychology, 21(2), 131–138. https://www.ncbi.nlm.nih.gov/pubmed/11950103 [PubMed] [Google Scholar]
- Stice, E., & Shaw, H. E. (2002). Role of body dissatisfaction in the onset and maintenance of eating pathology: A synthesis of research findings. Journal of Psychosomatic Research, 53(5), 985–993. 10.1016/s0022-3999(02)00488-9 [DOI] [PubMed] [Google Scholar]
- Stice, E., Telch, C. F., & Rizvi, S. L. (2000). Development and validation of the Eating Disorder Diagnostic Scale: A brief self‐report measure of anorexia, bulimia, and binge‐eating disorder. Psychological Assessment, 12(2), 123–131. https://www.ncbi.nlm.nih.gov/pubmed/10887758 [DOI] [PubMed] [Google Scholar]
- Suokas, J. T., Suvisaari, J. M., Gissler, M., Lofman, R., Linna, M. S., Raevuori, A., & Haukka, J. (2013). Mortality in eating disorders: A follow‐up study of adult eating disorder patients treated in tertiary care, 1995‐2010. Psychiatry Research, 210(3), 1101–1106. 10.1016/j.psychres.2013.07.042 [DOI] [PubMed] [Google Scholar]
- van Eeden, A. E., Hoek, H. W., van Hoeken, D., Deen, M., & Oldehinkel, A. J. (2020). Temperament in preadolescence is associated with weight and eating pathology in young adulthood. International Journal of Eating Disorders, 53(5), 466–475. 10.1002/eat.23241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hoeken, D., & Hoek, H. W. (2020). Review of the burden of eating disorders: Mortality, disability, costs, quality of life, and family burden. Current Opinion in Psychiatry, 33(6), 521–527. 10.1097/YCO.0000000000000641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson, H. J., Diemer, E. W., Zerwas, S., Gustavson, K., Knudsen, G. P., Torgersen, L., … Bulik, C. M. (2019). Prenatal and perinatal risk factors for eating disorders in women: A population cohort study. International Journal of Eating Disorders, 52(6), 643–651. 10.1002/eat.23073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- West, C. E., Goldschmidt, A. B., Mason, S. M., & Neumark‐Sztainer, D. (2019). Differences in risk factors for binge eating by socioeconomic status in a community‐based sample of adolescents: Findings from project EAT. International Journal of Eating Disorders, 52(6), 659–668. 10.1002/eat.23079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (2007). Growth reference data for 5–19 years; BMI‐for‐age (5– 19 years). https://www.who.int/toolkits/growth-reference-data-for-5to19-years/indicators/bmi-for-age.
- Wonderlich, S. A., Bulik, C. M., Schmidt, U., Steiger, H., & Hoek, H. W. (2020). Severe and enduring anorexia nervosa: Update and observations about the current clinical reality. International Journal of Eating Disorders, 53(8), 1303–1312. 10.1002/eat.23283 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
AppendixS1. Supporting Information.
Data Availability Statement
The data that support the findings of this study are available on reasonable request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


